Abstract
Background
Mid-term clinical and radiological evaluation of a carbon-fiber cage in multilevel cervical spondylosis (MCS). Anterior cervical corpectomy and fusion (ACCF) using titanium mesh cages (TMC) has shown satisfactory outcomes, but with subsidence of up to 20%. Conventional long-fiber carbon fiber cages have shown a safe profile in discectomy/fusion (ACDF) but with minimal data in the setting of corpectomy.
Methods
Retrospective review of a single centre multi-surgeon cohort of MCS patients from 2007–2012. Follow-up period was a minimum of 3.5 years, mean 6 years. Outcomes included peri-operative, clinical [Nurick, European Myelopathy, Visual Analogue Scores (VAS), modified Japanese Orthopaedic Association (mJOA) scores and radiographic (C2C7, Cobb & ROM angles)].
Results
A total of 102 consecutive patients were included. Mean length of stay was 5.5 (SD 3.5) days, blood loss 322 (SD 358) mL and operative time 98 (SD 31) min. Corpectomy levels included 72 single-level ACCF and 30 multiple ACCF. Fourteen had peri-operative complications. Three patients required early cage revisions. Mean pain scores improved from VAS neck 4.6 to 2.6 (P<0.01) and VAS arm 5.1 to 2.0 (P<0.01). Mean Nurick score improved from 1.2 to 0.4/4 (P<0.01). Mean follow-up EMS was 15.9/18 and mJOA was 14.0/17. Seventy follow-up radiographs were obtained. Flexion-extension angulation differences of >3 mm across the instrumented level were present in 5 patients, all of which displayed fusion of either grade 1 or 2. 7 had C2C7 kyphosis. Severe subsidence (>3 mm) was seen in 9 cases (13%).
Conclusions
Mid-term outcomes of this carbon-fiber cage indicate that it is safe and durable for the treatment of MCS with a similar radiological profile to that of TMC.
Keywords: Cervical spondylotic myelopathy, cervical corpectomy, cervical spondylosis, carbon fibre, reconstruction, titanium mesh cage (TMC), adjacent segment degeneration, PEEK
Introduction
Multilevel cervical spondylosis (MCS) is painful disc degeneration with arthropathy of the cervical spine, causing cervicobrachialgia, myelopathy or both. Anterior cervical corpectomy and fusion (ACCF) is frequently indicated as a surgical solution as it can address multiple levels of anterior based pathology, where stenotic pathology is posterior to the vertebral body [inaccessible with anterior cervical discectomy and fusion (ACDF)] and where it can restore lost cervical lordosis. Controversy persists regarding the optimal choice of reconstruction (1). Case series have indicated good mid-term results with ACCF using graft-impregnated titanium mesh cages (TMC), achieving greater than 95% fusion rates (2-4). However significant subsidence occurs in 11–19% (2,3) particularly with increasing levels and osteopenia, correlating with kyphosis and poorer clinical outcomes (5,6).
Carbon fibre is an alternative material of interest for reconstruction in the spine as it is demonstrates high versatility, a modulus approximating that of cortical bone, bio-inert characteristics and ease of radiographic or MRI assessment (5). The long fibers are aligned in the sagittal plane, according to the normal trajectory of the dominant bone trabeculae. 18-month outcomes have been described for stacked carbon-fiber cages in all-pathology ACCF, noting that subsidence may only be significant if greater than 3 mm (7). More recent literature has reported average graft subsidence for carbon fiber cages was 0.7 mm without revision surgery, compared to 2.9 mm subsidence and 11.1% revision rate within the same series for TMC (8).
There is no published case series with a large number of patients treated with ACCF with carbon fibre cages, and including an extended follow up. The aim of this study is therefore to establish the clinical and radiographic outcomes of a carbon-fiber polymer cage in the setting of MCS. Given the evolution of materials for ACCF, this is relevant to the current debate on optimal reconstructive material.
