Abstract
Objectives
Patients suitable for radical chemoradiotherapy for lung cancer routinely have radiotherapy (planning) volumes based on positron emission tomography (PET)-computed tomography (CT) imaging alone. Endobronchial ultrasound (EBUS)-guided transbronchial needle aspiration (TBNA) can identify PET-occult malignancy and benign PET-avid regions. We investigated the impact of EBUS-TBNA on curative-intent radiotherapy in non-small cell lung cancer (NSCLC).
Methods
A prospective multicentre trial was undertaken, investigating the impact of systematic EBUS-TBNA in addition to PET-CT for patients considered for radical chemoradiotherapy with NSCLC. A subset analysis of patients with discordant findings between PET-CT and EBUS-TBNA was performed. Radiotherapy plans investigated tumour coverage and dose to critical organs at risk (OARs) using PET-CT alone in comparison to PET-CT and EBUS-TBNA.
Results
Of 30 patients enrolled, 10 had discordant findings between PET-CT and EBUS-TBNA. EBUS-TBNA-derived plans allowed for reduction in dose to OARs in patients downstaged by EBUS-TBNA, and reduced the risk of geographic miss in treating PET-occult disease in four patients where EBUS-TBNA identified malignant involvement of PET-negative lymphadenopathy. With the addition of EBUS-TBNA to radiotherapy planning, reductions were noted of 5.7%, 3.7% and 12.5% for the risks of symptomatic pneumonitis, mean heart dose and mean oesophageal dose, respectively.
Conclusions
This study demonstrates for the first time that systematic EBUS-TBNA prior to radical-intent radiotherapy significantly improves coverage of subclinical disease through detection of PET-occult metastases. Identification of false-positive lymph node involvement in highly selected cases may reduce radiation dose to critical structures, and risk of organ toxicity.
Short abstract
Systematic EBUS-TBNA can identify areas of PET-occult malignancy, improving tumour coverage with radiation, and identify benign nodal regions that are PET positive, which may lead to reduced dose to critical structures such as heart, lung and spinal cord http://bit.ly/2QP42et
Introduction
Mediastinal nodal sampling or comprehensive nodal staging at time of surgery is standard of care for lung cancer patients undergoing surgical resection [1]. However, many patients undergoing radical chemoradiotherapy will have decisions relating to treatment volumes dictated by noninvasive radiological findings such as positron emission tomography (PET)-computed tomography (CT), occasionally coupled with limited exploration and biopsy of select lymph nodes. This disparity may influence the efficacy of radical interventions and their interpretation in clinical practice and clinical trials, as it is documented in several surgical series that up to 21.6% of patients with radiologically negative mediastinum will have pathological involvement (N2 disease, particularly with central tumours) [2].
Despite clear benefits of PET-CT in pre-operative staging, false-negative rates range from 6% to 13% depending on nodal size in stage III patients [3]; previous studies in both operative [4] and clinical stage III non-small cell lung cancer (NSCLC) cohorts [3, 5] have clearly demonstrated that systematic lymph node staging with endobronchial ultrasound (EBUS)-guided transbronchial needle aspiration (TBNA) can improve staging information in conjunction with PET. PET-occult metastases confer significant risk of subsequent treatment failure due to suboptimal gross tumour volume (GTV) delineation in radiotherapy planning. Conversely, false-positive nodal uptake on PET-CT may lead to increased treated volumes with potential increases in acute and long-term radiation toxicity or dose reduction.
To date, few studies have explored systematic mediastinal staging for patients with locally advanced NSCLC [3, 5]. In many institutions, the use of endoscopic techniques targets a specific node or region of concern. The current study had two main aims. First, we aimed to examine the impact on radiotherapy planning for 1) PET-planned radiotherapy versus 2) radiotherapy planned through both PET and EBUS-TBNA. This comparison evaluated the dose delivered to the tumour and additional margin accounting for set-up and movement, described as the planning target volume (PTV). Secondly, we examined the influence on theoretical risks of toxicity to critical organs (lungs, spinal cord, oesophagus and heart) based on dose–volume histograms when using EBUS-TBNA and PET compared with PET only.
