Abstract
The incidence of depressive symptoms in patients with stable coronary artery disease (SCAD) has significantly increased. However, its pathogenesis and treatment mechanisms are still incompletely understood. In this study, 144 patients with SCAD were recruited. Depressive symptoms of patients with SCAD were evaluated using Zung Self-Rating Depression Scale during hospitalization, and the patients were categorized into two subgroups: the non-depressive and depressive groups (further divided into mild and moderate/severe depressive groups). The rate of moderate/severe depressive symptoms in patients with SCAD was 18.8%. The mean age of patients in the depressive and mild depressive groups was older than that of those in the non-depressive group, and patients in the moderate/severe depressive group had higher high-density lipoprotein (HDL) and lower creatinine (Cr) levels. Binary logistic regression analysis showed that lower low-density lipoprotein (LDL) levels were significantly associated with increased risks of mild depressive symptoms, whereas higher HDL and lower Cr levels were significantly associated with moderate/severe depressive symptoms, suggesting that patients with SCAD were prone to experience depressive symptoms, especially in the elderly. Abnormality in LDL, HDL, and Cr levels might contribute to the depressive symptoms.
Keywords: depressive symptoms, stable coronary artery disease, elderly, lipoprotein, creatinine
INTRODUCTION
Depression, ranging widely from mild depressive symptoms to clinically diagnosed major depression, mainly characterized by depressed mood and loss of willpower, and accompanied by significant somatic or cognitive impairment, is an increasingly serious global problem [1, 2]. Approximately 20%–51% of patients with coronary heart disease (CHD) have been afflicted by clinical depression or depressive symptoms, which are significantly higher than that of 4.3% of the local population estimated by the World Health Organization (WHO, 2017) [3, 4]. However, the causal linkage between CHD and depression is still incompletely understood [5]. CHD accompanied by depression may be caused by multiple factors, including physiological and psychosocial factors, such as inflammation, endothelial dysfunction, hypothalamic–pituitary–adrenal axis hyperactivity, various behavioral factors, gut microbiome, and endocrine signaling [5, 6].
In patients with stable coronary artery disease (SCAD), the quality of life and health conditions decline sharply when complicated by depression, and depression is also one of the independent risk factors for adverse cardiovascular events [5, 7, 8]. Indeed, the 2012 American Heart Association Guidelines and 2013 European Society of Cardiology Guidelines on the management of SCAD (also known as stable ischemic heart disease) have already emphasized the need to screen depression in patients with SCAD and the necessity to provide appropriate interventions [9, 10]. However, because of the lack of necessary and sufficient understanding, depressive symptoms are usually masked under physical illness or manifest as severe somatic symptoms inconsistent with disease severity, for which making a correct diagnosis and taking appropriate intervention are difficult for clinicians.
To date, there are no definite data on the prevalence of depressive symptoms in patients with SCAD, particularly in the Chinese population. We investigated the prevalence rate and severity of depressive symptoms in patients with SCAD and identified the risk factors related to depressive symptoms by comparing clinical characteristics among patients to clarify the relationship between SCAD and depressive symptoms and to increase the attention of clinicians to the comorbidity.
RESULTS
Clinical characteristics of patients with SCAD in the non-depressive and depressive groups
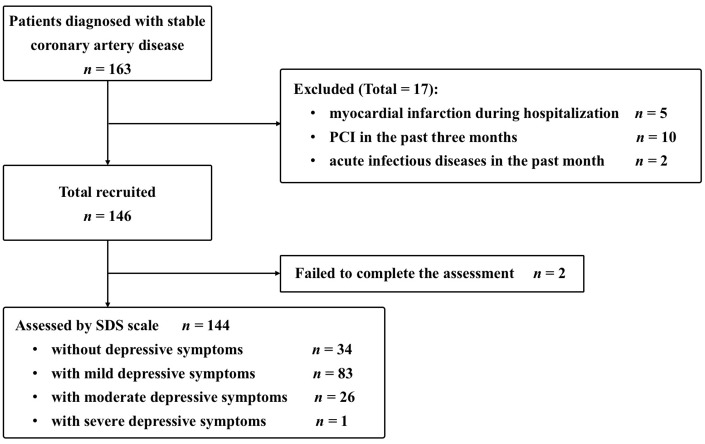
Of 163 patients with SCAD at baseline, 19 were excluded from this analysis: 5 with myocardial infarction during hospitalization, 10 with percutaneous coronary intervention (PCI) in the past 3 months, 2 with acute infectious diseases in the past month, and 2 who failed to complete the Zung Self-Rating Depression Scale (SDS) (Figure 1). No significant differences were found in the demographic and clinical characteristics between individuals and those excluded. The study sample was composed of 144 patients with SCAD, and the rates of no depressive symptoms, mild depressive symptoms, and moderate/severe depressive symptoms were 23.6%, 57.6%, and 18.8%, respectively.
