Abstract
Purpose
The family caregiver's role is an important influence factor of patient's adaptation behaviour and quality of life after stroke. The purpose of this research was to identify the effect of caregiver empowerment program based on the adaptation model (CEP-BAM) on functional capacity and quality of life of patients after stroke.
Methods
This research was a quasi-experimental research with a pre- and post-test control group design. The total participants who completed the research were 80 patients and their families, 40 participants in the intervention group and 40 participants in the control group. We conducted home visits to perform the intervention. The measurement of functional capacity and quality of life performed four times (pre-test and three times post-test). Data analysis was performed using the repeated measurement ANOVA or general linear model repeated measure (GLM-RM).
Results
This research proves a significant difference in functional capacity and quality of life between the two groups and between pre-test and sixth months after intervention (P < 0.05). The quality of life of the intervention group in the sixth month after intervention was better than that of the control group (33.40 ± 3.65 vs 30.60 ± 2.78) with a significant difference (P < 0.05).
Conclusion
It is concluded that CEP-BAM effectively increased patients' functional capacity and quality of life after a stroke in the sixth month after intervention.
Keywords: Adaptation, Psychological, Caregivers, Empowerment, Indonesia, Quality of life, Stroke
1. Introduction
Stroke is the most prevalent disease and the greatest cause of disability in Indonesia. In 2013, the prevalence of stroke in the country was 0.82% in urban areas and 0.57% in rural areas [1]. The stroke prevalence in the provinces of Jakarta and West Kalimantan was higher in urban areas than in the whole nation. The prevalence of stroke in Jakarta was 1.46% among individuals 15 years and older. Stroke is also the leading cause of death in urban areas (15.9%) and the second-leading cause of death in rural areas (11.5%) in the 45–54 year age range and the leading cause of death both in urban areas (28.8%) and rural areas (17.4%) in the 55–64 year age range [1].
The main burden of stroke is long-term residual impairment or physical disability due to neurological impairment. Residual impairment and disability are present in more than 75% of stroke survivors; 15%–30% of these patients report a significant level of disability [2]. The patients with significant disability at 3 months after stroke include the elderly, females, those with a history of diabetes mellitus or prior stroke or transient ischemic attack, those with severe strokes and those unable to ambulate at hospital discharge [3].
Smith, Lawrence, Kerr, Langhorne and Leas reported that the burden on the family increases when they are not knowledgeable or skilled enough to care for the patient at home [4]. Families did not know about resources that could be accessed to gain knowledge and skills to care for patients. They did not prepare themselves to care for patients at home, causing most of them to feel burdened whilst caring for their patients. The inadequacy of family caregivers' knowledge and skill may decrease their support for the patient and consequently affect the patient's quality of life [4].
The role of the family caregiver as part of the patient support system is important in improving the quality of life in post-stroke patients. The family caregiver provides long-term intensive assistance to patients [5]. They should be empowered to care and guide the patient to adapt to life after stroke. Thus, the caregiver's knowledge and skills in helping patients to adapt to life after stroke must be improved. Caregiver empowerment program based on adaptation model (CEP-BAM) is an intervention model that aims to improve the adaptability and quality of life of post-stroke patients by empowering the family caregiver. This research aimed to identify the effect of the CEP-BAM on the functional capacity and quality of life of patients after stroke.
2. Methods
2.1. Research design
This research was a quasi-experimental research with a pre- and post-test control group design.
2.2. Setting and sample
The samples used in this research were post-stroke patients (haemorrhagic or non-haemorrhagic) and their families. Inclusion criteria for patients were as follows: suffering physical disabilities, needing help in their daily activities (Barthel's index score less than 75) and post-discharge from hospital of less than one month (currently undergoing treatment at home). Inclusion criteria for family member were as follows: have the dominant role in caring for or assisting the patient at home and are less than 60 years old. The sampling method used in this research was consecutive sampling. We selected patients who satisfied the selection criteria until the sample size was met. The data of the samples were obtained from medical records at two hospitals in West Kalimantan and two hospitals in Jakarta, Indonesia (four hospitals in total, two in each group). We allocated the samples in each group by matching hospitals, and each group consisted of stroke patients who were discharged from the two hospitals. Basing on these data, we conducted home visits to perform the intervention.
2.3. Sample size calculation
We used the formula of hypothesis testing for the difference between two population means (two-sided test) to calculate the sample size as
| N1 = N2 = 2 [(uα + uβ) σ/δ]2, |
where δ is defined as the mean difference of the outcome variable (quality of life) between the intervention and control group. Mean difference of the quality of life between two groups based on the previous study was 6.3. With the assumption of one-sided 5% α, 80% power of the test and maximum of 0.82% lost-to-follow-up, the required sample size was 42 for each group (total = 84 samples). The total participants who completed the research were 80 patients and their families (40 participants in the intervention group and 40 participants in the control group).
