Abstract
Background:
We explore relationships between place characteristics and HIV viral suppression among HIV-positive men who have sex with men (MSM) in New York City (NYC).
Methods:
We conducted multilevel analyses to examine associations of United Hospital Fund (UHF)-level characteristics to individual-level suppression and durable suppression among MSM. Individual-level independent and dependent variables came from MSM in NYC’s HIV surveillance registry who had been diagnosed in 2009–2013 (N=7,159). UHF-level covariates captured demographic composition, economic disadvantage, healthcare access, social disorder, and police stop and frisk rates.
Results:
56.89% of MSM achieved suppression; 35.49% achieved durable suppression. MSM in UHFs where 5–29% of residents were Black had a greater likelihood of suppression (reference:≥30% Black; adjusted relative risk [ARR]=1.07, p=0.04). MSM in UHFs with <30 MSM-headed households/10,000 households had a lower likelihood of achieving durable suppression (reference:≥ 60 MSM-headed households/10,000; ARR=0.82; p=0.05).
Conclusions:
Place characteristics may influence viral suppression. Longitudinal research should confirm these associations.
Keywords: HIV Viral Suppression, Place-based Predictors, Men who have Sex with Men, New York City
INTRODUCTION
The US National HIV/AIDS Strategy 2020 prioritizes achieving viral suppression for all people living with HIV(1). Viral suppression occurs when the number of HIV virions in the blood falls below a specified threshold (2). Achieving viral suppression improves the health of people living with HIV and reduces HIV transmission (3). Achieving suppression is vital among men who have sex with men (MSM), who represented 58% of people living with diagnosed HIV infection and 67% of new transmissions in the US in 2013, though only 42% were virally suppressed in 2010 (4–6). Non-Hispanic Black (“Black”) and Latino MSM have especially high burdens of HIV: in 2010, 30% of MSM living with HIV were Black and 20% were Hispanic (6). Although Black and Latino MSM do not report greater risk behavior than White MSM (7), CDC models predict that 50% of Black MSM and 25% of Latino MSM will seroconvert in their lifetimes (8). HIV-positive Black and Latino MSM are also less likely to achieve suppression than their non-Hispanic White (“White”) counterparts: the percentages of HIV-diagnosed MSM achieving suppression in 2010 were 37%, 42%, and 44% for Black, Latino, and White MSM, respectively (6).
With rare exception, studies exploring determinants of viral suppression have focused on individual-level exposures, such as medication adherence (9), substance use (10), or age (11). Recently, however, an emerging line of research has begun to investigate whether features of the environments where HIV-positive people live might shape suppression (12–15). The emergence of this line of inquiry is consistent with the broader shift in public health toward considering multilevel etiologies that conceptualize health and disease as shaped by characteristics of networks, neighborhoods, and other spheres of the social world, as well as by characteristics of individuals. Such multilevel perspective embraces a key tenet of Urie Bronfenbrenner’s Social ecological model, that humans are affected both by internal traits and social contexts (16). Five layers of social context that affect individuals include: immediate interactions between an individual and their social environment (the microsystem), interactions between elements within an individual’s immediate social environment (the mesosystem), social institutions which surround and can have power over an individual’s immediate social environment (the exosystem), and overall cultural values and norms which engender social institutions and interactions (the macrosystem) (16). Multilevel research on place-based health exposures investigates how elements in the exosystem influence health, after accounting for salient individual-level characteristics.
Exemplifying new multilevel research, Beattie et al. (15) found that HIV-positive patients at a large urban health center in New York City (NYC) were less likely to be suppressed if they lived in a high-poverty neighborhood, though an analysis of HIV surveillance data from NYC found no relationship between neighborhood socioeconomic conditions and time to suppression (14). To our knowledge, no research has explored whether characteristics of the places where people live are associated with viral suppression among MSM.
Extending research on place characteristics and viral suppression among HIV-diagnosed MSM could help develop community-level interventions or policies that target place characteristics or mediators of place/suppression relationships for HIV-diagnosed MSM. The present multilevel study explores relationships between select place characteristics and viral suppression among HIV-diagnosed MSM in NYC. Scholarship on place-based-exposures as social determinants of health is a (re)emerging inquiry in public health research (17). As such, many relationships between place-based exposures and health outcomes are untested. Place-based exposures for this analysis were selected based on past research about the influence of place characteristics on AIDS-related survival and on access to highly active anti-retroviral therapy (HAART) or other forms of healthcare. This past research suggested that we include the following domains of place-based exposures: sociodemographic composition (18), rates of economic disadvantage (19), healthcare access (20), and social disorder (21). Sociodemographic composition and rates of economic disadvantage could plausibly affect survival by affecting access to nutritious food, safe and healthy housing, social support, and freedom from violence (18). Healthcare access could affect survival by shaping medication use and adherence (22). Social disorder could affect survival by affecting psychosocial stressors and substance use (23, 24). We also explored police use of Terry stops (“stop and frisk”) (25) as an exposure, conceptualizing it as a form of community violence that might adversely affect healthcare seeking and immune response (26, 27). Critical race theory and social geography scholarship both suggest that people’s experience of, access to, and meanings of neighborhoods and neighborhood characteristics is racialized (28–30). Given this, and given large racial/ethnic disparities in suppression (6, 8), we explore whether individual race/ethnicity moderates relationships between place-based exposures and suppression.
METHODS
Overview and Units of Analysis
This cross-sectional multilevel study had two units of analysis: individuals diagnosed with HIV and NYC’s United Hospital Fund (UHF) districts. UHFs are aggregations of adjacent ZIP codes that are relatively homogenous (31). The NYC Department of Health and Mental Hygiene (NYC DOHMH) uses UHFs for planning purposes. In 2010, there were 42 UHF districts in NYC, and the median UHF adult population size was 128,117 (25th percentile= 83,451; 75th percentile= 162,871) (32).
Data on individuals were drawn from the NYC DOHMH’s HIV surveillance registry. NYC DOHMH is authorized by the New York State Department of Health to conduct population-based NYC HIV/AIDS surveillance. Since 2000, all NYC diagnostic and clinical providers have been required to report new diagnoses of HIV to NYC DOHMH. Laboratories performing HIV-related tests for NYC providers must report positive HIV diagnostic tests, HIV viral loads, and other clinical indicators (e.g., CD4 counts) to NYC DOHMH. New York State, including NYC, began comprehensive electronic HIV laboratory reporting in 2005. The surveillance registry includes demographic characteristics, residential ZIP code, place of birth, and transmission risk information for each individual; these data are primarily extracted from medical chart reviews. In 2016, the surveillance registry contained a cumulative total of >230,000 cases and >8 million laboratory reports.
