ABSTRACT
Zinc is an essential trace element that is crucial for growth, development, and the maintenance of immune function. Its influence reaches all organs and cell types, representing an integral component of approximately 10% of the human proteome, and encompassing hundreds of key enzymes and transcription factors. Zinc deficiency is strikingly common, affecting up to a quarter of the population in developing countries, but also affecting distinct populations in the developed world as a result of lifestyle, age, and disease-mediated factors. Consequently, zinc status is a critical factor that can influence antiviral immunity, particularly as zinc-deficient populations are often most at risk of acquiring viral infections such as HIV or hepatitis C virus. This review summarizes current basic science and clinical evidence examining zinc as a direct antiviral, as well as a stimulant of antiviral immunity. An abundance of evidence has accumulated over the past 50 y to demonstrate the antiviral activity of zinc against a variety of viruses, and via numerous mechanisms. The therapeutic use of zinc for viral infections such as herpes simplex virus and the common cold has stemmed from these findings; however, there remains much to be learned regarding the antiviral mechanisms and clinical benefit of zinc supplementation as a preventative and therapeutic treatment for viral infections.
Keywords: zinc, virus, metallothionein, antiviral, immunity, zinc deficiency, zinc supplementation
Introduction
Zinc deficiency was first recognized by Prasad et al. >50 y ago in a malnourished group of individuals presenting with hepatosplenomegaly, dwarfism, hypogonadism, and an elevated risk of infection (1). Unbeknownst to Dr. Prasad and his colleagues at the time, their discovery would highlight the importance of zinc as an integral component of human physiology, and inspire decades of zinc research. It is now understood that zinc is the second-most abundant trace metal in the human body after iron, and an essential component of protein structure and function. Importantly, zinc is a structural constituent of ∼750 zinc-finger transcription factors (2) enabling gene transcription, and is a catalytic component of approximately 2000 enzymes, encompassing all 6 classes (hydrolase, transferase, oxido-reductase, ligase, lyase, and isomerase) (3). Hence, zinc is biologically essential for cellular processes, including growth and development, as well as DNA synthesis and RNA transcription (4).
The global prevalence of zinc deficiency is estimated to range from ∼17% to 20% (5, 6), with the vast majority occurring in developing countries of Africa and Asia. Although significantly less common in high-income nations, zinc deficiency occurs most frequently in the elderly, vegans/vegetarians, and individuals with chronic disease such as liver cirrhosis (7) or inflammatory bowel disease (8). Importantly, zinc deficiency results in a compromised immune system, as evidenced by thymic atrophy, lymphopenia, and defective lymphocyte responses in animal studies (9). These data underscore the importance of zinc nutrition, particularly in underdeveloped countries where the risk of infection is heightened because of poor sanitation, public health, and vaccination strategies (5).
This review focuses on the role of zinc as an essential micronutrient that is required to mount an effective antiviral response. Although zinc possesses direct antiviral properties (e.g. influenza), it is also critical in generating both innate and acquired (humoral) antiviral responses. To complicate matters, zinc is an integral component of many viral enzymes, proteases, and polymerases, highlighting the importance of regulating cellular and systemic zinc distribution to inhibit viral replication and dissemination.
Current Status of Knowledge
Zinc homeostasis and viral infection
Systemic and intracellular zinc are tightly regulated, such that free zinc ions (Zn2+) represent a minimal fraction of total cellular zinc (∼0.0001%) (10–12). The vast majority of zinc remains bound to zinc-binding proteins such as serum albumin or intracellular metallothionein proteins, where it can be transferred to zinc-binding enzymes and transcription factors as necessary. Zinc transport is principally mediated by 2 groups of proteins: the ZnT [solute-linked carrier 30 (SLC30A)] family, which is responsible for efflux of zinc outside the cell or influx into organelles, and the ZIP [Zrt- and Irt-like proteins (SLC39A)] family of proteins, which performs the opposite role, transporting zinc into the cytoplasm from extracellular sources or cellular organelles (13). The >30 human proteins responsible for zinc homeostasis collectively ensure that zinc does not become toxic in the case of dietary excess, nor limited in the case of dietary insufficiency. Of course, this balance cannot be maintained indefinitely, and may result in zinc-induced copper deficiency if consumed in excess (14), and severe zinc deficiency if it is lacking in the diet (1).
Sequestration and toxic accumulation of metals are well-documented antibacterial immune responses. Calprotectin is a prime example, binding and sequestering extracellular calcium and zinc, thus preventing bacterial and fungal overgrowth (15). Conversely, toxic endosomal zinc accumulation can inhibit intracellular Mycobacterium growth in macrophages (16). Unfortunately, these mechanisms are not well described in the case of viral infections, perhaps because of a lack of efficacy. Calprotectin, for example, has no proven antiviral role, nor is it significantly upregulated in response to viral gastroenteritis (17). This absence of a zinc-mediated antiviral response may reflect the “parasitic” nature of viral infection, hijacking host machinery to self-replicate. Changes in intracellular zinc concentrations necessary to inhibit viral replication may also prove toxic to eukaryotic cells for the same reason.
Although antiviral modulation of zinc homeostasis in humans remains unproven, papilloma viruses have evolved mechanisms to alter zinc homeostasis to favor viral replication and persistence (18). The human papilloma virus (HPV) E5 protein can interact with the zinc transporter ZnT-1 in complex with EVER2, thus stimulating nuclear accumulation of zinc (19). The ZnT-1:EVER2 complex responsible for zinc export from the nucleus is inhibited by HPV E5, subsequently increasing both nuclear zinc and the activation of AP1 (20), a transcription factor required for HPV genome expression. Interestingly, homozygous mutations in either EVER1 or EVER2 result in a rare condition termed epidermodysplasia verruciformis (EV). EV patients are particularly susceptible to HPV strains 5 and 8, which significantly increases the risk of developing nonmelanoma skin cancers. HPV strains 5 and 8 lack expression of the E5 protein, which may explain 1) their limited replication in the normal population because of their inability to control zinc homeostasis, and 2) the susceptibility of EV patients to strains 5 and 8 from the loss of EVER protein function, favoring HPV replication. Interestingly, HPV E5 genes have co-evolved with the major HPV oncogenes, E6 and E7, and indicate the potential involvement of E5 in carcinogenesis (21, 22). Clinical trials using both oral and topical zinc have proven effective for the treatment of viral warts, and will be reviewed in a later section.
Metallothioneins, zinc homeostasis, and antiviral activity
Metallothioneins are small, cysteine-rich proteins capable of binding divalent cations such as zinc and copper. As vessels for much of the labile intracellular zinc pool, metallothioneins possess numerous functions through their ability to bind and release metals from their thiol groups. These include storage and transfer of zinc ions and heavy metal detoxification, as well as involvement in oxidative stress, apoptosis, and immune responses (23). Humans express 4 metallothionein isoforms (MT1–4), including the ubiquitously expressed MT1 and MT2 genes (MT1A, B, E, F, G, H, I, J, L, M, X, MT2A), as well as MT3 and MT4 whose expression is limited, and function remains poorly understood (24). Importantly, MT1 and 2 gene expression is extremely responsive to zinc, and therefore serves as an ideal indicator of an individual's zinc status (25). Upon taking a zinc supplement, for example, an increase in protein-bound zinc in the bloodstream is internalized by cells in various tissues and organs through the ZIP transporters. In response to increased intracellular zinc, the metal-responsive transcription factor (MTF1) becomes active, and binds the metal responsive element in metallothionein gene promoters to upregulate their transcription (26). Although there are additional stimuli that influence metallothionein expression, this primarily occurs in a zinc-dependent fashion. Oxidative stress, for example, induces zinc release from metallothioneins as a mechanism to reduce reactive oxygen species generated by mitochondrial dysfunction or viral infection (26). Zinc released from metallothioneins binds MTF1 to stimulate additional metallothionein expression.
It should be noted that metallothioneins, although highly responsive to zinc, have long been classified as interferon stimulated genes (ISGs) (27). IFNs are immunostimulatory cytokines secreted from infected cells and nearby immune cells that induce the expression of hundreds of antiviral genes. They possess diverse roles including chemoattraction, immune cell activation, and direct antiviral activity. In response to IFNs, we suggest that there are 2 mechanisms of metallothionein induction. Most ISGs possess binding sites for STAT- or IFN regulatory factor (IRF) transcription factor-mediated expression, as is the case for MT1X and MT2A (28, 29). Other metallothioneins such as MT1F and MT1G do not possess known IFN regulatory regions in their promoters, but are instead more sensitive to zinc (28). IFNs stimulate an influx of zinc into the target cell, as is the case with some inflammatory cytokines such as IL-6, which in turn drives metallothionein expression.
Because metallothioneins possess such a diverse functional repertoire, their specific roles during viral infection remain undefined. However, both in vitro and in vivo studies have made it abundantly clear that metallothioneins are induced by viruses. The mechanisms often remain undefined; however, metallothionein expression has been attributed to zinc influx or redistribution (19, 28), by viral means, cytokine exposure, or oxidative stress (30). Metallothionein upregulation has been observed in response to measles virus (31), influenza (31, 32), HIV (33), hepatitis C virus (HCV) (34), and coxsackie virus (35), among others. In the case of HIV, zinc appears to be the key driver of metallothionein expression to favor viral persistence. HIV-infected monocytes demonstrate a significant increase in both MT1 gene expression as well as intracellular zinc (33). Elevated intracellular zinc increases monocyte resistance to apoptosis via inhibition of caspase 3 activation [as has been reported previously (36)], thus providing a reservoir for HIV replication. The role of metallothioneins remains unclear in this study; however, they have been described as negative regulators of apoptosis, albeit not through direct caspase 3 inhibition (37). Zinc and metallothioneins also facilitate human cytomegalovirus (HCMV) replication by activating the immediate-early HCMV promoter (38, 39). Kanekiyo et al. demonstrated that both zinc and metallothionein overexpression increased NF-κB binding in the HCMV promoter. Because no complex was detected between metallothionein and NF-κB, it was suggested that metallothioneins served as a zinc donor necessary for NF-κB binding. In addition, as NF-κB transcription factors are known potent activators of HIV and HSV replication, and several other viruses (40), metallothioneins may be proviral. Zinc has also been reported to inhibit NF-κB in numerous studies (41–43). Despite these contrasting data, Kim et al. have bridged these inconsistencies, demonstrating that MT2A can serve as a sink for excess zinc (44), thus limiting its proximity to NF-κB and favoring NF-κB-mediated transcription.
In the case of HCV infection, metallothioneins possess an antiviral role. Using a pan-metallothionein siRNA to knockdown all MT1 and 2 genes, we demonstrated both an increase in HCV replication and a decrease in intracellular zinc content in vitro (34). Interestingly, although ZnSO4 can reduce HCV replication, this effect was ablated when metallothionein genes were knocked down. These data suggest that metallothioneins are either 1) directly antiviral, potentially by sequestering zinc away from viral metalloproteins such as HCV NS5A (45), or 2) indirectly antiviral by acting as zinc chaperones and facilitating antiviral signaling. Further, metallothioneins possess antiviral properties against other viruses as well, as demonstrated in an antiviral screen of 380 human ISGs performed by Schoggins et al. (46). Overexpression of multiple members of the MT1 family inhibited replication of flaviviruses including yellow fever virus and HCV, as well as the alphavirus Venezuelan equine encephalitis virus. This effect was not observed in West Nile virus, and Chikungunya virus. These data indicate that metallothioneins, like many ISGs, are selectively antiviral, perhaps reflecting specific viral zinc requirements during replication. This is particularly evident for HIV, which demonstrated an increase in viral replication as a result of metallothionein overexpression in the Schoggins et al. ISG screen (46), validating previous works (33).
Zinc as an antiviral: bench to bedside and back again
Many studies have evaluated the efficacy of zinc as an antiviral agent in vitro. Unfortunately, zinc concentrations used to assess antiviral activity often far exceed physiological concentrations. Human plasma zinc, for example, ranges from approximately 10 to 18 µM (47), whereas antiviral concentrations of zinc can reach into mM concentrations (48). Intracellular zinc concentrations range from 10s to 100s of µM, but are significantly buffered by zinc-binding proteins such as metallothioneins, rendering free zinc concentrations at picomolar to low nanomolar concentrations (49, 50). The antiviral properties of zinc are certainly virus-specific, but it would appear that zinc ion availability plays a significant role in the antiviral efficacy of zinc (51). Here we describe the role of zinc as a virus-specific antiviral: both in vitro mechanistic studies, as well as human-based clinical trials using zinc supplementation. In vitro and in vivo studies are summarized in Tables 1 and 2, respectively.
