Abstract
In recent years, cardiovascular diseases (CVDs) have become a focus topic and global concern. There have been mixed reports on the relationship between whole grain or cereal fiber intake and the risk of type 2 diabetes. To evaluate whole grain or cereal intake on the risk of type 2 diabetes, we collected related literature on the relationship between whole grain or cereal fiber intake and the risk of type 2 diabetes. Methods: Eligible studies were identified from PubMed, Web of Science, and EBSCO (from 2007 to 2015). A total of three studies on whole grains were included, three studies about cereal fiber, and two on both whole grains and cereal fiber. We calculated the summary relative risks (RRs) using the random effects model. Eight studies contained 14,728 type 2 diabetes cases out of 434,903 subjects. Whole grain or cereal fiber intake is associated with type 2 diabetes (the overall RR was 0.68; 95% CI was 0.64-0.73) with significant heterogeneity in study-specific estimates (I2=0%, P=0.452). Whole grain and cereal fiber intake are inversely associated with the risk of type 2 diabetes.
Keywords: Diabetes mellitus, dietary fiber, meta-analysis
Introduction
In recent years, cardiovascular diseases (CVDs) have become a focus topic and global concern. According to the WHO reports in January 2015 on CVDs, CVDs are the leading cause of death globally: more people die annually from CVDs than from any other cause [1]. Diabetes is a chronic disease that occurs either when the pancreas does not produce enough insulin or when the body cannot effectively use the insulin it produces [2]. There was a prediction that diabetes will be the seventh leading cause of death in 2030 [3]. According to an analysis report of the National Health Services Survey in China (2008), the top three chronic diseases with the highest prevalence in urban areas are hypertension, diabetes, and ischemic heart disease [4]. The prevalence of diabetes is also high in rural areas.
Whole grains and cereal are beneficial for health. Whole grain consumption can reduce the risk of major chronic diseases and cereal is beneficial for diabetes because it slows the availability of glucose from breakfast [5-7]. Studies have identified associations between whole grain and cereal intake and type 2 diabetes. Some studies have focused on whole grains and type 2 diabetes, some have aimed at the relationship between cereal intake and type 2 diabetes, while others have focused on both whole grain and cereal intake [8,9]. Among these studies, all relative risks were less than 1. However, some 95% confidential intervals (CIs) of random risk (RR) were 1, while others were not. This means that there is a discrepancy in the relationship between whole grain and cereal intake and the risk of type 2 diabetes.
Therefore, this study aimed to perform a meta-analysis to find out whether whole grain or cereal intake would affect the incidence of type 2 diabetes among healthy individuals.
Methods
Search strategy and selection criteria
We systematically searched the PubMed electronic database up to June 30, 2015, using the terms “diabetes” and “whole grain” or “diabetes” and “cereal”. Studies were eligible if they met the following criteria: English language publication; cohort study or case-control study; the exposure of the cohort was to whole grains or cereal; for the cohort study, the outcome of interest was type 2 diabetes; for the cohort study, the incidence of type 2 diabetes or from type 2 diabetes to death was less than 5% (in this case, the association reported as hazard ratio (HR) was regarded as RR in our study [10]); the results were reported by RR (relative risk) or hazard ratio (HR) or OR (odds ratio) with 95% CI; whole grain and cereal intake was assessed by the food frequency questionnaire (FFQ) or the German Food Code and Nutrient Data Base, version II.3.
Data extraction
We collected the following data from the studies: the first author’s name, year of publication, gender, age, years of follow-up, number of cohort and cases, case ascertainment, exposure measurement, exposure categories, adjustment and adjusted RRs with their 95% CI. All RRs were extracted from the highest degree and adjusted for potential confounding factors.
Statistical analysis
For cohort studies included in our study, five studies used quintile, one quartile, and one used quintile to analyze the relationship between whole grain and cereal intake and the risk of type 2 diabetes. However, one study did not mention what kind of variable they treated the whole grain intake as [11]. In our study, RRs from studies focused on whole grains or cereals were combined because whole grains and cereals have a similar influence on blood glucose. RRs or OR was adjusted for age, gender, smoking status, physical activity, body mass index, family history of diabetes, and other potential confounding variables. For studies treating RRs as continuous intake, the estimates for categories were obtained from included studies.
