Abstract
Parents play a critical role in children,s experience of, and recovery from, chronic pain. Although several parental factors have been linked to child pain and functioning, these factors are typically examined in isolation or as moderators or mediators. Structural equation modeling affords the opportunity to examine the extent to which parental factors are interrelated, and if there are differential associations among parental factors and child outcomes. Based on extant literature, a unified model of parental factors, including chronic pain status, physical functioning, responses to child pain, and psychological factors, and their effect on child pain and functioning, was conceptualized. This model was evaluated using structural equation modeling based on data from 146 dyads recruited from a multidisciplinary pain clinic. Modifications to model iterations were made based on theoretical and statistical justification. The final model revealed associations among all parental factors, with significant loadings on child pain and functioning. Findings indicated the conceptual model was supported, with the exception of parent responses to child pain. Findings support the inclusion of parent chronic pain status and physical and psychological functioning as part of a comprehensive assessment of youth with chronic pain and may inform new parental intervention targets to improve child outcomes.
Perspective:
A unified structural equation model indicated parents, own chronic pain characteristics and physical and psychological functioning represent important factors associated with child pain and functioning. Current family-based interventions that often primarily focus on parent responses to child pain may need to be adapted to more comprehensively address parental factors.
Keywords: Parents, youth, chronic pain, anxiety, protectiveness
Parents are important influencers of symptoms and functioning in youth with chronic pain.37 A number of parental factors are associated with child pain and functioning, including responses to child pain (eg, protectiveness),10,33 psychological functioning (eg, anxiety),4,34 and chronic pain history.4,7,22,40 However, these parental factors typically have been evaluated as separate domains with few studies examining their interrelations.28,30,37,45,46,56 Understanding the extent to which parental factors are interrelated, and exhibit differential associations with child adjustment to chronic pain may help to improve interventions for parents of youth with chronic pain.
One approach to examining the interrelation of multiple parental factors is to evaluate a theoretically derived structural equation model. For example, Vowles and colleagues55 found support for a theoretical model that included caregiver responses to adolescent pain and adolescent,s own psychological responses to pain as interrelated constructs that individually covaried with adolescent functioning. One limitation was the omission of parent chronic pain and psychological status, which could be associated with child adjustment to chronic pain. Indeed, parent chronic pain status heightens the risk for a child’s chronic pain maintenance into adulthood.1,44 Further, greater parent psychological distress (eg, anxious response, protective behavior) and cata-strophizing about child pain have been associated with poorer child adjustment to chronic pain.26 However, owing to the high comorbidity between chronic pain and anxiety and depressive disorders,15,31,44 it is difficult to disentangle whether associations between parent chronic pain and child adjustment to chronic pain are due to the association between parent chronic pain and increased parent psychological distress or if each exhibit unique associations with children,s pain.
Further, the relation between parent chronic pain and psychological status and child pain and function could be explained by social learning factors, specifically parental modeling of pain behaviors or behavioral responses to child pain. Parental modeling has traditionally been inferred based on the presence of a parent with chronic pain. However, for modeling to occur, parents need to display pain behaviors that a child can observe. Modeling may be better captured by assessing parents, own pain-related behaviors instead of pain status.48,49 In adults with chronic pain, greater depressive symptoms and catastrophizing have been associated with greater disability and pain chronicity38; thus, both parent chronic pain and psychological symptoms could be associated with greater modeling of pain behaviors.
Greater parent anxiety, catastrophizing about child pain, and parent chronic pain have been associated with more protective responses to child pain.30,45,58 Both parent protective responses and parent modeling of pain behaviors are associated with greater pain, functional impairment, and emotional distress in children with chronic pain.6,7,19,22 However, emerging evidence suggests that the association between parent chronic pain and child outcomes is more strongly accounted for by parent modeling of pain behaviors than parent reinforcement of child pain.48 Therefore, when considering a comprehensive model of parental factors, parental factors (eg, protective responses, anxiety, catastrophizing) that have exhibited statistical significance in univariate models may exhibit substantially weaker associations when taking into account other parental factors.
Evaluating parent chronic pain status, parent psychological status, parent pain-related functioning (as a proxy for parental modeling of pain behaviors), and parent reinforcement of child pain as separate, but potentially interrelated, factors may elucidate which parental factors are most closely related to child pain and psychological functioning. Thus, this study evaluated a comprehensive model of parental factors that may be associated with chronic pain in youth. The hypothesized model (Fig 1) included parent chronic pain features (ie, chronic pain status, number of pain locations, pain frequency, pain intensity), parent physical function as a proxy for parental modeling (ie, pain interference, physical function), parent psychological factors (ie, anxiety, depressive symptoms, catastrophizing about their child’s pain), and parent behavioral responses to child pain (ie, protectiveness, monitoring) as interrelated, but distinct, constructs that covary with child pain and functioning and psychological symptoms. It was hypothesized that all parent constructs would be uniquely associated with child pain and function and child psychological factors.
Fig 1.
