Clinical indications for high tibial osteotomy (HTO) include patients with unicompartmental arthritis, patients with malalignment of the leg and ligament instability of the knee, and patients with complex deformities. Deformity of the knee results in an asymmetric load on 1 compartment and leads to degeneration of the joint.
The osteotomy realigns the anatomic axis of the knee and transfers the mechanical axis to the center of or lateral to the joint to reduce the medial stress, thus preventing progression of the medial arthritis.1 Satisfactory results are best achieved when the mechanical axis passes through the Fujisawa point (the lateral one-third of the lateral femorotibial compartment).5 Widening of a previously narrow joint space may lead to regression of the subchondral cysts and sclerosis if stress is sufficiently reduced,14,17 and the degenerative articular cartilage in the medial compartment may regenerate after surgery.9
Various models of HTO have been proposed since Jackson and Waugh8 introduced the concept in 1961. Coventry3 first popularized the HTO by using a lateral closed-wedge procedure proximal to the tibial tuberosity. Lateral closed and medial opening osteotomies are still the most common procedures. Less commonly used techniques for the management of axial deformities of the knee include dome osteotomies, chevron osteotomies, and callus distractions with external fixation. These procedures have a high success rate when appropriate correction has been obtained in a properly select patient.2 Excellent or good 10-year results were obtained in 70% of 51 knees in which a lateral closing-wedge osteotomy had been performed.6
Undercorrection or failure to maintain valgus alignment has been shown to be associated with failure of HTO.13 As cited in Tsuda et al,19 Sprenger and Doerzbacher reported 10-year outcomes of HTO showing that 90% of 41 knees that had retained a valgus alignment between 8° and 16° at 1 year had survived and functioned well, whereas 45% of 28 knees with <8° or >16° of valgus at 1 year had to be converted to a total knee arthroplasty. These results suggest that long-term joint survival can be predicted by the knee alignment in the early postoperative period. In addition, if further osteoarthritic changes have not occurred, recurrent varus alignment during the early postoperative phase might be correctable with revision realignment surgery, thus enhancing the long-term results.19 At the same time, some authors16 have found that an accurate correction of the knee deformity does not appear to be essential for pain relief, nor does the best correction gives the best results.
This case report describes the 5-year follow-up results of a patient who received a dome-shaped HTO with the TomoFix (Anatomical) Lateral High Tibia Plate (DePuy-Synthes) to correct a recurrent varus deformity as a result of a failed lateral closing-wedge HTO.
Methods
In 2009, a 37-year-old man presented to another institution with a 3-year history of right knee pain isolated to the medial compartment. His personal history revealed previous left knee surgery in his childhood, but he was without any pain or limitations in daily activities.
Standard weightbearing radiographs and 30° Schuss views of the right knee showed femorotibial osteoarthritis with medial joint space narrowing and varus alignment. He underwent simultaneous right knee arthroscopic debridement and closing-wedge HTO, stabilized with 3 staples and plaster immobilization. Initially, the patient was able to return to his daily life without using walking aids. Subsequently, he developed moderate pain around the patella and medial compartment of the knee, and he became unable to fully perform recreational activities. In 2011, the patient was referred to our institution because of persistent pain in the right knee.
Clinical Examination
The subjective pain intensity (full weightbearing position) was determined by means of a visual analog scale (VAS) line 100 mm in length: no pain, 0-4 mm; mild pain, 5-44 mm; moderate pain, 45-74 mm; severe pain, 75-100 mm. The range of passive motion (flexion/extension) was measured with a goniometer. To avoid the functional score deteriorating as the patient gets older (although the knee remains unchanged), we also used the Knee Society Knee Scoring System7 (Table 1).
TABLE 1.
Preoperative Clinical Examinationa
| Right Knee (Before Surgery) | Left Knee | |
|---|---|---|
| VAS (full weightbearing), mm | 89 (severe pain) | 11 (mild pain) |
| Range of passive motion: extension/flexion, deg | 10/100 | 0/120 |
| KSS (out of 100) | ||
| Knee rating (pain, ROM, stability) | 8 | 87 |
| Functional assessment (walking/stairs) | 30 | 100 |
aVAS, visual analog scale; KSS, Knee Scoring System; ROM, range of motion.
