Abstract
Introduction
Healthcare-associated infections (HCAIs) are the most frequent adverse event compromising patient safety globally. Patients in healthcare facilities (HCFs) in low-income and middle-income countries (LMICs) are most at risk. Although water, sanitation and hygiene (WASH) interventions are likely important for the prevention of HCAIs, there have been no systematic reviews to date.
Methods
As per our prepublished protocol, we systematically searched academic databases, trial registers, WHO databases, grey literature resources and conference abstracts to identify studies assessing the impact of HCF WASH services and practices on HCAIs in LMICs. In parallel, we undertook a supplementary scoping review including less rigorous study designs to develop a conceptual framework for how WASH can impact HCAIs and to identify key literature gaps.
Results
Only three studies were included in the systematic review. All assessed hygiene interventions and included: a cluster-randomised controlled trial, a cohort study, and a matched case-control study. All reported a reduction in HCAIs, but all were considered at medium-high risk of bias. The additional 27 before-after studies included in our scoping review all focused on hygiene interventions, none assessed improvements to water quantity, quality or sanitation facilities. 26 of the studies reported a reduction in at least one HCAI. Our scoping review identified multiple mechanisms by which WASH can influence HCAI and highlighted a number of important research gaps.
Conclusions
Although there is a dearth of evidence for the effect of WASH in HCFs, the studies of hygiene interventions were consistently protective against HCAIs in LMICs. Additional and higher quality research is urgently needed to fill this gap to understand how WASH services in HCFs can support broader efforts to reduce HCAIs in LMICs.
PROSPERO registration number
CRD42017080943.
Keywords: health education and promotion, systematic review, prevention strategies, hygiene, public health
Key questions.
What is already known?
Healthcare-associated infections (HCAIs) are the most frequent adverse event affecting patient safety globally and the burden is estimated to be much greater in low-income and middle-income countries (LMICs) than in high-income countries.
HCAIs are transmitted via pathways for which water, sanitation and hygiene (WASH) interventions are plausibly effective however, no previous reviews have assessed this and WASH coverage in LMIC healthcare facilities (HCFs) remains low.
What are the new findings?
There exist very few high-quality studies assessing the impact of WASH interventions on HCAIs in LMIC HCFs and most focus on hygiene interventions leaving a paucity of evidence around the impact of water and sanitation services.
Most WASH interventions are combined with broader infection prevention and control strategies, making it difficult to attribute change in health outcomes to the WASH interventions alone and to quantify their contribution.
What do the new findings imply?
Our findings indicate that hygiene interventions are consistently protective against HCAIs in LMICs and offer support to their continued use; however, due to poor study design their effect cannot be quantified.
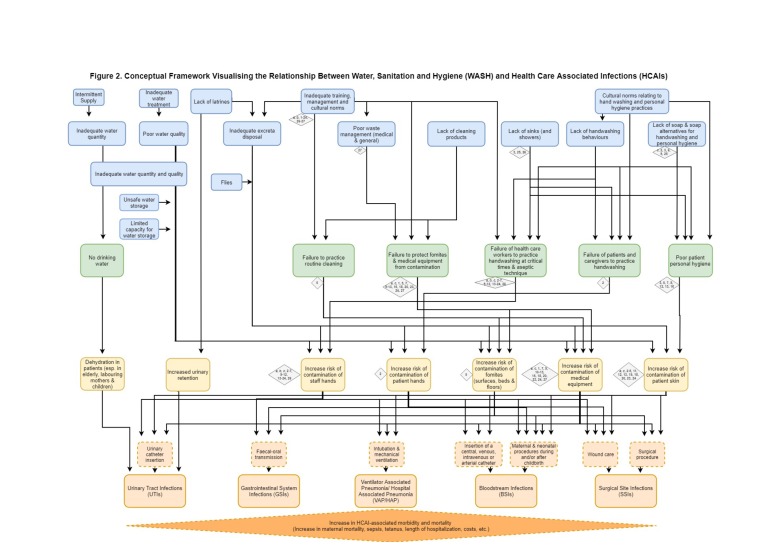
Additional and higher quality research is needed on the impact of different WASH interventions on HCAIs in LMIC HCFs to allow prioritisation of the most effective approaches in these often resource-poor settings; the conceptual framework we present illustrates plausible pathways between inadequate WASH and HCAIs and could guide future research efforts and investments.
Introduction
Healthcare-associated infections (HCAIs) are the most frequent adverse event compromising patient safety globally.1 HCAIs are infections acquired by patients while receiving treatment for medical or surgical conditions, or after coming into contact with a healthcare setting, and occurring 48 hours or more postexposure.2 The most frequent types are urinary tract infections (UTIs), bloodstream (vascular catheter-associated) infections (BSIs), ventilator-associated pneumonia (VAP), hospital-acquired pneumonia (HAP) and surgical site infections (SSIs). There are, however, a number of other infections that can occur in the healthcare setting, including gastrointestinal system infections (GSIs) commonly caused by Clostridium difficile, norovirus and Escherichia coli, among others.2
The global burden of HCAIs is unknown but the WHO estimates that at least 7% of all patients admitted to hospital in high-income countries (HICs) will contract a HCAI.3 This proportion increases significantly for intensive care unit admissions, where one in three patients will suffer from a HCAI, due to the greater risks associated with mechanical ventilation.4
In low-income and middle-income countries (LMICs), the risk of HCAIs is estimated to be much greater, with a pooled prevalence estimate of 15.5% of all patients developing one or more infections during a healthcare facility (HCF) stay.1 3 Rates of HCAIs are particularly high for newborns in these settings, who have between three and twenty times higher risk of acquiring a HCAI than newborns delivered in a HIC facility.5 Pregnant women in LMICs are also at greater risk from HCAIs; global maternal mortality studies estimate a 9.7% prevalence of sepsis-related deaths, independent of the place of birth6 and in LMICs, 22% of all maternal deaths following a caesarean section are attributable to sepsis7 and SSI.8 Furthermore, lack of WASH services, along with other essentials, such as energy, infection prevention and control (IPC) resources, skilled birth attendants and basic medicines, contributes to lower quality of care for mothers and newborns.9 Although it is widely accepted that the global HCAI burden is considerably larger in LMICs, existing reviews have been unable to provide a complete picture due to a paucity of reliable data.4
The risk of acquiring HCAIs is ubiquitous and pervades all domains of the formal healthcare system (home-based, ambulatory, primary, secondary and tertiary care). The human cost of these infections in HICs is well documented—prolonged suffering and hospital stay, long-term disability, and a higher risk of mortality.4 10 The financial costs are also significant, with the treatment costs for a single HCAI in the USA estimated to be between $23 000 and $25 000.4 The implications of HCAIs are far worse when caused by a drug resistant organism. For example, patients that contract methicillin-resistant Staphylococcus aureus—an antibiotic-resistant bacterium, have a 50% higher mortality rate than patients with methicillin-susceptible Staphylococcus aureus—an infection responsive to readily available antibiotics.11 HCAIs also have implications on the emergence of new antimicrobial resistance (AMR) and the increased demand for antibiotics—also a catalyst for increasing drug resistance.12
Safe water, sanitation and hygiene (WASH) are key public health interventions.13–25 An adequate quantity and quality of water, facilities for safely managing excreta and healthcare waste, and the application of hygienic practices such as hand hygiene and environmental cleaning, are essential to the functioning of any HCF.26 27 The causal link between hand hygiene practices of birth attendants and maternal infection has long been established.28–30 More recently however, studies have linked neonatal sepsis, maternal mortality and increasing AMR to poor access to water and sanitation, and unclean birth environments.12 31–33 WASH services and practices are a prerequisite for the delivery of most IPC practices and are additionally important for improving quality of care.34
