Abstract
Ultrasound exams need skilled examiners, and simulation-based training could provide standardized and safe skill training. This study aims to give an overview of different types of virtual-reality simulators for use in abdominal diagnostic ultrasound training in radiology. Fifteen specialized radiologists and radiological residents were presented with two similar cases on four different simulators for abdominal ultrasound training. A feedback sheet for each individual simulator and for an overall comparison was filled out by all participants. All means of scores were compared, and simulators were ranked from least to most favorable. One simulator was ranked most favorable in seven out of nine questions, but none of the mean scores had statistically significant differences. All simulators were recommended for training radiologists, and all simulators were perceived to benefit trainees more than experienced ultra-sonographers.
Keywords: simulation, ultrasound, education, abdominal, virtual-reality, radiology
1. Introduction
Ultrasound is a safe and readily available diagnostic tool that, in the hands of a skilled examiner, can play a crucial role in the diagnostic process. In radiology, the diagnostic abdominal ultrasound exam is a highly valued skill in the practical curriculum [1]. Supervised scanning on patients can provide these skills, but relies on patient load, randomly represented pathologies, and the availability of expert supervisors. New virtual-reality simulators provide standardized training conditions, systematic case presentations including rare but crucial pathologies, and readily available automatic feedback [2].
Several simulators are available for training the diagnostic abdominal ultrasound examination using different types of technics and interfaces. Each have their own strengths and weaknesses, and all come at a certain cost and need trained instructors to oversee the training. Training on simulators can be effective and even cost-effective when the right simulator is chosen, but no current studies have explored which simulator best fits a specific need [3,4]. This study aims to give an overview of different types of virtual-reality simulators for use in abdominal diagnostic ultrasound training in radiology.
2. Materials and Methods
The participants in this study were specialized radiologists with more than five years of ultrasound experience or physicians starting specialization in radiology with less than six months of ultrasound experience (Table 1). They were recruited from two hospitals and one private ultrasound practice in Copenhagen, Denmark. Data collection was done in a standardized setting at Copenhagen Academy for Medical Education and Simulation, Rigshospitalet in June 2018 [5].
Table 1.
Demographics.
| Demographics | Radiological Residents | Radiologists | All |
|---|---|---|---|
| Group size | 7 | 8 | 15 |
| Female | 3 | 2 | 5 |
| Male | 4 | 6 | 10 |
| Ultrasound experience in weeks (SD) | 13.9 (17.5) | 1093 (491.7) | - |
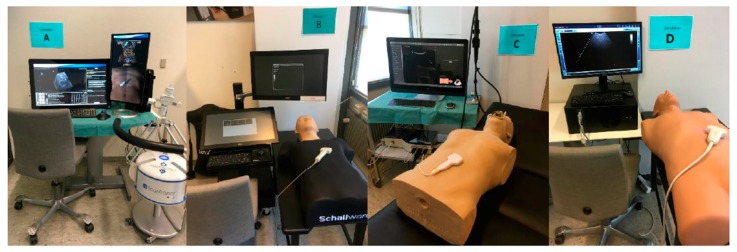
By searching the internet, five simulation companies were identified as having abdominal ultrasound simulators for diagnostic use. One company declined to participate, and four simulators were assigned a letter in alphabetical order and evaluated: A = ScanTrainer (Intelligent Ultrasound), B = Schallware, C = Simbionix (3D Systems), and D = Vimedix (Figure 1, Table 2).
Figure 1.
Simulators in the Study’s Setting.
Table 2.
The Simulators.
| Simulator | MedaPhor | Schallware | Simbionix (3D Systems) |
CAE Healthcare |
|---|---|---|---|---|
| Study mark | A | B | C | D |
| Version | ScanTrainer TVS & TAS, 2017x |
Ultrasound Simulator Station-128 |
U/S Mentor | CAE Vimedix |
| Primary based | Cardiff, UK Available worldwide |
Berlin, Germany Available worldwide |
Tel Aviv, Israel Available worldwide |
Sarasota, Florida, US Available worldwide |