To be included in the analytic database, individuals (≥13 years old) had to be newly diagnosed with HIV between January 1, 2009 and December 31, 2013 and: assigned male at birth; identify as Black, White, or Hispanic/Latino; report a history of sex with men; and live in a NYC UHF district at HIV diagnosis. People were linked to UHF districts via their ZIP code of residence at diagnosis. Of 8,259 Black, White, or Hispanic/Latino males ≥13 years old who reported a history of sex with men and were diagnosed between 2009–2013, 13% (N= 1,100) did not have a NYC ZIP code at diagnosis and were excluded.
Measures
Individual-Level Outcomes
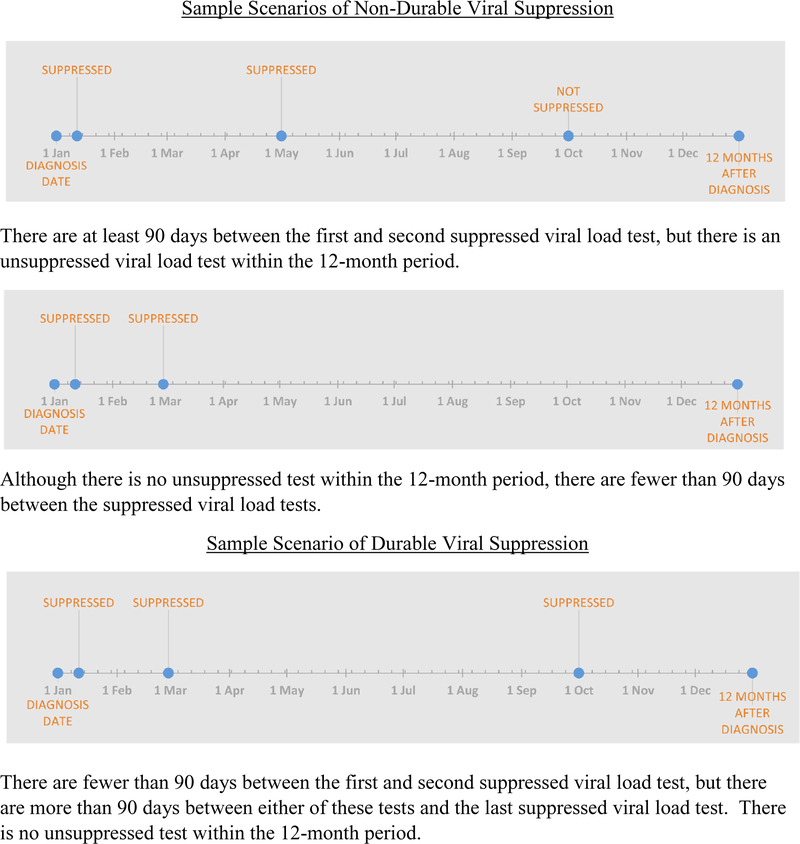
This analysis had two HIV-related outcomes, both assessed at the individual level using NYC DOHMH HIV surveillance data: viral suppression and durable viral suppression within 12 months of initial HIV diagnosis. In accordance with the standardized cut-off used by the Centers for Disease Control (33), NYC DOHMH pre-classified individuals in the surveillance registry as “virally suppressed” if they had ≤200 copies of HIV per ml of blood at any point within 12 months after their diagnosis. Individuals were classified as “durably virally suppressed” if, within 12 months after their diagnosis, they (A) had at least two suppressed viral load tests that were at least 90 days apart with no intervening unsuppressed viral load tests, and (B) had no unsuppressed viral load tests after they had achieved durable viral suppression (Figure 1).
Figure 1.
Two sample scenarios of non-durable viral suppression. (1) There are at least 90 days between the first and second suppressed viral load test, but there is a subsequent unsuppressed viral load test within the 12-month period. (2) Although there is no unsuppressed test within the 12-month period, there are fewer than 90 days between the suppressed viral load tests. Sample scenario of durable viral suppression. There are fewer than 90 days between the first and second suppressed viral load test, but there are more than 90 days between either of these tests and the last suppressed viral load test. There is no unsuppressed test within the 12-month period.
UHF-Level Predictors
We analyzed administrative data to create measures of five domains of UHF-level predictors: demographic composition, economic disadvantage, healthcare access, social disorder, and police stop and frisk.
Demographic Composition
The number of households headed by male couples per 10,000 households (“MSM-headed households”) was calculated by dividing the number of male-couple headed households by the total number of households within a UHF, and multiplying by 10,000; data were derived from the 2010 Census (32). This variable was skewed and was divided into three categories representing a multimodal distribution: low (<30 of 10,000 households MSM-headed), medium (30 to <60), and higher (≥60). The percent of residents who self-identified as non-Hispanic Black/African-American was calculated using 2007–2011 American Community Survey (ACS) data (34). This variable was skewed, and three categories representing a multimodal distribution were created: low (<5% of residents were Black), medium (5 to 29%), and high (≥30%). The percent of residents who were 21 to 54 years old was calculated using 2007–2011 ACS data (34).
Economic Disadvantage
We used principal components analysis (PCA) to create a measure of UHF-level economic disadvantage. Constituent variables were UHF-level median income; the percent of people aged ≥16 years in the workforce who were unemployed; the percent of individuals at or below federal poverty level; the percent of households that had received public assistance in the last 12 months; and the percent of adults ≥25 years old who did not have a high school degree/GED. Each of these variables was constructed using 2007–2011 ACS data (34). The first extracted component accounted for 88% of the variance in the variable set and was retained to represent economic disadvantage (Table 4).
Table 4.
Components generated by principal components analysis of economic disadvantage and healthcare access variables
| Component | Constituent variables | Correlations of constituent variables with component |
|---|---|---|
| Economic disadvantagea | ||
| Eigenvalue: 4.39 | Median income | −0.47 |
| Variance explained: 88% | Percent unemployed | 0.43 |
| Percent in poverty | 0.45 | |
| Percent on public assistance | 0.46 | |
| Percent without a high school education | 0.43 | |
| Poor access to healthcareb | ||
| Eigenvalue: 0.005 | Percent uninsured | 0.93 |
| Variance explained: 87% | Percent went without needed care | 0.37 |
Correlation matrix used
Covariance matrix used as there are only two constituent variables, both measured on the same scale. Note the correlation matrix eigenvector was 1.60 and it explained 80% of the variance
Healthcare Access
We used PCA to create a measure of poor access to healthcare, using pooled 2009 and 2010 NYC DOHMH Community Health Survey data, weighted to adjust for selection in both years. Constituent variables were the percent of UHF residents without health insurance and the percent of UHF residents who reported an unmet need for care in the last 12 months (35). The first extracted component accounted for 87% of the variance in the variable set and was retained to represent poor access to healthcare (Table 4).
Social Disorder
We considered off-premises alcohol outlet density (from the 2009 U.S Census Bureau’s ZIP Code Business Patterns database) (36), homicide rate (from NYC DOHMH 2009 Bureau of Vital Records) (37), and residential vacancies and business vacancies (from the 2009 United States Postal Service/Department of Housing and Urban Development database) (38) as variables capturing social disorder. After examining correlations among these variables we entered homicide rate and residential vacancy into a PCA. On the basis of PCA we retained only residential vacancy to measure social disorder because it accounted for most of the component loading (eigenvector of 0.9998). Residential vacancy captured the number of residential homes or apartments per square mile that had once been occupied but were now vacant.