The heterogeneity of the study was estimated by the I2 statistic. I2 describes the difference between studies with random error or chance [12]. If I2 > 50%, the random effect model was adopted to combine RRs or the fixed effect model was used as the combining method. To assess the possible publication bias among studies, we applied Egger’s test and Begg’s test. Subgroup analysis for gender, and sensitivity analysis were conducted in this study, also. For sensitivity analysis, after dropping the unqualified studies, RRs were combined again and compared with previous results. If the results did not change acutely, then the result of our study had high reliability.
Stata11.0 was used for all statistical analyses. The statistically significant p-value was less than 0.05.
Results
Characteristics of the included studies
We searched 36 studies through our literature screening, and 28 studies were not eligible and were excluded. In the end, seven cohort studies and one case-control study met the criteria (Figure 1). There were 434,903 participants among eight studies with 14,728 cases of type 2 diabetes with an average of 12.6 years of follow-up (Table 1).
Figure 1.
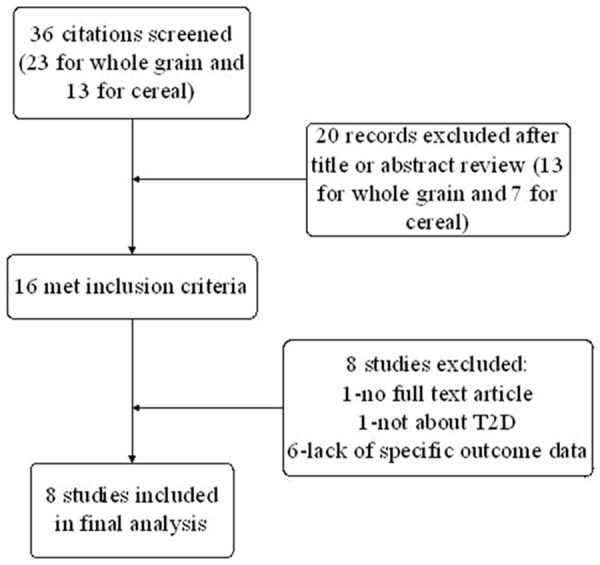
Study selection flow chart for the literature screening.
Table 1.
Characteristics of the included studies
| References | Type of study | Follow years (y) | Gender | Age (mean or range, y) | Number of cohort | Number of cases | Case ascertainment | Exposure measurement | Exposures categories |
|---|---|---|---|---|---|---|---|---|---|
| Matthias B. Schulze [15] | Cohort | 12 | M/F | 49.8 | 25067 | 844 | Physician diagnosis | German Food Code and Nutrient Data Base, version II.3 | 5 |
| S.Goya Wannamwtheew [16] | Cohort | 7 | M | 60-79 | 3482 | 162 | Self report | 7-day recall FFQ | 4 |
| Tina Wirström et al. [8] | Case control | - | M | 47.2 | 5477 | 701 | Physician diagnosis | FFQ | - |
| Meian He [17] | Cohort | 26 | F | 46 | 7822 | 295 | Self report | Semi-quantitative FFQ | 5 |
| Supriya Krishnan, DSc [9] | Cohort | 8 | F | 37 | 59000 | 1938 | Physician diagnosis | FFQ | 5 |
| Jeroen S.L.deMunter NSH I [13] | Cohort | 19 | F | 50.2 | 121,700 | 4747 | Self report | Semi-quantitative FFQ | 5 |
| Jeroen S.L.deMunter NSH II [13] | Cohort | 13 | F | 36 | 116,609 | 1739 | Self report | Semi-quantitative FFQ | 5 |
| Emily D Parker [14] | Cohort | 7.9 | F | 50-79 | 72215 | 3465 | Self report | WHI FFQ | 6 |
| A von Ruesten [11] | Cohort | 8 | M/F | 35-65 | 23531 | 837 | Self report | FFQ | - |
The measurements of whole grain and cereal intake were different. The FFQ was used in three studies; one was a case-control study and two were cohort studies. Three studies used semi-quantitative FFQ, and all research objects of these studies were female. Among the rest of three, one applied the German Food Code and Nutrient Data Base (version II.3), one used a seven-day recall FFQ, and another one used WHI FFQ (FFQ for female particularly).