| Description | A hard drive, two screens, a floor-mounted haptic device, keyboard and mouse with rollerball. One screen displays image, buttons and help features, and the other screen displays the virtual patient and probe | A hard drive, two touch screens, keyboard with a rollerball, probes and a sensor table with a mannequin torso. One screen mimics ultrasound buttons and one shows the scan image | A hard drive, one touch screen with screen divisions, keyboard, probes and a sensor table with a mannequin torso. The split screen displays the scan image on one side, and buttons plus anatomical helping model on the other side | A hard drive, one split-screen, keyboard, mouse, probes and a sensor table with a mannequin torso. The screen displays the scan image, buttons and help features |
| Price | €20,000 to €90,000 | €20,000 to €65,000 | 50,0000 to 100,000 USD | Not disclosed |
| Abdominal cases | About 250 | About 250 | 8 diagnostic and 11 FAST | 10 cases |
| Custom cases | Yes, customers can upload their own scans from patients | Yes, with additional equipment | All cases can be customized for severity and/or presence of pathology | All cases can be customized for severity and/or presence of pathology |
| Source of scan | Real patient CT scans blended with computer data | Real patient ultrasound b-mode scans | Computer generated data | Computer generated data |
| Feedback options | ScanTutor will test user against set metrics. Metrics can be customized. Full diagnostic list for each case | Region of interest (RoI) with the option of turning RoIs into questions/answers. Full diagnostic list for each case | Case severity feature/multiple scenarios pr. case. Skill tasks. Full diagnostic list for each case | Performance assessments with kinematic metrics. Full diagnostic list for each case |
| Dynamic features | Computer animated doppler incl. CFM, PW & CW. Breathing patient | Doppler pre-recorded | Computer animated Doppler Breathing patient |
Computer animated Doppler Breathing patient |
| Other modules available | OBGYN eFAST/FAST Emergency Medicine General Medicine Breast |
Obstetrics/Gynecology Cardiology TEE Pediatric (new born manikin) Irritable Boule Disease Virtual model, adult Heart/lungs animated Virtual fetus model |
Basic sonography skills Obstetrics/Gynecology Fetal Neurosonography + Echo Cardiology TEE/Echo eFAST/RUSH Emergency Medicine Lung |
Obstetrics/Gynecology Cardiology TEE FAST/eFAST Emergency Medicine |
Simulator information, obtained from intelligentultrasoundsimulation.com, schallware.de, simbionix.com, and cae.com.
All participants were given a short, standardized introduction to each simulator, including identification of gain, debt and focus buttons, feedback options, and probe handling. Each simulator was presented with two cases: a patient with a hyperechoic liver tumor and a patient with free fluid visible in the splenorenal space. Participants were not presented with the more detailed information on each simulator, e.g., price, number of cases, or other available modules. The participants evaluated the simulators in a randomized order to minimize the risk of bias.
Each participant had a maximum of three minutes to view each case, and, after completing both cases on each simulator, a standardized feedback sheet was filled out for that particular simulator. The feedback sheets were identical for all simulators, and participants were asked to evaluate three areas of educational value: fidelity, usability, and overall satisfaction respectively, on a five-point Likert’s scale, as shown in Table 3. After all four simulators were individually evaluated, an overall questionnaire was filled out ranking the simulators from most to least favorable in nine different categories. Free text comments were possible on all questionnaires and all comments are included in the results.
Table 3.
Comparative Questionnaires.
| Overall Ranking | MedaPhor | Schallware | Simbionix | ViMedix |
|---|---|---|---|---|
| Overall Educational value |