Police Stop and Frisk
We used 2009 NYC Police Department Stop, Question, and Frisk (SQF) data to measure the rate of stops without an arrest per 100,000 adult residents (39). This rate was skewed and three categories reflecting a multimodal distribution were created: low (<6,000 stops without arrest per 100,000 residents), medium (6,000-<22,000), and high (≥22,000).
Individual-Level Covariates
Data on individual-level covariates came from NYC DOHMH HIV surveillance. Race/ethnicity, lifetime history of homelessness at diagnosis, year of HIV diagnosis, nativity (born within vs. outside U.S.), and age at HIV diagnosis were abstracted from patient medical records.
Analysis
Because individuals from the surveillance registry were nested in UHFs, multilevel logistic models were used to analyze the associations of UHF-level predictors to individual-level suppression and durable suppression. Suppression and durable suppression were both binary outcomes: individuals were classified as suppressed or durably suppressed if they matched the study’s definition of suppression or durable suppression (see ‘Individual-Level Outcomes’ above). Level 2 consisted of the 42 UHF districts and Level 1 consisted of individuals in the surveillance registry living in those districts. Because suppression and durable suppression were defined as individual-level attributes observed in the year following each person’s diagnosis, level 1 data were all time invariant.
Variables were transformed to be continuous if possible. All normally distributed continuous variables were mean-centered for analysis. Parameters were estimated in SAS 9.3 software’s (40) PROC GLIMMIX using maximum likelihood with Laplace approximation, random intercepts, a binomial distribution, a log link, and an unstructured error covariance matrix.
Model building preceded in stages. In stage one we built bivariate multilevel models to examine relationships of each predictor to viral suppression. In stage two, we extended the model to examine whether individual race/ethnicity (comparing Latino and White to Black MSM) might moderate relationships of UHF-level predictors to viral suppression. In stage three, we built a multivariable viral suppression model consisting of UHF-level variables that were significant at p≤0.15, either as main effects or in interactions with individual level race/ethnicity; models also included the following theoretically relevant individual-level variables: individual race/ethnicity, nativity, history of homelessness, age at HIV diagnosis, and year of HIV diagnosis. In interactions of UHF-level covariates with individual race/ethnicity, we interpret the main effect for the UHF-level covariate as the association for Black MSM, the reference group for the race/ethnicity variable. We repeated this three stage process for the durable viral suppression outcome. Because multiple interactions existed between UHF-level variables and race/ethnicityfor durable viral suppression, we ran separate models for each UHF-race/ethnicity interaction to address power concerns (i.e., Table 3, Models A and B).
Table 3.
Bivariate and multivariable results of a multilevel regression of HIV durable viral suppression on individual- and United Hospital Fund- (UHF-) level covariates in a sample of HIV-positive men who have sex with men (MSM; N = 7159) in New York City diagnosed between 2009 and 2013
| Variables | Bivariate models | Multivariable models | ||||
|---|---|---|---|---|---|---|
| Relative risk | p value | Model A relative riskc | p value | Model B relative riskd | p value | |
| UHF level variables | ||||||
| % Residents who were non-Hispanic Black (ref = high) | ||||||
| Low (<5.00%) | 1.17 | 0.01 | 0.95 | 0.47 | 0.95 | 0.48 |
| Medium (5.00 to <30.00%) | 1.16 | 0.002 | 1.04 | 0.44 | 1.03 | 0.53 |
| Male couple headed households per 10,000 households (ref = high) | ||||||
| Male couple households per 10,000a | ||||||
| Low (< 30) | 0.80 | 0.01 | 0.82 | 0.05 | 0.93 | 0.34 |
| Medium (30 to <60) | 0.90 | 0.14 | 0.89 | 0.10 | 0.96 | 0.46 |
| Male couple households per 10,000 × Latino | ||||||
| Low (<30) | 1.12 | 0.35 | 1.16 | 0.19 | ||
| Medium (30 to <60) | 1.03 | 0.74 | 1.03 | 0.68 | ||
| Male couple households per 10,000 × White | ||||||
| Low (<30) | 1.09 | 0.58 | 1.13 | 0.49 | ||
| Medium (30 to <60) | j 22 | 0.03 | 1.26 | 0.01 | ||
| % Residents who were 21–54 years old | ||||||
| % Residents 21–54 yearsa | 1.01 | 0.07 | 0.997 | 0.59 | 1.01 | 0.46 |
| % Residents 21–54 years × Latino | 0.995 | 0.53 | 0.99 | 0.37 | ||
| % Residents 21–54 years × White | 0.99 | 0.05 | 0.99 | 0.08 | ||
| Economic disadvantageb | 0.97 | 0.001 | 0.98 | 0.18 | 0.98 | 0.24 |
| Residential vacancy | 0.999 | 0.09 | 1.00 | 0.54 | 0.9995 | 0.52 |
| Poor access to healthcare | 0.71 | 0.256 | ||||
| Stops without arrest per 100,000 residents (ref = high) | ||||||
| Low < 6000 | 1.18 | 0.01 | 1.02 | 0.80 | 1.02 | 0.75 |
| Medium 6000 to <22,OOO | 1.11 | 0.12 | 1.02 | 0.80 | 1.02 | 0.71 |
| Individual-level variables | ||||||
| Race/ethnicity (ref = Black) | ||||||
| Latino | 1.22 | <0.0001 | 1.05 | 0.41 | 1.12 | 0.02 |
| White | 1.35 | <0.0001 | 1.08 | 0.19 | 1.25 | <0.0001 |
| Foreign born | 1.19 | <0.0001 | 1.13 | 0.002 | 1.12 | 0.002 |
| History of homelessness | 0.47 | 0.0002 | 0.49 | 0.0003 | 0.5 | 0.0004 |
| Age at diagnosis (ref = 20–29) | ||||||
| 13–19 | 0.75 | 0.002 | 0.82 | 0.03 | 0.82 | 0.03 |
| 30–39 | 1.19 | <0.0001 | 1.15 | 0.0004 | 1.15 | 0.0005 |
| 40–49 | 1.45 | <0.0001 | 1.39 | <0.0001 | 1.39 | <0.0001 |
| 50–59 | 1.51 | <0.0001 | 1.39 | <0.0001 | 1.38 | <0.0001 |
| 60+ | 1.23 | 0.08 | 1.13 | 0.31 | 1.14 | 0.28 |
| Year of diagnosis (ref = 2009) | ||||||
| 2010 | 1.26 | 0.0003 | 1.26 | 0.0004 | 1.27 | 0.0003 |
| 2011 | 1.60 | <0.0001 | 1.62 | <0.0001 | 1.62 | <0.0001 |
| 2012 | 1.90 | <0.0001 | 1.88 | <0.0001 | 1.88 | <0.0001 |
| 2013 | 2.23 | <0.0001 | 2.23 | <0.0001 | 2.23 | <0.0001 |
This is the main effect. In our interaction model it is the effect for Black alone
Higher values mean more disadvantage
Model A focused on the percent of households headed by male couples as the exposure. This was interacted with individual-level race/ethnicity with non-Hispanic Black race/ethnicity as the reference
Model B focused on the percent of residents who were between 21 and 54 years of age. This was interacted with individual-level race/ethnicity with non-Hispanic Black race/ethnicity as the reference
As an analysis of surveillance data, this can be considered an analysis of a population (rather than a sample) that has no sampling error. In such cases, researchers studying similar populations have used p-values as heuristic devices to avoid over-interpreting model parameters (41–43). We follow this tradition here. We also follow the suggestion of epidemiologists to report relative risks, rather than odds ratios, as a more accurate and intuitive estimate of likelihood (44, 45).