Radiological Assessment and Preoperative Planning
The radiological documentation comprised standard knee radiographs, including the Schuss view, which usually shows more advanced disease; a patellar axial view in 30° of flexion with the knee loaded in a single-legged stance; and a standing anteroposterior view on a long cassette (Figure 1). To obtain an adequate anteroposterior weightbearing view, the patient was instructed to place his weight on both legs with the patella facing forward. The measurements were calculated with the use of a picture archiving and communication system (PACS; Impax, v 6.6.1.4024; Agfa).
Figure 1.
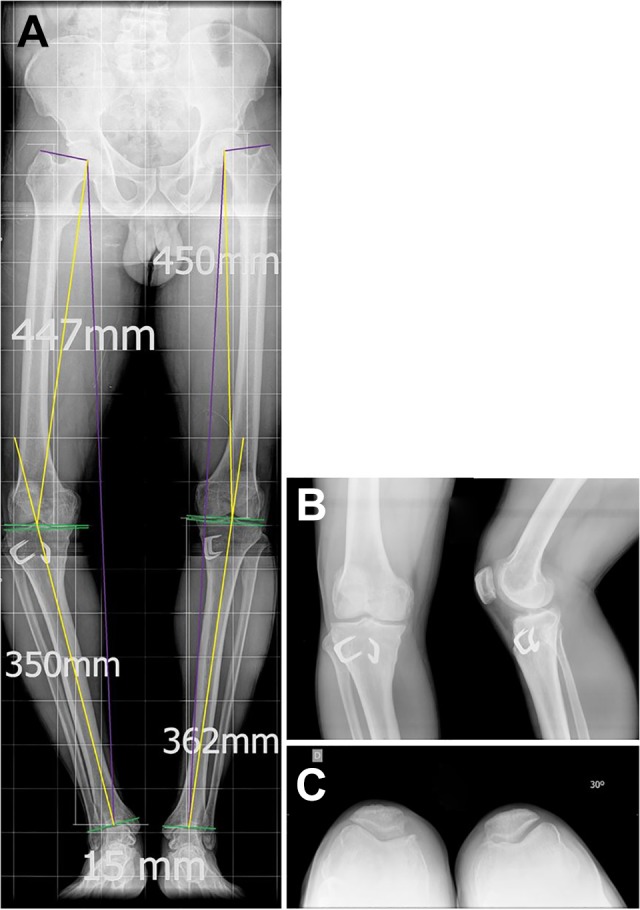
(A) Frontal plane weightbearing view. (B) Standard knee radiographs and (C) patellar axial view (30° of flexion). Right knee: mechanical tibiofemoral angle, –22° varus (femur, 8°; tibia, 14°); mechanical lateral distal femoral angle, 97°; mechanical medial proximal tibial angle, 77°. The midjoint line orientation is normal, and the joint line convergence angle is ±2°. Limb-length discrepancy: 15 mm.
The pre- and postoperative analysis consisted of determining the mechanical axis deviation and the hip-knee-ankle angle. The mechanical axis deviation was expressed in millimeters from standard values. The hip-knee-ankle angle was defined as the angle between a line from the center of the femoral head to the middle of the tibial plateau and a line from the middle of the tibial plateau to the center of the talus. Besides this, a line was drawn from the tip of the greater trochanter to the center of the femoral head to define hip joint orientation to the mechanical axis (Table 2). Only a radiograph of the loaded knee in the single-legged stance can provide accurate information of the conditions during gait when the joint is functionally stressed.10 We always do an overcorrection12 to compensate for the weakness of lateral muscles. The desired overcorrection was 3°.
TABLE 2.
Preoperative Values of Mechanical Leg Axes and Joint Angles in Frontal Planea
| Right Knee (Before Surgery) | Left Knee | |
|---|---|---|
| mLDFA, deg | 97 (↑) | 93 (↑) |
| mMPTA, deg | 77 (↓) | 85 (N) |
| MAD, mm | 72 | 23 |
| mTFA, deg | –22 varus (femur, 8; tibia, 14) | –8 varus (femur, ↑; tibia, N) |
| Limb length, mm | 797 | 812 |
| LLD, mm | 15 | |
| Hip orientation to mechanical axis | 98° | 94° |
aLLD, limb-length discrepancy; MAD, mechanical axis deviation; mLDFA, mechanical lateral distal femoral angle; mMPTA, mechanical medial proximal tibial angle; mTFA, mechanical tibiofemoral angle; N, normal.
