Abstract
Purpose
Medication adherence (MA) is a key factor for hypertensive patients’ blood pressure control and forgetfulness is one of the main reasons that cause medication non-adherence. If effective, low-cost reminder package (LCRP) has great potentials for large-scale promotion. Therefore, this study aims to evaluate the effectiveness of combining LCRP and health education to improve MA among hypertensive patients.
Patients and methods
A clustered randomized controlled trial was performed in Beijing. A total of 518 hypertensive patients recruited from 8 community health care centers were randomized to receive LCRP combined with case-based health education or usual care. Randomization was performed at community level. Multilevel modeling was used to evaluate the study effect.
Results
MA scores did not differ significantly at baseline between the intervention group and the control group. The results of multilevel modeling indicated that MA scores increased more in the intervention group, and the intervention effect on MA was 0.287 (95% CI: [0.103, 0.471], P=0.002). Patients’ systolic blood pressure (SBP) and diastolic blood pressure (DBP) were not improved (SBP: difference=0.536, 95% CI [−3.207, 4.278]; DBP: difference=−0.927, 95% CI [−3.283, 1.428]).
Conclusion
LCRP combined with case-based health education could significantly improve hypertensive patients’ MA.
Keywords: low-cost reminder package, medication adherence, multilevel modeling, case-based health education
Introduction
Globally, hypertension has become a major public health threat, consuming a large percentage of health expenditures.1 The estimated prevalence of hypertension in 2000 was 26.4% (972 million), and the number continues to rise.2 In 2015, there were 1.13 billion hypertensive patients and the age-standardized prevalence in adults aged 18 and over was around 22%.3 Meanwhile, the disease burden brought by hypertension also continues to deteriorate. In 2000, hypertension claimed 7.6 million deaths and 6% of the disease burden (calculated by disability-adjusted life year) while the number climbed to 9.4 million and 7% in 2010.4,5 However, although the prevalence and burden of hypertension continue to rise, its treatment and control rate remains at a poor level. It was estimated that in 2010, among 31.1% adults with hypertension globally, only 36.9% were treated with antihypertensive medication and only 13.8% had their blood pressure under control.6 Elevated blood pressure greatly contributes to increased risks of cardiovascular-related deaths, and Global Burden of Disease Study revealed that hypertension was the main risk factor for disability-adjusted life year.5 Therefore, helping hypertensive patients to improve blood pressure control is of critical importance both for patients themselves and society as a whole.
Some studies have shown that medication adherence (MA) was a key factor for hypertensive patients’ blood pressure control and clinical outcomes, such as risks for coronary heart disease, stroke, and heart failure.7–9 A research by Baily et al found that if patients with poor adherence increased one pill per week for a once-a-day medication, the risk for stroke would decrease by 8–9% and death by 7%.10 Several large cohort studies have shown that hypertensive patients with good MA had significantly lower risks of cardiovascular events (up to 38%), compared with those having poor adherence.11–13 Reducing the risks of hypertensive complications such as coronary heart disease and stroke could reduce the rate of outpatient visits, emergency visits, and hospitalizations, and thus further alleviate patients’ economic burden and the tension of limited health resources.14–16 However, although MA has a significant influence on patients’ blood pressure, the rate of high MA varies across region to region. A meta-analysis including 25 studies from 15 countries reported that 45.2% (95% CI: [34.4, 56.1]) of hypertensive patients had poor MA, and another meta-analysis examining studies from low and middle-income countries revealed that 63.35% (95% CI: [38.8, 87.9]) of hypertensive patients was non-compliant.17,18 The situation in China was even more severe. A cross-sectional study conducted in mainland China found that among elderly hypertensive patients, only 34.2% had good MA19 As a result, exploring the way of improving MA has both clinical and practical implications.
Studies have shown that forgetfulness was one of the main reasons that caused medication non-adherence.20,21 Among various interventions addressing MA in patients with chronic diseases, some researchers suggested that reminder package was more effective than other forms such as medication counseling and social support, and others also proposed that a combination of education and reminder strategies might better improve MA.22,23 However, the number of research examining the efficacy of package intervention in hypertensive patients was limited and a consistent conclusion was not reached.20,24 Furthermore, most of the reminder packages used in these interventions were directed at non-Chinese populations and somewhat expensive as they could not only record the exact time of bottle opening but also provide adherence feedback to patients.25,26 Therefore, considering the large population basis in China, exploring an effective and low-cost intervention that could be promoted on a large scale has significant implications.
As a result, this study aims to examine the effectiveness of a low-cost reminder package (LCRP) combined with case-based health education in improving MA among Chinese hypertensive patients. Case-based education normally refers to education that “prepares students for clinical practice through the use of authentic clinical cases”.27 This study borrowed this term and hoped to test the effectiveness of combining reminder package and authentic cases in improving hypertensive patients’ MA.
To our knowledge, this study was one of the few that examined the effectiveness of low-cost reminder devices combined with case-based health education in patients with chronic diseases, especially in a Chinese hypertensive population.