RESULTS
There were 7,159 Black, Latino, or White MSM in the HIV surveillance registry who lived in one of the 42 UHF districts and were diagnosed with HIV between 2009–2013 (Table 1). Fifty-seven percent achieved HIV viral suppression within 12 months of diagnosis, but only 35.49% were durably suppressed during that period. Thirty-seven percent of the MSM were Latino, 36.32% were Black, and 26.36% were White. Few people reported a history of homelessness (2.23%), and the modal age at diagnosis was 20–29 (44.46%).
Table 1.
Descriptive statistics for characteristics of 7159 Black, White, and Latino HIV-positive men who have sex with men (MSM) in New York City, and of the United Hospital Fund districts (UHFs; N = 42) where they lived at diagnosis between 2009 and 2013
| Variable | Mean (StdErr/Std) | Median | 25th and 75th percentiles |
|---|---|---|---|
| UHF level variables | |||
| Demographic composition | |||
| Percent of residents who were non-Hispanic Black | 20.83 (3.33) | 11.367 | 3.07, 29.25 |
| Male couple headed households per 10,000 households | 61.77 (60.31) | 39.50 | 26.81, 71.38 |
| Percent of residents who were 21 to 54 years old | 51.39 (0.89) | 49.42 | 47.71, 54.19 |
| Social disorder | |||
| Residential vacancy (vacancies per mi2) | 40.96 (4.29) | 35.20 | 19.69. 55.52 |
| Policing | |||
| Stops without arrest per 100,000 residents | 12.116.11 (10,917.43) | 9489.81 | 3007.8. 17,163.63 |
| Economic disadvantage | |||
| Median income (US dollars) | 57,714.10 (3748.18) | 54,629.50 | 38,087.50, 74,518.00 |
| Percent unemployed | 9.44 (0.47) | 8.90 | 7.40, 11.61 |
| Percent in poverty | 19.00 (1.45) | 16.53 | 12.46, 26.77 |
| Percent on public assistance | 4.35 (0.47) | 3.23 | 2.23, 5.88 |
| Percent without a high school education | 20.38 (1.64) | 19.28 | 12.46. 25.97 |
| UHF economic disadvantage component | 0 (2.09) | −0.03 | −1.33. 1.69 |
| Poor access to healthcare | |||
| Percent uninsured | 16.16 (1.05) | 15.14 | 12.41. 21.89 |
| Percent went without needed care | 11.46 (0.59) | 10.93 | 8.73, 14.63 |
| Poor access to healthcare component | 0 (0.07) | −0.01 | −0.05, 0.07 |
| Individual level variables N (%) | |||
| Race/ethnicity | |||
| Hispanic/Latino | 2672 (37.32) | ||
| Non-Hispanic White | 1887 (26.36) | ||
| Non-Hispanic Black | 2600 (36.32) | ||
| Nativity | |||
| Foreign born | 1905 (26.61) | ||
| Not foreign born | 5254 (73.39) | ||
| History of homelessness | |||
| Yes | 160 (2.23) | ||
| No or unknown | 6999 (97.77) | ||
| Age at diagnosis | |||
| 13–19 | 433 (6.05) | ||
| 20–29 | 3183 (44.46) | ||
| 30–39 | 1857 (25.94) | ||
| 40–49 | 1183 (16.52) | ||
| 50–59 | 389 (5.43) | ||
| 60+ | 114 (1.59) | ||
| Year of diagnosis | |||
| 2009 | 1451 (20.27) | ||
| 2010 | 1450 (20.25) | ||
| 2011 | 1466 (20.48) | ||
| 2012 | 1401 (19.57) | ||
| 2013 | 1391 (19.43) | ||
| Suppression status | |||
| Suppressed | 4073 (56.89) | ||
| Durably suppressed | 2541 (35.49) | ||
Untransformed variables reported
In the 42 UHFs where these MSM lived, the median number of MSM-headed households per 10,000 was 39.50 (25th percentile=26.81; 75th percentile=71.38). The median percent of residents who were Black was 11.37%, and varied substantially across UHFs (25th percentile= 3.07%; 75th percentile= 29.25%). See Table 1 for distributions of other UHF-level variables.
Suppression
Regardless of individual race/ethnicity, there appeared to be a U-shaped association between the percent of the UHF population who were Black and suppression (Table 2). In the bivariate model, MSM living in UHF districts where 5%−29% of residents were Black were more likely to be suppressed than MSM living in districts where >30% residents were Black (relative risk [RR]=1.14, p<0.0001). This association also existed in the multivariable model which controlled for individual-level covariates (i.e., nativity, homeless history, age at diagnosis, year of diagnosis, and race/ethnicity): MSM living in UHF districts where 5%−29% of residents were Black were 7% more likely to be suppressed than MSM living in districts where ≥30% of residents were Black (adjusted relative risk [ARR]=1.07, p=0.04). The positive bivariate association between living in a district with a low percentage (<5%) of Black residents and suppression (RR=1.11, p=0.01) was not found in the multivariable model (ARR=1.00, p=1.00).
Table 2.
