Abstract
One of the main characteristics of carcinogenesis relies on genetic alterations in DNA and epigenetic changes in histone and non-histone proteins. At the chromatin level, gene expression is tightly controlled by DNA methyl transferases, histone acetyltransferases (HATs), histone deacetylases (HDACs), and acetyl-binding proteins. In particular, the expression level and function of several tumor suppressor genes, or oncogenes such as c-Myc, p53 or TRAIL, have been found to be regulated by acetylation. For example, HATs are a group of enzymes, which are responsible for the acetylation of histone proteins, resulting in chromatin relaxation and transcriptional activation, whereas HDACs by deacetylating histones lead to chromatin compaction and the subsequent transcriptional repression of tumor suppressor genes. Direct acetylation of suppressor genes or oncogenes can affect their stability or function. Histone deacetylase inhibitors (HDACi) have thus been developed as a promising therapeutic target in oncology. While these inhibitors display anticancer properties in preclinical models, and despite the fact that some of them have been approved by the FDA, HDACi still have limited therapeutic efficacy in clinical terms. Nonetheless, combined with a wide range of structurally and functionally diverse chemical compounds or immune therapies, HDACi have been reported to work in synergy to induce tumor regression. In this review, the role of HDACs in cancer etiology and recent advances in the development of HDACi will be presented and put into perspective as potential drugs synergizing with TRAIL’s pro-apoptotic potential.
Keywords: histone deacetylase (HDAC), histone deacetylase inhibitors (HDACIs), chromatin remodeling, cancer, tumor necrosis factor (TNF), TRAIL, methylation, silencing
1. Introduction
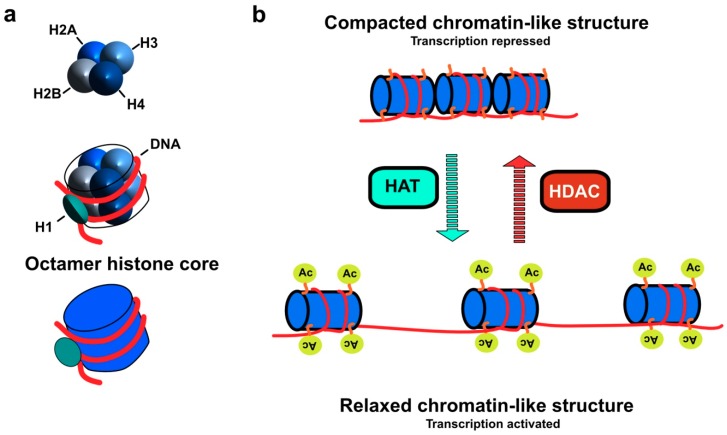
Cancer is considered as the leading cause of death worldwide. It has been reported to occur as a result of epigenetic modifications, including amplifications, translocations, deletions, and point mutations [1,2]. These epigenetic modifications are linked to abnormal cellular transformation, characterized, among other things, by uncontrolled proliferation and resistance to cell death, forming a lump or what is called a tumor. In addition, DNA methylation and the post-translational modification of proteins such as histones, including acetylation and methylation, are also believed to play a central role in tumorigenesis by modifying the structure of chromatin and the subsequent negative regulation of tumor suppressor genes or oncogenes without any change in the DNA sequence [3]. The main function of histones is the packaging of genomic DNA inside the nucleus. Histone proteins are rich with positively charged amino acids, lysine and arginine, which makes their overall structure positive. In this context, histones can interact with the negatively charged phosphate group of DNA. These proteins are composed of several types of histone including H1, H2A, H2B, H3, and H4. H2A, H2B, H3, and H4 represent the main histone core, while H1 is known as a linker histone [4]. The core multimeric protein is an octamer molecule, mainly consisting of two copies of each histone type (2H2A, 2H2B, 2H3, and 2H4) forming a globular structure called the nucleosome (Figure 1a). Each nucleosome is wrapped by approx. 146 bp of DNA and separated by 50 base pair (bp) linker DNA. The N-terminal domain of histones possesses an unstructured part that has also been suggested to be involved in the epigenetic modification of chromatin. Considering the process by which histone proteins are post-translationally modified, chromatin adopts various structural conformations that regulate both the repression and activation of gene transcription (Figure 1b and [5]).
Figure 1.
Illustration of histone core composition and impact of chromatin relaxation or compaction by histone acetyltransferases (HAT) or histone deacetylases (HDAC) on gene expression (a) Histone protein consists of five main types H1, H2A, H2B, H3, and H4. Two copies of each histone type (2H2A, 2H2B, 2H3, and 2H4) constitute the octamer histone core (nucleosome), wrapped by approx. 146 bp of DNA. H1 is known as linker histone that is associated to linker DNA between each nucleosome. (b) Epigenetic modification of histone proteins by HDAC/HAT. HAT stimulates transcriptional activation of the tumor suppressor genes via acetylation of N-ε-lysine residues of histone results in more relaxed chromatin, which facilitates the accessibility of target gene promoter to transcription factors. Conversely, HDAC induces transcriptional repression of tumor suppressor genes by deacetylating N-ε-lysine residues of histone in which the chromatin adopts compacted structure conformation, thus hiding the target gene promoter from the transcription factors.
Acetylation/deacetylation of the N-ε-lysine residues of histones is regulated by a group of acetylating and deacetylating enzymes. Histone acetyltransferases (HATs) transfer an acetyl group from an acetyl-coA molecule to the N-ε-lysine residues of histone, resulting in the neutralization of its positive charge and in the activation of gene transcription. In contrast, histone deacetylases (HDACs) remove the acetyl group from the N-ε-lysine residues of histone providing a tight interaction between DNA and histone protein (Figure 1b). In this case, the chromatin exhibits more compacted conformation [6]. Excessive histone deacetylation induced by HDAC can have a significant impact on the pathology of cancer via the silencing of tumor suppressor genes, including p53. For instance, the more the chromatin is condensed, the fewer promoters of these target genes are accessible to transcription factors, whereas when cells exhibit higher HAT activity, chromatin relaxation is associated with an increased transcriptional activation of tumor suppressor genes [7,8]. Given that dysregulation of HDAC and/or HAT function has been associated to cancer etiology, intensive research is being conducted worldwide to develop HDAC inhibitors. In this review the role of HDAC and epigenetic modifications in cancer will be discussed with a special emphasis on the potential interest of HDAC inhibitors for immunotherapies based on TRAIL or TRAIL-derivatives.
2. Classification and Localization of HDACs
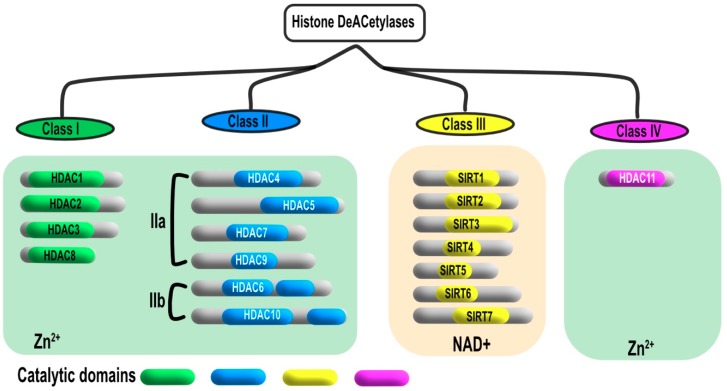
HDAC can be classified into four groups according to their homology with yeast function and sequence (Figure 2). Class I histone deacetylases contains four proteins ranging from 42 to 45 kDa; known respectively as HDAC1, 2, 3 and 8, which are mostly localized in the nucleus. Class II HDACs are larger in size (120-130 kDa) and includes HDAC4, 5, 6, 7, 9, and 10. Class II histone deacetylases have been further subdivided in two groups, Class 2a that encompasses HDAC4, 5, 7, and 9, which display high sequence homology. HDAC6 and 10 have been grouped in class 2b due to the presence of an extra catalytic domain. Class II HDAC members are mainly localized in the cytoplasm, however they shuttle from the cytoplasm to the nucleus when phosphorylated. Class III histone deacetylases are also known as sirtuins due to their homology with the yeast silent information regulator 2 (Sir2) gene and to their requirement of NAD+ for their enzymatic activity. Class IV is considered as a category in its own, with HDAC-11 as a single member. Similar to class I and II members, HDAC11 is a metalloenzyme that contains Zn+2 ion in its binding pocket [9,10,11,12,13,14].
Figure 2.
Different classes of HDACs. Four different classes of HDACs were identified in mammalian cell based on their sequence homology and structure similarity to the corresponding yeast HDACs. Class I is homologous to the yeast reduced potassium dependency 3 (RPD3) and includes HDAC1, 2, 3, 8. Class II is homologous to yeast Hda1 and divided into two sub classes, class IIa HDAC4, 5, 7, 9 and class IIb HDAC6, 10. Class III is also known as sirtuins that contain SIRT1-7. Class IV has its own character and shows structural similarity to classes I and II.
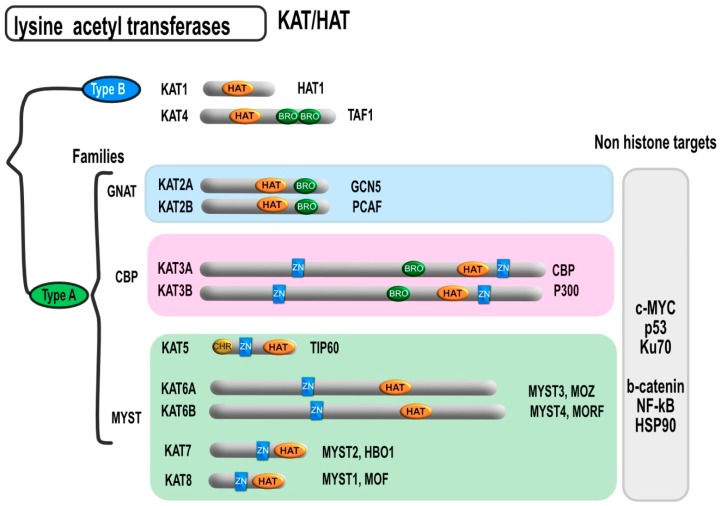
Besides histones, HDACs can also deacetylate non-histone proteins, some of which are transcription factors such as E2F1, c-Jun, GATA1, TFIIE, TFIIF, p65 (RelA), transcription repressors like Yin Yang 1, Mad/Max, the tumor suppressor gene p53 [12,15,16], and the oncogene c-Myc [17] to cite a few. Other non-histone proteins are frequently regulated by HDACs such as the steroid hormone receptor binding protein, the cytoskeletal protein (α-tubulin), nuclear transport (importin-α7), DNA helicase (WRN), signal transduction (β-catenin), and the heat shock protein (Hsp90) [18,19,20,21]. On the other hand, like deacetylation, hyperacetylation of given proteins can change their function. Likewise, hyperacetylation of p53 was shown to increase its stability and subsequent induction of apoptotic cell death [18,20,21,22]. Moreover, acetylation of Hsp90 leads to the activation of the proteosomal degradation of the receptor tyrosine-protein kinase (ErbB2) oncoprotein [23]. Non-histone protein acetylation can also be induced by a large majority of histone acetyl transferases (HATs). Thus, HATs have recently been renamed as lysine acetyl transferases (KATs). This family of enzyme has been divided into two main groups (Figure 3). Type A is the larger group and includes several sub-families. The members of type A HATs are mostly localized in the nucleus and classified into families according to their sequence homology. The Gcn5-related N-acetyltransferases (GNAT) family, includes both KAT2A and KAT2B. The p300/CBP family consists of KAT3A and 3B.
Figure 3.
Different HAT/KAT subtypes and their domains. Besides the lysine acetyltransferase domain, KAT can harbor a bromodomain that can facilitate interactions with modified histones. The MYST and CBP families also contain a zinc-binding domain which facilitates DNA binding. Some MYST family HATs contain in addition an N-terminal chromodomain, which binds to methylated lysine residues. HAT = catalytic histone acetyltransferase domain, BRO = bromodomain, CHR = chromodomain, ZN = zinc-binding domain.
The MYST family represents the largest HAT family, which includes KAT5, KAT6A, KAT6B, KAT7, and KAT8. Type B HATs are abundant in the cytoplasm such as KAT1 and KAT4. The members of both CBP/P300 and GNAT families contain a bromodomain (BD) that mainly binds to the acetylated lysine rich region of histone proteins. Moreover, the members of CBP/P300 and MYST family members possess a cysteine rich, zinc-binding domain which facilitates binding to acetyl group. Some MYST family HATs contain in addition an N-terminal chromodomain, which binds to methylated lysine residues [24]. HATs can also acetylate non-histone proteins that could influence their promotor activities and specificities, such as β-catenin, Myc proto-oncogene protein (C-MYC), tumor suppressor protein p53, and the nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) [25,26,27].
3. Molecular Mechanism of HDAC Action
HDACs are involved in the epigenetic modification of histone proteins via removal of acetyl group of N-ε-lysine residues of histone. Considering that HDACs induce hypoacetylation, the distance between the nucleosome molecule and chromatin DNA is markedly decreased and hence the histone adopts a compacted structure of wrapped DNA (Figure 1). Chromatin compaction impedes the access of transcription factors to the promoter of the target genes present within the area, including tumor suppressor genes, resulting in uncontrolled cell proliferation and cancer development. The catalytic domain of HDAC consists of approx. 390 amino acid residues (Figure 2), which comprises a set of conserved amino acids. The substrate binding site of HDAC adopts a curved tunnel with a wider bottom, similar to Zn+2-binding proteins like thermolysin and carboxypeptidase [28,29,30]. The structural environment of the HDAC substrate binding site encompasses two adjacent histidine residues (His142 & His 143), two aspartic acid residues (Asp176 & Asp183), and one tyrosine residue (Tyr306). Deacetylation process occurs through a charge-relay system in the presence of Zn+2 ions. The carbonyl group of the acetyl lysine residues is polarized for nucleophilic attack as a result of coordination with Zn+2 bonded water molecules and hydrogen bonding with Tyr306 [31,32]. Zn+2 coordinated residues along with substrate binding constitute a tetrahedral structure, mainly consisting of five coordinates including water molecules. This step was reported to be the rate limiting step in the hydrolysis of the acetyl group of lysine residue by HDAC8 [30]. Furthermore, activation of the nucleophile is mediated by the general base character of the adjacent His142 and His134 residues in the substrate binding site, which are influenced by hydrogen bonding with Asp176 and Asp183, respectively [33]. H143 residue is localized in a close vicinity to the leaving amino group of acetyl lysine. Therefore, it acts as a proton donor and hence mediates the separation of the amino group as a result of tetrahedral structural conformation [34].
4. Physiological Function of HDAC
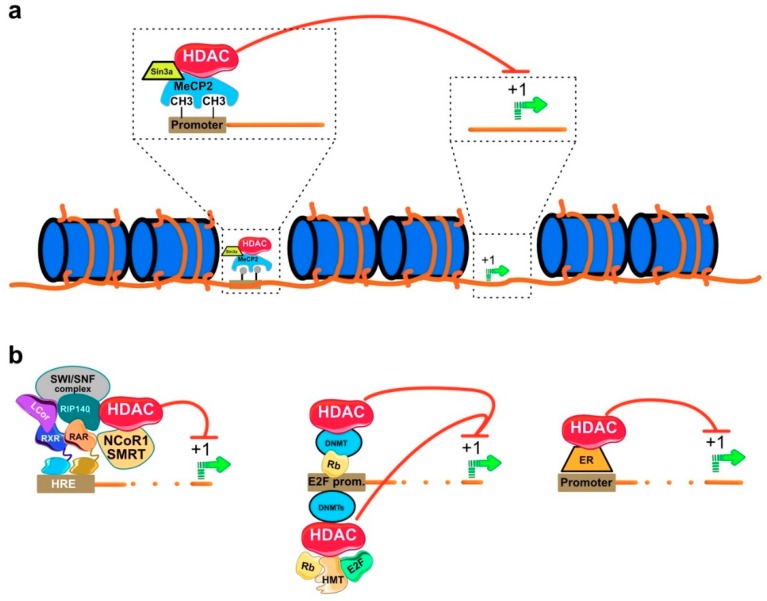
HDACs are recruited to the gene promoter in the form of multiprotein complex (see examples Figure 4 and [35]). The interacting protein partners of HDACs are mostly acting as transcriptional coregulators. They include proteins such as mSin3 interacting domain of the paired amphipathic helix protein (sin3a), the nuclear receptor co-repressor 1 (N-CoR), and the nuclear receptor co-repressor 2/ silencing mediator for retinoid and thyroid hormone receptors (SMRT). The binding of a specific DNA sequence by transcriptional regulatory proteins along with HDACs can also occur with the help of epigenetic modifying proteins such as methyl binding proteins (MBDs), DNA methyl transferases (DNMTs), and histone methyl transferases (HMTs). For example, the MBDs, methyl-CpG binding domain (MeCP2), is believed to recruit HDAC to methylated promoters resulting in transcriptional repression (Figure 4a and [36]). The receptor interacting protein 140 (RIP140) is a negative co-regulator, which binding to HDAC1 and HDAC3 represses expression of nuclear receptors (Figure 4b and [37]). Hyperacetylation of histones can also occur independently of the loss of HDAC activity. For example, knockout of DNMT1 revealed a significant increase of the acetylated histone H3 and a decrease in the level of the methylated form. The decreased level of methylated H3 was mainly attributed to the dissociation of HDAC-DMNT1 complex leading to hyperacetylation of H3 [38].
Figure 4.
Illustrating the physiological function of HDAC. HDAC can be recruited to gene promoter associated with coregulatory proteins including (a) methyl binding protein (MeCP2), (b) DNA methyl transferases (DMNT), Estrogen receptor (ER), and transcription factors Rb and E2F, which are responsible for gene silencing and subsequent chromatin remodeling [37].