Figure 1.
Inclusive cases. PCI, percutaneous coronary intervention; SDS, Self-Rating Depression Scale.
Table 1 shows the clinical characteristics of the two groups. The mean age of patients in the depressive group was older than that of those in the non-depressive group (P = 0.007). No significant differences were found between the two groups in other parameters. However, higher incidence of diabetes mellitus and higher Gensini scores were noted in the depressive group than those in the non-depressive group, although the differences did not show a statistical significance.
Table 1. Clinical characteristics of SCAD patients with or without depressive symptoms.
| Parameters | non-depressive symptoms group (n = 34) | depressive symptoms group (n = 110) | P value |
| Age (years) | 62.2 ± 14.2 | 63.2 ± 8.6 | 0.007 |
| Male (%) | 23(67.6) | 79(71.8) | 0.640 |
| Systolic blood pressure (mmHg) | 136 ± 19 | 134 ± 18 | 0.982 |
| Diastolic blood pressure (mmHg) | 80 ± 13 | 79 ± 10 | 0.236 |
| BMI (kg/m2) | 25.0 ± 3.2 | 24.6 ± 3.1 | 0.961 |
| Diabetes mellitus (%) | 8(23.5) | 38(34.5) | 0.229 |
| Current smoking (%) | 10(29.4) | 40(36.4) | 0.457 |
| ALT (U/L) | 27.5 ± 16.4 | 24.1 ± 14.7 | 0.195 |
| AST (U/L) | 25.1 ± 8.5 | 23.0 ± 7.6 | 0.151 |
| STB (μm/L) | 10.6 ± 3.5 | 10.4 ± 4.9 | 0.358 |
| High density lipoprotein (mmol/L) | 1.01 ± 0.22 | 2.13 ± 1.25 | 0.329 |
| Low density lipoprotein (mmol/L) | 2.12 ± 0.76 | 1.97 ± 0.64 | 0.300 |
| A/G | 1.69 ± 0.37 | 2.00 ± 0.37 | 0.495 |
| BUN (mg/dl) | 6.72 ± 2.77 | 7.39 ± 2.43 | 0.787 |
| Cr (μmmol/L) | 80.8 ± 30.0 | 75.5 ± 45.6 | 0.081 |
| Hb (g/L) | 138.1 ± 12.7 | 139.3 ± 12.0 | 0.809 |
| WBC (×109/L) | 6.82 ± 1.73 | 6.41 ± 1.49 | 0.206 |
| N (%) | 61.6 ± 7.2 | 64.6 ± 8.6 | 0.297 |
| L (%) | 28.8 ± 9.5 | 26.0 ± 8.7 | 0.626 |
| BNP (pg/ml) | 76.5 ± 57.1 | 63.4 ± 54.8 | 0.856 |
| Medications (%) | |||
| β Blockers | 9(26.5) | 44(40.0) | 0.153 |
| Statins | 15(44.1) | 52(47.3) | 0.747 |
| LVEF (%) | 61.7 ± 3.0 | 61.6 ± 2.77 | 0.841 |
| Gensini scores | 22.10 ± 13.99 | 28.69 ± 22.28 | 0.370 |
A/G, albumin/globulins; ALT, alanine aminotransferase; AST, aspartate aminotransferase; BMI, body mass index; BNP, brain natriuretic peptide; BUN, blood urea nitrogen; Cr, creatinine; Hb, hemoglobin; L%, lymphocyte percentage; LVEF, left ventricular ejection fraction; N%, neutrophil percentage; SCAD, stable coronary artery disease; STB, blood total bilirubin; WBC, white blood cell.