TABLE 1.
In vitro studies assessing the antiviral efficacy of zinc1
| Virus | Antiviral effect | Zinc | Effective dose | Reference |
|---|---|---|---|---|
| Coronavirus | Inhibition of RdRp template binding and elongation | PT + Zn(OAc)2 | 2–320 μM PT + 2–500 μM Zn | (60) |
| Encephalomyocarditis virus | Inhibition of viral polyprotein cleavage | ZnCl2 | 0.4–1.5 mM | (61) |
| Inhibition of viral polyprotein cleavage | ZnCl2 | 0.1–1 mM | (62) | |
| Inhibition of viral polyprotein tertiary structure | PT, HK | 5–20 μM PT, 60–125 μM HK | (63) | |
| Inhibition of viral polyprotein tertiary structure | PDTC | 15–125 μM PDTC | (63) | |
| Foot and mouth disease virus | Inhibition of viral polyprotein cleavage | ZnCl2, Zn(OAc)2 | 0.1–2 mM | (64) |
| Inhibition of viral RNA and procapsid synthesis | ZnCl2 | 10–150 μM | (65) | |
| Hepatitis C virus | Inhibition of RNA polymerase | ZnCl2 | 60–300 μM | (66) |
| Inhibition of viral replication | ZnCl2, ZnSO4 | 50–150 μM | (67) | |
| Metallothionein-dependent inhibition of viral replication | ZnSO4 | 50 μM | (34) | |
| Herpes simplex virus | Viral protein synthesis | ZnSO4 | N/A | (53) |
| Inhibition of viral DNA polymerase | Zn(OAc)2 | 0.1–2 mM | (52) | |
| Free virus inactivation | ZnSO4 | 0.1–6 mM | (48) | |
| Free virus inactivation | Zn(Glu)2, Zn(Lac)2 | 1–50 mM | (54) | |
| Inhibition of protein ubiquitination and NF-κB activity | PT | 1.2–18.9 mM | (41) | |
| Human immunodeficiency virus | HIV protease inhibition | Not listed | 0.2–2 mM | (68) |
| Inhibition of viral transcription and particle production | ZnCl2 | 70–700 μM | (69) | |
| Inhibition of reverse transcriptase | ZnCl2 | 25–800 μM | (70) | |
| Human papilloma virus | Stimulates proviral transcription factor activity, reversed by EVER2 | N/A | N/A | (19) |
| Inhibition of viral protein E6 and E7 synthesis stimulating apoptosis | CIZAR | 500–750 μM | (71) | |
| Respiratory syncytial virus | Reduction in viral titer and plaque count | ZnCl2, Zn(OAc)2, Zn(Lac)2 | 0.01–10 mM | (72) |
| Rhinovirus | Inhibition of viral polyprotein cleavage | ZnCl2 | 100–800 μM | (73, 74) |
| Inhibition of viral polyprotein cleavage | ZnCl2 | 0.1–1.2 mM | (61) | |
| Inhibition of viral polymerase | not listed | >0.6 μM | (75) | |
| Inhibition of viral polyprotein processing | PT, HK | 5–20 μM PT, 60–125 μM HK | (63) | |
| Inhibition of viral polyprotein processing | PDTC | 15–125 μM PDTC | (63) | |
| Semliki Forest virus | Inhibition of endosomal membrane fusion | ZnCl2 | 25–100 μM | (76) |
| Inhibition of endosomal membrane fusion | ZnCl2 | 2 mM | (77) | |
| Sindbis virus | Inhibition of viral particle production and polyprotein cleavage | ZnCl2 | 0.1–1.8 mM | (78) |
| Transmissible gastroenteritis virus | Inhibition of viral RNA and protein synthesis | ZnCl2, ZnSO4 | 10–200 μM | (79) |
| Vaccinia virus | Inhibition of RNA synthesis and viral yield | ZnSO4 | 100–300 μM | (80) |
| Inhibition of viral particle production and polyprotein cleavage | ZnCl2 | 50–400 μM | (81) | |
| Inhibition of viral topoisomerase | Not listed | 2.5 mM | (82) | |
| Varicella-zoster virus | Free virus inactivation | Zn(Pic)2, Zn(Asp)2 | 10 μM | (59) |
1CIZAR, zinc citrate compound; HK, hinokitiol; N/A, not applicable; PDTC, pyrrolidine-dithiocarbamate; PT, pyrithione; RdRp, RNA-dependent RNA polymerate; Zn(Asp)2, zinc aspartate; ZnCl2, zinc chloride; Zn(Glu)2, zinc gluconate; Zn(Lac)2, zinc lactate; Zn(OAc)2, zinc acetate; Zn(Pic)2, zinc picolinate; ZnSO4, zinc sulfate.
TABLE 2.
Human clinical studies using zinc as an antiviral therapy 1
| Viral infection/condition | Antiviral/therapeutic effect | Effective dose | Treatment | Reference |
|---|---|---|---|---|
| Torque teno virus | Reduced viral load following stem cell transplant | 600 mg ZnSO4/d | Oral | (83) |
| Herpes simplex | Reduced duration and severity of outbreak | ZnO/glycine cream (0.3% ionic Zn) | Topical | (57) |
| Reduction in outbreak recurrence | 0.025% ZnSO4 solution | Topical | (84) | |
| Reduction in outbreak recurrence | 1–4% ZnSO4 solution | Topical | (58) | |
| Experimental rhinovirus | Reduced duration of illness with Zn(Glu)2 only | Zn(Glu)2 (13.3 mg) or Zn(OAc)2 (5/11.5 mg) lozenges, every 2–3 h/d | Lozenge | (85) |
| Common cold | Reduced symptom severity, frequency, and duration | ZGG lozenges containing 23 mg Zn, every 2 h/d | Lozenge | (86) |
| Reduced symptom severity, frequency, and duration | ZGG lozenges containing 24 mg Zn, every 2–3 h/d (Max 8) | Lozenge | (87) | |
| Reduced duration of symptoms | ZGG lozenges containing 13 mg Zn, every 2 h/d | Lozenge | (88) | |
| Reduced symptom severity and duration | Zn(OAc)2 lozenges each containing 9 mg Zn, every 2 h/d | Lozenge | (89) | |
| Reduced symptom severity and duration | Zn(OAc)2 lozenges each containing 13 mg Zn, every 2–3 h/d | Lozenge | (90) | |
| No effect on duration or severity | Zn(Glu)2 (13.3 mg) or Zn(OAc)2 (5/11.5 mg) lozenges, every 2–3 h/d | Lozenge | (85) | |
| Reduced symptom severity and duration | Zn(OAc)2 lozenges each containing 13 mg Zn, every 2–3 h/d | Lozenge | (91) | |
| Viral warts | Improved clearance of warts after 1–2 mo | 10 mg/ kg ZnSO4 to a maximum dose of 600 mg/d | Oral | (92) |
| Clearance of warts based on concentration of zinc used | 3 × 5 or 10% ZnSO4/d | Topical | (93) | |
| Improved clearance of warts after 1–2 mo | 10 mg/ kg ZnSO4 to a maximum dose of 600 mg/d | Oral | (94) | |
| No benefit | 10 mg/ kg ZnSO4/d | Oral | (95) | |
| Resolution of 88% of lesions after 6 wk/3 sessions | Up to 3 intralesional injections with 2% ZnSO4 | Injection | (96) | |
| Laryngeal papillomatosis | Resolution of papillomatosis (2 case studies) | 10 mg/ kg ZnSO4/d | Oral | (97) |
| HIV | Reduced infection, increased CD4 T cell count | 200 mg/d ZnSO4/d | Oral | (98) |
| Increased CD4 T cell count | 45 mg Zn(Glu)2 every 8 h for 15 d, then 15 mg for 15 d | Oral | (99) | |
| Reduced incidence of diarrhea | 10 mg elemental zinc as ZnSO4/d | Oral | (100) | |
| No benefit | 25 mg/d ZnSO4/d | Oral | (101) | |
| Chronic hepatitis C virus | Enhanced response to IFN treatment | 2 × 75 mg polaprezinc/d | Oral | (102) |
| No benefit to IFN treatment response | 5 × 78 mg Zn(Glu)2/d | Oral | (103) | |
| Reduced serum AST, ALT, and ferritin | 3 × 75 mg polaprezinc/d | Oral | (104) | |
| Reduced serum ALT and Th2 cells (%) | 2 × 75 mg polaprezinc/d | Oral | (105) | |
| Reduced incidence of HCC (albumin-dependent) | 2 × 150 mg polaprezinc/d | Oral | (106) |
1ALT, alanine aminotransferase; AST, aspartate aminotransferase; HCC, hepatocellular carcinoma; ZGG, zinc gluconate/glycine; Zn(Glu)2, zinc gluconate; ZnO, zinc oxide; Zn(OAc)2, zinc acetate; ZnSO4, zinc sulfate.
Herpesviridae
The effect of zinc on HSV-1 and -2 has been studied for >40 y, with in vitro studies suggesting that zinc plays an inhibitory role on almost every aspect of the viral life cycle: viral polymerase function (52), protein production and processing (53), and free virus inactivation (48, 54). Although these studies were performed >20 y ago, a more recent study using the zinc ionophore pyrithione demonstrated a reduction in HSV replication from reduced NF-κB activation by interfering with the protein ubiquitination pathway (41). Unfortunately, no recent experimental data can demonstrate with any certainty the mechanism by which zinc inhibits HSV infection. Nonetheless, in vivo studies in mice and humans have shown a significant reduction of infection and disease burden. Mouse studies performing intravaginal zinc inoculation in liquid (55) or gel (56) form both resulted in significant reductions in HSV-2 infection. Several topical zinc application studies have been performed in humans, which demonstrated a significantly reduced recurrence and duration of infection (outbreak) (57–58). The efficacy of topical application, together with in vitro results (48, 54), suggest that free zinc may indeed coat HSV virions, thus preventing infection. Further research into this molecular mechanism is warranted.
Apart from HCMV mentioned above, the effect of zinc on other members of the Herpesviridae family remains unknown because of a lack of clinical data. Mechanistically, zinc ions have been shown to inhibit Varicella-Zoster virus by inactivating free virus in vitro (59). Both HSV and Varicella-Zoster virus belong to the Alphaherpesvirinae subfamily, reflecting their genetic relatedness, and similar mechanism of inhibition.
Picornaviridae
It was clear as early as 1974 that zinc possessed an inhibitory effect on picornovirus polyprotein processing (73). Before 1980, zinc inhibition of picornovirus proteases from human rhinovirus isolates (73, 74), encephalomyocarditis virus (62), poliovirus (61), and foot and mouth disease virus (64, 65) had all been demonstrated. More recent studies using zinc ionophores have illustrated that zinc interferes with the autocatalytic processing of the viral protease 3CDpro into 3Cpro in the picornavirus coxsackievirus B3, thus inhibiting processing of the viral polyprotein (107). However, this was not the case for encephalomyocarditis virus, where zinc appeared to inhibit the tertiary structure within the viral polyprotein (107). Together, these data suggest that zinc may interfere with proteolytic processing of the viral polyprotein because of misfolding, or through direct actions on the viral protease 3CDpro.
Clinical studies using zinc supplementation are primarily limited to rhinovirus infection, and are often grouped with other “common cold” viruses such as influenza and coronaviruses. The majority of studies use zinc lozenges with various zinc formulations and concentrations, possibly explaining the large variability in results [extensively reviewed in (108) and (109)]. Importantly, the amount of ionic zinc present at the site of infection (oral and nasal mucosa) is highly correlated to the study outcome (51, 108), and is dependent on the zinc formulation. At a physiological pH and 37°C, zinc gluconate for example, releases high amounts of ionic zinc, whereas zinc aspartate releases none (108). Upon examining only the relevant studies where high doses of ionic zinc were used, a clear reduction in cold duration of 42% was calculated (109). Whether this was caused by viral inhibition, improved local immune response, or an amelioration of symptoms remains uncertain.
