It has been 10 years since we published the first report describing use of the ShangRing for circumcision in boys and men. That report, by Peng et al.1 from China, showed that the device was safe and that ShangRing circumcision was quicker than with conventional surgical techniques commonly used. The ShangRing, pictured in Figure 1, is a novel collar clamp circumcision device that was invented by Mr. Jian-Zhong Shang in China in the early 2000s to reduce potential surgical complications following male circumcision. Based on its successful use in 2006, Mr. Shang started SNNDA Medical Company to produce and distribute the ShangRing. The device has two parts consisting of an inner ring and an outer ring. The foreskin is sandwiched between the two rings, ensuring hemostasis without the need for suturing, which greatly simplifies the circumcision. The device is typically removed by a clinician 7–10 days later.
Figure 1.
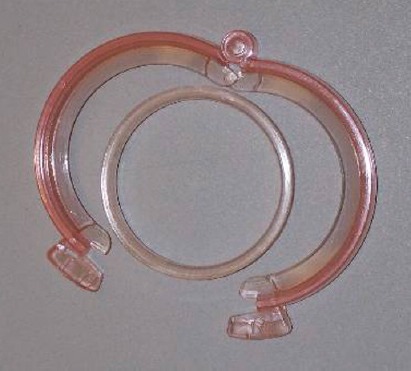
The picture of the ShangRing.
The ShangRing came to the attention of Dr. Philip S Li, a Weill Cornell Medical College urologist, while he attended a meeting at Shanghai Renji Hospital of Shanghai Jiao Tong University School of Medicine in China in December, 2007. Back then, it had only recently been reported that male circumcision significantly reduced the risk of human immunodeficiency virus (HIV) acquisition in men. A number of countries in Sub-Saharan Africa, where HIV prevalence was high and the rate of male circumcision was low, were beginning to develop national strategies for rolling out services for what because known as voluntary medical male circumcision (VMMC). Dr. Li thought that this device, now known as the ShangRing, could potentially play a role in these public health programs, so in 2008, he invited technical advisors from EngenderHealth, Weill Cornell Medical College, FHI 360, and the Bill & Melinda Gates Foundation to visit China with him to explore the device's potential usefulness for circumcision programs in Sub-Saharan Africa.2,3,4 Since then, VMMC has become one of the most promising interventions to reduce HIV transmission, and it now represents a key HIV prevention approach in Sub-Saharan Africa, with national programs established in 14 priority countries, resulting in nearly 19 million VMMCs, primarily in adolescent boys and men.
The ShangRing has been commercially available in China since 2006, with no serious or severe adverse events reported related to its use. The device comes in a number of sizes to suit different penile circumferences, from neonates to adults. It has been safely used for circumcision in more than 1.4 million boys and men since it was introduced in China. Independent experts from a World Health Organization (WHO) Technical Advisory Group reported that over 99% of the circumcisions conducted in African studies using the ShangRing were safely and effectively performed with no serious adverse events.5 Devices like the ShangRing could potentially increase the productivity and efficiency of health care workers in Sub-Saharan Africa, allowing them to perform many more circumcisions per day, at a similar or lower cost.
Much progress has been made over the past 10 years since that original article was published in Asian Journal of Andrology in 2008. In studies conducted in Kenya, Malawi, Uganda, and Zambia, the ShangRing has been shown to be safe, effective, and well-accepted by men and boys and by providers of adult and adolescent VMMC services.6,7,8,9,10,11 The device received a CE mark in 2008, FDA 510(k) clearance in 2012, and the WHO prequalification in 2015. In addition, the use of this innovative no-flip ShangRing technique, spontaneous detachment that reported in this article obtained a new amended WHO prequalification in March 2019. The ShangRing has also been registered for sale in several countries in Africa, including Kenya, Malawi, Namibia, Zambia, and Zimbabwe. Currently, the ShangRing is the only WHO prequalified device for use in boys and men aged 10 years or older in Africa.
While the original ShangRing technique has proven to be very quick, safe, effective, and easy, the procedure has since evolved based on work done in China, to facilitate an even simpler and easier procedure. The results of a study in Kenya show that two of these innovations, a modification of the original technique, called the “no-flip technique,” and spontaneous detachment, where the ring is allowed to fall off on its own (as opposed to removing it 7 days after circumcision), are safe, effective, and acceptable both to clients and providers.12 Other recent research, also conducted in Kenya, has shown that use of topical anesthesia instead of injectable anesthesia is also safe, effective, and acceptable.13 In March 2019, WHO amended the original prequalification to include use of these new innovations, the no-flip technique, spontaneous detachment and use of topical anesthesia. Use of the ShangRing could accelerate task-shifting from physicians to no-physician medical providers in Africa.
Currently, there is ongoing work to assist countries in eastern and southern Africa, including Kenya, Malawi, Mozambique, Namibia, Tanzania, Uganda, and Zambia to introduce the ShangRing into national VMMC programs, which will provide these countries with an opportunity to increase the efficiency and acceptability of VMMC services and may reduce the cost to ensure longer-term sustainability of these programs. Studies are also getting underway in Kenya, Tanzania, and Uganda to explore the use of the ShangRing for early infant male circumcision using topical anesthesia.