Materials and methods
This pre-specified analysis included patients from a multicentre prospective observational cohort study [5] who had changes in NSCLC staging based on systematic staging with EBUS-TBNA in addition to PET-CT. The trial was approved by the Melbourne Health Institutional Review Board; all patients provided written informed consent. Patients from this cohort with discordant findings between PET-CT and EBUS-TBNA were identified. The details pertaining to the acquisition of PET-CT and EBUS-TBNA techniques have been previously described [5]. PET-CT scans were carried out in three different centres. No attempt was made to statistically analyse differences in standardised uptake value (SUV) between the primary and node positive/negative regions, due to the expected variances that may occur between institutions [6].
EBUS was performed in a systematic fashion, sampling any identified lymph nodes ≥6 mm in diameter, regardless of sonographic finding, in stations 2R/L, 4R/L, 7, 10R/L and 11R/L. To assure the quality of the aspirations, rapid on-site cytological examination was performed for each TBNA aspirate. Patients were EBUS-TBNA negative for a particular nodal station if the nodal biopsy from that particular echelon did not confirm malignancy (i.e. was benign or inflammatory). In discordant cases, PET-CT imaging underwent independent blinded review to confirm findings from the original PET report. Positive nodes were classified as those demonstrating 2-fluoro-2-deoxy-d-glucose (FDG) uptake greater than mediastinal blood pool uptake. Due to the multicentre acquisition of PET, no direct SUV comparisons were made. A priori analysis was performed to determine the dosimetric impact based on discordance. Where a greater extent of mediastinal lymph node involvement was indicated by EBUS-TBNA, radiotherapy plans incorporated this information. For negative EBUS-TBNA results, planning was undertaken on the basis of the PET alone (i.e. treatment fields were not amended based on the potential for downstaging).
Treatment planning
All patients had PET-CT planning scans or PET-CT fused with their 4D-CT (i.e. respiratory-correlated) simulation scan. Two intensity-modulated radiotherapy (IMRT) treatment plans were created to deliver 60 Gray (Gy) to the primary tumour and involved mediastinal nodes, as identified using 1) PET only or 2) both EBUS-TBNA and PET. Using the 4D maximum intensity projection image, GTV was outlined, with an additional internal target volume (ITV) margin to account for movement, and a 5-mm ITV to clinical target volume (CTV) margin (accounting for microscopic spread). A further 10-mm CTV to PTV expansion was added to account for set-up uncertainties. Volumes were delineated by experienced radiation oncologists and peer reviewed prior to planning. Standard organs at risk (OARs) including spinal cord, lungs, heart and oesophagus were contoured. IMRT plans were carried out by a single planner using the Eclipse treatment planning system with analytical anisotropic dose calculation algorithm (V13.6; Varian Medical Systems, Palo Alto, CA, USA).
Tumour and OAR doses were compared between the plans created on the PET-only or EBUS-TBNA combined with PET target volumes. Mean oesophageal and mean heart doses and normal tissue complication probability (NTCP) for symptomatic radiation pneumonitis were computed for patients with EBUS-negative/PET-positive nodal regions, to determine potential treatment detriment in the absence of EBUS-TBNA staging.
Results
30 patients underwent systematic EBUS-TBNA and PET-CT imaging. 20 patients (67%) had concordant findings; 10 had discordant findings, with four upstaged and six downstaged with respect to extent of lymph node involvement [5]. The median (range) SUV maximum of the primary tumour in this group with discordant findings was 11.1 (5.0–25.0). The key characteristics of these 10 patients with discordant findings are summarised in table 1.
TABLE 1.
Patient demographics and staging information
| Patient | Site | Pathology | EBUS-sampled stations | Stations sampled n | EBUS positive | EBUS negative | Discrepant sites# | |
| Upstaged | 1 | RLL | Adenocarcinoma | 7, 4R | 2 | 7, 4R | None | 4R |
| 2 | RUL | NSCLC | Pre-carinal, 7, 2R | 3 | Pre-carinal | 7, 2R | 4R | |
| 3 | Left hilum | Squamous | 7, LLL, 4L | 3 | 7, LLL | 4L | 7 | |
| 4 | RUL | Adenocarcinoma | 4R, 7, 11R | 3 | 7, 11R | 4R | 7 | |
| Downstaged | 5 | RLL | Squamous | 4R, 7 | 2 | 7 | 4R | 2R, 4R |
| 6 | RLL | Squamous | 4L, 2R, 4R, 2L, 7, 11R | 6 | 7, 11R | 4L, 2R, 4R, 2L | 2L, 4L, 2R, 4R | |
| 7 | RLL | NSCLC | 4R, 4L, 11R, 7 | 4 | 11R, 7 (atypia) | 4R, 4L | 4R, 4L | |
| 8 | RLL | NSCLC | 4R, 4L | 2 | 4R, 4L | None | 2R | |
| 9 | RUL | Squamous | 4R, 7, 10R | 3 | 7, 10R | 4R | 2R, 4R | |
| 10 | RUL | NSCLC | 2R, pre-carinal, 4R, right hilum | 4 | Pre-carinal | 2R, 4R, right hilum | 2R |
EBUS: endobronchial ultrasound; RLL: right lower lobe; RUL: right upper lobe; NSCLC: non-small cell lung cancer. #: between positron emission tomography-computed tomography and EBUS-guided transbronchial needle aspiration.