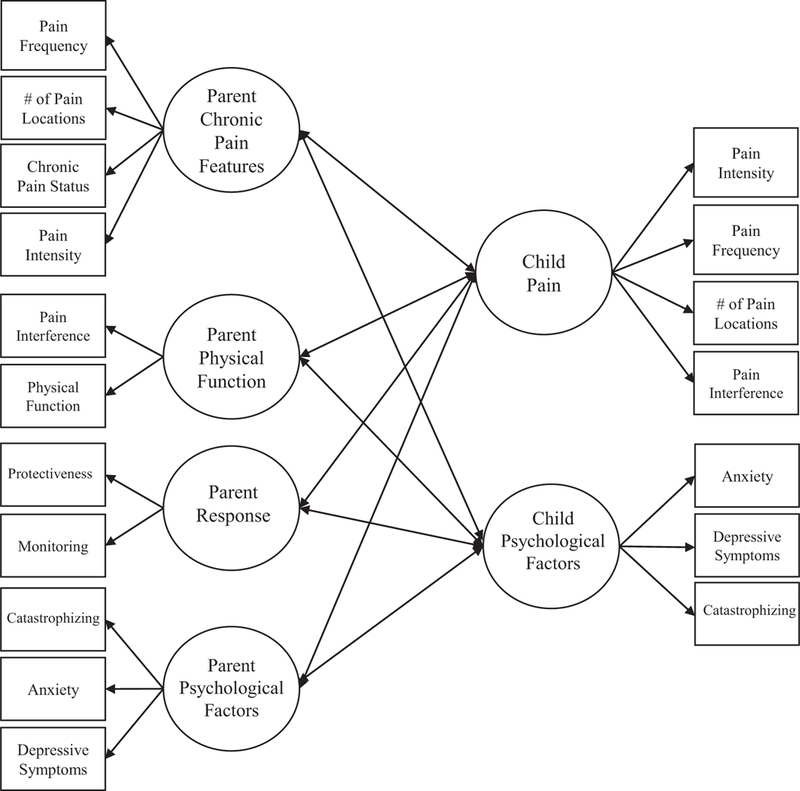
Hypothesized model of parental factors that may influence youth with chronic pain.
Methods
Participants
Participants included 146 children with chronic pain, and one of their parents. Children and parents were recruited from multidisciplinary pain assessment clinics within an outpatient pediatric pain program at a tertiary-level children’s hospital in Western Canada. Children were eligible if they had a diagnosis of a pain-related condition (eg, functional or recurrent abdominal pain, generalized pain disorder, headaches, musculoskeletal pain), reported pain lasting ≥3 months, were between 8 and 18 years old, and had English language fluency. Exclusion criteria included a diagnosis of a developmental disorder as reported by the parent. Parents were eligible if they had English language fluency.
Procedure
Potential participants were identified from the clinic schedules of complex pain, headache pain, and abdominal pain clinics of an outpatient pain program. A member of the clinic staff obtained permission from potential participants to contact them for research purposes and gave the contact information of interested patients to the research team. Before the child’s initial clinic appointment, a research assistant contacted parents via telephone with information about the study. A consent conference call with interested participants was then completed to screen for eligibility, explain the study procedures, and answer questions about the study. Once verbal consent was obtained, a research assistant emailed the parent and youth links to online consent and assent forms. Finally, written hardcopy consent and assent were also obtained at the time of the initial clinic appointment.
Parents and children completed self-report questionnaires at the time of their initial clinic appointment using Research Electronic Data Capture (REDCap), a secure online data collection tool.18 Parents and children were contacted up to 3 times with reminders to complete the questionnaires. The institutional research ethics board approved all study procedures.
Measures
Demographic Characteristics
Parents completed a measure of demographics that captured information about child age and school grade, child and parent gender, ethnicity, parent marital status, and annual household income.
Pain Characteristics
Parent and child pain characteristics were assessed through self-report using the well-validated Pain Questionnaire.36 Parent chronic pain status was identified using a single yes/no item that asked about a pain problem that had been present for ≥3 months and had been >0 on a 0 to 10 pain intensity scale in the last month. This assessment of chronic pain is consistent with the current definition endorsed by the International Association for the Study of Pain20 and aligns with previous epidemiologic research on chronic pain.50 Parents were asked to report on the frequency of their pain in the past week using a 5-point Likert scale with anchors of not at all and daily. Children rated the frequency of their pain on a 5-point Likert scale with anchors of always present and rarely present. Pain intensity was measured in parents and children using an 11-point Numerical Rating Scale with anchors of no pain and worst pain possible.54 Validated body maps2,42 were used to report on the number of body locations in which parents and children have pain. The Pain Questionnaire has demonstrated adequate validity36 and the single-item Numerical Rating Scale measure of pain intensity is well-validated.5,41,47,54
Child Pain Interference, Anxiety, and Depressive Symptoms
Children completed the 4-item pain interference, anxiety, and depressive symptoms subscales of the Patient-Reported Outcomes Measurement Information System (PROMIS)-25 Profile. The pain interference subscale was used to measure the degree to which children experienced impairment owing to their pain. Children rated how often pain interfered with daily activities such as sleeping and walking in the past week on a 5-point Likert scale with anchors of never and almost always. The anxiety subscale was used to measure children’s anxiety.
Children rated how often in the past week they experienced core anxiety symptoms such as feeling nervous or that something awful might happen on a 5-point Likert scale with anchors of never and almost always. The depressive symptoms subscale was used to measure children’s depressive symptoms. Children rated how often in the past week they experienced core depression symptoms such as feeling sad or that it was hard for me to have fun on a 5-point Likert scale with anchors of never and almost always. The PROMIS-25 Profile was developed by the National Institutes of Health using item response theory. The pain interference, anxiety, and depressive symptoms subscales of the PROMIS-25 have demonstrated construct validity and convergent validity with other legacy measures among youth with chronic pain.23,53
Parent Pain Interference, Physical Functioning, Anxiety, and Depression
Parents completed the 4-item pain interference, physical function, anxiety, and depression subscales of the PROMIS-29 Profile. The pain interference subscale was used to measure the degree to which parents experienced impairment owing to their own pain. Parents rated how often pain interfered with daily activities such as household chores in the past week on a 5-point Likert scale with anchors of not at all and very much. On the physical function subscale, parents rated their ability to engage in various physical activities (eg, going for a walk for 15 minutes, going up and down stairs at a normal pace) on a 5-point Likert scale with anchors of without any difficulty and unable to do. The anxiety subscale was used to measure parents’ anxiety symptoms. Parents rated how often in the past week they had anxious thoughts or feelings (eg, I felt fearful) on a 5-point Likert scale with anchors of never and always. The depression subscale was used to measure parents’ depressive symptoms. Parents rated how often in the past week they experienced depressive symptoms such as feeling worthless or hopeless on a 5-point Likert scale with anchors of never and always. The PROMIS-29 Profile was developed by the National Institutes of Health using item response theory. The pain interference, physical function, anxiety, and depression subscales have all been validated among adults with chronic pain,14 and demonstrate good internal consistency, substantial test–retest reliability, and established construct validity. The anxiety and depression subscales have also shown strong convergent validity with other legacy measures in chronic pain patients.24 Values were converted to T-scores for ease of use and interpretability.