In recent years there has been increased recognition of the role of WASH in HCFs. This includes a global call to action on WASH in HCFs launched in 2018,35–37 envisioning universal and sustainable access to safe WASH in HCFs particularly in LMICs, where services are frequently lacking. With support from over 35 partners, WHO and Unicef are co-leading the implementation of a global roadmap to improve WASH services in HCFs. Eight practical steps have been identified including actions such as developing national roadmaps and setting targets, improving infrastructure and maintenance, and engaging communities.38
Progressing from the Millennium Development Goals, the Sustainable Development Goals (SDGs) for 2030 consider access to WASH beyond the household, including in HCFs, and the WHO/Unicef Joint Monitoring Programme will regularly report on global coverage figures for WASH in HCFs from 2019. In addition, the UN Special Rapporteur on the Human Right to Safe Drinking Water and Sanitation identified the provision of WASH, in HCF settings, as a central vehicle for advancing human rights.39 Finally, in January 2019, the WHO executive board unanimously approved a resolution on WASH in HCFs which calls on Member States and, in particular ministries of health, to increase investments in and strengthen systems around maintaining WASH in HCFs.40
Despite this, WASH coverage in HCFs is low. The SDG baseline data released in 2019 indicates that one in four HCFs lack basic water services and one in five have no sanitation service, impacting almost 2 billion and 1.5 billion people, respectively. Most of these people are in LMICs.41 Similar gaps exist for basic hand hygiene facilities and safe segregation and disposal of healthcare waste.41
In HICs it has been estimated that between 10% and 70% of HCAIs are preventable, depending on the setting, baseline infection rates and type of infection.42 These infections have been reduced through multi-modal interventions, including increasing the availability of hand hygiene products and improving the hand hygiene practices of healthcare workers.42
There is strong biological plausibility to the hypothesis that pathogens responsible for HCAIs are more prevalent in facilities with substandard WASH services.1 5 43 In LMICs the majority of pathogenic micro-organisms that have been isolated in HCFs are directly linked to environmental contamination, for example, through low quality water, poor hand hygiene or contaminated equipment and surfaces.1 3 Inadequate environmental hygiene in these settings has been identified as a potentially important determinant of the high burden of HCAIs, and other adverse outcomes such as maternal and newborn mortality.1 31 44 45
To date, there have been no published systematic reviews investigating the effect of WASH improvements on HCAIs in LMICs. Understanding this relationship will help to better define the role of WASH as part of the global effort to improve healthcare quality, including meeting the SDG targets on maternal and child mortality (SDG 3.1 and 3.2), universal health coverage (SDG 3.8) and achieving the aims of global campaigns such as the WHO’s ‘Clean Care is Safer Care’ Programme,46 and reductions in AMR.47 Importantly, it will enhance existing actions to reduce HCAIs globally and establish an agenda for future research for resource-constrained settings in this area of public health.
The objective of this review was to estimate the impact of WASH interventions in HCFs on HCAIs. As outlined in our prepublished protocol,48 we conducted a systematic review of the literature. This was supplemented by a subsequent scoping review covering the before-and-after studies excluded from the original review due to lack of a control group (the most common study design in this field of research). This scoping review was undertaken to allow us to utilise the evidence currently available in order to identify key characteristics of WASH interventions targeting HCAIs and gain a broad overview of effect. All the studies from the systematic and scoping reviews were mapped to a conceptual framework illustrating the plausible pathways between inadequate WASH and HCAIs to highlight gaps in the knowledge base and guide future research efforts.
Methods
Search strategy
The search strategy was created, using three concepts: (1) WASH interventions; (2) HCAIs; (3) LMICs. Search terms were adapted and run in each database by one reviewer (LDG) and a librarian (JF). We sought to identify all relevant studies regardless of publication status (published, unpublished, in press and ongoing), however, where possible, searches were limited to primary studies or reviews. Publications were limited to those published in or after 1970 in the English language. Searches were run on the 24th and 25th April 2018.
Electronic searches
We searched the following databases using keywords and controlled vocabulary, adapted according to the requirements of each database: Cochrane Public Health Group Special Register, Cochrane Central Register of Controlled Trials (CENTRAL) (Wiley interface), MEDLINE (OvidSP interface), MEDLINE-In-Process (OvidSP interface), Web of Science Core Collection (Web of Science interface), EMBASE (OvidSP interface), Global Health (OvidSP interface), Africa Wide Information (Ebsco Interface), CINAHL Plus (Ebsco interface), SciELO (Web of Science interface), Trial registers (metaRegister of Controlled Trials, ClinicalTrials.gov and the International Clinical Trials Registry Platform Search Portal (www.who.int/trialsearch). We also searched the WHO regional databases: Western Pacific Region Index Medicus, Latin America and Caribbean Health Sciences, African Index Medicus, Index Medicus for the Eastern Mediterranean Region Database and Index Medicus for the South-East Asian Region.
In our search for relevant grey literature, we used the following sources: www.nyam.org/library/online-resources/grey-literature-report/, 3ie Impact; and http://www.opengrey.eu.
Reference lists of key articles were also hand-searched for any additional relevant articles.
Searching other resources
We contacted leading researchers (n=19) and organisations (n=13) for relevant articles including the Soapbox Collaborative; Water, Sanitation, Hygiene and Health Programme (WHO); Infection Prevention and Control Unit and Service Delivery and Safety Department (WHO); Maternal, Newborn, Child and Adolescent Health (WHO); Infection Control Africa Network (ICAN); Unicef; World Bank Water and Sanitation Programme; Environmental Health Project (USAID); Centres for Disease Control and Prevention; Viral and Bacterial Infections, Barcelona Institute for Global Health (ISGlobal); the Water Institute at the University of North Carolina (UNC); United States Agency for International Development (USAID); and UK Department for International Development.
We also searched the proceedings of the following conferences for relevant abstracts: International Water Association; UNC Water and Health (North Carolina, USA); Water, Engineering and Development Centre Conference (Loughborough University, UK); and public health conferences (eg, American Public Health Association; European Public Health Association, Federation of Gynaecology and Obstetrics World Congress; Global Women’s Research Society Conference; International Confederation of Midwives; Global Symposium on Health Systems Research; American Society of Tropical Medicine and Hygiene Annual Conference; Maternal and Newborn Health Conference; ICAN Conference; International Federation of Infection Control Conference; International Conference on Infection Control and Prevention; Asia Pacific Society of Infection Control Conference).
Inclusion criteria
Studies were eligible for inclusion if they adhered to the below criteria.
Type of studies
The following study designs—as defined by the Cochrane guidelines49—were eligible for inclusion:
Randomised (including cluster-randomised) controlled trials (RCTs).