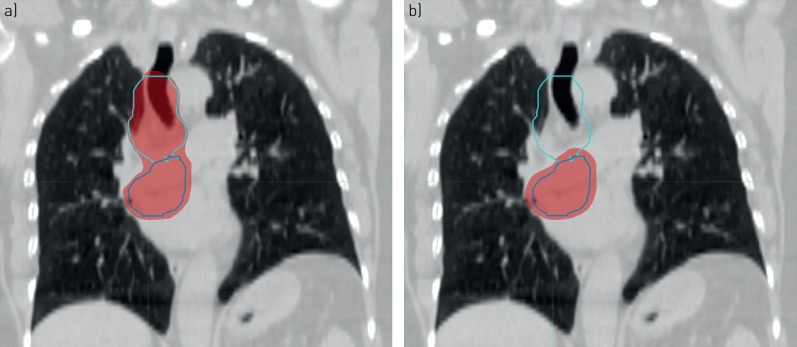
Four patients (upstaged by EBUS-TBNA) had a significant geographic miss of nodal GTV when planned to PET-positive nodes only (figure 1). This is illustrated further in figure 2, where the curative dose value of 57 Gy covers the PET-avid disease whereas the disease which is PET negative but EBUS-TBNA positive receives negligible dose (<5 Gy). Table 2 shows the target and OAR doses for both groups of patients with discordant findings. When planned using PET-CT only, the EBUS-positive/PET-negative target volume was significantly under-dosed. For instance, the mean dose delivered to 95% of the volume of the PTV (PTV D95%) was 58.1 Gy for plans using EBUS-TBNA information compared with 16.3 Gy for PET-only plans (optimally the dose for a 60-Gy plan (i.e. curative radiotherapy plan) should be >57 Gy (i.e. >95%)). Inclusion of the EBUS-positive volume ensured sufficient target coverage at the expense of only modest increases in heart, oesophagus and lung doses (table 2). The risk of anticipated adverse clinical outcome with these increases in dose to normal tissue is low, as these tolerances remain within expected radiation normal tissue constraints as standardly set by radiotherapy planning protocols.
FIGURE 1.
Illustration of value of detection of positron emission tomography (PET)-occult lymph node metastases in patient 1, where nodal station 4R was PET negative but transbronchial needle aspiration (TBNA) demonstrated malignant involvement. a) Endobronchial ultrasound (EBUS)-guided TBNA and PET-planned radiotherapy. b) PET-only planned radiotherapy. The area in red is the planning target volume.
FIGURE 2.
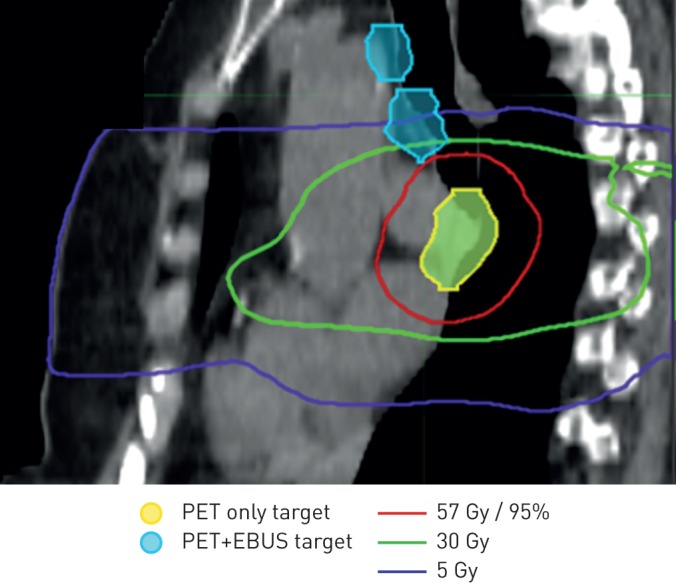
Sagittal view illustrating dose distribution with endobronchial ultrasound (EBUS)-proven malignancy (blue) receiving negligible doses of radiation; positron emission tomography (PET)-positive disease (yellow) received a high dose (>57 Gy).