Operative Technique
Surgery was performed under spinal anesthesia. Intravenous antibiotic and thromboembolic prophylaxis was used. The patient underwent surgery in a supine position with his leg extended on the surgical table and with a rotating image intensifier for anteroposterior and lateral views of the knee. The leg was drape-free, including the iliac crest, to be able to check alignment intraoperatively, even under image intensification. In these circumstances, a rod could be placed in a straight line between the center of the hip and the ankle. A sterile tourniquet was applied to the thigh as a precautionary measure, should excessive bleeding occur.
Operative Procedure
Prior to planned dome osteotomy, a diagnostic knee joint arthroscopy was made under the same anesthesia in standard technique via the anterolateral portal. The previously debrided medial meniscus was found to be slightly fibrillated, and the cartilage fibrillation of the medial femorotibial compartment was classified as grade II/III according to the Outerbridge classification system.4 The patellofemoral and lateral femorotibial joint surfaces appeared normal, confirming a suitable indication for realignment osteotomy.
As the first step, we made an incision laterally over the fibula, between the middle and lower third, taking care to not disturb the peroneal nerve and vein.10 The amount of fibula removed was proportional to the amount of correction planned. As the patient had a residual femoral varus of the left limb and normal tibial values (mechanical lateral distal femoral angle [mLDFA]: ↑ / mechanical medial proximal tibial angle [mMPTA]: normal), we decided to correct only the tibial varus of the right limb (approximately 14°) since the mLDFA values of both limbs were quite similar. This attitude allows balancing the knee and also obtaining axial correction. Therefore, in a tibial varus deformity of 14°, we removed 17 mm of fibula (14° plus 3° for overcorrection).
Subsequently, the tibial osteotomy could be performed easily through a midline vertical incision extending distally about 12 cm from the lower pole of the patella. The knee was flexed to 90°, the patellar tendon cleared, and the periosteum and muscles stripped from the upper tibia, passing bone levers in contact with the bone to protect posterior structures.16 A curved line was then marked on the bone just above the tibial tuberosity with a curved osteotome, adapted to the size of the tibia, which has a safe zone for the patellar tendon (Figure 2).
Figure 2.

Curved osteotome with a safe zone for patellar tendon.
A series of 2.5-mm drill holes were made along this line (just penetrating the posterior cortex). Curved Hohmann retractors were used to ensure complete exposure and protection of posterior neurovascular structures. Two thin Steinmann pins were inserted parallel to each other on either side of the osteotomy site to help define the angular correction. The osteotomy was then completed with a 15-mm osteotome, and after this, it could be rotated until the marker wires subtended the desired angle (17° in this case). It is important to always verify that there is no tibial slope changes and intraoperative assessment of knee extension. The distal tibia was brought forward approximately 10 mm to improve patellar pain.10 At this point, it is highly recommended to check if the limb alignment is as intended under fluoroscopy control. In normal circumstances, the new weightbearing line should now intersect with the tangent to the tibial plateau by 62% of the lateral compartment at the Fujisawa point.5
In this patient, the new weightbearing line was adjusted by the same level of the left knee, about 25% in the medial compartment, in the precise point that both legs reached the same length (as checked during surgery). The final position was then secured with an angular stable plate. We used the TomoFix lateral high tibial plate, which is precontoured to fit the anatomy of the lateral proximal tibia in a right-specific design (Figure 3).
Figure 3.