Moreover, HDACs were reported to regulate neuronal differentiation via direct interaction with the N-terminal domain of DMNT3b. Inhibition of HDACs in pheochromocytoma cell line (PC12) prevented cell differentiation stimulated by nerve growth factor (Figure 4b). The case was reversed when DMNT3b was overexpressed in the same cell line in which a significant cell differentiation was detected [39]. HDAC can also interact with transcription factors and nuclear receptors other than MBDs. The interaction of HDAC with the cell cycle regulator retinoblastoma protein (Rb) leads to uncontrolled cell progression [40]. Rb is a family of tumor suppressor proteins involved in the inhibition of cell growth via the suppression of cell cycle progression. When a cell is ready to divide, Rb is inactivated by phosphorylation allowing cell cycle progression. Defects in Rb proteins were found to play a central role in the initiation of cancer [41]. Transcription factor E2F belongs to a protein family that is responsible for cell cycle control and the synthesis of DNA in eukaryotes. It consists of nine members, of which three (E2F1, E2F2, and E2F3a) are transcription activators and the remaining six (E2F3b, E2F4, E2F5, E2F6, E2F7, and E2F8) are cell cycle repressors. The gene promoters of E2F transcription repressors was suggested to be inactivated by HDAC-Rb complex in transformed cells [39,42,43]. It has been reported that the interaction between HDAC and Rb promotes uncontrolled cellular proliferation and the initiation of cancer. Trichostatin A (TSA), a classical HDAC inhibitor (HDACI) is able to prevent HDAC-Rb complex assembly hence repressing the transcription of genes essential for cell cycle progression [44].
In addition, HDAC has the ability to bind nuclear receptors, thus mediating the regulation of gene expression. For example, estrogen receptors (ERs) are nuclear receptors involved in the transcriptional regulation of genes that determine the function of both breast and ovary. For instance, the nuclear receptor ER-α is activated by its ligand 17β-estradiol, which is implicated in the transcriptional regulation of estrogen responsive genes in different cell types. Such an interaction was found to mediate the normal development of breasts as well as progression of breast cancer. The downregulation of ER-α expression in the breast epithelium is critical for the initiation of breast cancer. The reason behind was mainly assigned to the in vivo interaction between HDAC1 and ER-α in its promoter region suppressing its transcriptional activity (Figure 4b). This interaction can be reversed by the availability of estrogens and also in the breast cancer MCF7 cell line with the HDAC inhibitor TSA, resulting in the upregulation of ER-α on both mRNA and protein levels [45]. Macaluso and coworkers [46] demonstrated that the transcriptional silencing of ER-α is mediated by two multiprotein repression complexes (1) pRb2/p130-E2F4/5-HDAC1-histone methyl transferase (SUV39H1)-p300 and (2) pRb2/p130-E2F4/5-HDAC1-DNMT1-SUV-39H1 that are recruited to the ER-α promoter of breast cancer cells.
5. Role of HDAC in Cancer
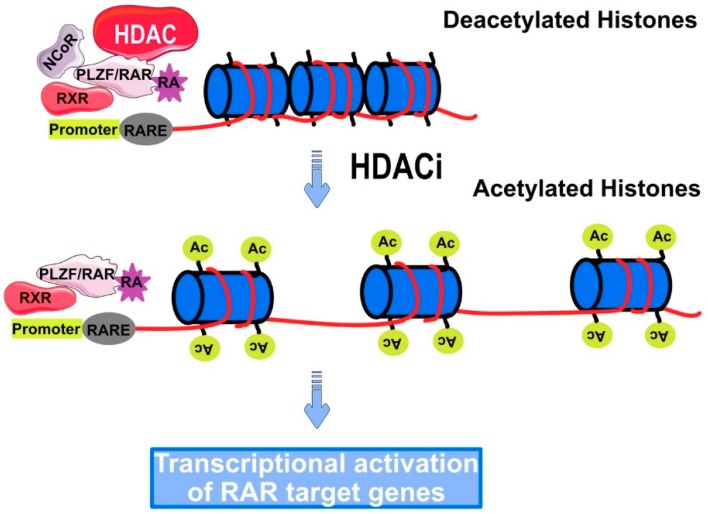
Strong evidence suggests that defects in the DNA methylation as well as defects in the post-translational modification of histones are directly causative of cancer initiation in humans. Indeed, the loss of acetylated lysine residue (Lys16) and trimethylated Lys20 of histone H4 is considered as an initial event for the development of cancer [47]. Furthermore, the decreased rate of histone acetylation in gastrointestinal tumors was also found to be associated with invasion and metastasis [48]. The mechanism by which HDACs deacetylate lysine residues of histone proteins still remains enigmatic. However, hypoacetylation due to decreased levels of HATs was mainly attributed to either mutations or chromosomal translocation such as leukemias. This was found to be accompanied by increasing in HDAC activity [49]. The most available data regarding the mechanism of HDAC in cancer is restricted in the formation of HDAC-fusion protein complex during binding to a specific gene promoter. These fusion proteins are considered as an end product of chromosomal translocation in case of hematological malignancies [50]. Acute promyelocytic leukemia (APL) is a subtype of acute myelocytic leukemia (AML), known as the cancer of white blood cells. The genotypic character of APL is represented in the chromosomal translocation between chromosome 15 and 17 including the retinoic receptor-α (RARα). Some fusion proteins like promyelocytic leukemia/retinoic acid receptor (RAR-PML) and retinoic acid receptor promyelocytic leukemia zinc finger protein (RAR-PLZF) are recruited along with HDAC to a specific DNA sequence located in the promoter region (Figure 5) known as retinoic acid-responsive elements (RAREs). Consequently, the expression of genes that are responsible for the normal differentiation and proliferation of myeloid cells is inhibited [51,52].
Figure 5.
Recruitment of HDAC to retinoic acid-responsive elements (RARE) in Promyelocytic leukemia (PML). HDAC forms a multiprotein complex with RAR-PLZF, resulting in the transcriptional repression of retinoic acid receptor (RAR) target gene, responsible for normal differentiation and proliferation of myeloid cells. HDACi can reverse this case by restoring the sensitivity of PML to retinoic acids.
Several studies have reported the overexpression of HDAC in different types of cancer such as HDAC1 in gastric [53], prostate [54], colon [55], and breast [56] cell carcinomas. Overexpression of HDAC2 was also reported in cervical [57], gastric [58], and colorectal cancers [59]. HDAC3 and HDAC6 were found to be overexpressed in colon and breast cancers [54,60]. In this context, overexpression of HDAC can lead to the transcriptional repression of tumor suppressor genes via recruitment of HDAC in the form of multiprotein complex to their specific promoter regions. Cyclin-dependent kinase inhibitor (p21WAF1) is a cell cycle progression inhibitor. Expression of p21WAF1 is significantly influenced by promoter hypoacetylation. Inhibition of HDAC significantly increases the acetylation of p21WAF1 promoter and subsequent inhibition of tumor growth [61].
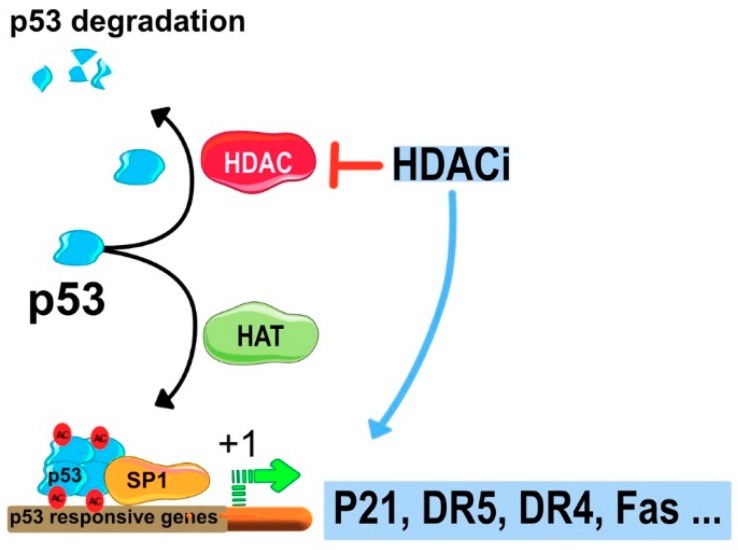
Expression of p21 is also influenced by p53 that competes with HDAC1 to specific promoter region of p21 known as promoter-specific RNA polymerase II transcription factor (Sp1). This results in the release of HDAC1 from Sp1, leading to an increase in the expression of p21 ([62] and Figure 6). Inhibition of HDAC increases the acetylation of p53 and enhances its stability, which subsequently strengthens the interaction with p21 promoter. Moreover, HDAC inhibitors have been described to induce hyperacetylation of sp1 [63] and sp3 [64] and to change the promoter acetylation profile and expression levels of several death receptors involved in the transduction of apoptotic signals (Figure 6). These include the tumor necrosis factor-related apoptosis-inducing ligand (TRAIL) death receptors (DRs) DR4 [65,66,67] and DR5 [66,68,69,70,71], as well as FAS ligand/CD95 ligand (FASL) [72,73], and FAS [74].
Figure 6.
Schematic representation of the molecular mechanism of HDCAIs-induced cell cycle arrest and induction of apoptotic cell death. P21 gene promoter Sp1 can bind HDAC multi protein complex repressing gene transcription. Inhibition of HDAC activates transcription of p21 that stimulates cell cycle arrest. HDACIs can also induce apoptosis via stimulation of tumor necrosis factor (TNF) protein members like TRAIL and CD95.
Class III HDAC/sirtuins are of growing interest in oncology due to their ability to regulate gene expression, apoptosis, stress responses, genome integrity, and cancer metabolism [75,76,77,78,79,80,81,82,83,84]. Lys16 residue of H4 (lys16-H4) and Lys9-H3 were reported to be the substrate of this group of HDACs [85,86]. Dysregulation of their expression levels has been described in cancer cells associated or not with oncogenic or tumor suppressor functions. For example, SIRT1 was found to be highly expressed in human lung cancer [87], prostate cancer [88], and leukemia [89], however its expression is reduced in colon cancer, when compared to normal tissues [90]. Mechanistically, sirtuins such as SIRT1 are able to deacetylate p53 leading to the inhibition of its DNA damage functions [91] or to induce the hypoacetylation of the DNA repair enzyme Ku70, enhancing its non-homologous end joining DNA repair ability [92,93] and allowing the survival of cancer cells [21]. On the contrary, treatment with SIRT1 inhibitors leads to the increased expression of tumor suppressor genes and increased level of the acetylated lys16-H4 and lys9-H3 in both colon and breast cancer cell lines [86].
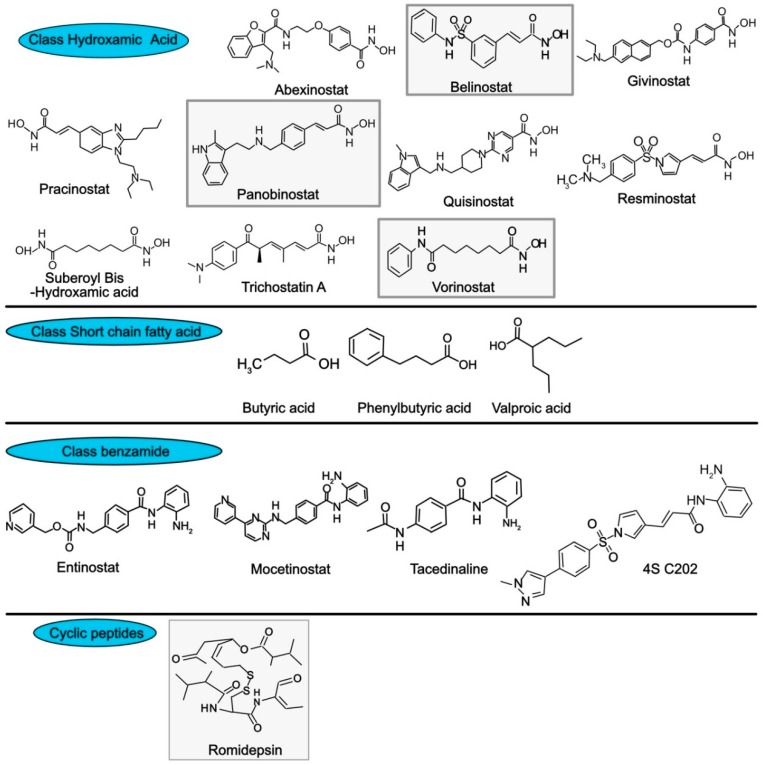
Inhibition of HDAC gained the attention of several research groups in the field of cancer drug discovery, making HDAC a promising drug target for the treatment of cancer [94,95]. HDACIs are suggested to induce apoptosis by inhibiting multiple signaling pathways. The effect of HDACIs is not restricted to histone proteins, these inhibitors can also directly impact non-histone proteins [48,96]. They are categorized into two categories: (1) HDAC isoform-selective inhibitors, which target several types of HDAC, and (2) pan-inhibitors, which act against all type of HDACs [97]. Clinical trials have been conducted for various HDAC inhibitors against different type of tumors. These inhibitors are divided into four different classes based on their chemical structures (Figure 7), which include (I) hydroxamic acids, (II) short chain fatty acids, (III) benzamides, and (IV) cyclic peptides [98]. The group of hydroxamic acid-based HDACIs assessed in clinical trials include abexinostat, belinostat, givinostat, pracinostat, panobinostat, quisinostat, resminostat, and vorinostat [99]. Trichostatin A (TSA) and suberoyl bis hudroxamic acid also belong to the hydroxamic acid group.
Figure 7.
Structure of selected HDAC inhibitors. FDA approved inhibitors are highlighted in the grey boxes.
TSA is a natural HDAC inhibitor that was originally isolated from actinomycete Streptomyces hygroscopicus and is used for its antifugal property. Like belinostat, panobinostat, vorinostat and TSA are able to inhibit all classes of HDACs. However, TSA is solely used in laboratories due to the fact that this pan-HDAC inhibitor displays high toxicity [100]. Valproic acid (VPA), butyric acid and phenylbutyric acid, belong to the HDACi class of short-chain fatty acids (Figure 7). VPA targets class I and IIa HDACs [101], whereas butyric and phenylbutyric acids target HDACs of class I and II [96]. This class of HDAC inhibitors is probably the least potent of the family of HDAC inhibitors. Benzamides, represent another subclass. It includes the class I HDACi’s entinostat, tacedinaline, and 4SC202, as well as mocetinostat a class I and IV HDAC selective inhibitor. The last subgroup of HDAC inhibitor is represented by romidepsin, a class I HDAC inhibitor.
To date, only four compounds have been investigated as HDAC inhibitor and approved by US Food and Drug Administration (FDA) in clinical trials. These compounds, including vorinostat (suberoylanilide hydroxamic acid, SAHA) and Romidepsin (cyclic tetrapeptide) which revealed a promising HDAC inhibition against different type of cancers were approved for the treatment of cutaneous T-cell lymphoma [102,103,104,105]. Belinostate (Class I) was approved for the treatment of peripheral T-cell lymphoma [106]. Panabinostat is a member of the hydroxamic acid group and has recently been tested in clinical trials and approved for the treatment of multiple myeloma [96]. Other inhibitors are under development.
Class III HDAC inhibitors, which selectively target the NAD+-containing HDACs sirtuins have mostly been implemented in the treatment of various clinical diseases like cardiovascular disorders, aging, neurodegenerative disorders, and cancer [107]; however, recent studies have reported the investigation of sirtuins, particularly sirtinol, cambinol, and EX-527 as therapeutic agents for cancer [108,109]. It should be noted though that cambinol was found to display stronger affinity to neutral sphingomyelinase-2 than class III HDACs [110], questioning its specificity for sirtuins.
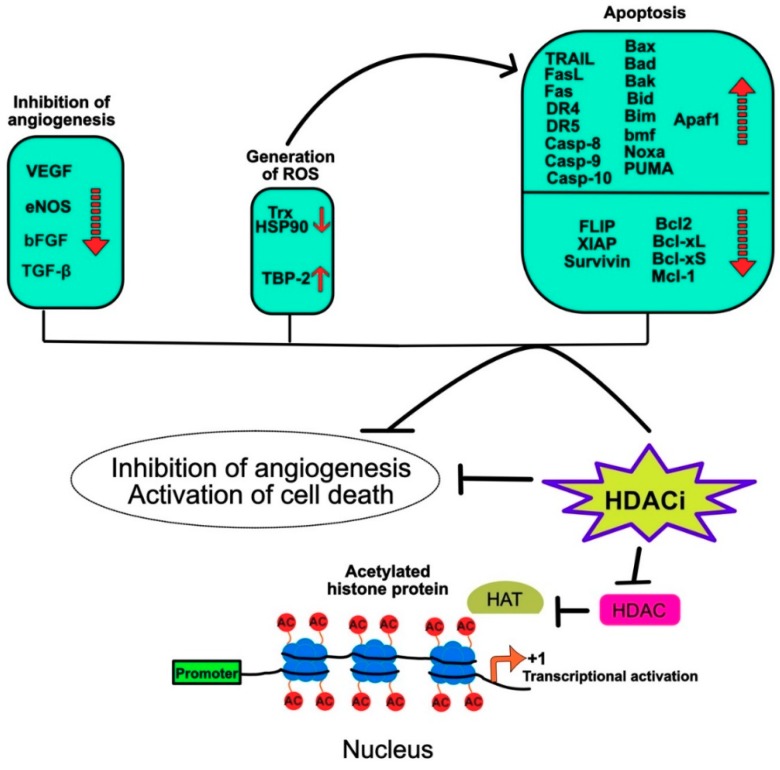
The anticancer effect of HDAC inhibitors have been found to involve a number of molecular events including inhibition of angiogenesis, generation of reactive oxygen species (ROS), and apoptosis (Figure 8). Inhibition of angiogenesis by HDAC inhibitors was found to prevent cancer metastasis. Their anti-angiogenic properties were associated with their ability to inhibit pro-angiogenic proteins such as vascular endothelial growth factor (VEGF), endothelial nitric oxide synthase (eNOS), bFGF and TGFbeta1 [111,112,113], to cite a few.