The results of the meta-analysis
The results of the meta-analysis are shown in Figure 2. The combined RR was 0.74, 95% CI: 0.67~0.82. The summary RRs were close in whole grain and cereal studies. Heterogeneity was significant (I2=56.8%, P=0.06). Heterogeneity was not significant in the cereal studies but was significant in the whole grain studies (I2=0.0%, P=0.956; I2=74.6%, P=0.001).
Figure 2.
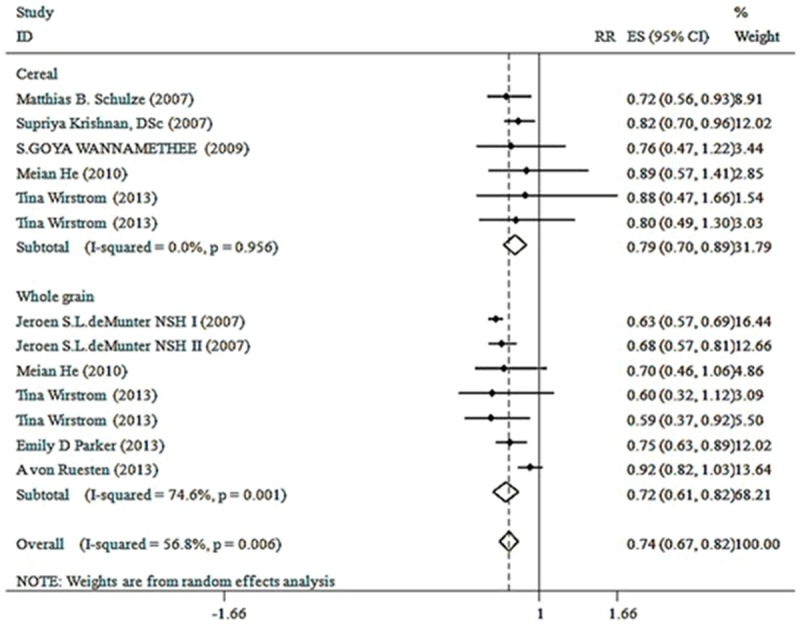
Forest plot of random effects meta-analysis.
Publication bias is shown in Figures 3 and 4. According to these figures, there was no bias among studies (t=0.14, P=0.89).
Figure 3.
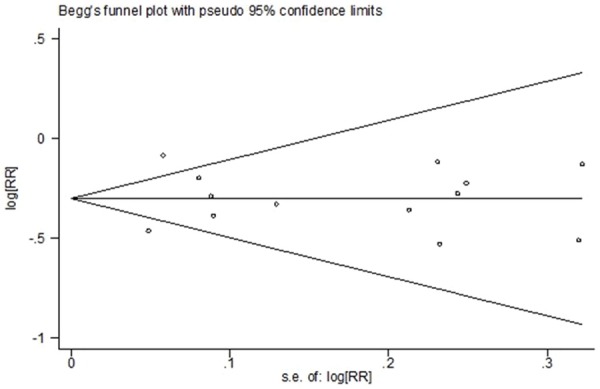
Begg’s funnel plot for publication bias.
Figure 4.