Clinical characteristics of patients with SCAD in the non-depressive and mild depressive groups
Table 2 shows the clinical characteristics of the two groups. The mean age of patients in the mild depressive group was older than that of those in the non-depressive group (P = 0.012). No significant differences were found between the two groups in other parameters. However, higher incidence of diabetes mellitus and higher Gensini scores were noted in the mild depressive group than those in the non-depressive group, although the differences did not show a statistical significance.
Table 2. Clinical characteristics of SCAD patients without or with mild depressive symptoms.
| Parameters | non-depressive symptoms group (n = 34) | mild depressive symptoms group (n = 83) | P value |
| Age (years) | 62.2 ± 14.2 | 63.3 ± 8.5 | 0.012 |
| Male (%) | 23(67.6) | 61(73.5) | 0.523 |
| Systolic blood pressure (mmHg) | 136 ± 19 | 132 ± 18 | 0.747 |
| Diastolic blood pressure (mmHg) | 80 ± 13 | 78 ± 10 | 0.121 |
| BMI (kg/m2) | 25.0 ± 3.2 | 24.6 ± 3.2 | 0.912 |
| Diabetes mellitus (%) | 8(23.5) | 29(34.9) | 0.228 |
| Current smoking (%) | 10(29.4) | 32(38.6) | 0.349 |
| ALT (U/L) | 27.5 ± 16.4 | 22.6 ± 12.9 | 0.080 |
| AST (U/L) | 25.1 ± 8.5 | 22.1 ± 7.2 | 0.051 |
| STB (μm/L) | 10.6 ± 3.5 | 10.6 ± 4.8 | 0.544 |
| High density lipoprotein (mmol/L) | 1.01 ± 0.22 | 1.03 ± 0.25 | 0.792 |
| Low density lipoprotein (mmol/L) | 2.12 ± 0.76 | 1.94 ± 0.64 | 0.259 |
| A/G | 1.69 ± 0.37 | 1.81 ± 0.67 | 0.538 |
| BUN (mg/dl) | 4.95 ± 1.65 | 5.07 ± 1.75 | 0.782 |
| Cr (μmmol/L) | 80.8 ± 30.0 | 81.3 ± 48.8 | 0.303 |
| Hb (g/L) | 138.1 ± 12.7 | 139.0 ± 12.5 | 0.928 |
| WBC (×109/L) | 6.82 ± 1.73 | 6.48 ± 1.50 | 0.315 |
| N (%) | 61.6 ± 7.2 | 65.1 ± 8.4 | 0.502 |
| L (%) | 28.8 ± 9.5 | 25.3 ± 8.6 | 0.515 |
| BNP (pg/ml) | 76.5 ± 57.1 | 65.5 ± 55.2 | 0.572 |
| Medications (%) | |||
| β Blockers | 9(26.5) | 33(39.8) | 0.174 |
| Statins | 15(44.1) | 35(42.2) | 0.847 |
| LVEF (%) | 61.7 ± 3.0 | 61.8 ± 4.1 | 0.861 |
| Gensini scores | 22.10 ± 13.99 | 27.33 ± 20.85 | 0.593 |
A/G, albumin/globulins; ALT, alanine aminotransferase; AST, aspartate aminotransferase; BMI, body mass index; BNP, brain natriuretic peptide; BUN, blood urea nitrogen; Cr, creatinine; Hb, hemoglobin; L%, lymphocyte percentage; LVEF, left ventricular ejection fraction; N%, neutrophil percentage; SCAD, stable coronary artery disease; STB, blood total bilirubin; WBC, white blood cell.
Table 3 shows the risk factors associated with mild depressive symptoms among patients with SCAD via binary logistic regression analysis. Lower low-density lipoprotein (LDL) levels (odds ratio [OR], 0.338; 95% confidence interval [CI], 0.131–0.875; P = 0.025), lower white blood cell (WBC) count (OR, 0.617; 95% CI, 0.430–0.884; P = 0.009), and β-blocker medication (OR, 0.236; 95% CI, 0.063–0.885; P = 0.032) were significantly associated with increased risks of mild depressive symptoms.