Quasi-randomised and non-RCTs including before and after studies with control group.
Case-control and cohort studies when they were related to a clearly specified intervention.
Studies using time-series and interrupted time-series design where there are three or more data points before and after the intervention, the intervention was introduced at specific time point, and the analysis took in to account the secular trend.
Observational studies using specific matching methods such as propensity score matching.
Types of participants/population
We included persons of all ages from any low-income and/or middle-income country according to the 2017 World Bank Country Classification by Income.50
Types of facility
We included studies conducted within primary, secondary and tertiary HCFs. Where HCFs were not already categorised as primary, secondary or tertiary we made this classification according to the following definitions:
Primary HCFs
Facilities which provide the first point of contact between individuals and the healthcare system, for example, general practice surgeries and community or allied health centres.
Secondary HCFs
Facilities providing treatment over a short period of time for a brief but serious illness, injury or other health condition, such as hospital emergency departments and outpatient clinics. Secondary HCFs are usually at the district or county level and cover childbirth, intensive care and medical imaging services, among other services.
Tertiary HCFs
Facilities providing specialised consultative care usually on referral from primary and secondary HCFs. Tertiary HCFs are usually at the regional or national level and include medical and teaching hospitals.
It should be noted that it can be difficult to distinguish between a secondary and tertiary HCF if there is no reference to patient referral. In these cases, we made a judgement based on the geographic level of the facility (district/county level or regional/national) and whether it was a specialist or teaching hospital. If this information was also not available, the HCF was classified as ‘secondary/tertiary’. Where the HCF was already classified by authors as primary, secondary or tertiary we simply adopted this.
Types of intervention(s), exposure(s)
We developed definitions for WASH interventions with specific regard to HCFs. However, these were broadly consistent with definitions used in previous reviews for the effect of household and community WASH interventions on other health outcomes and are in line with the WHO Essential Environmental Health Standards in Health Care (2008).26 We defined WASH interventions in HCFs under the below three categories.
Water
-
Any intervention to improve the microbiological quality of water at the HCF, including
Removing or inactivating microbiological pathogens (eg, water source level water treatment systems, filtration, sedimentation, chemical treatment, heat treatment, UV radiation, flocculation).
Protecting the microbiological quality of water prior to consumption (treatment, residual disinfection, protected distribution, improved storage).
Any intervention to provide a new and/or improved water supply or distribution system at the HCF, or both (eg, installation of piped water supply, installation of a hand pump, extension of the distribution network).
Any intervention to introduce or improve the quality of medical grade water (for autoclaving, medical procedures, sterilisation), water used for laundry, or water used for personal hygiene (ie, showering).
Sanitation
Any intervention to introduce, improve or expand the coverage of facilities for the safe management, disposal and treatment of excreta, that is, to reduce direct and indirect contact with human faeces (eg, pour flush, composting or water sealed flush toilet, piped sewer system, septic tank, simple pit latrines, VIP latrine or use of a potty or scoop for the disposal of child faeces).
Handwashing facilities
Any intervention to improve hand hygiene through improved availability and access to soap, sinks and other facilities.
Healthcare worker and patient WASH education
Interventions that promote or educate healthcare workers to improve any component from the above list. We also included any intervention that combined two or more of the above. There was no minimum duration of intervention.
Comparator(s)/control
The comparator/control was study participants who continued with usual practice, or a less stringent version of the intervention.
Types of outcome measure
Primary outcomes
HCAIs were subdivided into the following categories:
UTIs.
SSIs.
HAP.
VAP.
Vascular catheter-associated infection including bacteraemia/BSIs.
GSIs and other infections.
Secondary outcomes
Maternal or neonatal sepsis and/or tetanus infection.
Specific detail on an infection with an antimicrobial resistant organism.
Associated all-age, all-cause, neonatal, child and maternal mortality.
Care-seeking behaviour, experience of care.
Study selection, data extraction and analysis
All results retrieved from database searches were entered into Endnote X8 (Clarivate Analytics, Boston, Massachusetts, USA) and duplicates removed. Articles were independently screened in two stages: screening of titles and abstracts followed by the retrieval and screening of full-text articles by two reviewers (JW and LDG). Disagreements where resolved by a third reviewer (OC). All articles excluded during the full text review are listed in online Supplementary Appendix 1, with reasons for exclusion. Data from all relevant articles were independently extracted by two reviewers (JW and LDG) and cross-checked for accuracy. Data were extracted into a prespecified data extraction table on the following: (i) study authors and publication date (ii) study design, (iii) study setting (iv) study population, (v) population characteristics, (vi) participant selection, (vii) sample size, (viii) study duration, (ix) type of facility, (x) intervention, (xi) description of intervention, (xii) length of intervention and postintervention follow-up, (xiii) definition of HCAI used, (xiv) primary and secondary outcomes, (xv) any additional outcomes of interest (eg, length of hospitalisation), (xvi) laboratory-based outcome measurements, (xvii) effect estimate, (xviii) process and implementation factors, (xix) intervention uptake and (xxii) cost of intervention. A quantitative meta-analysis was not possible due to the limited number of studies, and the heterogeneity in study interventions and outcomes, and instead a narrative synthesis of results was undertaken. The review was reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.51
bmjgh-2019-001632supp001.pdf (73.8KB, pdf)
Risk of bias assessment
The risk of bias of each included study was independently assessed by two reviewers (JW and LDG) using the Cochrane Risk of Bias Tool for RCTs52 and the Newcastle-Ottawa risk of bias tool for cohort studies and case-control studies.53 Any discrepancies were resolved by a third author (OC).
Patient and public involvement
There was no patient or public involvement in this research.
Results
The results are reported in two parts—first the results of the systematic review, and second, the results of the supplementary scoping review.
Results of the systematic review
Search results
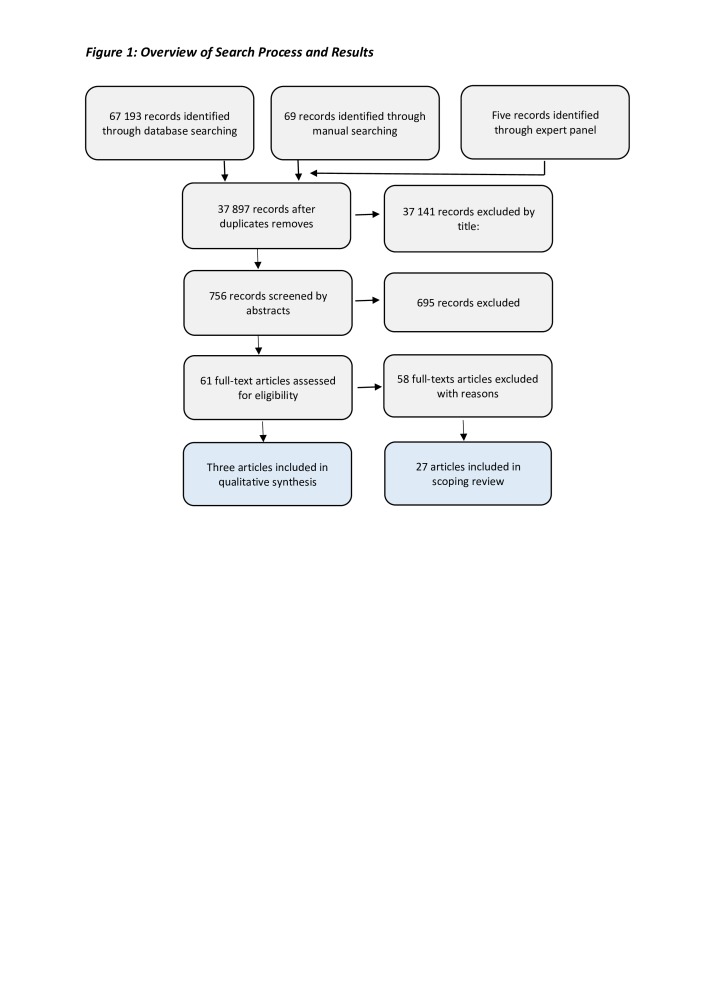
Searches identified a total of 67 267 records (67 193 through database searching, 69 through manual searching and five through consultation with experts). Full search strategies for bibliographic databases have been published in the DataCompass data repository54 and the search strategy is available in online Supplementary Appendix 2.