Figure 8.
Schematic representation of the main molecular events-induced by HDAC inhibitors preventing tumor metastasis and inducing tumor cell death.
Some inhibitors such as entinostat, also known as MS-275, were also found to induce radical oxygen species (ROS) leading to cell death in leukemia cells through the regulation of BH3 interacting domain death agonist protein (Bid) and B-cell lymphoma-2 (Bcl-2) expression levels [114,115]. Mechanistically it was found in prostate (LNCaP), breast (MCF7), and bladder (T24) cancer cell lines that both vorinostat and entinostat induce ROS by inhibiting the binding protein-2 (TBP-2), an inhibitor of the cellular thioredoxin (Trx) [116]. Interestingly, the induction of ROS in leukemia cells by vorinostat was also associated with activation of caspase-10 and Hsp90 cleavage [117].
More specifically, cellular cell death induced by HDAC inhibitors is largely associated with their ability to regulate selectively both the intrinsic and extrinsic pro-apoptotic pathways in tumor cells [118,119,120,121], but not in normal cells [122,123]. Vorinostat for example is able to induce the transcriptional activation of pro-apoptotic genes like Bcl-2-associated X protein (Bax), Bcl-2 associated agonist of cell death protein (Bad) and Phorbol-12-myristate-13-acetate-induced protein 1 (Noxa), promoting apoptosis through mitochondrial membrane changes and leading to the release of the pro-apoptotic factors such as Diablo/second mitochondria-derived activator of caspases (Smac), ATP and Apoptotic protease activating factor 1 (Apaf1), caspase-9, Serine protease (HtrA2), and cytochrome c (cyt c) in transformed fibroblast cell ([123] and Figure 8).
Other BH3-containing pro-apoptotic Bcl2 family members have been described to account for histone deacetylase inhibitor-induced cell death, including Bmf [124], Bak [125], Bid [126], and PUMA [125,127]. Along the line, it was found that Apaf1 expression level is significantly upregulated by the HDAC inhibitor TSA or siRNAs targeting HDAC1, HDAC2 and HDAC3 in hepatocellular carcinoma cell lines [128]. Concomitantly, HDAC inhibitors are also able to trigger apoptosis by down-regulating the anti-apoptotic proteins of the Bcl-2 family such as Bcl-2 itself [129], Bcl-xL [130,131], Bcl-xS [132], Mcl-1 [115,131], as well as XIAP [115,131] and survivin [133,134], two cellular inhibitors acting downstream of the mitochondria. Remarkably, the tumor properties of histone deacetylase inhibitors, consistent with their selective effect on pro-apoptotic genes involved in the intrinsic cell death pathway, also regulate genes associated with the extrinsic pathway, largely regulated by receptors of the TNF superfamily, including FasL, TRAIL and their cognate receptors ([132,135,136,137] and Figure 8).
6. DNA Methylation and Cancer
DNA methylation is another important epigenetic modification that occurs in the mammalian genome leading to regulation of gene expression. It acts in concert with other epigenetic mechanisms, including acetylation, to regulate normal gene expression and is often found to be exacerbated in cancer. Likewise, genome-wide hypermethylation has been described in primary and metastatic tumors [138,139,140,141,142]. Methylation occurs at specific DNA sequences such CpG dinucleotides, representing 5–10% of the human genome [143,144,145]. CpG dinucleotide-rich genomic DNA regions are also known as CpG islands, they are repeated in the human genome every 100 kb. DNA methylation is controlled by a group of DNA methyl transferases (DNMTs) [146] and demethylases (See the following reviews for detail [147,148,149,150,151]) [152]. Dysregulation of TRAIL signal transduction by methylation will be further described in the Section 7.1.
7. Epigenetic Regulation of TRAIL Proapoptotic Signaling
TRAIL belongs to the tumor necrosis factor (TNF) family, which encompasses 19 ligands and 29 receptors. These members were found to play a major role in the induction of apoptotic cell death and cell survival as well [153,154,155,156,157]. TNF-α, tumor necrosis factor related apoptosis-inducing ligand (TRAIL), and Fas ligand (FasL/CD95L) are considered as the major cytokines/proteins in this family with proapoptotic potential. The apoptotic pathway mediated by these cytokines occurs through two different signaling pathways, mainly the extrinsic (cytoplasmic) pathway and the intrinsic (mitochondrial) pathway (Figure 9). The extrinsic pathway is initiated when ligands such as FasL and TRAIL bind to their agonistic cell surface cognate death receptors (DR). Consequently, DR tends to oligomerize and induces the recruitment of Fas-associated death domain (FADD) and procaspase-8/-10 to form the death-inducing signaling complex (DISC). Following the assembly of DISC, a cascade of controlled programmed suicide signals is mediated by the activation of cellular caspases including the initiator caspases-8/-10 and the executioner caspases-3, -6, -7. The intrinsic pathway occurs via the cleavage of Bid by caspase-8 into truncated Bid (tBid) which subsequently translocates to the outer mitochondrial membrane in combination with Bax. This results in changing the equilibrium potential of the outer mitochondrial membrane and release of cyt c. Release of cyt c in the cytosol enables its interaction with Apaf1, leading to the formation of a large protein complex known as apoptosome, which recruits and activates the initiator caspase-9, allowing activation of the effector caspase-3, the apoptosis executioner [158,159,160]. In some instances, such as during ER stress, some receptors of this family, including DR4, DR5 and TNFR1 are able to engage apoptosis or necroptosis in a ligand-independent manner by inducing the recruitment and activation of the caspase-8 [161,162,163,164] or through RIPK1/RIPK3 and MLKL [164].
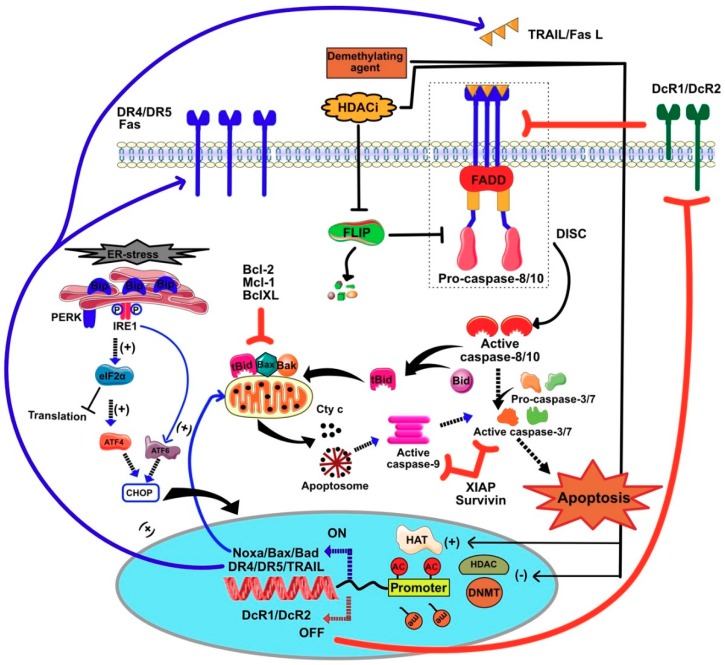
Figure 9.
Schematic diagram summarizing the different cell death signaling pathways-induced by epigenetic modification of chromatin following treatment with HDAC inhibitors and demethylating agents.
Like HDAC inhibitors, TRAIL was found to display selective antitumoral properties [165] and whereas it has raised major interest for cancer therapy [166], it soon became clear that a number of tumor cell lines or primary cells derived from patients suffering from cancer exhibit inherited secondary resistance toward TRAIL-induced cell death [167]. Such resistance may arise due to (1) the downregulation of cell surface DRs, (2) insufficient expression of caspase-8, and (3) overexpression of some antiapoptotic agents including caspase-8 and FADD-like apoptosis regulator (c-FLIP), Bcl-2, B-cell lymphoma-extra-large (Bcl-xL), myeloid cell leukemia 1 (Mcl-1), survivin, and (XIAP), X-linked inhibitor of apoptosis [160]. Epigenetic drugs such as HDAC inhibitors and demethylating agents have been found, however, to regulate the expression levels of both the receptors and downstream signal executioners or regulators of TRAIL (Figure 9). Moreover, histone deacetylase inhibitors have also been found, in some instances, to trigger selective apoptosis in cancer cells through death receptors ([135,137,168,169] and Figure 9). The molecular mechanisms by which these compounds trigger or restore the sensitivity of cancer cells toward apoptosis induced by the extrinsic or intrinsic pathway are often specific of the cell type, the drug itself, and the dose. In the following paragraph we will summarize the current understanding of the molecular mechanisms induced by epigenetic modulators associated specifically with TRAIL, its cognate receptors and downstream proximal signal transduction partners or regulators.
7.1. Restoration of TRAIL-Induced Apoptosis by Demethylating Agents
7.1.1. Regulation of Survivin and XIAP by Methylation
Survivin is one of the most distal inhibitors of TRAIL pro-apoptotic signaling. Its promoter is often hypomethylated in tumors, including hepatocellular, cervical or ovarian carcinomas and astrocytomas or multiform gliomas ([170,171,172,173,174] and Figure 10a). Although, none of these reports investigated the corresponding protein expression levels in these biopsies, contrary to normal counterpart cells, these findings suggest that survivin may be highly expressed in these tumors and thus likely to inhibit TRAIL-induced cell death. Indeed, overexpression of survivin in tumor cells and biopsies, at the protein level, has largely been described in the literature and is most of the time associated with poor outcome, prompting interest in its targeting [175,176]. However, the hypomethylation of the promoter of survivin was also found to allow p53 binding, thus leading to the repression of survivin transcription and protein expression ([177] and Figure 10a). Supporting these findings, the same authors demonstrated that hypermethylation of survivin promoter, in endometrial tumors, was associated with high expression levels of the protein [177]. Demethylating drugs such as decitabine have been shown to be poor inhibitors of survivin expression in small cell lung carcinoma (SCLC) cells [178]. However, the combination of class I & II HDAC inhibitor with decitabine inhibits survivin expression in these cells and increases their sensitivity to TRAIL-induced cell death [178]. The second most important and downstream inhibitor of TRAIL, XIAP, is not directly regulated by methylation, but its regulator, XIAP-associated factor 1 (XAF1), which is itself negatively regulated by hypermethylation [179]. As with survivin, the methylation status of XAF-1 promoter is not the only determinant of its basal transcription expression level, since it was found that restoration of XAF1 expression could be achieved by stimulating cells with IFN-beta, in spite of sustained promoter hypermethylation in these cells [180].
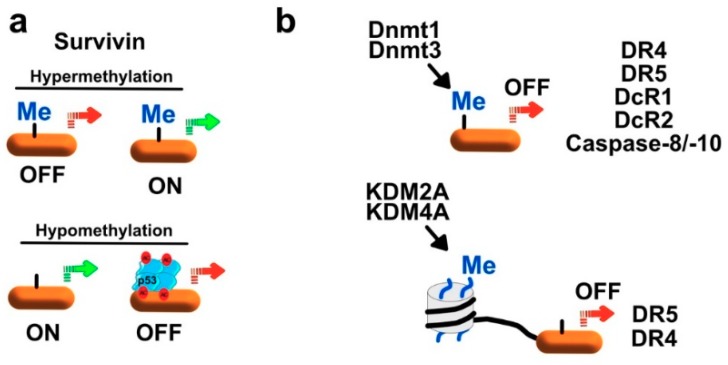
Figure 10.
(a) Epigenetic regulation of survivin in transformed cells. The promoter region of survivin is hypermehylated thus inhibiting TRAIL-dependent apoptotic signaling pathway. In contrast, hypomethylation of survivin promoter facilitates the binding of p53 repressing its transcriptional activation. (b) Epigenetic alterations represented in the methylation of TRAIL death receptors (DR4, DR5, DcR1, and DcR2) confer significant contributions to TRAIL-resistance in different type of tumors. Several DNA (Dmnt1&Dmnt3) and histone (KDM2B&KDM4A) methylases control the regulation of these receptors on the genomic level. Demethylation drugs such as azacitidine and decitabine as well as HDACIs like SAHA, TSA, and sodium butyrate can restore TRAIL sensitization.
7.1.2. Regulation of Initiator Caspases by Methylation
Further upstream are the caspase-8 and caspase-10, two cysteine proteases whose expression is required to enable TRAIL-induced apoptosis. Deregulation of the caspase-8 expression associated with CASP8 gene promoter hypermethylation has been described in neuroblastoma [181], retinoblastoma (Rb) [182], von Hippel-Lindau, and sporadic phaeochromocytoma cells [183]. Contrary to survivin or even XAF1, treatment of corresponding cells with decitabine, alone, restores both expression levels of caspase-8 and sensitivity to TRAIL-Induced apoptosis [181,182,184,185]. Methylation-induced regulation of caspase-8 expression has also been described in SCLC [178,186] and hepatocellular carcinomas (HCC) [187,188]. Of interest, silencing both DNMT1 and DNMT3b in HCC was found to be sufficient to restore caspase-8 expression and sensitivity to TRAIL-induced cell death ([188] and Figure 10b). In another study performed on 76 patients associated with glioblastomas, the loss of caspase-8 by methylation of its promoter reached more than 50% of the patients [189].
7.1.3. Regulation of TRAIL Receptors by Methylation
Besides caspase-8, the most important genes regulated by methylation and impacting TRAIL-induced cell death are those encoding its cognate receptors, namely DR4, DR5, DcR1 and DcR2. One of the earliest study performed on pediatric neuroblastoma cell lines, represented by nine neuroblastomas, three peripheral primitive neuro-ectodermal tumors (PNETs), and three cell lines from adult tumors, demonstrated that a loss of DcR1, and DcR2 mRNA expression occurred in 86% and 66% of tumor cells respectively, due to methylation of their promoter (Figure 10b). Methylation of DR4 and DR5 was also demonstrated, but to a much lesser extent, 47% and 20%, respectively [190]. Inhibiting methylation using 5-Azacytidine (Vidaza), restored in all cases transcription of DcR1 and DcR2 in these cells. Remarkably, methylation of DcR1 and DcR2 promoters was not observed in normal tissues, originating from heart, liver, lung, muscle, ovary, spleen or kidney [190,191].
Aberrant methylation of DR4 (41%), DR5 (10%), DcR1 (24%), and DcR2 (26%) were also described in von Hippel-Lindau and sporadic phaeochromocytomas [183]. The same authors also found out that similar methylation profiles could be detected in neuroblastomas and that 5-aza-2′-deoxycytidine (decitabine), by inhibiting promoter methylation of these genes could restore their expression. In glioblastomas, like CASP8, more than 40% of the cell lines studied displayed significant methylation in DR4 gene promoter, explaining at least partially the heterogeneity of the disease [189].
A high throughput quantitative DNA methylation analysis, performed on 17 gene promoter regions associated with DNA damage response (DDR) and death receptor apoptotic pathway with 162 normal and cancerous breast tissues from 81 sporadic breast cancer patients, demonstrated that sporadic breast tumor tissues displayed an obvious hypermethylation of TRAIL receptor genes DR5, DcR1, DcR2 associated with an hypomethylation of DR4 [192]. In another study focusing on invasive cervical cancers (9 cell lines and 114 primary tumors), it was demonstrated that DcR1 and, to a lesser extent, DcR2 are hypermethylated, but not DR4 and DR5 [193]. Hypermethylation of DcR1 gene promoter was found to be associated with 56 (45.5%) of the 123 invasive cervical cancers (CC). Methylation in SCLC was less frequently detected with 5.7% of the investigated tumors [193]. While it remains unclear why these receptors are differentially regulated by methylation in different tumor cell types and whether this has any influence toward TRAIL-induced apoptosis, a number of studies provide evidence that indeed silencing of TRAIL agonist receptors can impair TRAIL-induced cell death. It has been demonstrated for instance that silencing DR4 by methylation in astrocytic gliomas impedes TRAIL-induced cell death [194]. The resistance of cancer cell lines to TRAIL attributed to the hypermethylation of the promoter region of DR4 was abrogated by decitabine and associated with the re-expression of DR4 at the cell surface [194]. Methylation of DcR1 promoter was demonstrated in malignant melanoma cells to require the DNA methyl transferase DNMT1, whereas DcR2 methylation involved both DNMT1 and DNMT3a ([195] and Figure 10b). In breast cancer cells, however DcR2 methylation was proposed to be solely mediated by DNMT1 [196]. Like DcR2, methylation of DR5 may be governed by DNMT1 and DNMT3a [188,197]. Transcriptional regulation of DR4 and DR5 has, in addition been demonstrated to be also tightly controlled by two histone lysine demethylases, namely KDM2B [198] and KDM4A ([199], respectively (Figure 10b). Differential activity or expression of these DNA and histone methyl transferases is thus likely to account for selective expression of TRAIL receptors in tumor cells. Likewise, the DNMT1 inhibitor, brominated alkaloid Isofistularin-3 (Iso-3), from the marine sponge Aplysina aerophoba restores selectively DR5 but not DR4 expression in the B lymphoma cell line Raji, increasing its sensitivity to TRAIL-induced cell death [197]. In the same vein, silencing DNMT1 and DNMT3b in human hepatoma cells restores DR5 expression and TRAIL sensitivity [188].
Inhibition or silencing of KDM4A or KDM2B was also found to be sufficient to restore DR4 and DR5 expression, respectively and enhance or confer sensitivity to TRAIL [198,199]. It should nonetheless be mentioned here, that in addition to DR4 or DR5, the effects associated with the regulation of the methylation status of their promoter or histone neighborhood can also involve the coordinated negative regulation of antiapoptotic proteins such as c-FLIP, survivin, XAF1 or Mcl-1 [198], or the upregulation of pro-apoptotic proteins such as TRAIL itself [199].