|

|

|

|
| Residents/Experienced |

|
|

|
|
| Resembles real scanning on image |

|

|

|

|
| Residents/Experienced.tif |
|
|

|

|
| Resembles real scanning on probe handling |

|

|

|

|
| Residents/Experienced |
|
|
|
|
| Resembles real scanning knobology |

|

|

|

|
| Residents/Experienced |
|
|
|
|
| intuitive Use |

|

|

|

|
| Residents/Experienced.tif |
|
|
|
|
| Case description. |

|

|

|

|
| Residents/Experienced |
|
|
|
|
| Usable hints |

|

|

|

|
| Residents/Experienced |
|
|
|

|
| Useful Feedback |

|

|

|

|
| Residents/Experienced |

|
|
|
|
| Overall feel |

|

|

|

|
| Residents/Experienced |
|
|
|

|
Overall ranking with first, second, third, and fourth place, represented by green, yellow, orange, and red smileys, respectively. The collective ranking is shown (large smiley) with the ranking divided by groups underneath (small smileys). If ranking scores are identical, two simulators share the respective placing, e.g., two simulators share first place in feedback, and no second placing is listed.
The means of scores for the overall questionnaires were compared for each question, and the first, second, third, and fourth places were represented by green, orange, yellow, or red markers respectably, as seen in Table 3.
The mean scores for the individual and overall questionnaires were compared between the experienced radiologists and the residents to explore potential different perceptions between experts and trainees.
3. Results
A total of 15 participants completed the simulator evaluation: eight experienced radiologists and seven radiological residents.
Combined overall ranking was most favorable for Schallware (simulator B) in seven of the nine ranked areas (resembles real scanning images, probe handling, knobology, case description, hints, and overall feel). The experienced radiologists gave the same simulator best ranking in all categories, while the residents gave it best ranking in two categories (resembles real scans and knobology) and worst in one (probe handling). Best ranking from the residents was given to 3D systems (simulator C) in six of the nine categories (educational value, probe handling, intuitive use, hints, feedback, and overall feel), while one worst rankings was given by the experienced radiologists (resembles real scans). Intelligent Ultrasound (simulator A) was ranked second best in two categories (resembles real scans and case description) in the combined score and best by the residents in case description. The combined ranking put CAE Healthcare (simulator D) as third best in four categories (educational value, resembles real scans, intuitive use, and hints), while residents ranked the same simulator second-best in probe handling and intuitive use.
As seen in Table 4, there were no statistically significant differences between the perceptions of experienced ultrasonographers and trainees in any of the four main topics: educational value, fidelity, usability, and overall satisfaction. As seen in Table 5, the collective scores for educational value were similar between the four simulators, with all simulators scoring higher for educational use for novices than for intermediates and receiving the lowest scores for educating advanced learners. Fidelity scores indicated that Simulator B had the best images. Probe handling was judged positively for all simulators using mannequins (B, C, and D), while knobs were rated high for all simulators not using a mouse (A, B, and C). All simulators scored high for intuitive use and slightly lower for providing useful instructions and feedback. An above-average score was awarded to all simulators for easy use, and for the overall feel for two of the simulators (B and C). Simulator B was specifically recommended for radiological departments, and no simulators were considered non-recommendable, as seen in Table 5.
Table 4.
Comparing Mean Scores by Groups.
| Comparing Mean Score by Groups | Radiological Residents | Radiologists | P Value |
|---|---|---|---|
| Simulator A | |||
| Educational Value (SD) | 3.1 (1.2) | 2.9 (1.2) | >0.05 |
| Fidelity (SD) | 2.9 (0.9) | 3.3 (1.3) | >0.05 |
| Usability (SD) | 3.1 (0.9) | 3.5 (1.3) | >0.05 |
| Overall Satisfaction (SD) | 2.9 (1.4) | 2.9 (1.6) | >0.05 |
| Simulator B | |||
| Educational Value (SD) | 4.0 (0.6) | 3.8 (0.8) | >0.05 |
| Fidelity (SD) | 3.8 (0.8) | 4.1 (0.5) | >0.05 |
| Usability (SD) | 4.1 (0.8) | 3.9 (0.9) | >0.05 |
| Overall Satisfaction (SD) | 3.8 (1.0) | 3.9 (0.7) | >0.05 |
| Simulator C | |||
