Abstract
To assess safety of the no-flip ShangRing male circumcision technique and to determine clinical course and safety of spontaneous detachment (i.e., allowing the device to fall off), we conducted a case series of no-flip ShangRing circumcision combined with a randomized controlled trial of removal 7 days postcircumcision versus spontaneous detachment at two health facilities in Kenya. The primary outcome was the safety of the no-flip technique based on moderate and severe adverse events (AEs) during the procedure and through 42-day follow-up. A main secondary outcome was clinical course and safety of spontaneous detachment. Two hundred and thirty males 10 years and older underwent no-flip circumcision; 114 randomized to 7-day removal and 116 to spontaneous detachment. All circumcisions were successfully completed. Overall 5.3% (6/114) of participants in the 7-day group and 1.7% (2/116) in the spontaneous group had an AE; with no differences when compared to the 3% AE rate in historical data from African studies using the original flip technique (P = 0.07 and P = 0.79, respectively). Overall 72.4% (84/116) of participants in the spontaneous group wore the ShangRing until it detached. Among the remaining (27.6%; 32/116), the ring was removed, primarily at the participants' request, due to pain or discomfort. There was no difference in AE rates (P = 0.169), visit day declared healed (P = 0.324), or satisfaction (P = 0.371) between randomization groups. The median time to detachment was 14.0 (IQR: 7–21, range: 5–35) days. The no-flip technique and spontaneous detachment are safe, effective, and acceptable to boys and men 10 years and older. Phimosis and penile adhesions do not limit successful ShangRing circumcision with the no-flip technique.
Keywords: HIV prevention, male circumcision device, no-flip technique, ShangRing, voluntary medical male circumcision
INTRODUCTION
Voluntary medical male circumcision (VMMC) is one of the most promising human immunodeficiency virus (HIV) prevention approaches in the Sub-Saharan Africa, and the only one that an HIV-negative man can use to substantially reduce his HIV risk, without continuous action or behavior change.1 It is also the most cost-effective approach.2 Two meta-analyses found a 70%–72% reduction in risk of HIV acquisition in men engaging in heterosexual intercourse due to VMMC.3,4 The protective effect of circumcision is sustained for at least 5 years,5,6 with incidence and prevalence reductions attributable to VMMC seen in males and females.7,8,9
VMMC programs are well established in 14 Sub-Saharan African countries, resulting in over 14.5 million circumcisions till date.10 Although the original goal of 21 million VMMCs by 2016 was not achieved,11 VMMC scale-up has been one of the most successful recent public health interventions.3,12,13 A new goal of 27 million by 2020 was set in 2016.14,15 This will require roughly doubling the annual number of VMMCs in priority countries to 5 million.15
VMMC devices may reduce some challenges in service scale-up needed to reach these ambitious goals, making the procedure simpler and faster.12,13,16 The ShangRing, a single-use collar clamp circumcision device, is safe, easy to use, and acceptable in Africa.17,18,19,20,21 It received World Health Organization (WHO) prequalification for use in males 13 years and older following studies in Africa (the ShangRing has US FDA 510(k) clearance for use in adult males).16,22,23,24 These studies used the original technique described by Peng et al.,25,26,27,28 which involves everting the foreskin over the inner ring. Everting the foreskin has been reported to be the most difficult step.29 A modification, known as the no-flip technique, eliminates the need to evert the foreskin and also simplifies device removal (Supplementary Figure 1 (586.1KB, pdf) shows the differences between the original flip and the modified no-flip ShangRing techniques). The no-flip technique has been shown to be safe in studies conducted in China.30,31,32,33,34
The instructions for use include ShangRing removal 7–10 days after circumcision.24 Use of the no-flip technique may facilitate the device falling off (called spontaneous detachment), alleviating the need for a removal visit and reducing the burden on health services (Supplementary Figure 2 (1.5MB, pdf) shows the healing process after ShangRing circumcision).30,31,32,33,34
The present study was designed to gather data for submission to the WHO to amend the prequalification to include the use of the no-flip technique and spontaneous detachment, and to extend the lower age to 10 years. The primary objective was to assess the safety of the no-flip technique in males 10 years and older. The main secondary objective was to determine the clinical course and safety of spontaneous device detachment.
PARTICIPANTS AND METHODS
Study design, participants, and setting
We combined a case series of the ShangRing no-flip technique (to address our primary objective) with an open-label, parallel randomized controlled trial (RCT) with randomization to: (1) removal 7 days postcircumcision or (2) allowing the device to fall off, called spontaneous detachment (to address our main secondary objective). The study was conducted at two sites in Kenya: Homa Bay County Teaching and Referral Hospital (Homa Bay), and the Vipingo Health Centre in Kilifi County (Vipingo).
Since we aimed to gather data to amend the WHO prequalification, our sample size was based on WHO recommendations.16,22 To ensure follow-up on at least 200 cases of the new no-flip technique (100 in the 7-day and 100 in the spontaneous groups), 230 participants were recruited. Healthy, uncircumcised males 10 years and older seeking VMMC were informed of the study. Uncircumcised males in good health and without a sexually transmitted infection were eligible. Males were ineligible if they had a known allergy to lidocaine or other local anesthesia; a bleeding/clotting disorder; a congenital genitourinary abnormality; or active genital infection, anatomic abnormality, or other condition that prevented safe participation. HIV testing was offered, but not compulsory for enrollment. Although there is no evidence from Chinese studies that age impacts outcomes after no-flip ShangRing circumcision or spontaneous detachment,30,31,33 we recruited participants in two equal groups; 50% between 10 and 15 years and 50% over 15 years, to explore possible age-related differences.
Providers were experienced with conventional circumcision. Those at Homa Bay had considerable experience with the flip ShangRing technique, while those in Vipingo had not previously used the ShangRing. All providers received training on the no-flip technique before the study.
Procedures
Participants/parents were interviewed to gather baseline demographic information. A clinical examination ensured participants met eligibility criteria. Participants received oral paracetamol (acetaminophen, Paratol® Tablets, Laboratory & Allied Ltd., Nairobi, Kenya) 20–30 min precircumcision. We administered dorsal penile nerve and ring blocks with 1% lidocaine (Anasica™, Barat Parenterals Limited, Vadodara, India). All participants underwent no-flip circumcision, described previously.30,31 Follow-up visits were on days 7, 14, 21, 28, 35, and 42 following circumcision, although participation ended if a participant's wound was determined to be clinically healed before 42 days. Participants that were not healed at day 42 were asked to return for additional follow-up.