Parent Responses to Child Pain
Parent behavioral responses to child pain were assessed using the parent-report Protect and Monitoring subscales of the Adult Responses to Children’s Symptoms with a pain-specific stem.33,52 Parents were asked to respond to 17 statements about how often they engage in protective (eg, bring your child special treats or little gifts) or monitoring (eg, ask your child what you can do to help, try to make your child as comfortable as possible) behaviors when their child has pain on a 5-point Likert scale with anchors of never and always. Scores for the subscale were computed as averages, with higher scores indicating greater occurrence of the behavior. The protect subscale of the Adult Responses to Children’s Symptoms is widely used, and has established external validity,57 showing strong associations with self-reported parent behaviors, and good internal consistency. The monitoring subscale has been linked to child pain and functioning.13 The factor validity of the protect and monitoring subscales for a combined sample of children and adolescents (7–18 years) with chronic pain has been established, with good fit indices.33
Pain Catastrophizing
Child and parent catastrophizing about child pain were assessed using the Pain Catastrophizing ScaleChild Version (PCS-C) and the Pain Catastrophizing Scale-Parent Version (PCS-P).12,16 The PCS-C is composed of 13 items that assess thoughts and feelings children may have when they are in pain (eg, “When I am in pain, I worry all the time about whether the pain will end.”). The PCS-P is composed of the same 13 items, but asks about thoughts and feelings parents may have when their child is in pain (eg, “When my child is in pain, I can’t keep it out of my mind.”). Children and parents rate how strongly they have these thoughts and feelings on a 5-point Likert scale with anchors of not at all and extremely. Total scores are obtained by summing the items, with higher scores indicating greater catastrophizing about child pain. The PCS-C and PCS-P have demonstrated good validity and reliability, and have been previously validated among children with chronic pain and their parents.12,16
Data Analysis
Measurement and structural modeling was performed in Mplus 7.0.32 Model specifications included correlated factors, uncorrelated error terms, and factor variances set to 1. Several variables (ie, parent pain frequency, parent pain problem, child pain frequency) were classified as categorical to account for the ordinal nature of the responses. Weighted least squares with mean and variance adjustment estimation procedures were used, as this estimator tends to be more appropriate for data that are categorical or not normally distributed.32,43
Model fit statistics were used to evaluate the degree to which the hypothesized model fit the observed data. All models were evaluated by examining the χ2 test of significance, which indicates the overall fit of the model. Because the χ2 statistic may be sensitive to large degrees of freedom and sample size, other fit indices were evaluated using guidelines put forth by Little,29 including the root mean squared error of approximation, comparative fit index, Tucker–Lewis index, and weighted root mean square residual. Model fit was considered to have acceptable fit if the root mean squared error of approximation was <.08 (good <.06); the comparative fit index and Tucker-Lewis index values were deemed acceptable >.90 (close >.95),19,39 and the weighted root mean square residual of <1.0 were deemed acceptable.11 In addition to fit indices, localized areas of strain were also used to inform model changes. Modification indices greater than 10% of the χ2 were evaluated and theoretical justification was used to determine the clinical utility of stepwise changes to the proposed model structure.17
Results
Participant Sociodemographic and Pain Characteristics
Table 1 summarizes participant characteristics. Participating children were primarily female (68.5%) with a mean age of 12.97 years (standard deviation [SD] = 2.78). Pain presentations were varied and tended to be-specific (73.6%; eg, abdominal pain, headache) or more general (18.7%; eg, musculoskeletal, neuropathic pain). The remaining parents (7.6%) identified their child’s primary pain complaint as other, but did not provide further information. No diagnoses of complex regional pain syndrome were reported. There were no significant differences in child age or gender across pain conditions. Average child self-reported pain intensity was 4.12 out of 10 (SD = 2.45). There was a statistically significant difference between child pain intensity and pain complaint as determined by a 1-way analysis of variance, F(4, 138) = 3.88, P < .01. A Tukey post hoc test revealed pain intensity was significantly lower for children with headache (3.53 § 2.46) relative to those with musculoskeletal (5.53 ± 1.81) pain. Independent sample t-tests examining gender differences across study variables revealed females reported higher pain frequency, t(138) = 2.79, P < .01; 2.93 ± 1.23; pain intensity, t(144) = 2.09, P < .05, 4.40 ± 2.37; pain interference, t (70.79) = 3.65, P < .01; 58.39 ± 9.30; and pain catastrophizing, t(144) = 2.13, P < .05; 26.34 ± 10.75. The majority of caregivers were mothers (90.4%) and were predominantly white (87.0%). Caregivers self-reported a mean pain intensity of 2.81 out of 10 (SD = 2.53) and pain interference T-score of 49.86 (SD = 8.54).
Table 1.
Participant Sociodemographic and Pain Characteristics
| Characteristic | Mean ± SD or No. (%) |
|---|---|
| Child age, y | 12.97 ± 2.78 |
| Child gender | |
| Female | 100 (68.5) |
| Male | 46 (31.5) |
| Child primary pain complaint | |
| Abdominal pain | 14(9.7) |
| Nerve (neuropathic) pain | 12 (8.3) |
| Headache | 91 (63.2) |
| Pelvic pain | 1 (.7) |
| Musculoskeletal pain | 15 (10.4) |
| Other | 11 (7.6) |
| Parent gender | |
| Female | 132 (90.4) |
| Male | 14(9.6) |
| Parent marital status | |
| Single | 6(4.1) |
| Married | 113(77.9) |
| Common law | 7(4.8) |
| Separated/divorced | 15 (10.3) |
| Widowed | 3(1.4) |
Data Screening and Preliminary Analyses
Before performing the proposed analyses, data were screened for normality. Mild to moderate skew was observed in several variables. Based on these findings, data were modeled using weighted least squares with mean and variance adjustment estimation to account for non-normality. Pearson’s correlations were performed to explore the relationships among continuous variables of interest (Table 2). All associations were in the expected direction with statistical significance. Child age was significantly associated with a greater pain intensity, number of pain locations, pain interference, anxiety, and depressive symptoms.