Table 3. Association of mild depressive symptoms and clinical characteristics.
| Parameters | B | OR (95% CI) | P value |
| Age (years) | -0.012 | 0.988 (0.938–1.041) | 0.653 |
| Male (%) | −0.558 | 0.572 (0.125–2.627) | 0.473 |
| Systolic blood pressure (mmHg) | 0.006 | 1.006 (0.966–1.049) | 0.758 |
| Diastolic blood pressure (mmHg) | −0.035 | 0.966 (0.904–1.032) | 0.303 |
| BMI (kg/m2) | 0.002 | 1.002 (0.841–1.193) | 0.982 |
| Diabetes mellitus (%) | −0.0497 | 0.608 (0.191–1.943) | 0.402 |
| Current smoking (%) | −0.959 | 0.383 (0.106–1.384) | 0.143 |
| ALT (U/L) | 0.018 | 1.019 (0.967–1.073) | 0.485 |
| AST (U/L) | −0.114 | 0.892 (0.797–0.998) | 0.051 |
| STB (μm/L) | −0.016 | 0.984 (0.864–1.121) | 0.811 |
| High density lipoprotein (mmol/L) | 1.192 | 4.914 (0.439–54.992) | 0.196 |
| Low density lipoprotein (mmol/L) | −1.084 | 0.338 (0.131–0.875) | 0.025 |
| A/G | 0.018 | 1.018 (0.716–1.448) | 0.919 |
| BUN (mg/dl) | −0.082 | 0.921 (0.671–1.265) | 0.613 |
| Cr (μmmol/L) | 0.003 | 1.003 (0.991–1.016) | 0.576 |
| Hb (g/L) | 0.034 | 1.035 (0.985–1.087) | 0.172 |
| WBC (×109/L) | −0.483 | 0.617 (0.430–0.884) | 0.009 |
| N (%) | 0.085 | 1.089 (0.968–1.225) | 0.157 |
| L (%) | 0.012 | 1.012 (0.917–1.117) | 0.815 |
| BNP (pg/ml) | −0.004 | 0.996 (0.989–1.004) | 0.345 |
| Medications (%) | |||
| β Blockers | −1.443 | 0.236 (0.063–0.885) | 0.032 |
| Statins | 1.204 | 3.335 (0.861–12.917) | 0.081 |
| LVEF (%) | −0.036 | 0.964 (0.822–1.131) | 0.654 |
| Gensini scores | 0.016 | 1.016 (0.992–1.041) | 0.186 |
A/G, albumin/globulins; ALT, alanine aminotransferase; AST, aspartate aminotransferase; BMI, body mass index; BNP, brain natriuretic peptide; BUN, blood urea nitrogen; Cr, creatinine; Hb, hemoglobin; L%, lymphocyte percentage; LVEF, left ventricular ejection fraction; N%, neutrophil percentage; SCAD, stable coronary artery disease; STB, blood total bilirubin; WBC, white blood cell.
Clinical characteristics of patients with SCAD in the non-depressive and moderate/severe depressive groups
Table 4 shows the clinical characteristics of the two groups. Patients with SCAD with moderate/severe depressive symptoms had higher HDL levels (P = 0.022) and lower creatinine (Cr) levels (P = 0.027). No significant differences were found between the two groups in other parameters. However, higher incidence of diabetes mellitus and higher Gensini scores were noted in the moderate/severe depressive group than those in the non-depressive group, although the differences did not show a statistical significance.
Table 4. Clinical characteristics of SCAD patients without or with moderate/severe depressive symptoms.