Participants randomized to the 7-day group had their ShangRings removed 7 days after circumcision as previously described.26 Participants randomized to the spontaneous detachment group were followed to document the course of the device falling off on its own but could request removal at any time. At follow-up, a genital examination was conducted, and participants/parents were interviewed about their experience, including an assessment of overall satisfaction at the last visit.
Randomization and masking
Randomization was in a 1:1 ratio to the removal of the ShangRing at 7 days following circumcision (7-day removal group) or observation to follow the course of the ring falling off (spontaneous detachment group). Randomization was stratified by age-group (10–15 and over 15 years) and restricted with randomly varying blocks of 4–8 within strata. Random allocation concealment was achieved using a text-message service (Sealed Envelope Ltd., London, UK). The allocation sequence was computer-generated by a researcher unaffiliated with the study and uploaded to Sealed Envelope.
Participants were randomized by a research assistant at each site just before the circumcision. Participants were recruited at both sites until the total sample size was reached. Because of the nature of the study, and the limited availability of clinical staff at the study sites, it was not possible to blind participants, providers, those assessing outcomes, or other study staff to treatment allocation.
Outcomes
The primary outcome was the safety of the no-flip technique based on the rate of moderate and severe adverse events (AEs) during the procedure and follow-up. Rates were compared to those from previous African studies, which used the original flip technique and removal at 7 days. We analyzed AE rates separately for those allocated to device removal at 7 days and those allocated to spontaneous detachment, to account for any differences related to the removal approach. AEs were classified based on a widely used consensus guide.17,35 Events of mild severity were considered within the normal range of circumcision sequelae and not reported. Other safety endpoints included device-related malfunctions, device displacement, and time to clinical wound healing, defined as intact epithelium covering the wound as judged by the provider on visual inspection.
Prespecified secondary outcomes were as follows: (1) clinical course and safety of spontaneous detachment based on timing, comparison of problems or AEs between the randomization groups, and comparison of time/course of clinical wound healing between the randomization groups; (2) ease of use of the no-flip technique, measured by circumcision procedure and device removal times, and problems encountered during both; and (3) participant satisfaction, based on pain experienced approximately 20 min after circumcision and during removal (visual analog scale; 0 = no pain, 10 = worst possible pain), time to return to normal activity, experience wearing the ShangRing and during spontaneous detachment, and comparison of overall satisfaction between the randomization groups. We also analyzed the data for these outcomes based on age category (10–15 and over 15 years).
Statistical analyses
For our primary objective, we examined data from previous ShangRing studies in Africa that used the flip technique with removal at 7 days. The range of AE rates was 0.8%–7.6%.17,18,19,20,21,36,37 We used 3% to represent the baseline AE rate for the flip technique. To this, we compared AEs following no-flip circumcision in participants in the 7-day removal group and the spontaneous detachment group. From a statistical perspective, our sample size of 100 in each group would provide 80% power to detect a 7% increase in AEs with either no-flip and 7-day removal or no-flip and spontaneous detachment, relative to historical data, using a one-sided test and alpha of 0.05. Power calculations were conducted in Stata, version 14.0 (StataCorp LLC, College Station, TX, USA), using one-sample proportion tests comparing observed values to a reference.
For our main secondary objective, our sample provides 80% power to detect a difference of 15% assuming an alpha of 0.05, a two-sided test and an AE level no higher than 8% in the 7-day removal group (7.6% is the highest AE rate reported following circumcision with the flip technique).17
One planned interim analysis was conducted by a three-member Data and Safety Monitoring Board (DSMB) after 40 participants had their ShangRing removed at 7 days. At the same time, a similar number of participants had been randomized to spontaneous detachment. The DSMB was asked to recommend stopping recruitment if there was a clear benefit or harm to use of the no-flip technique or spontaneous detachment or evidence of futility. The O'Brien-Fleming approach (alpha of 0.005) was used. Following a review of the interim analysis, the DSMB recommended the study continue.
We used an intention-to-treat analysis. No missing data were imputed. Available data from participants lost to follow-up were included. Quantitative variables were described using means, medians, or percentages. AE rates were compared to historical data, and between randomization groups and age categories, using Fisher's exact test. Statistical tests used to compare other outcomes between randomization groups and age categories included: circumcision and removal time – Wilcoxon rank sum test; clinical wound healing time – Student's t-test; circumcision and removal outcomes (other than time) and participant satisfaction variables – Pearson's Chi-square test; and pain scores – Welch's t-test. Kaplan–Meier analysis was used to determine the cumulative probability of spontaneous detachment. To compare survival distribution between the age-groups, the log-rank test was used.
We used R version 3.2.3 (The R Foundation for Statistical Computing, www.r-project.org/foundation/) for all analyses except for AE rate comparisons, for which we used Stata version 14.0.
Ethical approval
Ethical approvals were obtained from Weill Cornell Medical College (New York, NY, USA) and the Kenya Medical Research Institute (Nairobi, Kenya). Regulatory approval was obtained from the Kenya Pharmacy and Poisons Board (Nairobi, Kenya). Informed consent was obtained from participants 18 years and older. Parental/guardian consent was obtained for participants under 18 years, with assent when minors understood study participation. The trial was registered on ClinicalTrials.gov NCT02390310.
RESULTS
Trial overview
Between May 8 and September 16, 2015, 230 participants were enrolled (115 10–15 years and 115 older than 15 years; 103 in Homa Bay and 127 in Vipingo), with 49.6% (114/230) randomly allocated to the 7-day removal and 50.4% (116/230) to the spontaneous groups (Figure 1). Follow-up was completed on October 28, 2015. Overall 97.8% (225/230) of participants completed the study; among the 2.2% (5/230) lost to follow-up, 1.3% (3/230) were in the 7-day group and 0.9% (2/230) in the spontaneous group. Baseline sociodemographic characteristics were similar between the groups (Table 1).
Figure 1.