Other respiratory tract infections: influenza, coronavirus, and metapneumovirus
Few studies have examined the antiviral effects of zinc on other respiratory viruses. In vitro replication of influenza (PR/8/34) is significantly inhibited by the addition of the zinc ionophore pyrrolidine dithiocarbamate (110), perhaps through inhibition of the RNA-dependent RNA polymerase (RdRp), as had been suggested 30 y earlier (111). In similar fashion, severe acute respiratory syndrome (SARS) coronavirus RdRp template binding and elongation was inhibited by zinc in Vero-E6 cells (60). Moreover, zinc salts were shown to inhibit respiratory syncytial virus, even while zinc was incubated with HEp-2 cells only before infection, and then removed (72). The authors suggest that this indicates an inhibitory mechanism similar to HSV by preventing viral membrane fusion; however, no measures were taken to assess changes in intracellular zinc content, nor inhibition of other aspects of the viral life cycle.
Flaviviridae: a focus on HCV
Flaviviruses represent a number of insect-borne viruses including dengue and West Nile virus, as well as the hepatotrophic virus, HCV. The effect of zinc on insect-borne flaviviruses is scarce; however, in vitro studies by our group (34) and others (67) have demonstrated that zinc salts can reduce HCV replication (∼50% at 100 µM ZnSO4), perhaps by inhibiting the HCV RdRp, as shown in E. coli [half maximal inhibitory concentration (IC50) ∼60 µM] (66). Although this is a potential mechanism, it has not been examined in eukaryotic cells in which zinc homeostasis is significantly different.
If left untreated, HCV becomes a chronic hepatic infection in around two-thirds of individuals (112), resulting in a significant reduction in plasma zinc (113). Consequently, zinc supplementation in HCV studies have focused on improved patient outcomes, particularly decreased liver inflammation, and enhanced response to antiviral treatment. Supplementation with 150 mg/d polaprezinc (a bioavailable zinc l-carnosine chelate) has been shown to reduce markers of hepatic inflammation alanine aminotransferase and aspartate aminotransferase alone (105), and in combination with the antiviral treatment IFN-α (106). Moreover, polaprezinc significantly improved the rate of viral clearance, particularly in patients with lower viral loads at baseline (102). The mechanisms underlying these observations remain uncertain; however, are likely a combination of direct antiviral effects and strengthening of the antiviral response. Zinc supplementation and the antiviral response is reviewed below.
Togaviridae
Like flaviviruses, togaviruses primarily consist of arthropod-borne viruses such as Semliki Forest virus, Western equine encephalitis virus, and Chikungunya virus. Viral infection occurs by receptor-mediated endocytosis, followed by fusion of virus and endosomal membranes, and particle release into the cytoplasm (114). Using liposome (76), red blood cell (115), and BHK-21 (77) cell model systems, zinc has been shown to efficiently inhibit membrane fusion of Semliki Forest virus and sindbis viruses. Zinc ions interfere with membrane fusion by binding to a specific histidine residue revealed on the viral E1 protein at low endosomal pH (77). Unfortunately, the in vivo relevance of this model is unclear because of the high concentration of zinc (>1 mM) used. Notably, concentrated zinc is present in vesicular zincosomes that are thought to serve as intracellular zinc storage vesicles (116). Similar to the mechanism used by macrophages to inhibit intracellular Mycobacterium spp., zincosome fusion to viral endosomes may inhibit key aspects of the viral life cycle such as togavirus membrane fusion.
Retroviridae: HIV
Retroviruses are named after their ability to transcribe RNA into DNA using their unique reverse transcriptase (RT), consequently allowing integration of retroviral DNA into the host genome. The integrated provirus can then establish a latent infection for the life of the host and is a major barrier to virus cure strategies, particularly for HIV-1 (117). Similar to viral RdRps, zinc has also been identified as an inhibitor of retrovirus RTs (118, 119). Fenstermacher and DeStefano demonstrated in 2011 that Zn2+ cations can displace Mg2+ ions from HIV-1 RT, promoting the formation of an excessively stable, but incredibly slow and inefficient replication complex (70). Zinc was also shown to inhibit the HIV-1 protease in 1991 (68), and to inhibit viral transcription in 1999 (69), but has received little attention since, with the exception of molecular simulation experiments that identified the zinc-binding sites at the catalytic aspartate-25 residue (120). As stated above, HIV can also stimulate zinc influx into monocytes (33), which may appear contradictory based on its antiretroviral properties. Latently infected monocytes and macrophages, however, can act as viral reservoirs for HIV (121), and could therefore benefit from zinc-mediated inhibition of cell death. In fact, unlike the majority of CD4+ T cells, low levels of replication in macrophages do not result in cell death (122), making them a viable reservoir, in addition to long-lived resting CD4+ T cells, for viral recrudescence after cessation of antiretroviral treatment.
Zinc deficiency is common in HIV-infected individuals, where it is associated with inflammation (123), immunological failure (124), and death (125). A recent Cochrane Review examined the role of micronutrient supplementation in people living with HIV (126). Although a number of studies demonstrated beneficial effects of zinc supplementation, the majority were underpowered. The authors concluded that zinc supplementation probably increases blood zinc concentration (moderate certainty), and may increase CD4+ counts (low certainty).
Unlike zinc supplements, prophylactic zinc gels have shown a substantial benefit to limit HIV infection in vivo. Complete protection against vaginal SHIV-RT (a simian HIV virus expressing the human RT) infection in macaques was obtained by pretreating animals with an antiviral gel containing 14 mM zinc acetate and 50 µM MIV-150, a reverse transcriptase inhibitor (127). When used alone, zinc acetate is a potent antiviral, providing 66% protection against SHIV-RT vaginal infection (56) and an EC50 <100 µM in peripheral blood mononuclear cells against a range of HIV strains (128). Importantly, zinc treatment did not affect viral titers in macaques that became infected, nor did it result in zinc resistant HIV mutants with conserved pol (RT) mutations. These data suggest that zinc may not interfere with the HIV RT, but instead inactivate free virus or prevent viral attachment/penetration as reported for HSV (48, 54).
Papillomaviridae
HPVs are oncogenic viruses that infect basal epithelial cells, where they stimulate proliferation resulting in warts. Although cutaneous warts are usually self-limiting and harmless, mucosal strains of HPV (e.g. high risk HPV-16 and -18) are a primary cause of cervical cancers (129). HPV oncoproteins E6 and E7 in particular, are significant drivers of cell proliferation and resistance to cell death by stimulating the degradation of tumor suppressor p53 and pRb, respectively [reviewed in (130)]. Although nuclear zinc appears to enhance HPV replication (see Zinc homeostasis and viral infection), exogenous zinc treatment (CIZAR, zinc chloride and citric acid anhydrous) can effectively inhibit production of viral oncogenic proteins E6 and E7 (71). The inhibition of E6 and E7 by zinc results in apoptosis of cervical carcinoma cells, as they regain the function of tumor suppressors p53 and pRb (71). The mechanism by which zinc downregulates E6 and E7 expression is unknown, but may be preceded by a zinc-driven blockade in another component of the viral life cycle.
It would appear that both topical and oral zinc supplementation strategies have proven tremendously effective for cutaneous and genital warts. Unfortunately, the vast majority of studies are either underpowered, lacking suitable controls, or single case studies. Nonetheless, a recent systematic review concluded that zinc supplementation was the most effective systemic treatment for cutaneous warts, when compared to other available options (131). It should be noted, however, that individuals with persistent viral warts are often zinc-deficient or have lower concentrations than their healthy counterparts (132). In fact, studies demonstrating the most significant responses to zinc treatment had engaged patients that were primarily zinc-deficient (>70 µg/dL) (92, 94). Nonetheless, 78% (94) and 100% (92) of patients showed clearance of lesions in response to oral zinc sulfate (10 mg/kg up to 600 mg/d) compared to 13% and 0% of the placebo group, respectively. Topical zinc formulations have also proved efficacious for treatment of viral warts. A small study using a 4-wk topical 10% zinc sulfate regimen for plane warts demonstrated an 86% response rate (6/7), compared to a 10% response rate (1/10) in the control group (93).
Recent work suggests that treatment of vaginal HPV infections with topical zinc formulations may benefit the millions of women that remain unvaccinated against HPV. A recent pilot study demonstrated that intravaginal infusion of 500 µM zinc citrate in women diagnosed with high-risk HPV resulted in a 64% clearance rate, compared to 15% in the control group (133). Additional studies in mice have demonstrated that MZC, a formulation containing MIV-50, zinc acetate, and carrageenan, efficiently inhibited vaginal and anorectal HPV-16 pseudoviral particle infection (134).
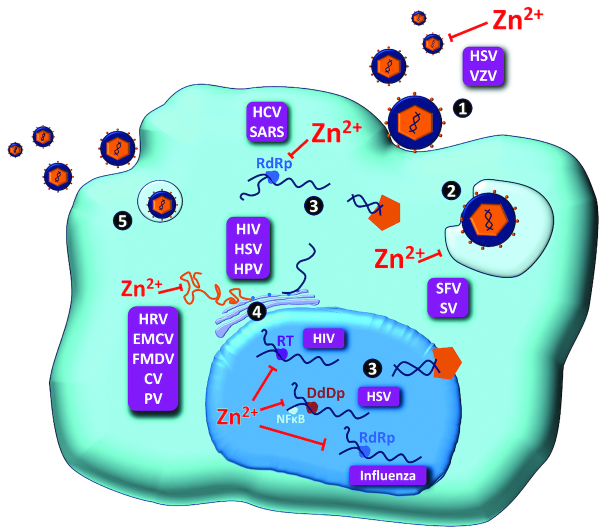
In summary, it is evident that zinc possesses antiviral properties against a number of viral species. Although mechanistic studies are lacking, zinc appears to inhibit viral protease and polymerase enzymatic processes, as well as physical processes such as virus attachment, infection, and uncoating (Figure 1). Unfortunately, these mechanisms have not been well scrutinized in clinical studies, where zinc may provide inexpensive and effective adjunct treatments for many viral infections.
FIGURE 1.
The diverse stages of viral replication cycles that are inhibited by zinc. In vitro studies have demonstrated a number of mechanisms by which zinc interferes with the viral replication cycle. These include free virus inactivation (1), inhibition of viral uncoating (2), viral genome transcription (3), and viral protein translation and polyprotein processing (4). No studies to date, however, have demonstrated zinc-mediated inhibition of virus assembly and/or particle release. CV, coronavirus; DdDp, DNA-dependent DNA polymerase; EMCV, encephalomyocarditis virus; FMDV, foot and mouth disease virus; HCV, hepatitis C virus; HIV, human immunodeficiency virus; HPV, human papilloma virus; HRV, human rhinovirus; HSV, herpes simplex virus; PV, polio virus; RdRp, RNA-dependent RNA polymerase; RT, reverse transcriptase; SARS, severe acute respiratory syndrome coronavirus; SFV, Semliki Forest virus; SV, sindbis virus; VZV, varicella-zoster virus; Zn, zinc.
The role of zinc in antiviral immune signaling
Ionic zinc possesses unique and distinct antiviral properties against a number of human viruses; however, the antiviral immune response led by IFNs is invariably required to clear infections. Zinc has been shown to contribute to a number of innate and adaptive immune signaling pathways that have been comprehensively reviewed recently (135). As such, this review will focus specifically on the role of zinc in the immune response to viruses.
Viral infections are recognized by a number of innate immune receptors termed pattern recognition receptors (PRRs). These include the cell surface and endosomal Toll-like receptors (TLRs), as well as a variety of cytosolic PRRs such as RIGI, MDA5, and IFI16 that primarily bind viral nucleic acids (136). Following ligand binding, PRRs share a number of downstream signaling intermediates, that ultimately activate both inflammatory (NF-κB, AP1) and innate immune (IRF1/3/7) transcription factors. These transcription factors cooperate to induce expression of IFNs, of which there are 3 types: type I (IFN-α and IFN-β), type II (IFN-γ), and type III (IFN-λs). Type I and III IFNs activate very similar antiviral signaling pathways; however, the type I IFN response is ubiquitous, whereas the type III IFN response is limited to a subset of immune cells, as well as epithelial cells of the liver, gastrointestinal, and pulmonary tracts (137). Although both IFN types bind unique receptors, they activate a common signaling cascade where STAT1 and STAT2 heterodimerize and bind IRF9, followed by translocation into the nucleus and subsequent binding of the IFN-sensitive response element that is present in hundreds of gene promoters. As stated previously, these ISGs possess numerous roles including immune cell chemotaxis and activation, as well as numerous antiviral mechanisms to inhibit viral replication within infected and neighboring cells.