bmjgh-2019-001632supp002.pdf (122.8KB, pdf)
After de-duplication of records, a total of 37 897 records were screened by title and abstract and 61 studies selected for full text screening. Following assessment, only three studies met the inclusion criteria and were included in the qualitative synthesis. The study selection process is outlined in figure 1.
Figure 1.
Overview of search process and results.
Characteristics of included studies
Full details of the characteristics of the three included studies can be found in online Supplementary Appendix 3 and a brief overview in table 1.
Table 1.
Overview of included studies
| # | Study | Study design | Study population | WASH intervention component | Outcomes | Reduction in HCAI |
| a | Korbkitjaroen et al (2011)55 | Cluster randomised control trial | Adult patients (Mean age=60) |
Hand hygiene education+sterilisation of skin and equipment | Overall HCAIs | ✓ |
| Catheter associated-urinary tract infections | ✗ | |||||
| Ventilator-associated pneumonia | ✓ | |||||
| Catheter associated-bloodstream infections | ✓ | |||||
| b | Chen et al (2015)56 |
Cohort study | Neonates (preterm) Born <33 weeks gestational age (Mean age=2 days) |
Hand hygiene education | Invasive Candida infections | ✓ |
| c | Raza and Avan (2013) | Matched case-control study | Neonates (Ages not reported) |
Clean care delivery kits (soap, spirit for clean cord care, sterile equipment) | Neonatal tetanus infection | ✓ |
HCAI, healthcare-associated infection; WASH, water, sanitation and hygiene.
bmjgh-2019-001632supp003.pdf (64.3KB, pdf)
Study settings
All three studies took place in hospitals in urban settings across Asia classified as tertiary HCFs. One study, Korbkitjaroen et al, was conducted in Thailand,55 the second, Chen et al, in China,56 and the third, Raza and Avan, in Pakistan.57
Study design and length
Study duration ranged from 4 to 25 months. Korbkitjaroen et al reported a cluster RCT of a 4-month long intervention, Chen et al reported a 4-year retrospective cohort study assessing a 12-month long intervention, and Raza and Avan reported a matched case-control study assessing a 25-month long intervention.
Interventions and participants
The WASH interventions in all studies made up just one component of larger IPC bundles and are detailed in table 1.
The study in Korbkitjaroen et al tested an intervention where adult patients in general medical wards, at high risk of HCAIs (ie, patients required the use of an indwelling urethral or central vascular catheter, were immunocompromised, on antibiotic therapy or were immobilised), received general infection control measures as well as other specific infection control measures for identified risk factors. The WASH component of this consisted of healthcare worker education on hand hygiene and sterilisation of patient skin and medical equipment. The control group received only the general infection control measures.
The study in Chen et al had three cohorts of preterm neonatal infants in an intensive care unit—the control group, the fluconazole only intervention group who received prophylactic treatment with intravenous fluconazole, and the integrated measures intervention group who received treatment with fluconazole, and in addition, hand hygiene education was delivered to healthcare workers caring for these infants and supervision of hand hygiene was implemented.
The study in Raza and Avan assessed the use of clean care delivery kits by healthcare workers in two tertiary care hospitals. The kits included soap and gauze/spirit for clean cord care, a plastic sheet, a clean razor blade and clean string for tying the umbilical cord of neonatal infants post-delivery.
Outcomes
Korbkitjaroen et al measured catheter-associated UTIs (CA-UTIs), VAP, catheter-associated BSIs (CA-BSIs), overall rates of HCAIs (though this was not detailed further), and mortality due to HCAIs. Chen et al measured invasive Candida infections (ICIs) and infant mortality. Raza and Avan reported neonatal tetanus (NNT).
Korbkitjaroen et al reported that overall prevalence of HCAIs was significantly lower in the intervention wards compared with the control wards (5.6%, or 5.5 episodes/1000 hospitalisation days vs 9.2%, or 8.7 episodes/1000 hospitalisation-days, p=0.003). Rates of VAP and CA-UTIs were also significantly lower in the patients in the intervention wards (VAP rates in intervention group=6.5 episodes per 1000 respirator days vs VAP rates in the control group=16.3 episodes per 1000 respirator days, p=0.009; CA-UTI rates in intervention group=2.9 episodes per 1000 catheter days vs CA-UTI rates in control group=7.3 episodes per 1000 catheter days, p=0.013). The rate of CA-BSIs, however, did not differ significantly between the two groups (intervention group=2.9 episodes per 1000 catheter days and control group=3.9 episodes per 1000 catheter days, p=0.84). Mortality due to HCAIs was lower in the intervention group (15%) compared with the control group (37%), however this difference did not reach statistical significance (p=0.07).
Chen et al reported that the incidence of ICIs was significantly less frequent in the integrated measures group compared with the control group (p<0.001) and fluconazole only group (p=0.003); however, there was no significant difference between the control group and the fluconazole only group (p=0.5) suggesting that fluconazole prophylaxis alone does not significantly reduce the incidence of ICIs without promotion of hand hygiene. Mortality in the infants with ICIs was 9.5% in the control group, 5.6% in the fluconazole only group, and 0% in the integrated measures group though no significance tests were undertaken.
Raza and Avan found, after adjustment for socioeconomic factors, clean delivery kits were independently associated with reduced NNT (adjusted matched OR (amOR) 2.0; 95% CI 1.3 to 3.1). The association with clean delivery kits remained significant when additionally adjusted for attendance of skilled birth attendants (amOR 2.0; 95% CI 1.0 to 3.9; p=0.05).
None of the studies reported process or implementation factors, uptake or cost of the intervention.