7.2. HDACIs Sensitize Tumor Cells to TRAIL-Mediated Apoptosis
Regulation of Gene Expression by HDACi
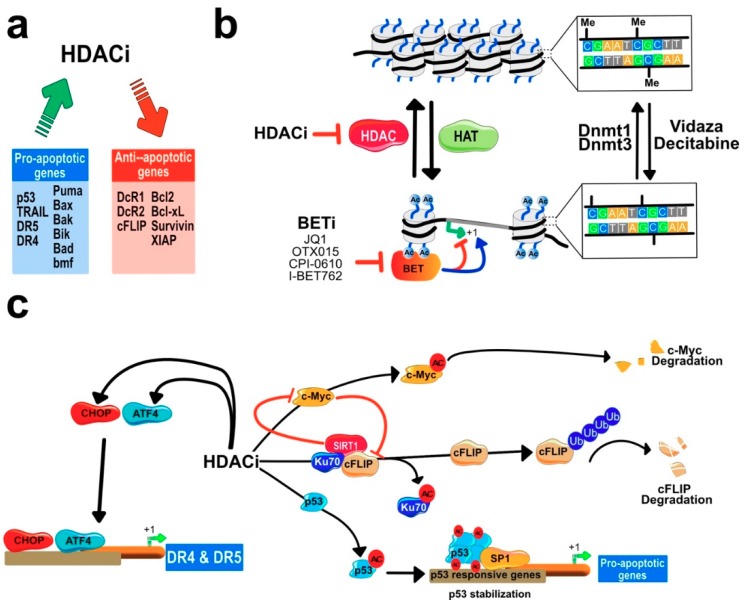
As illustrated in Figure 9 and Figure 11c, HDACi have often been described to enhance apoptosis induced by death-domain-containing receptors of the TNF family by coordinating proapoptotic and anti-apoptotic gene expression. For the sake of clarity, only the effects of HDACi on TRAIL-induced cell death will be presented here.
Figure 11.
Schematic representation of epigenetic events regulating TRAIL-induced apoptosis. (a) Main genes regulated by HDACi, either positively or negatively. (b) Illustration of the main epigenetic events affecting chromatin compaction and inhibitors that stimulate chromatin relaxation-based histone acetylation. Bromo-and extra terminal domains (BET) specifically bind to acetylated histones, regulating either positively or negatively genes in the neighborhood. Methylation of CpG island by DNA methylases also contribute to gene silencing. (c) HDACi can also regulate gene expression and increase sensitivity to TRAIL-induced apoptosis through acetylation of non-histone proteins. Acetylation of c-Myc induce its degradation whereas acetylation of Ku70 and p53, on the other hand, lead to enhanced TRAIL-induced cell death due to degradation of c-FLIP and upregulation of pro-apoptotic gene expression. HDACi can also induce regulation of TRAIL death receptors (DR4 & DR5) gene expression through the ER-stress sensors ATF4 and CHOP, see text.
In melanoma cell lines, the HDAC 1 and 3 inhibitor suberoyl bis-hydroxamic acid (SBHA) is able, alone, to enhance TRAIL-induced cell death by coordinating the upregulation of the pro-apoptotic proteins caspase-8, caspase-3, Bid, Bak, Bax, and Bim, while downregulating at the same time the antiapoptotic proteins, Bcl-xL, Mcl-1, and XIAP [126,131,200]. VPA, SAHA, and TSA on several melanoma cell lines were found to allow acetylation of H3 and H4 histones, leading to an increase in DR4 and DR5 expression levels and to concomitant inhibition of Bcl-xS, Bcl-xL [132]. Keeping in mind that immunotherapy has dramatically changed the treatment paradigm of melanoma, it is interesting to note that another study demonstrated that SAHA by inducing DR5 expression on the cell surface and downregulating c-IAP-2 and Bcl-xL is able to sensitize resistant melanoma cells to human cytotoxic T-lymphocytes (CTL) [201,202]. Coordinating the up-regulation of death receptors and downregulation of cFLIP and Bcl-2 family members by HDACi (Figure 11a) has also been described to a variable extent in leukemia ([66,118,120,121,203,204], breast carcinoma [199,205], lung carcinoma [119,178,199], glioblastoma [197,206], neuroblastoma [168,207], hepatocellular carcinoma [208,209], or bladder carcinoma [119,210,211]. Regardless of the molecular mechanism, HDACi are often able to restore TRAIL-induced apoptosis in resistant cancer cells [95,125,135,137,178,185,197,200,201,202,206,207,212,213,214,215,216,217,218,219].
By inhibiting histone deacetylases, HDACi induce the accumulation of acetylated lysine residues on histones, which leads to the relaxation of the chromatin and allows gene expression (Figure 11b). However, gene expression or repression is also regulated by BET (bromodomain and extra terminal) proteins, which have a strong affinity for acetylated histones. BET proteins represent thus an attractive target for cancer therapy, in particular when combined with HDACi, since it was found that BET inhibitors such as JQ1 can inhibit c-Myc [220]. Combination treatments associating HDACi and BETi induce strong apoptosis in advanced-stage cutaneous T-cell Lymphoma through inhibition of c-Myc and upregulation of pro-apoptotic proteins, including DR4, DR5 and TRAIL [221]. Interestingly, BETi, such as JQ1, OTX015, CPI-0610 or I-BET762, in non-small cell lung carcinoma (NSCLC), induce strong and preferential inhibition of XIAP and c-FLIP [222], suggesting that like HDACi, these inhibitors are able to coordinate selectively and differentially the expression levels of pro-apoptotic and anti-apoptotic proteins regulating TRAIL-induced cell death. Alone, JQ1 was found to inhibit both the short and the long isoform of c-FLIP in the NSCLC H157, H1299 and A549 cell lines and combined with TRAIL, synergistically induced apoptosis [223]. Its effect on c-FLIP was proposed to occur regardless of c-Myc, through a mechanism involving the proteosomal degradation [223].
This caspase-8 inhibitor, prevents apoptosis induced by death-domain containing receptors of the TNF superfamily [156,224], as well cell death induced by TLR3 [225]. c-FLIP is targeted by HDAC in almost all tumor cell type [66,69,121,205,208,209,226,227,228,229,230,231]. Mechanistically, this short-lived protein was found to interact, in colorectal cancer cells, with the DNA repair protein Ku70 [232]. By inducing Ku70 acetylation, vorinostat was found in these cells to disrupt Ku70 binding to c-FLIP, allowing polyubiquitination and degradation of c-FLIP by the proteasome (Figure 11c). These effects were recapitulated by an HDAC6 inhibitor [232]. It was next found in the hepatocellular carcinoma cell line HepG2 that SIRT1 interacts with c-FLIP and Ku70, inhibiting Ku70 acetylation and leading to c-FLIP stabilization [69]. Inhibiting SIRT1 expression using siRNAs or its function using the SIRT1 inhibitor amurensin G, a specific SIRT1 inhibitor, induced c-FLIP degradation and increased cell death-induced by TRAIL [69]. It should be noted here, though, that SIRT1 was also found to inhibit c-Myc, repressing in turn expression of ATF4, CHOP and DR5 ([69] and Figure 11c). Consistent with these findings, it has been demonstrated that DR5 and DR4 expression levels increase in cells submitted to acute or persistent endoplasmic reticulum (ER) stress through the regulation of ATF4 and CHOP, and that the upregulation of DR4 an DR5, in these conditions, can contribute to apoptosis induced by ER stress in a TRAIL-independent manner [161,162,163]. Notably, salermide, a class III HDAC inhibitor, was found to induce an ER stress leading to the upregulation of DR5 at the cell surface of NSCL cells and to trigger apoptosis, mediated at least in part by DR5 [233]. Salermide-induced DR5 upregulation was mediated through the activation of the ER-stress sensors inositol-requiring enzyme 1 α (IRE-1α), binding immunoglobulin protein (Bip), cyclic AMP-dependent transcription factor (ATF3), ATF4, and CCAAT/-enhancer-binding protein homologous protein (CHOP) [233].
Finally, histone deacetylase inhibitors have been found to act at the very proximal level of the TRAIL signal transduction pathway. For instance, in chronic lymphocytic leukemia cells, romidepsin has been described to facilitate FADD recruitment to DR4, enhancing thus TRAIL DISC formation and activation [203]. In leukemia cells, HDAC inhibitors, including VPA, SAHA, TSA and entinostat, used alone, have also been demonstrated to induce apoptosis through upregulation of TRAIL itself contributing to their pro-apoptotic activity ([135,137] and Figure 9). Along the line, it may be worth mentioning that association of the protein synthesis inhibitor homoharringtonine, also known as omacetaxine mepesuccinate, recently approved by the FDA, acts synergistically with vorinostat to induce apoptosis in a TRAIL/TRAIL receptor-dependent manner in acute myeloid leukemia cells [234]. Altogether these findings further highlight the importance of the epigenetic regulation of TRAIL and its cognate receptors in cancer cells.
8. Conclusions
The epigenetic modification of histone and non-histone proteins plays a central role in the physiopathology of cancer as a result of imbalanced acetylation/deacetylation and methylation/demethylation ratios. While several HDACi are approved by the FDA as a single agent in the treatment of different type of cancers, combination of HDACi with chemotherapeutic agents, epigenetic regulators such as demethylating agents or Bet inhibitors may increase their therapeutic potential. Alternatively, since HDAC inhibitors like TRAIL display apparent selective antitumoral properties, their association with TRAIL, which restores the sensitivity of resistant tumor cells to apoptosis by coordinating the downregulation of antiapoptotic genes, including c-FLIP, XIAP, and survivin or the upregulation of TRAIL agonist receptors (DR4 and DR5), could represent a promising antitumoral approach. To date, only one clinical trial has been conducted to determine the safety and tolerability of combinations associating a TRAIL derivative and a HDACi. Conatumumab, a fully human monoclonal agonist antibody against DR5, was combined with vorinostat in a phase Ib study with patients suffering from low grade lymphoma, mantle lymphoma, diffuse lymphoma, or Hodgkin’s disease. While the overall response of this study was reported to be poor (Clinical study report 20060340) despite the fact that the combination demonstrated a safety profile, the evaluation of TRAIL, or derivatives combined to HDACi or other epigenetic regulators, such as demethylating agents, is likely to represent an interesting therapeutic opportunity to treat patients suffering from cancer.
Author Contributions
O.M and M.I.Y.E. conceived and wrote this review.
Funding
O.M. is supported by grants from the ANR (Agence Nationale de la Recherche) program “Investissements d’Avenir” program, project ISITE-BFC (contract ANR-15-IDEX-0003) and LabEx LipSTIC (contract ANR-11-LABX-0021-01), la Ligue Nationale Contre le Cancer and the fondation ARC (Association pour la Recherche sur le cancer). M.I.Y.E. was supported by the Science and Technology Development Fund (STDF), Egypt (grant no. 4930).
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Richmond T.J., Davey C.A. The structure of DNA in the nucleosome core. Nature. 2003;423:145–150. doi: 10.1038/nature01595. [DOI] [PubMed] [Google Scholar]
- 2.Khorasanizadeh S. The nucleosome: from genomic organization to genomic regulation. Cell. 2004;116:259–272. doi: 10.1016/S0092-8674(04)00044-3. [DOI] [PubMed] [Google Scholar]
- 3.Brown R., Strathdee G. Epigenomics and epigenetic therapy of cancer. Trends Mol. Med. 2002;8:S43–S48. doi: 10.1016/S1471-4914(02)02314-6. [DOI] [PubMed] [Google Scholar]
- 4.Kouzarides T. Chromatin modifications and their function. Cell. 2007;128:693–705. doi: 10.1016/j.cell.2007.02.005. [DOI] [PubMed] [Google Scholar]
- 5.Mottamal M., Zheng S., Huang T.L., Wang G. Histone deacetylase inhibitors in clinical studies as templates for new anticancer agents. Molecules. 2015;20:3898–3941. doi: 10.3390/molecules20033898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Glozak M.A., Sengupta N., Zhang X., Seto E. Acetylation and deacetylation of non-histone proteins. Gene. 2005;363:15–23. doi: 10.1016/j.gene.2005.09.010. [DOI] [PubMed] [Google Scholar]
- 7.Kramer O.H., Gottlicher M., Heinzel T. Histone deacetylase as a therapeutic target. Trends Endocrinol. Metab. 2001;12:294–300. doi: 10.1016/S1043-2760(01)00438-6. [DOI] [PubMed] [Google Scholar]
- 8.Pandolfi P.P. Histone deacetylases and transcriptional therapy with their inhibitors. Cancer Chemother. Pharm. 2001;48(Suppl. S1):S17–S19. doi: 10.1007/s002800100322. [DOI] [PubMed] [Google Scholar]
- 9.Yang X.J., Gregoire S. Class II histone deacetylases: from sequence to function, regulation, and clinical implication. Mol. Cell. Biol. 2005;25:2873–2884. doi: 10.1128/MCB.25.8.2873-2884.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Marks P., Rifkind R.A., Richon V.M., Breslow R., Miller T., Kelly W.K. Histone deacetylases and cancer: causes and therapies. Nat. Rev. Cancer. 2001;1:194–202. doi: 10.1038/35106079. [DOI] [PubMed] [Google Scholar]
- 11.De Ruijter A.J., van Gennip A.H., Caron H.N., Kemp S., van Kuilenburg A.B. Histone deacetylases (HDACs): characterization of the classical HDAC family. Biochem. J. 2003;370:737–749. doi: 10.1042/bj20021321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fischle W., Kiermer V., Dequiedt F., Verdin E. The emerging role of class II histone deacetylases. Biochem. Cell. Biol. 2001;79:337–348. doi: 10.1139/o01-116. [DOI] [PubMed] [Google Scholar]
- 13.Gregoretti I.V., Lee Y.M., Goodson H.V. Molecular evolution of the histone deacetylase family: functional implications of phylogenetic analysis. J. Mol. Biol. 2004;338:17–31. doi: 10.1016/j.jmb.2004.02.006. [DOI] [PubMed] [Google Scholar]
- 14.Brosch G., Loidl P., Graessle S. Histone modifications and chromatin dynamics: A focus on filamentous fungi. FEMS Microbiol. Rev. 2008;32:409–439. doi: 10.1111/j.1574-6976.2007.00100.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Johnstone R.W. Histone-deacetylase inhibitors: Novel drugs for the treatment of cancer. Nat. Rev. Drug Discov. 2002;1:287–299. doi: 10.1038/nrd772. [DOI] [PubMed] [Google Scholar]
- 16.Kopito R.R. The missing linker: an unexpected role for a histone deacetylase. Mol. Cell. 2003;12:1349–1351. doi: 10.1016/S1097-2765(03)00498-2. [DOI] [PubMed] [Google Scholar]
- 17.Faiola F., Liu X., Lo S., Pan S., Zhang K., Lymar E., Farina A., Martinez E. Dual regulation of c-Myc by p300 via acetylation-dependent control of Myc protein turnover and coactivation of Myc-induced transcription. Mol. Cell. Biol. 2005;25:10220–10234. doi: 10.1128/MCB.25.23.10220-10234.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lindemann R.K., Gabrielli B., Johnstone R.W. Histone-deacetylase inhibitors for the treatment of cancer. Cell Cycle. 2004;3:779–788. doi: 10.4161/cc.3.6.927. [DOI] [PubMed] [Google Scholar]
- 19.Drummond D.C., Noble C.O., Kirpotin D.B., Guo Z., Scott G.K., Benz C.C. Clinical development of histone deacetylase inhibitors as anticancer agents. Annu. Rev. Pharm. Toxicol. 2005;45:495–528. doi: 10.1146/annurev.pharmtox.45.120403.095825. [DOI] [PubMed] [Google Scholar]
- 20.Cohen H.Y., Lavu S., Bitterman K.J., Hekking B., Imahiyerobo T.A., Miller C., Frye R., Ploegh H., Kessler B.M., Sinclair D.A. Acetylation of the C terminus of Ku70 by CBP and PCAF controls Bax-mediated apoptosis. Mol. Cell. 2004;13:627–638. doi: 10.1016/S1097-2765(04)00094-2. [DOI] [PubMed] [Google Scholar]
- 21.Bali P., Pranpat M., Bradner J., Balasis M., Fiskus W., Guo F., Rocha K., Kumaraswamy S., Boyapalle S., Atadja P., et al. Inhibition of histone deacetylase 6 acetylates and disrupts the chaperone function of heat shock protein 90: A novel basis for antileukemia activity of histone deacetylase inhibitors. J. Biol. Chem. 2005;280:26729–26734. doi: 10.1074/jbc.C500186200. [DOI] [PubMed] [Google Scholar]
- 22.Acharya M.R., Sparreboom A., Venitz J., Figg W.D. Rational development of histone deacetylase inhibitors as anticancer agents: a review. Mol. Pharm. 2005;68:917–932. doi: 10.1124/mol.105.014167. [DOI] [PubMed] [Google Scholar]
- 23.Kovacs J.J., Murphy P.J., Gaillard S., Zhao X., Wu J.T., Nicchitta C.V., Yoshida M., Toft D.O., Pratt W.B., Yao T.P. HDAC6 regulates Hsp90 acetylation and chaperone-dependent activation of glucocorticoid receptor. Mol. Cell. 2005;18:601–607. doi: 10.1016/j.molcel.2005.04.021. [DOI] [PubMed] [Google Scholar]