Table 2.
Descriptive Information and Correlations Across Study Variables
| Measure | M | SD | α | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Parent factors | |||||||||||||||||||
| 1) No. of pain locations | 2.80 | 3.51 | — | — | |||||||||||||||
| 2) Pain intensity | 2.81 | 2.54 | — | .53* | — | ||||||||||||||
| 3) Pain interference | 49.86 | 8.54 | .96 | .64* | .77* | — | |||||||||||||
| 4) Physical function | 52.47 | 6.97 | .89 | −.60* | −.61* | −.75* | — | ||||||||||||
| 5) Protectiveness | 19.24 | 8.44 | .85 | −.01 | −.01 | .02 | −.04 | — | |||||||||||
| 6) Monitoring | 13.11 | 2.53 | .75 | .15 | −.00 | .05 | −.06 | .52* | — | ||||||||||
| 7) Catastrophizing | 21.00 | 9.29 | .89 | .08 | .12 | .26* | −.11 | .25* | .26* | — | |||||||||
| 8) Anxiety | 49.02 | 9.44 | .92 | .28* | .28* | .33* | −.34* | .12 | .02 | .41* | — | ||||||||
| 9) Depressive symptoms | 46.47 | 8.01 | .92 | .39* | .26* | .40* | −.45* | .04 | −.02 | .38* | .70* | ||||||||
| Child factors | |||||||||||||||||||
| 10) Age | 12.97 | 2.78 | — | −.00 | .01 | .06 | −.05 | −.09 | −.07 | .07 | .14 | .18* | — | ||||||
| 11) Pain intensity | 4.12 | 2.45 | — | .09 | .18* | .20* | −.19* | −.20* | −.24* | .17* | .24* | .19* | .21* | — | |||||
| 12) No. of pain locations | 3.17 | 3.63 | — | .40* | .22* | .35* | −.39* | −.02 | −.05 | .09 | .17* | .23* | .18* | .28* | — | ||||
| 13) Pain interference | 56.13 | 10.60 | .86 | .17* | .11 | .21* | −.20* | −.01 | −.08 | .32* | .28* | .27* | .24* | .52* | .40* | — | |||
| 14) Anxiety | 49.19 | 12.01 | .90 | .19* | .06 | .26* | −.31* | −.08 | −.04 | .22* | .26* | .26* | .17* | .26* | .24* | .45* | — | ||
| 15) Depressive symptoms | 48.89 | 10.84 | .90 | .18* | .01 | .24* | −.31* | .02 | −.01 | .22* | .23* | .37* | .30* | .19* | .30* | .35* | .74* | — | |
| 16) Catastrophizing | 24.99 | 11.41 | .92 | .08 | .08 | .15 | −.15 | .05 | .03 | .45* | .19* | .19* | .04 | .32* | .21* | .54* | .40* | .35* | — |
NOTE:
P < .05;
α = Cronbach’s alpha. Categorical variables not included.
Model Specification
Initially, a model was specified in which parent chronic pain status, physical function, behavioral responses to child pain, and psychological factors were explored in relation to child pain. In the baseline model, fit was found to be mediocre (Table 3). Upon closer review of characteristics, several modifications were indicated to improve model fit.
Table 3.
Fit Statistics Presented by Model Modification
| χ2 (df) | Δχ2 (Δdf) | CFI | TLI | RMSEA (90% CI) | WRMR | |
|---|---|---|---|---|---|---|
| Baseline model | 197.50* (120) | — | .87 | .84 | .07 (.05–.08) | .78 |
| Adjusted model | 163.96* (94) | 33.54 (26) | .88 | .84 | .07 (.05–.09) | .75 |
| Final model | 144.32* (93) | 19.64* (1) | .91 | .88 | .06 (.04–.08) | .69 |
NOTE:
P < .001.
CFI = comparative fit index; TLI = Tucker-Lewis index; RMSEA= root mean squared error of approximation; WRMR = weighted root mean square residual.
First, the behavioral responses to child pain factor performed poorly and yielded weak factor loadings (≤.4).3 The justification for removing the behavioral responses to child pain factor was based on both statistical and theoretical reasoning. Previous research indicates a maladaptive association between parent protectiveness and child pain behavior through reinforcement of passive coping strategies.46 However, in a sample of children with chronic headaches, parent protectiveness was not associated with pain frequency, duration, or intensity.21 Furthermore, previous research has documented some concerns regarding the reliability and validity of the parent monitoring construct.6,25,30 In light of these findings and the weak correlation between parent behavioral responses indicator items (ie, protectiveness and monitoring) and other factors in preliminary analyses of the present study (of which 63.2% of children reported chronic headaches), this factor was removed from the model.
Second, modification indices suggested an area of localized strain involving 2 child indicators, pain intensity and frequency. Although these items assess the same construct, both indicators significantly contribute to the model through robust, statistically significant factor loadings. These items were allowed to co-vary in the final model. This last modification yielded an acceptable fit to the data, χ2(93, N = 165) = 144.32, P < .001, comparative fit index = .91, Tucker-Lewis index = .88, and root mean squared error of approximation = .06. All factor loadings were significant and significant correlations were observed among all latent factors. Standardized coefficients for the baseline and adjusted model can be found in Supplementary Table 1. The final model is displayed in Fig 2 and shows significant, moderate associations between parent psychological function, physical function, and chronic pain features with child pain and child psychological function. More specifically, parent chronic pain features exhibited a greater correlation with child pain and function than child psychological factors. As one would expect, parent psychological factors exhibited a greater correlation with child psychological factors than pain and function.