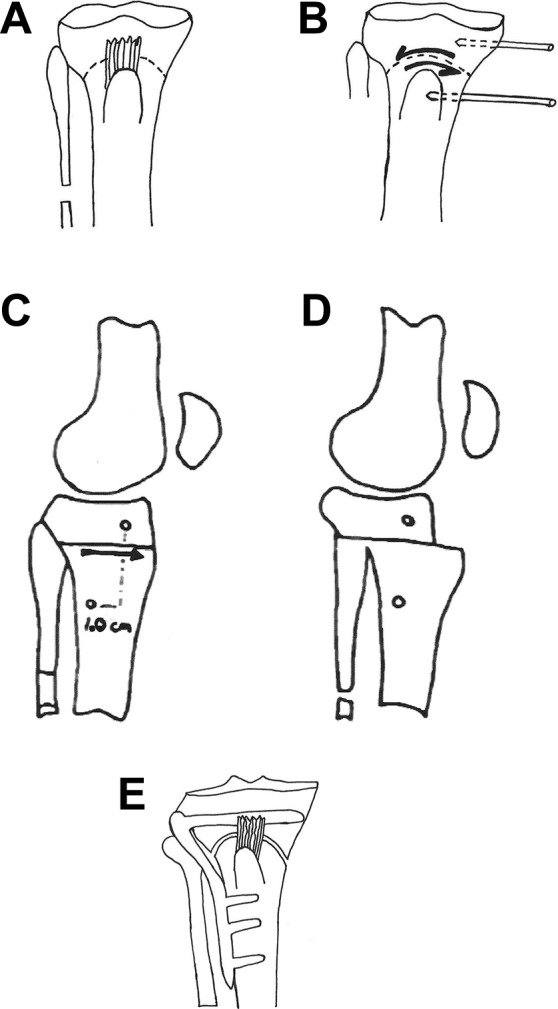
Diagram explaining the main steps of the surgery. (A) Series of 2.5-mm drill holes marked on a curved line above the tibial tuberosity. (B) Two Steinmann pins inserted on either side of the osteotomy to define angular correction. (C/D) Sagittal view: the distal tibia brought forward approximately 10 mm. (E) When desired angle is achieved, the TomoFix plate fix fragments are applied under compression.
In dome HTO, the prevention of secondary loss of correction by poor stability is essential. Because of this, it is recommended to insert the screws as close as possible to the osteotomy. Image intensifier radiographs of the knee in 2 planes are taken for documentation before the subcutaneous soft tissue and skin are closed.
The soft tissue and skin must be closed with great accuracy to ensure sufficient implant cover. Suction drainage is not usually necessary; however, an overflow drainage that exists proximally should be used. Elastic banding of the leg is completed before the patient leaves the operating room.
Postoperative Management
Cryotherapy was begun immediately after the operation. The bandage was changed on the first postoperative day to assess the soft tissue condition. Ambulation with underarm crutches began on the first postoperative day and continued for 4 weeks. However, active flexion was encouraged once the wound had healed. One month after the procedure, partial weightbearing of approximately 20 kg (Figure 4) was started. In weeks 5 to 6, weightbearing was increased, and full weightbearing was permitted in the seventh postoperative week.
Figure 4.

Radiograph: (A) anteroposterior, (B) lateral, and (C) axial postoperative views at 4 weeks.
Results
In this 5-year follow-up study, the VAS score for pain in the right knee improved from severe to mild (15 of 100 mm). The range of passive motion also improved its previous limits of flexion contracture and extension lag to increase to values similar to the contralateral knee (flexion/extension, 0°/120°). Similarly, the Knee Scoring System showed a significant upward trend on both knee clinical rating and functional outcome to peak at 82 of 100 points and 100 of 100 points, respectively (Table 3).
TABLE 3.
Postoperative (5-Year) Clinical Examinationa
| Right Knee (After Surgery) | Left Knee | |
|---|---|---|
| VAS: full weightbearing, mm | 15 (mild pain) | 12 (mild pain) |
| Range of passive motion: extension/flexion, deg | 0/120 | 0/120 |
| KSS (out of 100) | ||
| Knee rating (pain, ROM, stability) | 82 | 87 |
| Functional assessment (walking/stairs) | 100 | 100 |
aVAS, visual analog scale; KSS, Knee Scoring System; ROM, range of motion.
During the follow-up period, the patient did not mention complaints related to the lateral implant. Moreover, he did not report any peroneal nerve–related injuries or weakness of the extensor hallucis longus. The medial approach was not chosen, as it was necessary to remove the retained staples and this would have involved an additional skin incision. The alignment was measured by using a full weightbearing long-standing anteroposterior radiograph of the lower extremity (Figure 5).
Figure 5.