Methods
This was a retrospective study of 102 consecutive MCS patients treated with a ACCF and carbon-fiber cage from 2007–2012. The cages are designed with anisotropic long continuous carbon-fibers (PolyEtherKetoneEtherKetoneKetone), aligned along the biomechanical axis (ostaPek® composite, coLigne, Zurich, Switzerland), ranging from 17 to 63 mm height and 4° lordosis. Large fenestrations allow filling of morcelised autologous bone graft (Figure 1). In cases where the opposing end-plates were not almost parallel, then an alternative reconstruction was considered to prevent point-loading of the construct—these patients were excluded from the study. All patients were originally indicated for the procedure if they had cervical spondylosis with stenosis at multiple levels that mandated removal of the interposed vertebral body to provide adequate decompression. Patients were contacted for clinical and radiographic assessment. Patients were excluded for fracture, oncologic or infective pathology, or ossification of the posterior longitudinal ligament (OPLL), as these were treated from a posterior approach. Patients who had a prior ACDF were included. Ethical approval was granted by the local ethics committee.
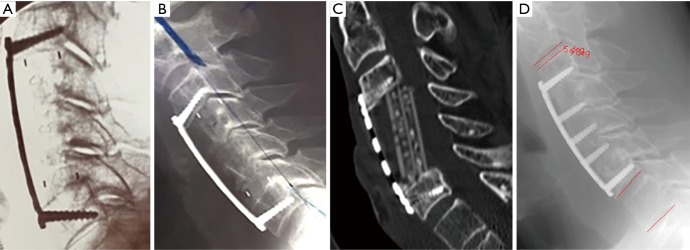
Figure 1.
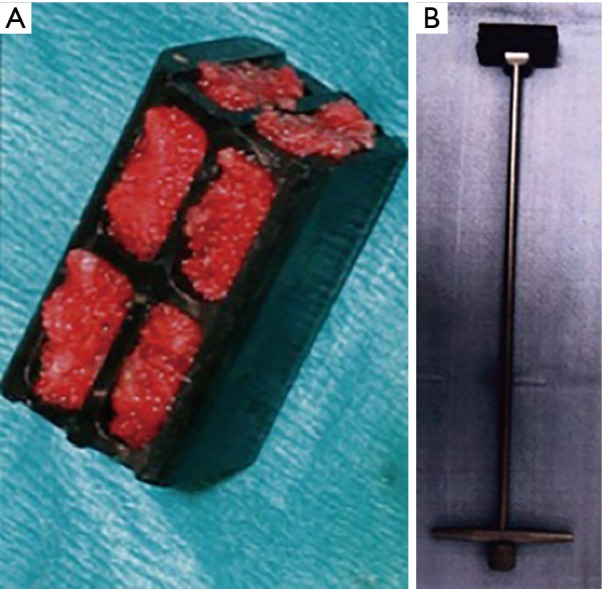
Cage and inserter. (A) Two-level carbon-fiber cage packed with autologous bone graft for insertion; (B) cage on its insertion handle.
Pre-operative details were recorded including Visual Analogue Scores (VAS) for pain, neurological deficit (Nurick grade), smoking status, ASA grade and co-morbidities. Peri-operative details were recorded including blood loss, operative time and corpectomy levels, peri-operative complications, additional clinical visits and additional cervical spine operations.
Patients were issued clinical questionnaires including Nurick, European Myelopathy Score (EMS), modified Japanese Orthopedic Association (mJOA) score and VAS for arm and neck.
Radiological outcomes included routine post-operative radiography. For the purposes of the study patients were additionally requested to undergo erect and dynamic radiographs. The fusion assessments were performed by the primary author (…) who was not involved in clinical management. Timepoints for the study were at a minimum of 2 years. Evaluations included:
❖ Segmental Cobb angle (sagittal alignment of the construct from the superior cephalad endplate to the inferior caudal endplate);
❖ Cervical lordosis: C2C7 angle (inferior endplate C2 to superior endplate C7);
❖ Fusion was defined as <2 mm difference between the tip of the supra- and subjacent spinous processes between flexion and extension views (9);
❖ Instrumentation integrity;
❖ Subsidence, defined as either none, mild (1–3 mm) or severe (>3 mm) (8);
❖ Adjacent segment degeneration at adjacent levels (<5° flexion-extension difference).
The neutral position was defined when the endplates were parallel, the kyphotic orientation when the angle between the two previous described lines were open posteriorly (a negative value), the lordotic orientation were described when the angle is open anteriorly (positive).