2.4. Procedures
2.4.1. Intervention
CEP-BAM is a program that aims to improve the patients' quality of life and decrease the burden on families to train and promote the adaptation of post-stroke patients through family empowerment. CEP-BAM was developed based on the integration of Roy's Adaptation Model (RAM) [6] and the qualitative themes of an effective adaptation process as expressed by stroke patients. We used the concepts in RAM as the main framework for the intervention model, whereas the qualitative themes of an effective adaptation process post-stroke were applied as the main educational topic to improve post-stroke adaptation responses. RAM can be used to explain the adaptation process of post-stroke patients. According to RAM, a human is an adaptive system that can adapt to complex problems throughout their life. An individual can adapt to different levels, and this level of adaptation affects the human ability to respond positively to a situation. An individual can also control stimuli in his or her life as a coping strategy. The use of coping strategies results in an individual's adaptation response. According to RAM, the human adaptation response is divided into four modes, namely, physiological mode, self-concept mode, role function mode and interdependent mode. Effective human adaptation responses show that individuals can maintain their integrity to achieve their life goals [7].
Basing on preliminary studies, we found 10 themes of effective adaptation responses after stroke, consisting of 3 themes of stimuli or stressors perceived by patients and families, 3 themes of adaptive coping strategies used to control the problem and 4 themes related to effective adaptation behaviour. We integrated these qualitative themes with RAM to form an intervention model (CEP-BAM). The theme of stimuli perceived by the participants as a general problem of post-stroke patients should be intervened, whereas the themes of adaptive coping strategies and effective post-stroke adaptation behaviour are used as a guide in preparing the educational topic in the CEP-BAM.
The family caregiver is trained to facilitate and help the stroke patient to adapt to various disabilities to achieve their optimal quality of life after stroke. Effective post-stroke adaptation is achieved through three means, such as by decreasing stimulus, improving coping strategies and improving post-stroke adaptation response. The family caregiver is empowered to perform the role of a patient's companion and are also given the opportunity to learn post-stroke adaptation training, including interventions to reduce post-stroke stimuli, improve patient coping strategies and improve adaptation responses and action to maintain optimal psychological conditions during patient care.
CEP-BAM is divided into three phases, such as pre-education, intervention and monitoring/evaluation. In the pre-education phase, we employed a psychological approach to build a trusting relationship with the patient and their family caregiver. In the intervention phase, we conducted the following six interventions during meetings with family caregivers and patients:
-
(1)
Family caregiver education about stroke, prevention of recurrent stroke and stroke survivor problems (first meeting with family caregiver in the first week).
-
(2)
Family caregiver education and training about adaptive coping strategies after stroke, such as psychological coping, spiritual-religious coping and coping to achieve optimal physical recovery after stroke. Psychological coping training included the patient's efforts to accept their current condition, positive thinking and emotional control. Spiritual-religious coping included praying, obedient worship and belief in all events as God's will. Attempts to achieve physical recovery included regular physical examination, treatment, physical exercise and stroke diet (second meeting with family caregiver in the first week).
-
(3)
Family caregiver training about adaptation exercises after stroke includes body movement part 1, including ambulation on the bed, sitting on the bed, standing up and moving from the bed to the wheelchair and vice versa (third meeting with family caregiver in the first week).
-
(4)
Family caregiver training about adaptation exercises after stroke includes body movement part 2, such as walking exercise and joint movement (fourth meeting with family caregiver in the second week).
-
(5)
Family caregiver training about adaptation exercises after stroke, such as performing basic daily activities and roles, including bathing, using the toileting, dressing and feeding exercises (fifth meeting with family caregiver in the second week).
-
(6)
Family caregiver education about strategies to support the patient and maintain an adequate self-psychological condition whilst caring for the patient (sixth meeting with family caregiver in the third week).
In the monitoring and evaluation step, we encourage family caregivers to guide the patients to perform adaptation exercises regularly. We monitor notes made by the caregiver, including exercise type and time and the patient's ability to adapt. We also support the family caregiver when they experienced difficulties in caring for the patient. CEP-BAM intervention was given within a 6-month period, comprising three steps, such as pre-education, intervention and monitoring/evaluation (Table 1).
Table 1.