Risk of bias assessment
None of the included studies were considered at a low risk of bias. Korbkitjaroen et al was an cRCT but did not specify the method of randomisation, was not able to blind participants or personnel to the intervention and did not adjust for potential confounders or control for clustering in the analysis. The cohort study design in Chen et al was inherently at a higher risk of bias, cohorts were not comparable on the basis of the design and the analysis did not adjust for potential confounders. The case-control study by Raza and Avan used a study design at high risk of bias and controls were poorly described. For detailed information on the risk of bias in each study, see online Supplementary Appendix 4.
bmjgh-2019-001632supp004.pdf (72.3KB, pdf)
Results of the supplementary scoping review
In our scoping review we extracted data from 27 before-after studies excluded from the systematic review. Two of these studies resembled interrupted time series studies but neither accounted for trends and did not have more than three data collection points in the post intervention period.58 These were reclassified as before-after studies and included in the scoping review. A summary of these studies can be found in table 2 and more details can be found in online Supplementary Appendix 5.
Table 2.
Summary of before-after studies
| # | Study | WASH intervention component | WASH only/combined intervention | Reduction in any HCAI |
| 1 | Abramczyk, 2011 |
Education on catheter hub disinfection | Combined | ✗ |
| 2 | Allegranzi, 2018 |
Education on hand hygiene and aseptic patient-care techniques. Provision of antiseptic soaps to patients | Combined | ✓ |
| 3 | Alp, 2014 |
Education on hand hygiene. Provision of hand basins, alcohol-based hand rub, and antiseptic soap. Daily chlorhexidine bathing of patients | Combined | ✓ |
| 4 | Alvarez-Moreno, 2016 | Education on hand hygiene and aseptic techniques | Combined | ✓ |
| 5 | Apisarnthanarak, 2014 | Education on hand hygiene. Disinfection of environment, patient bathing and oral hygiene with chlorhexidine | Combined | ✓ |
| 6 | Apisarnthanarak, 2010 | Education on hand hygiene and aseptic techniques. Provision of alcohol-based hand rub dispensers | Combined | ✓ |
| 7 | Azab, 2015 |
Education on hand hygiene. Sterilisation of equipment and antiseptic oral cleaning of patients | Combined | ✓ |
| 8 | Guanche-Garcell, 2013 | Education on hand hygiene. Antiseptic oral cleaning of patients. Hand hygiene compliance monitoring | Combined | ✓ |
| 9 | Jagi, 2013 |
Education on hand hygiene. Provision of chlorhexidine for skin preparation. Sterilisation of medical equipment | Combined | ✓ |
| 10 | Kurlat, 1998 |
Education on hand hygiene and sterilisation | Combined | ✓ |
| 11 | Leblebicioglu, 2013 | Education on hand hygiene. Disinfection of skin and equipment | Combined | ✓ |
| 12 | Leblebicioglu, 2013 | Education on hand hygiene. Disinfection of skin and equipment. Daily bathing with chlorhexidine | Combined | ✓ |
| 13 | Leblebicioglu, 2013 | Education on hand hygiene. Disinfection of skin and equipment. Patient oral care with antiseptic solution | Combined | ✓ |
| 14 | Lenz, 2018 |
Education on hand hygiene | Combined | ✓ |
| 15 | Marra, 2010 |
Education on hand hygiene. Disinfection of skin and equipment. Hand hygiene compliance monitoring | Combined | ✓ |
| 16 | Mehta, 2013 |
Education on hand hygiene. Antiseptic oral cleaning of patients | Combined | ✓ |
| 17 | Murni, 2015 |
Education on hand hygiene | Combined | ✓ |
| 18 | Navoa, 2013 |
Education on hand hygiene. Sterilisation of skin and equipment | Combined | ✓ |
| 19 | Ng Y.Y, 2015 |
Education on hand hygiene and aseptic techniques | WASH only | ✓ |
| 20 | Ogwang, 2013 |
Education on hand hygiene. Skin and equipment disinfection | Combined | ✓ |
| 21 | Rosenthal, 2006 |
Education on hand hygiene | Combined | ✓ |
| 22 | Rosenthal, 2005 |
Education on hand hygiene | WASH only | ✓ |
| 23 | Rosenthal, 2012 |
Education on hand hygiene. Disinfection of skin and equipment | Combined | ✓ |
| 24 | Rosenthal, 2012 |
Education on hand hygiene. Disinfection of skin and equipment | Combined | ✓ |
| 25 | Von Dolinger de Brito, 2007 | Provision of sinks, automated taps, paper towels and chlorhexidine dispensers for hand cleaning | Combined | ✓ |
| 26 | Zhou, 2015 |
Education on hand hygiene and sterile techniques. Easily accessible positioning of handwashing and hand disinfection facilities | Combined | ✓ |
| 27 | Zhou, 2013 |
Education on hand hygiene and waste segregation (separating normal and infectious waste). Ventilator disinfection | Combined | ✓ |
HCAI, healthcare-associated infection; WASH, water, sanitation and hygiene.
bmjgh-2019-001632supp005.pdf (442.6KB, pdf)
All 27 studies took place in hospitals which were classified as secondary or tertiary HCFs and all took place in urban settings, although one study also included HCFs in rural settings as well as urban. Nine studies assessed HCAIs across patients of all ages, eight studies assessed HCAIs in adult patients only, five studies assessed HCAIs in paediatric patients only and five studies assessed HCAIs in neonate patients only.
Only two studies assessed dedicated WASH interventions, that is, they were not combined with other non-WASH interventions. In all other studies, the WASH intervention formed just one component of a larger IPC strategy. All studies included a hygiene intervention. Hand hygiene was part of the hygiene intervention in 26 of the 27 studies. The majority of the hand hygiene interventions focused on hand hygiene education (25/26). Soap or alcohol-based hand rub was distributed in only five of these 26 studies and further handwashing infrastructure (sinks, automatic taps, paper towels) were provided in only two of the 26 studies. Other hygiene interventions among the 27 studies included education on equipment disinfection, aseptic techniques, patient hygiene (bathing and oral hygiene with chlorohexidine) and environmental cleaning. One study also included education on medical waste management. Of the 27 studies included in the scoping review, 26 reported a statistically significant reduction in at least one HCAI.
Discussion
This systematic review highlights a dearth of rigorous intervention studies preventing quantification of the causal effect of WASH in HCFs on HCAIs in LMICs. Only three studies met our predefined inclusion criteria. All reported statistically significant reductions in HCAIs, indicating a positive impact of WASH (specifically hygiene) interventions on HCAIs. Each of these were heterogenous in study design, intervention and outcome meaning a meta-analysis was not possible. Instead, we find a large observational literature exists, with various design deficits. Although low quality, existing studies consistently indicate a protective effect of HCF hygiene interventions on HCAIs and thus support the biological plausibility of inadequate WASH leading to HCAIs and reinforce the potential value of further research in this currently overlooked area. Qualitative synthesis of existing studies and the mapping of these studies to a conceptual framework presented here highlights a number of research priorities pertaining to WASH interventions in the control of HCAIs in HCFs in LMICs.
We identified many before-after studies that could not be included because they lacked a control group. The majority of these (26/27) support a positive effect of hygiene interventions and report a significant decrease in at least one HCAI. The large proportion of non-controlled before-after studies is likely due to the ethical difficulty in justifying the use of a control arm unless another alternative intervention is offered, and the additional resources required for this are likely prohibitive. While simple before-after studies may be the logical choice in terms of resources and ease, this study design is at high risk of bias. Risk factors for HCAIs may be different in the patient populations in the periods before and after the intervention and the design cannot control for contemporaneous changes in other elements of care making it difficult to infer causality. Advocating for more randomised controls may be unrealistic in the HCF setting but higher quality study designs which do not require a concurrent control group and are feasible to implement in this context should be considered.