- 24.Wapenaar H., Dekker F.J. Histone acetyltransferases: challenges in targeting bi-substrate enzymes. Clin. Epigenet. 2016;8:59. doi: 10.1186/s13148-016-0225-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Patel J.H., Du Y., Ard P.G., Phillips C., Carella B., Chen C.J., Rakowski C., Chatterjee C., Lieberman P.M., Lane W.S., et al. The c-MYC oncoprotein is a substrate of the acetyltransferases hGCN5/PCAF and TIP60. Mol. Cell. Biol. 2004;24:10826–10834. doi: 10.1128/MCB.24.24.10826-10834.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ghizzoni M., Haisma H.J., Maarsingh H., Dekker F.J. Histone acetyltransferases are crucial regulators in NF-kappaB mediated inflammation. Drug Discov. Today. 2011;16:504–511. doi: 10.1016/j.drudis.2011.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Grossman S.R. p300/CBP/p53 interaction and regulation of the p53 response. Eur. J. Biochem. 2001;268:2773–2778. doi: 10.1046/j.1432-1327.2001.02226.x. [DOI] [PubMed] [Google Scholar]
- 28.Holden H.M., Matthews B.W. The binding of L-valyl-L-tryptophan to crystalline thermolysin illustrates the mode of interaction of a product of peptide hydrolysis. J. Biol. Chem. 1988;263:3256–3260. doi: 10.2210/pdb3tmn/pdb. [DOI] [PubMed] [Google Scholar]
- 29.Lombardi P.M., Cole K.E., Dowling D.P., Christianson D.W. Structure, mechanism, and inhibition of histone deacetylases and related metalloenzymes. Curr. Opin. Struct. Biol. 2011;21:735–743. doi: 10.1016/j.sbi.2011.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dowling D.P., Gattis S.G., Fierke C.A., Christianson D.W. Structures of metal-substituted human histone deacetylase 8 provide mechanistic inferences on biological function. Biochemistry. 2010;49:5048–5056. doi: 10.1021/bi1005046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gantt S.L., Joseph C.G., Fierke C.A. Activation and inhibition of histone deacetylase 8 by monovalent cations. J. Biol. Chem. 2010;285:6036–6043. doi: 10.1074/jbc.M109.033399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Somoza J.R., Skene R.J., Katz B.A., Mol C., Ho J.D., Jennings A.J., Luong C., Arvai A., Buggy J.J., Chi E., et al. Structural snapshots of human HDAC8 provide insights into the class I histone deacetylases. Structure. 2004;12:1325–1334. doi: 10.1016/j.str.2004.04.012. [DOI] [PubMed] [Google Scholar]
- 33.Vannini A., Volpari C., Gallinari P., Jones P., Mattu M., Carfi A., De Francesco R., Steinkuhler C., Di Marco S. Substrate binding to histone deacetylases as shown by the crystal structure of the HDAC8-substrate complex. EMBO Rep. 2007;8:879–884. doi: 10.1038/sj.embor.7401047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Haider S., Joseph C.G., Neidle S., Fierke C.A., Fuchter M.J. On the function of the internal cavity of histone deacetylase protein 8: R37 is a crucial residue for catalysis. Bioorg. Med. Chem. Lett. 2011;21:2129–2132. doi: 10.1016/j.bmcl.2011.01.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Glass C.K., Rosenfeld M.G. The coregulator exchange in transcriptional functions of nuclear receptors. Genes Dev. 2000;14:121–141. [PubMed] [Google Scholar]
- 36.Jones P.L., Veenstra G.J., Wade P.A., Vermaak D., Kass S.U., Landsberger N., Strouboulis J., Wolffe A.P. Methylated DNA and MeCP2 recruit histone deacetylase to repress transcription. Nat. Genet. 1998;19:187–191. doi: 10.1038/561. [DOI] [PubMed] [Google Scholar]
- 37.Wei L.N., Hu X., Chandra D., Seto E., Farooqui M. Receptor-interacting protein 140 directly recruits histone deacetylases for gene silencing. J. Biol. Chem. 2000;275:40782–40787. doi: 10.1074/jbc.M004821200. [DOI] [PubMed] [Google Scholar]
- 38.Espada J., Ballestar E., Fraga M.F., Villar-Garea A., Juarranz A., Stockert J.C., Robertson K.D., Fuks F., Esteller M. Human DNA methyltransferase 1 is required for maintenance of the histone H3 modification pattern. J. Biol. Chem. 2004;279:37175–37184. doi: 10.1074/jbc.M404842200. [DOI] [PubMed] [Google Scholar]
- 39.Bai S., Ghoshal K., Datta J., Majumder S., Yoon S.O., Jacob S.T. DNA methyltransferase 3b regulates nerve growth factor-induced differentiation of PC12 cells by recruiting histone deacetylase 2. Mol. Cell. Biol. 2005;25:751–766. doi: 10.1128/MCB.25.2.751-766.2005. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 40.Robertson K.D., Ait-Si-Ali S., Yokochi T., Wade P.A., Jones P.L., Wolffe A.P. DNMT1 forms a complex with Rb, E2F1 and HDAC1 and represses transcription from E2F-responsive promoters. Nat. Genet. 2000;25:338–342. doi: 10.1038/77124. [DOI] [PubMed] [Google Scholar]
- 41.Murphree A.L., Benedict W.F. Retinoblastoma: clues to human oncogenesis. Science. 1984;223:1028–1033. doi: 10.1126/science.6320372. [DOI] [PubMed] [Google Scholar]
- 42.Brehm A., Miska E.A., McCance D.J., Reid J.L., Bannister A.J., Kouzarides T. Retinoblastoma protein recruits histone deacetylase to repress transcription. Nature. 1998;391:597–601. doi: 10.1038/35404. [DOI] [PubMed] [Google Scholar]
- 43.Ferreira R., Magnaghi-Jaulin L., Robin P., Harel-Bellan A., Trouche D. The three members of the pocket proteins family share the ability to repress E2F activity through recruitment of a histone deacetylase. Proc. Natl. Acad. Sci. USA. 1998;95:10493–10498. doi: 10.1073/pnas.95.18.10493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Siddiqui H., Solomon D.A., Gunawardena R.W., Wang Y., Knudsen E.S. Histone deacetylation of RB-responsive promoters: requisite for specific gene repression but dispensable for cell cycle inhibition. Mol. Cell. Biol. 2003;23:7719–7731. doi: 10.1128/MCB.23.21.7719-7731.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kawai H., Li H., Avraham S., Jiang S., Avraham H.K. Overexpression of histone deacetylase HDAC1 modulates breast cancer progression by negative regulation of estrogen receptor alpha. Int. J. Cancer. 2003;107:353–358. doi: 10.1002/ijc.11403. [DOI] [PubMed] [Google Scholar]
- 46.Macaluso M., Cinti C., Russo G., Russo A., Giordano A. pRb2/p130-E2F4/5-HDAC1-SUV39H1-p300 and pRb2/p130-E2F4/5-HDAC1-SUV39H1-DNMT1 multimolecular complexes mediate the transcription of estrogen receptor-alpha in breast cancer. Oncogene. 2003;22:3511–3517. doi: 10.1038/sj.onc.1206578. [DOI] [PubMed] [Google Scholar]
- 47.Fraga M.F., Ballestar E., Villar-Garea A., Boix-Chornet M., Espada J., Schotta G., Bonaldi T., Haydon C., Ropero S., Petrie K., et al. Loss of acetylation at Lys16 and trimethylation at Lys20 of histone H4 is a common hallmark of human cancer. Nat. Genet. 2005;37:391–400. doi: 10.1038/ng1531. [DOI] [PubMed] [Google Scholar]
- 48.Yasui W., Oue N., Ono S., Mitani Y., Ito R., Nakayama H. Histone acetylation and gastrointestinal carcinogenesis. Ann. N. Y. Acad. Sci. 2003;983:220–231. doi: 10.1111/j.1749-6632.2003.tb05977.x. [DOI] [PubMed] [Google Scholar]
- 49.Bolden J.E., Peart M.J., Johnstone R.W. Anticancer activities of histone deacetylase inhibitors. Nat. Rev. Drug Discov. 2006;5:769–784. doi: 10.1038/nrd2133. [DOI] [PubMed] [Google Scholar]
- 50.Ropero S., Esteller M. The role of histone deacetylases (HDACs) in human cancer. Mol. Oncol. 2007;1:19–25. doi: 10.1016/j.molonc.2007.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gudas L.J., Wagner J.A. Retinoids regulate stem cell differentiation. J. Cell. Physiol. 2011;226:322–330. doi: 10.1002/jcp.22417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lin R.J., Sternsdorf T., Tini M., Evans R.M. Transcriptional regulation in acute promyelocytic leukemia. Oncogene. 2001;20:7204–7215. doi: 10.1038/sj.onc.1204853. [DOI] [PubMed] [Google Scholar]
- 53.Choi J.H., Kwon H.J., Yoon B.I., Kim J.H., Han S.U., Joo H.J., Kim D.Y. Expression profile of histone deacetylase 1 in gastric cancer tissues. Jpn. J. Cancer Res. 2001;92:1300–1304. doi: 10.1111/j.1349-7006.2001.tb02153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Halkidou K., Gaughan L., Cook S., Leung H.Y., Neal D.E., Robson C.N. Upregulation and nuclear recruitment of HDAC1 in hormone refractory prostate cancer. Prostate. 2004;59:177–189. doi: 10.1002/pros.20022. [DOI] [PubMed] [Google Scholar]
- 55.Wilson A.J., Byun D.S., Popova N., Murray L.B., L’Italien K., Sowa Y., Arango D., Velcich A., Augenlicht L.H., Mariadason J.M. Histone deacetylase 3 (HDAC3) and other class I HDACs regulate colon cell maturation and p21 expression and are deregulated in human colon cancer. J. Biol. Chem. 2006;281:13548–13558. doi: 10.1074/jbc.M510023200. [DOI] [PubMed] [Google Scholar]
- 56.Zhang Z., Yamashita H., Toyama T., Sugiura H., Ando Y., Mita K., Hamaguchi M., Hara Y., Kobayashi S., Iwase H. Quantitation of HDAC1 mRNA expression in invasive carcinoma of the breast. Breast Cancer Res. Treat. 2005;94:11–16. doi: 10.1007/s10549-005-6001-1. [DOI] [PubMed] [Google Scholar]
- 57.Huang B.H., Laban M., Leung C.H., Lee L., Lee C.K., Salto-Tellez M., Raju G.C., Hooi S.C. Inhibition of histone deacetylase 2 increases apoptosis and p21Cip1/WAF1 expression, independent of histone deacetylase 1. Cell Death Differ. 2005;12:395–404. doi: 10.1038/sj.cdd.4401567. [DOI] [PubMed] [Google Scholar]
- 58.Song J., Noh J.H., Lee J.H., Eun J.W., Ahn Y.M., Kim S.Y., Lee S.H., Park W.S., Yoo N.J., Lee J.Y., et al. Increased expression of histone deacetylase 2 is found in human gastric cancer. APMIS. 2005;113:264–268. doi: 10.1111/j.1600-0463.2005.apm_04.x. [DOI] [PubMed] [Google Scholar]
- 59.Zhu P., Martin E., Mengwasser J., Schlag P., Janssen K.P., Gottlicher M. Induction of HDAC2 expression upon loss of APC in colorectal tumorigenesis. Cancer Cell. 2004;5:455–463. doi: 10.1016/S1535-6108(04)00114-X. [DOI] [PubMed] [Google Scholar]
- 60.Zhang Z., Yamashita H., Toyama T., Sugiura H., Omoto Y., Ando Y., Mita K., Hamaguchi M., Hayashi S., Iwase H. HDAC6 expression is correlated with better survival in breast cancer. Clin. Cancer Res. 2004;10:6962–6968. doi: 10.1158/1078-0432.CCR-04-0455. [DOI] [PubMed] [Google Scholar]
- 61.Gui C.Y., Ngo L., Xu W.S., Richon V.M., Marks P.A. Histone deacetylase (HDAC) inhibitor activation of p21WAF1 involves changes in promoter-associated proteins, including HDAC1. Proc. Natl. Acad. Sci. USA. 2004;101:1241–1246. doi: 10.1073/pnas.0307708100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ocker M., Schneider-Stock R. Histone deacetylase inhibitors: signalling towards p21cip1/waf1. Int. J. Biochem. Cell Biol. 2007;39:1367–1374. doi: 10.1016/j.biocel.2007.03.001. [DOI] [PubMed] [Google Scholar]
- 63.Torigoe T., Izumi H., Wakasugi T., Niina I., Igarashi T., Yoshida T., Shibuya I., Chijiiwa K., Matsuo K., Itoh H., et al. DNA topoisomerase II poison TAS-103 transactivates GC-box-dependent transcription via acetylation of Sp1. J. Biol. Chem. 2005;280:1179–1185. doi: 10.1074/jbc.M410499200. [DOI] [PubMed] [Google Scholar]
- 64.Braun H., Koop R., Ertmer A., Nacht S., Suske G. Transcription factor Sp3 is regulated by acetylation. Nucleic. Acids Res. 2001;29:4994–5000. doi: 10.1093/nar/29.24.4994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Aguilera D.G., Das C.M., Sinnappah-Kang N.D., Joyce C., Taylor P.H., Wen S., Hasselblatt M., Paulus W., Fuller G., Wolff J.E., et al. Reactivation of death receptor 4 (DR4) expression sensitizes medulloblastoma cell lines to TRAIL. J. Neurooncol. 2009;93:303–318. doi: 10.1007/s11060-008-9788-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Guo F., Sigua C., Tao J., Bali P., George P., Li Y., Wittmann S., Moscinski L., Atadja P., Bhalla K. Cotreatment with histone deacetylase inhibitor LAQ824 enhances Apo-2L/tumor necrosis factor-related apoptosis inducing ligand-induced death inducing signaling complex activity and apoptosis of human acute leukemia cells. Cancer Res. 2004;64:2580–2589. doi: 10.1158/0008-5472.CAN-03-2629. [DOI] [PubMed] [Google Scholar]
- 67.Wu S., Meng Q., Zhang C., Sun H., Lu R., Gao N., Yang H., Li X., Aschner M., Chen R. DR4 mediates the progression, invasion, metastasis and survival of colorectal cancer through the Sp1/NF1 switch axis on genomic locus. Int. J. Cancer. 2018;143:289–297. doi: 10.1002/ijc.31318. [DOI] [PubMed] [Google Scholar]
- 68.Chuang C.H., Chan S.T., Chen C.H., Yeh S.L. Quercetin enhances the antitumor activity of trichostatin A through up-regulation of p300 protein expression in p53 null cancer cells. Chem. Biol. Interact. 2019;306:54–61. doi: 10.1016/j.cbi.2019.04.006. [DOI] [PubMed] [Google Scholar]
- 69.Kim M.J., Hong K.S., Kim H.B., Lee S.H., Bae J.H., Kim D.W., Dao T.T., Oh W.K., Kang C.D., Kim S.H. Ku70 acetylation and modulation of c-Myc/ATF4/CHOP signaling axis by SIRT1 inhibition lead to sensitization of HepG2 cells to TRAIL through induction of DR5 and down-regulation of c-FLIP. Int. J. Biochem. Cell Biol. 2013;45:711–723. doi: 10.1016/j.biocel.2012.12.005. [DOI] [PubMed] [Google Scholar]
- 70.Kim Y.H., Park J.W., Lee J.Y., Kwon T.K. Sodium butyrate sensitizes TRAIL-mediated apoptosis by induction of transcription from the DR5 gene promoter through Sp1 sites in colon cancer cells. Carcinogenesis. 2004;25:1813–1820. doi: 10.1093/carcin/bgh188. [DOI] [PubMed] [Google Scholar]
- 71.Shetty S., Graham B.A., Brown J.G., Hu X., Vegh-Yarema N., Harding G., Paul J.T., Gibson S.B. Transcription factor NF-kappaB differentially regulates death receptor 5 expression involving histone deacetylase 1. Mol. Cell. Biol. 2005;25:5404–5416. doi: 10.1128/MCB.25.13.5404-5416.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kavurma M.M., Santiago F.S., Bonfoco E., Khachigian L.M. Sp1 phosphorylation regulates apoptosis via extracellular FasL-Fas engagement. J. Biol. Chem. 2001;276:4964–4971. doi: 10.1074/jbc.M009251200. [DOI] [PubMed] [Google Scholar]
- 73.Xiao S., Matsui K., Fine A., Zhu B., Marshak-Rothstein A., Widom R.L., Ju S.T. FasL promoter activation by IL-2 through SP1 and NFAT but not Egr-2 and Egr-3. Eur J. Immunol. 1999;29:3456–3465. doi: 10.1002/(SICI)1521-4141(199911)29:11<3456::AID-IMMU3456>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- 74.Minucci S., Pelicci P.G. Histone deacetylase inhibitors and the promise of epigenetic (and more) treatments for cancer. Nat. Rev. Cancer. 2006;6:38–51. doi: 10.1038/nrc1779. [DOI] [PubMed] [Google Scholar]
- 75.Mei Z., Zhang X., Yi J., Huang J., He J., Tao Y. Sirtuins in metabolism, DNA repair and cancer. J. Exp. Clin. Cancer Res. 2016;35:182. doi: 10.1186/s13046-016-0461-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Alhazzazi T.Y., Kamarajan P., Verdin E., Kapila Y.L. Sirtuin-3 (SIRT3) and the Hallmarks of Cancer. Genes Cancer. 2013;4:164–171. doi: 10.1177/1947601913486351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Huang G., Zhu G. Sirtuin-4 (SIRT4), a therapeutic target with oncogenic and tumor-suppressive activity in cancer. Oncotargets. 2018;11:3395–3400. doi: 10.2147/OTT.S157724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.McGlynn L.M., Zino S., MacDonald A.I., Curle J., Reilly J.E., Mohammed Z.M., McMillan D.C., Mallon E., Payne A.P., Edwards J., et al. SIRT2: tumour suppressor or tumour promoter in operable breast cancer? Eur J. Cancer. 2014;50:290–301. doi: 10.1016/j.ejca.2013.10.005. [DOI] [PubMed] [Google Scholar]
