Abstract
Purpose of review:
Many observational studies have demonstrated a survival benefit with home dialysis compared with in-center dialysis; however, results have been conflicting. The purpose of this review was to identify pitfalls and limitations in existing literature and examine the challenges of studying home and in-center dialysis populations.
Sources of information:
Original research articles were identified from MEDLINE using search terms “in-center hemodialysis,” “home hemodialysis,” “conventional hemodialysis,” “nocturnal hemodialysis,” and “short daily hemodialysis.”
Methods:
A focused review and critical appraisal of existing home versus in-center hemodialysis survival literature was conducted to identify potential causes for variability in the observed survival outcomes.
Key findings:
The controversy in existing literature stems from the challenges of randomizing patients to home versus in-center hemodialysis modalities, and therefore a reliance on observational comparisons for study. In many cases, these observational analyses have been limited by selection bias (variabilities in populations included, inclusion of both incident and prevalent cohorts, and variabilities in dialysis intensity), as well as residual confounding. Furthermore, the studies that do exist lack generalizability in many cases.
Limitations:
There are few randomized controlled trials examining the survival benefit of home versus in-center hemodialysis and existing observational studies are often limited by bias and reduced generalizability. These limitations comprise the body of this review.
Implications:
This review examines challenges surrounding survival comparisons with home versus in-center hemodialysis and identify important directions for future study.
Keywords: review, home dialysis, in-center dialysis, hemodialysis, survival
Abrégé
Objectif de la revue:
Plusieurs études observationnelles ont démontré que la dialyse à domicile présentait des avantages de survie comparativement à la dialyse en centre, mais les résultats sont contradictoires. L’étude visait à présenter les pièges et les limites de la littérature existante et à examiner les défis que représente l’étude de populations dialysées à domicile ou en centre.
Sources:
Les articles de recherche originaux ont été répertoriés dans MEDLINE à l’aide des termes suivants: in-center hemodialysis (hémodialyse en centre), home hemodialysis (hémodialyse à domicile), conventional hemodialysis (hémodialyse conventionnelle), nocturnal hemodialysis (hémodialyse nocturne) et short daily hemodialysis (hémodialyse quotidienne de courte durée).
Méthodologie:
Un examen ciblé et une évaluation critique de la littérature discutant de la survie selon la modalité de dialyse (à domicile ou en centre) ont été menés pour cibler les causes potentielles de variabilité dans les résultats observés pour la survie.
Principaux résultats:
Les divergences constatées dans la littérature existante découlent de la difficulté de répartir aléatoirement les patients selon la modalité de dialyse (à domicile ou en centre). Il faut, par conséquent, compter sur des comparaisons observationnelles pour l’étude. Dans plusieurs cas, les analyses observationnelles étaient limitées par des biais de sélection (variabilité dans les populations incluses, inclusion de cohortes à la fois incidentes et prévalentes, variabilité dans l’intensité de la dialyse), et des facteurs de confusion résiduels. Enfin, la généralisabilité des études existantes est bien souvent limitée.
Limites:
Peu d’essais cliniques à répartition aléatoire ont étudié les avantages sur la survie de la dialyse à domicile en comparaison avec la dialyse en centre De plus, les études observationnelles existantes sont souvent limitées par des biais ou une faible généralisabilité. Ces limites constituent l’essentiel de la discussion de la présente revue.
Conclusion:
Cette revue de la littérature examine les défis entourant les comparaisons entre l’hémodialyse à domicile ou en centre en regard des avantages sur la survie, et propose d’importantes orientations pour la recherche à venir.
What was known before?
Many earlier studies have demonstrated a survival benefit with home dialysis compared with in-center dialysis; however, results have been conflicting. Importantly, this narrative review appraises existing literature to identify causes for these discrepant results and provide commentary on existing survival conclusions.
What this adds?
The conflicting results with existing literature relates to the challenges of randomizing patients to home versus in-center hemodialysis modalities, and therefore a reliance on observational comparisons for study. As with all observational studies, in many cases, these analyses have been limited by selection bias and residual confounding.