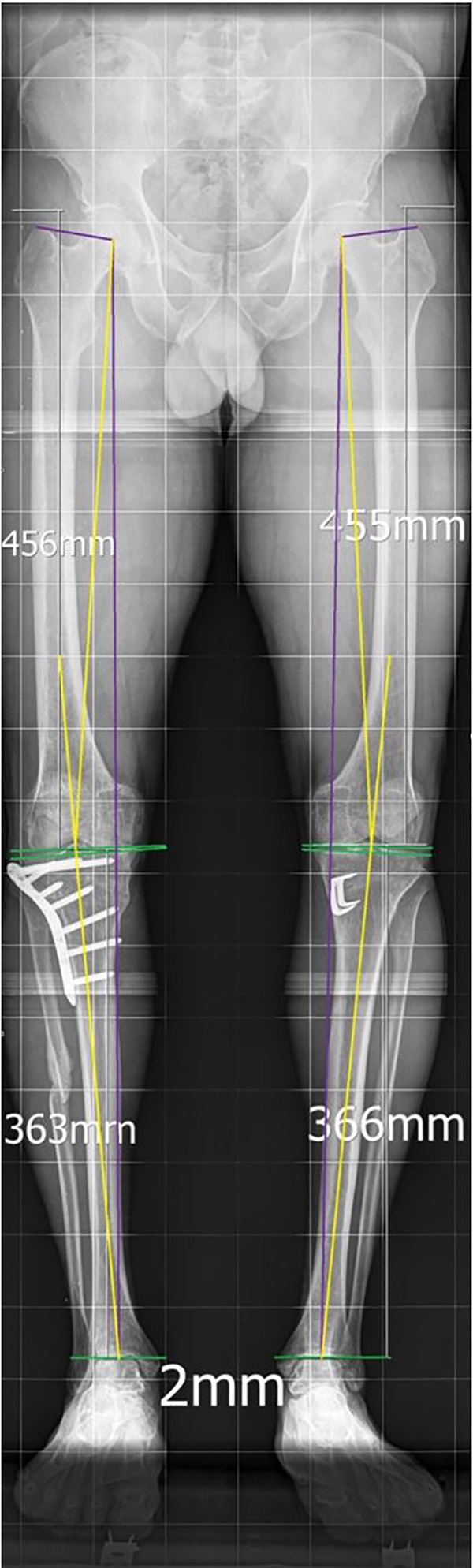
Full weightbearing long-standing anteroposterior radiograph of the lower extremity postoperatively. Right knee: mechanical tibiofemoral angle, –8° varus; mechanical lateral distal femoral angle, 95°; mechanical medial proximal tibial angle, 90°. The midjoint line orientation is normal, and the joint line convergence angle is ±1°. Limb-length discrepancy: 2 mm.
The aims of correction were a mechanical tibiofemoral angle of –8° varus, equal to the left knee, as well as an adjusted limb-length difference. Therefore, the tibial varus correction angle was 14° to reach –8° of residual femoral varus of the left knee. The joint-related angles were as follows: preoperatively—mLDFA, 97°; mMPTA, 77°; postoperatively—mLDFA, 95°; mMPTA, 90°. The limb-length difference was reduced from 15 mm to 2 mm (Table 4).
TABLE 4.
Postoperative Values of Mechanical Leg Axes and Joint Angles in Frontal Planea
| Right Knee (After Surgery) | Left Knee | |
|---|---|---|
| mLDFA, deg | 95 (↑) | 93 (↑) |
| mMPTA, deg | 90 (N) | 89 (N) |
| MAD, mm | 23 | 23 |
| mTFA, deg | –8 (varus) | –8 (varus) |
| Limb length, mm | 819 | 821 |
| LLD, mm | 2 | |
| Hip orientation to mechanical axis, deg | 96 | 94 |
aLLD, limb-length discrepancy; MAD mechanical axis deviation; mLDFA, mechanical lateral distal femoral angle; mMPTA, mechanical medial proximal tibial angle; mTFA, mechanical tibiofemoral angle; N, normal.
After a postoperative period of 5 years, we can report good relief of pain and improved knee function. No delayed consolidation, recurrence of deformity, or osteonecrosis was observed.