| Educational Value (SD) | 3.4 (1.3) | 1.3 (1.0) | >0.05 |
| Fidelity (SD) | 3.2 (0.8) | 3.2 (0.9) | >0.05 |
| Usability (SD) | 3.8 (0.7) | 4.0 (0.7) | >0.05 |
| Overall Satisfaction (SD) | 3.8 (1.0) | 3.3 (0.9) | >0.05 |
| Simulator D | |||
| Educational Value (SD) | 3.2 (1.1) | 2.9 (1.0) | >0.05 |
| Fidelity (SD) | 2.6 (0.7) | 3.0 (1.1) | >0.05 |
| Usability (SD) | 3.5 (0.5) | 3.2 (1.5) | >0.05 |
| Overall Satisfaction (SD) | 3.2 (1.3) | 3.0 (1.2) | >0.05 |
Means for both groups combined on the individual questionnaires. The values refer to the Likert’s scale of 1 (least favorable answer) to 5 (most favorable answer).
Table 5.
Comparing Means for All Scores Combined.
| Comparing Means Collective Score, Individual Questionnaires |
Simulator A MedaPhor |
Simulator B Schallware |
Simulator C Simbionix |
Simulator D ViMedix |
|---|---|---|---|---|
| Educational Value | ||||
| Benefits for novices | 3.8 (1.2) | 4.7 (0.5) | 4.4 (0.7) | 4.2 (0.9) |
| Benefits for intermediates | 3.1 (1.5) | 4.3 (1.0) | 3.3 (1.6) | 2.9 (1.5) |
| Benefits for advanced | 2.1 (1.1) | 2.7 (1.2) | 2.2 (1.3) | 2.0 (1.1) |
| Fidelity | ||||
| Scans resemble real life images | 3.5 (1.2) | 4.8 (0.4) | 2.5 (1.2) | 2.5 (1.2) |
| Probe resemble real life use | 2.5 (1.5) | 3.7 (1.1) | 4.0 (1.2) | 3.9 (1.0) |
| Knobs resemble real life use | 3.1 (1.6) | 3.5 (1.3) | 3.2 (1.4) | 2.1 (1.2) |
| Usability | ||||
| Intuitive use | 3.7 (1.3) | 4.4 (0.9) | 4.5 (0.6) | 4.2 (1.3) |
| Useful instructions | 3.1 (1.2) | 3.9 (1.1) | 3.9 (0.9) | 3.1 (1.4) |
| Useful feedback | 3.1 (1.1) | 3.7 (1.0) | 3.3 (1.1) | 2.7 (1.2) |
| Overall Satisfaction | ||||
| Easy to use | 3.3 (1.5) | 4.3 (0.9) | 4.5 (0.6) | 4.1 (1.5) |
| Overall feel | 2.9 (1.6) | 3.7 (1.0) | 3.7 (1.2) | 3.0 (1.5) |
| Recommend it to department | 2.4 (1.4) | 3.6 (1.1) | 2.6 (1.5) | 2.3 (1.3) |
Means compared using collective scores for all participants from the individual simulator questionnaires. The values refer to the Likert’s scale of 1 (least favorable answer) to 5 (most favorable answer).
The most commented-on item with eight mentions for all simulators was the wish for keyboard/knobs resembling a clinical ultrasound machine, as none of the simulators had turning or click buttons, as seen on most conventional scanners. Simulator A was thought to have distorted images by one reviewer, and another had trouble without a physical torso to scan on. Two participants found the lack of full body scans for all cases problematic for simulator B, while two participants commented that the scans were highly realistic. Simulator C was thought to have unrealistic images by four participants, and three found the anatomical markings on the image very helpful and learner-friendly. For simulator D, the images were also found to be unrealistic by three participants; one commented that the depth was too automated, two thought it highly suitable for beginners, and one resident simply “loved it”.
Overall comments stated that the simulated images were generally easier to obtain than real-life images and novices therefore could get a head start before scanning on patients. The use of mannequins was generally favored. The feel of the shirt-covered mannequin for simulator B was positively commented on by two participants as being close to the feeling of a probe on real skin with scanning gel, and one participant preferred the feel of simulator D’s mannequin. Two participants wished for the images from simulator B with the anatomical help markers of simulator C or D.
4. Discussion
This study compared four virtual-reality abdominal ultrasound simulators for diagnostic training in radiology. One simulator (B) was positively rated as recommendable, and none of the simulators were rated as non-recommendable.
Simulation training is being increasingly implemented in the curriculum for specialized training of physicians, and ultrasound training has a high-ranking placement in the national needs assessment for radiology in Denmark [1,6].