Materials and methods
Ethics statement
This study was approved by the Institutional Review Board of Peking University Health Science Center. All participants provided written informed consent, and this study was conducted in accordance with the Declaration of Helsinki.
Study design
A clustered-randomized controlled trial was conducted to examine the effectiveness of an LCRP intervention combined with case-based health education in improving hypertensive patients’ MA. The patients in the intervention group received a pill box and two classes of health education delivered by health care professionals. Patients in the control group received usual care. Data were collected at baseline and at six months follow-up.
Participants and study settings
A clustered randomized controlled trial was performed in Shunyi District, Beijing, between May and December 2016. Shunyi District covers 1021 square kilometers and has a population of 983,000. With a rapid economic growth due to the construction of Beijing Capital International Airport, the local residents experienced a substantial improvement in living conditions and also an ensuing high prevalence of chronic diseases such as hypertension.28 Therefore, in this study, in order to explore an effective method to help manage patients’ blood pressure, a clustered randomized controlled trial was conducted in eight community health care centers in Shunyi District.
Essential hypertensive patients who volunteered to participate, aged above 18, diagnosed according to ICD-9 codes 401–401.9, and currently taking at least one kind of antihypertensive medications were included. Those who failed or were unable to sign informed consent, had mental disorders, had a life expectancy less than 6 months, or had the intention of moving out of the region within half a year were excluded.
Interventions
Patients in the intervention group received a commercially available low-cost pillbox at the start of the intervention. The pillbox had 28 detachable compartments (4 for each day) and 1 alarm that could produce audible beeps. Patients could put a week’s medication into the pillbox and set at most four alarms at different times of the day. Each time the patient needed to take medication, the pillbox would produce large beeps to remind them. If the alarm was missed, it would beep every 2 mins for half an hour until it was turned off. Detailed instructions on its use were provided by medical personnel.
Apart from the reminder package, patients in the intervention group also received two health education classes. Patients were called before each health education, and they could come at their wish. As hypertensive patients tended to be elderly and less-educated, health education in this study was based on vivid cases, with the aim to maximize patients’ understanding and internalization. The first health education was delivered after completion of baseline questionnaire at the start of intervention. The content of health education was structured around how to measure blood pressure correctly and the basic knowledge about hypertension, such as related complications, treatments, hypertension grade, and corresponding severity. The first education was delivered by health care providers for 20–30 mins at the community health care center, with the aim to help patients recognize the importance of MA and blood pressure control. Three months after baseline, patients in the intervention group received their second health education. Vivid examples of other hypertensive patients were presented here to give participants a concrete impression of the benefits of MA and the possible consequences of non-adherence, such as medication discontinuance after blood pressure was controlled. Fear for side effects was especially addressed. Furthermore, patients’ possible somatic and emotional issues were also addressed here. This class presented patients with several vivid cases which contained the psychological issues that might occur in the course of medication taking and informed them how to seek help or deal with them. This session was delivered by health care providers at the center for 20–30 mins. Three months after the second health education, the six-month follow-up questionnaire survey was conducted.
Patients in the control group received usual care.
Outcomes and measurements
Patients in both groups completed two questionnaires on baseline and six-month follow-up, respectively. Information on sociodemographic characteristics (eg, age, gender, the degree of education, and income), disease history, medication history, and hypertension-related knowledge were collected. MA was measured both at baseline and follow-up by self-designed MA scale. The self-designed MA scale included five items to measure patients’ MA and the total score was 5. The first two items were dichotomous and coded as 0 and 1. The rest three items used Likert 5-point scale and coded as 0, 0.25, 0.50, 0.75, and 1, respectively. Higher scores represented higher MA. This scale had a Cronbach’s α of 0.726.
Physical examinations including height, weight, waistline, and blood pressure measurements were also performed at baseline and 3-month follow-up. Patients’ blood pressure was measured three times in each time point, and the average value was used in data analysis. Both questionnaire survey and physical examination were conducted by well-trained community health workers and research staff.
Sample size and randomization
The sample size was determined with PASS 11. The Module of "Test for Two Means (Two Sample Student's t-Test )" was used, with an α of 0.05 and β of 0.1. We expected to observe a difference of 5 mmHg of SBP between 2 groups after intervention and literature showed that the standard deviation of SBP among Chinese population was 15.4.29 Therefore, based on the earlier information, a sample of 200 participants in the control group and intervention group each was calculated. Considering the possibility of loss to follow-up, the final sample was expanded to 600. Eight community health care centers were sampled from a total of 26 centers in Shunyi District and were randomly assigned to the control group or intervention group in a 1:1 ratio using concealed random allocation. Randomization was achieved with random numbers. Each community health care center was expected to recruit 75 hypertensive patients, and a total of 596 patients were finally included in this study. Due to the nature of intervention, both patients and health care providers were aware of their treatment allocation.