Fig 2.
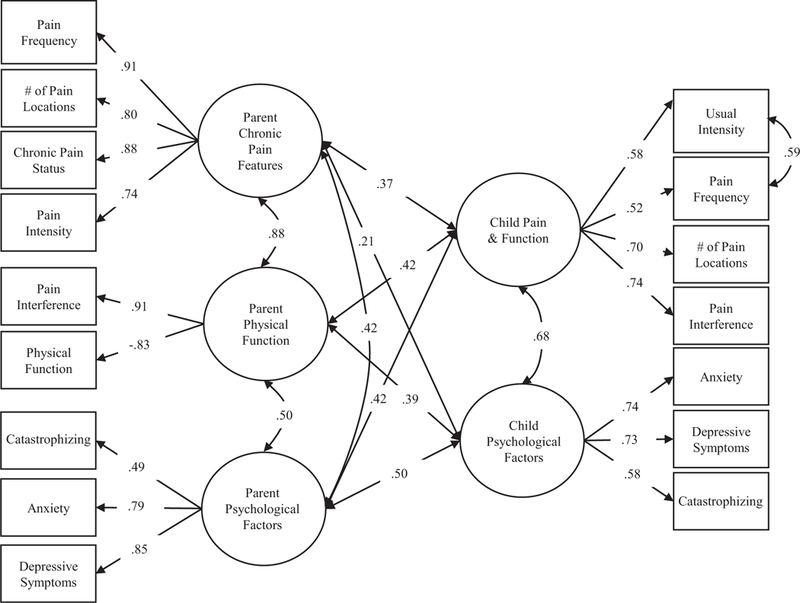
Standardized coefficients for the final model.
Finally, as an exploratory aim, we specified an alternative model in which we examined the possibility of a parent’s own psychological functioning construct versus a parent responses to child pain construct. In this iteration, catastrophizing was moved to the parent response construct. The modification to the parent response construct did not produce a tenable solution and was ultimately dropped owing to high collinearity among the indicators and nonsignificant associations with other factors.
Discussion
It is widely established that parents have a strong influence on the pain experience of youth with chronic pain. Although a number of parental factors have been previously identified as contributing to children’s experience of chronic pain, multivariate models representing the complex interrelations among factors have been underexplored. This study builds on the existing literature by contributing a unified model of parental factors and assessing their direct association with child pain and psychological functioning. Results from the current study found support for a theoretical model in which a number of parental factors were interrelated and contributed to child pain and function and psychological factors. In addition to parent behavioral responses to child pain and parent psychological factors, which have frequently been examined, the initial theoretical multivariate model also included parent chronic pain characteristics and physical functioning as a proxy for parent modeling of pain behaviors. The model specified that these 4 parent domains would be associated with each other, and would directly impact child pain and psychological function outcomes. The initial conceptual model was supported with the exception of the latent variable of parent behavioral responses to pain, which did not yield a good fit.
The finding that parental responses to child pain, specifically protectiveness and monitoring, were unrelated to child pain and pain-related interference contradicts prior work.55 Although parent responses to child pain are often emphasized in family-based interventions and considered a key factor in the development and maintenance of pediatric chronic pain,27 a systematic review of parent behavioral responses to pediatric abdominal pain found little evidence to support these assertions.51 Two studies have evaluated the longitudinal trajectory of parent responses to child pain in the context of randomized, controlled trials of cognitive-behavioral therapy for pediatric chronic pain.26,27 Although both studies found decreases in parents, maladaptive behavioral responses to child pain in response to cognitive-behavioral therapy, these decreases did not correspond with significant decreases in children’s self-reported pain27 or disability.26 Thus, the extent to which parent behavioral responses to child pain is a key factor in the maintenance of child pain and disability remains questionable. It is possible that parent protective responses may have fit better with a model examining children’s social or physical functioning as independent factors, as has been supported in previous work.55 Further, parent and child report measurement tools available for assessing parent responses to child pain may not adequately capture the moment-to-moment or daily parent behaviors that might serve as inadvertent reinforcement of pain behaviors, because the parent behaviors that serve this function may be idiosyncratic or specific to the individual child or family.9 The further development of observational or electronic momentary assessment tools might inform future measure development in this area.
Other parental factors, such as emotional distress and parents’ own physical health and functioning, may be equally if not more important to consider as targets for parent interventions for pediatric chronic pain. Furthermore, present results indicate that the intensity or severity of a parent’s emotional response (eg, anxiety, catastrophizing) may be more impactful on a child’s pain and functioning than the focus of their worry (eg, their own pain vs their child’s pain). Indeed, a recent study found that parental modeling of pain behaviors, but not parent reinforcement, accounted for the relation between parent chronic pain and child pain and functional impairment.48 A major strength of the current study was that the conceptual model incorporated parents, own pain experiences and physical function as direct predictors of child pain and functioning. Parent pain experiences may influence children through both genetic and social learning pathways, the latter depending on the extent to which parents model pain behaviors. In the present analysis, these pathways may have represented social learning pathways, such as modeling pain and pain coping behaviors, and the results indicated that these parental factors made a direct contribution to child pain outcomes. It is also possible that some of the direct pathways from parent to child pain represent genetic risk for chronic pain. The current analysis focused on child pain experiences, including pain characteristics and pain interference, as well as psychological functioning, as key outcomes.