Zinc and pathogen recognition
Upon recognition of microbial antigens by TLRs, a rapid and transient influx of free zinc ions occurs. Interestingly, this has been demonstrated in response to viral stimuli, imiquimod, ssRNA40 (TLR7), and CpG (TLR9), but not polyI: C (TLR3) in the mouse macrophage RAW 264.7 cell line (138). In response to TLR7 activation, zinc was shown to reduce the production of type I IFNs and ISGs CD80 and CD86. Based on results using other stimuli, the authors suggest that zinc can inhibit IRF3-, and perhaps IRF7-dependent IFNB production, by limiting activation and/or nuclear translocation (138). The role of the zinc influx in this context remains undefined, but may reflect a regulatory mechanism to prevent excessive IFN production.
Although no direct inhibition of IRF signaling by zinc has been demonstrated, zinc can modulate a number of factors upstream of IRF activation. For example, the IκB kinase (IKK) members IKKα and IKKβ are inhibited by zinc, albeit at high concentrations of ∼0.5 µM (139). IKKα has been shown to activate IRF7 in response to TLR7/9 stimulation (140), whereas IKKβ (141), IKKε and TANK-binding kinase-1 (TBK1) (142) can activate IRF3 following TLR3 stimuli. Zinc can also stimulate expression of the deubiquitinating enzyme A20 (43) to inhibit the pathogen response. A20 is a regulator of NF-κB- (143), TLR3- (144), and RIGI-mediated (145) IFN production, most likely by targeting PRR signaling components TIR-domain-containing adapter-inducing interferon-β (TRIF), TNF Receptor Associated Factor (TRAF) 2, and TRAF6. A20-deficient cells are hyper-responsive to viral infection, possess increased activation of NF-κB, IRF3, and IRF7, and improved viral clearance (146).
Zinc and the interferon response
After pathogen recognition, NF-κB, AP1, and IRF3/7 bind IFN promoters to stimulate type I/III IFN production. Zinc plays a significant role in the response to IFNs by modulating secretion, cytokine potency, and receptor binding, as well as influencing signaling intermediates and pathway inhibitors. A recent study has demonstrated that intracellular zinc can reduce IFN secretion by destabilizing sortilin mRNA transcripts (147). Sortilin is an endosomal protein that facilitates secretion of cytokines such as IFN-γ and IL6 (148), and its depletion results in a significant reduction in secretion of IFN-α. Consequently, because sortilin ensures trafficking and secretion of numerous cytokines, it is possible that zinc also inhibits the secretion of other IFNs.
Structural studies have demonstrated that zinc ions can mediate dimerization of IFNA molecules (149). Nonetheless, apart from crystallization studies, dimers were difficult to generate despite using concentrated IFN (50 µM) and zinc (1 mM). It is therefore likely that the circulating active form of IFN-α is monomeric. A single study performed in 2001 showed that zinc can increase the antiviral activity of IFN-α 10-fold against rhinovirus challenge (150). Although this study drew radical conclusions, antiviral activity was based on cytopathic effect alone, and its results have not been reproduced since. Moreover, zinc was added before viral infection, which is known to interfere with rhinovirus polyprotein processing (73, 74), as reviewed above.
Unlike type I IFNs, a recent study by our group has shown that zinc can inhibit IFN-λ3 signaling, most likely by preventing receptor binding and subsequent signaling (28). Upon demonstrating in 2014 that metallothionein expression was IFNL genotype-dependent, and inversely associated with ISG expression in HCV (151), we showed that serum zinc was the driver of hepatic metallothionein expression. Although zinc had minimal effect on IFN-α signaling, it could almost ablate IFN-λ3 signaling at a concentration of 50 µM, resulting in a significant reduction in its antiviral activity (28). Interestingly, we found no inhibition of IFN-λ1 activity using 50 µM ZnSO4, suggesting a highly specific interaction. The mechanism by which zinc interferes with the IFN:receptor interaction remains uncertain; however, we have ruled out an effect of zinc on IFN-λ3 disulfide bond formation.
Type I and III IFNs bind to unique receptor complexes composed of IFN-α receptors IFNAR1/IFNAR2 and IFN-λ receptors IFNLR1/IL10RB, respectively, but signal via almost identical pathways. Consequently, zinc may act to reinforce the shared IFN signaling cascade by inhibiting protein tyrosine phosphatase enzymatic activity (152). Following receptor engagement by IFNs, intracellular Janus protein tyrosine kinases Jak1 and Tyk2 become phosphorylated, which in turn phosphorylate STAT molecules to stimulate ISG expression. By dephosphorylating these key signaling molecules, a number of phosphatases have been shown to “put the brakes” on IFN signaling. Phosphatases tyrosine-protein phosphatase non-receptor type 6 (SHP1), type 11 (SHP2), and protein phosphatase 2A (PP2A) have all been shown to inhibit JAK-STAT phosphorylation (153–155), and are all inhibited by zinc ions, predominantly in the nanomolar range (156–158). Interestingly, PP2A can also inhibit the phosphorylation of IRF3, thus regulating antigen recognition by PRRs (159). Conversely, the tumor suppressor phosphatase and tensin homologue (PTEN) stimulates IRF3 activation by removing inhibitory phosphorylation at Ser97 (160), and is also inhibited by zinc at nanomolar concentrations (161). Zinc inhibits numerous pro- and antiviral phosphatases, with the net effect on virus recognition and response being undefined, which clearly requires further study.
To enable a highly controlled IFN response, negative regulators of IFN signaling are often ISGs. These include the suppressors of cytokine signaling (SOCS-1 and SOCS-3), which bind and inhibit JAK protein signaling, thus preventing signaling from numerous inflammatory (IL-6) and antiviral stimuli (162). Interestingly, zinc-driven activation of the MTF-1 transcription factor can induce expression of SOCS-3 in HepG2 cells (163). The zinc importer ZIP-14, which is responsible for zinc influx following inflammatory stimuli, was required for SOCS-3 expression, and may represent yet another zinc-mediated mechanism to limit the inflammatory response. Although the transporter responsible for hepatic zinc influx following IFN stimulation remains unknown, it is perceivable that ZIP-14 may drive zinc influx and subsequent SOCS-3 expression.
Zinc deficiency caused by disease, age, and lifestyle factors: lessons from supplementation
Zinc status is primarily determined by dietary zinc intake; however, additional factors such as dietary composition, alcohol intake, and disease state can significantly reduce zinc uptake and storage, or increase zinc excretion (164). With respect to dietary composition, zinc supplementation as part of a meal can significantly reduce zinc absorption when compared to water-based solutions of zinc (164). Moreover, dietary phytate, a natural chelator of zinc ions that is present in corn, rice, and cereals, can severely restrict zinc absorption (165). Consequently, diets containing high phytate: zinc molar ratios, can result in zinc deficiency, even with adequate zinc intake. Unfortunately, rural diets in low-income nations are often zinc-poor and phytate-rich because of a dietary reliance on rice and vegetables.
Aged individuals are also significantly more susceptible to zinc deficiency, increasing their likelihood of acquiring life-threatening viral infections (166). Ex vivo, zinc supplementation has been shown to improve leukocyte IFN-α production (167) and to reduce mononuclear cell TNF production (168). Year-long supplementation with 45 mg elemental zinc/d in elderly subjects (aged 55–87 y), has also demonstrated a dramatic reduction in the incidence of infection as well as plasma oxidative stress markers (168).
Alcoholism can stimulate severe zinc deficiency developed via numerous sociological and physiological mechanisms, with factors including but not limited to 1) increased urinary zinc excretion (169), 2) reduced zinc intake (poor diet) (170), 3) reduced zinc absorption (171), and 4) and a reduction in hepatic zinc stores (172). Alcohol also stimulates microbial dysbiosis and gastrointestinal permeability (173), a phenotype that can increase the likelihood of viral infection in the gut (174). Importantly, dietary zinc supplementation can improve intestinal barrier dysfunction as a result of alcohol and microbial infection (175, 176).
As previously discussed, zinc deficiency is common among chronic infections such as HPV, HCV, and HIV (113, 123). Consequently, a number of studies have examined the effects of zinc supplementation on antiviral immunity, inflammation, and treatment response. As described above, zinc supplementation can improve HCV treatment response and liver inflammation caused by chronic infection. In addition, long-term zinc treatment over 7 y has been shown to reduce the risk of hepatocellular carcinoma progression in chronic HCV patients, as assessed by multivariate analysis, compared to controls (P < 0.05) (105). Zinc supplementation has also been assessed as an adjunct therapy to antiretroviral administration in patients with HIV. One study reported a 4-fold reduction in the rate of immune failure, as well as decreased diarrhea in patients treated with zinc compared to controls (P < 0.05 for both groups) (124). A more recent study revealed an increase in CD4+ T cell count in patients treated with a combination of zinc and antiretroviral therapy, compared to patients on antiretroviral therapy alone (P < 0.05) (177). Taken together, these data indicate that zinc deficiency is associated with greater disease activity in the context of chronic viral infection. Oral zinc supplementation may act in a synergistic manner when co-administered with antiviral therapy and contribute to improved clinical outcomes.
Vaccination studies
Zinc supplementation during vaccination strategies has provided an opportunity to examine the role of zinc in the humoral response to viruses. A particular focus has been applied to the effect of zinc supplementation on rotavirus vaccination because of the high rate of mortality associated with childhood diarrhea in developing countries. Unfortunately, although zinc deficiency is associated with increased risk of rotavirus gastroenteritis (178), it does not greatly increase the development of humoral immunity followed by vaccination (rotarix), as defined by seroconversion rate (179). Nonetheless, a pooled analysis of randomized trials performed in 2000, demonstrated that zinc supplementation shortens the length of diarrheal episodes and reduced the rate of treatment failure or death by 42% in zinc-deficient children (180).
Comparable studies of supplementation with zinc before vaccination have produced similar disappointing results. Zinc supplementation did not improve seroconversion following administration of the oral poliovirus vaccine in infants (181), nor did it improve the immunological response to HBV (182) or influenza vaccination (183) in the elderly. Although there remains little evidence that zinc improves viral vaccination responses, a small number of studies suggest that zinc may improve antibody titers and antibacterial responses to pneumococcus (184) and cholera infections (185).
Conclusions and Future Perspectives
The tight regulation of zinc homeostasis both systemically and intracellularly indicates that zinc plays an essential role in human health. Although zinc is a component of ∼10% of the human proteome, zinc in different forms (free compared with protein-bound) can stimulate a variety of signaling events, including the antiviral response. In vitro studies suggest that free zinc may possess potent antiviral effects, and are supported by trials of creams, lozenges, and supplements with high free zinc content. Moreover, zinc-binding proteins such as the metallothioneins may possess antiviral roles, although their specific function remains uncertain. Nonetheless, zinc treatment applied at a therapeutic dose and in the right form has the potential to drastically improve the clearance of both chronic and acute viral infections, as well as their accompanying pathologies and symptoms. Consequently, the role of zinc as an antiviral can be separated into 2 categories: 1) zinc supplementation implemented to improve the antiviral response and systemic immunity in patients with zinc deficiency, and 2) zinc treatment performed to specifically inhibit viral replication or infection-related symptoms (75, 78–82, 83, 85–91, 95–101, 103, 104).
Acknowledgments
The authors’ responsibilities were as follows—SR and GA designed the review, all authors performed the study selection, all authors read and approved the final paper.
Notes
Supported by Sylvia and Charles Viertel Charitable Foundation Investigatorship (VTL2015C022).
Author disclosures: SAR, SO, CA, and GA, no conflicts of interest.
Abbreviations used: EV, epidermodysplasia verruciformis; HCMV, human cytomegalovirus; HCV, hepatitis C virus; HPV, human papilloma virus; HSV, herpes simplex virus; IRF, IFN regulatory factor; ISG, interferon stimulated gene; MT, metallothionein isoforms; MTF1, metal-responsive transcription factor; PRR, pattern recognition receptor; RdRp, RNA-dependent RNA polymerase; RT, reverse transcriptase; SOCS, suppressors of cytokine signaling; TLR, Toll-like receptor; ZIP, Zrt- and Irt-like proteins.