Statistical analysis
Data were entered with Epidata 3.1. Normality test was performed on continuous data. Those that followed the normal distribution was reported as mean±SD and others were described by median and interquartile range. Categorical data were reported in frequency and proportion. Two sample t-test and paired samples t-test were performed to compare MA score. Chi-square test was used to determine whether characteristics differed significantly between the control group and the intervention group. Furthermore, multilevel modeling with an interaction term was applied to account for clustering and to assess the treatment effects. A time dummy was created to indicate the time trend in treatment and control group, and an interaction term between the intervention and time dummy was generated to represent the net effect of intervention impact on patient outcomes. The analysis was adjusted for gender, age, education, ethnicity, marital status, antihypertensive medication history, and other chronic medication-taking history. Intention-to-treat analysis was also used to examine the intervention effect. P<0.05 was considered statistically significant. Statistical analysis was performed in Stata SE 14.1.
Results
Demographic characteristics
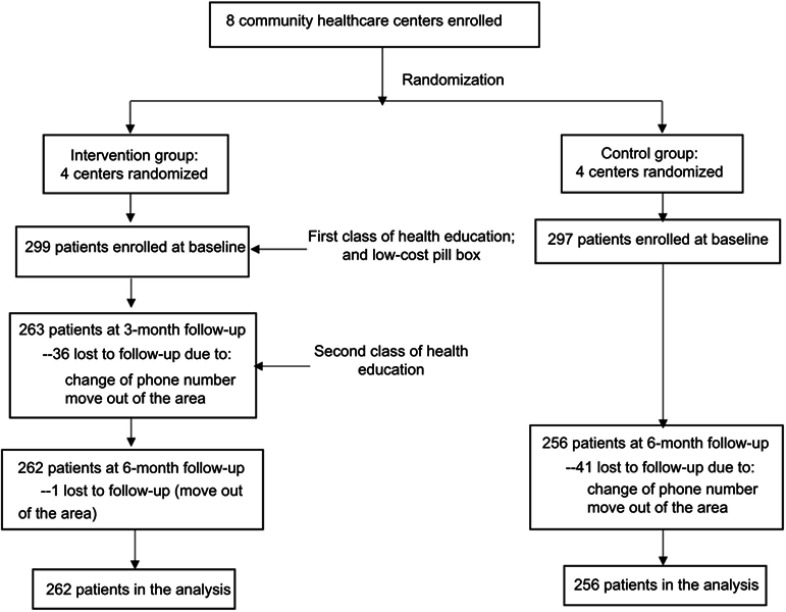
A total of 596 hypertensive patients were recruited at baseline, with a mean age of 56±6.7, 299 in the intervention group and 297 in the control group. A significant difference was observed in gender, age, and education between intervention and control group (P<0.05). More patients in the control group were male, young, and well-educated. Other characteristics at baseline were balanced between the two groups. A total of 194 (64.9%) patients in the intervention group and 182 (61.3%) in the control group had their blood pressure under control (SBP<140 mmHg and DBP <90 mmHg). At follow-up, a total of 518 patients completed the trial, with 262 in the intervention group and 256 in the control group (Figure 1). As high as 13.1% of the patients were lost to follow-up (12.4% for the intervention group and 13.8% for the control group). Similar to the baseline, there was also a significant difference between intervention and control group in terms of gender, age, and education. Comparison of patients’ characteristics between baseline and six-month follow-up in two groups revealed no significant difference. Detailed information are presented in Table 1.
Figure 1.
Flowchart
Table 1.