Introduction
Dialysis options for eligible patients with end-stage kidney disease (ESKD) include peritoneal dialysis (PD) and hemodialysis (HD), performed either at home or at an institution (in-center). At the patient level, home dialysis has been associated with more flexibility in terms of scheduling and prescription, better quality of life, and lessened burden of transportation (ie, no need for transport to and from a dialysis center).1
Hemodialysis can be performed as conventional HD (usually 3 times weekly, 4 h/session), nocturnal hemodialysis (NHD) (usually 3-6 times weekly, 6-8 h/session), and short daily hemodialysis (SDHD) (usually 5-7 times weekly, 1.5-3 h/session), performed either in center or at home.2 Home HD may allow for more frequent or longer dialysis sessions that may not be possible in a hospital setting due to capacity constraints. Home HD and PD are felt by many to be equivalent with choice between the two ultimately distilling down to patient preference.
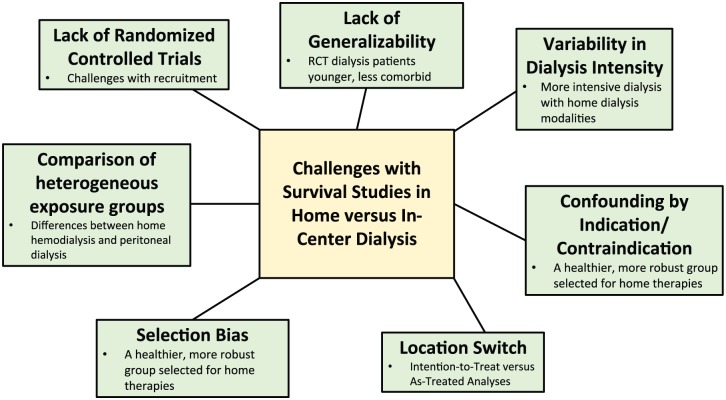
Although many observational studies have demonstrated a survival benefit with home dialysis compared with in-center dialysis, results have been conflicting. The cause for the discrepant results is likely multifactorial and presumably relates to the limitations of observational comparisons including treatment selection bias and residual confounding (see Figure 1). In this review, we will discuss the complexities and limitations surrounding survival comparisons with home versus in-center HD and identify important directions for future study.
Figure 1.
The Challenges with Survival Studies in Home versus In-Center Dialysis.
Note. RCT = randomized controlled trial.
Limitations of Existing Literature
Lack of Randomized Controlled Trials (RCTs)
Most survival comparisons for home versus in-center HD are based on observational studies. This stems from the challenges with randomizing patients to different locations. This is best demonstrated by the Frequent Hemodialysis Network (FHN) Nocturnal trial3 wherein patients were randomized to home NHD or conventional in-center HD. Enrollment was challenging with barriers to participation being patients’ unwillingness to be randomized to a strategy where there was only a 50% chance of receiving a home therapy.1 In response to low enrollment rates, after 1 year of study, the target sample size was accordingly decreased and a protocol revision was adopted in which all of the last 72 participants were home HD trained.3 Despite this, the FHN Nocturnal trial only achieved a maximum recruitment of approximately one-third of their original intent.3 Other major perceived barriers included lack of patient motivation and fear of self-cannulation.1 Another earlier attempt at an RCT comparing survival and quality of life outcomes for HD and PD was performed in the Netherlands in 2003. The trial was prematurely stopped due to low inclusion rates (only 38% of target sample size was achieved in over 3 years).4 Of the 735 patients eligible for enrolment, only 38 (5%) agreed to be randomized due to patient preference for one modality over another.4
Another challenge with RCTs is that home dialysis has been associated with relatively low mortality rates necessitating long patient follow-up or very large patient numbers to perform survival comparisons. One paper demonstrated low mortality rates in home dialysis cohorts (6, 4, and 5 patient deaths/100 patient-years for conventional HD, SDHD, and NHD, respectively).5 Likewise, a low mortality rate of 3 patient deaths/100 patient-years was demonstrated for patients in the conventional home HD group in a post hoc analysis of the FHN nocturnal trial.3,6 This therefore necessitates the use of composite or surrogate markers (eg, the use of left ventricular mass or a physical health composite score in the FHN nocturnal trial) as opposed to definitive ones.3
Although an RCT would be the ideal study design to explore differences related to dialysis locale free of bias, as evidenced by earlier attempts,3,4 achieving an adequate sample size to adequately power the study (especially in light of the low mortality event rates demonstrated in many earlier studies) would be nearly impossible.5
Bias and Confounding
Several observational studies have demonstrated a survival benefit with home HD compared with in-center HD.7-12 It is important to remember however that associations do not imply causality. It is unclear if the observed survival advantage with home dialysis reflects a true improvement in survival due to the location itself, or if it instead reflects the fact that the home and in-center populations differ in terms of other determinants of survival.