References
- 1. Prasad AS, Miale A Jr., Farid Z, Sandstead HH, Schulert AR. Zinc metabolism in patients with the syndrome of iron deficiency anemia, hepatosplenomegaly, dwarfism, and hypogonadism. J Lab Clin Med. 1963;61:537–49. [PubMed] [Google Scholar]
- 2. Lambert SA, Jolma A, Campitelli LF, Das PK, Yin Y, Albu M, Chen X, Taipale J, Hughes TR, Weirauch MT. The human transcription factors. Cell. 2018;172(4):650–65. [DOI] [PubMed] [Google Scholar]
- 3. Andreini C, Bertini I. A bioinformatics view of zinc enzymes. J Inorg Biochem. 2012;111:150–6. [DOI] [PubMed] [Google Scholar]
- 4. Overbeck S, Rink L, Haase H. Modulating the immune response by oral zinc supplementation: a single approach for multiple diseases. Arch Immunol Ther Exp (Warsz). 2008;56(1):15–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wessells KR, Brown KH. Estimating the global prevalence of zinc deficiency: results based on zinc availability in national food supplies and the prevalence of stunting. PLoS One. 2012;7(11):e50568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kumssa DB, Joy EJ, Ander EL, Watts MJ, Young SD, Walker S, Broadley MR. Dietary calcium and zinc deficiency risks are decreasing but remain prevalent. Sci Rep. 2015;5:10974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Himoto T, Masaki T. Associations between zinc deficiency and metabolic abnormalities in patients with chronic liver disease. Nutrients. 2018;10(1). doi: ARTN 88 10.3390/nu10010088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Siva S, Rubin DT, Gulotta G, Wroblewski K, Pekow J. Zinc deficiency is associated with poor clinical outcomes in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2017;23(1):152–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Shankar AH, Prasad AS. Zinc and immune function: the biological basis of altered resistance to infection. Am J Clin Nutr. 1998;68(2):447s–63s. [DOI] [PubMed] [Google Scholar]
- 10. Bozym RA, Thompson RB, Stoddard AK, Fierke CA. Measuring picomolar intracellular exchangeable zinc in PC-12 cells using a ratiometric fluorescence biosensor. ACS Chem Biol. 2006;1(2):103–11. [DOI] [PubMed] [Google Scholar]
- 11. Malavolta M, Costarelli L, Giacconi R, Muti E, Bernardini G, Tesei S, Cipriano C, Mocchegiani E. Single and three-color flow cytometry assay for intracellular zinc ion availability in human lymphocytes with Zinpyr-1 and double immunofluorescence: relationship with metallothioneins. Cytometry A. 2006;69a(10):1043–53. [DOI] [PubMed] [Google Scholar]
- 12. Vinkenborg JL, Nicolson TJ, Bellomo EA, Koay MS, Rutter GA, Merkx M. Genetically encoded FRET sensors to monitor intracellular Zn2+ homeostasis. Nat Methods. 2009;6(10):737–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kambe T, Tsuji T, Hashimoto A, Itsumura N. The physiological, biochemical, and molecular roles of zinc transporters in zinc homeostasis and metabolism. Physiol Rev. 2015;95(3):749–84. [DOI] [PubMed] [Google Scholar]
- 14. Duncan A, Yacoubian C, Watson N, Morrison I. The risk of copper deficiency in patients prescribed zinc supplements. J Clin Pathol. 2015;68(9):723–5. [DOI] [PubMed] [Google Scholar]
- 15. Becker KW, Skaar EP. Metal limitation and toxicity at the interface between host and pathogen. FEMS Microbiol Rev. 2014;38(6):1235–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Botella H, Peyron P, Levillain F, Poincloux R, Poquet Y, Brandli I, Wang C, Tailleux L, Tilleul S, Charriere GM et al.. Mycobacterial p(1)-type ATPases mediate resistance to zinc poisoning in human macrophages. Cell Host Microbe. 2011;10(3):248–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Chen CC, Huang JL, Chang CJ, Kong MS. Fecal calprotectin as a correlative marker in clinical severity of infectious diarrhea and usefulness in evaluating bacterial or viral pathogens in children. J Pediatr Gastroenterol Nutr. 2012;55(5):541–7. [DOI] [PubMed] [Google Scholar]
- 18. Lazarczyk M, Favre M. Role of Zn2+ ions in host-virus interactions. J Virol. 2008;82(23):11486–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lazarczyk M, Pons C, Mendoza JA, Cassonnet P, Jacob Y, Favre M. Regulation of cellular zinc balance as a potential mechanism of EVER-mediated protection against pathogenesis by cutaneous oncogenic human papillomaviruses. J Exp Med. 2008;205(1):35–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kim YM, Reed W, Wu W, Bromberg PA, Graves LM, Samet JM. Zn2+-induced IL-8 expression involves AP-1, JNK, and ERK activities in human airway epithelial cells. Am J Physiol Lung Cell Mol Physiol. 2006;290(5):L1028–35. [DOI] [PubMed] [Google Scholar]
- 21. Bravo IG, Alonso A. Mucosal human papillomaviruses encode four different E5 proteins whose chemistry and phylogeny correlate with malignant or benign growth. J Virol. 2004;78(24):13613–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Schiffman M, Herrero R, Desalle R, Hildesheim A, Wacholder S, Rodriguez AC, Bratti MC, Sherman ME, Morales J, Guillen D et al.. The carcinogenicity of human papillomavirus types reflects viral evolution. Virology. 2005;337(1):76–84. [DOI] [PubMed] [Google Scholar]
- 23. Subramanian Vignesh K, Deepe GS Jr. Metallothioneins: emerging modulators in immunity and infection. Int J Mol Sci. 2017;18(10). doi: 10.3390/ijms18102197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Babula P, Masarik M, Adam V, Eckschlager T, Stiborova M, Trnkova L, Skutkova H, Provaznik I, Hubalek J, Kizek R. Mammalian metallothioneins: properties and functions. Metallomics. 2012;4(8):739–50. [DOI] [PubMed] [Google Scholar]
- 25. Hennigar SR, Kelley AM, McClung JP. Metallothionein and zinc transporter expression in circulating human blood cells as biomarkers of zinc status: a systematic review. Adv Nutr. 2016;7(4):735–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Grzywacz A, Gdula-Argasinska J, Muszynska B, Tyszka-Czochara M, Librowski T, Opoka W. Metal responsive transcription factor 1 (MTF-1) regulates zinc dependent cellular processes at the molecular level. Acta Biochim Pol. 2015;62(3):491–8. [DOI] [PubMed] [Google Scholar]
- 27. Friedman RL, Manly SP, McMahon M, Kerr IM, Stark GR. Transcriptional and posttranscriptional regulation of interferon-induced gene expression in human cells. Cell. 1984;38(3):745–55. [DOI] [PubMed] [Google Scholar]
- 28. Read SA, O'Connor KS, Suppiah V, Ahlenstiel CLE, Obeid S, Cook KM, Cunningham A, Douglas MW, Hogg PJ, Booth D et al.. Zinc is a potent and specific inhibitor of IFN-λ3 signalling. Nat Commun. 2017;8:15245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kent WJ, Sugnet CW, Furey TS, Roskin KM, Pringle TH, Zahler AM, Haussler D. The human genome browser at UCSC. Genome Res. 2002;12(6):996–1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Li K, Prow T, Lemon SM, Beard MR. Cellular response to conditional expression of hepatitis C virus core protein in Huh7 cultured human hepatoma cells. Hepatology. 2002;35(5):1237–46. [DOI] [PubMed] [Google Scholar]
- 31. Zilliox MJ, Parmigiani G, Griffin DE. Gene expression patterns in dendritic cells infected with measles virus compared with other pathogens. Proc Natl Acad Sci U S A. 2006;103(9):3363–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Mindaye ST, Ilyushina NA, Fantoni G, Alterman MA, Donnelly RP, Eichelberger MC. Impact of influenza A virus infection on the proteomes of human bronchoepithelial cells from different donors. J Proteome Res. 2017;16(9):3287–97. [DOI] [PubMed] [Google Scholar]
- 33. Raymond AD, Gekonge B, Giri MS, Hancock A, Papasavvas E, Chehimi J, Kossenkov AV, Nicols C, Yousef M, Mounzer K et al.. Increased metallothionein gene expression, zinc, and zinc-dependent resistance to apoptosis in circulating monocytes during HIV viremia. J Leukoc Biol. 2010;88(3):589–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Read SA, Parnell G, Booth D, Douglas MW, George J, Ahlenstiel G. The antiviral role of zinc and metallothioneins in hepatitis C infection. J Viral Hepat. 2018;25(5):491–501. [DOI] [PubMed] [Google Scholar]
- 35. Ilback NG, Glynn AW, Wikberg L, Netzel E, Lindh U. Metallothionein is induced and trace element balance changed in target organs of a common viral infection. Toxicology. 2004;199(2–3):241–50. [DOI] [PubMed] [Google Scholar]
- 36. Perry DK, Smyth MJ, Stennicke HR, Salvesen GS, Duriez P, Poirier GG, Hannun YA. Zinc is a potent inhibitor of the apoptotic protease, caspase-3—a novel target for zinc in the inhibition of apoptosis. J Biol Chem. 1997;272(30):18530–3. [DOI] [PubMed] [Google Scholar]
- 37. Shimoda R, Achanzar WE, Qu W, Nagamine T, Takagi H, Mori M, Waalkes MP. Metallothionein is a potential negative regulator of apoptosis. Toxicol Sci. 2003;73(2):294–300. [DOI] [PubMed] [Google Scholar]
- 38. Kanekiyo M, Itoh N, Mano M, Kawasaki A, Tanaka J, Muto N, Tanaka K. Cellular zinc status regulates cytomegalovirus major immediate-early promoter. Antiviral Res. 2000;47(3):207–14. [DOI] [PubMed] [Google Scholar]
- 39. Kanekiyo M, Itoh N, Kawasaki A, Tanaka J, Nakanishi T, Tanaka K. Zinc-induced activation of the human cytomegalovirus major immediate-early promoter is mediated by metallothionein and nuclear factor-κB. Toxicol Appl Pharmacol. 2001;173(3):146–53. [DOI] [PubMed] [Google Scholar]
- 40. Zhao J, He SP, Minassian A, Li JH, Feng PH. Recent advances on viral manipulation of NF-κB signaling pathway. Curr Opin Virol. 2015;15:103–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Qiu M, Chen Y, Chu Y, Song S, Yang N, Gao J, Wu Z. Zinc ionophores pyrithione inhibits herpes simplex virus replication through interfering with proteasome function and NF-κB activation. Antiviral Res. 2013;100(1):44–53. [DOI] [PubMed] [Google Scholar]
- 42. Zhou Z, Wang L, Song Z, Saari JT, McClain CJ, Kang YJ. Abrogation of nuclear factor-κB activation is involved in zinc inhibition of lipopolysaccharide-induced tumor necrosis factor-α production and liver injury. Am J Pathol. 2004;164(5):1547–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Prasad AS, Bao B, Beck FWJ, Sarkar FH. Zinc-suppressed inflammatory cytokines by induction of A20-mediated inhibition of nuclear factor-κB. Nutrition. 2011;27(7–8):816–23. [DOI] [PubMed] [Google Scholar]
- 44. Kim CH, Kim JH, Lee J, Ahn YS. Zinc-induced NF-κB inhibition can be modulated by changes in the intracellular metallothionein level. Toxicol Appl Pharmacol. 2003;190(2):189–96. [DOI] [PubMed] [Google Scholar]
- 45. Tellinghuisen TL, Marcotrigiano J, Gorbalenya AE, Rice CM. The NS5A protein of hepatitis C virus is a zinc metalloprotein. J Biol Chem. 2004;279(47):48576–87. [DOI] [PubMed] [Google Scholar]
- 46. Schoggins JW, Wilson SJ, Panis M, Murphy MY, Jones CT, Bieniasz P, Rice CM. A diverse range of gene products are effectors of the type I interferon antiviral response. Nature. 2011;472(7344):481–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Rukgauer M, Klein J, Kruse-Jarres JD. Reference values for the trace elements copper, manganese, selenium, and zinc in the serum/plasma of children, adolescents, and adults. J Trace Elem Med Biol. 1997;11(2):92–8. [DOI] [PubMed] [Google Scholar]