All simulators can be used to provide basic skills training outside the clinic without burdening the patients, as well as provide a standardized and uniform training platform in a safe environment [7]. All simulators in this study have been used for educational development, and some have been used to produce training set ups and tests with validity evidence. Training on the CAE Vimedix showed improved examination scores on visual skills for 10 medical students after simulation training, and a study with 56 medical students training on the Intelligent Ultrasound supported the use of errors as a training tool for better transfer of skills to the clinical environment [8,9]. A study with 60 medical students also using the Intelligent Ultrasound simulator supported the use of individualized training on simulators to steepen the learning curve for trainees. The same simulator was used to show that performance of FAST (focused assessment with sonography for trauma) scans could be assessed in a non-clinical setting on simulators [10,11]. The Schallware simulator was used for test development for the diagnostic abdominal ultrasound exam using the European curriculum, and training on the simulator prior to clinical training was shown to improve scanning performance on patients [12,13]. The Schallware simulator was also used to establish a valid assessment tool for FAST and shown to provide basic skills for physicians using FAST [14].
The use of simulators could relieve some of the pressure on the clinical patients and supervisors as well as provide a safe and standardized educational environment for trainees [2]. This could provide a more unified knowledge basis of trainees and ensure that all trained personnel have a basic skill level. Optimized learning strategies in an environment with increasing safety and efficiency demands are also possible with the use of simulators [15]. This could include goal setting, continued skill assessments, spacing practice sessions, and more. Finally, physicians’ skill development would be ensured while providing standardized skill assessment and curriculums [16]. The use of simulation training has been shown to be effective for skill development in many medical specialties, e.g., gynecology and respiratory medicine, and a randomized controlled trial from 2015 found simulation training to be more effective than the apprenticeship model [3,17].
All simulators in this study could provide several pathological scans for image recognition training and a broad variety of scans such as FAST, POC (point of care), and TEE (transesophageal echocardiogram).
Limitations
All simulators were evaluated by radiologists who are used to high-end scanning equipment and interpreting a broad array of image details. Therefore, the ranking might not reflect use for training more constricted diagnostic tasks such as FAST or eFAST (extended focused assessment with sonography for trauma). The limited number of participants also calls for care of interpretation and elaboration of the results. As simulators are not the same as real life, care should be taken to find other ways to train the non-simulated areas of diagnostic ultrasound such as doctor-patient communication and pressure sensitivity. However, simulation training in abdominal ultrasound has been shown to elevate the trainee before scanning on patients with possible benefits for patients and supervisors as well as the trainee [18]. The Doppler features of the simulators were not presented due to time restrictions, and are therefore not included in the ranking score. The field of simulation is moving fast, and new simulators are emerging rapidly, e.g., Intelligent Ultrasound launched a mannequin-based simulator shortly after this study ended, and 3D Systems has changed their name from Simbionix to 3D Systems.
5. Conclusions
All simulators were usable for diagnostic abdominal ultrasound, and learning benefits were ranked higher for novices than for more experienced ultrasonographers. Hopefully, this study can assist decision makers in ultrasound training programs to choose the simulator that optimally fits their local needs and budget.
Acknowledgments
The authors would like to thank all involved simulation companies for leading their simulators without further attachments.
Author Contributions
Conceptualization, M.L.Ø., L.K., M.B.N., and K.R.N.; Data curation, M.L.Ø., N.K., and K.R.N.; Formal analysis, M.L.Ø. and L.K.; Funding acquisition, M.L.Ø., M.B.N., and K.R.N.; Investigation, M.L.Ø. and K.R.N.; Methodology, M.L.Ø., L.K. and K.R.N.; Project administration, M.L.Ø. and K.R.N.; Resources, E.A.-B.; Software, M.L.Ø. and K.R.N.; Supervision, L.K., M.B.N., and K.R.N.; Validation, M.L.Ø., L.K., N.K., E.A.-B., M.B.N., and K.R.N.; Visualization, M.L.Ø.; Writing—original draft, M.L.Ø.; Writing—review and editing, M.L.Ø., L.K., N.K., E.A.-B., M.B.N., and K.R.N.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- 1.Nayahangan L.J., Nielsen K.R., Albrecht-Beste E., Bachmann Nielsen M., Paltved C., Lindorff-Larsen K.G., Nielsen B.U., Konge L. Determining procedures for simulation-based training in radiology: A nationwide needs assessment. Eur. Radiol. 2018;28:2319. doi: 10.1007/s00330-017-5244-7. [DOI] [PubMed] [Google Scholar]