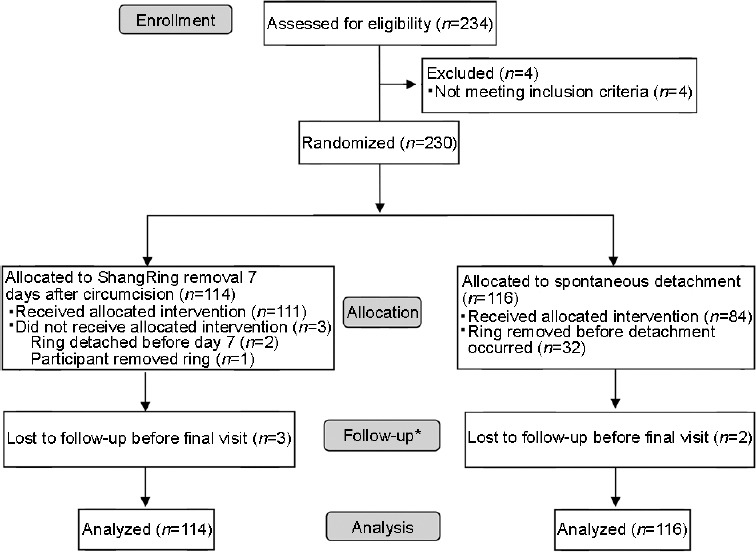
Flow of study participants. *Scheduled follow-up was through 42 days postcircumcision, although study participation ended prior to 42 days if a participant's circumcision wound was determined to be clinically healed before that time. Seventeen participants were not completely healed at day 42. They were asked to return one week later and determined to be completely healed at that time. Five participants missed one or more follow-up visits before clinical healing was documented, including their day 42 visit, but eventually returned and were documented to be healed.
Table 1.
Selected baseline sociodemographic characteristics of men and boys undergoing no-flip ShangRing circumcision, by randomization group
| Characteristic | Randomization group | Total (n=230), n (%) | |
|---|---|---|---|
| 7-day removal (n=114) | Spontaneous detachment (n=116) | ||
| Age (year) | |||
| 10–12, n (%) | 41 (36.0) | 42 (36.5) | 83 (36.4) |
| 13–15, n (%) | 17 (14.9) | 16 (13.9) | 33 (14.4) |
| 16–18, n (%) | 19 (16.7) | 18 (15.7) | 37 (16.2) |
| 19–21, n (%) | 14 (12.3) | 5 (4.4) | 19 (8.3) |
| 22–24, n (%) | 6 (5.3) | 8 (7.0) | 14 (6.1) |
| 25–30, n (%) | 10 (8.8) | 7 (6.1) | 17 (7.4) |
| ≥31, n (%) | 7 (6.1) | 19 (16.5) | 26 (11.4) |
| Mean (s.d.) | 17.4 (8.2) | 19.0 (10.3) | 18.2 (9.3) |
| Median (IQR) | 15 (12–20) | 15 (11–23) | 15 (11–21) |
| Range | 10–54 | 10–53 | 10–54 |
| Highest level of education completed | |||
| No formal education, n (%) | 1 (0.9) | 1 (0.9) | 2 (0.9) |
| Some primary, n (%) | 71 (63.4) | 69 (60.5) | 140 (61.9) |
| Completed primary, n (%) | 10 (8.9) | 9 (7.9) | 19 (8.4) |
| Some secondary, n (%) | 8 (7.1) | 11 (9.6) | 19 (8.4) |
| Completed secondary, n (%) | 10 (8.9) | 7 (6.1) | 17 (7.5) |
| Postsecondary, n (%) | 12 (10.7) | 17 (14.9) | 29 (12.8) |
| Total (n) | 112 | 114 | 226 |
| Ethnic group | |||
| Luo, n (%) | 61 (54.5) | 67 (58.8) | 128 (56.6) |
| Giriama, n (%) | 28 (25.0) | 27 (23.7) | 55 (24.3) |
| Kamba, n (%) | 5 (4.5) | 2 (1.8) | 7 (3.1) |
| Other, n (%) | 18 (16.1) | 18 (15.8) | 36 (15.9) |
| Total (n) | 112 | 114 | 226 |
| Primary reason for seeking VMMC | |||
| Hygiene, n (%) | 41 (36.6) | 46 (40.4) | 87 (38.5) |
| Social/religious, n (%) | 43 (38.4) | 36 (31.6) | 79 (35.0) |
| HIV protection, n (%) | 24 (21.4) | 31 (27.2) | 55 (24.3) |
| Stigma, n (%) | 4 (3.6) | 1 (0.9) | 5 (2.2) |
| Total (n) | 112 | 114 | 226 |
| HIV status at study entry | |||
| HIV-negative, n (%) | 83 (73.5) | 83 (72.8) | 166 (73.1) |
| HIV-positive, n (%) | 4 (3.5) | 3 (2.6) | 7 (3.1) |
| Not tested on day of VMMC, n (%) | 10 (8.8) | 13 (11.4) | 23 (10.1) |
| Tested on day of VMMC but did not want to disclose results to study staff, n (%) | 16 (14.2) | 15 (13.2) | 31 (13.7) |
| Total (n) | 113 | 114 | 227 |
VMMC: voluntary medical male circumcision; HIV: human immunodeficiency virus; s.d.: standard deviation; IQR: interquartile range. For some characteristics, data are missing for up to four participants, and percentages may not total to 100% due to rounding
Safety outcomes
Overall, 3.5% (8/230; 95% confidence interval [CI]: 1.1%–5.8%; Table 2) of participants had an AE. All were moderate, occurred during follow-up, were considered definitely related to the circumcision, and resolved with conservative management and without sequelae. Among participants with the no-flip technique and removal at 7 days, 5.3% (6/114; 95% CI: 1.2%–9.4%) had an AE, which was not higher, using a one-sided test, than the 3% from historical data with the flip technique (P = 0.07).17,18,19,20,21,36,37 Following circumcision with the no-flip technique and spontaneous detachment, 1.7% (2/116; 95% CI: 0–4.1%) of participants had an AE, also not different from previously published studies (P = 0.79).
Table 2.