Steps of caregiver empowerment program based on adaptation model (CEP-BAM).
| Step 1: Pre-Education | Step 2: Interventions | Step 3: Monitoring and Evaluation | |
|---|---|---|---|
| Psychological approach and build a trusting relationship with the patient and their family caregiver. | The first week |
|
|
| Intervention 1 | Teach the family caregiver about stroke, prevention of recurrent stroke and stroke survivor problems (the first week). | ||
| Intervention 2 | Teach and train the family caregiver about adaptive coping strategies after stroke: psychological coping, spiritual-religious coping, and coping to achieve optimal physical recovery after stroke. | ||
| Intervention 3 | Train the family caregiver about adaptation exercise: Body movement part 1 (ambulation). | ||
| The second week | |||
| Intervention 4 | Train the family caregiver about adaptation exercise: Body movement part 2 (walking and joint movement). | ||
| Intervention 5 | Train the family caregiver about adaptation exercise: perform basic daily activities and role function after stroke include: bathing, toileting, dressing and feeding exercise. | ||
| Intervention 6 | Train the family caregiver about strategy to support the patient and maintain adequate self-psychological condition while caring the patient. | ||
The application of CEP-BAM was supported by tools, such as an intervention manual, standard operational procedures (SOP), a module for nurses, a booklet and a monitoring book for family caregivers. CEP-BAM has been reviewed by expert reviewers (senior professional nurses in a stroke unit, senior professional nurses in community health care and a consultant doctor who was a medical rehabilitation specialist). We tested the CEP-BAM on a small group of stroke patients before it was used in this study.
2.4.2. Control
The control group received the standard intervention in the form of Community Health Nursing (CHN) program, which was integrated with the health program in Public Health Centres. The CHN program was given by community nurses to post-stroke patients, including interventions as follows: early detection of recurrent stroke, health counselling, basic health care and referral to the nearest health service if the patient has health problems. The community nurse conducted six times home visit to do the CHN program, including assessment, formulation of nursing diagnoses, planning, implementation and evaluation.
2.5. Data collection
Data collection in this research was conducted for 6 months from May to October 2016. Qualified and trained nurses measured the functional capacity and quality of life after intervention. We maintained the double-blind principle in this research. Observers did not know the respondents' allocation to the intervention or control groups, and respondents did not know whether they were allocated to the intervention or control group. Instruments used in this research consist of Barthel's index to measure functional capacity after stroke and the stroke-specific quality of life (SSQoL) 12 item-scale (short version) to measure the quality of life after stroke [8]. Psychometric testing of Barthel's index proved the internal consistency with a Cronbach's α coefficient of 0.94, with coefficients for each domain ranging from 0.89 to 0.92 [9]. Barthel's index has good inter-rater reliability, internal consistency and excellent predictive validity and responsiveness. Test validity and reliability of the SSQoL-12 items in three different places yields Cronbach's α coefficients ranging from 0.78 to 0.89 [8]. The SSQoL-12 items was predicted to be 88%–95% of the actual variants of SSQoL.
We measured the outcomes four times, namely, before intervention (pre-test), on the last week of the fourth month (post-test 1), fifth month (post-test 2) and the sixth month after intervention (post-test 3).
2.6. Data analysis
We conducted univariate, bivariate and multivariate data analyses. Univariate analysis was used to describe the dependent variables. The bivariate analysis was conducted to test the equality of respondent characteristics and the mean difference of outcome variables between groups. Multivariate analysis was performed to determine the effectiveness of the CEP-BAM on the functional capacity and quality of life after controlling for confounding variables (sex, patient's age, type of stroke, aphasia, hemiparesis, family caregiver's age, family caregiver's education level and caregiver–patient relationship).
2.7. Ethical aspects
With regards to the protection of human rights and welfare in nursing research, this research has been reviewed carefully by The Ethical Clearance Division, FK-Untan Indonesia, with Institutional Review Board (IRB) number 5321/UN22.9/DT/2016.
3. Results
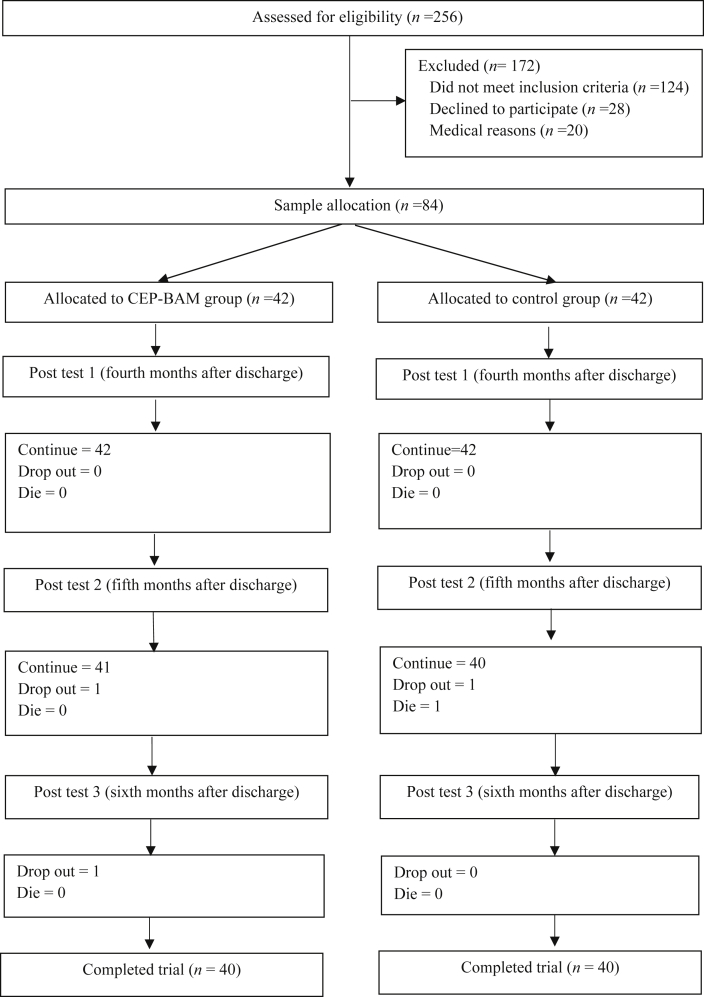
Forty-two participants were in the intervention group and 42 participants in the control group. Two participants in the intervention group and two in the control group dropped out during intervention (Fig. 1). Equality tests of the respondents and family caregivers' characteristics and stroke characteristics between the groups showed no significant differences as shown in Table 2. Repeated measurement ANOVA analysis as a whole showed a significant difference of outcome between measurements and between the two groups(F = 2.098, P = 0.029).