In all studies included in the systematic review, the WASH interventions were only one component of broader IPC strategies and within the WASH interventions there were often various different intervention components. While it is widely accepted that the control of HCAIs requires a multi-pronged approach, studies assessing combined interventions are unable to identify the individual effects of each intervention component. There is no doubt that WASH services and practices are essential to a functioning HCF, however, incremental improvements to services and practices may be more appropriate, particularly in settings where resources are limited. Risk-based assessment and identification of the most effective intervention components will aid practitioners when prioritising improvements and allocating resources and could potentially save more lives.
The well-documented benefits of household and community WASH interventions for a range of infectious disease outcomes15 16 18–20 22 24 59–65 and consistently protective effect of the combined interventions included in this systematic review and scoping review support the widely held, if poorly researched view that WASH in HCFs are a fundamental component of effective IPC. While this view may be widely held, the reality in LMICs is that WASH infrastructure and interventions are often overlooked. This is evident across the interventions reported in our systematic and scoping reviews where few (17%) included provisions of soap or alcohol-based hand rub and even fewer (10%) included handwashing-related infrastructural improvements.
To specify the salient evidence gaps in order to support future research efforts, we mapped the WASH interventions identified in our review to a conceptual framework of the pathways between inadequate WASH and HCAIs. The conceptual framework linking poor WASH in HCF with HCAIs identifies both direct pathways, namely the transmission of pathogens from the environment to the patient and resultant HCAI; and indirect pathways, namely the ability of WASH, used by the healthcare worker or patient, to provide safe and clean healthcare environments and adequate quality of care. The framework is shown in figure 2 (the letters and numbers in the boxes refer to the studies in tables 1 and 2).
Figure 2.
Conceptual framework visualising the relationship between water, sanitation and hygiene (WASH) and healthcare-associated infections (HCAIs).
As can be observed in the conceptual framework, this review identified only one study which included medical waste management as part of the intervention. No study assessed an intervention to improve water quality or quantity, or sanitation facilities. Hand hygiene education, in particular, featured most prominently. As most HCAIs are transmitted via the hands of healthcare workers or patients through direct contact or environmental contamination, hand hygiene is recognised as one of the most important means to reduce HCAIs.66 However, more research is needed to ascertain which other WASH interventions are the among the most effective at reducing HCAIs in these settings, and therefore should be prioritised, and to what extent they are reliant on the concurrent delivery of other IPC interventions.
Further important research gaps highlighted by this review include the effect of WASH on HCAIs in primary HCFs (we found no studies conducted in primary HCFs) and in rural settings. This is particularly relevant in LMICs where access to secondary and tertiary level HCFs is generally more limited, particularly for rural populations. Given high HCAI rates in LMICs and given that WASH coverage tends to be lowest in primary HCFs,67 addressing this gap should be a priority in future research.
This review has a number of limitations. First, the exclusion of non-controlled before-after studies from our systematic review subsequently excluded the majority of existing studies assessing the impact of WASH interventions on HCAIs. This decision was made a priori as this study design is highly vulnerable to confounding and other biases and cannot be used to reliably estimate causal effects. However, on finding so few studies that met our inclusion criteria, we deemed it beneficial to extract data from these before-after studies in a subsequent scoping review to allow us to make a broader qualitative assessment of WASH in HCFs and to more realistically reflect the repertoire of available evidence. Second, of the three studies we included in the systematic review, only one was a randomised control trial and the other two were also observational studies and hence also inherently at high risk of bias. Further limitations of these studies included the lack of blinding, failure to control for confounding variables, and assumed intervention exposure; none of the researchers measured compliance to the interventions and whether the healthcare workers received the intervention in a consistent and complete manner during the intervention period. Finally, the inclusion of only English language papers may have excluded valid international work.
Conclusion
Previous systematic reviews have considered the impact of WASH interventions at the community and household level on different health outcomes in LMICs, but this is the first review to consider the effect of WASH in HCFs on HCAIs. No studies were identified for the effect of water or sanitation interventions in HCF but three studies of hygiene interventions in HCF were identified which all showed protective effects. These consistently protective effects provide some evidence for their continuing priority, but additional and higher quality evidence is urgently needed to identify the most effective and efficient interventions to support broader strategies for HCAI prevention and control in LMICs. Our accompanying scoping review, and the resulting conceptual framework, can guide future research efforts in this area to address the major gaps identified in the evidence base.
Footnotes
Handling editor: Seye Abimbola
Contributors: LDM-G, EF, JF, JE-M, AP, PH, BA, MM and OC conceived the idea for the review and contributed to the published protocol. LDM-G, JF and OC developed the search strategies. LDM-G and JF executed the searches. JF conducted screening of titles and JW, LDM-G and OC screened abstracts and full texts for inclusion. JW, LDM-G and OC extracted data from studies. JW and LDM-G conducted a risk of bias assessment and synthesised results. JW, LDM-G and OC prepared first draft of manuscript. All authors contributed to later drafts of the manuscript. The corresponding author (JW) attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted. JW and LDM-G contributed equally to this paper.
Funding: This review received funding from WHO, Unicef and DFID through the SHARE Research Programme. The funders had no institutional involvement in the study design, collection, analysis and interpretation of the data, in the writing of the report, or in the decision to submit the paper for publication. Authors from WHO (MM, BA) and Unicef (AP) contributed independently in their own right as individuals.
Disclaimer: The authors alone are responsible for the views expressed in this article and they do not necessarily represent the views, decisions or policies of the institutions with which they are affiliated. WHO takes no responsibility for the information provided or the views expressed in this paper.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: All data relevant to the study are included in the article or uploaded as supplementary information.