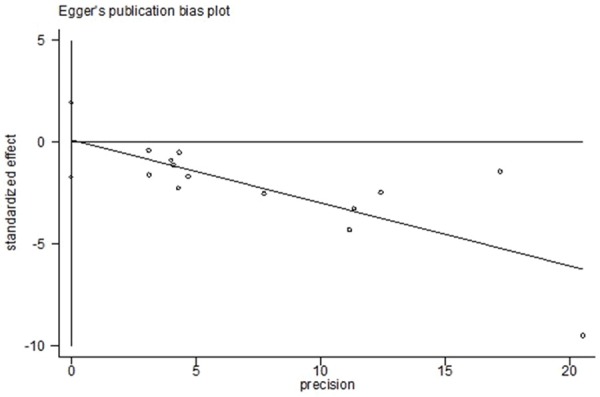
Egger’s funnel plot for publication bias.
Results of a subgroup meta-analysis
Figure 5 shows the meta-analysis by gender. The relationship between whole grain and cereal and type 2 diabetes was significant in both the male group and female group (RR=0.68, 95% CI 0.49-0.88; RR=0.74, 95% CI 0.64-0.77).
Figure 5.
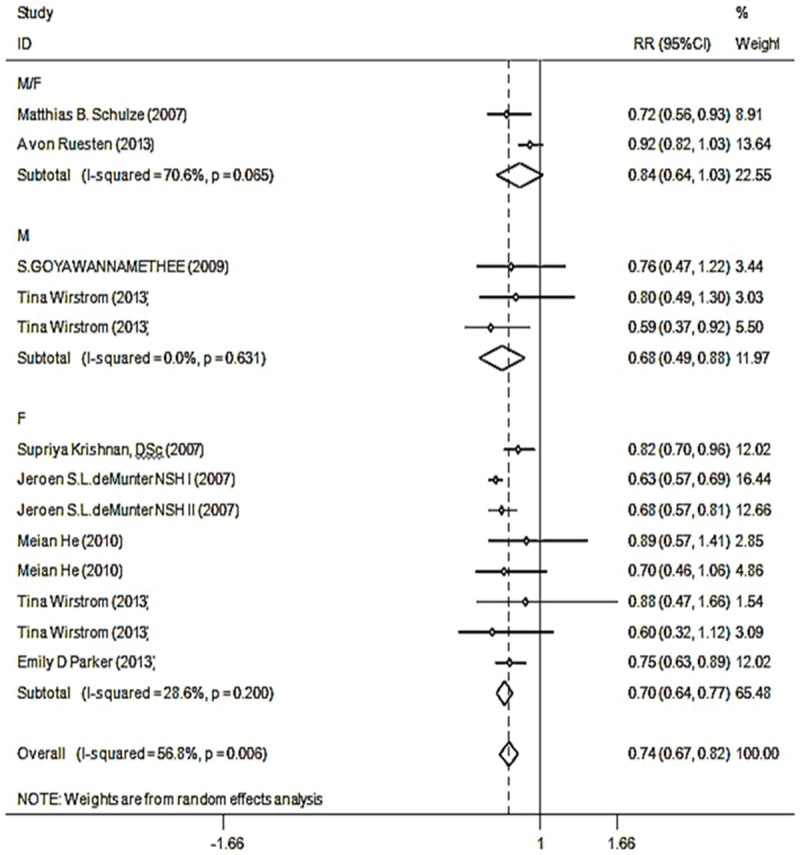
Forest plot by subgroup of different genders.
Sensitivity analysis
Sensitivity analysis is shown in Figure 6. In a further analysis shown in Figure 7, the study conducted by von Ruesten [11] was deleted. The pool RR was 0.68, 95% CI: 0.64-0.73. The I2 was 0.0% (P=0.452), which was very different from the first result (RR=0.74, 95% CI: 0.67-0.82). Therefore, the study by von Ruesten [11] had a great effect on the publication bias of this study.
Figure 6.