Sociodemographic characteristics of participants before and after intervention
| Sociodemographic characteristics | Baseline (%) | Endpoint (%) | Comparison between baseline and endpoint: χ2 | |||||
|---|---|---|---|---|---|---|---|---|
| Control | Intervention | χ2 | Control | Intervention | χ2 | Control | Intervention | |
| Number (%) | 297(49.8) | 299(50.2) | 256(49.4) | 262(50.6) | ||||
| Gender | 7.675* | 8.061* | 0.058 | 0.261 | ||||
| Male | 112(37.7) | 81(27.1) | 94(36.7) | 66(25.2) | ||||
| Female | 185(62.3) | 218(72.9) | 162(63.3) | 196(74.8) | ||||
| Age (years) | 10.619* | 11.947* | 0.053 | 0.059 | ||||
| ≤49 | 64(21.5) | 35(11.7) | 57(22.3) | 29(11.1) | ||||
| 50-59 | 144(48.5) | 158(52.8) | 124(48.4) | 140(53.4) | ||||
| 60+ | 89(30.0) | 106(35.5) | 75(29.3) | 93(35.5) | ||||
| Education | 17.042* | 14.791* | 0.466 | 0.114 | ||||
| Primary school and below | 33(11.1) | 52(17.4) | 31(12.1) | 44(16.8) | ||||
| Middle school | 157(52.9) | 183(61.2) | 128(50.0) | 159(60.7) | ||||
| High school and above | 107(36.0) | 64(21.4) | 97(37.9) | 59(22.5) | ||||
| Marital status | 0.198 | 0.497 | 0.167 | 0.012 | ||||
| Married | 280(94.2) | 285(96.0) | 239(93.4) | 251(95.8) | ||||
| Unmarried | 14(4.8) | 12(4.0) | 14(5.4) | 11(4.2) | ||||
| Missing | 3(1.0) | 3(1.2) | ||||||
| Family income | 6.963 | 4.514 | 0.359 | 0.227 | ||||
| <900 | 90(30.3) | 87(29.1) | 72(28.1) | 79(30.2) | ||||
| 900-1409 | 50(16.8) | 61(20.4) | 46(18.0) | 54(20.6) | ||||
| 1410-2499 | 72(24.2) | 79(26.4) | 63(24.6) | 65(24.8) | ||||
| 2500-3499 | 30(10.1) | 46(15.4) | 27(10.6) | 40(15.3) | ||||
| 3500+ | 38(12.8) | 25(8.4) | 33(12.9) | 23(8.8) | ||||
| Missing | 17(5.7) | 1(0.3) | 15(5.9) | 1(0.4) | ||||
| Ethnicity | 0.175 | 0.033 | 0.009 | 0.014 | ||||
| Han | 287(96.6) | 287(96.0) | 247(96.5) | 252(96.2) | ||||
| Other | 10(3.4) | 12(4.0) | 9(3.5) | 10(3.8) | ||||
| Antihypertensive medication history | 2.467 | 1.887 | 0.030 | 0.065 | ||||
| <5 | 110(37.0) | 95(31.8) | 96(37.5) | 85(32.5) | ||||
| 5-9 | 77(25.9) | 77(25.8) | 68(26.6) | 69(26.3) | ||||
| 10+ | 108(36.4) | 126(42.1) | 92(35.9) | 108(41.2) | ||||
| missing | 2(0.7) | 1(0.3) | 0 | 0 | ||||
| Other chronic medication-taking history | 1.414 | 1.252 | 0.052 | 0.057 | ||||
| No | 143(48.1) | 130(43.5) | 121(47.3) | 112(42.8) | ||||
| Yes | 150(50.5) | 166(55.5) | 132(51.5) | 149(56.9) | ||||
| Missing | 4(1.4) | 3(1.0) | 3(1.2) | 1(0.3) | ||||
Note: *P<0.05.
Patients’ usage of reminder package
A total of 106 (40.5%) patients in the intervention group used the reminder package. Among them, 67.9% were frequent users and 32.1% were intermittent users. As high as 54.3% of the patients reported that the reminder package was simple to use and 50.9% reported it as a very helpful tool. The survey conducted among the nonusers revealed that the primary reason (57.6%) that they did not use the device was they could remember taking medicine on their own without the help of a reminder. Other reasons included the device was a little complex to use (15.2%), they only took a few kinds of medication (11.9%), and they did not know how to use the device (9.3%). Furthermore, a total of 299 patients participated the first health education class and 263 patients participated the second.
Overall intervention impact on MA
The MA score for the control group and the intervention group did not differ significantly at baseline, with 4.36±1.02 for the control group and 4.39±1.02 for the intervention group (P=0.713). However, at six-month follow-up, patients in the intervention group had a significantly higher MA score than those in the control group (control group: 4.39±1.02; intervention group: 4.62±0.78; difference=0.226, P=0.005). After adjusting for pre-defined covariates, the multilevel modeling result indicated that the intervention effect on MA was 0.287 (95% CI: [0.103, 0.471], P=0.002). The intracluster correlation coefficient of MA for hypertensive patients in Shunyi District was 0.006 (Table 2). Furthermore, an intention-to-treat analysis was also conducted, and the result indicated that the intervention effect on MA was 0.287 (95% CI: [0.102, 0.473], P=0.002).
Table 2.
Results of multi-level modeling on intervention effectiveness in patients’ medication adherence, SBP and DBP
| Variable | Baseline (SD) | 6-month follow-up(SD) | Difference in change between groups (95% CI)a | ICC |
|---|---|---|---|---|
| MAb | ||||
| Control | 4.36 (1.02) | 4.39 (1.02) | 0.287 (0.103,0.471)* | 0.006 |
| Intervention | 4.33 (1.02) | 4.62 (0.78) | ||
| MA (ITTc) | ||||
| Control | 4.30 (1.09) | 4.39 (1.02) | 0.287 (0.102, 0.473)* | 0.002 |
| Intervention | 4.28 (1.08) | 4.62 (0.78) | ||
| SBP | ||||
| Control | 135.3 (16.9) | 136.6 (14.8) | 0.536 (−3.207, 4.278) | 0.020 |
| Intervention | 134.1 (16.6) | 136.1 (14.9) | ||
| DBP | ||||
| Control | 81.6 (10.5) | 83.9 (9.9) | −0.927 (−3.283, 1.428) | 0.022 |
| Intervention | 77.0 (10.2) | 78.6 (9.6) |
Notes: aDifference in change between groups was calculated with multilevel modeling, adjusting for clustering level, gender, age, education, ethnicity, marital status, antihypertensive medication history, self-efficacy, and other chronic medication-taking history. bN=518 (those who completed the intervention). cN=596, Intention-to-treat analysis. *P<0.05.