Results from the current study provide additional support for consideration of parent chronic pain status and parent functioning as part of a comprehensive assessment of youth with chronic pain and their families. The inclusion of these types of parent measures in clinical and research samples might elucidate intergenerational mechanisms of influence on child outcomes and help to clarify which parent factors are most important to target in treatment. There is some initial evidence to suggest that addressing parental distress in the context of treatment for child pain can improve child outcomes,35 but it is largely unknown whether effective treatment for other parental factors (eg, pain, physical function) might improve child outcomes or change parent modeling. Among youth with chronic pain, understanding whether these factors influence a parent’s ability to support their child’s recovery may be just as important. For instance, a parent’s own pain and functioning may interfere with a child’s ability to implement treatment recommendations. In such cases, identifying potential barriers impacting treatment efficacy during the initial evaluation could be used to inform treatment targets. Alternatively, at the very least, this information may help clinicians to make appropriate referrals to adult providers that can carry out individual psychological treatment with the parent early on. Further, the development of family-based interventions to address chronic pain in both youth and their parent may also promote treatment effectiveness and bolster outcomes.
Although the current study had several strengths, including consideration of multiple parent factors in a single model, and use of data from multiple informants, there were limitations that should be noted. First, given the cross-sectional nature of the data, no conclusions about directionality or causality could be drawn. There is evidence that parent psychological distress is higher among the parents of youth who experience more severe pain and disability compared with those who are less disabled by pain,8 and it is possible that the presence of more severe pain in children drives parent distress over time. Furthermore, the timing of the collection of these measures should be considered. It is conceivable that parent anxiety and feelings of uncertainty may be uniquely increased before the child’s initial pain clinic evaluation. Future research may wish to reassess the relation among these variables to ascertain whether a dynamic association exists.
Another limitation of the current study is that the sample was primarily composed of youth with chronic headaches and participating parents were primarily mothers. Although parent functioning is likely to impact child pain regardless of the child’s pain location, there may be some associations between parent factors and child pain that are more or less strong depending on the child’s pain condition. The majority of previous research using the Adult Responses to Children’s Symptoms has been performed in children with abdominal pain; our sample was predominantly composed of youth with headaches.33 Therefore, future work should test similar models in other pain conditions. The majority of the sample was composed of mothers. Although mothers are often more involved in children’s medical care than fathers, including pain care,35 children of 2-parent households (regardless of parent gender or marital status) are still exposed to 2 parent models who demonstrate pain behaviors and pain coping. Future models might also consider comparing patterns of associations across mothers and fathers, and across parents who are and are not biological parents.
In conclusion, this study provides preliminary support for a unified model of parental factors in pediatric chronic pain, and to include parent chronic pain status and physical and psychological functioning as key domains for assessment and intervention. Future work is needed to examine the complexity of parent influences on child pain over time using longitudinal designs. Further, replications of the present findings using novel or alternative methods for capturing relevant factors (eg, observational methods for parent behavioral responses) will also be important. Additionally, future invariance testing of parent health (ie, with and without chronic pain) in this unified model may provide nuanced insight into parental modeling and reinforcement behaviors as they relate to these relationships. Finally, this work will inherently require that attention be paid to children’s developmental stage, as well as to individual child characteristics (eg, temperament, anxiety sensitivity) that may increase vulnerability to these parental factors.
Supplementary Material
Acknowledgments
The authors thank the parents and children who participated in this study.
Supported by funding from the Vi Riddell Pediatric Pain Initiative and the Alberta Children’s Hospital Research Institute awarded to Dr. Noel. Dr. Stone,s effort was supported in part by Oregon Clinical and Translational Research Institute (OCTRI), grant number TL1TR002371 from the National Center for Advancing Translational Sciences (NCATS) of the National Institutes of Health (NIH) and the NIH-funded Vanderbilt Department of Anesthesiology Clinician Scientist Training in Perioperative Science Fellowship (T32GM108554). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Supplementary data
Supplementary data related to this article can be found at https://doi:10.1016/j.jpain.2019.01.004.
Supplementary data accompanying this article are available online at www.jpain.org and www.sciencedirect.com.
The authors have no conflicts of interest to declare.
References
- 1.Aasland A, Flato B, Vandvik IH: Psychosocial factors in children with idiopathic musculoskeletal pain: A prospective, longitudinal study. Acta Paediatr 86:740–746, 1997 [DOI] [PubMed] [Google Scholar]
- 2.Baeyer CLv, Lin V, Seidman LC, Tsao JC, Zeltzer: Pain charts (body maps or manikins) in assessment of the location of pediatric pain. Pain Manage 1:61–68, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brown TA: Confirmatory Factor Analysis for Applied Research. New York, NY: Guilford Publications, 2014 [Google Scholar]
- 4.Campo JV, Bridge J, Lucas A, Savorelli S, Walker L, Di Lorenzo C, Iyengar S, Brent DA: Physical and emotional health of mothers of youth with functional abdominal pain. Arch Pediatr Adolesc Med 161:131–137, 2007 [DOI] [PubMed] [Google Scholar]