Variability in populations
It has been shown that there are significant differences between those patients selected for home therapies and those who are dialyzed in center. Patients on home HD tend to undergo more intensive dialysis,5 but are also younger, less comorbid, and more likely to be eligible for and subsequently undergo kidney transplantation.11 In addition, it has been shown that home dialysis populations generally have better social circumstances with more supports, higher socioeconomic status, and increased health literacy and motivation than their in-center counterparts. These factors are associated with better dialysis and medication adherence,13 which in turn are associated with lower mortality risk.14 An early study published in 1996 noted significantly improved survival in home HD patients compared with in-center HD patients (Relative Risk [RR] = 0.58, P = .03); however, when they studied a subgroup of patients selected for home HD but instead training for in-center self-care HD, there remained a 22% survival advantage compared with the in-center cohort who were not selected for home HD (RR = 0.78, P = .001). This likely reflects a healthier subset of patients chosen to undergo training for home HD.11 In addition, in France, older adults >75 years are preferentially offered assisted PD. Survival in this cohort was comparable to a similar cohort in the United Kingdom where most older patients are treated with in-center HD.15
Variability in incident and prevalent populations
Another potential source of confounding is the inclusion of both incident and prevalent dialysis populations in observational studies. It is known that there is a higher up-front mortality in the 120-day period following dialysis initiation.16 If the proportion of incident and prevalent patients differs between comparator groups (home vs in-center modalities), this can lead to an immortal time bias with prevalent patients already having survived the high risk period following dialysis initiation. In addition, residual kidney function can wane over time on dialysis, and given the known association of residual kidney function with survival,17 comparing incident and prevalent populations may confound results, with prevalent patients having less residual kidney function than incident comparators.
Variability in dialysis intensity
Finally, a significant bias in survival comparisons of home versus in-center dialysis is the fact that in the literature, in-center HD typically reflects conventional HD (usually 4 hours, 3 times weekly). Conversely, home HD is often treated as synonymous with intensive dialysis given that >50% of patients on a home modality perform >12 hours of dialysis weekly.5 Intensive dialysis has been shown to have a survival advantage compared with conventional dialysis,18,19 although results are conflicting.20 The potential reason for the improved patient survival with intensive therapies demonstrated in some observational studies is felt to relate to better fluid balance and improved solute removal. NHD (most often done at home) has been associated with a number of benefits including better control of intradialytic weight gain and blood pressure, and improved phosphate control.18 It is known that in prevalent HD patients, volume overload is associated with an increased risk of mortality,21 and thus the improved volume management with NHD may lend itself to a survival advantage. The improved solute clearance observed with NHD may also allow patients to liberalize their diets, thus improving nutrition.22 In addition, a more frequent dialysis schedule (short daily or frequent nocturnal) may mitigate the known mortality risk associated with a 2-day dialysis break with conventional thrice weekly HD (22.1 vs 18.0 deaths per 100 person-years on the day after the long interval vs all other days, P < .001).23
One attempt at an RCT randomized 9 home dialysis patients in a cross-over study to long (6-8 hours, 3 times weekly) home HD or short conventional in-center HD (3.5-4.5 hours, 3 times weekly) to assess impact on blood pressure.24 As above, the sample size was very limited for this trial and each patient served as their own control. Blood pressure was significantly higher in those undergoing conventional HD in center, which the authors attributed to the duration of dialysis, not the location.24
Informative Censoring
A major limitation with existing survival studies of home versus in-center dialysis is the challenge related to potential modality or location switching over time. Switching from a home to an in-center facility is common with one study demonstrating that 15% of daily home HD and 44% of PD patients changed to in-center conventional HD over a 5-year study period, with >80% of modality failures occurring in the first year after dialysis start.25 In the same study, 1% of daily home HD patients transitioned to PD and 25% of PD patients transitioned to home HD.25 Patients on a home therapy who develop a comorbid condition or have a deterioration in their functional capacity may no longer be able to dialyze at home. Censoring a patient’s survival time at the time of a modality switch could then represent informative censoring. For example, it is likely not appropriate to attribute a person’s death to an in-center dialysis modality if after being on a home therapy for a year they have a catastrophic stroke and die the first day after transitioning to a full care in-center dialysis location.