Fig. 1.
Flowchart of the trial.
Table 2.
The characteristics of stroke patients and their family caregivers (n = 80).
| Variables | Intervention group |
Control group |
χ2 or t value | P value | ||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Sex | 0.050 | 0.823 | ||||
| Male | 22 | 55 | 20 | 50 | ||
| Female | 18 | 45 | 20 | 50 | ||
| Stroke type | 0.561 | 0.712 | ||||
| Non haemorrhagic | 37 | 92.5 | 35 | 87.5 | ||
| Haemorraghic | 3 | 7.5 | 5 | 12.5 | ||
| Hemiparesis | 0.464 | 0.496 | ||||
| Right side | 22 | 55 | 25 | 62.5 | ||
| Left side | 18 | 45 | 15 | 37.5 | ||
| Aphasia | 0.200 | 0.655 | ||||
| Yes | 18 | 45 | 21 | 52.5 | ||
| No | 22 | 55 | 19 | 47.5 | ||
| Education level of caregiver | 5.804 | 0.214 | ||||
| Under graduate | 5 | 12.5 | 7 | 17.5 | ||
| Senior high school | 19 | 47.5 | 19 | 47.5 | ||
| Junior high school | 9 | 22.5 | 3 | 7.5 | ||
| Elementary school | 6 | 15 | 11 | 27.5 | ||
| None | 1 | 2.5 | 0 | 0 | ||
| Caregiver-patient relationship | 1.808 | 0.613 | ||||
| Husband/wife | 15 | 37.5 | 14 | 35 | ||
| Child | 16 | 40 | 20 | 50 | ||
| Son in law/daughter in law | 4 | 10 | 4 | 10 | ||
| Brother/sister | 5 | 12.5 | 2 | 5 | ||
| Patient's age (Mean, SD) | 59.05 | 6.6 | 58.1 | 7.5 | 0.584 | 0.561 |
| Caregiver's age (Mean, SD) | 43.60 | 12.1 | 42.3 | 14.5 | 0.444 | 0.658 |
Table 3 describes the differences in functional capacity (Barthel's index) between measurements in both groups, after controlling for confounding variables, such as sex, patient's age, type of stroke, aphasia, hemiparesis, the family caregiver's age, caregiver's education level and caregiver–patient relationship. Multivariate analysis showed significant differences in functional capacity between measurements and between the two groups. The repeated measurement ANOVA showed a significant difference of functional capacity between measurements and between the two groups (F = 3.289, P = 0.044). A significant difference occurred between pre-test and post-test 3 (F = 4,981, P = 0.028). These results indicate that CEP-BAM effectively improved the functional capacity of patients in the sixth month after the intervention.
Table 3.
The patient's functional capacity (Barthel's index).
| Time | Intervention group (n = 40) |
Control group (n = 40) |
t value | P value | ||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| Pre-test | 54.50 | 10.18 | 54.88 | 9.44 | −0.171 | 0.865 |
| Post-test 1 | 55.13 | 9.90 | 55.25 | 9.19 | −0.059 | 0.953 |
| Post-test 2 | 56.25 | 11.42 | 55.50 | 7.99 | 0.340 | 0.735 |
| Post-test 3 | 58.38 | 12.00 | 55.75 | 5.83 | 1.244 | 0.217 |
Based on measuring the functional capacity in the intervention group, several domains increased after CEP-BAM. Of the 10 domains, nine increased after the intervention, whereas two domains increased significantly. Table 4 shows that the average score of functional capacity in nine domains increased in post-test 3 compared to pre-test. Statistical analysis proved that two domains of functional capacity increased significantly after CEP-BAM, including feeding and dressing (P < 0.05).