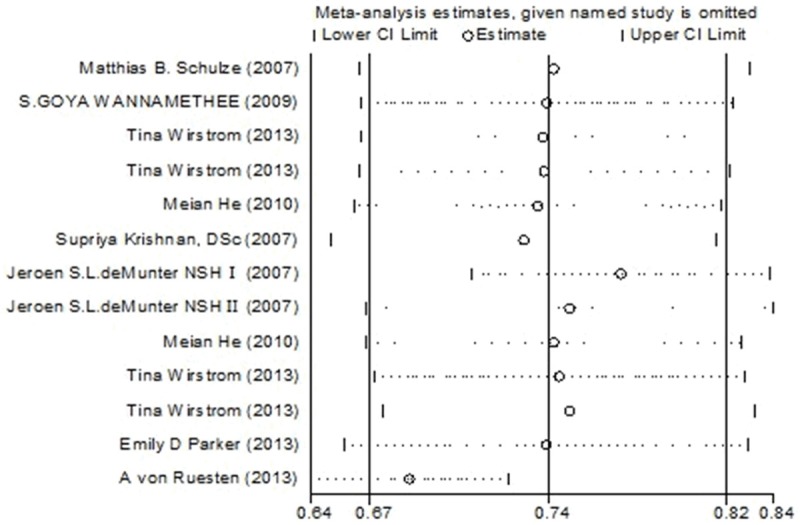
Sensitivity analyses on whole grain and cereal intake and type 2 diabetes.
Figure 7.
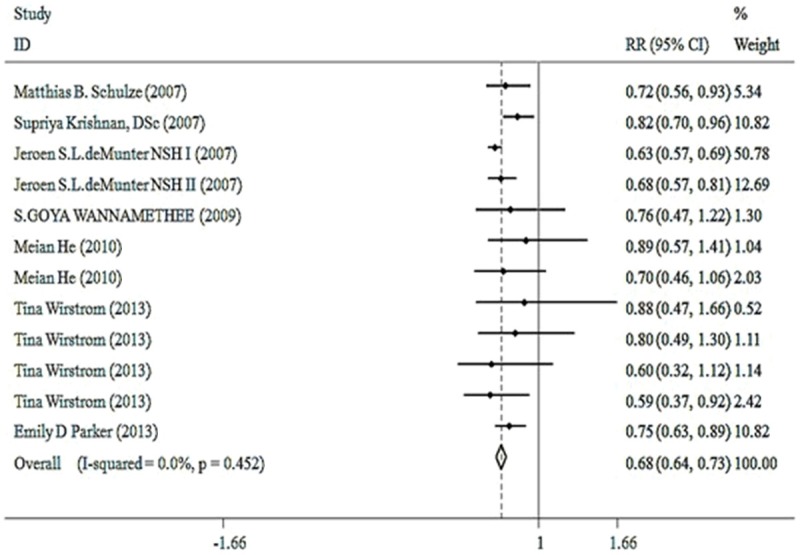
Forest plot by fixed model meta-analysis from which the study by von Ruesten was deleted.
Discussion
Our meta-analysis provides evidence for the role of whole grain and cereal intake as a risk factor for type 2 diabetes. The results of this study suggest that increased whole grain and cereal intake can reduce the risk of type 2 diabetes. The influence that whole grain and cereal intake has on the risk of type 2 diabetes was similar for both males and females. According to the publication bias test, the result is significant and can be trusted.
The results from single studies of whole grain and cereal intake and the risk of type 2 diabetes have been mixed. For whole grains, two studies found an inverse association between whole grain intake and the risk of type 2 diabetes and suggest that increasing whole grain consumption can prevent type 2 diabetes [13,14]. One study supported no significant association; however, the author still suggested that high consumption of whole grain bread is beneficial to health [11]. For cereal intake, two studies showed an inverse association and concluded that increasing cereal in the diet might be a way to decrease the occurrence of type 2 diabetes [9,15]. However, one study found no significant association between cereal intake and the incidence of type 2 diabetes [16]. Two studies focused on both whole grain and cereal consumption, but only one study found whole grains to be significantly associated with the risk of type 2 diabetes and suggested that a higher intake of whole grains decreased the risk of a deteriorating glucose tolerance including the progression from prediabetes to type 2 diabetes [8,17]. One study pointed out that it is time to confirm the relationship between cereals and type 2 diabetes by randomized controlled trials [18].