| Parameters | non-depressive symptoms group (n = 34) | moderate/severe depressive symptoms group (n = 27) | P value |
| Age (years) | 62.2 ± 14.2 | 62.8 ± 9.0 | 0.099 |
| Male (%) | 23(67.6) | 18(66.7) | 0.935 |
| Systolic blood pressure (mmHg) | 136 ± 19 | 140 ± 19 | 0.776 |
| Diastolic blood pressure (mmHg) | 80 ± 13 | 83 ± 11 | 0.855 |
| BMI (kg/m2) | 25.0 ± 3.2 | 24.7 ± 2.9 | 0.895 |
| Diabetes mellitus (%) | 8(23.5) | 9(33.3) | 0.396 |
| Current smoking (%) | 10(29.4) | 8(29.6) | 0.985 |
| ALT (U/L) | 27.5 ± 16.4 | 28.7 ± 18.7 | 0.816 |
| AST (U/L) | 25.1 ± 8.5 | 25.7 ± 8.4 | 0.765 |
| STB (μm/L) | 10.6 ± 3.5 | 9.8 ± 5.2 | 0.168 |
| High density lipoprotein (mmol/L) | 1.01 ± 0.22 | 1.14 ± 0.24 | 0.022 |
| Low density lipoprotein (mmol/L) | 2.12 ± 0.76 | 2.04 ± 0.66 | 0.665 |
| A/G | 1.69 ± 0.37 | 1.62 ± 0.25 | 0.647 |
| BUN (mg/dl) | 4.95 ± 1.65 | 5.30 ± 2.75 | 0.902 |
| Cr (μmmol/L) | 80.8 ± 30.0 | 68.7 ± 13.0 | 0.027 |
| Hb (g/L) | 138.1 ± 12.7 | 140.3 ± 10.4 | 0.316 |
| WBC (×109/L) | 6.82 ± 1.73 | 6.21 ± 1.46 | 0.127 |
| N (%) | 61.6 ± 7.2 | 63.0 ± 9.3 | 0.168 |
| L (%) | 28.8 ± 9.5 | 28.0 ± 8.8 | 0.851 |
| BNP (pg/ml) | 76.5 ± 57.1 | 56.9 ± 54.2 | 0.420 |
| Medications (%) | |||
| β Blockers | 9(26.5) | 11(40.7) | 0.238 |
| Statins | 15(44.1) | 17(62.9) | 0.143 |
| LVEF (%) | 61.7 ± 3.0 | 61.0 ± 7.3 | 0.843 |
| Gensini scores | 22.10 ± 13.99 | 32.87 ± 26.20 | 0.140 |
A/G, albumin/globulins; ALT, alanine aminotransferase; AST, aspartate aminotransferase; BMI, body mass index; BNP, brain natriuretic peptide; BUN, blood urea nitrogen; Cr, creatinine; Hb, hemoglobin; L%, lymphocyte percentage; LVEF, left ventricular ejection fraction; N%, neutrophil percentage; STB, blood total bilirubin; WBC, white blood cell.
Table 5 shows the risk factors associated with moderate/severe depressive symptoms among patients with SCAD via binary logistic regression analysis. Higher high-density lipoprotein (HDL) levels (OR, 82.553; 95% CI, 1.311–5196.951; P = 0.037) and lower Cr levels (OR, 0.876; 95% CI, 0.774–0.986; P = 0.029) were significantly associated with increased risks of moderate/severe depressive symptoms.
Table 5. Association of moderate/severe depressive symptoms and clinical characteristics.
| Parameters | B | OR (95% CI) | P value |
| Age (years) | 0.104 | 1.110 (0.923–1.334) | 0.269 |
| Male (%) | 0.194 | 1.214 (0.130–11.358) | 0.865 |
| Systolic blood pressure (mmHg) | −0.044 | 0.957 (0.882–1.040) | 0.301 |
| Diastolic blood pressure (mmHg) | 0.044 | 1.045 (0.925–1.182) | 0.479 |
| BMI (kg/m2) | −0.218 | 0.804 (0.581–1.112) | 0.187 |
| Diabetes mellitus (%) | −0.228 | 0.796 (0.107–5.935) | 0.824 |
| Current smoking (%) | −0.769 | 0.464 (0.44–4.928) | 0.524 |
| ALT (U/L) | 0.114 | 1.121 (0.979–1.284) | 0.098 |
| AST (U/L) | 0.214 | 0.807 (0.629–1.036) | 0.093 |
| STB (μm/L) | −0.053 | 0.949 (0.768–1.171) | 0.623 |
| High density lipoprotein (mmol/L) | 4.413 | 82.553 (1.311–5196.951) | 0.037 |
| Low density lipoprotein (mmol/L) | −0.130 | 0.878 (0.225–3.433) | 0.852 |
| A/G | 0.206 | 1.229 (0.037–40.618) | 0.908 |
| BUN (mg/dl) | 0.002 | 1.002 (0.528–1.903) | 0.994 |
| Cr (μmmol/L) | −0.135 | 0.874 (0.774–0.986) | 0.029 |
| Hb (g/L) | 0.099 | 1.104 (0.978–1.245) | 0.109 |
| WBC (×109/L) | −0.481 | 0.618 (0.342–1.118) | 0.111 |
| N (%) | 0.054 | 1.056 (0.828–1.346) | 0.661 |
| L (%) | 0.058 | 1.060 (0.865–1.298) | 0.573 |
| BNP (pg/ml) | −0.013 | 0.987 (0.973–1.002) | 0.099 |
| Medications (%) | |||
| β Blockers | −0.329 | 0.720 (0.048–10.724) | 0.811 |
| Statins | −2.173 | 0.114 (0.009–1.524) | 0.101 |
| LVEF (%) | −0.245 | 0.783 (0.567–1.081) | 0.137 |
| Gensini scores | 0.028 | 1.028 (0.999–1.059) | 0.063 |
A/G, albumin/globulins; ALT, alanine aminotransferase; AST, aspartate aminotransferase; BMI, body mass index; BNP, brain natriuretic peptide; BUN, blood urea nitrogen; Cr, creatinine; Hb, hemoglobin; L%, lymphocyte percentage; LVEF, left ventricular ejection fraction; N%, neutrophil percentage; STB, blood total bilirubin; WBC, white blood cell.