- 79.Miyo M., Yamamoto H., Konno M., Colvin H., Nishida N., Koseki J., Kawamoto K., Ogawa H., Hamabe A., Uemura M., et al. Tumour-suppressive function of SIRT4 in human colorectal cancer. Br. J. Cancer. 2015;113:492–499. doi: 10.1038/bjc.2015.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Paredes S., Villanova L., Chua K.F. Molecular pathways: emerging roles of mammalian Sirtuin SIRT7 in cancer. Clin. Cancer Res. 2014;20:1741–1746. doi: 10.1158/1078-0432.CCR-13-1547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Sebastian C., Zwaans B.M., Silberman D.M., Gymrek M., Goren A., Zhong L., Ram O., Truelove J., Guimaraes A.R., Toiber D., et al. The histone deacetylase SIRT6 is a tumor suppressor that controls cancer metabolism. Cell. 2012;151:1185–1199. doi: 10.1016/j.cell.2012.10.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Tang X., Shi L., Xie N., Liu Z., Qian M., Meng F., Xu Q., Zhou M., Cao X., Zhu W.G., et al. SIRT7 antagonizes TGF-beta signaling and inhibits breast cancer metastasis. Nat. Commun. 2017;8:318. doi: 10.1038/s41467-017-00396-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Torrens-Mas M., Oliver J., Roca P., Sastre-Serra J. SIRT3: Oncogene and tumor suppressor in cancer. Cancers. 2017;9:90. doi: 10.3390/cancers9070090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Xu L., Che X., Wu Y., Song N., Shi S., Wang S., Li C., Zhang L., Zhang X., Qu X., et al. SIRT5 as a biomarker for response to anthracycline-taxane-based neoadjuvant chemotherapy in triple-negative breast cancer. Oncol. Rep. 2018;39:2315–2323. doi: 10.3892/or.2018.6319. [DOI] [PubMed] [Google Scholar]
- 85.Pruitt K., Zinn R.L., Ohm J.E., McGarvey K.M., Kang S.H., Watkins D.N., Herman J.G., Baylin S.B. Inhibition of SIRT1 reactivates silenced cancer genes without loss of promoter DNA hypermethylation. PLOS Genet. 2006;2:e40. doi: 10.1371/journal.pgen.0020040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Vaquero A., Scher M., Lee D., Erdjument-Bromage H., Tempst P., Reinberg D. Human SirT1 interacts with histone H1 and promotes formation of facultative heterochromatin. Mol. Cell. 2004;16:93–105. doi: 10.1016/j.molcel.2004.08.031. [DOI] [PubMed] [Google Scholar]
- 87.Yeung F., Hoberg J.E., Ramsey C.S., Keller M.D., Jones D.R., Frye R.A., Mayo M.W. Modulation of NF-kappaB-dependent transcription and cell survival by the SIRT1 deacetylase. EMBO J. 2004;23:2369–2380. doi: 10.1038/sj.emboj.7600244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Kuzmichev A., Margueron R., Vaquero A., Preissner T.S., Scher M., Kirmizis A., Ouyang X., Brockdorff N., Abate-Shen C., Farnham P., et al. Composition and histone substrates of polycomb repressive group complexes change during cellular differentiation. Proc. Natl. Acad. Sci. USA. 2005;102:1859–1864. doi: 10.1073/pnas.0409875102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Bradbury C.A., Khanim F.L., Hayden R., Bunce C.M., White D.A., Drayson M.T., Craddock C., Turner B.M. Histone deacetylases in acute myeloid leukaemia show a distinctive pattern of expression that changes selectively in response to deacetylase inhibitors. Leukemia. 2005;19:1751–1759. doi: 10.1038/sj.leu.2403910. [DOI] [PubMed] [Google Scholar]
- 90.Ozdag H., Teschendorff A.E., Ahmed A.A., Hyland S.J., Blenkiron C., Bobrow L., Veerakumarasivam A., Burtt G., Subkhankulova T., Arends M.J., et al. Differential expression of selected histone modifier genes in human solid cancers. BMC Genom. 2006;7:90. doi: 10.1186/1471-2164-7-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Chen W.Y., Wang D.H., Yen R.C., Luo J., Gu W., Baylin S.B. Tumor suppressor HIC1 directly regulates SIRT1 to modulate p53-dependent DNA-damage responses. Cell. 2005;123:437–448. doi: 10.1016/j.cell.2005.08.011. [DOI] [PubMed] [Google Scholar]
- 92.Jeong J., Juhn K., Lee H., Kim S.H., Min B.H., Lee K.M., Cho M.H., Park G.H., Lee K.H. SIRT1 promotes DNA repair activity and deacetylation of Ku70. Exp. Mol. Med. 2007;39:8–13. doi: 10.1038/emm.2007.2. [DOI] [PubMed] [Google Scholar]
- 93.Zhang W., Wu H., Yang M., Ye S., Li L., Zhang H., Hu J., Wang X., Xu J., Liang A. SIRT1 inhibition impairs non-homologous end joining DNA damage repair by increasing Ku70 acetylation in chronic myeloid leukemia cells. Oncotarget. 2016;7:13538–13550. doi: 10.18632/oncotarget.6455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Hull E.E., Montgomery M.R., Leyva K.J. HDAC Inhibitors as Epigenetic Regulators of the Immune System: Impacts on Cancer Therapy and Inflammatory Diseases. Biomed. Res. Int. 2016;2016:8797206. doi: 10.1155/2016/8797206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Perego P., Zuco V., Gatti L., Zunino F. Sensitization of tumor cells by targeting histone deacetylases. Biochem. Pharm. 2012;83:987–994. doi: 10.1016/j.bcp.2011.11.010. [DOI] [PubMed] [Google Scholar]
- 96.Peng L., Seto E. Deacetylation of nonhistone proteins by HDACs and the implications in cancer. Handb. Exp. Pharm. 2011;206:39–56. doi: 10.1007/978-3-642-21631-2_3. [DOI] [PubMed] [Google Scholar]
- 97.Eckschlager T., Plch J., Stiborova M., Hrabeta J. Histone deacetylase inhibitors as anticancer drugs. Int. J. Mol. Sci. 2017;18:1414. doi: 10.3390/ijms18071414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Ceccacci E., Minucci S. Inhibition of histone deacetylases in cancer therapy: lessons from leukaemia. Br. J. Cancer. 2016;114:605–611. doi: 10.1038/bjc.2016.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Rajak H., Singh A., Raghuwanshi K., Kumar R., Dewangan P.K., Veerasamy R., Sharma P.C., Dixit A., Mishra P. A structural insight into hydroxamic acid based histone deacetylase inhibitors for the presence of anticancer activity. Curr. Med. Chem. 2014;21:2642–2664. doi: 10.2174/09298673113209990191. [DOI] [PubMed] [Google Scholar]
- 100.Lobera M., Madauss K.P., Pohlhaus D.T., Wright Q.G., Trocha M., Schmidt D.R., Baloglu E., Trump R.P., Head M.S., Hofmann G.A., et al. Selective class IIa histone deacetylase inhibition via a nonchelating zinc-binding group. Nat. Chem. Biol. 2013;9:319–325. doi: 10.1038/nchembio.1223. [DOI] [PubMed] [Google Scholar]
- 101.Su J.M., Li X.N., Thompson P., Ou C.N., Ingle A.M., Russell H., Lau C.C., Adamson P.C., Blaney S.M. Phase 1 study of valproic acid in pediatric patients with refractory solid or CNS tumors: a children’s oncology group report. Clin. Cancer Res. 2011;17:589–597. doi: 10.1158/1078-0432.CCR-10-0738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Ganai S.A. Histone deacetylase inhibitor sulforaphane: The phytochemical with vibrant activity against prostate cancer. Biomed. Pharm. 2016;81:250–257. doi: 10.1016/j.biopha.2016.04.022. [DOI] [PubMed] [Google Scholar]
- 103.Mann B.S., Johnson J.R., Cohen M.H., Justice R., Pazdur R. FDA approval summary: vorinostat for treatment of advanced primary cutaneous T-cell lymphoma. Oncologist. 2007;12:1247–1252. doi: 10.1634/theoncologist.12-10-1247. [DOI] [PubMed] [Google Scholar]
- 104.Piekarz R.L., Frye R., Turner M., Wright J.J., Allen S.L., Kirschbaum M.H., Zain J., Prince H.M., Leonard J.P., Geskin L.J., et al. Phase II multi-institutional trial of the histone deacetylase inhibitor romidepsin as monotherapy for patients with cutaneous T-cell lymphoma. J. Clin. Oncol. 2009;27:5410–5417. doi: 10.1200/JCO.2008.21.6150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Whittaker S.J., Demierre M.F., Kim E.J., Rook A.H., Lerner A., Duvic M., Scarisbrick J., Reddy S., Robak T., Becker J.C., et al. Final results from a multicenter, international, pivotal study of romidepsin in refractory cutaneous T-cell lymphoma. J. Clin. Oncol. 2010;28:4485–4491. doi: 10.1200/JCO.2010.28.9066. [DOI] [PubMed] [Google Scholar]
- 106.Foss F., Advani R., Duvic M., Hymes K.B., Intragumtornchai T., Lekhakula A., Shpilberg O., Lerner A., Belt R.J., Jacobsen E.D., et al. A Phase II trial of Belinostat (PXD101) in patients with relapsed or refractory peripheral or cutaneous T-cell lymphoma. Br. J. Haematol. 2015;168:811–819. doi: 10.1111/bjh.13222. [DOI] [PubMed] [Google Scholar]
- 107.Houtkooper R.H., Pirinen E., Auwerx J. Sirtuins as regulators of metabolism and healthspan. Nat. Rev. Mol. Cell. Biol. 2012;13:225–238. doi: 10.1038/nrm3293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Kozako T., Suzuki T., Yoshimitsu M., Arima N., Honda S., Soeda S. Anticancer agents targeted to sirtuins. Molecules. 2014;19:20295–20313. doi: 10.3390/molecules191220295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Medda F., Russell R.J., Higgins M., McCarthy A.R., Campbell J., Slawin A.M., Lane D.P., Lain S., Westwood N.J. Novel cambinol analogs as sirtuin inhibitors: synthesis, biological evaluation, and rationalization of activity. J. Med. Chem. 2009;52:2673–2682. doi: 10.1021/jm8014298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Figuera-Losada M., Stathis M., Dorskind J.M., Thomas A.G., Bandaru V.V., Yoo S.W., Westwood N.J., Rogers G.W., McArthur J.C., Haughey N.J., et al. Cambinol, a novel inhibitor of neutral sphingomyelinase 2 shows neuroprotective properties. PLoS ONE. 2015;10:e0124481. doi: 10.1371/journal.pone.0124481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Montgomery R.L., Potthoff M.J., Haberland M., Qi X., Matsuzaki S., Humphries K.M., Richardson J.A., Bassel-Duby R., Olson E.N. Maintenance of cardiac energy metabolism by histone deacetylase 3 in mice. J. Clin. Investig. 2008;118:3588–3597. doi: 10.1172/JCI35847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Zhang Z.H., Hao C.L., Liu P., Tian X., Wang L.H., Zhao L., Zhu C.M. Valproic acid inhibits tumor angiogenesis in mice transplanted with Kasumi1 leukemia cells. Mol. Med. Rep. 2014;9:443–449. doi: 10.3892/mmr.2013.1834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Zhou H., Jiang S., Chen J., Su S.B. Suberoylanilide hydroxamic acid suppresses inflammation-induced neovascularization. Can. J. Physiol. Pharm. 2014;92:879–885. doi: 10.1139/cjpp-2014-0117. [DOI] [PubMed] [Google Scholar]
- 114.Gao S., Mobley A., Miller C., Boklan J., Chandra J. Potentiation of reactive oxygen species is a marker for synergistic cytotoxicity of MS-275 and 5-azacytidine in leukemic cells. Leuk. Res. 2008;32:771–780. doi: 10.1016/j.leukres.2007.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Rosato R.R., Almenara J.A., Grant S. The histone deacetylase inhibitor MS-275 promotes differentiation or apoptosis in human leukemia cells through a process regulated by generation of reactive oxygen species and induction of p21CIP1/WAF1 1. Cancer Res. 2003;63:3637–3645. [PubMed] [Google Scholar]
- 116.Lincoln D.T., Ali Emadi E.M., Tonissen K.F., Clarke F.M. The thioredoxin-thioredoxin reductase system: over-expression in human cancer. Anticancer Res. 2003;23:2425–2433. [PubMed] [Google Scholar]
- 117.Park S., Park J.A., Kim Y.E., Song S., Kwon H.J., Lee Y. Suberoylanilide hydroxamic acid induces ROS-mediated cleavage of HSP90 in leukemia cells. Cell Stress Chaperones. 2015;20:149–157. doi: 10.1007/s12192-014-0533-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Bokelmann I., Mahlknecht U. Valproic acid sensitizes chronic lymphocytic leukemia cells to apoptosis and restores the balance between pro- and antiapoptotic proteins. Mol. Med. 2008;14:20–27. doi: 10.2119/2007-00084.Bokelmann. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Kim H.R., Kim E.J., Yang S.H., Jeong E.T., Park C., Lee J.H., Youn M.J., So H.S., Park R. Trichostatin A induces apoptosis in lung cancer cells via simultaneous activation of the death receptor-mediated and mitochondrial pathway? Exp. Mol. Med. 2006;38:616–624. doi: 10.1038/emm.2006.73. [DOI] [PubMed] [Google Scholar]
- 120.Morales J.C., Ruiz-Magana M.J., Carranza D., Ortiz-Ferron G., Ruiz-Ruiz C. HDAC inhibitors with different gene regulation activities depend on the mitochondrial pathway for the sensitization of leukemic T cells to TRAIL-induced apoptosis. Cancer Lett. 2010;297:91–100. doi: 10.1016/j.canlet.2010.04.029. [DOI] [PubMed] [Google Scholar]
- 121.Shankar S., Singh T.R., Fandy T.E., Luetrakul T., Ross D.D., Srivastava R.K. Interactive effects of histone deacetylase inhibitors and TRAIL on apoptosis in human leukemia cells: involvement of both death receptor and mitochondrial pathways. Int. J. Mol. Med. 2005;16:1125–1138. doi: 10.3892/ijmm.16.6.1125. [DOI] [PubMed] [Google Scholar]
- 122.Dawson M.A., Kouzarides T. Cancer epigenetics: from mechanism to therapy. Cell. 2012;150:12–27. doi: 10.1016/j.cell.2012.06.013. [DOI] [PubMed] [Google Scholar]
- 123.Bolden J.E., Shi W., Jankowski K., Kan C.Y., Cluse L., Martin B.P., MacKenzie K.L., Smyth G.K., Johnstone R.W. HDAC inhibitors induce tumor-cell-selective pro-apoptotic transcriptional responses. Cell Death Dis. 2013;4:e519. doi: 10.1038/cddis.2013.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Zhang Y., Adachi M., Kawamura R., Imai K. Bmf is a possible mediator in histone deacetylase inhibitors FK228 and CBHA-induced apoptosis. Cell Death Differ. 2006;13:129–140. doi: 10.1038/sj.cdd.4401686. [DOI] [PubMed] [Google Scholar]
- 125.Fandy T.E., Shankar S., Ross D.D., Sausville E., Srivastava R.K. Interactive effects of HDAC inhibitors and TRAIL on apoptosis are associated with changes in mitochondrial functions and expressions of cell cycle regulatory genes in multiple myeloma. Neoplasia. 2005;7:646–657. doi: 10.1593/neo.04655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Gillespie S., Borrow J., Zhang X.D., Hersey P. Bim plays a crucial role in synergistic induction of apoptosis by the histone deacetylase inhibitor SBHA and TRAIL in melanoma cells. Apoptosis. 2006;11:2251–2265. doi: 10.1007/s10495-006-0283-6. [DOI] [PubMed] [Google Scholar]
- 127.Feng L., Pan M., Sun J., Lu H., Shen Q., Zhang S., Jiang T., Liu L., Jin W., Chen Y., et al. Histone deacetylase 3 inhibits expression of PUMA in gastric cancer cells. J. Mol. Med. 2013;91:49–58. doi: 10.1007/s00109-012-0932-x. [DOI] [PubMed] [Google Scholar]
- 128.Buurman R., Sandbothe M., Schlegelberger B., Skawran B. HDAC inhibition activates the apoptosome via Apaf1 upregulation in hepatocellular carcinoma. Eur. J. Med. Res. 2016;21:26. doi: 10.1186/s40001-016-0217-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Duan H., Heckman C.A., Boxer L.M. Histone deacetylase inhibitors down-regulate bcl-2 expression and induce apoptosis in t(14;18) lymphomas. Mol. Cell. Biol. 2005;25:1608–1619. doi: 10.1128/MCB.25.5.1608-1619.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Chueh A.C., Tse J.W.T., Dickinson M., Ioannidis P., Jenkins L., Togel L., Tan B., Luk I., Davalos-Salas M., Nightingale R., et al. ATF3 repression of BCL-XL determines apoptotic sensitivity to HDAC inhibitors across tumor types. Clin. Cancer Res. 2017;23:5573–5584. doi: 10.1158/1078-0432.CCR-17-0466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Zhang X.D., Gillespie S.K., Borrow J.M., Hersey P. The histone deacetylase inhibitor suberic bishydroxamate regulates the expression of multiple apoptotic mediators and induces mitochondria-dependent apoptosis of melanoma cells. Mol. Cancer. 2004;3:425–435. doi: 10.1186/1476-4598-3-14. [DOI] [PubMed] [Google Scholar]
- 132.Facchetti F., Previdi S., Ballarini M., Minucci S., Perego P., La Porta C.A. Modulation of pro- and anti-apoptotic factors in human melanoma cells exposed to histone deacetylase inhibitors. Apoptosis. 2004;9:573–582. doi: 10.1023/B:APPT.0000038036.31271.50. [DOI] [PubMed] [Google Scholar]