Adverse events by randomization group and age category
| Randomization group | 7-day removal group, n (%) | Spontaneous group, n (%) | Total, n (%, 95% CI) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 10–15 years (n=57) | >15 years (n=57) | Total (n=114) | 10–15 years (n=58) | >15 years (n=58) | Total (n=116) | 10–15 years (n=115) | >15 years (n=115) | Total (n=230) | |
| Total AEs | 2 (3.5) | 4 (7.4) | 6 (5.3) | 2 (3.4) | 0 (0) | 2 (1.7) | 4 (3.5) | 4 (3.5) | 8 (3.5, 1.1–5.8) |
| Severity of AE | |||||||||
| Severe | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0, 0–0) |
| Moderate | 2 (3.5) | 4 (7.4) | 6 (5.3) | 2 (3.4) | 0 (0) | 2 (1.7) | 4 (3.5) | 4 (3.5) | 8 (3.5, 1.1–5.8) |
| Type of AE | |||||||||
| Edema | 2 (100) | 0 (0) | 2 (33.3) | 2 (100) | 0 (0) | 2 (100) | 4 (100) | 0 (0) | 4 (50.0) |
| Infection | 0 (0) | 4 (100) | 4 (66.7) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 4 (100) | 4 (50.0) |
Any event was counted only once using highest severity. No participant had more than one AE. There were no differences between randomization groups or age categories. AE: adverse event; CI: confidence interval
There were no differences in AEs between randomization groups, overall (P = 0.169), or within either age category; 10–15 years old (P = 1.0), over 15 years old (P = 0.057) (Table 2). Further, there were no differences by age category overall (P = 1.0), within the 7-day removal group (P = 0.679), or within the spontaneous detachment group (P = 0.469). There were no device-related malfunctions or device displacements.
Ease of use of the no-flip technique
Nurses conducted most circumcisions (81.7%; 187/229) and removals (86.7%; 124/143). The following ShangRing sizes were used (presented as ring size [number of participants]): 39 mm (n = 1), 38 mm (n = 1), 37 mm (n = 5), 36 mm (n = 4), 35 mm (n = 9), 34 mm (n = 13), 33 mm (n = 18), 32 mm (n = 21), 31 mm (n = 17), 30 mm (n = 16), 29 mm (n = 10), 28 mm (n = 11), 26 mm (n = 8), 24 mm (n = 5), 22 mm (n = 2), 20 mm (n = 12), 18 mm (n = 40), 16 mm (n = 14), 15 mm (n = 12), 14 mm (n = 5), 13 mm (n = 3), and 12 mm (n = 2) (data missing from one participant). All ShangRing procedures were successfully completed (Table 3). More 10–15-year-old participants required a dorsal slit (P < 0.001) and/or lysis of penile adhesions (P < 0.001) than those over 15 years (Table 3). There were no differences between the age groups in other aspects of the procedures.
Table 3.
No-flip ShangRing circumcision and removala procedure outcomes, by age category
| Age categoryd | Total | ||
|---|---|---|---|
| 10–15 years old | >15 years old | ||
| Circumcision successfully completed, n (%) | 115/115 (100) | 115/115 (100) | 230/230 (100) |
| Dorsal slit needed to insert inner ring, n (%) | 43/114 (37.7)* | 17/115 (14.8)* | 60/229 (26.2) |
| Lysis of penile adhesions required, n (%) | 55/113 (48.2)** | 4/114 (3.5)** | 59/227 (25.8) |
| Circumcision duration (min), median (IQR) | 6.7 (5.4–8.5) | 6.7 (5.2–7.9) | 6.7 (5.2–8.3) |
| Minor problems during the circumcision, n (%) | 0/115 (0) | 2/115 (1.7) | 2/230 (0.9) |
| AEs during circumcision, n (%) | 0/115 (0) | 0/115 (0) | 0/230 (0) |
| Postoperative painb, median (IQR) | 3 (2–5) | 3 (2–4) | 3 (2–4) |
| Removal duration (min), median (IQR) | 2.2 (1.7–4.3) | 2.3 (1.6–3.7) | 2.2 (1.6–3.9) |
| Minor problems during the removal, n (%) | 3/66 (4.5) | 0/77 (0) | 3/143 (2.1) |
| AEs during removal, n (%) | 0/66 (0) | 0/77 (0) | 0/143 (0) |
| Highest degree of pain during the removalc, median (IQR) | 4 (3–6)*** | 3 (2–4)*** | 4 (2–6) |
*P<0.001, **P<0.001, ***P=0.007. aIncludes all participants who underwent ShangRing removal: 111 in the 7-day group and 32 in the spontaneous detachment group. bMeasured approximately 20 min after completion of the circumcision; 0: no pain; 10: worst possible pain. cMeasured at the end of the removal procedure; 0: no pain; 10: worst possible pain. dUnless otherwise noted, there were no differences between age categories. IQR: interquartile range; AE: adverse event
Spontaneous detachment
A total of 72.4% (84/116) of participants in the spontaneous group wore the ShangRing until it detached. Among the remaining (27.6%; 32/116) participants, the ring was removed, primarily due to complaints of pain or discomfort. Most (75.0%; 24/32) of the requested removals occurred at the time of a scheduled follow-up visit (Figure 2). More participants over 15 years (37.9%; 22/58) requested removal than those 10–15 years (17.2%; 10/58) (P = 0.02).
Figure 2.
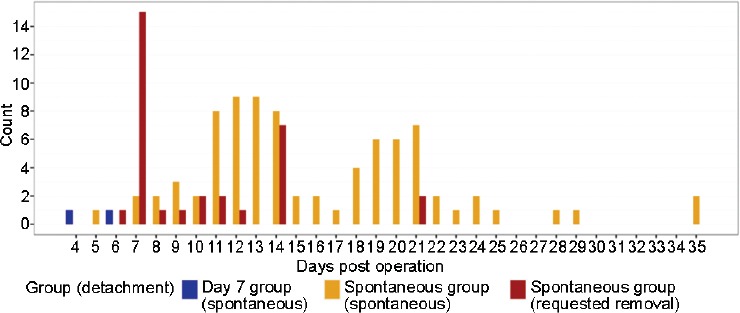
Disposition of the ShangRing among study participants. Participants randomized to the 7-day removal group who had their ring removed as scheduled on day 7 are not shown in the graph (n = 112). The ring detached spontaneously in two participants randomized to the 7-day group before they returned for removal on day 7 (blue bars). Most participants (n = 84) randomized to the spontaneous detachment group wore the ShangRing until it fell off on its own (orange bars). The ShangRing was removed for the remaining participants (n = 32), primarily at their request (red bars).
