Abstract
Despite a rapid increase in the use of anticancer immunotherapy, our understanding of the mechanisms of action and the patients’ responses remains limited. The discovery of immune inhibitory markers in the tumour microenvironment following immunotherapy should improve our understanding and might enable us to better apply combination therapies.
The advance of immunotherapy across the field of oncology in recent years has been remarkable, but a mechanistic understanding of the antitumour immune response — especially within the tumour micro-environment — remains in its relative infancy. Furthermore, although the breadth of responses across multiple tumour types has been noted, the fact that a minority of patients have objective responses to immune-based therapies is often overlooked. A recent publication by Gao and colleagues1 in Nature Medicine provides a detailed analysis of the immunological effects of ipilimumab in patients with prostate cancer, suggesting upregulation of the immune checkpoints programmed cell death ligand 1 (PD-L1) and V-type immunoglobulin domain-containing suppressor of T-cell activation (VISTA). These findings might provide guidance on how immune-based therapies can be optimized in patients with advanced solid tumours.
Prostate cancer presents a perplexing immunotherapeutic dilemma. A therapeutic cancer vaccine, sipuleucel-T, demonstrated an overall survival advantage in a phase III trial and an ability to mobilize immune cells to the tumour microenvironment in the neoadjuvant setting2,3. By contrast, immune checkpoint inhibitors (anti-PD-1 or anti-PD-L1 antibodies) have demonstrated modest success in small cohorts or — in the case of ipilimumab, an anti-CTLA4 therapy — no success in two phase III trials4–6. Nonetheless, in a study of patients with prostate cancer, Gao and colleagues report increased tumour infiltration with CD4+ and CD8+ T cells after treatment with ipilimumab, similar to that observed in bladder cancer and melanoma, in which this treatment has a better clinical track record1. Markers consistent with the presence of natural killer cells (granzyme B), macrophages (CD68+), and memory T cells (CD45RO+) were also increased in the tumours, suggesting a multilineage antitumour response. A broader analysis suggested that these findings were independent of androgen deprivation therapy (a standard of care for patients with prostate cancer) and consistent regardless of whether the patients had localized or metastatic disease.
In conjunction with the reported immune response in the tumour microenvironment, upregulation of PD-L1 was also observed. This upregulation could be predicted, based on previous data suggesting that immune infiltration of the tumour microenvironment might be accompanied by increased PD-L1 expression, leading to neutralization of the antitumour immune effect7. This mechanism could explain why the combination of ipilimumab and nivolumab has demonstrated greater efficacy in melanoma than ipilimumab alone8. Particularly provocative in the current study was the increased expression of a second immune checkpoint in the tumour micro-environment, VISTA, which is predominantly expressed on cells of a myeloid lineage9.
CD68+ macrophages nearly doubled in the tumour after treatment with ipilimumab from a median of ~20% to ~35% (P = 0.0001), and many of them expressed PD-L1 (29.4%) or VISTA (26.5%)1. Notably, only 2% of the CD68+ cells expressed both PD-L1 and VISTA. These data highlight the complex biology of an antitumour immune response that has multiple compensatory hurdles to overcome before clinically relevant responses could be observed. These data also suggest that altered expression of VISTA could be an important immunoregulatory mechanism in prostate cancer.
This analysis could also inform the clinical findings of the phase III study in chemotherapy-naive, metastatic castration-resistant prostate cancer that evaluated ipilimumab versus placebo4. The study did not yield an overall survival benefit, but it did demonstrate a progression-free survival advantage favouring ipilimumab (median 5.6 months versus 3.8 months, HR 0.67). Although toxicity might have been a mitigating factor affecting long-term outcomes, could the short-term clinical benefit have been overcome by compensatory immune mechanisms of regulation such as VISTA-positive macrophages?
“…VISTA could be an important immunoregulatory mechanism in prostate cancer.”
The effect of VISTA on the outcomes of past clinical trials in prostate cancer cannot be ascertained, but the report from Gao and colleagues1 has important implications for future studies. Firstly, and perhaps most importantly, these findings give a pause to the assumption that tumours that do not respond to PD-1 and/or PD-L1 inhibition are not immune-responsive — on the contrary, they might be responsive, but PD-1 and PD-L1 might not be the only relevant or sufficient targets. Secondly, and from a broader perspective, these data highlight the need for immunotherapy to be deployed as multi faceted platforms that can both mobilize immune cells to the tumour micro-environment (as is the case for ipilimumab and therapeutic vaccines) and then keep such cells functional once they get there (the role of microenvironment checkpoint inhibitors).