Surgical technique
Patients undergo general anaesthetic, a gel-foam ring is placed under the head and the endotracheal tube is directed to the opposite side of the operator. Positioning is checked with fluoroscopy prior to incision to ensure adequate visualisation, optimal orientation of the cervical spine and an orthogonal radiographic view. A Smith-Robinson approach is taken and rechecked on fluoroscopy. The midline is identified, and lateral self-retaining retractors are placed. Kaspar pins were placed in the midline. A trench of no more than 2 cm width is resected from the vertebral body(ies) to preserve the lateral vertebral body wall thus protecting the vertebral artery. A pituitary rongeur and high-speed burr are used for piecemeal resection, continued to the posterior longitudinal ligament, thus decompressing the spinal cord and enough space to allow resection of osteophytes at the cephalad and caudal disc spaces. Once the endplates are denuded of cartilage, the space is measured for the cage. The footprint must be as wide as possible to spread the load. Fluoroscopy is a useful aid to insertion and should be assessed for adequacy of decompression, cage position, cage-endplate congruity and segmental lordosis. If the cage has opened the space to recreate any lost lordosis, the facets should be opening anteriorly (intervertebral lordosis). An overlying spanning plate and screws are applied while avoiding violating adjacent disc spaces. The earlier plates were used with non-locked screws and later plates had constrained non-locked screws. A wound drain is advised with interrupted sutures to close the fascia and skin.
Statistics
Results are quoted in mean values (and/or percentages) with standard deviations (SD). Paired student t-test was used to identify pre- and post-operative clinical and radiological differences. ANOVA was used to analyse subsidence subgroups (none, mild, severe) for clinical outcomes. Two-tailed p-values significance was <0.05.
Results
Demographic (Table 1) and perioperative (Table 2) details are shown. Corpectomy levels included 72 single level ACCF, 19 two-level and 5 three-level ACCF, 6 ACCF plus pre-existing adjacent ACDF, all with an overlying plate (Table 3). Fourteen had peri-operative complications including five dural tears, two respiratory infections, one lower limb ischemia, three cervical hematomas and three revision procedures. Two of the hematomas were evacuated immediately post-index procedure and the second was performed at 48 hours.
Table 1. Demographic details.
| Characters | Outcome |
|---|---|
| Gender | 30 female, 72 male |
| Age | 64.5 years (SD 10.7 years) |
| Follow-up | Min 3.5 years, mean 6 years |
| Indication | Cervicobrachialgia 63, myelopathy 20, cervicobrachialgia & myelopathy 19 |
SD, standard deviation.
Table 2. Summary of peri-operative outcomes.
| Peri-operative outcome | Value (SD) |
|---|---|
| Blood loss | 322 mL [358] |
| Operative time | 98 min [31] |
| Peri-operative complications | 12 |
| Length of stay | 5.5 days (3.5) |
SD, standard deviation.
Table 3. Levels of corpectomy and long-term clinical outcomes.
| No. of levels | Cervical level | No. of patients | VAS neck/arm (SD) | Mean follow-up EMS max. 18 (SD) | Mean follow-up mJOA max. 17 (SD) |
|---|---|---|---|---|---|
| 1 | C4 | 11 | 2.9/2.4 (2.6/3.2) | 15.5 (2.6) | 12.7 (2.7) |
| C5 | 15 | 2.4/1.7 (1.3/1.6) | 16.0 (13.7) | 13.9 (2.8) | |
| C6 | 45 | 2.8/2.2 (2.0/2.4) | 15.8 (2.0) | 14.1 (2.2) | |
| C7 | 1 | 0/0 | 18.0 | 17.0 | |
| 1 & ACDF | C5 +/− ACDF C6C7 | 4 | 3.3/2.2 | 15.8 | 15.5 |
| 2 & ACDF | C5C6/C7 +/− ACDF C3C4 | 2 | 16.0 | 14.0 | |
| 2 | Mostly C5C6 | 19 | 2.3/2.7 (2.0/3.0) | 15.9 (2.4) | 13.6 (3.3) |
| 3 | C4C5C6 | 5 | 1.4/1 | 16.6 | 15.4 |
VAS, Visual Analogue Scores; mJOA, modified Japanese Orthopaedic Association; ACDF, anterior cervical discectomy and fusion.