- 2.Konge L., Albrecht-Beste E., Nielsen M.B. Virtual-reality simulation-based training in ultrasound. Ultraschall. Med. 2014;35:95–97. doi: 10.1055/s-0034-1366191. [DOI] [PubMed] [Google Scholar]
- 3.Konge L., Clementsen P.F., Ringsted C., Minddal V., Larsen K.R., Annema J.T. Simulator training for endobronchial ultrasound: a randomised controlled trial. Eur. Respir. J. 2015;46:2352. doi: 10.1183/13993003.02352-2015. [DOI] [PubMed] [Google Scholar]
- 4.Østergaard M.L., Ewertsen C., Konge L., Albrecht-Beste E., Nielsen M.B. Simulation-Based Abdominal Ultrasound Training—A Systematic Review. Ultraschall. Med. 2016;37:253–261. doi: 10.1055/s-0042-100452. [DOI] [PubMed] [Google Scholar]
- 5.Konge L., Ringsted C., Bjerrum F., Tolsgaard M.G., Bitsch M., Sørensen J.L., Schroeder T.V. The Simulation Centre at Rigshospitalet, Copenhagen, Denmark. J. Surg. Educ. 2015;72:362–365. doi: 10.1016/j.jsurg.2014.11.012. [DOI] [PubMed] [Google Scholar]
- 6.Moore C.L., Copel J.A. Point-of-care ultrasonography. N. Engl. J. Med. 2011;364:749–757. doi: 10.1056/NEJMra0909487. [DOI] [PubMed] [Google Scholar]
- 7.Motola I., Devine L.A., Chung H.S., Sullivan J.E., Issenberg S.B. Simulation in healthcare education: A best evidence practical guide. AMEE Guide No. 82. Med. Teach. 2013;35:1511–1530. doi: 10.3109/0142159X.2013.818632. [DOI] [PubMed] [Google Scholar]
- 8.Le C.-K., Lewis J., Steinmetz P., Dyachenko A., Oleskevich S. The Use of Ultrasound Simulators to Strengthen Scanning Skills in Medical Students: A Randomized Controlled Trial. J. Ultrasound. Med. 2018 doi: 10.1002/jum.14805. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 9.Dyre L., Tabor A., Ringsted C., Tolsgaard M.G. Imperfect practice makes perfect: Error management training improves transfer of learning. Med. Educ. 2017;51:196–206. doi: 10.1111/medu.13208. [DOI] [PubMed] [Google Scholar]
- 10.Taksøe-Vester C., Dreisler E., Andreasen L.A., Dyre L., Ringsted C., Tabor A., Tolsgaard M.G. Up or down? A randomized trial comparing image orientations during transvaginal ultrasound training. Acta Obstet. Gynecol. Scand. 2018;97:1455–1462. doi: 10.1111/aogs.13444. [DOI] [PubMed] [Google Scholar]
- 11.Jensen J.K., Dyre L., Jørgensen M.E., Andreasen L.A., Tolsgaard M.G. Collecting Validity Evidence for Simulation-Based Assessment of Point-of-Care Ultrasound Skills. J. Ultrasound. Med. Off. 2017;36:2475–2483. doi: 10.1002/jum.14292. [DOI] [PubMed] [Google Scholar]
- 12.Østergaard M.L., Nielsen K.R., Albrecht-Beste E., Konge L., Nielsen M.B. Development of a reliable simulation-based test for diagnostic abdominal ultrasound with a pass/fail standard usable for mastery learning. Eur. Radiol. 2018;28:51–57. doi: 10.1007/s00330-017-4913-x. [DOI] [PubMed] [Google Scholar]
- 13.European Society of Radiology The Minimum Training Recommendations for the Practice of Medical Ultrasound. Ultraschall. Med. 2006;27:79–105. doi: 10.1055/s-2006-933605. [DOI] [PubMed] [Google Scholar]
- 14.Russel L., Østergaard M.L., Nielsen M.B., Konge L., Nielsen K.R. Standardized assessment of competence in Focused Assessment with Sonography for Trauma. Acta Anaesthesiol. Scand. 2018 doi: 10.1111/aas.13141. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 15.Ericsson K.A. Acquisition and maintenance of medical expertice: A perspective from the expert-performance approach with delibrate practice. Acad. Med. J. 2015;90:1471–1486. doi: 10.1097/ACM.0000000000000939. [DOI] [PubMed] [Google Scholar]
- 16.McGaghie W.C. Mastery Learning: It Is Time for Medical Education to Join the 21st Century. Acad. Med. 2015;90:1438–1441. doi: 10.1097/ACM.0000000000000911. [DOI] [PubMed] [Google Scholar]
- 17.Tolsgaard M.G., Ringsted C., Rosthøj S., Nørgaard L., Møller L., Freiesleben N.L.C., Dyre L., Tabor A. The Effects of Simulation-based Transvaginal Ultrasound Training on Quality and Efficiency of Care: A Multicenter Single-blind Randomized Trial. Ann. Surg. 2017;265:630–637. doi: 10.1097/SLA.0000000000001656. [DOI] [PubMed] [Google Scholar]
- 18.Østergaard M.L., Rue Nielsen K., Albrecht-Beste E., Kjær Ersbøll A., Konge L., Bachmann Nielsen M. Simulator training improves ultrasound scanning performance on patients: A randomized controlled trial. Eur. Radiol. 2019 doi: 10.1007/s00330-018-5923-z. Epub ahead of print. [DOI] [PubMed] [Google Scholar]