- 48. Kumel G, Schrader S, Zentgraf H, Daus H, Brendel M. The mechanism of the antiherpetic activity of zinc-sulfate. J Gen Virol. 1990;71:2989–97. [DOI] [PubMed] [Google Scholar]
- 49. Krezel A, Maret W. Zinc-buffering capacity of a eukaryotic cell at physiological pZn. J Biol Inorg Chem. 2006;11(8):1049–62. [DOI] [PubMed] [Google Scholar]
- 50. Colvin RA, Bush AI, Volitakis I, Fontaine CP, Thomas D, Kikuchi K, Holmes WR. Insights into Zn2+ homeostasis in neurons from experimental and modeling studies. Am J Physiol Cell Physiol. 2008;294(3):C726–C42. [DOI] [PubMed] [Google Scholar]
- 51. Eby GA. Zinc ion availability—the determinant of efficacy in zinc lozenge treatment of common colds. J Antimicrob Chemother. 1997;40(4):483–93. [DOI] [PubMed] [Google Scholar]
- 52. Fridlender B, Chejanovsky N, Becker Y. Selective inhibition of herpes simplex virus type 1 DNA polymerase by zinc ions. Virology. 1978;84(2):551–4. [DOI] [PubMed] [Google Scholar]
- 53. Gupta P, Rapp F. Effect of zinc ions on synthesis of herpes simplex virus type 2-induced polypeptides. Proc Soc Exp Biol Med. 1976;152(3):455–8. [DOI] [PubMed] [Google Scholar]
- 54. Arens M, Travis S. Zinc salts inactivate clinical isolates of herpes simplex virus in vitro. J Clin Microbiol. 2000;38(5):1758–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Bourne N, Stegall R, Montano R, Meador M, Stanberry LR, Milligan GN. Efficacy and toxicity of zinc salts as candidate topical microbicides against vaginal herpes simplex virus type 2 infection. Antimicrob Agents Chemother. 2005;49(3):1181–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Kenney J, Rodriguez A, Kizima L, Seidor S, Menon R, Jean-Pierre N, Pugach P, Levendosky K, Derby N, Gettie A et al.. A modified zinc acetate gel, a potential nonantiretroviral microbicide, is safe and effective against simian-human immunodeficiency virus and herpes simplex virus 2 infection in vivo. Antimicrob Agents Chemother. 2013;57(8):4001–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Godfrey HR, Godfrey NJ, Godfrey JC, Riley D. A randomized clinical trial on the treatment of oral herpes with topical zinc oxide/glycine. Altern Ther Health Med. 2001;7(3):49–56. [PubMed] [Google Scholar]
- 58. Mahajan BB, Dhawan M, Singh R. Herpes genitalis—topical zinc sulfate: an alternative therapeutic and modality. Indian J Sex Transm Dis AIDS. 2013;34(1):32–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Shishkov S, Varadinova T, Bontchev P, Nachev C, Michailova E. Complexes of zinc with picolinic and aspartic acids inactivate free varicella-zoster virions. Met Based Drugs. 1996;3(1):11–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. te Velthuis AJ, van den Worm SH, Sims AC, Baric RS, Snijder EJ, van Hemert MJ. Zn(2+) inhibits coronavirus and arterivirus RNA polymerase activity in vitro and zinc ionophores block the replication of these viruses in cell culture. PLoS Pathog. 2010;6(11):e1001176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Butterworth BE, Korant BD. Characterization of the large picornaviral polypeptides produced in the presence of zinc ion. J Virol. 1974;14(2):282–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Nakai K, Lucas-Lenard J. Processing of mengovirus precursor polypeptides in the presence of zinc ions and sulfhydryl compounds. J Virol. 1976;18(3):918–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Krenn BM, Gaudernak E, Holzer B, Lanke K, Van Kuppeveld FJM, Seipelt J. Antiviral activity of the zinc ionophores pyrithione and hinokitiol against picornavirus infections. J Virol. 2009;83(1):58–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Polatnick J, Bachrach HL. Effect of zinc and other chemical agents on foot-and-mouth-disease virus replication. Antimicrob Agents Chemother. 1978;13(5):731–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Firpo EJ, Palma EL. Inhibition of foot and mouth disease virus and procapsid synthesis by zinc ions. Brief report. Arch Virol. 1979;61(1–2):175–81. [DOI] [PubMed] [Google Scholar]
- 66. Ferrari E, Wright-Minogue J, Fang JW, Baroudy BM, Lau JY, Hong Z. Characterization of soluble hepatitis C virus RNA-dependent RNA polymerase expressed in Escherichia coli. J Virol. 1999;73(2):1649–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Yuasa K, Naganuma A, Sato K, Ikeda M, Kato N, Takagi H, Mori M. Zinc is a negative regulator of hepatitis C virus RNA replication. Liver Int. 2006;26(9):1111–8. [DOI] [PubMed] [Google Scholar]
- 68. Zhang ZY, Reardon IM, Hui JO, Oconnell KL, Poorman RA, Tomasselli AG, Heinrikson RL. Zinc inhibition of renin and the protease from human immunodeficiency virus type 1. Biochemistry (Mosc). 1991;30(36):8717–21. [DOI] [PubMed] [Google Scholar]
- 69. Haraguchi Y, Sakurai H, Hussain S, Anner BM, Hoshino H. Inhibition of HIV-1 infection by zinc group metal compounds. Antiviral Res. 1999;43(2):123–33. [DOI] [PubMed] [Google Scholar]
- 70. Fenstermacher KJ, DeStefano JJ. Mechanism of HIV reverse transcriptase inhibition by zinc formation of a highly stable enzyme-(primer-template) complex with profoundly diminished catalytic activity. J Biol Chem. 2011;286(47):40433–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Bae SN, Lee KH, Kim JH, Lee SJ, Park LO. Zinc induces apoptosis on cervical carcinoma cells by p53-dependent and -independent pathway. Biochem Biophys Res Commun. 2017;484(1):218–23. [DOI] [PubMed] [Google Scholar]
- 72. Suara RO, Crowe JE Jr. Effect of zinc salts on respiratory syncytial virus replication. Antimicrob Agents Chemother. 2004;48(3):783–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Korant BD, Kauer JC, Butterworth BE. Zinc ions inhibit replication of rhinoviruses. Nature. 1974;248(5449):588–90. [DOI] [PubMed] [Google Scholar]
- 74. Korant BD, Butterworth BE. Inhibition by zinc of rhinovirus protein cleavage: interaction of zinc with capsid polypeptides. J Virol. 1976;18(1):298–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Hung M, Gibbs CS, Tsiang M. Biochemical characterization of rhinovirus RNA-dependent RNA polymerase. Antiviral Res. 2002;56(2):99–114. [DOI] [PubMed] [Google Scholar]
- 76. Corver J, Bron R, Snippe H, Kraaijeveld C, Wilschut J. Membrane fusion activity of Semliki Forest virus in a liposomal model system: specific inhibition by Zn2+ ions. Virology. 1997;238(1):14–21. [DOI] [PubMed] [Google Scholar]
- 77. Liu CY, Kielian M. Identification of a specific region in the E1 fusion protein involved in zinc inhibition of Semliki Forest virus fusion. J Virol. 2012;86(7):3588–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Bracha M, Schlesinger MJ. Inhibition of Sindbis virus-replication by zinc ions. Virology. 1976;72(1):272–7. [DOI] [PubMed] [Google Scholar]
- 79. Wei ZY, Burwinkel M, Palissa C, Ephraim E, Schmidt MFG. Antiviral activity of zinc salts against transmissible gastroenteritis virus in vitro. Vet Microbiol. 2012;160(3–4):468–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Zaslavsky V. Inhibition of vaccinia virus growth by zinc ions—effect on early RNA and thymidine kinase synthesis. J Virol. 1979;29(1):405–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Katz E, Margalith E. Inhibition of vaccinia virus maturation by zinc-chloride. Antimicrob Agents Chemother. 1981;19(2):213–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Shuman S, Golder M, Moss B. Characterization of vaccinia virus-DNA topoisomerase-I expressed in Escherichia c oli. J Biol Chem. 1988;263(31):16401–7. [PubMed] [Google Scholar]
- 83. Iovino L, Mazziotta F, Carulli G, Guerrini F, Morganti R, Mazzotti V, Maggi F, Macera L, Orciuolo E, Buda G et al.. High-dose zinc oral supplementation after stem cell transplantation causes an increase of TRECs and CD4+ naïve lymphocytes and prevents TTV reactivation. Leuk Res. 2018;70:20–4. [DOI] [PubMed] [Google Scholar]
- 84. Iraji F, Faghihi G. A randomized double-blind placebo-controlled clinical trial of two strengths of topical zinc sulfate solution against recurrent herpes simplex. Arch Iranian Med. 2002;6(1):13–5. [Google Scholar]
- 85. Turner RB, Cetnarowski WE. Effect of treatment with zinc gluconate or zinc acetate on experimental and natural colds. Clin Infect Dis. 2000;31(5):1202–8. [DOI] [PubMed] [Google Scholar]
- 86. Eby GA, Davis DR, Halcomb WW. Reduction in duration of common colds by zinc gluconate lozenges in a double-blind study. Antimicrob Agents Chemother. 1984;25(1):20–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Godfrey JC, Sloane BC, Smith DS, Turco JH, Mercer N, Godfrey NJ. Zinc gluconate and the common cold—a controlled clinical-study. J Int Med Res. 1992;20(3):234–46. [DOI] [PubMed] [Google Scholar]
- 88. Mossad SB, Macknin ML, Medendorp SV, Mason P. Zinc gluconate lozenges for treating the common cold—a randomized, double-blind, placebo-controlled study. Ann Intern Med. 1996;125(2):81–8.. doi: 10.7326/0003-4819-125-2-199607150-00001. [DOI] [PubMed] [Google Scholar]
- 89. Petrus EJ, Lawson KA, Bucci LR, Blum K. Randomized, double-masked, placebo-controlled clinical study of the effectiveness of zinc acetate lozenges on common cold symptoms in allergy-tested subjects. Curr Ther Res. 1998;59(9):595–607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Prasad AS, Fitzgerald JT, Bao B, Beck FWJ, Chandrasekar PH. Duration of symptoms and plasma cytokine levels in patients with the common cold treated with zinc acetate—a randomized, double-blind, placebo-controlled trial. Ann Intern Med. 2000;133(4):245–52. [DOI] [PubMed] [Google Scholar]
- 91. Prasad AS, Beck FWJ, Bao B, Snell D, Fitzgerald JT. Duration and severity of symptoms and levels of plasma interleukin-1 receptor antagonist, soluble tumor necrosis factor receptor, and adhesion molecules in patients with common cold treated with zinc acetate. J Infect Dis. 2008;197(6):795–802. [DOI] [PubMed] [Google Scholar]
- 92. Al-Gurairi FT, Al-Waiz M, Sharquie KE. Oral zinc sulphate in the treatment of recalcitrant viral warts: randomized placebo-controlled clinical trial. Br J Dermatol. 2002;146(3):423–31. [DOI] [PubMed] [Google Scholar]
- 93. Sharquie KE, Khorsheed AA, Al-Nuaimy AA. Topical zinc sulphate solution for treatment of viral warts. Saudi Med J. 2007;28(9):1418–21. [PubMed] [Google Scholar]
- 94. Yagboobi R, Sadighha A, Baktash D. Evaluation of oral zinc sulfate effect on recalcitrant multiple viral warts: a randomized placebo-controlled clinical trial. J Am Acad Dermatol. 2009;60(4):706–8. [DOI] [PubMed] [Google Scholar]
- 95. Lopez-Garcia DR, Gomez-Flores M, Arce-Mendoza AY, de la Fuente-Garcia A, Ocampo-Candiani J. Oral zinc sulfate for unresponsive cutaneous viral warts: too good to be true? A double-blind, randomized, placebo-controlled trial. Clin Exp Dermatol. 2009;34(8):E984–E5. [DOI] [PubMed] [Google Scholar]