Three revision procedures
One patient had a malpositioned cage that required revision within 24 hours. One cage migration progressed over 6 weeks to ultimately require revision (Figure 2). One patient had a posteriorly mal-placed cage requiring a posterior laminectomy at six weeks (the anterior cage was left in situ). Anterior revisions were performed with exchange of the cage for iliac crest cortical graft. One additional patient had a subsequent ACDF at C6C7 three years post C5 ACCF.
Figure 2.
Progression of radiographs of a 3 level ACCF. (A) Intra-operative, (B) 1 day, (C) CT at 6 weeks, (D) post-revision with iliac tricortical graft. While no posterior migration was noted on intra-operative fluoroscopy, the inferior footprint was not matched to the inferior endplate thus leaving the cage potentially unstable. The patient was then revised and did very well-follow-up NRS neck 2/10, arm 1/10, mJOA 17/18. ACCF, anterior cervical corpectomy and fusion; mJOA, modified Japanese Orthopaedic Association.
Eight patients were lost to follow-up but were included in the peri-operative analysis. Three were deceased, four had moved from the area (nursing facilities). Two of the eight had peri-operative complications as noted above. One was revised for early migration for a misplaced cage and was last seen at one year without problems. One had multiple dural adhesions with a mal-placed cage, who had a lower limb ischemia from an atheromatous embolism post-operatively, then had a posterior laminectomy at six months which resolved symptoms apart from pre-operative left arm weakness. The other patients had no complaints at 3 months’ follow-up.
Mean pre-operative pain scores were VAS neck 4.6 (SD 2.4) and VAS arm 5.1 (SD 2.8) and on follow-up, VAS neck was 2.6 (SD 1.9) (P<0.01) and VAS arm was 2.0 (SD 2.3) (P<0.01). Mean Nurick score improved from 1.2 (SD 1.2) to 0.4/4 (SD 0.8) (P<0.01). Mean EMS was 15.9/18 (SD 2.0) and mean mJOA was 14.0/17 (SD 2.3) at follow-up.
Radiological (Table 4)
Table 4. Summary of long-term radiographic outcomes.
| Radiographic variables | Outcome (70 patients) |
|---|---|
| Total pseudoarthroses | 5 (2 2 level, 3 1 level) |
| Total subsidence cases | 18 (26%) |
| Mean C2C7 cobb angle | 9.9° (SD 11.9°) |
| Mean segmental cobb angle | 2.3° (8.4°) |
| Severe subsidence | 9 (13%) |
| Total adjacent segment degenerations | 16/63 levels |
SD, standard deviation.
Seventy patients attended follow-up radiographs. Mean JOA, VAS Neck and VAS Arm of 13.8, 2.6 and 2.8 for those who attended for radiographic follow up were not significantly different to 14.3, 2.8 and 1.1 for those who did not (P>0.05). In some cases, the caudal aspect was not visible or assessable. CT scans were additionally provided during the follow up where available (Figures 2,3). An example of a patient with 5-year follow up is shown in Figure 4.
Figure 3.
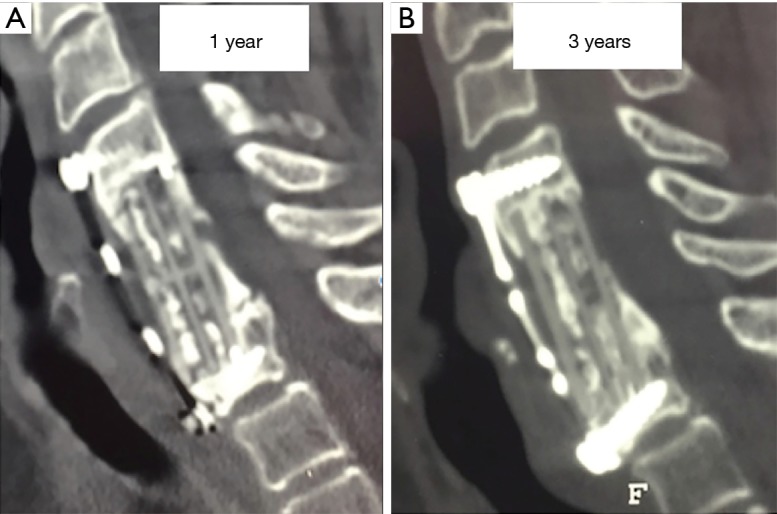
Sagittal CT scans of a patient with a 2 level C5C6 corpectomy and carbon-fiber cage reconstruction at (A) 1 year and (B) 3 years. The differences between both scans include the evolution of a persistent healing interface, the consolidation of bone within the cage and the resolution of a posterior osteophyte. Also evident is the broken screw inferiorly, potentially caused by the cage in contact with it. Subsidence (>3 mm) had occurred before one year.