TABLE 2.
Target and organ at risk doses
| EBUS-upstaged# | EBUS-downstaged¶ | |||
| EBUS-TBNA+PET | PET | EBUS-TBNA+PET | PET | |
| PTV D95% Gy | 58.1±2.7 | 16.3±3.3 | 59.7±0.6 | 58.6±1.1 |
| Mean heart Gy | 10.9±7.9 | 8.4±7.4 | 12.2±3.5 | 15.9±8.4 |
| Mean oesophagus Gy | 18.5±5.6 | 12.0±5.7 | 16.6±10.4 | 29.1±5.2 |
| Lung NTCP % | 9.6±2.0 | 7.6±1.5 | 12.6±5.3 | 18.3±5.3 |
Data are presented as mean±sd. EBUS: endobronchial ultrasound; TBNA: transbronchial needle aspiration; PET: positron emission tomography; PTV: planning target volume; D95%: treatment volume receiving >95% of planned dose; NTCP: normal tissue complication probability. #: EBUS-positive/PET-negative, n=4, dose was changed; ¶: EBUS-negative/PET-positive, n=4 (because two out of six patients where EBUS identified a lesser extent of lymph node disease could not reasonably be encompassed within a radical radiotherapy field when planned based on PET alone and therefore plans were not created), potential change in dose.
Six patients had cytology demonstrating benign lymphoid cells obtained from PET-avid nodal regions. Pathological descriptions of the negative nodes included reactive nodes, anthracotic pigmented macrophages and dendritic reticulum cells. There was no clear evidence of granulomatous disease noted. In four patients, inclusion of EBUS-negative/PET-positive nodes conferred significant increases in mean oesophagus, heart dose and lung NTCP over plans based on EBUS-TBNA-positive nodes alone (table 2).
Discussion
Systematic minimally invasive staging with EBUS-TBNA is recommended in guidelines for management of early-stage NSCLC given its demonstrated ability to identify PET-occult mediastinal lymph node metastases [7]. The clinical impact of pre-operative detection of PET-occult NSCLC is clear. Limited studies have confirmed that systematic mediastinal lymph node staging with EBUS-TBNA can identify PET-occult lymph node metastases and, in the current study, we confirm for the first time the dosimetric significance of this. Detection of PET-occult lymph node disease in four patients significantly reduced the likelihood of geographical miss of the involved tumour; planning incorporating EBUS and PET findings resulted in a mean PTV D95% of 58 Gy, compared to radiation planning based on PET alone, where PTV D95% in these four patients was just 16 Gy.
PET-occult lymph node metastases were demonstrated by EBUS in four patients in this subset analysis, whereas a lesser extent of mediastinal involvement, compared with FDG-PET, was demonstrated by EBUS in six patients (including two patients downstaged from cN3 to pN2). Lymph nodes upstaged by EBUS were significantly smaller than nodes downstaged by EBUS (7.5 mm (range 7–9 mm) versus 12 mm (range 6–21 mm); p<0.005) [5]. Overall, from the cohort of 30 patients, 13.3% (four out of 30) would have additional PET-occult disease included in the radiotherapy volume, while 20% (six out of 30) had presumed PET-positive disease with negative cytology.
We additionally note the potential to significantly reduce likelihood of radiation toxicity in patients where EBUS identifies benign results from FDG-avid mediastinal lymph nodes. This reduction in dose to normal structures could lead to a reduction in a number of acute and late radiotherapy complications, including pneumonitis, oesophagitis and cardiac toxicity. For instance, significant reductions in mean dose to the oesophagus (43% reduction) and heart (24% reduction) are clearly beneficial in terms of reducing dose to critical organs. Lung tissue is exquisitely sensitive to radiation damage as dose increases and the NTCP of significant grade 2 or higher pneumonitis as measured in this study confers a reduction in risk of toxicity by one-third (18.3% to 12.6%).