- 133.Chuang Y.F., Huang S.W., Hsu Y.F., Yu M.C., Ou G., Huang W.J., Hsu M.J. WMJ-8-B, a novel hydroxamate derivative, induces MDA-MB-231 breast cancer cell death via the SHP-1-STAT3-survivin cascade. Br. J. Pharm. 2017;174:2941–2961. doi: 10.1111/bph.13929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.De Schepper S., Bruwiere H., Verhulst T., Steller U., Andries L., Wouters W., Janicot M., Arts J., Van Heusden J. Inhibition of histone deacetylases by chlamydocin induces apoptosis and proteasome-mediated degradation of survivin. J. Pharm. Exp. 2003;304:881–888. doi: 10.1124/jpet.102.042903. [DOI] [PubMed] [Google Scholar]
- 135.Insinga A., Monestiroli S., Ronzoni S., Gelmetti V., Marchesi F., Viale A., Altucci L., Nervi C., Minucci S., Pelicci P.G. Inhibitors of histone deacetylases induce tumor-selective apoptosis through activation of the death receptor pathway. Nat. Med. 2005;11:71–76. doi: 10.1038/nm1160. [DOI] [PubMed] [Google Scholar]
- 136.Zimmerman M.A., Singh N., Martin P.M., Thangaraju M., Ganapathy V., Waller J.L., Shi H., Robertson K.D., Munn D.H., Liu K. Butyrate suppresses colonic inflammation through HDAC1-dependent Fas upregulation and Fas-mediated apoptosis of T cells. Am. J. Physiol. Gastrointest. Liver Physiol. 2012;302:G1405–G1415. doi: 10.1152/ajpgi.00543.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Nebbioso A., Clarke N., Voltz E., Germain E., Ambrosino C., Bontempo P., Alvarez R., Schiavone E.M., Ferrara F., Bresciani F., et al. Tumor-selective action of HDAC inhibitors involves TRAIL induction in acute myeloid leukemia cells. Nat. Med. 2005;11:77–84. doi: 10.1038/nm1161. [DOI] [PubMed] [Google Scholar]
- 138.Feltus F.A., Lee E.K., Costello J.F., Plass C., Vertino P.M. Predicting aberrant CpG island methylation. Proc. Natl. Acad. Sci. USA. 2003;100:12253–12258. doi: 10.1073/pnas.2037852100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Costello J.F., Fruhwald M.C., Smiraglia D.J., Rush L.J., Robertson G.P., Gao X., Wright F.A., Feramisco J.D., Peltomaki P., Lang J.C., et al. Aberrant CpG-island methylation has non-random and tumour-type-specific patterns. Nat. Genet. 2000;24:132–138. doi: 10.1038/72785. [DOI] [PubMed] [Google Scholar]
- 140.Teschendorff A.E., Menon U., Gentry-Maharaj A., Ramus S.J., Weisenberger D.J., Shen H., Campan M., Noushmehr H., Bell C.G., Maxwell A.P., et al. Age-dependent DNA methylation of genes that are suppressed in stem cells is a hallmark of cancer. Genome Res. 2010;20:440–446. doi: 10.1101/gr.103606.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Bartlett T.E., Zaikin A., Olhede S.C., West J., Teschendorff A.E., Widschwendter M. Corruption of the intra-gene DNA methylation architecture is a hallmark of cancer. PLoS ONE. 2013;8:e68285. doi: 10.1371/journal.pone.0068285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Gkountela S., Castro-Giner F., Szczerba B.M., Vetter M., Landin J., Scherrer R., Krol I., Scheidmann M.C., Beisel C., Stirnimann C.U., et al. Circulating tumor cell clustering shapes DNA methylation to enable metastasis seeding. Cell. 2019;176:98–112. doi: 10.1016/j.cell.2018.11.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Singal R., Ginder G.D. DNA methylation. Blood. 1999;93:4059–4070. [PubMed] [Google Scholar]
- 144.Jones P.A., Baylin S.B. The fundamental role of epigenetic events in cancer. Nat. Rev. Genet. 2002;3:415–428. doi: 10.1038/nrg816. [DOI] [PubMed] [Google Scholar]
- 145.Bae M.G., Kim J.Y., Choi J.K. Frequent hypermethylation of orphan CpG islands with enhancer activity in cancer. BMC Med. Genom. 2016;9(Suppl. S1):38. doi: 10.1186/s12920-016-0198-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Costello J.F., Plass C. Methylation matters. J. Med. Genet. 2001;38:285–303. doi: 10.1136/jmg.38.5.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Gujar H., Weisenberger D.J., Liang G. The roles of human DNA methyltransferases and their isoforms in shaping the epigenome. Genes (Basel) 2019;10:172. doi: 10.3390/genes10020172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Van der Wijst M.G., Venkiteswaran M., Chen H., Xu G.L., Plosch T., Rots M.G. Local chromatin microenvironment determines DNMT activity: from DNA methyltransferase to DNA demethylase or DNA dehydroxymethylase. Epigenetics. 2015;10:671–676. doi: 10.1080/15592294.2015.1062204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Wang K.Y., Chen C.C., Shen C.K. Active DNA demethylation of the vertebrate genomes by DNA methyltransferases: deaminase, dehydroxymethylase or demethylase? Epigenomics. 2014;6:353–363. doi: 10.2217/epi.14.21. [DOI] [PubMed] [Google Scholar]
- 150.Koivunen P., Laukka T. The TET enzymes. Cell. Mol. Life Sci. 2018;75:1339–1348. doi: 10.1007/s00018-017-2721-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Kohli R.M., Zhang Y. TET enzymes, TDG and the dynamics of DNA demethylation. Nature. 2013;502:472–479. doi: 10.1038/nature12750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Carey N., Marques C.J., Reik W. DNA demethylases: a new epigenetic frontier in drug discovery. Drug Discov. Today. 2011;16:683–690. doi: 10.1016/j.drudis.2011.05.004. [DOI] [PubMed] [Google Scholar]
- 153.Bremer E. Targeting of the tumor necrosis factor receptor superfamily for cancer immunotherapy. ISRN Oncol. 2013;2013:371854. doi: 10.1155/2013/371854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Cavallini C., Lovato O., Bertolaso A., Pacelli L., Zoratti E., Zanolin E., Krampera M., Zamo A., Tecchio C., Cassatella M.A., et al. The TNF-family cytokine TL1A inhibits proliferation of human activated B cells. PLoS ONE. 2013;8:e60136. doi: 10.1371/journal.pone.0060136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Ma J., Bang B.R., Lu J., Eun S.Y., Otsuka M., Croft M., Tobias P., Han J., Takeuchi O., Akira S., et al. The TNF family member 4-1BBL sustains inflammation by interacting with TLR signaling components during late-phase activation. Sci. Signal. 2013;6:ra87. doi: 10.1126/scisignal.2004431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Micheau O. Posttranslational modifications and death receptor signalling. In: Micheau O., editor. TRAIL, Fas Ligand, TNF and TLR3 in Cancer. Springer International Publishing; Cham, Switzerland: 2017. [Google Scholar]
- 157.Micheau O. Regulation of TNF-related apoptosis-inducing ligand signaling by glycosylation. Int. J. Mol. Sci. 2018;19:715. doi: 10.3390/ijms19030715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Elmallah M.I., Micheau O. Marine drugs regulating apoptosis induced by tumor necrosis factor-related apoptosis-inducing ligand (TRAIL) Mar. Drugs. 2015;13:6884–6909. doi: 10.3390/md13116884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Pavet V., Portal M.M., Moulin J.C., Herbrecht R., Gronemeyer H. Towards novel paradigms for cancer therapy. Oncogene. 2011;30:1–20. doi: 10.1038/onc.2010.460. [DOI] [PubMed] [Google Scholar]
- 160.Srivastava R.K. Intracellular mechanisms of TRAIL and its role in cancer therapy. Mol. Cell. Biol. Res. Commun. 2000;4:67–75. doi: 10.1006/mcbr.2001.0265. [DOI] [PubMed] [Google Scholar]
- 161.Lu M., Lawrence D.A., Marsters S., Acosta-Alvear D., Kimmig P., Mendez A.S., Paton A.W., Paton J.C., Walter P., Ashkenazi A. Opposing unfolded-protein-response signals converge on death receptor 5 to control apoptosis. Science. 2014;345:98–101. doi: 10.1126/science.1254312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Dufour F., Rattier T., Constantinescu A.A., Zischler L., Morle A., Ben Mabrouk H., Humblin E., Jacquemin G., Szegezdi E., Delacote F., et al. TRAIL receptor gene editing unveils TRAIL-R1 as a master player of apoptosis induced by TRAIL and ER stress. Oncotarget. 2017;8:9974–9985. doi: 10.18632/oncotarget.14285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Iurlaro R., Puschel F., Leon-Annicchiarico C.L., O’Connor H., Martin S.J., Palou-Gramon D., Lucendo E., Munoz-Pinedo C. Glucose deprivation induces ATF4-mediated apoptosis through TRAIL death receptors. Mol. Cell. Biol. 2017:37. doi: 10.1128/MCB.00479-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Saveljeva S., Mc Laughlin S.L., Vandenabeele P., Samali A., Bertrand M.J. Endoplasmic reticulum stress induces ligand-independent TNFR1-mediated necroptosis in L929 cells. Cell Death Dis. 2015;6:e1587. doi: 10.1038/cddis.2014.548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Walczak H., Miller R.E., Ariail K., Gliniak B., Griffith T.S., Kubin M., Chin W., Jones J., Woodward A., Le T., et al. Tumoricidal activity of tumor necrosis factor-related apoptosis-inducing ligand in vivo. Nat. Med. 1999;5:157–163. doi: 10.1038/5517. [DOI] [PubMed] [Google Scholar]
- 166.Micheau O., Shirley S., Dufour F. Death receptors as targets in cancer. Br. J. Pharm. 2013;169:1723–1744. doi: 10.1111/bph.12238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Hersey P., Zhang X.D. How melanoma cells evade trail-induced apoptosis. Nat. Rev. Cancer. 2001;1:142–150. doi: 10.1038/35101078. [DOI] [PubMed] [Google Scholar]
- 168.Glick R.D., Swendeman S.L., Coffey D.C., Rifkind R.A., Marks P.A., Richon V.M., La Quaglia M.P. Hybrid polar histone deacetylase inhibitor induces apoptosis and CD95/CD95 ligand expression in human neuroblastoma. Cancer Res. 1999;59:4392–4399. [PubMed] [Google Scholar]
- 169.Kwon S.H., Ahn S.H., Kim Y.K., Bae G.U., Yoon J.W., Hong S., Lee H.Y., Lee Y.W., Lee H.W., Han J.W. Apicidin, a histone deacetylase inhibitor, induces apoptosis and Fas/Fas ligand expression in human acute promyelocytic leukemia cells. J. Biol. Chem. 2002;277:2073–2080. doi: 10.1074/jbc.M106699200. [DOI] [PubMed] [Google Scholar]
- 170.Hervouet E., Vallette F.M., Cartron P.F. Impact of the DNA methyltransferases expression on the methylation status of apoptosis-associated genes in glioblastoma multiforme. Cell Death Dis. 2010;1:e8. doi: 10.1038/cddis.2009.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Teodoridis J.M., Hall J., Marsh S., Kannall H.D., Smyth C., Curto J., Siddiqui N., Gabra H., McLeod H.L., Strathdee G., et al. CpG island methylation of DNA damage response genes in advanced ovarian cancer. Cancer Res. 2005;65:8961–8967. doi: 10.1158/0008-5472.CAN-05-1187. [DOI] [PubMed] [Google Scholar]
- 172.Yu J., Ni M., Xu J., Zhang H., Gao B., Gu J., Chen J., Zhang L., Wu M., Zhen S., et al. Methylation profiling of twenty promoter-CpG islands of genes which may contribute to hepatocellular carcinogenesis. BMC Cancer. 2002;2:29. doi: 10.1186/1471-2407-2-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Yu J., Zhang H., Gu J., Lin S., Li J., Lu W., Wang Y., Zhu J. Methylation profiles of thirty four promoter-CpG islands and concordant methylation behaviours of sixteen genes that may contribute to carcinogenesis of astrocytoma. BMC Cancer. 2004;4:65. doi: 10.1186/1471-2407-4-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Chaopatchayakul P., Jearanaikoon P., Yuenyao P., Limpaiboon T. Aberrant DNA methylation of apoptotic signaling genes in patients responsive and nonresponsive to therapy for cervical carcinoma. Am. J. Obs. Gynecol. 2010;202:281.e1–281.e9. doi: 10.1016/j.ajog.2009.11.037. [DOI] [PubMed] [Google Scholar]
- 175.Jaiswal P.K., Goel A., Mittal R.D. Survivin: A molecular biomarker in cancer. Indian J. Med. Res. 2015;141:389–397. doi: 10.4103/0971-5916.159250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Martinez-Garcia D., Manero-Ruperez N., Quesada R., Korrodi-Gregorio L., Soto-Cerrato V. Therapeutic strategies involving survivin inhibition in cancer. Med. Res. Rev. 2019;39:887–909. doi: 10.1002/med.21547. [DOI] [PubMed] [Google Scholar]
- 177.Nabilsi N.H., Broaddus R.R., Loose D.S. DNA methylation inhibits p53-mediated survivin repression. Oncogene. 2009;28:2046–2050. doi: 10.1038/onc.2009.62. [DOI] [PubMed] [Google Scholar]
- 178.Kaminskyy V.O., Surova O.V., Vaculova A., Zhivotovsky B. Combined inhibition of DNA methyltransferase and histone deacetylase restores caspase-8 expression and sensitizes SCLC cells to TRAIL. Carcinogenesis. 2011;32:1450–1458. doi: 10.1093/carcin/bgr135. [DOI] [PubMed] [Google Scholar]
- 179.Straszewski-Chavez S.L., Visintin I.P., Karassina N., Los G., Liston P., Halaban R., Fadiel A., Mor G. XAF1 mediates tumor necrosis factor-alpha-induced apoptosis and X-linked inhibitor of apoptosis cleavage by acting through the mitochondrial pathway. J. Biol. Chem. 2007;282:13059–13072. doi: 10.1074/jbc.M609038200. [DOI] [PubMed] [Google Scholar]
- 180.Micali O.C., Cheung H.H., Plenchette S., Hurley S.L., Liston P., LaCasse E.C., Korneluk R.G. Silencing of the XAF1 gene by promoter hypermethylation in cancer cells and reactivation to TRAIL-sensitization by IFN-beta. BMC Cancer. 2007;7:52. doi: 10.1186/1471-2407-7-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Hopkins-Donaldson S., Bodmer J.L., Bourloud K.B., Brognara C.B., Tschopp J., Gross N. Loss of caspase-8 expression in highly malignant human neuroblastoma cells correlates with resistance to tumor necrosis factor-related apoptosis-inducing ligand-induced apoptosis. Cancer Res. 2000;60:4315–4319. [PubMed] [Google Scholar]
- 182.Poulaki V., Mitsiades C.S., McMullan C., Fanourakis G., Negri J., Goudopoulou A., Halikias I.X., Voutsinas G., Tseleni-Balafouta S., Miller J.W., et al. Human retinoblastoma cells are resistant to apoptosis induced by death receptors: role of caspase-8 gene silencing. Invest. Ophthalmol. Vis. Sci. 2005;46:358–366. doi: 10.1167/iovs.04-0324. [DOI] [PubMed] [Google Scholar]
- 183.Margetts C.D., Astuti D., Gentle D.C., Cooper W.N., Cascon A., Catchpoole D., Robledo M., Neumann H.P., Latif F., Maher E.R. Epigenetic analysis of HIC1, CASP8, FLIP, TSP1, DCR1, DCR2, DR4, DR5, KvDMR1, H19 and preferential 11p15.5 maternal-allele loss in von Hippel-Lindau and sporadic phaeochromocytomas. Endocr. Relat. Cancer. 2005;12:161–172. doi: 10.1677/erc.1.00865. [DOI] [PubMed] [Google Scholar]
- 184.Eggert A., Grotzer M.A., Zuzak T.J., Wiewrodt B.R., Ho R., Ikegaki N., Brodeur G.M. Resistance to tumor necrosis factor-related apoptosis-inducing ligand (TRAIL)-induced apoptosis in neuroblastoma cells correlates with a loss of caspase-8 expression. Cancer Res. 2001;61:1314–1319. [PubMed] [Google Scholar]
- 185.Fulda S., Debatin K.M. 5-Aza-2′-deoxycytidine and IFN-gamma cooperate to sensitize for TRAIL-induced apoptosis by upregulating caspase-8. Oncogene. 2006;25:5125–5133. doi: 10.1038/sj.onc.1209518. [DOI] [PubMed] [Google Scholar]
- 186.Hopkins-Donaldson S., Ziegler A., Kurtz S., Bigosch C., Kandioler D., Ludwig C., Zangemeister-Wittke U., Stahel R. Silencing of death receptor and caspase-8 expression in small cell lung carcinoma cell lines and tumors by DNA methylation. Cell Death Differ. 2003;10:356–364. doi: 10.1038/sj.cdd.4401157. [DOI] [PubMed] [Google Scholar]
- 187.Cho S., Lee J.H., Cho S.B., Yoon K.W., Park S.Y., Lee W.S., Park C.H., Joo Y.E., Kim H.S., Choi S.K., et al. Epigenetic methylation and expression of caspase 8 and survivin in hepatocellular carcinoma. Pathol. Int. 2010;60:203–211. doi: 10.1111/j.1440-1827.2009.02507.x. [DOI] [PubMed] [Google Scholar]