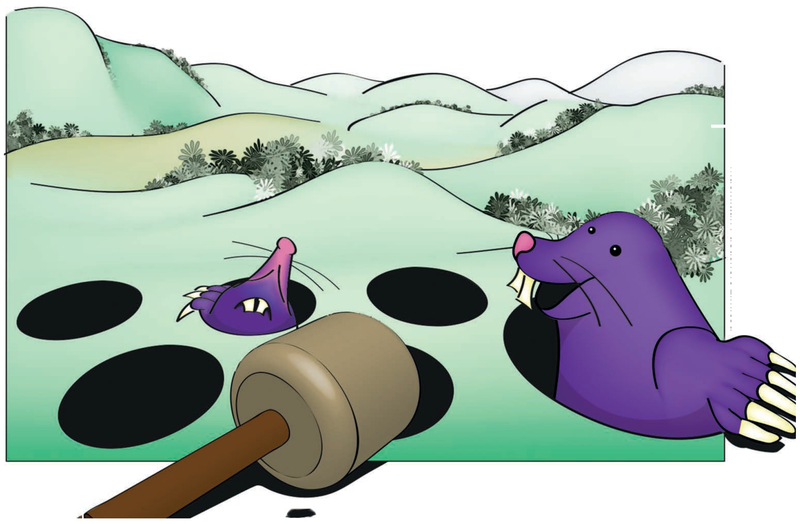
Perhaps the most important upshot of this study is that those working in the immunotherapy field must evaluate the effect of immunotherapies within the tumour microenvironment, in order to identify potentially relevant counter-regulatory or resistance mechanisms. The tumour microenvironment could present an immunological ‘whack-a-mole’ of sorts, whereby rolling mechanisms of immune compensation result in (possibly sequential) upregulation of multiple regulatory immune checkpoints that could hinder clinical benefit, even if the underlying immune-based therapy (in this case, ipilimumab) is effective at increasing immune recognition and mobilizing these cells to the tumour. Furthermore, emerging data suggest that, even within each patient, a heterogeneous immunological milieu might exist that differs from lesion to lesion within the same patient10. In this context, perhaps certain other checkpoints are more relevant in specific bone, lymph node, or visceral tumour microenvironments. Further studies, similar to that carried out by Gao and colleagues1, will be required to fully understand these points.
Gao and colleagues’ paper1 illustrates how far the field has progressed in a few short years, but also highlights how much remains undiscovered. Ipilimumab, despite failed phase III trials, is shown to mobilize immune cells to the tumour; regulatory mechanisms blunting its potential anti-tumour effects can be identified and targeted — anti-VISTA agents are in clinical development. However, important questions remain, including the ubiquity of VISTA expression across all men with prostate cancer and among patients with other cancers. Furthermore, whether any immune-based therapy that mobilizes T cells can induce VISTA expression as a regulatory mechanism, or whether this effect is specific to ipilimumab-based immune mobilization remains to be elucidated.
Finally, studies like this report from Gao et al.1 highlight the fact that clinical development of immunotherapy needs to move quickly into the combination phase. Although limited studies currently combine more than just one or two of these agents, these data illustrate the potential futility and missed opportunities when these agents are evaluated as single agents. Medical oncology might finally have the therapeutic tools to match the heterogeneity of cancer but, as these data show, we must not be shy in deploying them together in order to overcome this disease.
Figure 1.
Macmillan Publishers Limited.
Footnotes
Competing interests statement
The authors declare no competing interests.
References
- 1.Gao J et al. VISTA is an inhibitory immune checkpoint that is increased after ipilimumab therapy in patients with prostate cancer. Nat. Med 23, 551–555 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fong L et al. Activated lymphocyte recruitment into the tumor microenvironment following preoperative sipuleucel-T for localized prostate cancer. J. Natl Cancer Inst. 106, dju268 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kantoff PW et al. Sipuleucel-T immunotherapy for castration-resistant prostate cancer. N. Engl. J. Med 363, 411–422 (2010). [DOI] [PubMed] [Google Scholar]
- 4.Beer TM et al. Randomized, double-blind, Phase III trial of ipilimumab versus placebo in asymptomatic or minimally symptomatic patients with metastatic chemotherapy-naive castration-resistant prostate cancer. J. Clin. Oncol 35, 40–47 (2017). [DOI] [PubMed] [Google Scholar]
- 5.Graff JN et al. Early evidence of anti-PD-1 activity in enzalutamide-resistant prostate cancer. Oncotarget 7, 52810–52817 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kwon ED et al. Ipilimumab versus placebo after radiotherapy in patients with metastatic castration-resistant prostate cancer that had progressed after docetaxel chemotherapy (CA184–043): a multicentre, randomised, double-blind, phase 3 trial. Lancet Oncol. 15, 700–712 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Benci JL et al. Tumor interferon signaling regulates a multigenic resistance program to immune checkpoint blockade. Cell 167, 1540–1554.e12 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Larkin J et al. Combined nivolumab and ipilimumab or monotherapy in untreated melanoma. N. Engl. J. Med 373, 23–34 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nowak EC et al. Immunoregulatory functions of VISTA. Immunol. Rev 276, 66–79 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dhodapkar KM et al. Distinct dominant T-cell receptors with a tissue resident memory phenotype in individual melanoma metastases [abstract]. J. Clin. Oncol 35 (suppl 7S), 3 (2017). [Google Scholar]