DISCUSSION
The results of this study showed that the incidence of depressive symptoms in patients with SCAD were significantly higher than that in the local population, which was estimated by the WHO (2017), and the rate of moderate/severe depressive symptoms was 18.8%. Interestingly, elderly patients were prone to experience depressive symptoms, and abnormality in LDL, HDL, and Cr levels might contribute to the depressive symptoms. Therefore, elderly patients with SCAD with LDL, HDL, and Cr abnormalities would promote the occurrence of depressive symptoms.
An increasing number of studies have suggested that age was an independent risk factor for the development of mood disorders, especially depression [11, 12], which may be highly related to the emotional instability caused by thalamic dysfunction in the elderly [13]. A 2 year follow-up study by Schaakxs et al. reported that older patients had a worse course of depressive disorder than younger patients, which was mainly manifested in the presence of any depression diagnosis (OR, 1.08; 95% CI, 1.00–1.17), chronic symptom course (OR, 1.24; 95% CI, 1.13–1.35), time to remission (hazard ratio, 0.91; P < 0.0001), and depression severity change (regression coefficient, 1.06; P < 0.0001), all of which were still mostly significant after adjusting for prognostic clinical, social, and health factors [12]. Furthermore, elderly people are more likely to take antidepressant drugs rather than psychotherapy when experiencing depression [14]. However, antidepressants could lead to dyslipidemia, thereby exacerbating cardiovascular diseases [15–17]. Moreover, the interaction between drugs and various chronic diseases (such as metabolic syndrome and cardiovascular disease) in elderly patients would have an influential impact on the effectiveness and risk of antidepressants [18]. These factors may affect the outcome of patients with SCAD accompanied by depressive symptoms. In addition, a known factor affecting the pathogenesis of depression in the elderly is cognitive decline, through multiple mechanisms, including hippocampal abnormalities, white matter hyperintensities, and amyloid beta levels [19, 20]. Therefore, assessment of cognitive decline is critical in subsequent studies attempting to reveal the role of age in the development of depressive symptoms in patients with SCAD.
Lipoprotein plays an important role in the development of CHD. Cholesterol in atherosclerotic plaque was proven to be derived from serum LDL, deemed as the atherogenic lipid. By contrast, HDL was considered to be the anti-atherosclerotic lipid, acting as a protective factor for CHD [21, 22]. Interestingly, the results of this study indicate that lower LDL and higher HDL levels in patients with SCAD are risk factors for depressive symptoms. Previous studies based on the data from the Korean National Health and Nutrition Examination Survey have identified that adjusted for other covariates, lower LDL and higher HDL levels were significantly associated with increased risk of depressive symptoms [23, 24]. Similarly, Persons et al. showed that lowering LDL levels could increase risk of depression, and improving the psychological status of patients could help regulate blood lipid levels [25]. The above evidence is consistent with the findings in the present study. Furthermore, after adjustment of demographic variables and cardiovascular risk factors, depression was associated with an increase in calcified plaque by measurement using coronary computed tomography angiography [26], which fully displayed the relationship between depression and atherosclerosis. The linkage between depressive symptoms and LDL and HDL levels may be due to differences in serotonin function and activity. Troisi et al. reported that cholesterol not only was a major component of cell membrane and myelin but also played a vital role in the development, activity, and stability of synapses [27]. Reduced cholesterol levels in the brain cell membrane would cause a decrease in lipid viscosity, which affects the exposure of serotonin receptors, thereby leading to depression [27]. Given that LDL and HDL levels are risk factors for depressive symptoms in patients with SCAD, increasing attention should be paid to the pathological basis of atherosclerosis and the risk of depression, as well as considering possible effects of lipid-lowering drugs on both aspects.