Bivariate and multivariable results of a multilevel regression of HIV viral suppression on individual-and United Hospital Fund- (UHF-) level covariates in a sample of HIV-positive men who have sex with men (MSM; N = 7159) in New York City diagnosed between 2009 and 2013
| Variables | Bivariate models | Multivariable model | ||
|---|---|---|---|---|
| Relative risk | p alue | Relative risk | p value | |
| UHF-level variables | ||||
| % Residents who were non-Hispanic Black (ref = high) | ||||
| Low < 5.00 | 1.11 | 0.01 | 0.9998 | 0.996 |
| Medium 5.00 to <30.00 | 1.14 | <0.0001 | 1.07 | 0.04 |
| Male couple headed households per 10,000 households (ref = high) | ||||
| Low < 30 | 0.89 | 0.006 | 0.95 | 0.28 |
| Medium 30 to <60 | 0.98 | 0.52 | 1.01 | 0.76 |
| % Residents who were 21 to 54 years old | 1.01 | 0.06 | 0.997 | 0.28 |
| Economic disadvantagea | 0.99 | 0.23 | ||
| Residential vacancy | 0.999 | 0.01 | 0.9997 | 0.53 |
| Poor access to healthcare | 1.01 | 0.96 | ||
| Stops without arrest per 100,000 residents (ref = high) | ||||
| Stops without arrest per 100,000 residentsb | ||||
| Low < 6000 | 1.11 | 0.17 | 1.06 | 0.41 |
| Medium 6000 to <22,000 | 1.11 | 0.14 | 1.06 | 0.37 |
| Stops without arrest per 100,000 residents × Latino | ||||
| Low < 6000 | 0.99 | 0.90 | 0.997 | 0.97 |
| Medium 6000 to <22,000 | 0.95 | 0.56 | 1.03 | 0.73 |
| Stops without arrest per 100,000 residents × While | ||||
| Low < 6000 | 0.93 | 0.43 | 0.91 | 0.31 |
| Medium 6000 to <22,000 | 0.84 | 0.06 | 0.84 | 0.05 |
| Individual level variables | ||||
| Race/ethnicity (ref = Black) | ||||
| Latino | 1.13 | <0.0001 | 1.05 | 0.48 |
| White | 1.21 | <0.0001 | 1.27 | 0.004 |
| Foreign born | 1.05 | 0.03 | 1.02 | 0.35 |
| History of homelessness | 0.70 | 0.001 | 0.71 | 0.001 |
| Age at diagnosis (ref = 20–29) | ||||
| 13–19 | 0.83 | 0.0008 | 0.85 | 0.005 |
| 30–39 | 1.11 | 0.0001 | 1.08 | 0.002 |
| 40–49 | 1.22 | <0.0001 | 1.2 | <0.0001 |
| 50–59 | 1.28 | <0.0001 | 1.23 | <0.0001 |
| 60+ | 1.23 | 0.0025 | 1.16 | 0.02 |
| Year of diagnosis (ref = 2009) | ||||
| 2010 | 1.21 | <0.0001 | 1.2 | <0.0001 |
| 2011 | 1.42 | <0.0001 | 1.42 | <0.0001 |
| 2012 | 1.57 | <0.0001 | 1.55 | <0.0001 |
| 2013 | 1.70 | <0.0001 | 1.7 | <0.0001 |
Higher values mean more disadvantage
This is the main effect. In our interaction model it is the effect for Black alone
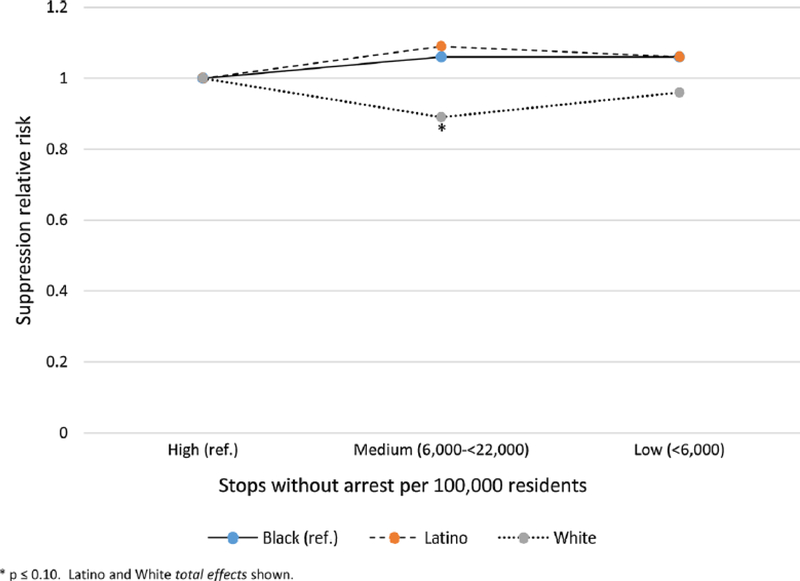
The association of the rate of police stops without an arrest to suppression varied by individual race/ethnicity (Figure 2). In both bivariate and multivariable models, there was no significant association between rates of stop without arrest and suppression for Black or Latino MSM. However, for White MSM living in UHFs with a medium rather than a high amount of stops (i.e., between 6,000–22,000 stops without arrest vs. >22,000 stops without an arrest per 100,000 residents) was associated with lower viral suppression (RR=0.84, p=0.06; ARR=0.84, p=0.05).
Figure 2.
Association of United Hospital Fund (UHF)-level rate of stop and frisk without an arrest per 100,000 residents with HIV suppression by individual race/ethnicity in a sample of 7,159 men who have sex with men (MSM in New York City diagnosed with HIV between 2009–2013
The UHF-level concentration of households headed by MSM couples, residential vacancy, and percent of residents aged 21–54 years were significantly associated with suppression in bivariate models but not in multivariable models.
Durable Suppression
Living in UHFs with a lower concentration of MSM-headed households was generally associated with a smaller likelihood of durable suppression than living in UHFs with a higher concentration of MSM (Model A, Table 3), though the magnitude of this relationship varied by individual race/ethnicity. Bivariate and multivariable models suggest that Black MSM living in a UHF with a low concentration of MSM-coupled households (<30/10,000) were 18% less likely to achieve durable suppression than those living in a UHF with a higher concentration of MSM-coupled households (≥60/10,000; RR=0.80, p=0.01; ARR=0.82. p=0.05). Among Black MSM, the chances of achieving durable suppression were also less if they lived in a UHF with a medium concentration of MSM-coupled households (30 to< 60 MSM-coupled households/10,000 households) compared to a higher concentration (RR=0.90, p=0.14; ARR=0.89, p=0.10). Relationships between the concentration of MSM-coupled households and durable suppression were the same for Latino MSM as for Black MSM (i.e., the Latino interaction p-value was not significant). As with Black and Latino MSM, models indicate that White MSM had a lower likelihood of durable suppression if they lived in a UHF with a low concentration of MSM-coupled households (i.e., the White interaction p-value comparing low to high was not significant). However, for White MSM, as compared to Black MSM, living in a UHF district with a medium concentration of MSM-coupled households, compared to a UHF with a high concentration, was also associated with a larger chance of achieving durable suppression (RR=1.22, p=0.03; ARR=1.26, p=0.01).
The moderation effect of race/ethnicity on the association between UHF age composition and durable suppression found in bivariate models was not present in the multivariable model; there was no effect for Blacks (Model B, Table 3). Several other UHF-level variables were significant in bivariate models but not in multivariable models (i.e., percent of residents who were Black; economic disadvantage; residential vacancy; stops without arrest per resident).
DISCUSSION
The present analyses extend the fledgling line of multilevel research on place characteristics and viral suppression. In this analysis of NYC surveillance data, we found that MSM were more likely to achieve suppression if they lived in a UHF where between 5% and 29% of residents were Black, compared to UHFs with a higher percentage of Black residents. They were more likely to achieve durable suppression if they lived in a UHF with a higher concentration of MSM-headed households.