Discussion
There are few reports of revision of a failed HTO without conversion to arthroplasty.19 Despite not introducing a technical innovation, this case report is, to our knowledge, original in that it describes a revision HTO with a dome-type technique to treat the failure of a primary closed-wedge HTO in a young patient. This may challenge some paradigmata and present an alternative to total knee arthroplasty in active young patients. In addition, patient clinical and radiological examination did not indicate progression to tricompartmental arthrosis. However, the metaphysis of a long bone is the region of best healing capacity, and with a healthy young person who did not smoke, the risk of osteonecrosis after previous corrective surgery was considered acceptable.
Preoperative values of mechanical leg axes and joint angles showed a severe right knee varus with an elevated mLDFA (femoral varus deformity), decreased mMPTA (tibial varus deformity), and normal mid–joint line orientation. The contralateral limb presented a left knee varus with high mLDFA (femoral varus deformity), normal mMPTA, and approximately normal joint line converge angle.
If our first objective was only to correct the mechanical axis deviation and match its postoperative values to intersect the tibial plateau at 62% of the lateral compartment (Fujisawa point), we would have considered performing a double osteotomy on the right side: lateral closed-wedge distal femoral osteotomy and possibly a medial open-wedge HTO. However, these procedures would not have restored limb-length difference to normal values. Limb-length inequality of 10 mm or more leads to an asymmetric increase in muscle group activity and lateral imbalance in the erect posture and future chondral damage with arthrosis progression as a result of greater stress at the articulating surfaces.
Based on these conditions, it was decided to correct only the right-side tibial varus deformity (14° varus). Different surgical options were considered, such as medial open-wedge HTO or dome-shaped HTO. Originally, the dome HTO technique was described for large corrections (eg, >18 to 20 mm opening or closing HTO or angle of correction >20°). Both surgical options would ensure minimal tibial slope changes if performed correctly. In the open-wedge technique, we would have to consider that a gap width of 13 mm or more required harvesting and transplantation of cancellous bone graft from the iliac crest. This technique also includes an additional medial incision and for severe deformities, there is a risk of disrupting the lateral hinge because of the wide correction angle. However, in dome-shaped HTO, there is a good bone-on-bone contact area that favors faster bone healing, and no bone graft is needed. Besides, this technique has other advantages: it provides accurate angular corrections18 and also corrects both patellofemoral and medial compartment diseases. Because the osteotomy is performed proximal to the insertion of the deep collateral ligament when the tibia is brought into valgus, this ligament is effectively lengthened, and the knee is stable on weightbearing.10
In addition, it is well documented that when forces are eliminated across a joint and when weightbearing surfaces are increased, the joint may regenerate.10 As the cartilage regenerates, the knee becomes stable in flexion.10 When the tibial tubercle is bought forward, the force pressing the patella against the femur is effectively reduced.
Many complications in HTO partly depend on the fixation technique. The application of angular stable plate fixators (TomoFix plate) offers good potential to prevent both uniplanar and multiplanar postoperative deformities.11 The bending forces are distributed over a long plate length distance during axial loading, and this permits hinge-like stability of the osteotomy. These principles decrease anterior tibial collapse and also permit having none or minor effects on the tibial slope changes.11,15
Conclusion
The current study has shown the effectiveness of a dome-type HTO to correct a previously failed closed-wedge HTO in a young active patient with a severe varus right knee malalignment. We also demonstrated that limb-length difference adjustment and matching mechanical axes of both legs could achieve a high level of pain relief and knee function, even though a physiological varus deformity remained.
Acknowledgment
The authors thank the José de Mello Saúde Library, and Alberto Monteiro and the Saint Francis Xavier Hospital Library (Lisbon, Portugal) for their constant support.