The issue of treating observational analyses in an “intention-to-treat” versus “as-treated” manner has been questioned in many earlier studies. As an example, a 2017 study comparing PD to HD in patients deemed eligible for either modality analyzed patients in an intention-to-treat fashion grouped by their initial dialysis modality, acknowledging that this would not adequately capture events related to modality switches and may lead to misclassification bias.26 Unlike in RCTs, however, in nonrandomized observational studies, an intention-to-treat analysis will only preserve preexisting selection bias between patients.27 The rationale often cited for using this analysis strategy is that it may provide information to physicians when discussing modality choice/location with patients who are starting dialysis, before knowledge of future modality switches is available.27 Conversely, a 2011 study performed an as-treated analysis of in-center conventional HD versus home conventional, SDHD, NHD, and PD,7 and analyzed patients according to the modality they were using at the time they experienced an event. This study may have been limited by the fact that patients changing modalities or location due to declining health status (eg, moving from home to in center) may have been destined to have a poor outcome that was independent of their current dialysis location and/or modality. Ideally, to avoid bias related to modality switch, both intention-to-treat and as-treated analyses should be performed. If these results are similar, then one can be reassured that this bias is likely minimal; however, any differences in results between the 2 analyses should be explored.
To account for potential confounding by indication/contraindication relating to modality/location switch, some studies have included a lag time wherein any events in the first 60 days after a modality/location switch are attributed to the preceding modality and/or location.4,5 Alternatively, in studies where the primary analysis was performed as an intention-to-treat, a second as-treated sensitivity analysis has been performed to confirm results.4 The implications of modality/location switching in intention-to-treat versus as-treated analyses is demonstrated by a 2003 RCT exploring HD versus PD wherein in the original intention-to-treat analysis, PD patients had a significantly better survival than HD patients in the first 4 years of dialysis treatment. Conversely, in an as-treated analysis of the same patients, there was no difference in survival between the 2 modalities.4
Lack of Generalizability
It is important to note that situational barriers to home dialysis (eg, inadequate housing, access to water, motivation, or family/social supports) may impact generalizability to those patients who are candidates for home dialysis.1 In fact, one recent study showed no survival advantage for PD versus in-center HD amongst patients who were deemed eligible for both modalities.26 In observational studies, individuals selected for home therapies are generally healthier and more robust than their in-center counterparts.11 In addition, not all centers may offer home HD and center size and experience may play a role on observed outcomes (as has been shown in literature surrounding PD).
Not only are patients eligible for home therapies systematically different from those who are dialyzed in-center, but earlier studies have highlighted differences between subgroups of dialysis patients who are willing to participate in RCTs. These include being a younger, less likely to smoke, less comorbid cohort who is less likely to be waitlisted for kidney transplant.28 An analysis of patients who ultimately underwent enrollment in the FHN Nocturnal trial demonstrated significant differences between the Canadian and US prevalent dialysis populations and study participants, with study participants more likely to be men, have shorter dialysis vintage, and be more likely to have a postsecondary education.1 This also leads to reduced generalizability of trial results.
Lessons Learned and Future Directions
Given the observed challenges with enrolling patients in RCTs to assess the effect of dialysis location (home vs in-center) on survival, well-designed observational studies may be the best available source of information. It may not be appropriate to combine all home dialysis prescriptions under one overarching “home therapy” umbrella as conventional HD, SDHD, NHD, and PD are quite heterogeneous dialysis modalities.