Research suggests that higher concentrations of MSM may be protective against adverse HIV-related outcomes. Frye et al. found that MSM living in NYC neighborhoods with higher percentages of MSM-headed households were more likely to consistently use condoms (46); Mills et al. found that they were more likely to get tested for HIV (47). Druyts et al. report that HIV-positive individuals living in areas with a high concentration of people who inject drugs had a 3 time higher mortality risk than those living in areas with a high concentration of MSM, regardless of these individuals’ transmission mode (48). The mechanisms driving these associations are unclear, but several pathways are possible. Neighborhoods with a higher concentration of MSM residents may provide “safe spaces” within MSM’s mesosystems where MSM can more freely express their sexuality and full personhood. Such neighborhoods have historically been loci of AIDS activism and community-driven HIV-related services (49). These neighborhoods have also benefited from exosystem resources as they have been prioritized by the NYC DOHMH and other organizations for HIV-related services. Given the long history of HIV - and of collectively acting to survive HIV - among MSM in NYC, these neighborhoods may have protective macrosystem norms facilitating routine HIV testing, linkage to care for people who are HIV-diagnosed, and long-term HAART engagement. Residents of these safer, less stigmatizing, service-rich spaces may thus be more likely to learn their status early, disclose their status, and receive support to engage in long-term HAART. Future research should explore which - if any - of these possible pathways connects higher concentrations of MSM to durable suppression. Our measure of the percent of households in a UHF that were headed by MSM was derived from that variable’s distribution. Future research could explore whether there are tipping points in the relationship between MSM-headed households and durable suppression.
Pathways explaining the relationship between the percent of residents who are Black and suppression may be similar to those described above. Because of the long history of surviving HIV/AIDS in Black communities, NYC UHFs with a medium percent of residents who are Black may have macrosystem norms promoting HIV testing and risk-reduction practices (50). These UHFs have exosystem resources in that they often have community-driven HIV-related services (51), and have been prioritized by the NYC DOHMH and other organizations for these services. These norms, practices, and services may facilitate early HIV detection, linkage to care, and HAART initiation. Future research should explore these possible pathways. It is also necessary to investigate why residence in a UHF with a high percentage of Black residents (i.e., ≥30%) was not positively associated with suppression. We hypothesize that these same norms, practices, and services exist in these UHFs, but that their beneficial effects are undermined by high levels of exosystem structural discrimination(52) and the intense macrosystem social scrutiny experienced by Black men (53). Future research could explore this, and also whether or not there are tipping points in the relationship between the percent of residents who are Black and durable suppression.
The percent of residents who are Black in a UHF was not associated with durable suppression. We hypothesize that (A) MSM are better able to consistently adhere to HAART over time when they live in a context that is home to resourced MSM networks and to services specifically designed for MSM(54); and (B) that high levels of exosystem structural discrimination (52) undermines resources and services that are protective for MSM in UHFs with a high percent of residents who are Black.
While there was no association of stops without arrest to suppression for Black and Latino MSM, White MSM living in a UHF with a high rather than a medium amount of such stops were more likely to be suppressed. Analyses of Stop and Frisk data indicate that Blacks and Latinos are disproportionately stopped across all NYC neighborhoods (55). This disproportionate targeting is part of the exosystem and may raise Black and Latino MSM’s risk of not achieving suppression across all UHFs. Another interpretation may be that White MSM actively benefit from feelings of safety generated by seeing police in their neighborhoods. This last interpretation is consistent with minority threat theories of policing, which state that police structurally and interpersonally function to uphold the interests of Whites in society (56). Future research should be undertaken to identify changes in these results following the end to the practice of Stop and Frisk in 2014.
Several of the UHF-level characteristics that were statistically significant in bivariate models had lower effect estimates and were not statistically significant in multivariable models. Post-hoc analyses suggest that these associations lost magnitude and significance when individual-level covariates were added to the model. Individual level variables associated with suppression and durable suppression were in expected directions. For example, year of diagnosis associated with both suppression and durable suppression such that individuals diagnosed more recently were more likely to achieve suppression and durable suppression. This is not surprising, given NYC DOHMH efforts to engage and retain newly diagnosed people in care. Consistent with prior research (57–60), individuals in this study who had a history of homelessness were less likely to achieve suppression than those without this history. Also consistent with prior research (6), individuals who were Latino or White were more likely to achieve suppression than individuals who were Black. Arnold et al. (2009), studying the effects of neighborhood on HIV mortality and HAART initiation, found that being Black was not associated with HIV mortality after accounting for neighborhood residence(19). However, being Black was independently associated with no or delayed HAART uptake. Such findings and the shifts in magnitude and significance of place-based characteristics to the outcomes seen here testify to the importance of using multilevel models to explore relationships of place to health instead of ecologic models. Future studies should explore the extent to which individual-level variables might moderate relationships between place-based characteristics and suppression or durable suppression.
Limitations
This analysis has several limitations. We were restricted to individual-level variables available in the NYC DOHMH surveillance registry. We were therefore unable to control for some potentially important covariates, such as individual income and education. We were also unable to create a specific measure of geographic access to HIV care. Analyses were not longitudinal. We could not examine whether or how selection into UHFs shaped UHF/suppression relationships or make causal claims. We operationalized “place” in terms of residential UHF at diagnosis. This may have misclassified place-based exposures. UHFs are large and often contain several subjectively defined neighborhoods; moreover if individuals moved to a new UHF post-diagnosis these new neighborhoods might affect outcomes. Additionally, MSM are likely to be exposed to other places routinely when they travel outside their UHF (61), which may have shaped suppression outcomes in ways that we could not measure. Finally, persons who did not report an address within a NYC UHF at diagnosis were excluded from analyses.
CONCLUSION
Despite these limitations, this analysis expands our current understanding of how place characteristics are associated with HIV viral suppression and durable viral suppression among NYC MSM. We found that living in neighborhoods with a “medium” percent of residents who were Black was associated with suppression among MSM, and that durable suppression among MSM was associated with living in a neighborhood with a greater concentration of MSM-coupled households. Future multilevel research should explore these associations in longitudinal panels or cohorts, and investigate causal pathways through which place characteristics affect viral suppression, in order to inform interventions. Such causal pathways may include retention in HIV care, or behaviors such as adherence to HAART treatment regimes. Understanding these causal pathways may provide insights into increasing viral suppression within communities. If longitudinal studies support our findings, interventions to build community capacity might seek to enhance protective norms and resources in Black communities, and in communities home to many MSM-headed households.
Acknowledgements:
This work was supported by R01 DA035707 (Campbell, Des Jarlais) and by the Emory Center for AIDS Research (P30 AI050409; Curran).
Footnotes
Conflict of interest: The authors declare that they have no conflict of interest.