References
- 1.Allegranzi B, Bagheri Nejad S, Combescure C, et al. . Burden of endemic health-care-associated infection in developing countries: systematic review and meta-analysis. Lancet 2011;377:228–41. 10.1016/S0140-6736(10)61458-4 [DOI] [PubMed] [Google Scholar]
- 2.Garner JS, Jarvis WR, Emori TG, et al. . CDC definitions for nosocomial infections, 1988. Am J Infect Control 1988;16:128–40. 10.1016/0196-6553(88)90053-3 [DOI] [PubMed] [Google Scholar]
- 3.WHO Report on the burden of endemic health care-associated infection worldwide. Geneva, Switzerland: World Health Organisation, 2011. [Google Scholar]
- 4.O'Neill J. Infection Prevention, Control and Surevillance: Limiting the development and spread of drug resistance : O'Neill J, The review on Antimicrobial resistance. London, UK, 2016. [Google Scholar]
- 5.Zaidi AKM, Huskins WC, Thaver D, et al. . Hospital-acquired neonatal infections in developing countries. The Lancet 2005;365:1175–88. 10.1016/S0140-6736(05)71881-X [DOI] [PubMed] [Google Scholar]
- 6.Kassebaum NJ, Bertozzi-Villa A, Coggeshall MS, et al. . Global, regional, and national levels and causes of maternal mortality during 1990-2013: a systematic analysis for the global burden of Disease Study 2013. Lancet 2014;384:980–1004. 10.1016/S0140-6736(14)60696-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sobhy S, Arroyo-Manzano D, Murugesu N, et al. . Maternal and perinatal mortality and complications associated with caesarean section in low-income and middle-income countries: a systematic review and meta-analysis. The Lancet 2019;393:1973–82. 10.1016/S0140-6736(18)32386-9 [DOI] [PubMed] [Google Scholar]
- 8.Biccard BM, Madiba TE, Kluyts H-L, et al. . Perioperative patient outcomes in the African surgical outcomes study: a 7-day prospective observational cohort study. The Lancet 2018;391:1589–98. 10.1016/S0140-6736(18)30001-1 [DOI] [PubMed] [Google Scholar]
- 9.Kruk ME, Leslie HH, Verguet S, et al. . Quality of basic maternal care functions in health facilities of five African countries: an analysis of national health system surveys. Lancet Glob Health 2016;4:e845–55. 10.1016/S2214-109X(16)30180-2 [DOI] [PubMed] [Google Scholar]
- 10.WHO Health care without avoidable infections:The critical role of infection prevention and control. Geneva, Switzerland: WHO, 2016. [Google Scholar]
- 11.Hanberger H, Walther S, Leone M, et al. . Increased mortality associated with meticillin-resistant Staphylococcus aureus (MRSA) infection in the intensive care unit: results from the EPIC II study. International Journal of Antimicrobial Agents 2011;38:331–5. 10.1016/j.ijantimicag.2011.05.013 [DOI] [PubMed] [Google Scholar]
- 12.Graham WJ, Morrison E, Dancer S, et al. . What are the threats from antimicrobial resistance for maternity units in low- and middle- income countries? Global Health Action 2016;9 10.3402/gha.v9.33381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bartram J, Cairncross S, Hygiene CS. Hygiene, sanitation, and water: forgotten foundations of health. PLoS Med 2010;7:e1000367 10.1371/journal.pmed.1000367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Esrey SA, Potash JB, Roberts L, et al. . Effects of improved water supply and sanitation on ascariasis, diarrhoea, dracunculiasis, hookworm infection, Schistosomiasis, and trachoma. Bull World Health Organ 1991;69:609–21. [PMC free article] [PubMed] [Google Scholar]
- 15.Clasen TF, Alexander KT, Sinclair D, et al. . Interventions to improve water quality for preventing diarrhoea. Cochrane Database Syst Rev 2015;12 10.1002/14651858.CD004794.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Clasen TF, Bostoen K, Schmidt W-P, et al. . Interventions to improve disposal of human excreta for preventing diarrhoea. Cochrane Database Syst Rev 2010;84 10.1002/14651858.CD007180.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fink G, Günther I, Hill K. The effect of water and sanitation on child health: evidence from the demographic and health surveys 1986–2007. International Journal of Epidemiology 2011;40:1196–204. 10.1093/ije/dyr102 [DOI] [PubMed] [Google Scholar]
- 18.Peletz R, Mahin T, Elliott M, et al. . Water, sanitation, and hygiene interventions to improve health among people living with HIV/AIDS. AIDS 2013;27:2593–601. 10.1097/QAD.0b013e3283633a5f [DOI] [PubMed] [Google Scholar]
- 19.Ejemot-Nwadiaro RI, Ehiri JE, Arikpo D, et al. . Hand washing promotion for preventing diarrhoea. Cochrane Database Syst Rev 2015;127 10.1002/14651858.CD004265.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dangour AD, Watson L, Cumming O, et al. . Interventions to improve water quality and supply, sanitation and hygiene practices, and their effects on the nutritional status of children. Cochrane Database Syst Rev 2013;37 10.1002/14651858.CD009382.pub2 [DOI] [PubMed] [Google Scholar]
- 21.Ejere HO, Alhassan MB, Rabiu M. Face washing promotion for preventing active trachoma. Cochrane Database Syst Rev 2012;4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Grimes JET, Croll D, Harrison WE, et al. . The relationship between water, sanitation and schistosomiasis: a systematic review and meta-analysis. PLoS Negl Trop Dis 2014;8:e3296 10.1371/journal.pntd.0003296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.FitzGerald D, Grainger RJ, Reid A, et al. . Interventions for preventing the spread of infestation in close contacts of people with scabies. Cochrane Database Syst Rev 2014;74 10.1002/14651858.CD009943.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Freeman MC, Strunz E, Utzinger J, et al. . Interventions to improve water, sanitation, and hygiene for preventing soil-transmitted helminth infection. Cochrane Database Syst Rev 2016;5:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Burton M, Habtamu E, Ho D, et al. . Interventions for trachoma trichiasis. Cochrane Database Syst Rev 2015;40 10.1002/14651858.CD004008.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.WHO Essential environmental health standards in health care. Geneva, Switzerland: World Health Organisation, 2008. [Google Scholar]
- 27.WHO Who guidelines on hand hygiene in health care. First global patient safety challenge: clean care is safer care. Geneva, Switzerland: World Health Organisation, 2009. [PubMed] [Google Scholar]
- 28.Robinson J. A treatise on the epidemic puerperal fever of Aberdeen. London, 1795. [PubMed] [Google Scholar]
- 29.Gould IM. Alexander Gordon, puerperal sepsis, and modern theories of infection control—Semmelweis in perspective. The Lancet Infectious Diseases 2010;10:275–8. 10.1016/S1473-3099(09)70304-4 [DOI] [PubMed] [Google Scholar]
- 30.Semmelwis I. The etiology. the Concept and the Prophlyaxis of Childbed Fever Open Letters to Sundry Professors of Obstetrics 1861. [Google Scholar]
- 31.Benova L, Cumming O, Campbell OMR. Systematic review and meta-analysis: association between water and sanitation environment and maternal mortality. Trop Med Int Health 2014;19:368–87. 10.1111/tmi.12275 [DOI] [PubMed] [Google Scholar]
- 32.Benova L, Cumming O, Gordon BA, et al. . Where there is no toilet: Water and sanitation environments of domestic and facility births in Tanzania. PLoS ONE 2014;9:e106738 10.1371/journal.pone.0106738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Blencowe H, Cousens S, Mullany LC, et al. . Clean birth and postnatal care practices to reduce neonatal deaths from sepsis and tetanus: a systematic review and Delphi estimation of mortality effect. BMC Public Health 2011;11(Suppl 3). 10.1186/1471-2458-11-S3-S11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.WHO Core components for infection prevention and control programmes : Otaíza CP-S F, Report of the second meeting informal network on infection prevention and control in health care. Geneva, Switzerland: World Health Organisation, 2009. [Google Scholar]
- 35.UN Call to action on WASH in HCF, 2018. Available: https://news.un.org/en/story/2018/03/1005671 [Accessed 22/03/2018].