Although the inherent bias to initiate healthier, more robust patients on home therapies would best be mitigated with randomization, sophisticated modeling techniques to adjust for factors likely to bias patients toward a home therapy or make home dialysis contraindicated can be employed. Given the heterogeneity of the populations being studied, propensity score matching has been used to adjust for baseline differences in home versus in-center dialysis populations. As an example, in 2015, Suri et al25 used a propensity match score to compare home daily HD, in-center HD, and PD obtained using US Renal Data System (USRDS) data. Another modeling design used to adjust for potential confounding by indication is a main-effects marginal structural model using inverse probability of treatment and censoring weights to adjust for time-varying modality exposure and comorbid conditions.7 This has been used to examine potential outcomes of dialysis modality with weights that redistribute the population in a way that minimizes confounding, in the setting of home therapies, adjusting for comorbidities which may be barriers to home dialysis to minimize risk of selection bias. The concern is that if a particular comorbidity is caused by a specific dialysis modality, adjusting for that comorbidity would attenuate the effect of modality exposure. In a main-effects marginal structural model, weights remove associations between dialysis modality and preexisting comorbidities as well as comorbidities and prior modality exposure.7
Surrogate measures of health including transplant eligibility and functional status should be included in future study as a means of ensuring all patients in a cohort meet a minimum standard such that both home and in-center dialysis modalities are considered reasonable from a clinical perspective. Another comparator group that could be analyzed would be patients treated with self-care in center or those training for home dialysis as although these patients are treated at an institution, they are likely to be more similar to a home dialysis population.
Finally, while an RCT may be challenging in nations with established access to home dialysis, recruitment may be improved by conducting such a trial in a geographic location where home dialysis is not yet considered a standard of care.
Is There Still a Role for Survival Comparisons?
There is literature to support the fact that patients care more about their quality of life than how long they will live.29,30 Patients on maintenance dialysis have been shown to have significantly reduced quality of life—in one study comparable to that reported for metastatic cancer. A 2014 study addressed patient-identified research priorities for patients with ESKD on or near to starting dialysis. Out of 30 patient-reported concerns, only one related to the effects of dialysis modality, whereas most patient concerns related to quality of life factors including low energy, chronic itch, depression, poor sleep, and sexual dysfunction.29 In addition, in 2012, Morton et al demonstrated that patients on maintenance dialysis would be willing to give up 7 months of life expectancy to reduce the number of required hospital visits and 15 months of life expectancy to decrease their travel restrictions.30
If home dialysis allows people the ability to dialyze more hours per week than is possible with in-center dialysis, however, is longer dialysis truly a confounder or is this more so a reflection of what it means to dialyze at home? From a strictly physiologic perspective looking at dialysis location, one would need to adjust for differences in dialysis prescriptions between home and in-center patients. From a more holistic perspective, however, if we treat dialysis intensity as a feature of the home versus in-center exposure definition (intensive dialysis more likely to be possible with home but not in-center dialysis), then perhaps we should not be adjusting for dialysis intensity. If we adjust for dialysis time, given that most home patients do more than 12 hours of dialysis weekly, this could unfairly attenuate the survival advantage seen with home therapies, because generally these patients will not be on a conventional dialysis schedule. What matters more to patients? These questions remain.
Survival analyses will always have a role, but given the difficulties in demonstrating a clear survival advantage/disadvantage with one dialysis location versus another, it is unlikely that studies of survival differences are able to provide conclusive recommendations surrounding the optimal choice of therapy. In light of this, and the limitations with the available survival literature comparing home versus in-center dialysis therapies, perhaps more focus should be placed on qualitative studies addressing quality of life and other patient factors. Even if one dialysis location was consistently shown to result in a small survival advantage, it is not clear that this knowledge would significantly influence decision making as many patients may base their treatment decisions more on lifestyle preferences, for example, willingness to stay at home, reluctance to travel, and flexibility in dialysis scheduling.
Conclusion
Home dialysis therapies have been associated with more flexibility in terms of dialysis schedule and prescription, improved quality of life, and reduced costs. Home therapies have also been associated with an improvement in patient survival in most studies, but whether this is causative or simply a reflection of a healthier population being selected for home therapies remains unclear. To better delineate if home dialysis in and of itself leads to a physiologic change which impacts survival, well-constructed observational studies that account for treatment selection bias, residual confounding, and differences in dialysis prescription at home versus in center are required. To truly understand the relationship between dialysis location and survival, these factors must be addressed, a fact which may be easier said than done. In the interim, the importance of quality of life outcomes and other patient lifestyle factors should not be understated.