Figure 4.
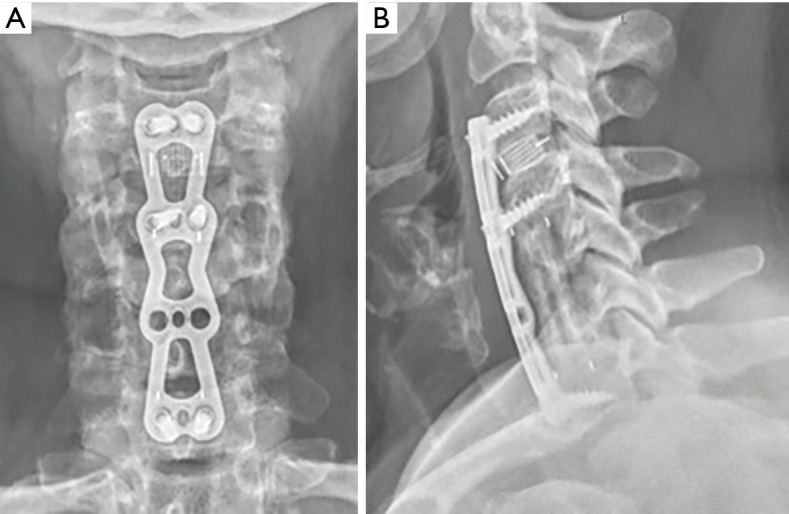
AP & lateral radiographs of patient at 5 years post ACCF C5C6 ACDF C3C4 fixation with evidence of good alignment in both coronal and sagittal planes, fusion, preservation of adjacent segments and lack of subsidence. ACCF, anterior cervical corpectomy and fusion; ACDF, anterior cervical discectomy and fusion.
Five patients demonstrated both segmental Cobb angle and overall C2C7 kyphosis. 3 further cases with a lordotic segmental Cobb angle had C2C7 kyphosis, totaling 8 with C2C7 kyphosis. Mean VAS Neck and Arm scores in those with C2C7 kyphosis were 3.4 and 4.6, which when combined were significantly higher than cases without kyphosis (P<0.05).
Collectively, there were five pseudarthrosis cases where dynamic radiographs displayed >2 mm spinous process differences. All of these were smokers, two were diabetic and two had recent trauma-induced central cord symptoms. Two had two-level and three had single level ACCF. Screw loosening or breakages were observed in 11 cases, including all pseudarthrosis cases described and separately, associated with segmental kyphosis in 2. There were no failed plates or cages. Some patients had interval CT scans as part of their follow up which demonstrated increasing osseous formation within and around the cage (Figure 3).
Subsidence was present in 20 cases (28.6%), 1 mm in 11 (mild, 15.7%) and >3 mm in 9 (severe, 13%). One severe and 4 mild subsidence cases were associated with a segmental kyphosis and 3 had an overall C2C7 kyphosis. Affected cases of severe subsidence included 6 single level, 2 two-level and 1 three level. Age, gender or smoking status did not affect subsidence rates. In some cases, the juxtaposition of the screws and cage prevented subsidence of the cage beyond the neck of the screw, particularly inferiorly (Figure 3). VAS neck, VAS arm, VAS combined, JOA and EMS were not significantly different when comparing subgroups of subsidence (none, mild, severe, P>0.1).
Five cages migrated posteriorly warranting revision surgery in 3 cases, as described above. This was related to either end-plate obliquity and footprint mismatch, or posterior or oblique positioning of the cephalad aspect.
Assessment of adjacent levels revealed flexion-extension angle differences in 9/40 proximal adjacent levels and 7/23 distal adjacent levels, excluding those who had radiographic evidence of degeneration or osteophytosis pre-operatively. One case had preserved motion at a caudal adjacent segment but with significant disc degeneration and neck pain.