- 36.Water WHO. Sanitation and hygiene in health care facilities – urgent needs and actions. Geneva. 36 Switzerland: World Health Organisation/UNICEF, 2015. [Google Scholar]
- 37.Allegranzi B, Kilpatrick C, Storr J, et al. . Global infection prevention and control priorities 2018-22: a call for action. Lancet Glob Health 2017;5:e1178–80. 10.1016/S2214-109X(17)30427-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.World Health Organization and UNICEF Water, sanitation and hygiene in health care facilities: practical steps to achieve universal access to quality care. Geneva.: World Health Organization, 2019. [Google Scholar]
- 39.Assembly UG. Stigma and the realization of the human rights to water and sanitation. in: sanitation. USRothrtsdwa, ed. Geneva, Switzerland: United Nations 2012.
- 40.World Health Organization Water, sanitation and hygiene in health care facilities: 144th session, agenda item 6.6. 2019.; (EB144/30). Available: http://apps.who.int/gb/ebwha/pdf_files/EB144/B144_R5-en.pdf [Accessed 31st March 2019].
- 41.World Health Organization and UNICEF Water, sanitation and hygiene in health care facilities. Global baseline report 2019. Geneva: World Health Organization, 2019. [Google Scholar]
- 42.Harbarth S, Sax H, Gastmeier P. The preventable proportion of nosocomial infections: an overview of published reports. J Hosp Infect 2003;54:258–66. 10.1016/S0195-6701(03)00150-6 [DOI] [PubMed] [Google Scholar]
- 43.Pickering AJ, Djebbari H, Lopez C, et al. . Effect of a community-led sanitation intervention on child diarrhoea and child growth in rural Mali: a cluster-randomised controlled trial. The Lancet Global Health 2015;3:e701–11. 10.1016/S2214-109X(15)00144-8 [DOI] [PubMed] [Google Scholar]
- 44.Campbell OMR, Benova L, Gon G, et al. . Getting the basic rights - the role of water, sanitation and hygiene in maternal and reproductive health: a conceptual framework. Trop Med Int Health 2015;20:252–67. 10.1111/tmi.12439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Velleman Y, Mason E, Graham W, et al. . From joint thinking to joint action: a call to action on improving water, sanitation, and hygiene for maternal and newborn health. PLoS Med 2014;11:e1001771 10.1371/journal.pmed.1001771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pittet D, Donaldson L. Clean care is safer care: a worldwide priority. The Lancet 2005;366:1246–7. 10.1016/S0140-6736(05)67506-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.UN Sustainable development goals: un, 2015. Available: https://sustainabledevelopment.un.org/?menu=1300 [Accessed 02 Sept 2016].
- 48.D'Mello-Guyett L, Flynn E, Falconer J, et al. . Interventions to improve drinking water supply and quality, sanitation and hand washing facilities in health care facilities, and their effect on health care-associated infections in low and middle income countries. PROSPERO International prospective register of systematic reviews: University of York, 2018. [Google Scholar]
- 49.The Cochrane Collaboration Glossary of Cochrane terms. Available: https://community.cochrane.org/glossary [Accessed cited 2019 27th February].
- 50.World Bank World bank country and lending groups: world bank list of economies (July 2016), 2017. Available: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups [Accessed cited 2019 28th March].
- 51.Moher D, Liberati A, Tetzlaff J, et al. . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Medicine 2009;6:e1000097 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Higgins JPT, Altman DG, Gøtzsche PC, et al. . The Cochrane collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011;343 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wells G, Shea B, O’Connell D, et al. . The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses 2008.
- 55.Falconer J. Search strategies for: "Interventions to improve drinking water supply and quality, sanitation and handwashing facilities in health care facilities, and their effect on health care-associated infections in low and middle-income countries: A systematic review and supplementary scoping review. London, United Kingdom: London School of Hygiene and Tropical Medicine, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Korbkitjaroen M, Vaithayapichet S, Kachintorn K, et al. . Effectiveness of comprehensive implementation of individualized bundling infection control measures for prevention of health care–associated infections in general medical wards. American Journal of Infection Control 2011;39:471–6. 10.1016/j.ajic.2010.09.017 [DOI] [PubMed] [Google Scholar]
- 56.Chen J, Yu X, Zhou Y, et al. . Integrated measures for prevention of invasive Candida infections in preterm infants in a Chinese neonatal intensive care unit. American Journal of Infection Control 2015;43:1321–5. 10.1016/j.ajic.2015.07.011 [DOI] [PubMed] [Google Scholar]
- 57.Raza SA, Avan BI. Disposable clean delivery kits and prevention of neonatal tetanus in the presence of skilled birth attendants. Int J Gynaecol Obstet 2013;120:148–51. [DOI] [PubMed] [Google Scholar]
- 58.Cochrane Effective Practice and Organisation of Care (EPOC) Interrupted time series (its) analyses.: EPOC resources for review authors, 2017. Available: https://epoc.cochrane.org/resources/epoc-resources-review-authors
- 59.Fewtrell L, Kaufmann RB, Kay D, et al. . Water, sanitation, and hygiene interventions to reduce diarrhoea in less developed countries: a systematic review and meta-analysis. The Lancet Infectious Diseases 2005;5:42–52. 10.1016/S1473-3099(04)01253-8 [DOI] [PubMed] [Google Scholar]
- 60.Stelmach R, Clasen T. Household water quantity and health: a systematic review. IJERPH 2015;12:5954–74. 10.3390/ijerph120605954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ziegelbauer K, Speich B, Mäusezahl D, et al. . Effect of sanitation on soil-transmitted helminth infection: systematic review and meta-analysis. PLoS Med 2012;9:e1001162 10.1371/journal.pmed.1001162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Stocks ME, Ogden S, Haddad D, et al. . Effect of water, sanitation, and hygiene on the prevention of trachoma: a systematic review and meta-analysis. PLoS Med 2014;11:e1001605 10.1371/journal.pmed.1001605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Rabie T, Curtis V. Handwashing and risk of respiratory infections: a quantitative systematic review. Trop Med Int Health 2006;11:258–67. 10.1111/j.1365-3156.2006.01568.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Groce N, Bailey N, Lang R, et al. . Water and sanitation issues for persons with disabilities in low- and middle-income countries: a literature review and discussion of implications for global health and international development. Journal of Water and Health 2011;9:617–27. 10.2166/wh.2011.198 [DOI] [PubMed] [Google Scholar]
- 65.Wolf J, Hunter PR, Freeman MC, et al. . Impact of drinking water, sanitation and handwashing with soap on childhood diarrhoeal disease: Updated meta-analysis and meta-regression. Trop Med Int Health 2018;23:508–25. 10.1111/tmi.13051 [DOI] [PubMed] [Google Scholar]
- 66.Mathur P. Hand hygiene: back to the basics of infection control. Indian J Med Res 2011;134:611–20. 10.4103/0971-5916.90985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.World Health Organization and UNICEF Water, sanitation and hygiene in health care facilities: status in low and middle income countries and way forward. Geneva World Health Organization, 2015. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2019-001632supp001.pdf (73.8KB, pdf)
bmjgh-2019-001632supp002.pdf (122.8KB, pdf)
bmjgh-2019-001632supp003.pdf (64.3KB, pdf)
bmjgh-2019-001632supp004.pdf (72.3KB, pdf)
bmjgh-2019-001632supp005.pdf (442.6KB, pdf)