Abbreviations: MA, medication adherence; ICC, intracluster correlation coefficient; SBP, systolic blood pressure; DBP, diastolic blood pressure.
Further analysis was performed on individual items of MA scale to examine which items of the scale were actually improved. Multilevel modeling results on individual items indicated that the intervention had significantly improved item 1 [Stopped taking medication without telling doctors when disease status deteriorated] and item 5 [Taking medications even if BP was normal for a consecutive period of time]. Detailed information are presented in Table 3.
Table 3.
Comparison of participants’ performance on individual items of medication adherence scale before and after intervention
| Items | Control group (N=256) | Intervention group (N=262) | Diffa | ||||
|---|---|---|---|---|---|---|---|
| Improve | Maintain | Deteriorate | Improve | Maintain | Deteriorate | ||
| 1. Stopped taking medication without telling doctors when disease status deteriorated | 11.3% | 75.0% | 13.7% | 17.6% | 76.3% | 6.1% | 0.134* |
| 2. Stopped taking medication once BP was under control | 11.7% | 82.8% | 5.5% | 15.3% | 81.3% | 3.4% | 0.064 |
| 3. Taking medication regularly and on time according to doctors’ recommendations | 9.8% | 77.7% | 12.5% | 11.1% | 79.4% | 9.5% | 0.024 |
| 4. Never forget taking medications | 20.3% | 59.4% | 20.3% | 18.3% | 66.0% | 15.6% | 0.015 |
| 5. Taking medications even if BP was normal for a consecutive period of time | 14.8% | 68.8% | 16.4% | 18.5% | 71.2% | 10.4% | 0.058* |
Notes: aDifference in change between groups in terms of individual items after controlling for clustering level, gender, age, education, ethnicity, marital status, antihypertensive medication history, self-efficacy, and other chronic medication-taking history (multilevel modeling results). *P<0.05.
Intervention effect on blood pressure control
Table 2 presents the blood pressure levels in both groups before and after the intervention. A significant difference of systolic blood pressure (SBP) was not found between two groups both at baseline (P=0.368) and six-month follow-up (P=0.597), though the SBP-value was elevated in both groups. Furthermore, the result of multilevel modeling indicated that the intervention effect on patients’ SBP was not significant. The intracluster correlation coefficient of SBP was 0.020.
The diastolic blood pressure (DBP) in the intervention group was significantly lower than that in the control group both before (P<0.001) and after the intervention (P<0.001). Result of multilevel modeling indicated that the intervention effect on patients’ DBP was not significant. The intracluster correlation coefficient of DBP was 0.022.
Discussion
Several studies have explored the prevalence of antihypertensive adherence and its determinants.8,28,29–31 However, although other Chinese residents have been closely examined, few studies shed lights upon Chinese mainland populations.29,31–35 Therefore, with the help of self-designed MA scale, this study examined the situation of antihypertensive adherence in a Chinese population and explored the effectiveness of an LCRP combined with case-based health education in improving MA
In this study, participants were predominantly female and elderly, with a mean age of 56±6.7 and a male-to-female proportion of 1:2. Some patients were lost to follow-up at six-month follow-up due to change of contact information or home addresses. However, the comparison between baseline and the six-month follow-up in both groups indicated no significant difference in socioeconomic characteristics. Therefore, it was reasonable to believe that loss to follow-up was random and comparable between the two groups.
After intervention, a significant increase in patients’ MA score was observed in both intervention group and control group. The baseline MA score did not differ between two groups while a significant difference was observed between two groups at six-month follow-up. The group difference at six-month follow-up remained significant after controlling for covariates and clustering effect. Based on the result of multilevel modeling, the group difference attributable to study intervention alone was 0.287 (95% CI: [0.103, 0.471]), indicating a significant impact of reminder package combined with health education on antihypertensive adherence. This result was not consistent with a study conducted in the United States, which suggested that low-cost reminders could not improve MA of patients with chronic disease or depression.21 However, another study found that low-cost reminder devices could improve HIV patients’ MA.36 As there were only few evidence examining low-cost devices on chronic disease MA, it was speculated that one of the reasons for the controversial result between Choudhry’s study and this study might be that their package adopted the form of visual reminder while ours provided audible beeps. To many patients, sounds might be harder to be missed or ignored than text. Another explanation might be that reminder package plus health education were more effective than reminder alone, as suggested in other studies.23 To sum up, this study suggests that more studies are needed to explore the effectiveness of low-cost devices in antihypertensive adherence.