Discussion
This retrospective follow-up of 102 MCS patients with ACCF and carbon-fiber cage has shown safety and durability in pain and neurological function and acceptable radiographic profile. The blood loss of 322 mL and operative time of 98 min compare favorably with the meta-analyses previously mentioned (340–986 mL, 211–264 min) (1). Clinical results demonstrate an overall sustained improvement of approximately 50% recovery of pain and neurological function, including a recovery of 0.8 Nurick grades with improved pain of 2.0 and 3.1 for VAS Neck and Arm respectively at a mean of 6 years’ follow-up.
Radiographic follow up in 70 cases had both clinical and radiographic follow up at six years, with similar clinical scores to those who did not attend. This demonstrated five pseudarthrosis cases, indicating a fusion rate of 92.8%. Loosening or breakage of screws occurred in 11 cases, including two with pseudarthrosis. Other series describe fusion rates of 96% (2,3). Given that the most accurate radiographic assessment of fusion is through spinous process tip distance measurement (10), the radiolucency of a carbon-fiber cage may confer an additional advantage for future MRI of the spinal cord but not regarding fusion when compared to TMC.
Defining subsidence for a series of ACCF can be difficult, as achieving comparative orthogonal radiographs to assess each end-plate is difficult. Subsidence was reported by Andaluz et al. as 18% in a series of 130 TMC without a strict definition (2). It has been defined as any loss of height by Raslan et al. (11), or of more than 3 mm by Gao et al. (in a series of 145 TMC with an incidence of 11%) (3). Perhaps the largest series of 300 ACCF with TMC was that by Chen et al. who reported mild subsidence (1–3 mm) in 182 (60.7%) and severe subsidence (>3 mm) in 57 (19.0%) (6). These are the criteria that we used in this study, with 1 mm subsidence in 11 (mild, 15.7%) and >3 mm in 9 (severe, 13%). Polyamide cages and carbon-fibre cages have both shown less subsidence than TMC (7,9). Like previous series, subsidence mostly occurred into the caudal superior endplate (12). Pain scores in the severe subsidence subgroup were not significantly higher than that of the overall cohort.
Adjacent segment degeneration occurred in 16/63 (25.4%) levels and adjacent segment disease requiring operation occurred in 1/94 (1%) of follow-up cases in this series. While ASD typically occurs more often at the cephalad level, the incidence in this series was higher for caudal levels. This may reflect the method for ASD evaluation (MRI follow up would be definitive) as one patient had ASD on MRI with preservation of movement, falling outside of the selection criteria. The series by Gao et al, using TMC and/or autograft demonstrated symptomatic ASD requiring operation in 16 patients (11.0%) (3). Andaluz et al. had 5 patients (3.8%) with ASD with operation 1–9 years later (mean 4.4±2.7 years) (2). However, the rate of ASD is relative to the mean age of the cohort (64.5 years in this series versus 54.4 years by Andaluz).
Technical considerations for insertion require thorough visual and radiographic evaluation of the compatibility of the cage with the void created by the corpectomy. This study highlights the potential for posterior malposition of the cephalad aspect of the cage. Given that insertion of the cage is aided by a handle (Figure 1B), one may be inclined to raise the handle on insertion thus risking posterior malpositioning. Footprint mismatch can predispose to posterior migration of the cage and subsidence as contact points are overloaded. While difficult to assess, one must be attentive to endplate preparation without violation, particularly on the caudal superior endplate. Over the lifetime of this implant, 15° lordosis cages have also been introduced thus increasing segmental lordotic reconstruction at the corpectomy site.
Limitations of this study include its retrospective nature, with variable time points after minimum 3.5 years follow up. Outcomes that were commonly recorded as part of the pre-operative assessment were then used on calling patients back as part of the study. While the study was based at a single institution, there were at least ten surgeons of variable amounts of experience involved in using this implant. The case series did not include a comparison group. The case series was heterogenous as the aim of the study was to evaluate the implant in all its clinical applications. Given that the series took place over a long period, there were few consistent clinical measures, thus VAS and Nurick score were the only scores applicable both pre-operatively and on follow-up. Perhaps a further drawback of mid-term follow-up in older patients is that eight patients were lost to clinical follow up despite three attempts to contact them and 32 patients declined radiographic follow up. Hence, 70% of cases had both clinical and radiographic follow up at six years, with similar clinical scores to those who did not attend. Most patients were referred with MRI without pre-operative radiographs. Thus pre-operative C2C7 lordotic angles were not used. Reporting outcomes of single level ACCF with this implant are part of an ongoing study.