In agreement with Peeters et al. [3], we do not advocate routine omission of PET-positive/EBUS-TBNA-negative nodes from radiation fields, due to the risk of an EBUS false-negative rate of 20%. However, the false-negative rate of PET-CT can range from 6% to 13%, dependent on lymph node size, and it is clear that if a separate cause for PET avidity such as sarcoidosis, silicosis, fibrosis or pneumonia is suspicious on imaging or clinically then the confirmation of the non-malignant histology can strengthen the decision to avoid radiotherapy to this node or nodal level [3, 8, 9].
While the use of PET-CT is a key component in the staging of NSCLC patients, it is important to note that the addition of minimally invasive pathological interrogation such as EBUS-TBNA has the ability to provide more accurate information on nodal involvement, which may reduce the likelihood of toxicity or local treatment failure. EBUS-TBNA is extremely safe and allows the sampling of most sites within the mediastinum. Limited access to stations 5 and 8 may be mediated through peri-oesophageal sampling using an endoscopic ultrasound bronchoscope (EUS-B), which may even be performed by pulmonologists at the time of staging EBUS [10]. Addition of an EUS-B is likely to be favourable with respect to detecting occult disease and is part of the protocol of a current multicentre study to confirm the preliminary results of this pilot study (Australian New Zealand Clinical Trials Registry, identifier ACTRN12617000333314).
Our findings are consistent with numerous prior studies examining the ability of systematic EBUS-TBNA to achieve a stage shift from PET-based lymph node staging results. In patients with clinical N2 NSCLC, Sanz-Santos et al. [11] reported that systematic EBUS-TBNA provided additional relevant staging information in 13% of cases. In a recent study by Vial et al. [12], evaluation of 246 patients comparing PET-CT and EBUS-TBNA revealed a stage shift in 19% of patients. 50% of patients with N1 disease were downstaged to N0 following EBUS-TBNA, enabling eligibility for stereotactic radiotherapy. While small sample size is a firm limitation in our study, it is clear that our results corroborate with the moderate concordance found between EBUS-TBNA and PET-CT in the aforementioned studies and the current study is the first to confirm not only a potential benefit in the prospect of disease control but also meaningful reductions in potential toxicity.
This study highlights that the false-negative rates for PET-CT can have significant implications in treatment volumes (under-dosing of tumour and potential increased dose to critical structures) and we advise using practical and pragmatic algorithms to guide radiation planning for NSCLC patients as discussed in Peeters et al. [3]. At present, for lymph nodes that are cytology negative and PET positive, radiotherapy plans should not be amended unless there is a clear benign cause noted on pathology (e.g. anthrasilicosis or granulomatosis), high suspicion of infection with symmetrical pattern and FDG discrepancy with the primary tumour or negative pathology confirmed at mediastinoscopy. If centres do omit PET-positive EBUS-negative nodes from radiotherapy fields, this study gives some insight into the potential dosimetric impact this may have. A prospective multicentre trial to validate these findings, and to address the potential impact of EBUS-TBNA in terms of local control and reduction in toxicity for patients presenting with locally advanced NSCLC, is currently underway (ACTRN12617000333314). The current standard of care for mediastinal staging may require revision to optimise curative-intent radiotherapy planning and delivery.
Conclusion
Systematic mediastinal staging with EBUS-TBNA may achieve a stage shift when compared to staging performed with PET alone. We demonstrate for the first time that identification of PET-occult lymph node metastases by systematic EBUS-TBNA prior to radical-intent radiotherapy for NSCLC significantly improves radiation coverage of subclinical disease. Identification of false-positive lymph node involvement in selected cases may also substantially reduce radiation dose to critical structures in selected cases.
Acknowledgements
The authors would like to acknowledge Nigel Anderson, Brayden Gearey and Tom Devereux (Dept of Radiation Oncology, Peter MacCallum Cancer Centre, Melbourne, Australia) for their assistance in the technical aspects, with particular regard to importing of radiological scans and radiotherapy planning assistance.
Footnotes
Conflict of interest: A.J. Cole has nothing to disclose.
Conflict of interest: N. Hardcastle has nothing to disclose.
Conflict of interest: G-A. Turgeon has nothing to disclose.