The secondary analysis of blood pressure control revealed that LCRP combined with case-based health education could not improve hypertensive patients’ blood pressure control. This result was similar to several other studies evaluating the effect of reminder services on hypertensive patients’ blood pressure control.25,37 In a study conducted by Ruppar et al, although patients’ MA was significantly improved after a nurse-delivered adherence intervention which involved the use of an electronic medication bottle cap, patients’ blood pressure remained unchanged.25 Furthermore, in another study, differences in terms of blood pressure between the intervention group and control group were far from significance at any time in the study.37 However, some other research also reported that participants’ blood pressure was significantly improved after reminder package intervention.26 In effect, MA study itself had varying and sometimes even small effect on patients’ blood pressure outcome, as blood pressure was influenced by many factors other than MA, such as medication choices and lifestyle.38–40 Therefore, linking MA directly to blood pressure performance was difficult. As a result, although patients’ blood pressure was not improved in this study, the importance of MA to hypertensive patients and the value of LCRP combined with case-based health education could not be denied. In addition, patients’ SBP and DBP were elevated in this study. This might be attributed to seasonal factors that people’s blood pressure generally was higher in winter than in summer. The baseline survey was conducted from May to June 2016 (Summer in China) while the six-month follow-up survey was conducted from November to December 2016 (Winter in China). Therefore, it was possible that the elevated blood pressure was caused by season.
Analysis on individual items of MA scale indicated that this intervention could effectively improve patients’ performance on item 1 [Stopped taking medication without telling doctors when disease status deteriorated] and item 5 [Taking medications even if BP was normal for a consecutive period of time]. In hypertensive patients, stop taking medication without telling doctors is a very serious issue and might lead to severe consequences. Therefore, an improvement on this item is very important and has clinical implications.
Limitations
This study also had some limitations. First of all, patients’ MA and blood pressure in this study was relatively good. Therefore, participants had relatively small room for improvement, and it was more difficult for the intervention to exert an effect. Second, only 40.5% of the patients in the intervention group actually used the reminder package. Although the primary reason for not using was that they could remember taking medication on their own, there was still 15.2% of the patients reporting that it was a little complex to use. Therefore, this study suggests that future intervention could further simplify reminder package and intensify instructions on its use.
Practice implications
L.C.R.P. combined with case-based health education is an economical way to help hypertensive patients improve disease management, as the devices are non-expensive and education class can reach a cluster of population at a time. Furthermore, it is relatively simple to conduct and easily reproducible in different communities. Therefore, in terms of the benefits returned, namely MA improved in this study, LCRP combined with health education is worth promoting in all communities. Furthermore, the audible alarm might be more effective for reminder packages.
Conclusion
This study suggested that LCRP combined with case-based health education could significantly improve patients’ MA, which was crucial to hypertension management. At the end of the study, patients’ adherence was improved overall, with more increase in the intervention group (0.370, 95% CI [0.027, 0.714]).
Acknowledgments
We appreciate the efforts of the community health workers in Shunyi District, who have contributed considerable energy and time in this study. This work was funded by the Natural Science Foundation of Beijing (Grant No. 7162105).
Abbreviation list
SBP, systolic blood pressure; DBP, diastolic blood pressure; MA, Medication Adherence; LCRP, Low cost reminder package.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Kotchen TA. Hypertension control: trends, approaches, and goals. Hypertension. 2007;49(1):19–20. doi: 10.1161/01.HYP.0000250394.05703.06 [DOI] [PubMed] [Google Scholar]
- 2.Kearney P, Whelton M, Reynolds K, Muntner P, Whelton P, HE J. Global burden of hypertension: analysis of worldwide data. The Lancet. 2005;365(9455):217–223. doi: 10.1016/S0140-6736(05)70151-3 [DOI] [PubMed] [Google Scholar]