Ethical Approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study formal consent in not required. This article does not contain any studies with animals performed by any of the authors. The study was approved by the Mount Sinai St. Luke’s IRB and the New York City Department of Health IRB.
RFERENCES
- 1.The Office of National AIDS Policy. NATIONAL HIV/AIDS STRATEGY for the UNITED STATES: UPDATED TO 2020 Washington, D.C: 2015. [Google Scholar]
- 2.Doshi RK, Matthews T, Isenberg D, Matosky M, Milberg J, Malitz F, et al. , editors. Continuum of HIV care among Ryan White HIV/AIDS Program clients, United States, 2010. Conference on Retroviruses and Opportunistic Infections; 2013. [Google Scholar]
- 3.Cohen SM, Hu X, Sweeney P, Johnson AS, Hall HI. HIV viral suppression among persons with varying levels of engagement in HIV medical care, 19 US jurisdictions. JAIDS Journal of Acquired Immune Deficiency Syndromes 2014;67(5):519–27. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. HIV Surveillance Report, 2014 November 2015.
- 5.Centers for Disease Control and Prevention. Diagnosed HIV infection among adults and adolescents in metropolitan statistical areas—United States and Puerto Rico, 2013 HIV Surveillance Supplemental Report 2015. September 2015. Contract No.: 4
- 6.Singh S, Bradley H, Hu X, Skarbinski J, Hall HI, Lansky A. Men living with diagnosed HIV who have sex with men: progress along the continuum of HIV care--United States, 2010. MMWR Morbidity and mortality weekly report 2014;63(38):829–33. [PMC free article] [PubMed] [Google Scholar]
- 7.Millett GA, Flores SA, Peterson JL, Bakeman R. Explaining disparities in HIV infection among black and white men who have sex with men: a meta-analysis of HIV risk behaviors. Aids 2007;21(15):2083–91. [DOI] [PubMed] [Google Scholar]
- 8.Hess KHX, Lansky A, Mermin J, Hall HI. Estimating the lifetime risk of a diagnosis of HIV infection in the United States. Conference on Retroviruses and Opportunistic Infections (CROI); February 22–25, 2016; Boston2016. [Google Scholar]
- 9.Gross R, Yip B, Lo Re V, Wood E, Alexander CS, Harrigan PR, et al. A simple, dynamic measure of antiretroviral therapy adherence predicts failure to maintain HIV-1 suppression. Journal of Infectious Diseases 2006;194(8):1108–14. [DOI] [PubMed] [Google Scholar]
- 10.Arnsten JH, Demas PA, Grant RW, Gourevitch MN, Farzodegan H, Howard AA, et al. Impact of active drug use on antiretroviral therapy adherence and viral suppression in HIV-infected drug users. Journal of general internal medicine 2002;17(5):377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yehia BR, Rebeiro P, Althoff KN, Agwu AL, Horberg MA, Samji H, et al. Impact of Age on Retention in Care and Viral Suppression. Jaids-Journal of Acquired Immune Deficiency Syndromes 2015;68(4):413–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Eberhart MG, Voytek C, Hillier A, Metzger D, Blank M, Brady K. Travel distance to HIV medical care: a geographic analysis of Weighted survey data from the medical monitoring project in Philadelphia, PA. AIDS and behavior 2014;18(4):776–82. [DOI] [PubMed] [Google Scholar]
- 13.Shacham E, Lian M, Onen NF, Donovan M, Overton ET. Are neighborhood conditions associated with HIV management? HIV medicine 2013;14(10):624–32. [DOI] [PubMed] [Google Scholar]
- 14.Wiewel EW, editor Association of neighborhood-level socioeconomic status (SES) with time from HIV diagnosis to viral suppression among newly diagnosed New Yorkers, 2006–2010 142nd APHA Annual Meeting and Exposition (November 15-November 19, 2014); 2014: APHA. [Google Scholar]
- 15.Beattie C, editor Structural barriers to HIV viral load suppression at an urban HIV/AIDS care center 143rd APHA Annual Meeting and Exposition (October 31-November 4, 2015); 2015: APHA. [Google Scholar]
- 16.Bronfenbrenner U Toward an experimental ecology of human development. American psychologist 1977;32(7):513. [Google Scholar]
- 17.Berkman LF, Kawachi I. A Historical Framework for Social Epidemiology: Social Determinants of Population Health In: Berkman LF, Kawachi I, Glymour MM, editors. Social epidemiology 2nd ed. New York. NY: Oxford University Press; 2014. p. 1–16. [Google Scholar]
- 18.Katz MH, Hsu L, Lingo M, Woelffer G, Schwarcz SK. Impact of socioeconomic status on survival with AIDS. American journal of epidemiology 1998;148(3):282–91. [DOI] [PubMed] [Google Scholar]
- 19.Arnold M, Hsu L, Pipkin S, McFarland W, Rutherford GW. Race, place and AIDS: the role of socioeconomic context on racial disparities in treatment and survival in San Francisco. Social science & medicine 2009;69(1):121–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Marconi VC, Grandits GA, Weintrob AC, Chun H, Landrum ML, Ganesan A, et al. Research Outcomes of highly active antiretroviral therapy in the context of universal access to healthcare: the US Military HIV Natural History Study 2010. [DOI] [PMC free article] [PubMed]
- 21.Wallace R Urban desertification, public health and public order: ‘planned shrinkage’, violent death, substance abuse and AIDS in the Bronx. Social science & medicine 1990;31(7):801–13. [DOI] [PubMed] [Google Scholar]
- 22.Mugavero MJ, Amico KR, Horn T, Thompson MA. The state of engagement in HIV care in the United States: from cascade to continuum to control. Clinical Infectious Diseases 2013;57(8): 1164–71. [DOI] [PubMed] [Google Scholar]
- 23.Chida Y, Vedhara K. Adverse psychosocial factors predict poorer prognosis in HIV disease: a meta-analytic review of prospective investigations. Brain, behavior, and immunity 2009;23(4):434–45. [DOI] [PubMed] [Google Scholar]
- 24.Canan CE, Lau B, McCaul ME, Keruly J, Moore RD, Chander G. Effect of alcohol consumption on all-cause and liver-related mortality among HIV-infected individuals. HIV medicine 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Terry v. Ohio US: Supreme Court; 1968. p. 1. [Google Scholar]
- 26.Liebschutz J, Schwartz S, Hoyte J, Conoscenti L, Christian AB Sr., Muhammad L, et al. A Chasm Between Injury and Care: Experiences of Black Male Victims of Violence. Journal of Trauma-Injury Infection and Critical Care 2010;69(6):1372–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Woods SJ, Wineman NM, Page GG, Hall RJ, Alexander TS, Campbell JC. Predicting immune status in women from PTSD and childhood and adult violence. Advances in Nursing Science 2005;28(4):306–19. [DOI] [PubMed] [Google Scholar]
- 28.Cooper HL, Arriola KJ, Haardörfer R, McBride CM. Population-Attributable Risk Percentages for Racialized Risk Environments. American journal of public health 2016;106(10):1789–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ford CL, Airhihenbuwa CO. Critical race theory, race equity, and public health: toward antiracism praxis. American journal of public health 2010;100(S1):S30–S5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sewell AA, Massey DS, Denton NA. A Different Menu: Racial Residential Segregation and the Persistence of Racial Inequality. Race and Ethnic Relations in the 21st Century: History, Theory, Institutions, and Policy 2010:287–96. [Google Scholar]
- 31.Goranson CKS, Jasek J, Olson C, Kerker B. The New York City Community Health Survey Atlas, 2007. The New York City Department of Health and Mental Hygiene; 2009. [Google Scholar]
- 32.United States Census Bureau. 2010 Census. 2010 Census Washington, DC: 2010. [Google Scholar]
- 33.Centers for Disease Control and Prevention. Selected National HIV Prevention and Care Outcomes in the United States Atlanta: 2016. [Google Scholar]
- 34.U.S. Census Bureau’s American Community Survey Office. 2007 – 2011 American Community Survey. American Community Survey 2011.