Among participants who wore the ring until it detached, the median (interquartile range [IQR]) time to spontaneous detachment was 14.0 (7–21) days, with no difference between age groups (P = 0.349); 14.0 (8–20) versus17.0 (9–25) days for the 10–15 and over 15 year olds, respectively. The earliest detachment occurred on day 3 after circumcision and the last on day 35, with two peaks – one at 11–14 days and another at 18–21 days (Figure 2). Cumulative probabilities of detachment at 7, 14, 21, 28, and 35 days were 2.6%, 47.4%, 84.2%, 95.3%, and 100.0%, respectively. There were no differences between age groups in mean time to detachment (P = 0.35) or cumulative probability of detachment at each follow-up (P = 0.133) (data not shown).
Clinical wound healing
Clinical wound healing was observed in 97.8% (225/230) of participants; five were lost to follow-up before they healed. Most (90.2%; 203/225) were documented to be clinically healed before or at 42 days. A minority (7.6%; 17/225) were not healed at day 42 but were healed one week later. The remaining participants (2.2%; 5/225) missed one or more follow-ups, including their day 42 visit, before clinical healing was documented. Among the 225 participants with healing data, the median (IQR) number of day at which they were declared clinically healed was 35 (28–42), with no difference between the randomization groups; 35 (28–42) versus 35 (28–42) days (P = 0.324) for the 7-day removal and spontaneous detachment groups, respectively. However, 10–15-year-old participants healed sooner than those over 15 years; 35 (31–38) versus 38 (35–42) days (P < 0.0001), respectively.
Participant satisfaction
There was no difference between the age categories in median pain scores reported by participants approximately 20 min postcircumcision (P = 0.557, Table 3). During removals, participants 10–15 years old reported higher pain scores compared to those over 15 years (P = 0.007; Table 3). There were no differences between the randomization groups in reported pain during erection, time to return to work, or interference with activities while wearing the ShangRing during the first week after circumcision (Table 4). Among those participants who wore the ring until it detached, wearing the ring beyond 7 days was generally not problematic, with little pain experienced with erections and minimal interference with activities such as work, walking, or sleeping (data not shown).
Table 4.
Experience while wearing the ShangRing among men and boys undergoing no-flip ShangRing circumcision, by randomization group (reported at day 7 follow-up visit)
| Characteristic | Randomization groupc | Total | |
|---|---|---|---|
| 7-day removal | Spontaneous detachment | ||
| Back to work/normal activities, n (%) | 112/114 (98.2) | 111/112 (99.1) | 222/226 (98.2) |
| Time after VMMC returned to work/normal activities (day), median (IQR) | 1 (1–2) | 1 (1–2) | 1 (1–2) |
| Time after VMMC returned to work/normal activities (day), range | 0–4 | 0–4 | 0–4 |
| Difficulty with erection, among those reporting an erection since VMMC, n (%) | 0/112 (0) | 1/108 (0.9) | 1/220 (0.5) |
| Highest degree of pain during erection, among those reporting an erection since VMMCa, median (IQR) | 2 (1–3) | 2 (1–3) | 2 (1–3) |
| Highest degree of pain during erection, among those reporting an erection since VMMCa, range | 0–6 | 0–8 | 0–8 |
| Interference with walking due to the ShangRingb, median (IQR) | 0 (0–0) | 0 (0–0) | 0 (0–0) |
| Interference with walking due to the ShangRingb, range | 0–5 | 0–6 | 0–6 |
| Interference with sleeping due to the ShangRingb, median (IQR) | 0 (0–0) | 0 (0–0) | 0 (0–0) |
| Interference with sleeping due to the ShangRingb, range | 0–7 | 0–7 | 0–7 |
a0: no pain; 10: worst possible pain. b0: no interference; 10: completely interfered. cThere were no differences between randomization groups for any of the characteristics. IQR: interquartile range; VMMC: voluntary medical male circumcision
At the final follow-up, 97.7% (208/213) of participants (or parents/guardians) said they were very satisfied with the appearance of the penis, and 99.5% (212/213) said they would recommend ShangRing circumcision. There were no differences between randomization groups (appearance, P = 0.371; recommendation, P = 1.0) or age groups (appearance, P = 0.975; recommendation, P = 1.0).
When participants (or parents/guardians) were asked what they liked about the procedure, top responses included: cosmetic appearance, short procedure time, less pain than expected, improved hygiene, and no stitches. Five participants said that there was nothing they liked. When participants (or parents/guardians) were asked what they disliked about the procedure, most (77.0%; 164/213) reported there was nothing they disliked, with a few (approximately 5% or less) reporting they felt wound care was difficult, experienced more pain than expected, or were bothered when the ring was partially detached.
DISCUSSION
Our results demonstrate that the no-flip ShangRing technique, whether with device removal at 7 days after circumcision or allowing it to fall off, is safe, effective, and acceptable to clients 10 years and older. Circumcision and device removal times, AE rates, time to clinical wound healing, and participant satisfaction with the no-flip technique appear similar to historical data from Africa with the original flip technique.17,18,19,20,21,36 Data from these studies show AE rates of 1.0%–7.5%, circumcision times of 5–7 min, and removal times of 2–5 min; consistent with our results for the no-flip technique. The no-flip technique simplifies the procedure since eversion of the foreskin and making 8–10 small slits needed in the tissue that remains after the foreskin is excised is unnecessary. Results from a study in Zambia showed that reducing the number of adult device sizes in half (from 14 to 7) by eliminating every other size did not reduce the safety, effectiveness, or acceptability of ShangRing VMMC.37 Having to stock fewer sizes would simplify supply chain logistics and inventory issues.