- 3.Collaboration NRF. Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19·1 million participants. Collaboration NRF, ed. The Lancet. 2017;389(10064):37–55. doi: 10.1016/S0140-6736(16)31919-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lawes CMM, Hoorn SV, Rodgers A. Global burden of blood-pressure-related disease, 2001. The Lancet. 2008;371(9623):1513–1518. doi: 10.1016/s0140-6736(08)60655-8 [DOI] [PubMed] [Google Scholar]
- 5.Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the global burden of disease study 2010. The Lancet. 2012;380(9859):2224–2260. doi: 10.1016/S0140-6736(12)61766-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mills KT, Bundy JD, Kelly TN, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. 2016;134(6):441–450. doi: 10.1161/CIRCULATIONAHA.115.018912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Krousel-Wood M, Thomas S, Muntner P, Morisky D. Medication adherence: a key factor in achieving blood pressure control and good clinical outcomes in hypertensive patients. Curr Opin Cardiol. 2004;19(4):357–362. doi: 10.1097/01.hco.0000126978.03828.9e [DOI] [PubMed] [Google Scholar]
- 8.Krousel-Wood MA, Muntner P, Islam T, Morisky DE, Webber LS. Barriers to and determinants of medication adherence in hypertension management: perspective of the cohort study of medication adherence among older adults. Med Clin North Am. 2009;93(3):753–769. doi: 10.1016/j.mcna.2009.02.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Matsumura K, Arima H, Tominaga M, et al. Impact of antihypertensive medication adherence on blood pressure control in hypertension: the COMFORT study. QJM. 2013;106(10):909–914. doi: 10.1093/qjmed/hct121 [DOI] [PubMed] [Google Scholar]
- 10.Bailey JE, Wan JY, Tang J, Ghani MA, Cushman WC. Antihypertensive medication adherence, ambulatory visits, and risk of stroke and death. J Gen Intern Med. 2010;25(6):495–503. doi: 10.1007/s11606-009-1240-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wong MC, Tam WW, Cheung CS, et al. Drug adherence and the incidence of coronary heart disease- and stroke-specific mortality among 218,047 patients newly prescribed an antihypertensive medication: a five-year cohort study. Int J Cardiol. 2013;168(2):928–933. doi: 10.1016/j.ijcard.2012.10.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Corrao G, Parodi A, Nicotra F, et al. Better compliance to antihypertensive medications reduces cardiovascular risk. J Hypertens. 2011;29(3):610–618. doi: 10.1097/HJH.0b013e328342ca97 [DOI] [PubMed] [Google Scholar]
- 13.Mazzaglia G, Ambrosioni E, Alacqua M, et al. Adherence to antihypertensive medications and cardiovascular morbidity among newly diagnosed hypertensive patients. Circulation. 2009;120(16):1598–1605. doi: 10.1161/CIRCULATIONAHA.108.830299 [DOI] [PubMed] [Google Scholar]
- 14.Pesa JA, Van Den Bos J, Gray T, et al. An evaluation of the impact of patient cost sharing for antihypertensive medications on adherence, medication and health care utilization, and expenditures. PPA. 2012;6:63–72. doi: 10.2147/PPA.S28396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pittman DG, Tao Z, Chen W, Stettin GD. Antihypertensive medication adherence and subsequent healthcare utilization and costs. Am J Manag Care. 2010;16(8):568–576. [PubMed] [Google Scholar]
- 16.Dragomir A, Côté R, Roy L, et al. Impact of adherence to antihypertensive agents on clinical outcomes and hospitalization costs. Med Care. 2010;48(5):418–425. doi: 10.1097/MLR.0b013e3181d567bd [DOI] [PubMed] [Google Scholar]
- 17.Abegaz TM, Shehab A, Gebreyohannes EA, Bhagavathula AS, Elnour AA. Nonadherence to antihypertensive drugs: a systematic review and meta-analysis. Medicine (Baltimore). 2017;96(4):e5641. doi: 10.1097/MD.0000000000005641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nielsen JØ, Shrestha AD, Neupane D, Kallestrup P. Non-adherence to anti-hypertensive medication in low- and middle-income countries: a systematic review and meta-analysis of 92 443 subjects. J Hum Hypertens. 2017;31(1):14–21. doi: 10.1038/jhh.2016.31 [DOI] [PubMed] [Google Scholar]
- 19.Hou Y, Zhang D, Gu J, et al. The association between self-perceptions of aging and antihypertensive medication adherence in older Chinese adults. Aging Clin Exp Res. 2015;28(6):1–8. [DOI] [PubMed] [Google Scholar]
- 20.Mahtani KR, Heneghan CJ, Glasziou PP, Perera R. Reminder packaging for improving adherence to self-administered long-term medications. Cochrane consumers and communication group, ed. Cochrane Database Syst Rev. 2011;36(9):CD005025. doi: 10.1002/14651858.CD005025.pub3 [DOI] [PubMed] [Google Scholar]
- 21.Choudhry NK, Krumme AA, Ercole PM, et al. Effect of reminder devices on medication adherence: the REMIND Randomized Clinical Trial.. JAMA Intern Med. 2017;177(5):624–631. doi: 10.1001/jamainternmed.2016.9627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ruppar TM, Dunbar-Jacob JM, Mehr DR, Lewis L, Conn VS. Medication adherence interventions among hypertensive black adults: a systematic review and meta-analysis. J Hypertens. 2017;35(6):1145–1154. doi: 10.1097/HJH.0000000000001260 [DOI] [PubMed] [Google Scholar]