Table 4.
The change of daily living activities pre- and post intervention in the intervention group.
| No | Items |
Mean |
Mean Difference | t value | P value | |
|---|---|---|---|---|---|---|
| Pre test | Post test 3 | |||||
| 1. | Feeding | 6.88 | 7.75 | 0.87 | −2.876 | 0.006 |
| 2. | Moving from wheelchair to bed and return (include sitting up in bed) | 6.75 | 7.25 | 0.50 | −1.433 | 0.160 |
| 3. | Personal toilet (wash face, comb hair, shave, clean teeth) | 3.13 | 3.50 | 0.37 | −1.000 | 0.323 |
| 4. | Getting on and off toilet (handling clothes, wipe, flush) | 5.00 | 4.88 | −0.12 | 1.000 | 0.323 |
| 5. | Bathing self | 1.00 | 1.63 | 0.63 | −1.706 | 0.096 |
| 6. | Walking on level surface (or if unable to walk, propel wheelchair) | 4.75 | 5.13 | 0.38 | −0.902 | 0.372 |
| 7. | Ascend and descend stairs | 2.88 | 3.38 | 0.50 | −1.433 | 0.160 |
| 8. | Dressing | 5.13 | 5.75 | 0.62 | −2.360 | 0.023 |
| 9. | Controlling bowels | 9.38 | 9.50 | 0.12 | −1.000 | 0.323 |
| 10. | Controlling bladder | 9.63 | 9.63 | 0 | 0 | 1.000 |
Table 5 describes differences in the quality of life between measurements in both groups after controlling for confounding variables, such as sex, patient's age, type of stroke, aphasia, hemiparesis, the family caregiver's age, caregiver's education level and caregiver–patient relationship. No significant differences in the quality of life between groups in pre-test, post-test 1 and post-test 2 (P > 0.05) were observed, and a significant difference occurred in the post-test 3 (P < 0.05). The repeated measurement ANOVA showed a significant difference in the quality of life between measurements and between the two groups (P = 0.007). A significant difference in the quality of life between groups occurred between pre-test and post-test 3 (P = 0.003) with a power difference of 11.1%. These results indicate that CEP-BAM effectively improved the patients' quality of life in the sixth month after intervention.
Table 5.
The patient's quality of life between measurements in the intervention and control groups (n = 80).
| Time | Intervention group (n = 40) |
Control group (n = 40) |
t value | P value | ||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| Pre-test | 30.38 | 4.06 | 30.48 | 3.33 | 0.001 | 1.000 |
| Post-test 1 | 30.70 | 4.19 | 30.45 | 3.71 | 0.282 | 0.778 |
| Post-test 2 | 31.75 | 3.40 | 30.48 | 3.27 | 1.710 | 0.091 |
| Post-test 3 | 33.40 | 3.65 | 30.60 | 2.78 | 3.859 | 0.001 |
4. Discussion
4.1. CEP-BAM increases functional capacity after stroke
We found that CEP-BAM effectively improved functional capacity after stroke. The increase in functional capacity after stroke was a positive effect of adaptation exercises or body movement. Yu proved that when a community based physical rehabilitation program in the form of basic technical training and functional rehabilitation is given to patients and their families, neurological function after stroke can be improved [10]. Stuart, Chard and Roettger also proved that physical adaptation exercises can improve the physical health and fitness of post-stroke patients [11]. Research conducted by Tseng, Chen, Wu and Lin showed that range of-motion exercises can improve joint mobility and decrease pain [12].
Adaptation exercises or body movements performed at the early stage of stroke recovery is the important factor in achieving better functional capacity at a late stage. Research by Ovbiagele and Saver showed a significant relationship in functional capacity between the first week and three months after stroke [13]. Patients who were guided by their families regularly to perform daily activities independently have better functional capacity. In line with our research, Sahebalzamani et al. also proved that a self-care exercise program can improve the independence of post-stroke patients [14].
The mechanism of adaptation exercise, or the way in which body movements improve functional capacity can be explained using the neurological function repair mechanism. The mechanism of nerve recovery begins with a spontaneous process by the resolution of dangerous local factors. This resolution process is the body's efforts to eliminate local edema and toxins, increase local blood circulation and recover nerve cells, which lasts from about 3 to 6 months after a stroke attack. The next stage is the process of neuroplasticity, which is the ability of the nervous system to organize its structure and function. Neuroplasticity includes the formation of new collateral synapses and the activation of functional nerve lines that already exist. This process is influenced by external factors, such as drugs, electrical stimulation and environmental stimulation. When taught to the patient every day by the family caregiver, adaptation exercises or body movements, including moving the weak limbs and daily living exercises can enhance the neuroplasticity process, thus improving the patient's neurological function. Alternatively, resting the weak limb can inhibit the nerve cell recovery process [15].