In this study, decreased Cr levels are risk factors for the onset of moderate/severe depressive symptoms, which are consistent with previous findings [28], which might be related to anorexia nervosa. Serum Cr has been known to be produced from both exogenous and endogenous processes. Exogenous Cr is the product of the digestible meat, whereas endogenous Cr is formed through irreversible non-enzymatic dehydration during muscle metabolism. Cr levels are relatively stable when there is a balance between meat intake and muscle metabolism but without renal failure (one of the exclusion criteria for this study) [29, 30]. Depression could lead to loss of appetite, reduced food intake, and decreased digestion function, which causes lower exogenous Cr levels. In addition, low mood and loss of willpower cause patients with depression to avoid social events and active exercise, thereby slowing muscle metabolism activity, which finally causes lower endogenous Cr levels [31, 32]. In this regard, clinical doctors must encourage patients to increase food intake and participate in exercise actively to increase the serum Cr levels, thereby improving depressive symptoms.
Furthermore, although the differences did not show a statistical significance, higher incidence of diabetes mellitus and higher Gensini scores were noted in the depressive group (both mild and moderate/severe groups), indicating that diabetes mellitus might be related to the occurrence of SCAD accompanied by depressive symptoms, and depressive symptoms could aggravate the degree of coronary artery stenosis. Given that these are all involved in inflammation, metabolism disorder, endothelial dysfunction, and platelet activation [5, 6, 33], a complex pathogenic network might likely exist in SCAD, diabetes mellitus, and depressive symptoms. Moreover, after searching the literature from January 1946 to December 2014, Doi-Kanno et al. showed that diabetes mellitus was a possible risk factor for depression in patients with myocardial infarction who underwent PCI [34]. In addition, numerous systematic reviews and prospective analyses agree that the involvement of depression could translate diabetes into increased CHD risk [33]. Thus, in future studies, more attention should be paid on patients with comorbid diseases, and appropriate interventions should be performed on patients with SCAD with predisposing factors playing a significant role in the progress of depressive symptoms.
The present study has some limitations. First, we did not assess other mental comorbidities and depressive symptoms by using other scales. Although SDS is one of the most widely used self-report scale, and its validity have been established in clinical depression evaluation [35–37], our results would have been more reliable if combined with the use of other scales. Second, we did not obtain data on some variables, such as social support, economic status, or marital status, which may influence the result to a certain extent. Third, it was a single-center, small-size study, and the patients recruited were from one hospital only, thereby raising concerns on generality from its findings. In addition, the significance of P value is discounted because of the strong standard deviations (SDs) in statistical analysis, which affects the reliability of the conclusions. Fourth, as a cross-sectional study, the results cannot affirm a causal relationship between depressive symptoms and the above-mentioned biochemical parameters. Future cohort studies will be necessary.
In conclusion, depressive symptoms are common among patients with SCAD, particularly in the elderly. Abnormalities in LDL, HDL, and Cr levels were significantly associated with the occurrence of depressive symptoms. These results underscore the importance of screening depressive symptoms in patients with SCAD and propose the potential intervention mechanisms of preventing the comorbidity. Large-scale prospective interventional studies should be encouraged to determine whether regulating LDL, HDL, and Cr levels can actually improve depressive symptoms of the SCAD population.
MATERIALS AND METHODS
Setting and participants
The study was a cross-sectional, observational, and single-center study. The patients surveyed in this study were randomly selected from all patients with SCAD in the Third Affiliated Hospital of Soochow University between July 2017 and October 2018. The study was approved by the Ethics Committee of the Third Affiliated Hospital of Soochow University and has been registered in the Chinese Clinical Trial Registry (ChiCTR1900020594).
Patients with SCAD meeting at least one of the following criteria were enrolled: (1) clinically diagnosed with myocardial infarction (>3 months); (2) coronary angiography showing a stenosis of >50% in one or more coronary arteries; (3) typical chest pain and noninvasive examination provided evidence of coronary artery stenosis or myocardial ischemia; and (4) underwent coronary artery bypass grafting or PCI (>3 months). All patients should have no evidence of myocardial injury (elevated myocardial enzymes) at the moment. The patients were able to complete the depression scale assessment and signed informed consent.