Conclusions
This series of 102 patients with anterior cervical carbon cage reconstruction demonstrated safety and durability for improvements in pain and neurological function at six years follow-up. Severe subsidence occurred in 13% without clinical consequences and fusion was achieved in 93%, demonstrating similar outcome profiles to TMC.
Acknowledgments
Société Française de Chirurgie Orthopédique et Traumatologique/Irish Orthopaedic Association/Irish Institute of Trauma and Orthopaedic Surgery.
Ethical Statement: Ethical approval was granted by the local ethics committee.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Zhu B, Xu Y, Liu X, et al. Anterior approach versus posterior approach for the treatment of multilevel cervical spondylotic myelopathy: a systemic review and meta-analysis. Eur Spine J 2013;22:1583-93. 10.1007/s00586-013-2817-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Andaluz N, Zuccarello M, Kuntz IV C. Long-term follow-up of cervical radiographic sagittal spinal alignment after 1-and 2-level cervical corpectomy for the treatment of spondylosis of the subaxial cervical spine causing radiculomyelopathy or myelopathy: a retrospective study: Clinical article. J Neurosurg Spine 2012;16:2-7. 10.3171/2011.9.SPINE10430 [DOI] [PubMed] [Google Scholar]
- 3.Gao R, Yang L, Chen H, et al. Long term results of anterior corpectomy and fusion for cervical spondylotic myelopathy. PLoS One 2012;7:e34811. 10.1371/journal.pone.0034811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Han YC, Liu ZQ, Wang SJ, et al. Is anterior cervical discectomy and fusion superior to corpectomy and fusion for treatment of multilevel cervical spondylotic myelopathy? A systemic review and meta-analysis. PLoS One 2014;9:e87191. 10.1371/journal.pone.0087191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hee HT, Majd ME, Holt RT, et al. Complications of multilevel cervical corpectomies and reconstruction with titanium cages and anterior plating. J Spinal Disord Tech 2003;16:1-8. 10.1097/00024720-200302000-00001 [DOI] [PubMed] [Google Scholar]
- 6.Chen Y, Chen D, Guo Y, et al. Subsidence of titanium mesh cage: a study based on 300 cases. J Spinal Disord Tech 2008;21:489-92. 10.1097/BSD.0b013e318158de22 [DOI] [PubMed] [Google Scholar]
- 7.Kabir SM, Alabi J, Rezajooi K, et al. Anterior cervical corpectomy: review and comparison of results using titanium mesh cages and carbon-fiber reinforced polymer cages. Br J Neurosurg 2010;24:542-6. 10.3109/02688697.2010.503819 [DOI] [PubMed] [Google Scholar]
- 8.Weber MH, Fortin M, Shen J, et al. Graft subsidence and revision rates following anterior cervical corpectomy: a clinical study comparing different interbody cages. Clin Spine Surg 2017;30:E1239-45. 10.1097/BSD.0000000000000428 [DOI] [PubMed] [Google Scholar]
- 9.Zhang Y, Quan Z, Zhao Z, et al. Evaluation of anterior cervical reconstruction with titanium mesh cages versus nano-hydroxyapatite/polyamide66 cages after 1-or 2-level corpectomy for multilevel cervical spondylotic myelopathy: a retrospective study of 117 patients. PLoS One 2014;9:e96265. 10.1371/journal.pone.0096265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cannada LK, Scherping SC, Yoo JU, et al. Pseudoarthrosis of the cervical spine: a comparison of radiographic diagnostic measures. Spine 2003;28:46-51. 10.1097/00007632-200301010-00012 [DOI] [PubMed] [Google Scholar]
- 11.Raslan F, Koehler S, Berg F, et al. Vertebral body replacement with PEEK-cages after anterior corpectomy in multilevel cervical spinal stenosis: a clinical and radiological evaluation. Arch Orthop Trauma Surg 2014;134:611-8. 10.1007/s00402-014-1972-1 [DOI] [PubMed] [Google Scholar]
- 12.Bartels RH, Donk RD, Feuth T. Subsidence of stand-alone cervical carbon fiber cages. Neurosurgery 2006;58:502-8. 10.1227/01.NEU.0000197258.30821.50 [DOI] [PubMed] [Google Scholar]