Footnotes
Ethics Approval and Consent to Participate: No ethics approval or consent to participate was required for this publication.
Consent for Publication: The authors have consented publication of this article.
Availability of Data and Materials: No additional data or materials are available for this review.
Author Contributions: All authors reviewed and approved the final manuscript.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: J.P. has received speaking honoraria from Baxter Healthcare, Amgen Canada, and DaVita Healthcare Partners and has consulting fees from Amgen, Boehringer Ingelheim Canada, Baxter Healthcare, Otsuka, Janssen Ortho Shire, and Takeda, as well as research support from Baxter Healthcare and salary support from Arbor Research Collaborative for Health. K.K.T. has received unrestricted grant funding from Astellas, Canada, and Otsuka, Canada, and has done consulting work for Otsuka and Astra Zeneca.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Pipkin M, Eggers PW, Larive B, et al. Recruitment and training for home hemodialysis: experience and lessons from the Nocturnal Dialysis Trial. Clin J Am Soc Nephrol. 2010;5(9):1614-1620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Pauly RP. Survival comparison between intensive hemodialysis and transplantation in the context of the existing literature surrounding nocturnal and short-daily hemodialysis. Nephrol Dial Transplant. 2013;28(1):44-47. [DOI] [PubMed] [Google Scholar]
- 3. Rocco MV, Lockridge RS, Jr, Beck GJ, et al. The effects of frequent nocturnal home hemodialysis: the frequent hemodialysis network nocturnal trial. Kidney Int. 2011;80(10):1080-1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Korevaar JC, Feith GW, Dekker FW, et al. Effect of starting with hemodialysis compared with peritoneal dialysis in patients new on dialysis treatment: a randomized controlled trial. Kidney Int. 2003;64(6):2222-2228. [DOI] [PubMed] [Google Scholar]
- 5. Tennankore KK, Na Y, Wald R, Chan CT, Perl J. Short daily-, nocturnal- and conventional-home hemodialysis have similar patient and treatment survival. Kidney Int. 2018;93(1):188-194. [DOI] [PubMed] [Google Scholar]
- 6. Rocco MV, Daugirdas JT, Greene T, et al. Long-term effects of frequent nocturnal hemodialysis on mortality: the Frequent Hemodialysis Network (FHN) Nocturnal Trial. Am J Kidney Dis. 2015;66(3):459-468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Marshall MR, Hawley CM, Kerr PG, Polkinghorne KR, Marshall RJ, Agar JW, McDonald SP. Home hemodialysis and mortality risk in Australian and New Zealand populations. Am J Kidney Dis. 2011;58(5):782-793. [DOI] [PubMed] [Google Scholar]
- 8. Marshall MR, Walker RC, Polkinghorne KR, Lynn KL. Survival on home dialysis in New Zealand. PLoS ONE. 2014;9(5):e96847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Nadeau-Fredette AC, Hawley CM, Pascoe EM, et al. An incident cohort study comparing survival on home hemodialysis and peritoneal dialysis (Australia and New Zealand dialysis and transplantation registry). Clin J Am Soc Nephrol. 2015;10(8):1397-1407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Weinhandl ED, Liu J, Gilbertson DT, Arneson TJ, Collins AJ. Survival in daily home hemodialysis and matched thrice-weekly in-center hemodialysis patients. J Am Soc Nephrol. 2012;23(5):895-904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Woods JD, Port FK, Stannard D, Blagg CR, Held PJ. Comparison of mortality with home hemodialysis and center hemodialysis: a national study. Kidney Int. 1996;49(5):1464-1470. [DOI] [PubMed] [Google Scholar]
- 12. Rydell H, Clyne N, Segelmark M. Home- or institutional hemodialysis?—a matched pair-cohort study comparing survival and some modifiable factors related to survival. Kidney Blood Press Res. 2016;41(4):392-401. [DOI] [PubMed] [Google Scholar]