- 5.Castarlenas E, Jensen MP, von Baeyer CL, Miró J: Psychometric properties of the numerical rating scale to assess self-reported pain intensity in children and adolescents: A systematic review. Clin J Pain 33:376–383, 2017 [DOI] [PubMed] [Google Scholar]
- 6.Claar RL, Guite JW, Kaczynski KJ, Logan DE: Factor structure of the Adult Responses to Children’s Symptoms: Validation in children and adolescents with diverse chronic pain conditions. Clin J Pain 26:410–417, 2010 [DOI] [PubMed] [Google Scholar]
- 7.Coenders A, Chapman C, Hannaford P, Jaaniste T, Qiu W, Anderson D, Glogauer M, Goodison-Farnsworth E, McCormick M, Champion D: In search of risk factors for chronic pain in adolescents: A case-control study of childhood and parental associations. J Pain Res 7:175–183, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cohen LL, Vowles KE, Eccleston C: Parenting an adolescent with chronic pain: An investigation of how a taxonomy of adolescent functioning relates to parent distress. J Pediatr Psychol 35:748–757, 2010 [DOI] [PubMed] [Google Scholar]
- 9.Connelly M, Anthony KK, Sarniak R, Bromberg MH, Gil KM, Schanberg LE: Parent pain responses as predictors of daily activities and mood in children with juvenile idiopathic arthritis: The utility of electronic diaries. J Pain Symptom Manag 39:579–590, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Connelly M, Bromberg MH, Anthony KK, Gil KM, Schanberg LE: Use of smartphones to prospectively evaluate predictors and outcomes of caregiver responses to pain in youth with chronic disease. Pain 158:629–636, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cook KF, Kallen MA, Amtmann D: Having a fit: Impact of number of items and distribution of data on traditional criteria for assessing IRT’s unidimensionality assumption. Qual Life Res 18:447–460, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Crombez G, Bijttebier P, Eccleston C, Mascagni T, Mertens G, Goubert L, Verstraeten K: The child version of the Pain Catastrophizing Scale (PCS-C): A preliminary validation. Pain 104:639–646, 2003 [DOI] [PubMed] [Google Scholar]
- 13.Cunningham NR, Lynch-Jordan A, Barnett K, Peugh J, Sil S, Goldschneider K, Kashikar-Zuck S: Child pain catastrophizing mediates the relation between parent responses to pain and disability in youth with functional abdominal pain. J Pediatr Gastroenterol Nutr 59:732–738, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Deyo RA, Ramsey K, Buckley DI, Michaels L, Kobus A, Eckstrom E, Forro V, Morris C: Performance of a Patient Reported Outcomes Measurement Information System (PROMIS) short form in older adults with chronic musculo-skeletal pain. Pain Med 17:314–324, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gatchel RJ: Comorbidity of chronic pain and mental health disorders: The biopsychosocial perspective. Am Psychol 59:795, 2004 [DOI] [PubMed] [Google Scholar]
- 16.Goubert L, Eccleston C, Vervoort T, Jordan A, Crombez G: Parental catastrophizing about their child’s pain. The parent version of the Pain Catastrophizing Scale (PCS-P): A preliminary validation. Pain 123:254–263, 2006 [DOI] [PubMed] [Google Scholar]
- 17.Guo B, Perron BE, Gillespie DF: A systematic review of structural equation modelling in social work research. Br J Social Work 39:1556–1574, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG: Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Informat 42:377–381, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lt Hu, Bentler PM: Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Model 6:1–55, 1999 [Google Scholar]
- 20.International Association for the Study of Pain (IASP) Task Force on Taxonomy. Classification of Chronic Pain In: Merskey H,, Bogduk N, eds. Classification of Chronic Pain, 2nd ed, Seattle, WA, IASP Press, 1994 [Google Scholar]
- 21.Kaczynski KJ, Claar RL, LeBel AA: Relations between pain characteristics, child and parent variables, and school functioning in adolescents with chronic headache: A comparison of tension-type headache and migraine. J Pediatr Psychol 38:351–364, 2013 [DOI] [PubMed] [Google Scholar]
- 22.Karabulut GS, Beser OF, Erginoz E, Kutlu T, Cokugras FC, Erkan T: The incidence of irritable bowel syndrome in children using the Rome III criteria and the effect of trimebutine treatment. J Neurogastroenterol Motil 19:90–93, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kashikar-Zuck S, Carle A, Barnett K, Goldschneider KR, Sherry DD, Mara CA, Cunningham N, Farrell J, Tress J, DeWitt EM: Longitudinal evaluation of Patient Reported Outcomes Measurement Information Systems (PROMIS) measures in pediatric chronic pain. Pain 157:339, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kroenke K, Yu Z, Wu J, Kean J, Monahan PO: Operating characteristics of PROMIS four-item depression and anxiety scales in primary care patients with chronic pain. Pain Med 15:1892–1901, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Langer SL, Romano JM, Levy RL, Walker LS, Whitehead WE: Catastrophizing and parental response to child symptom complaints. Child Health Care 38:169–184, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Law EF, Fisher E, Howard WJ, Levy R, Ritterband L, Palermo TM: Longitudinal change in parent and child functioning after internet-delivered cognitive-behavioral therapy for chronic pain. Pain 158:1992–2000, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Levy RL, Langer SL, Walker LS, Romano JM, Christie DL, Youssef N, DuPen MM, Feld AD, Ballard SA, Welsh EM, Jeffery RW, Young M, Coffey MJ, Whitehead WE: Cognitive-behavioral therapy for children with functional abdominal pain and their parents decreases pain and other symptoms. Am J Gastroenterol 105:946–956, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Levy RL, Whitehead WE, Walker LS, Von Korff M, Feld AD, Garner M, Christie D: Increased somatic complaints and health-care utilization in children: Effects of parent IBS status and parent response to gastrointestinal symptoms. Am J Gastroenterol 99:2442–2451, 2004 [DOI] [PubMed] [Google Scholar]
- 29.Little TD: Longitudinal Structural Equation Modeling. New York, NY, Guilford Press, 2013 [Google Scholar]
- 30.Logan DE, Simons LE, Carpino EA: Too sick for school? Parent influences on school functioning among children with chronic pain. Pain 153:437–443, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McWilliams LA, Cox BJ, Enns MW: Mood and anxiety disorders associated with chronic pain: An examination in a nationally representative sample. Pain 106:127–133, 2003 [DOI] [PubMed] [Google Scholar]