- 188.Kurita S., Higuchi H., Saito Y., Nakamoto N., Takaishi H., Tada S., Saito H., Gores G.J., Hibi T. DNMT1 and DNMT3b silencing sensitizes human hepatoma cells to TRAIL-mediated apoptosis via up-regulation of TRAIL-R2/DR5 and caspase-8. Cancer Sci. 2010;101:1431–1439. doi: 10.1111/j.1349-7006.2010.01565.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Skiriute D., Vaitkiene P., Saferis V., Asmoniene V., Skauminas K., Deltuva V.P., Tamasauskas A. MGMT, GATA6, CD81, DR4, and CASP8 gene promoter methylation in glioblastoma. BMC Cancer. 2012;12:218. doi: 10.1186/1471-2407-12-218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Van Noesel M.M., van Bezouw S., Salomons G.S., Voute P.A., Pieters R., Baylin S.B., Herman J.G., Versteeg R. Tumor-specific down-regulation of the tumor necrosis factor-related apoptosis-inducing ligand decoy receptors DcR1 and DcR2 is associated with dense promoter hypermethylation. Cancer Res. 2002;62:2157–2161. [PubMed] [Google Scholar]
- 191.Van Noesel M.M., van Bezouw S., Voute P.A., Herman J.G., Pieters R., Versteeg R. Clustering of hypermethylated genes in neuroblastoma. Genes Chromosomes Cancer. 2003;38:226–233. doi: 10.1002/gcc.10278. [DOI] [PubMed] [Google Scholar]
- 192.Pal R., Srivastava N., Chopra R., Gochhait S., Gupta P., Prakash N., Agarwal G., Bamezai R.N. Investigation of DNA damage response and apoptotic gene methylation pattern in sporadic breast tumors using high throughput quantitative DNA methylation analysis technology. Mol. Cancer. 2010;9:303. doi: 10.1186/1476-4598-9-303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Narayan G., Xie D., Ishdorj G., Scotto L., Mansukhani M., Pothuri B., Wright J.D., Kaufmann A.M., Schneider A., Arias-Pulido H., et al. Epigenetic inactivation of TRAIL decoy receptors at 8p12-21.3 commonly deleted region confers sensitivity to Apo2L/trail-Cisplatin combination therapy in cervical cancer. Genes Chromosomes Cancer. 2016;55:177–189. doi: 10.1002/gcc.22325. [DOI] [PubMed] [Google Scholar]
- 194.Elias A., Siegelin M.D., Steinmuller A., von Deimling A., Lass U., Korn B., Mueller W. Epigenetic silencing of death receptor 4 mediates tumor necrosis factor-related apoptosis-inducing ligand resistance in gliomas. Clin. Cancer Res. 2009;15:5457–5465. doi: 10.1158/1078-0432.CCR-09-1125. [DOI] [PubMed] [Google Scholar]
- 195.Venza M., Visalli M., Catalano T., Fortunato C., Oteri R., Teti D., Venza I. Impact of DNA methyltransferases on the epigenetic regulation of tumor necrosis factor-related apoptosis-inducing ligand (TRAIL) receptor expression in malignant melanoma. Biochem. Biophys. Res. Commun. 2013;441:743–750. doi: 10.1016/j.bbrc.2013.10.114. [DOI] [PubMed] [Google Scholar]
- 196.Jang J.Y., Jeon Y.K., Choi Y., Kim C.W. Short-hairpin RNA-induced suppression of adenine nucleotide translocase-2 in breast cancer cells restores their susceptibility to TRAIL-induced apoptosis by activating JNK and modulating TRAIL receptor expression. Mol. Cancer. 2010;9:262. doi: 10.1186/1476-4598-9-262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Florean C., Schnekenburger M., Lee J.Y., Kim K.R., Mazumder A., Song S., Kim J.M., Grandjenette C., Kim J.G., Yoon A.Y., et al. Discovery and characterization of Isofistularin-3, a marine brominated alkaloid, as a new DNA demethylating agent inducing cell cycle arrest and sensitization to TRAIL in cancer cells. Oncotarget. 2016;7:24027–24049. doi: 10.18632/oncotarget.8210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Kurt I.C., Sur I., Kaya E., Cingoz A., Kazancioglu S., Kahya Z., Toparlak O.D., Senbabaoglu F., Kaya Z., Ozyerli E., et al. KDM2B, an H3K36-specific demethylase, regulates apoptotic response of GBM cells to TRAIL. Cell Death Dis. 2017;8:e2897. doi: 10.1038/cddis.2017.288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Wang J., Wang H., Wang L.Y., Cai D., Duan Z., Zhang Y., Chen P., Zou J.X., Xu J., Chen X., et al. Silencing the epigenetic silencer KDM4A for TRAIL and DR5 simultaneous induction and antitumor therapy. Cell Death Differ. 2016;23:1886–1896. doi: 10.1038/cdd.2016.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Zhang X.D., Gillespie S.K., Borrow J.M., Hersey P. The histone deacetylase inhibitor suberic bishydroxamate: a potential sensitizer of melanoma to TNF-related apoptosis-inducing ligand (TRAIL) induced apoptosis. Biochem. Pharm. 2003;66:1537–1545. doi: 10.1016/S0006-2952(03)00509-4. [DOI] [PubMed] [Google Scholar]
- 201.Jazirehi A.R., Arle D. Epigenetic regulation of the TRAIL/Apo2L apoptotic pathway by histone deacetylase inhibitors: an attractive approach to bypass melanoma immunotherapy resistance. Am. J. Clin. Exp. Immunol. 2013;2:55–74. [PMC free article] [PubMed] [Google Scholar]
- 202.Jazirehi A.R., Kurdistani S.K., Economou J.S. Histone deacetylase inhibitor sensitizes apoptosis-resistant melanomas to cytotoxic human T lymphocytes through regulation of TRAIL/DR5 pathway. J. Immunol. 2014;192:3981–3989. doi: 10.4049/jimmunol.1302532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Inoue S., Harper N., Walewska R., Dyer M.J., Cohen G.M. Enhanced Fas-associated death domain recruitment by histone deacetylase inhibitors is critical for the sensitization of chronic lymphocytic leukemia cells to TRAIL-induced apoptosis. Mol. Cancer. 2009;8:3088–3097. doi: 10.1158/1535-7163.MCT-09-0451. [DOI] [PubMed] [Google Scholar]
- 204.D’Acunto C.W., Carratu A., Rodriquez M., Taddei M., Parente L., Petrella A. LGP1, A histone deacetylase inhibitor analogue of FR235222, sensitizes promyelocytic leukaemia U937 cells to TRAIL-mediated apoptosis. Anticancer Res. 2010;30:887–894. [PubMed] [Google Scholar]
- 205.Frew A.J., Lindemann R.K., Martin B.P., Clarke C.J., Sharkey J., Anthony D.A., Banks K.M., Haynes N.M., Gangatirkar P., Stanley K., et al. Combination therapy of established cancer using a histone deacetylase inhibitor and a TRAIL receptor agonist. Proc. Natl Acad. Sci. USA. 2008;105:11317–11322. doi: 10.1073/pnas.0801868105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Kim E.H., Kim H.S., Kim S.U., Noh E.J., Lee J.S., Choi K.S. Sodium butyrate sensitizes human glioma cells to TRAIL-mediated apoptosis through inhibition of Cdc2 and the subsequent downregulation of survivin and XIAP. Oncogene. 2005;24:6877–6889. doi: 10.1038/sj.onc.1208851. [DOI] [PubMed] [Google Scholar]
- 207.Muhlethaler-Mottet A., Flahaut M., Bourloud K.B., Auderset K., Meier R., Joseph J.M., Gross N. Histone deacetylase inhibitors strongly sensitise neuroblastoma cells to TRAIL-induced apoptosis by a caspases-dependent increase of the pro- to anti-apoptotic proteins ratio. BMC Cancer. 2006;6:214. doi: 10.1186/1471-2407-6-214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Schuchmann M., Schulze-Bergkamen H., Fleischer B., Schattenberg J.M., Siebler J., Weinmann A., Teufel A., Worns M., Fischer T., Strand S., et al. Histone deacetylase inhibition by valproic acid down-regulates c-FLIP/CASH and sensitizes hepatoma cells towards CD95- and TRAIL receptor-mediated apoptosis and chemotherapy. Oncol Rep. 2006;15:227–230. doi: 10.3892/or.15.1.227. [DOI] [PubMed] [Google Scholar]
- 209.Carlisi D., Lauricella M., D’Anneo A., Emanuele S., Angileri L., Di Fazio P., Santulli A., Vento R., Tesoriere G. The histone deacetylase inhibitor suberoylanilide hydroxamic acid sensitises human hepatocellular carcinoma cells to TRAIL-induced apoptosis by TRAIL-DISC activation. Eur. J. Cancer. 2009;45:2425–2438. doi: 10.1016/j.ejca.2009.06.024. [DOI] [PubMed] [Google Scholar]
- 210.Earel J.K., Jr., VanOosten R.L., Griffith T.S. Histone deacetylase inhibitors modulate the sensitivity of tumor necrosis factor-related apoptosis-inducing ligand-resistant bladder tumor cells. Cancer Res. 2006;66:499–507. doi: 10.1158/0008-5472.CAN-05-3017. [DOI] [PubMed] [Google Scholar]
- 211.Kim S.Y., Hong M., Heo S.H., Park S., Kwon T.K., Sung Y.H., Oh Y., Lee S., Yi G.S., Kim I. Inhibition of euchromatin histone-lysine N-methyltransferase 2 sensitizes breast cancer cells to tumor necrosis factor-related apoptosis-inducing ligand through reactive oxygen species-mediated activating transcription factor 4-C/EBP homologous protein-death receptor 5 pathway activation. Mol. Carcinog. 2018;57:1492–1506. doi: 10.1002/mc.22872. [DOI] [PubMed] [Google Scholar]
- 212.Fandy T.E., Srivastava R.K. Trichostatin A sensitizes TRAIL-resistant myeloma cells by downregulation of the antiapoptotic Bcl-2 proteins. Cancer Chemother. Pharm. 2006;58:471–477. doi: 10.1007/s00280-005-0184-3. [DOI] [PubMed] [Google Scholar]
- 213.Nakata S., Yoshida T., Horinaka M., Shiraishi T., Wakada M., Sakai T. Histone deacetylase inhibitors upregulate death receptor 5/TRAIL-R2 and sensitize apoptosis induced by TRAIL/APO2-L in human malignant tumor cells. Oncogene. 2004;23:6261–6271. doi: 10.1038/sj.onc.1207830. [DOI] [PubMed] [Google Scholar]
- 214.Iacomino G., Medici M.C., Russo G.L. Valproic acid sensitizes K562 erythroleukemia cells to TRAIL/Apo2L-induced apoptosis. Anticancer Res. 2008;28:855–864. [PubMed] [Google Scholar]
- 215.Frohlich L.F., Mrakovcic M., Smole C., Lahiri P., Zatloukal K. Epigenetic silencing of apoptosis-inducing gene expression can be efficiently overcome by combined SAHA and TRAIL treatment in uterine sarcoma cells. PLoS ONE. 2014;9:e91558. doi: 10.1371/journal.pone.0091558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Pathil A., Armeanu S., Venturelli S., Mascagni P., Weiss T.S., Gregor M., Lauer U.M., Bitzer M. HDAC inhibitor treatment of hepatoma cells induces both TRAIL-independent apoptosis and restoration of sensitivity to TRAIL. Hepatology. 2006;43:425–434. doi: 10.1002/hep.21054. [DOI] [PubMed] [Google Scholar]
- 217.Hacker S., Dittrich A., Mohr A., Schweitzer T., Rutkowski S., Krauss J., Debatin K.M., Fulda S. Histone deacetylase inhibitors cooperate with IFN-gamma to restore caspase-8 expression and overcome TRAIL resistance in cancers with silencing of caspase-8. Oncogene. 2009;28:3097–3110. doi: 10.1038/onc.2009.161. [DOI] [PubMed] [Google Scholar]
- 218.Wood T.E., Dalili S., Simpson C.D., Sukhai M.A., Hurren R., Anyiwe K., Mao X., Suarez Saiz F., Gronda M., Eberhard Y., et al. Selective inhibition of histone deacetylases sensitizes malignant cells to death receptor ligands. Mol. Cancer. 2010;9:246–256. doi: 10.1158/1535-7163.MCT-09-0495. [DOI] [PubMed] [Google Scholar]
- 219.Trivedi R., Mishra D.P. Trailing TRAIL resistance: Novel targets for TRAIL sensitization in cancer cells. Front. Oncol. 2015;5:69. doi: 10.3389/fonc.2015.00069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Mazur P.K., Herner A., Mello S.S., Wirth M., Hausmann S., Sanchez-Rivera F.J., Lofgren S.M., Kuschma T., Hahn S.A., Vangala D., et al. Combined inhibition of BET family proteins and histone deacetylases as a potential epigenetics-based therapy for pancreatic ductal adenocarcinoma. Nat. Med. 2015;21:1163–1171. doi: 10.1038/nm.3952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Zhao L., Okhovat J.P., Hong E.K., Kim Y.H., Wood G.S. Preclinical studies support combined inhibition of BET family proteins and histone deacetylases as epigenetic therapy for cutaneous T-cell lymphoma. Neoplasia. 2019;21:82–92. doi: 10.1016/j.neo.2018.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Klingbeil O., Lesche R., Gelato K.A., Haendler B., Lejeune P. Inhibition of BET bromodomain-dependent XIAP and FLIP expression sensitizes KRAS-mutated NSCLC to pro-apoptotic agents. Cell Death Dis. 2016;7:e2365. doi: 10.1038/cddis.2016.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Yao W., Yue P., Khuri F.R., Sun S.Y. The BET bromodomain inhibitor, JQ1, facilitates c-FLIP degradation and enhances TRAIL-induced apoptosis independent of BRD4 and c-Myc inhibition. Oncotarget. 2015;6:34669–34679. doi: 10.18632/oncotarget.5785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Irmler M., Thome M., Hahne M., Schneider P., Hofmann K., Steiner V., Bodmer J.L., Schroter M., Burns K., Mattmann C., et al. Inhibition of death receptor signals by cellular FLIP. Nature. 1997;388:190–195. doi: 10.1038/40657. [DOI] [PubMed] [Google Scholar]
- 225.Estornes Y., Toscano F., Virard F., Jacquemin G., Pierrot A., Vanbervliet B., Bonnin M., Lalaoui N., Mercier-Gouy P., Pacheco Y., et al. dsRNA induces apoptosis through an atypical death complex associating TLR3 to caspase-8. Cell Death Differ. 2012;19:1482–1494. doi: 10.1038/cdd.2012.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Bangert A., Cristofanon S., Eckhardt I., Abhari B.A., Kolodziej S., Hacker S., Vellanki S.H., Lausen J., Debatin K.M., Fulda S. Histone deacetylase inhibitors sensitize glioblastoma cells to TRAIL-induced apoptosis by c-myc-mediated downregulation of cFLIP. Oncogene. 2012;31:4677–4688. doi: 10.1038/onc.2011.614. [DOI] [PubMed] [Google Scholar]
- 227.Lauricella M., Ciraolo A., Carlisi D., Vento R., Tesoriere G. SAHA/TRAIL combination induces detachment and anoikis of MDA-MB231 and MCF-7 breast cancer cells. Biochimie. 2012;94:287–299. doi: 10.1016/j.biochi.2011.06.031. [DOI] [PubMed] [Google Scholar]
- 228.Rao-Bindal K., Koshkina N.V., Stewart J., Kleinerman E.S. The histone deacetylase inhibitor, MS-275 (entinostat), downregulates c-FLIP, sensitizes osteosarcoma cells to FasL, and induces the regression of osteosarcoma lung metastases. Curr. Cancer Drug Targets. 2013;13:411–422. doi: 10.2174/1568009611313040005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Sung E.S., Kim A., Park J.S., Chung J., Kwon M.H., Kim Y.S. Histone deacetylase inhibitors synergistically potentiate death receptor 4-mediated apoptotic cell death of human T-cell acute lymphoblastic leukemia cells. Apoptosis. 2010;15:1256–1269. doi: 10.1007/s10495-010-0521-9. [DOI] [PubMed] [Google Scholar]
- 230.Venza M., Visalli M., Beninati C., Benfatto S., Teti D., Venza I. miR-92a-3p and MYCBP2 are involved in MS-275-induced and c-myc-mediated TRAIL-sensitivity in melanoma cells. Int. Immunopharmacol. 2016;40:235–243. doi: 10.1016/j.intimp.2016.09.004. [DOI] [PubMed] [Google Scholar]
- 231.Zhang G., Park M.A., Mitchell C., Hamed H., Rahmani M., Martin A.P., Curiel D.T., Yacoub A., Graf M., Lee R., et al. Vorinostat and sorafenib synergistically kill tumor cells via FLIP suppression and CD95 activation. Clin. Cancer Res. 2008;14:5385–5399. doi: 10.1158/1078-0432.CCR-08-0469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Kerr E., Holohan C., McLaughlin K.M., Majkut J., Dolan S., Redmond K., Riley J., McLaughlin K., Stasik I., Crudden M., et al. Identification of an acetylation-dependant Ku70/FLIP complex that regulates FLIP expression and HDAC inhibitor-induced apoptosis. Cell Death Differ. 2012;19:1317–1327. doi: 10.1038/cdd.2012.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Liu G., Su L., Hao X., Zhong N., Zhong D., Singhal S., Liu X. Salermide up-regulates death receptor 5 expression through the ATF4-ATF3-CHOP axis and leads to apoptosis in human cancer cells. J. Cell. Mol. Med. 2012;16:1618–1628. doi: 10.1111/j.1582-4934.2011.01401.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Cao H., Cheng Y., You L., Qian J., Qian W. Homoharringtonine and SAHA synergistically enhance apoptosis in human acute myeloid leukemia cells through upregulation of TRAIL and death receptors. Mol. Med. Rep. 2013;7:1838–1844. doi: 10.3892/mmr.2013.1440. [DOI] [PubMed] [Google Scholar]