Conflict of interest: R. Thomas has nothing to disclose.
Conflict of interest: L.B. Irving has nothing to disclose.
Conflict of interest: B.R. Jennings has nothing to disclose.
Conflict of interest: D. Ball reports advisory board fees from Pfizer, paid to his institution, outside the submitted work.
Conflict of interest: T. Kron has nothing to disclose.
Conflict of interest: D.P. Steinfort has nothing to disclose.
Conflict of interest: S. Siva reports grants from Varian Medical Industries, outside the submitted work.
Support statement: Funding was received from the National Health and Medical Research Council (Australia), grant numbers APP1122347 and GNT1121880. Funding information for this article has been deposited with the Crossref Funder Registry.
References
- 1.De Leyn P, Dooms C, Kuzdzal J, et al. Revised ESTS guidelines for preoperative mediastinal lymph node staging for non-small-cell lung cancer. Eur J Cardiothorac Surg 2014; 45: 787–798. [DOI] [PubMed] [Google Scholar]
- 2.Lee PC, Port JL, Korst RJ, et al. Risk factors for occult mediastinal metastases in clinical stage I non-small cell lung cancer. Ann Thorac Surg 2007; 84: 177–181. [DOI] [PubMed] [Google Scholar]
- 3.Peeters ST, Dooms C, Van Baardwijk A, et al. Selective mediastinal node irradiation in non-small cell lung cancer in the IMRT/VMAT era: how to use E(B)US-NA information in addition to PET-CT for delineation? Radiother Oncol 2016; 120: 273–278. [DOI] [PubMed] [Google Scholar]
- 4.Yasufuku K, Pierre A, Darling G, et al. A prospective controlled trial of endobronchial ultrasound-guided transbronchial needle aspiration compared with mediastinoscopy for mediastinal lymph node staging of lung cancer. J Thorac Cardiovasc Surg 2011; 142: 1393–1400.e1. [DOI] [PubMed] [Google Scholar]
- 5.Steinfort DP, Siva S, Leong TL, et al. Systematic endobronchial ultrasound-guided mediastinal staging versus positron emission tomography for comprehensive mediastinal staging in NSCLC before radical radiotherapy of non-small cell lung cancer: a pilot study. Medicine 2016; 95: e2488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kinahan PE, Fletcher JW. Positron emission tomography-computed tomography standardized uptake values in clinical practice and assessing response to therapy. Semin Ultrasound CT MR 2010; 31: 496–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vilmann P, Clementsen PF, Colella S, et al. Combined endobronchial and esophageal endosonography for the diagnosis and staging of lung cancer: European Society of Gastrointestinal Endoscopy (ESGE) Guideline, in cooperation with the European Respiratory Society (ERS) and the European Society of Thoracic Surgeons (ESTS). Endoscopy 2015; 47: 545–559. [DOI] [PubMed] [Google Scholar]
- 8.Detterbeck FC, Jantz MA, Wallace M, et al. Invasive mediastinal staging of lung cancer: ACCP evidence-based clinical practice guidelines (2nd edition). Chest 2007; 132: Suppl. 3, 202S–220S. [DOI] [PubMed] [Google Scholar]
- 9.Micames CG, McCrory DC, Pavey DA, et al. Endoscopic ultrasound-guided fine-needle aspiration for non-small cell lung cancer staging: a systematic review and metaanalysis. Chest 2007; 131: 539–548. [DOI] [PubMed] [Google Scholar]
- 10.Wimaleswaran H, Farmer MW, Irving LB, et al. Pulmonologist-performed transoesophageal sampling for lung cancer staging using an endobronchial ultrasound video-bronchoscope: an Australian experience. Intern Med J 2017; 47: 205–210. [DOI] [PubMed] [Google Scholar]
- 11.Sanz-Santos J, Serra P, Torky M, et al. Systematic compared with targeted staging with endobronchial ultrasound in patients with lung cancer. Ann Thorac Surg 2018; 106: 398–403. [DOI] [PubMed] [Google Scholar]
- 12.Vial MR, Khan KA, O'Connell O, et al. Endobronchial ultrasound-guided transbronchial needle aspiration in the nodal staging of stereotactic ablative body radiotherapy patients. Ann Thorac Surg 2017; 103: 1600–1605. [DOI] [PMC free article] [PubMed] [Google Scholar]