The result of this study confirms the findings of former studies and meta-analysis. There was one cohort study with 61 males and females that reported that a twelve-week whole grain and cereal-based diet reduced postprandial insulin and triglyceride responses [19]. As for whole grains, one meta-analysis combining dose-response analysis with six studies of 316,051 participants found that each additional 10 g of whole grain ingredient consumed daily saw an overall absolute reduction of 0.3% in the rate of type 2 diabetes [20]. For cereal consumption, there was no meta-analysis about cereal consumption and type 2 diabetes. Our meta-analysis with 434,903 participants with 14,728 cases of type 2 diabetes is a new study that analyzes the influence of whole grain and cereal intake on type 2 diabetes. Whole grains and cereals have a similar effect on humans. The reason is probably that whole grains and cereals contain lots of dietary fiber, which is good for health, and is especially helpful for controlling plasma glucose in type 2 diabetes. The RRs of whole grain and cereal studies were similar, so it is feasible to combine them.
In our study, a cohort study conducted by von Ruesten [11] was included at first but then excluded. In a sensitivity analysis, two studies showed a difference, but only von Ruesten’s study was deleted. The reasons are as follows. First, the way in which von Ruesten dealt with whole grain intake was different from the other cohort studies that treated whole grain intake as a continuous variable and divided it into categories. The deleted study did not divide whole grain consumption into categories when doing the data analysis. Second, in the subgroup by gender, I2 from the group from von Ruesten was high, while I2 from the group with deMunter NSH I’s study in it was lower [13]. This means that deMunter NSH I’s study did not affect our study but von Ruesten’s did. Third, after deleting the study by von Ruesten, the I2 changed greatly, but the combined RR changed only slightly. In conclusion, the study by von Ruesten had a great effect on the precision of the combined RR in our study. Hence, von Ruesten’s study was deleted.
Conclusion
Whole grain and cereal intake are inversely associated with type 2 diabetes. A higher consumption of whole grains or cereals can delay the occurrence of type 2 diabetes.
Acknowledgements
This study supported by the Supported Project University of Youth Talents Found of Anhui province (Department of Education Anhui Province, 2014).
Disclosure of conflict of interest
None.
References
- 1.Organization WH. Global status report on noncommunicable diseases 2014. 2015 doi: 10.1161/STROKEAHA.115.008097. [DOI] [PubMed]
- 2.Organization WH. Diabetes. 2015
- 3.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3:e442. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Center for Health Statistics and Information, MOH. An Analysis Report of National Health Services Survey in China, 2008. 2009:1–153.
- 5.Péronnet F, Meynier A, Sauvinet V, Normand S, Bourdon E, Mignault D, St-Pierre DH, Laville M, Rabasa-Lhoret R, Vinoy S. Plasma glucose kinetics and response of insulin and GIP following a cereal breakfast in female subjects: effect of starch digestibility. Eur J Clin Nutr. 2015;69:740–745. doi: 10.1038/ejcn.2015.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhou AL, Hergert N, Rompato G, Lefevre M. Whole grain oats improve insulin sensitivity and plasma cholesterol profile and modify gut microbiota composition in C57BL/6J mice. J Nutr. 2015;145:222–230. doi: 10.3945/jn.114.199778. [DOI] [PubMed] [Google Scholar]