In addition, we found that spontaneous detachment was safe, effective and acceptable to most participants; 72% wore the device until it fell off. If similar numbers were seen in national VMMC programs, the burden of service delivery could be substantially reduced. Satisfaction was high among all participants. Those who requested ring removal were highly satisfied nonetheless, and those who wore the ring until it fell off reported no negative impacts on working, sleeping, or walking. These results confirm our earlier, smaller study, where spontaneous detachment was shown safe, effective, and acceptable to participants.38 It is reassuring to know that there are no safety concerns if clients do not return for ShangRing removal, since postcircumcision follow-up has been reported to be low (30%–50%) in VMMC programs.39,40,41
Allowing the ShangRing to fall off did not affect time to healing. In general, clinical wound healing after VMMC with devices takes an additional 1–2 weeks compared to conventional VMMC, presumably due to the nature of healing by secondary intention.17,42,43 This could place men and boys at an increased risk of HIV transmission for a longer period compared to conventional circumcision if they resume sex before complete wound healing. Our results suggest that healing may occur more quickly with the no-flip technique than with the original flip technique. The 10–15-year-old participants healed at a relatively quick 35.6 days, while those older than 15 years healed in 38.6 days, both faster than the mean time to healing of 44.1 days reported with the flip technique.17 Quicker healing would be another advantage of the no-flip technique.
As national VMMC programs move toward reaching all adults interested in VMMC and transition to sustained services, attention is being turned to services for boys and adolescents. The ShangRing can be used in nearly all clients, as shown in our study and previously published studies,17,18,19,20,21,36 regardless of the presence of a tight foreskin, frank phimosis or penile adhesions. The ShangRing, therefore, offers the promise of a single device that can be used across all ages, with a low likelihood that clients will need to have a conventional surgical circumcision. This contrasts with PrePex, the other WHO-prequalified device, where large numbers of adolescents (12%–52% depending on age) are unable to be circumcised with the device due to phimosis or preputial adhesions when using the device as described in the approved instructions for use.44,45,46 From a programmatic perspective, it would be most efficient to incorporate a device that could be successfully used on most men and boys, limiting those who would need a conventional circumcision.
Our study has several limitations. Assessment of the no-flip technique was non-comparative. We felt a case series would provide adequate evidence on outcomes of the no-flip technique, which could be compared to the large amount of historical data from flip ShangRing circumcisions conducted in Africa. Furthermore, it is difficult to achieve uniform interpretation between providers and study sites of outcomes such as AEs and clinical wound healing that depend on subjective clinical evaluation, even with well-described criteria. Finally, randomization was unmasked. In view of the nature of the intervention and the services at the sites, to mask staff or participants to treatment group, or to have the outcome assessment done by a provider who was unaware of treatment allocation, was not practical.
CONCLUSION
Our results show that no-flip ShangRing VMMC and spontaneous detachment are safe, effective, and acceptable to boys and men 10 years and older. Phimosis and penile adhesions do not limit eligibility, even in boys, where these conditions are common. A single device usable for all ages has substantial potential for simplification of service delivery, supply chain management, training and supervision, and educational materials. When complemented with strategies to ensure effective antiretroviral therapy for those with HIV infection, VMMC has been shown to be a cost-effective approach to move towards an AIDS-free generation.47 Use of the ShangRing could help achieve this goal.
AUTHOR CONTRIBUTIONS
MAB, QDA, PSL, RKL, JO, and MG conceived and designed the study. QDA, DO, MO, JO, PO, NN, MM, NK, MAB, PSL, RKL, and MG performed and oversaw the research. DO, MO, QDA, MAB, BC oversaw data management. QDA, MB, MAB analyzed the data. MAB wrote the original draft of the manuscript. All authors contributed to the interpretation of findings and critical review of the manuscript. All authors read and approved the final manuscript.
COMPETING INTERESTS
All authors declare no competing interests.
The original flip and modified no-flip ShangRing techniques.
The healing process after ShangRing circumcision
ACKNOWLEDGMENTS
The authors thank the participants (and their parents/guardians) who volunteered to take part in the study. The authors also thank the staff and administration of the study sites (Homa Bay County Teaching and Referral Hospital and Vipingo Health Centre), including Raymond O Simba and Judy Kinya, without whose assistance and support the study could not have been done. Staff of EngenderHealth in Kenya and New York, including Isaac Achwal, Sharone Beatty, Larisa Berezner, David Mwamkita, Eric Mwaura, Jared Nyanchoka, Nereah Obura, Herine Oriko, Denis Omwenga, and Sarah Sullivan provided vital support with study management and with implementation of the activities in Kenya. Michael Kirui and Paul Macharia from Bon Santé Consulting (Nairobi, Kenya) provided data management and statistical support. Emily Kemunto provided expert clinical monitoring of the study sites.
The authors are grateful to numerous officials of both the Kenya Ministry of Public Health and Sanitation and the Ministry of Medical Services, at the national and country-levels, as well as the National AIDS and STI Control Programme, for their long-standing support of our work. The authors thank the members of the Data and Safety Monitoring Board: Amy Herman-Roloff, from the US Centers for Disease Control and Prevention, in Pretoria, South Africa; Godfrey Kigozi, of the Rakai Health Sciences Program in Uganda; and John Ojal, from the London School of Hygiene and Tropical Medicine, London, England. In addition, the authors are grateful to Maaya Sundaram and Ray Yip from the Bill & Melinda Gates Foundation for their guidance and support, as well as to Renee Ridzon, who provided ongoing technical support from the initial inception of the idea for this study until its completion. The authors thank Jianzhong Shang, inventor of the ShangRing, for his generous donation of the ShangRings and associated supplies.
Finally, we thank the Bill & Melinda Gates Foundation who supported this work through Global Health Grant (Number OPP1084493) to EngenderHealth.
Supplementary Information is linked to the online version of the paper on the Asian Journal of Andrology website.