- 96. Mohamed EEM, Tawfik KM, Mahmoud AM. The clinical effectiveness of intralesional injection of 2% zinc sulfate solution in the treatment of common warts. Scientifica. 2016; ;2016:1082979 doi: 10.1155/2016/1082979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Al-Waiz MM, Al-Nuaimy AA, Aljobori HA, Abdulameer MJ. Laryngeal papillomatosis treated by oral zinc sulphate. Ann Saudi Med. 2006;26(5):411–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Mocchegiani E, Veccia S, Ancarani F, Scalise G, Fabris N. Benefit of oral zinc supplementation as an adjunct to zidovudine (Azt) therapy against opportunistic infections in AIDS. Int J Immunopharmacol. 1995;17(9):719–27. [DOI] [PubMed] [Google Scholar]
- 99. Zazzo JF, Rouveix B, Rajagopalon P, Levacher M, Girard PM. Effect of zinc on the immune status of zinc-depleted AIDS related complex patients. Clin Nutr. 1989;8(5):259–61. [DOI] [PubMed] [Google Scholar]
- 100. Bobat R, Coovadia H, Stephen C, Naidoo KL, McKerrow N, Black RE, Moss W. Safety and efficacy of zinc supplementation for children with HIV-1 infection in South Africa: a randomised double-blind placebo-controlled trial. Lancet. 2005;366(9500):1862–7. [DOI] [PubMed] [Google Scholar]
- 101. Villamor E, Aboud S, Koulinska IN, Kupka R, Urassa W, Chaplin B, Msamanga G, Fawzi WW. Zinc supplementation to HIV-1-infected pregnant women: effects on maternal anthropometry, viral load, and early mother-to-child transmission. Eur J Clin Nutr. 2006;60(7):862–9. [DOI] [PubMed] [Google Scholar]
- 102. Takagi H, Nagamine T, Abe T, Takayama H, Sato K, Otsuka T, Kakizaki S, Hashimoto Y, Matsumoto T, Kojima A et al.. Zinc supplementation enhances the response to interferon therapy in patients with chronic hepatitis C. J Viral Hepat. 2001;8(5):367–71. [DOI] [PubMed] [Google Scholar]
- 103. Ko WS, Guo CH, Hsu GS, Chiou YL, Yeh MS, Yaun SR. The effect of zinc supplementation on the treatment of chronic hepatitis C patients with interferon and ribavirin. Clin Biochem. 2005;38(7):614–20. [DOI] [PubMed] [Google Scholar]
- 104. Himoto T, Hosomi N, Nakai S, Deguchi A, Kinekawa F, Matsuki M, Yachida M, Masaki T, Kurokochi K, Watanabe S et al.. Efficacy of zinc administration in patients with hepatitis C virus-related chronic liver disease. Scand J Gastroenterol. 2007;42(9):1078–87. [DOI] [PubMed] [Google Scholar]
- 105. Matsumura H, Nirei K, Nakamura H, Arakawa Y, Higuchi T, Hayashi J, Yamagami H, Matsuoka S, Ogawa M, Nakajima N et al.. Zinc supplementation therapy improves the outcome of patients with chronic hepatitis C. J Clin Biochem Nutr. 2012;51(3):178–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Murakami Y, Koyabu T, Kawashima A, Kakibuchi N, Kawakami T, Takaguchi K, Kita K, Okita M. Zinc supplementation prevents the increase of transaminase in chronic hepatitis C patients during combination therapy with pegylated interferon alpha-2b and ribavirin. J Nutr Sci Vitaminol (Tokyo). 2007;53(3):213–8. [DOI] [PubMed] [Google Scholar]
- 107. Lanke K, Krenn BM, Melchers WJ, Seipelt J, van Kuppeveld FJ. PDTC inhibits picornavirus polyprotein processing and RNA replication by transporting zinc ions into cells. J Gen Virol. 2007;88(Pt 4):1206–17. [DOI] [PubMed] [Google Scholar]
- 108. Eby GA. Zinc lozenges as cure for the common cold—a review and hypothesis. Med Hypotheses. 2010;74(3):482–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Hemila H. Zinc lozenges may shorten the duration of colds: a systematic review. Open Respir Med J. 2011;5:51–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Uchide N, Ohyama K, Bessho T, Yuan B, Yamakawa T. Effect of antioxidants on apoptosis induced by influenza virus infection: inhibition of viral gene replication and transcription with pyrrolidine dithiocarbamate. Antiviral Res. 2002;56(3):207–17. [DOI] [PubMed] [Google Scholar]
- 111. Oxford JS, Perrin DD. Inhibition of the particle-associated RNA-dependent RNA polymerase activity of influenza viruses by chelating agents. J Gen Virol. 1974;23(1):59–71. [DOI] [PubMed] [Google Scholar]
- 112. Alter MJ. The epidemiology of acute and chronic hepatitis C. Clin Liver Dis. 1997;1(3):559–68., vi–vii. [DOI] [PubMed] [Google Scholar]
- 113. Nagamine T, Takagi H, Hashimoto Y, Takayama H, Shimoda R, Nomura N, Suzuki K, Mori M, Nakajima K. The possible role of zinc and metallothionein in the liver on the therapeutic effect of IFN-α to hepatitis C patients. Biol Trace Elem Res. 1997;58(1–2):65–76. [DOI] [PubMed] [Google Scholar]
- 114. Garoff H, Wilschut J, Liljestrom P, Wahlberg JM, Bron R, Suomalainen M, Smyth J, Salminen A, Barth BU, Zhao H et al.. Assembly and entry mechanisms of Semliki Forest virus. Arch Virol Suppl. 1994;9:329–38. [DOI] [PubMed] [Google Scholar]
- 115. Zaitseva E, Mittal A, Griffin DE, Chernomordik LV. Class II fusion protein of alphaviruses drives membrane fusion through the same pathway as class I proteins. J Cell Biol. 2005;169(1):167–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Wellenreuther G, Cianci M, Tucoulou R, Meyer-Klaucke W, Haase H. The ligand environment of zinc stored in vesicles. Biochem Biophys Res Commun. 2009;380(1):198–203. [DOI] [PubMed] [Google Scholar]
- 117. Klemm V, Mitchell J, Cortez-Jugo C, Cavalieri F, Symonds G, Caruso F, Kelleher AD, Ahlenstiel C. Achieving HIV-1 control through RNA-directed gene regulation. Genes-Basel. 2016;7(12). doi: ARTN 119 10.3390/genes7120119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Levinson W, Faras A, Woodson B, Jackson J, Bishop JM. Inhibition of RNA-dependent DNA polymerase of Rous sarcoma virus by thiosemicarbazones and several cations. Proc Natl Acad Sci U S A. 1973;70(1):164–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Palan PR, Eidinoff ML. Specific effect of zinc ions on DNA-polymerase activity of avian myeloblastosis virus. Mol Cell Biochem. 1978;21(2):67–9. [DOI] [PubMed] [Google Scholar]
- 120. York DM, Darden TA, Pedersen LG, Anderson MW. Molecular modeling studies suggest that zinc ions inhibit HIV-1 protease by binding at catalytic aspartates. Environ Health Perspect. 1993;101(3):246–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Xu YN, Zhu HY, Wilcox CK, van't Wout A, Andrus T, Llewellyn N, Stamatatos L, Mullins JI, Corey L, Zhu TF. Blood monocytes harbor HIV type 1 strains with diversified phenotypes including macrophage-specific CCR5 virus. J Infect Dis. 2008;197(2):309–18. [DOI] [PubMed] [Google Scholar]
- 122. Swingler S, Mann AM, Zhou J, Swingler C, Stevenson M. Apoptotic killing of HIV-1-infected macrophages is subverted by the viral envelope glycoprotein. PLoS Pathog. 2007;3(9):1281–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Poudel KC, Bertone-Johnson ER, Poudel-Tandukar K. Serum zinc concentration and C-reactive protein in individuals with human immunodeficiency virus infection: the POsitive Living with HIV (POLH) study. Biol Trace Elem Res. 2016;171(1):63–70. [DOI] [PubMed] [Google Scholar]
- 124. Baum MK, Lai SH, Sales S, Page JB, Campa A. Randomized, controlled clinical trial of zinc supplementation to prevent immunological failure in HIV-infected adults. Clin Infect Dis. 2010;50(12):1653–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Baum MK, Campa A, Lai SG, Lai H, Page JB. Zinc status in human immunodeficiency virus type 1 infection and illicit drug use. Clin Infect Dis. 2003;37:S117–S23. [DOI] [PubMed] [Google Scholar]
- 126. Visser ME, Durao S, Sinclair D, Irlam JH, Siegfried N. Micronutrient supplementation in adults with HIV infection. Cochrane Database Syst Rev. 2017;(5):CD003650 doi: ARTN CD003650 10.1002/14651858.CD003650.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Kenney J, Aravantinou M, Singer R, Hsu M, Rodriguez A, Kizima L, Abraham CJ, Menon R, Seidor S, Chudolij A et al.. An antiretroviral/zinc combination gel provides 24 hours of complete protection against vaginal SHIV infection in macaques. PLoS One. 2011;6(1):e15835 doi: ARTN e15835 10.1371/journal.pone.0015835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Mizenina O, Hsu M, Jean-Pierre N, Aravantinou M, Levendosky K, Paglini G, Zydowsky TM, Robbiani M, Fernandez-Romero JA. MIV-150 and zinc acetate combination provides potent and broad activity against HIV-1. Drug Deliv Transl Re. 2017;7(6):859–66. [DOI] [PubMed] [Google Scholar]
- 129. de Martel C, Plummer M, Vignat J, Franceschi S. Worldwide burden of cancer attributable to HPV by site, country and HPV type. Int J Cancer. 2017;141(4):664–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Hoppe-Seyler K, Bossler F, Braun JA, Herrmann AL, Hoppe-Seyler F. The HPV E6/E7 oncogenes: key factors for viral carcinogenesis and therapeutic targets. Trends Microbiol. 2018;26(2):158–68. [DOI] [PubMed] [Google Scholar]
- 131. Simonart T, de Maertelaer V. Systemic treatments for cutaneous warts: a systematic review. J Dermatol Treat. 2012;23(1):72–7. [DOI] [PubMed] [Google Scholar]
- 132. Raza N, Khan DA. Zinc deficiency in patients with persistent viral warts. J Coll Physicians Surg Pak. 2010;20(2):83–6. [PubMed] [Google Scholar]
- 133. Kim JH, Bae SN, Lee CW, Song MJ, Lee SJ, Yoon JH, Lee KH, Hur SY, Park TC, Park JS. A pilot study to investigate the treatment of cervical human papillomavirus infection with zinc-citrate compound (CIZAR®). Gynecol Oncol. 2011;122(2):303–6. [DOI] [PubMed] [Google Scholar]
- 134. Kizima L, Rodriguez A, Kenney J, Derby N, Mizenina O, Menon R, Seidor S, Zhang SM, Levendosky K, Jean-Pierre N et al.. A potent combination microbicide that targets SHIV-RT, HSV-2 and HPV. PLoS One. 2014;9(4):e94547 doi: ARTN e94547 10.1371/journal.pone.0094547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135. Maywald M, Wessels I, Rink L. Zinc signals and immunity. Int J Mol Sci. 2017;18(10). doi: ARTN 2222 10.3390/ijms18102222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Pandey S, Kawai T, Akira S. Microbial sensing by toll-like receptors and intracellular nucleic acid sensors. Cold Spring Harb Perspect Biol. 2015;7(1):a016246 doi: ARTN a016246 10.1101/cshperspect.a016246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137. Lazear HM, Nice TJ, Diamond MS. Interferon-λ: immune functions at barrier surfaces and beyond. Immunity. 2015;43(1):15–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. Brieger A, Rink L, Haase H. Differential regulation of TLR-dependent MyD88 and TRIF signaling pathways by free zinc ions. J Immunol. 2013;191(4):1808–17. [DOI] [PubMed] [Google Scholar]
- 139. Liu MJ, Bao SY, Galvez-Peralta M, Pyle CJ, Rudawsky AC, Pavlovicz RE, Killilea DW, Li CL, Nebert DW, Wewers MD et al.. ZIP8 regulates host defense through zinc-mediated inhibition of NF-κB. Cell Rep. 2013;3(2):386–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. Hoshino K, Sugiyama T, Matsumoto M, Tanaka T, Saito M, Hemmi H, Ohara O, Akira S, Kaisho T. IκB kinase-α is critical for interferon-α production induced by toll-like receptors 7 and 9. Nature. 2006;440(7086):949–53. [DOI] [PubMed] [Google Scholar]
- 141. Han KJ, Su XQ, Xu LG, Bin LH, Zhang J, Shu HB. Mechanisms of the TRIF-induced interferon-stimulated response element and NF-κB activation and apoptosis pathways. J Biol Chem. 2004;279(15):15652–61. [DOI] [PubMed] [Google Scholar]