- 13. Christensen AJ, Smith TW, Turner CW, Holman JM, Jr, Gregory MC. Type of hemodialysis and preference for behavioral involvement: interactive effects on adherence in end-stage renal disease. Health Psychol. 1990;9(2):225-236. [DOI] [PubMed] [Google Scholar]
- 14. Untas A, Thumma J, Rascle N, et al. The associations of social support and other psychosocial factors with mortality and quality of life in the dialysis outcomes and practice patterns study. Clin J Am Soc Nephrol. 2011;6(1):142-152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Brown EA, Wilkie M. Assisted peritoneal dialysis as an alternative to in-center hemodialysis. Clin J Am Soc Nephrol. 2016;11(9):1522-1524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Robinson BM, Zhang J, Morgenstern H, et al. Worldwide, mortality risk is high soon after initiation of hemodialysis. Kidney Int. 2014;85(1):158-165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Obi Y, Rhee CM, Mathew AT, et al. Residual kidney function decline and mortality in incident hemodialysis patients. J Am Soc Nephrol. 2016;27(12):3758-3768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lacson E, Jr, Xu J, Suri RS, et al. Survival with three-times weekly in-center nocturnal versus conventional hemodialysis. J Am Soc Nephrol. 2012;23(4):687-695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Nesrallah GE, Lindsay RM, Cuerden MS, et al. Intensive hemodialysis associates with improved survival compared with conventional hemodialysis. J Am Soc Nephrol. 2012;23(4):696-705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Marshall MR, Polkinghorne KR, Kerr PG, Hawley CM, Agar JW, McDonald SP. Intensive hemodialysis and mortality risk in Australian and New Zealand populations. Am J Kidney Dis. 2016;67(4):617-628. [DOI] [PubMed] [Google Scholar]
- 21. Kalantar-Zadeh K, Regidor DL, Kovesdy CP, et al. Fluid retention is associated with cardiovascular mortality in patients undergoing long-term hemodialysis. Circulation. 2009;119(5):671-679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ipema KJ, Struijk S, van der Velden A, et al. Nutritional status in nocturnal hemodialysis patients—a systematic review with meta-analysis. PLoS ONE. 2016;11(6):e0157621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Foley RN, Gilbertson DT, Murray T, Collins AJ. Long interdialytic interval and mortality among patients receiving hemodialysis. N Engl J Med. 2011;365(12):1099-1107. [DOI] [PubMed] [Google Scholar]
- 24. McGregor DO, Buttimore AL, Lynn KL, Nicholls MG, Jardine DL. A comparative study of blood pressure control with short in-center versus long home hemodialysis. Blood Purif. 2001;19(3):293-300. [DOI] [PubMed] [Google Scholar]
- 25. Suri RS, Li L, Nesrallah GE. The risk of hospitalization and modality failure with home dialysis. Kidney Int. 2015;88(2):360-368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Wong B, Ravani P, Oliver MJ, Holroyd-Leduc J, Venturato L, Garg AX, Quinn RR. Comparison of patient survival between hemodialysis and peritoneal dialysis among patients eligible for both modalities. Am J Kidney Dis. 2018;71(3):344-351. [DOI] [PubMed] [Google Scholar]
- 27. Vonesh EF, Schaubel DE, Hao W, Collins AJ. Statistical methods for comparing mortality among ESRD patients: examples of regional/international variations. Kidney Int. 2000;57:S19-S27. [Google Scholar]
- 28. Israni AK, Halpern SD, McFadden C, et al. Willingness of dialysis patients to participate in a randomized controlled trial of daily dialysis. Kidney Int. 2004;65(3):990-998. [DOI] [PubMed] [Google Scholar]
- 29. Manns B, Hemmelgarn B, Lillie E, et al. Setting research priorities for patients on or nearing dialysis. Clin J Am Soc Nephrol. 2014;9(10):1813-1821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Morton RL, Snelling P, Webster AC, et al. Factors influencing patient choice of dialysis versus conservative care to treat end-stage kidney disease. CMAJ. 2012;184(5):E277-E183. [DOI] [PMC free article] [PubMed] [Google Scholar]