- 7.Wu H, Flint AJ, Qi Q, van Dam RM, Sampson LA, Rimm EB, Holmes MD, Willett WC, Hu FB, Sun Q. Association between dietary whole grain intake and risk of mortality: two large prospective studies in US men and women. JAMA Intern Med. 2015;175:373–384. doi: 10.1001/jamainternmed.2014.6283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wirstrom T, Hilding A, Gu HF, Ostenson CG, Bjorklund A. Consumption of whole grain reduces risk of deteriorating glucose tolerance, including progression to prediabetes. Am J Clin Nutr. 2013;97:179–187. doi: 10.3945/ajcn.112.045583. [DOI] [PubMed] [Google Scholar]
- 9.Krishnan S, Rosenberg L, Singer M, Hu FB, Djousse L, Cupples LA, Palmer JR. Glycemic index, glycemic load, and cereal fiber intake and risk of type 2 diabetes in US black women. Arch Intern Med. 2007;167:2304–2309. doi: 10.1001/archinte.167.21.2304. [DOI] [PubMed] [Google Scholar]
- 10.Greenland S. Quantitative methods in the review of epidemiologic literature. Epidemiol Rev. 1987;9:1–30. doi: 10.1093/oxfordjournals.epirev.a036298. [DOI] [PubMed] [Google Scholar]
- 11.von Ruesten A, Feller S, Bergmann MM, Boeing H. Diet and risk of chronic diseases: results from the first 8 years of follow-up in the EPIC-potsdam study. Eur J Clin Nutr. 2013;67:412–419. doi: 10.1038/ejcn.2013.7. [DOI] [PubMed] [Google Scholar]
- 12.Yao B, Fang H, Xu W, Yan Y, Xu H, Liu Y, Mo M, Zhang H, Zhao Y. Dietary fiber intake and risk of type 2 diabetes: a dose-response analysis of prospective studies. Eur J Epidemiol. 2014;29:79–88. doi: 10.1007/s10654-013-9876-x. [DOI] [PubMed] [Google Scholar]
- 13.de Munter JS, Hu FB, Spiegelman D, Franz M, van Dam RM. Whole grain, bran, and germ intake and risk of type 2 diabetes: a prospective cohort study and systematic review. PLoS Med. 2007;4:e261. doi: 10.1371/journal.pmed.0040261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Parker ED, Liu S, Van Horn L, Tinker LF, Shikany JM, Eaton CB, Margolis KL. The association of whole grain consumption with incident type 2 diabetes: the women’s health initiative observational study. Ann Epidemiol. 2013;23:321–327. doi: 10.1016/j.annepidem.2013.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schulze MB, Schulz M, Heidemann C, Schienkiewitz A, Hoffmann K, Boeing H. Fiber and magnesium intake and incidence of type 2 diabetes: a prospective study and meta-analysis. Arch Intern Med. 2007;167:956–965. doi: 10.1001/archinte.167.9.956. [DOI] [PubMed] [Google Scholar]
- 16.Wannamethee SG, Whincup PH, Thomas MC, Sattar N. Associations between dietary fiber and inflammation, hepatic function, and risk of type 2 diabetes in older men: potential mechanisms for the benefits of fiber on diabetes risk. Diabetes Care. 2009;32:1823–1825. doi: 10.2337/dc09-0477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.He M, van Dam RM, Rimm E, Hu FB, Qi L. Whole-grain, cereal fiber, bran, and germ intake and the risks of all-cause and cardiovascular disease-specific mortality among women with type 2 diabetes mellitus. Circulation. 2010;121:2162–2168. doi: 10.1161/CIRCULATIONAHA.109.907360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Whincup PH, Donin AS. Cereal fibre and type 2 diabetes: time now for randomised controlled trials? Diabetologia. 2015;58:1383–5. doi: 10.1007/s00125-015-3644-2. [DOI] [PubMed] [Google Scholar]
- 19.Giacco R, Costabile G, Della Pepa G, Anniballi G, Griffo E, Mangione A, Cipriano P, Viscovo D, Clemente G, Landberg R, Pacini G, Rivellese AA, Riccardi G. A whole-grain cereal-based diet lowers postprandial plasma insulin and triglyceride levels in individuals with metabolic syndrome. Nutr Metab Cardiovasc Dis. 2014;24:837–844. doi: 10.1016/j.numecd.2014.01.007. [DOI] [PubMed] [Google Scholar]
- 20.Chanson-Rolle A, Meynier A, Aubin F, Lappi J, Poutanen K, Vinoy S, Braesco V. Systematic review and meta-analysis of human studies to support a quantitative recommendation for whole grain intake in relation to type 2 diabetes. PLoS One. 2015;10:e0131377. doi: 10.1371/journal.pone.0131377. [DOI] [PMC free article] [PubMed] [Google Scholar]