The increase in functional capacity in the intervention group was also a positive impact of following a healthy lifestyle after stroke. Living with a healthy lifestyle is an important way to prevent recurrent stroke and to improve functional capacity after stroke. Green, Haley, Eliasziw and Hoyte proved that education-counselling interview (ECI) was effective in improving patients' knowledge about stroke and in changing their lifestyle to be healthy [16].
The application of adaptive coping strategies or positive thinking, taught by the family caregiver to the patient, contributed to an increase in the functional capacity of patients. Patients and their families were taught how to accept their condition with sincerity and always think that other patients have more severe problems. Positive thinking will increase a patient's motivation to recover, not feel embarrassed by changes in the shape and function of their body and hope for a better future. Positive thinking meant that patients and their families were able to use their resources to adjust and adapt after stroke. Ch'ng, French and McLean proved that the ability to accept disability after a stroke, undergo a new role and undertake new activities were key to adjusting after stroke [17]. Patients and their families who regularly learn new activities will demonstrate better functional capacity. Alternatively, non-adaptive coping strategies for facing problems were the cause of slow improvement of functional capacity after stroke. They were unable to utilise their resources, i.e., use a healthy body part to prop up the weak parts, which means that the patient cannot perform daily activities independently at home.
4.2. CEP-BAM increases the quality of life after stroke
This research proves that CEP-BAM improved the quality of life after stroke. Family caregivers who have adequate knowledge and skills in caring for post-stroke patients will have the confidence to provide quality care to patients. Quality of care and assistance can restore the patients' quality of life to optimal levels. Empowering the family caregiver is an appropriate strategy to improve the quality of life in post-stroke patients because only the family, who is always with the patients, can understand the problems experienced by the patients and are able to provide their basic needs. Parveen, Morrison and Robinson stated that programs or interventions, which give attention to family values and coping responses, will produce benefits for patients and their families [18].
The focus of CEP-BAM is in improving family support to achieve adaptation response and optimal quality of life for patients. The family caregiver was empowered to provide support to fulfil the patient's basic needs (instrumental support) and to provide information and emotional support to the patient. Optimal family support during the rehabilitation stage can improve the quality of life in post-stroke patients. Ch'ng, French and McLean proved that family support will contribute at every stage of stroke recovery and can reduce patient confusion to the problems they experienced in the early stages following stroke. Family support will improve patients' coping strategies so that they can accept and adjust to various limitations in the rehabilitation phase [17].
Involving and empowering family caregiver in rehabilitation of stroke patients is useful for those who have cognitive and memory disorders post-stroke. Cognitive impairment causes the patient to find it difficult to accept and process information. Memory loss will make it difficult for the patient to remember and practice the adaptation skills taught by the nurse. Empowering the family caregiver is the right solution to improve the adaptability and quality of life of post-stroke patients. The family caregivers who accompanied patients in the intervention strived not to be replaced by other family members during the intervention. Education and empowerment were intended to be given to the family as a whole so that the family caregiver can provide optimal assistance to the patient.
Adaptation exercises or body movements taught to family caregivers also contributed to improving the quality of life of stroke patients. Done regularly, adaptation exercises can improve the functional capacity in post-stroke patients. Achieving optimal levels of functional capacity can improve the quality of life after stroke. Kyung, Young and Eun proved the positive relationship between the ability to perform daily living activities and the quality of life in post-stroke patients [19]. A comprehensive treatment program that aims to improve the quality of life should focus on functional capacity after stroke [20].
Kwon, Choi, Kwon, Kang and Kim proved that dependence on performing daily living activities, depression and low socio-economic status at three months after a stroke are factors that cause low quality of life three years after stroke [21]. Following the findings of this research, we trained the family caregiver to guide the patient in performing body movement exercises, applying effective coping strategies and applying effective adaptation behaviour in the early stages of rehabilitation at home. Optimal functional capacity in the early stages after a stroke is key to achieving long-term quality of life after stroke. We are certain that CEP-BAM can improve the quality of life in post-stroke patients not only at three months after stroke but also in the long-term.
Empowering the family caregiver to guide the patient in applying psychological adaptive coping and spiritual-religious coping also contributed in improving the quality of life of patients. The family caregiver was trained to guide the patient in applying psychological adaptive coping, including positive thinking, accepting their conditions of disability and controlling their emotions. Positive thinking can improve the patients' confidence in their ability to perform daily activities, thus allowing them to not be embarrassed by changes in their body shape, increase their motivation to recover and to have a positive view of themselves and the future after stroke. The ability to control their emotions allows patients to not be easily offended or upset, not drag on sustained thinking about their problem and think about and do things that are fun. Accepting the reality of their limitations can reduce emotional distress and improve self-esteem. Improving the patients' quality of life through applying adaptive coping strategies is potentially more cost effective than other intervention methods [22]. The high prevalence of stroke led to an increase in the number of patients who experience disability. Improving the quality of life by applying adaptive coping strategies should therefore be considered [22]. Visser, Aben, Heijenbrok, Busschbach and Ribbers proved that accommodative and assimilative coping strategies were related to the quality of life, especially in the domain of psychological health [23].