- 23.Zedler BK, Kakad P, Colilla S, Murrelle L, Shah NR. Does packaging with a calendar feature improve adherence to self-administered medication for long-term use? A systematic review. Clin Ther. 2011;33(1):62–73. doi: 10.1016/j.clinthera.2011.02.003 [DOI] [PubMed] [Google Scholar]
- 24.Checchi KD, Huybrechts KF, Avorn J, Kesselheim AS. Electronic medication packaging devices and medication adherence: a systematic review. JAMA. 2014;312(12):1237–1247. doi: 10.1001/jama.2014.10059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ruppar TM. Randomized pilot study of a behavioral feedback intervention to improve medication adherence in older adults with hypertension. J Cardiovasc Nurs. 2010;25(6):470–479. doi: 10.1097/JCN.0b013e3181d5f9c5 [DOI] [PubMed] [Google Scholar]
- 26.McKenney JM, Munroe WP, Wright JT. Impact of an electronic medication compliance aid on long-term blood pressure control. J Clin Pharmacol. 1992;32(3):277–283. [DOI] [PubMed] [Google Scholar]
- 27.McLean SF. Case-based learning and its application in medical and health-care fields: a review of worldwide literature. J Med Educ Curric Dev. 2016;3:JMECD.S20377–11. doi: 10.4137/JMECD.S20377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yang S, He C, Zhang X, et al. Determinants of antihypertensive adherence among patients in Beijing: application of the health belief model. Patient Educ Couns. 2016;99(11):1894–1900. doi: 10.1016/j.pec.2016.06.014 [DOI] [PubMed] [Google Scholar]
- 29.Yue Z, Li C, Weilin Q, Bin W. Application of the health belief model to improve the understanding of antihypertensive medication adherence among Chinese patients. Patient Educ Couns. 2015;98(5):669–673. doi: 10.1016/j.pec.2015.02.007 [DOI] [PubMed] [Google Scholar]
- 30.Vawter L, Tong X, Gemilyan M, Yoon PW. Barriers to antihypertensive medication adherence among adults–United States, 2005. J Clin Hypertens (Greenwich). 2008;10(12):922–929. doi: 10.1111/j.1751-7176.2008.00049.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wong MCS, Jiang JY, Griffiths SM. Factors associated with antihypertensive drug compliance in 83,884 Chinese patients: a cohort study. J Epidemiol Community Health. 2010;64(10):895–901. doi: 10.1136/jech.2009.091603 [DOI] [PubMed] [Google Scholar]
- 32.Kang CD, Tsang PPM, Li WTL, et al. Determinants of medication adherence and blood pressure control among hypertensive patients in Hong Kong: a cross-sectional study. Int J Cardiol. 2015;182:250–257. doi: 10.1016/j.ijcard.2014.12.064 [DOI] [PubMed] [Google Scholar]
- 33.Wu P-H, Yang C-Y, Yao Z-L, Lin W-Z, Wu L-W, Chang -C-C. Relationship of blood pressure control and hospitalization risk to medication adherence among patients with hypertension in Taiwan. Am J Hypertens. 2010;23(2):155–160. doi: 10.1038/ajh.2009.210 [DOI] [PubMed] [Google Scholar]
- 34.Chen S-L, Tsai J-C, Lee W-L. The impact of illness perception on adherence to therapeutic regimens of patients with hypertension in Taiwan. J Clin Nurs. 2009;18(15):2234–2244. doi: 10.1111/j.1365-2702.2008.02706.x [DOI] [PubMed] [Google Scholar]
- 35.Wang W, Lau Y, Loo A, Chow A, Thompson DR. Medication adherence and its associated factors among Chinese community-dwelling older adults with hypertension. Heart Lung. 2014;43(4):278–283. doi: 10.1016/j.hrtlng.2014.05.001 [DOI] [PubMed] [Google Scholar]
- 36.Petersen ML, Wang Y, van der Laan MJ, Guzman D, Riley E, Bangsberg DR. Pillbox organizers are associated with improved adherence to HIV antiretroviral therapy and viral suppression: a marginal structural model analysis. Clin Infect Dis. 2007;45(7):908–915. doi: 10.1086/521250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Christensen A, Christrup LL, Fabricius PE, et al. The impact of an electronic monitoring and reminder device on patient compliance with antihypertensive therapy: a randomized controlled trial. J Hypertens. 2010;28(1):194–200. doi: 10.1097/HJH.0b013e328331b718 [DOI] [PubMed] [Google Scholar]
- 38.Conn VS, Hafdahl AR, Cooper PS, Ruppar TM, Mehr DR, Russell CL. Interventions to improve medication adherence among older adults: meta-analysis of adherence outcomes among randomized controlled trials. Gerontologist. 2009;49(4):447–462. doi: 10.1093/geront/gnp037 [DOI] [PubMed] [Google Scholar]
- 39.Márquez Contreras E, Vegazo García O, Martel Claros N, et al. Efficacy of telephone and mail intervention in patient compliance with antihypertensive drugs in hypertension. ETECUM-HTA study. Blood Press. 2005;14(3):151–158. doi: 10.1080/08037050510008977 [DOI] [PubMed] [Google Scholar]
- 40.Santschi V, Rodondi N, Bugnon O, Burnier M. Impact of electronic monitoring of drug adherence on blood pressure control in primary care: a cluster 12-month randomised controlled study. Eur J Intern Med. 2008;19(6):427–434. doi: 10.1016/j.ejim.2007.12.007 [DOI] [PubMed] [Google Scholar]