- 32.Muthén LK, Muthen BO: Mplus: Statistical analysis with latent variables: User’s guide. Los Angeles, CA, Muthen & Muthen, 2010 [Google Scholar]
- 33.Noel M, Palermo TM, Essner B, Zhou C, Levy RL, Langer SL, Sherman AL, Walker LS: A developmental analysis of the factorial validity of the parent-report version of the Adult Responses to Children’s Symptoms in children versus adolescents with chronic pain or pain-related chronic illness. J Pain 16:31–41, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Page MG, Campbell F, Isaac L, Stinson J, Katz J: Parental risk factors for the development of pediatric acute and chronic postsurgical pain: A longitudinal study. J Pain Res 6:727–741, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Palermo TM, Law EF, Bromberg M, Fales J, Eccleston C, Wilson AC: Problem solving skills training for parents of children with chronic pain: A pilot randomized controlled trial. Pain 157:1213, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Palermo TM, Valenzuela D, Stork PP: A randomized trial of electronic versus paper pain diaries in children: Impact on compliance, accuracy, and acceptability. Pain 107:213–219, 2004 [DOI] [PubMed] [Google Scholar]
- 37.Palermo TM, Valrie CR, Karlson CW: Family and parent influences on pediatric chronic pain: A developmental perspective. Am Psychol 69:142–152, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pincus T, Burton AK, Vogel S, Field AP: A systematic review of psychological factors as predictors of chronicity/ disability in prospective cohorts of low back pain. Spine 27: E109–E120, 2002 [DOI] [PubMed] [Google Scholar]
- 39.Reeve BB, Hays RD, Bjorner JB, Cook KF, Crane PK, Ter-esi JA, Thissen D, Revicki DA, Weiss DJ, Hambleton RK, Liu H, Gershon R, Reise SP, Lai J-s, Cella D: PROMIS Cooperative Group. Psychometric evaluation and calibration of health-related quality of life item banks: Plans for the Patient-Reported Outcomes Measurement Information System (PROMIS). Med Care 45:S22–S31, 2007 [DOI] [PubMed] [Google Scholar]
- 40.Robinson JO, Alverez JH, Dodge JA: Life events and family history in children with recurrent abdominal pain. J Psychosom Res 34:171–181, 1990 [DOI] [PubMed] [Google Scholar]
- 41.Ruskin D, Lalloo C, Amaria K, Stinson JN, Kewley E, Campbell F, Brown SC, Jeavons M, McGrath PA: Assessing pain intensity in children with chronic pain: Convergent and discriminant validity of the 0 to 10 numerical rating scale in clinical practice. Pain Res Manag 19:141–148, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Savedra MC, Tesler MD, Holzemer WL, Wilkie DJ, Ward JA: Pain location: Validity and reliability of body outline markings by hospitalized children and adolescents. Res Nurs Health 12:307–314, 1989 [DOI] [PubMed] [Google Scholar]
- 43.Schmitt TA: Current methodological considerations in exploratory and confirmatory factor analysis. J Psychoeduc Assess 29:304–321, 2011 [Google Scholar]
- 44.Shelby GD, Shirkey KC, Sherman AL, Beck JE, Haman K, Shears AR, Horst SN, Smith CA, Garber J, Walker LS: Functional abdominal pain in childhood and long-term vulnerability to anxiety disorders. Pediatrics 132:475–482, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sieberg CB, Williams S, Simons LE: Do parent protective responses mediate the relation between parent distress and child functional disability among children with chronic pain? J Pediatr Psychol 36:1043–1051, 2011 [DOI] [PubMed] [Google Scholar]
- 46.Simons LE, Claar RL, Logan DL: Chronic pain in adolescence: Parental responses, adolescent coping, and their impact on adolescent’s pain behaviors. J Pediatr Psychol 33:894–904, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Stinson JN, Kavanagh T, Yamada J, Gill N, Stevens B: Systematic review of the psychometric properties, interpretability and feasibility of self-report pain intensity measures for use in clinical trials in children and adolescents. Pain 125:143–157, 2006 [DOI] [PubMed] [Google Scholar]
- 48.Stone AL, Bruehl S, Smith CA, Garber J, Walker LS: Social learning pathways in the relation between parental chronic pain and daily pain severity and functional impairment in adolescents with functional abdominal pain. Pain 159:298–305, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Stone AL, Walker LS: Adolescents’ observations of parent pain behaviors: Preliminary measure validation and test of social learning theory in pediatric chronic pain. J Pediatr Psychol 42:65–74, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Tunks ER, Crook J, Weir R: Epidemiology of chronic pain with psychological comorbidity: Prevalence, risk, course, and prognosis. Canadian J Psychiatry 53:224–234, 2008 [DOI] [PubMed] [Google Scholar]
- 51.Van Der Veek SM, Derkx H, De Haan E, Benninga MA, Plak RD, Boer F: Do parents maintain or exacerbate pediatric functional abdominal pain? A systematic review and meta-analysis. J Health Psychol 17:258–272, 2012 [DOI] [PubMed] [Google Scholar]
- 52.Van Slyke DA, Walker LS: Mothers’ responses to children’s pain. Clin J Pain 22:387–391, 2006 [DOI] [PubMed] [Google Scholar]
- 53.Vinall J, Pavlova M, Asmundson GJ, Rasic N, Noel M: Mental health comorbidities in pediatric chronic pain: A narrative review of epidemiology, models, neurobiological mechanisms and treatment. Children 3:40, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.von Baeyer CL, Spagrud LJ, McCormick JC, Choo E, Neville K, Connelly MA: Three new datasets supporting use of the Numerical Rating Scale (NRS-11) for children’s self-reports of pain intensity. Pain 143:223–227, 2009 [DOI] [PubMed] [Google Scholar]
- 55.Vowles KE, Cohen LL, McCracken LM, Eccleston C: Disentangling the complex relations among caregiver and adolescent responses to adolescent chronic pain. Pain 151:680–686, 2010 [DOI] [PubMed] [Google Scholar]
- 56.Walker LS, Garber J, Greene JW: Somatization symptoms in pediatric abdominal pain patients: Relation to chronicity of abdominal pain and parent somatization. J Abnorm Child Psychol 19:379–394, 1991 [DOI] [PubMed] [Google Scholar]
- 57.Walker LS, Levy RL, Whitehead WE: Validation of a measure of protective parent responses to children’s pain. Clin J Pain 22:712–716, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wilson AC, Fales JL: Parenting in the context of chronic pain: A controlled study of parents with chronic pain. Clin J Pain 31:689–698, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