Patients with self-confidence, a positive view of themselves and good adjustment to their problems will achieve an optimal psychological health status after stroke. Their psychological condition will influence their quality of life after stroke. Research by Jeong, Kang, Bae, Kim, Shin, Park et al. on the determinants of quality of life in the acute stage of stroke proved that psychological distress and impaired cognitive function lead to low quality of life in stroke patients. Jeong et al. stated the importance of psychological intervention to improve the quality of life during the acute phase of stroke [24].
4.3. Limitations of research
We did not measure the ability of families to facilitate and assist patients in adaptation exercises, so differences in interpersonal skills were not considered. We overcame this by monitoring and assisting the family caregiver. We gave the family reinforcement if they encounter difficulty.
CEP-BAM effectively empowers families in assisting or facilitating patients with mild to moderate disability conditions after stroke. However, the effectiveness of this intervention has not yet been proven in empowering families caring for patients with complex stroke conditions or severe disability. Under these conditions, multidisciplinary management is required, which involves the role of a neurologist, stroke nurse, physiotherapist, speech therapist, nutritionist and social worker.
5. Conclusion
CEP-BAM effectively increased the patients' functional capacity and quality of life after stroke in the sixth month after intervention. Nine out of ten domains of functional capacity increased in the intervention group after CEP-BAM, whereas two domains (feeding and dressing) increased significantly in the 6 months after CEP-BAM. This intervention model can be used as a standard procedure in the management of post-stroke patients in the community setting, especially for patients with mild to moderate disability conditions after stroke. Further research is needed to identify the effect of CEP-BAM in improving the quality of life in post-stroke patients in terms of cost-effectiveness and to determine the most effective strategies to enhance family support for post-stroke patients.
Acknowledgements
We are grateful to our patients, family caregivers and the nursing staff in the primary health care and public hospital in West Kalimantan dan Jakarta, Indonesia.
Footnotes
Peer review under responsibility of Chinese Nursing Association.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2018.09.002.
Conflicts of interest
No conflict of interest has been declared by the authors.
Funding
This research was supported by the Board for Development and Empowerment Human Resources of Health, the Indonesian Ministry of Health, with the number of decision letter: HK.02.03/III.1/004172/2016.
Appendix A. Supplementary data
The following is the supplementary data to this article:
References
- 1.Ministry of Health Indonesia . Health Research and Development Board; 2013. Basic medical research. [Google Scholar]
- 2.Go A.S., Mozaffarian D., Roger V.L., Benjamin E.J., Berry J.D., Blaha M.J., Dai S., Ford E.S., Fox C.S., Franco S., Fullerton H.J., Gillespie C., Hailpern S.M., Heit J.A., Howard V.J., Huffman M.D., Judd S.E., Kissela B.M., Kittner S.J., Lackland D.T., Lichtman J.H., Lisabeth L.D., Mackey R.H., Magid D.J., Marcus G.M., Marelli A., Matchar D.B., McGuire D.K., Mohler E.R., Moy C.S. Heart disease and stroke statistics–2014 update: a report from the American Heart Association. Circulation. 2014;129:e28–e209. doi: 10.1161/01.cir.0000441139.02102.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bettger J.P., Zhao X., Bushnell C., Zimmer L., Pan W., Williams L.S., Peterson E.D. The association between socioeconomic status and disability after stroke: findings from the Adherence Evaluation after Ischemic stroke Longitudinal (AVAIL) registry. BMC Publ Health. 2014;14:281. doi: 10.1186/1471-2458-14-281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Smith L.N., Lawrence M., Kerr S.M., Langhorne P., Lees K.R. Informal carers experience of caring for stroke survivors. J Adv Nurs. 2004;46(3):235–244. doi: 10.1111/j.1365-2648.2004.02983.x. [DOI] [PubMed] [Google Scholar]
- 5.Friedman M.M., Bowden V.R., Jones E.G. fifth ed. Prentice Hall; Englewood Cliffs. NJ: 2003. Family nursing: research, theory, and practice. [Google Scholar]