- 35.New York City Department of Health and Mental Hygiene. Community Health Survey 2009–2010. Community Health Survey2009–2010
- 36.United States Census Bureau. 2009. U.S Census Bureau’s Zip Code Business Patterns. Zip Code Business Patterns2009
- 37.New York City Department of Health and Mental Hygiene. Epiquery: NYC Interactive Health Data System - Vital Statistics 2009. Vital Statistics2009
- 38.United States Postal Service/Department of Housing and Urban Development. HUD Aggregated USPS Administrative Data On Address Vacancies 2009. USPS Delivery Stats Product2009.
- 39.New York Police Department. Stop Question and Frisk Data. Stop Question and Frisk Data 2009.
- 40.SAS Institute. The SAS system for Windows, 9.3. Cary, NC2011
- 41.Friedman SR, Cooper HL, Tempalski B, Keem M, Friedman R, Flom PL, et al. Relationships of deterrence and law enforcement to drug-related harms among drug injectors in US metropolitan areas. Aids 2006;20(1):93–9. [DOI] [PubMed] [Google Scholar]
- 42.Friedman SR, West BS, Tempalski B, Morton CM, Cleland CM, Des Jarlais DC, et al. Do metropolitan HIV epidemic histories and programs for people who inject drugs and men who have sex with men predict AIDS incidence and mortality among heterosexuals? Annals of epidemiology 2014;24(4):304–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Friedman SR, West BS, Pouget ER, Hall HI, Cantrell J, Tempalski B, et al. Metropolitan social environments and pre-HAART/HAART era changes in mortality rates (per 10,000 adult residents) among injection drug users living with AIDS. PloS one 2013;8(2):e57201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhang J, Kai FY. What’s the relative risk?: A method of correcting the odds ratio in cohort studies of common outcomes. Jama 1998;280(19):1690–1. [DOI] [PubMed] [Google Scholar]
- 45.Davies HTO, Crombie IK, Tavakoli M. When can odds ratios mislead? Bmj 1998;316(7136):989–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Frye V, Koblin B, Chin J, Beard J, Blaney S, Halkitis P, et al. Neighborhood-level correlates of consistent condom use among men who have sex with men: a multi-level analysis. AIDS and behavior 2010;14(4):974–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mills CW, Sabharwal CJ, Udeagu C-C, Bocour A, Bodach S, Shepard C, et al. Barriers to HIV testing among HIV/AIDS concurrently diagnosed persons in New York City. Sexually transmitted diseases 2011;38(8):715–21. [DOI] [PubMed] [Google Scholar]
- 48.Druyts EF, Rachlis BS, Lima VD, Harvard SS, Zhang W, Brandson EK, et al. Mortality is influenced by locality in a major HIV/AIDS epidemic. HIV medicine 2009;10(5):274–81. [DOI] [PubMed] [Google Scholar]
- 49.Chambré SM. Fighting for our lives: New York’s AIDS community and the politics of disease: Rutgers University Press; 2006.
- 50.Arnold EA, Bailey MM. Constructing home and family: How the ballroom community supports African American GLBTQ youth in the face of HIV/AIDS. Journal of gay & lesbian social services 2009;21(2–3):171–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Painter TM, Ngalame PM, Lucas B, Lauby JL, Herbst JH. Strategies used by community-based organizations to evaluate their locally developed HIV prevention interventions: Lessons learned from the CDC’s innovative interventions project. AIDS Education and Prevention 2010;22(5):387. [DOI] [PubMed] [Google Scholar]
- 52.Massey DS, Denton NA. American apartheid: Segregation and the making of the underclass: Harvard University Press; 1993.
- 53.Collins PH. Hegemonic Masculinity and Black Gender Ideology In: O’Hara RGaJF, editor. Composing Gender Boston: Bedford/St. Martin’s; 2014. [Google Scholar]
- 54.Keen L 2nd, Dyer TP, Whitehead NE, Latimer W Binge drinking, stimulant use and HIV risk in a sample of illicit drug using heterosexual Black men. Addictive behaviors 2014;39(9):1342–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gelman A, Fagan J, Kiss A. An analysis of the New York City police department’s “stop-and-frisk” policy in the context of claims of racial bias. Journal of the American Statistical Association 2012. [Google Scholar]
- 56.Holmes MD, Smith BW. Intergroup dynamics of extra-legal police aggression: An integrated theory of race and place. Aggression and Violent Behavior 2012;17(4):344–53. [Google Scholar]
- 57.Lim S, Nash D, Hollod L, Harris TG, Lennon MC, Thorpe LE. Influence of Jail Incarceration and Homelessness Patterns on Engagement in HIV Care and HIV Viral Suppression among New York City Adults Living with HIV/AIDS. PloS one 2015;10(11). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Loh J, Kennedy MC, Wood E, Kerr T, Marshall B, Parashar S, et al. Longer duration of homelessness is associated with a lower likelihood of non-detectable plasma HIV-1 RNA viral load among people who use illicit drugs in a Canadian setting. Aids Care-Psychological and Socio-Medical Aspects of Aids/Hiv 2016;28(11):1448–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Marshall BDL, Elston B, Dobrer S, Parashar S, Hogg RS, Montaner JSG, et al. The population impact of eliminating homelessness on HIV viral suppression among people who use drugs. Aids 2016;30(6):933–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Thakarar K, Morgan JR, Gaeta JM, Hohl C, Drainoni ML. Homelessness, HIV, and Incomplete Viral Suppression. Journal of health care for the poor and underserved 2016;27(1):145–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Koblin BA, Egan JE, Rundle A, Quinn J, Tieu H-V, Cerdá M, et al. Methods to measure the impact of home, social, and sexual neighborhoods of urban gay, bisexual, and other men who have sex with men. PloS one 2013;8(10):e75878. [DOI] [PMC free article] [PubMed] [Google Scholar]