Given that the ShangRing can potentially be used with all ages of boys and men, wider introduction of the device could significantly simplify delivery of VMMC services, an important part of comprehensive programs to reduce HIV transmission in Sub-Saharan Africa, helping to achieve the ambitious goal set by the World Health Organization and UNAIDS of achieving 27 million VMMCs by 2020.14
REFERENCES
- 1.Peng YF, Cheng Y, Wang GY, Wang SQ, Jia C, et al. Clinical application of a new device for minimally invasive circumcision. Asian J Androl. 2008;10:447–54. doi: 10.1111/j.1745-7262.2008.00411.x. [DOI] [PubMed] [Google Scholar]
- 2.Lu NQ, Li PS, Huang YR. [An innovative male circumcision technique in China and HIV prevention] Zhonghua Nan Ke Xue. 2008;14:195–6. [PubMed] [Google Scholar]
- 3.Li PS, Lu NQ, Cheng Y, Peng YF, Tian L, et al. [The need for high quality training and surgical standards for adult male circumcision in China. Special report] Zhonghua Nan Ke Xue. 2009;15:390–4. [Article in Chinese] [PubMed] [Google Scholar]
- 4.Lu NQ, Li PS, Sokal D, Cheng Y, Peng YF, et al. [Progress on the clinical studies of male circumcision using the Shang Ring] Zhonghua Nan Ke Xue. 2011;17:195–202. [Article in Chinese] [PubMed] [Google Scholar]
- 5.World Health Organization. Technical Advisory Group on Innovations in Male Circumcision: Evaluation of Two Devices. World Health Organization. 2013. [Last accessed on 2019 April 28]. Available from: https://apps.who.int/iris/bitstream/handle/10665/85269/9789241505635_eng.pdf .
- 6.Cao D, Liu L, Hu Y, Wang J, Yuan J, et al. A systemic review and meta-analysis of circumcision with Shang Ring vs conventional circumcision. Urology. 2015;86:799–804. doi: 10.1016/j.urology.2014.12.007. [DOI] [PubMed] [Google Scholar]
- 7.Barone MA, Li PS, Masson P, Awori Q, Okech J, et al. A pilot study of the Shang Ring: a novel male circumcision device for HIV prevention. J Acquir Immune Defic Syndr. 2011;57:e7–12. doi: 10.1097/QAI.0b013e3182158967. [DOI] [PubMed] [Google Scholar]
- 8.Kigozi G, Masoke R, Watya S, Kighoma N, Ssebbowa PB, et al. The acceptability and safety of the ShangRing for adult male circumcision in Rakai, Uganda. J Acquir Immune Defic Syndr. 2013;63:617–21. doi: 10.1097/QAI.0b013e3182968dda. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sokal DC, Li PS, Zulu R, Awori QD, Combes SL, et al. Randomized controlled trial of the Shang Ring versus conventional surgical techniques for adult male circumcision: safety and acceptability. J Acquir Immune Defic Syndr. 2014;65:447–55. doi: 10.1097/QAI.0000000000000061. [DOI] [PubMed] [Google Scholar]
- 10.Sokal DC, Li PS, Zulu R, Awori QD, Agot K, et al. Field study of adult male circumcision using the ShangRing in routine clinical settings in Kenya and Zambia. J Acquir Immune Deficiency Syndr. 2014;67:430–7. doi: 10.1097/QAI.0000000000000321. [DOI] [PubMed] [Google Scholar]
- 11.Feldblum PJ, Mwambula C, Selemani M, Long S, Telela DJ, et al. Prospective observational study of the ShangRing device for adult medical male circumcision in a routine clinical setting in Malawi. Afr J Reprod Health. 2016;20:60–6. doi: 10.29063/ajrh2016/v20i4.6. [DOI] [PubMed] [Google Scholar]
- 12.Barone MA, Li PS, Lee RK, Ouma D, Oundo M, et al. Simplifying the ShangRing technique for circumcision in boys and men: use of the no-flip technique with randomization to removal at 7 days versus spontaneous detachment. Asian J Androl. 2018 doi: 10.4103/aja.aja_91_18. Doi: 10.4103/aja.aja_91_18. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Barone MA, Awori Q, Lee R, Ouma D, Obura N, et al. Paris: 9th IAS Conference on HIV Science; 2017. [Last accessed on 2019 April 28]. ShangRing circumcision in boys and men with topical vs injectable anesthesia: results from a randomized controlled trial. Available from: http://programme.ias2017.org/PAGMaterial/eposters/2026.pdf . [Google Scholar]
- 14.World Health Organization. A Framework for Voluntary Medical Male Circumcision: Effective HIV Prevention and a Gateway to Improved Adolescent Boys’ & Men's Health in Eastern and Southern Africa by 2021. World Health Organization. 2016. [Last accessed on 2019 April 28]. Available from: http://www.who.int/hiv/pub/malecircumcision/Policy_brief_VMCC_2021_web.pdf?ua=1 .