- 142. Fitzgerald KA, McWhirter SM, Faia KL, Rowe DC, Latz E, Golenbock DT, Coyle AJ, Liao SM, Maniatis T. IKKε and TBK1 are essential components of the IRF3 signaling pathway. Nat Immunol. 2003;4(5):491–6. [DOI] [PubMed] [Google Scholar]
- 143. Shembade N, Ma A, Harhaj EW. Inhibition of NF-κB signaling by A20 through disruption of ubiquitin enzyme complexes. Science. 2010;327(5969):1135–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144. Wang YY, Li LY, Han KJ, Zhai ZH, Shu HB. A20 is a potent inhibitor of TLR3-and Sendai virus-induced activation of NF-κB and ISRE and IFN-β promoter. FEBS Lett. 2004;576(1–2):86–90. [DOI] [PubMed] [Google Scholar]
- 145. Lin RT, Yang L, Nakhaei P, Sun Q, Sharif-Askari E, Julkunen I, Hiscott J. Negative regulation of the retinoic acid-inducible gene I-induced antiviral state by the ubiquitin-editing protein A20. J Biol Chem. 2006;281(4):2095–103. [DOI] [PubMed] [Google Scholar]
- 146. Maelfait J, Roose K, Bogaert P, Sze M, Saelens X, Pasparakis M, Carpentier I, van Loo G, Beyaert R. A20 (Tnfaip3) deficiency in myeloid cells protects against influenza A virus infection. PLoS Pathog. 2012;8(3):e1002570 doi: ARTN e1002570 10.1371/journal.ppat.1002570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. Yabe-Wada T, Matsuba S, Takeda K, Sato T, Suyama M, Ohkawa Y, Takai T, Shi HF, Philpott CC, Nakamura A. TLR signals posttranscriptionally regulate the cytokine trafficking mediator sortilin. Sci Rep. 2016;6::26566 doi: ARTN 26566 10.1038/srep26566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Mortensen MB, Kjolby M, Gunnersen S, Larsen JV, Palmfeldt J, Falk E, Nykjaer A, Bentzon JF. Targeting sortilin in immune cells reduces proinflammatory cytokines and atherosclerosis. J Clin Invest. 2014;124(12):5317–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149. Radhakrishnan R, Walter LJ, Hruza A, Reichert P, Trotta PP, Nagabhushan TL, Walter MR. Zinc mediated dimer of human interferon-α 2b revealed by X-ray crystallography. Structure. 1996;4(12):1453–63. [DOI] [PubMed] [Google Scholar]
- 150. Berg K, Bolt G, Andersen H, Owen TC. Zinc potentiates the antiviral action of human IFN-α tenfold. J Interferon Cytokine Res. 2001;21(7):471–4. [DOI] [PubMed] [Google Scholar]
- 151. O'Connor KS, Parnell G, Patrick E, Ahlenstiel G, Suppiah V, van der Poorten D, Read SA, Leung R, Douglas MW, Yang JY et al.. Hepatic metallothionein expression in chronic hepatitis C virus infection is IFNL3 genotype-dependent. Genes Immun. 2014;15(2):88–94. [DOI] [PubMed] [Google Scholar]
- 152. Brautigan DL, Bornstein P, Gallis B. Phosphotyrosyl-protein phosphatase—specific inhibition by Zn-2+. J Biol Chem. 1981;256(13):6519–22. [PubMed] [Google Scholar]
- 153. Shanker V, Trincucci G, Heim HM, Duong HT. Protein phosphatase 2A impairs IFNα-induced antiviral activity against the hepatitis C virus through the inhibition of STAT1 tyrosine phosphorylation. J Viral Hepat. 2013;20(9):612–21. [DOI] [PubMed] [Google Scholar]
- 154. You M, Yu DH, Feng GS. Shp-2 tyrosine phosphatase functions as a negative regulator of the interferon-stimulated Jak/STAT pathway. Mol Cell Biol. 1999;19(3):2416–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155. David M, Chen HYE, Goelz S, Larner AC, Neel BG. Differential regulation of the α/β interferon-stimulated Jak/STAT pathway by the SH2 domain-containing tyrosine phosphatase SHPTP1. Mol Cell Biol. 1995;15(12):7050–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156. Xiong Y, Luo DJ, Wang XL, Qiu M, Yang Y, Yan X, Wang JZ, Ye QF, Liu R. Zinc binds to and directly inhibits protein phosphatase 2A in vitro. Neurosci Bull. 2015;31(3):331–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157. Haase H, Maret W. Intracellular zinc fluctuations modulate protein tyrosine phosphatase activity in insulin/insulin-like growth factor-1 signaling. Exp Cell Res. 2003;291(2):289–98. [DOI] [PubMed] [Google Scholar]
- 158. Haase H, Maret W. Fluctuations of cellular, available zinc modulate insulin signaling via inhibition of protein tyrosine phosphatases. J Trace Elem Med Biol. 2005;19(1):37–42. [DOI] [PubMed] [Google Scholar]
- 159. Long LY, Deng YZ, Yao F, Guan DX, Feng YY, Jiang H, Li XB, Hu PT, Lu XC, Wang H et al.. Recruitment of phosphatase PP2A by RACK1 adaptor protein deactivates transcription factor IRF3 and limits type I interferon signaling. Immunity. 2014;40(4):515–29. [DOI] [PubMed] [Google Scholar]
- 160. Li S, Zhu MZ, Pan RG, Fang T, Cao YY, Chen SL, Zhao XL, Lei CQ, Guo L, Chen Y et al.. The tumor suppressor PTEN has a critical role in antiviral innate immunity. Nat Immunol. 2016;17(3):241–9. [DOI] [PubMed] [Google Scholar]
- 161. Plum LM, Brieger A, Engelhardt G, Hebel S, Nessel A, Arlt M, Kaltenberg J, Schwaneberg U, Huber M, Rink L et al.. PTEN-inhibition by zinc ions augments interleukin-2-mediated Akt phosphorylation. Metallomics. 2014;6(7):1277–87. [DOI] [PubMed] [Google Scholar]
- 162. Yoshimura A, Naka T, Kubo M. SOCS proteins, cytokine signalling and immune regulation. Nat Rev Immunol. 2007;7(6):454–65. [DOI] [PubMed] [Google Scholar]
- 163. Liuzzi JP, Wong CP, Ho E, Tracey A. Regulation of hepatic suppressor of cytokine signaling 3 by zinc. J Nutr Biochem. 2013;24(6):1028–33. [DOI] [PubMed] [Google Scholar]
- 164. Lonnerdal B. Dietary factors influencing zinc absorption. J Nutr. 2000;130(5):1378s–83s. [DOI] [PubMed] [Google Scholar]
- 165. Hunt JR, Beiseigel JM, Johnson LK. Adaptation in human zinc absorption as influenced by dietary zinc and bioavailability. Am J Clin Nutr. 2008;87(5):1336–45. [DOI] [PubMed] [Google Scholar]
- 166. Yasuda H, Tsutsui T. Infants and elderlies are susceptible to zinc deficiency. Sci Rep. 2016;6:21850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167. Cakman I, Kirchner H, Rink L. Zinc supplementation reconstitutes the production of interferon-α by leukocytes from elderly persons. J Interferon Cytokine Res. 1997;17(8):469–72. [DOI] [PubMed] [Google Scholar]
- 168. Prasad AS, Beck FW, Bao B, Fitzgerald JT, Snell DC, Steinberg JD, Cardozo LJ. Zinc supplementation decreases incidence of infections in the elderly: effect of zinc on generation of cytokines and oxidative stress. Am J Clin Nutr. 2007;85(3):837–44. [DOI] [PubMed] [Google Scholar]
- 169. Mills PR, Fell GS, Bessent RG, Nelson LM, Russell RI. A study of zinc metabolism in alcoholic cirrhosis. Clin Sci. 1983;64(5):527–35. [DOI] [PubMed] [Google Scholar]
- 170. Manari AP, Preedy VR, Peters TJ. Nutritional intake of hazardous drinkers and dependent alcoholics in the UK. Addict Biol. 2003;8(2):201–10. [DOI] [PubMed] [Google Scholar]
- 171. Dinsmore W, Callender ME, McMaster D, Todd SJ, Love AHG. Zinc absorption in alcoholics using Zn-65. Digestion. 1985;32(4):238–42. [DOI] [PubMed] [Google Scholar]
- 172. Sun Q, Li Q, Zhong W, Zhang JY, Sun XH, Tan XB, Yin XM, Sun XG, Zhang X, Zhou ZX. Dysregulation of hepatic zinc transporters in a mouse model of alcoholic liver disease. Am J Physiol Gastrointest Liver Physiol. 2014;307(3):G313–G22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173. Zhong W, McClain CJ, Cave M, Kang YJ, Zhou ZX. The role of zinc deficiency in alcohol-induced intestinal barrier dysfunction. Am J Physiol Gastrointest Liver Physiol. 2010;298(5):G625–G33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174. Konig J, Wells J, Cani PD, Garcia-Rodenas CL, MacDonald T, Mercenier A, Whyte J, Troost F, Brummer RJ. Human intestinal barrier function in health and disease. Clin Transl Gastroenterol. 2016;7(10):e196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175. Lambert JC, Zhou ZX, Wang LP, Song ZY, McClain CJ, Kang YJ. Prevention of alterations in intestinal permeability is involved in zinc inhibition of acute ethanol-induced liver damage in mice. J Pharmacol Exp Ther. 2003;305(3):880–6. [DOI] [PubMed] [Google Scholar]
- 176. Alam AN, Sarker SA, Wahed MA, Khatun M, Rahaman MM. Enteric protein loss and intestinal permeability changes in children during acute shigellosis and after recovery—effect of zinc supplementation. Gut. 1994;35(12):1707–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177. Asdamongkol N, Phanachet P, Sungkanuparph S. Low plasma zinc levels and immunological responses to zinc supplementation in HIV-infected patients with immunological discordance after antiretroviral therapy. Jpn J Infect Dis. 2013;66(6):469–74. [DOI] [PubMed] [Google Scholar]
- 178. Colgate ER, Haque R, Dickson DM, Carmolli MP, Mychaleckyj JC, Nayak U, Qadri F, Alam M, Walsh MC, Diehl SA et al.. Delayed dosing of oral rotavirus vaccine demonstrates decreased risk of rotavirus gastroenteritis associated with serum zinc: a randomized controlled trial. Clin Infect Dis. 2016;63(5):634–41. [DOI] [PubMed] [Google Scholar]
- 179. Lazarus RP, John J, Shanmugasundaram E, Rajan AK, Thiagarajan S, Giri S, Babji S, Sarkar R, Kaliappan PS, Venugopal S et al.. The effect of probiotics and zinc supplementation on the immune response to oral rotavirus vaccine: a randomized, factorial design, placebo-controlled study among Indian infants. Vaccine. 2018;36(2):273–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180. Bhutta ZA, Bird SM, Black RE, Brown KH, Gardner JM, Hidayat A, Khatun F, Martorell R, Ninh NX, Penny ME et al.. Therapeutic effects of oral zinc in acute and persistent diarrhea in children in developing countries: pooled analysis of randomized controlled trials. Am J Clin Nutr. 2000;72(6):1516–22. [DOI] [PubMed] [Google Scholar]
- 181. Habib MA, Soofi S, Sheraz A, Bhatti ZS, Okayasu H, Zaidi SZ, Molodecky NA, Pallansch MA, Sutter RW, Bhutta ZA. Zinc supplementation fails to increase the immunogenicity of oral poliovirus vaccine: a randomized controlled trial. Vaccine. 2015;33(6):819–25. [DOI] [PubMed] [Google Scholar]
- 182. Afsharian M, Vaziri S, Janbakhsh AR, Sayad B, Mansouri F, Nourbakhsh J, Qadiri K, Najafi F, Shirvanii M. The effect of zinc sulfate on immunologic response to recombinant hepatitis B vaccine in elderly. Hepat Mon. 2011;11(1):33–6. [PMC free article] [PubMed] [Google Scholar]
- 183. Provinciali M, Montenovo A, Di Stefano G, Colombo M, Daghetta L, Cairati M, Veroni C, Cassino R, Della Torre F, Fabris N. Effect of zinc or zinc plus arginine supplementation on antibody titre and lymphocyte subsets after influenza vaccination in elderly subjects: a randomized controlled trial. Age Ageing. 1998;27(6):715–22. [DOI] [PubMed] [Google Scholar]
- 184. Osendarp SJM, Prabhakar H, Fuchs GJ, van Raaij JMA, Mahmud H, Tofail F, Santosham M, Black RE. Immunization with the heptavalent pneumococcal conjugate vaccine in Bangladeshi infants and effects of zinc supplementation. Vaccine. 2007;25(17):3347–54. [DOI] [PubMed] [Google Scholar]
- 185. Albert MJ, Qadri F, Wahed MA, Ahmed T, Rahman ASMH, Ahmed F, Bhuiyan NA, Zaman K, Baqui AH, Clemens JD et al.. Supplementation with zinc, but not vitamin A, improves seroconversion to vibriocidal antibody in children given an oral cholera vaccine. J Infect Dis. 2003;187(6):909–13. [DOI] [PubMed] [Google Scholar]