- 6.Roy S.C., Andrews H.A. second ed. Appleton & Lange; Stamford: 1999. Roy adaptation model. [Google Scholar]
- 7.Alligood M.R., Tommey A.N. 6rd ed. Mosby Inc; 2006. Nursing theorists and their work. [Google Scholar]
- 8.Post M.W.M., Bosman H., Zandvoort M.M.V., Passier P.E.C.A., Rinkel G.J.E., Visser-Meily JMA. Development and validation of a short version of the stroke-specific quality of life scale. J Neurol Neurosurg Psychiatr. 2010;82(3):283–286. doi: 10.1136/jnnp.2009.196394. https://hal.archives-ouvertes.fr/hal-00570138/document [DOI] [PubMed] [Google Scholar]
- 9.Hsueh I.P., Lee M.M., Ching L.H. Psicometric characteristics of the Barthel activities of daily living index in stroke patient. J Formos Med Assoc. 2001;100(8):526–532. [PubMed] [Google Scholar]
- 10.Yu J.J. The effects of community-based rehabilitation on stroke patients in China: a single-blind, randomized controlled multicentre trial. Clin Rehabil. 2009;23:408–417. doi: 10.1177/0269215508091870. [DOI] [PubMed] [Google Scholar]
- 11.Stuart M., Chard S., Roettger S. Exercise for chronic stroke survivors: a policy perspective. J Rehab Research & Dev. 2008;45(2):329–338. doi: 10.1682/JRRD.2007.02.0027. [DOI] [PubMed] [Google Scholar]
- 12.Tseng N.C., Chen C.C.H., Wu S.C., Lin L.C. Effect of a range-of-motion exercise programme. J Adv Nurs. 2007;57(2):181–191. doi: 10.1111/j.1365-2648.2006.04078.x. [DOI] [PubMed] [Google Scholar]
- 13.Ovbiagele B., Saver J.L. Day-90 acute ischemic stroke outcomes can Be derived from early functional activity level. Cerebrovasc Dis. 2010;29(1):50–56. doi: 10.1159/000255974. [DOI] [PubMed] [Google Scholar]
- 14.Sahebalzamani M., Aliloo L., Shakib A. The efficacy of self-care education on rehabilitation of stroke patients. Saudi Med J. 2009;30(4):550. https://www.ncbi.nlm.nih.gov/pubmed/19370286 [PubMed] [Google Scholar]
- 15.Motor Recovery in Stroke, Petrina, A.B. Medscape, http://emedicine.medscape.com/article/324386-overview#aw2aab6b4. Accessed November 2014.
- 16.Green T., Haley E., Eliasziw M., Hoyte K. Education in stroke prevention: efficacy of an educational counseling intervention to increase knowledge in stroke survivors. Can J Neurosci Nurs. 2007;29(2):13–20. [PubMed] [Google Scholar]
- 17.Ch’ng A.M., French D., McLean N. Coping with the challenges of recovery from stroke. J Health Psychol. 2008;13(8):1136–1146. doi: 10.1177/1359105308095967. [DOI] [PubMed] [Google Scholar]
- 18.Parveen S., Morrison V., Robinson C.A. Does coping mediate the relationship between familism and caregiver outcomes? Aging Ment Health. 2014;18(2):255–259. doi: 10.1080/13607863.2013.827626. [DOI] [PubMed] [Google Scholar]
- 19.Kyung K., Young M.K., Eun K.K. Correlation between the activities of daily living of stroke patients in a community setting and their quality of life. J Phys Ther Sci. 2014;26(3):417–419. doi: 10.1589/jpts.26.417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gurcay E., Bal A., Cakci A. Health-related quality of life in first-ever stroke patients. Ann Saudi Med. 2009;29(1):36–40. doi: 10.4103/0256-4947.51814. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2813619/ 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kwon S.C., Choi J.M., Kwon S.U., Kang D.W., Kim J.S. Factors that affect the quality of life at 3 Years post-stroke. J Clin Neurol. 2006;2(1):34–41. doi: 10.3988/jcn.2006.2.1.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Darlington A.S., Dippel D.W., Ribbers G.M., Van Balen R., Passchier J., Busschbach J.J. A prospective study on coping strategies and quality of life in patients after stroke, assessing prognostic relationships and estimates of cost-effectiveness. J Rehabil Med. 2009;41(4):237–241. doi: 10.2340/16501977-0313. [DOI] [PubMed] [Google Scholar]
- 23.Visser M.M., Aben L., Heijenbrok-Kal M.H., Busschbach J.V., Ribbers G.M. The relative effect of coping strategy and depression on health-related quality of life patients in the chronic phase after stroke. J Rehabil Med. 2014;46(6):514–519. doi: 10.2340/16501977-1803. [DOI] [PubMed] [Google Scholar]
- 24.Jeong B.O., Kang H.J., Bae1 K.Y., Kim S.W., Kim J.M., Shin I.S., Kim J.T., Park M.S., Cho K.H., Yoon J.S. Determinants of quality of life in the acute stage following stroke. Psychiatry Investig. 2012;9(2):127–133. doi: 10.4306/pi.2012.9.2.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.