Footnotes
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Chiang H, Hsu HC, Jiang CC. Dome-shaped high tibial osteotomy: a long-term follow-up study. J Formos Med Assoc. 2006;105(3):214–219. [DOI] [PubMed] [Google Scholar]
- 2. Coventry MB, Ilstrup DM, Wallrichs SL. Proximal tibial osteotomy: a critical long-term study of eighty-seven cases. J Bone Joint Surg Am. 1993;75(2):196–201. [DOI] [PubMed] [Google Scholar]
- 3. Coventry MB. Osteotomy of the upper portion of the tibia for degenerative arthritis of the knee: a preliminary report. J Bone Joint Surg Am. 1965;47:984–990. [PubMed] [Google Scholar]
- 4. Dougados M, Ayral X, Listrat V, et al. The SFA system for assessing articular cartilage lesions at arthroscopy of the knee. Arthroscopy. 1994;10(1):69–77. [DOI] [PubMed] [Google Scholar]
- 5. Fujisawa Y, Masuhara K, Shiomi S. The effect of high tibial osteotomy on osteoarthritis of the knee: an arthroscopic study of 54 knee joints. Orthop Clin North Am. 1979;10(3):585–608. [PubMed] [Google Scholar]
- 6. Holden DL, James SL, Larson RL, Slocum DB. Proximal tibial osteotomy in patients who are fifty years old or less: a long-term follow-up study. J Bone Joint Surg Am. 1988;70(7):977–982. [PubMed] [Google Scholar]
- 7. Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society Clinical Rating System. Clin Orthop Relat Res. 1989;248:13–14. [PubMed] [Google Scholar]
- 8. Jackson JP, Waugh W. Tibial osteotomy for osteoarthritis of the knee. J Bone Joint Surg Br. 1961;43:746–751. [DOI] [PubMed] [Google Scholar]
- 9. Koshino T, Wada S, Ara Y, Saito T. Regeneration of degenerated articular cartilage after high tibial valgus osteotomy for medial compartmental osteoarthritis of the knee. Knee. 2003;10(3):229–236. [DOI] [PubMed] [Google Scholar]
- 10. Krempen JF, Silver RA. Experience with the Maquet barrel-vault osteotomy. Clin Orthop Relat Res. 1982;168:86–96. [PubMed] [Google Scholar]
- 11. Levigne Ch, Bonnin M. Ostéotomie tibiale de valgisation pour arthrose femoro-tibiale interne In: Dejour H, Neyret Ph, eds. 7èmes journees lyonnaises de chirurgie du genou. Lyon, France: Hopital Lyon-Sud; 1991:142–168. [Google Scholar]
- 12. Maquet P. Valgus osteotomy for osteoarthritis of the knee. Clin Orthop Relat Res. 1976;120:143–148. [PubMed] [Google Scholar]
- 13. Naudie D, Bourne RB, Rorabeck CH, Bourne TJ. The Insall Award. Survivorship of the high tibial valgus osteotomy: a 10-to-22-year followup study. Clin Orthop Relat Res. 1999;367:18–27. [PubMed] [Google Scholar]
- 14. Pauwels F. Short survey of mechanical stress of bone and its importance for the functional adaptation. Z Orthop Ihre Grenzgeb. 1973;111:681–705. [PubMed] [Google Scholar]
- 15. Staubli AE. Principles of angular stable fixators In: Lobenhoffer P, Van Heerwaarden R, Staubli A, Jakob R, eds. Osteotomies Around the Knee. New York, NY: Thieme; 2008:233–239. [Google Scholar]
- 16. Sundaram NA, Hallett JP, Sullivan MF. Dome osteotomy of the tibia for osteoarthritis of the knee. J Bone Joint Surg Br. 1986;68(5):782–786. [DOI] [PubMed] [Google Scholar]
- 17. Takahashi S, Tomihisa K, Saito T. Decrease of osteosclerosis in subchondral bone of medial compartmental osteoarthritic knee seven to nineteen years after high tibial valgus osteotomy. Bull Hosp Jt Dis. 2002. –2003;61:58–62. [PubMed] [Google Scholar]
- 18. Takahashi T, Wada Y, Tanaka M, et al. Dome-shaped proximal tibial osteotomy using percutaneous drilling for osteoarthritis of the knee. Arch Orthop Trauma Surg. 2000;120(1-2):32–37. [DOI] [PubMed] [Google Scholar]
- 19. Tsuda E, Ishibashi Y, Sasaki K, Sato H, Toh S. Opening-wedge osteotomy for revision of failed closing-wedge high tibial osteotomy: a case report. J Bone Joint Surg Am. 2004;86(9):2045–2049. [DOI] [PubMed] [Google Scholar]