REFERENCES
- 1.Sgaier SK, Reed JB, Thomas A, Njeuhmeli E. Achieving the HIV prevention impact of voluntary medical male circumcision: lessons and challenges for managing programs. PLoS Med. 2014;11:e1001641. doi: 10.1371/journal.pmed.1001641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Geldsetzer P, Bloom D, Humair S, Bärnighausen T. Health HIV/AIDS Perspective Paper. Copenhagen: 2015. Benefits and costs of the HIV/AIDS targets for the post-2015 development agenda. [Google Scholar]
- 3.Lei JH, Liu LR, Wei Q, Yan SB, Yang L, et al. Circumcision status and risk of HIVacquisition during heterosexual intercourse for both males and females: a meta-analysis. PLoS One. 2015;10:e0125436. doi: 10.1371/journal.pone.0125436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sharma SC, Raison N, Khan S, Shabbir M, Dasgupta P, et al. Male circumcision for the prevention of HIV acquisition: a meta-analysis. BJU Int. 2018;121:515–26. doi: 10.1111/bju.14102. [DOI] [PubMed] [Google Scholar]
- 5.Gray R, Kigozi G, Kong X, Ssempiija V, Makumbi F, et al. The effectiveness of male circumcision for HIV prevention and effects on risk behaviors in a posttrial follow-up study. AIDS. 2012;26:609–15. doi: 10.1097/QAD.0b013e3283504a3f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mehta SD, Moses S, Agot K, Odoyo-June E, Li H, et al. The long-term efficacy of medical male circumcision against HIV acquisition. AIDS. 2013;27:2899–907. doi: 10.1097/01.aids.0000432444.30308.2d. [DOI] [PubMed] [Google Scholar]
- 7.Auvert B, Taljaard D, Rech D, Lissouba P, Singh B, et al. Association of the ANRS-12126 male circumcision project with HIV levels among men in a South African township: evaluation of effectiveness using cross-sectional surveys. PLoS Med. 2013;10:e1001509. doi: 10.1371/journal.pmed.1001509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kong X, Kigozi G, Ssekasanvu J, Nalugoda F, Nakigozi G, et al. Association of medical male circumcision and antiretroviral therapy scale-up with community HIV incidence in Rakai, Uganda. JAMA. 2016;316:182–90. doi: 10.1001/jama.2016.7292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jean K, Lissouba P, Taljaard D, Taljaard R, Singh B, et al. HIV Incidence among women is associated with their partners' circumcision status in the township of orange farm (South Africa) where the male circumcision roll-out is ongoing (ANRS-12126) Abstract FRAE0105LB. Melbourne: 20th International AIDS Conference. 2014 [Google Scholar]
- 10.World Health Organization. WHO progress brief: voluntary medical male circumcision for HIV prevention in 14 priority countries in East and Southern Africa. Geneva: World Health Organization; 2017. [Google Scholar]
- 11.UNAIDS/WHO. Joint strategic action framework to accelerate the scale-up of voluntary medical male circumcision for HIV prevention in Eastern and Southern Africa. 2011 [Google Scholar]
- 12.Tobian AA, Adamu T, Reed JB, Kiggundu V, Yazdi Y, et al. Voluntary medical male circumcision in resource-constrained settings. Nat Rev Urol. 2015;12:661–70. doi: 10.1038/nrurol.2015.253. [DOI] [PubMed] [Google Scholar]
- 13.Ridzon R, Reed JB, Sgaier SK, Hankins C. VMMC devices – introducing a new innovation to a public health intervention. J Acquir Immune Defic Syndr. 2016;72:1–4. doi: 10.1097/QAI.0000000000000967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.UNAIDS. On the fast-track to end AIDS. Geneva: UNAIDS; 2011. [Google Scholar]
- 15.WHO/UNAIDS. A framework for voluntary medical male circumcision: effective HIV prevention and a gateway to improved adolescent boys' & men's health in Eastern and Southern Africa by 2021. Geneva: World Health Organization; 2016. [Google Scholar]
- 16.Samuelson J, Hargreave T, Ridzon R, Farley T. Innovative methods of male circumcision for HIV prevention – getting the right evidence. J Acquir Immune Defic Syndr. 2016;72:5–12. doi: 10.1097/QAI.0000000000000738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sokal DC, Li PS, Zulu R, Awori QD, Combes SL, et al. Randomized controlled trial of the Shang Ring versus conventional surgical techniques for adult male circumcision: safety and acceptability. J Acquir Immune Defic Syndr. 2014;65:447–55. doi: 10.1097/QAI.0000000000000061. [DOI] [PubMed] [Google Scholar]
- 18.Sokal DC, Li PS, Zulu R, Awori QD, Agot K, et al. Field study of adult male circumcision using the Shang Ring in routine clinical settings in Kenya and Zambia. J Acquir Immune Deific Syndr. 2014;67:430–7. doi: 10.1097/QAI.0000000000000321. [DOI] [PubMed] [Google Scholar]
- 19.Kigozi G, Musoke R, Watya S, Kighoma N, Ssebbowa P, et al. The acceptability and safety of the Shang Ring for adult male circumcision in Rakai, Uganda. J Acquir Immune Defic Syndr. 2013;63:617–21. doi: 10.1097/QAI.0b013e3182968dda. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Feldblum PJ, Mwambula C, Selemani M, Long S, Telela DJ, et al. Prospective observational study of the Shang Ring device for adult medical male circumcision in a routine clinical setting in Malawi. Afr J Reprod Health. 2016;20:60–6. doi: 10.29063/ajrh2016/v20i4.6. [DOI] [PubMed] [Google Scholar]
- 21.Kigozi G, Musoke R, Kighoma N, Nkale J, Serwada D, et al. The acceptability and safety of the shang ring for adolescent male circumcision in Rakai, Uganda. AIDS 2014 Poster Presentation TUPE148. 2014 [Google Scholar]
- 22.World Health Organization. Framework for clinical evaluation of devices for male circumcision. Geneva: World Health Organization; 2012. [Google Scholar]
- 23.World Health Organization. Meeting report: WHO technical advisory group on innovations in male circumcision: evaluation of two adult devices. Geneva: World Health Organization; 2013. [Google Scholar]
- 24.World Health Organization. WHO prequalification of male circumcision devices public report product: ShangRingTM number: PQMC 0003-003-00. Geneva: World Health Organization; 2015. [Google Scholar]
- 25.Peng YF, Cheng Y, Wang GY, Wang SQ, Jia C, et al. Clinical application of a new device for minimally invasive circumcision. Asian J Androl. 2008;10:447–54. doi: 10.1111/j.1745-7262.2008.00411.x. [DOI] [PubMed] [Google Scholar]
- 26.Barone MA, Li PS, Awori QD, Lee R, Goldstein M. Clinical trials using the Shang Ring device for male circumcision in Africa: a review. Transl Androl Urol. 2014;3:113–24. doi: 10.3978/j.issn.2223-4683.2014.01.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Masson P, Li PS, Barone MA, Goldstein M. The Shang Ring device for simplified adult circumcision. Nat Rev Urol. 2010;7:638–42. doi: 10.1038/nrurol.2010.167. [DOI] [PubMed] [Google Scholar]
- 28.Cheng Y, Peng YF, Liu YD, Tian L, Lü NQ, et al. A recommendable standard protocol of adult male circumcision with the Chinese Shang Ring: outcomes of 328 cases in China. Zhonghua Nan Ke Xue. 2009;15:584–92. Article in Chinese. [PubMed] [Google Scholar]
- 29.Hart C, Combes S, Li PS, Barone MA, Cheng Y, et al. 19th International AIDS Conference. Washington, DC: 2012. Ease of Shang Ring method key to scale up of male circumcision in Africa. Abstract MOPE683. [Google Scholar]
- 30.Yan B, You H, Zhang K, Tang H, Mao W, et al. Circumcision with the Chinese Shang Ring in children: outcomes of 824 cases. Zhonghua Nan Ke Xue. 2010;16:250–3. Article in Chinese. [PubMed] [Google Scholar]
- 31.Pan F, Pan L, Zhang A, Liu Y, Zhang F, et al. Circumcision with a novel disposable device in Chinese children: a randomized controlled trial. Int J Urol. 2013;20:220–6. doi: 10.1111/j.1442-2042.2012.03132.x. [DOI] [PubMed] [Google Scholar]
- 32.Yang BH, Jia C, Liu T, Peng YF. Novel no-flip Shang Ring circumcision for adult males: a clinical application study of 528 cases. Zhonghua Nan Ke Xue. 2014;20:709–14. Article in Chinese. [PubMed] [Google Scholar]
- 33.Cao DH, Liu LR, Yang L, Qian SQ, Lei JH, et al. No-flip method versus external method for Shang Ring circumcision: a meta-analysis. Zhonghua Nan Ke Xue. 2014;20:1113–9. Article in Chinese. [PubMed] [Google Scholar]
- 34.Lei J, Liu L, Lü X, Cheng S, Cai Y, et al. Circumcision with no-flip Shang Ring technique for adult males: analysis of 168 cases. Zhonghua Nan Ke Xue. 2014;20:320–4. Article in Chinese. [PubMed] [Google Scholar]
- 35.Rech D, Samkange C, Hatzold K, Ridzon R. Adverse event action guide. 2014. [Last accessed on 2018 Oct 24]. Available from: https://www.malecircumcision.org/file/33277/download?token=RwemJMR5 .
- 36.Awori Q, Lee R, Li P, Nyanchoka J, Ouma D, et al. Use of the Shang Ring for male circumcision in boys in Kenya: results from a pilot study. J Int AIDS Soc. 2017;20:1–8. doi: 10.7448/IAS.20.1.21588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Feldblum PJ, Zulu R, Linyama D, Long S, Nonde TJ, et al. Randomized controlled trial of the shangring for adult medical male circumcision: safety, effectiveness, and acceptability of using 7 versus 14 device sizes. J Acquir Immune Defic Syndr. 2016;72:S30–5. doi: 10.1097/QAI.0000000000001015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Barone MA, Awori Q, Li PS, Simba RO, Weaver MA, et al. Randomized trial of the Shang Ring for adult male circumcision with removal at one to three weeks: delayed removal leads to detachment. J Acquir Immune Defic Syndr. 2012;60:82–9. doi: 10.1097/QAI.0b013e31824ea1f2. [DOI] [PubMed] [Google Scholar]
- 39.Centers for Disease Control and Prevention. Progress in voluntary medical male circumcision service provision – Kenya, 2008–2011. MMWR Morb Mortal Wkly Rep. 2012;61:957–61. [PubMed] [Google Scholar]
- 40.Golub G, Herman-Roloff A, Hoffman S, Jaoko W, Bailey RC. The relationship between distance and post-operative visit attendance following medical male circumcision in Nyanza Province, Kenya. AIDS Behav. 2016;20:2529–37. doi: 10.1007/s10461-015-1210-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Masina D, Ndirangu J, Choge I, Dayanund L, Bonnecwe C, et al. Abstract WEPEE489. 21st International AIDS Conference. Durban: 2016. Improving client follow-up in voluntary medical male circumcision (VMMC) programs through continuous quality improvement (CQI): experiences from South Africa. [Google Scholar]
- 42.Cao D, Liu L, Hu Y, Wang J, Yuan J, et al. A systematic review and meta-analysis of circumcision with Shang Ring vs. conventional circumcision. Urology. 2015;85:799–804. doi: 10.1016/j.urology.2014.12.007. [DOI] [PubMed] [Google Scholar]
- 43.World Health Organization. Guideline on the use of devices for adult male circumcision for HIV prevention. Geneva: World Health Organization; 2013. [PubMed] [Google Scholar]
- 44.Tshimanga M, Hatzold K, Mugurungi O, Mangwiro T, Ncube G, et al. Safety profile of PrePex male circumcision device and client satisfaction with adolescent males aged 13–17 years in Zimbabwe. J Acquir Immune Defic Syndr. 2016;72:S36–42. doi: 10.1097/QAI.0000000000000799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lebina L, Taruberekera N, Milovanovic M, Hatzold K, Mhazo M, et al. Piloting PrePex for adult and adolescent male circumcision in South Africa – pain is an issue. PLoS One. 2015;10:e0138755. doi: 10.1371/journal.pone.0138755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Agot K, Ambia J, Bosire R, Muhuaya D, Juma J, et al. Abstract 1067. Boston: CROI; 2018. Safety and acceptability of PrePex circumcision among adolescents in Kisumu, Kenya. [Google Scholar]
- 47.Kripke K, Reed J, Hankins C, Smiley G, Laube C, et al. Impact and cost of scaling up voluntary medical male circumcision for HIV prevention in the context of the new 90-90-90 HIV treatment targets. PLoS One. 2016;11:1–14. doi: 10.1371/journal.pone.0155734. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The original flip and modified no-flip ShangRing techniques.
The healing process after ShangRing circumcision