Exclusion criteria were as follows: (1) severe liver or kidney failure; (2) history of depression or other psychiatric disorders (on anti-depressant medication, clinical diagnosis, or previous treatment); (3) acute infectious disease within the past month; (4) other severe cardiovascular diseases, such as acute pericarditis, myocarditis, end-stage heart failure, or secondary heart disease; (5) diseases seriously affecting life expectancy (such as connective tissue disease, tumors, drug abuse, and dementia); (6) pregnant women; and (7) recent major stressful life events, trauma, or surgery.
Physical and clinical examination
Baseline data were obtained through interviews, medical records, and actual measurement, including age, sex, body mass index, blood pressure, diabetes history, smoking history, and β blocker and statin medication. Fasting venous blood samples were collected and sent to our laboratory for measurement of alanine aminotransferase, aspartate aminotransferase, blood total bilirubin, HDL, LDL, albumin/globulins, blood urea nitrogen, Cr, hemoglobin, WBC, neutrophil percentage, lymphocyte percentage, and brain natriuretic peptide. All patients underwent echocardiography to obtain left ventricular ejection fraction, and all the tests were performed and reported by the same physician in the hospital. All patients underwent coronary angiography via the brachial or radial artery, and the results were determined by two experienced cardiologists. The degree of stenosis of the left main artery, left anterior descending artery, circumflex artery, and right coronary artery lumen was recorded, and the Gensini score was calculated to quantitatively evaluate the degree of coronary artery stenosis.
Assessment of depression symptoms
Patients with SCAD were evaluated for depressive symptoms by using SDS during hospitalization. SDS is a self-reported clinical scale consisting of 20 items and scored on a 4-point scale to assess the psychological and physical symptoms of depression. The patients were categorized into three subgroups based on the results of SDS: non-depressive (score ≤52), mild depressive (score ≥53 but ≤62), and moderate/severe depressive groups (score ≥63).
Statistical analysis
Statistical analyses were performed using SPSS 24.0. Continuous data were presented as mean ± SD and compared using Student t test or Mann–Whitney U test. The categorical data were presented as percentage frequency (%) and compared using chi-squared test. Binary logistic regression analyses were used to determine the factors associated with depressive symptoms. The results were presented as ORs and 95% CIs. A two-tailed P < 0.05 indicates statistical significance.
ACKNOWLEDGMENTS
We thank all staff members and participants involved in the study.
Footnotes
AUTHOR CONTRIBUTIONS: All authors critically reviewed and approved the final version of the paper.
CONFLICTS OF INTEREST: The authors declare no conflicts of interest.
FUNDING: This work was supported by grants from the National Natural Science Foundation of China (81703482) and Major Science and Technology Project of Changzhou Municipal Commission of Health and Family Planning (ZD201601).
REFERENCES
- 1.Kendler KS. The genealogy of major depression: symptoms and signs of melancholia from 1880 to 1900. Mol Psychiatry. 2017; 22:1539–53. 10.1038/mp.2017.148 [DOI] [PubMed] [Google Scholar]
- 2.Uher R, Payne JL, Pavlova B, Perlis RH. Major depressive disorder in DSM-5: implications for clinical practice and research of changes from DSM-IV. Depress Anxiety. 2014; 31:459–71. 10.1002/da.22217 [DOI] [PubMed] [Google Scholar]
- 3.Lichtman JH, Froelicher ES, Blumenthal JA, Carney RM, Doering LV, Frasure-Smith N, Freedland KE, Jaffe AS, Leifheit-Limson EC, Sheps DS, Vaccarino V, Wulsin L, and American Heart Association Statistics Committee of the Council on Epidemiology and Prevention and the Council on Cardiovascular and Stroke Nursing. Depression as a risk factor for poor prognosis among patients with acute coronary syndrome: systematic review and recommendations: a scientific statement from the American Heart Association. Circulation. 2014; 129:1350–69. 10.1161/CIR.0000000000000019 [DOI] [PubMed] [Google Scholar]
- 4.Ren Y, Yang H, Browning C, Thomas S, Liu M. Prevalence of depression in coronary heart disease in China: a systematic review and meta-analysis. Chin Med J (Engl). 2014; 127:2991–98. [PubMed] [Google Scholar]
- 5.Vaccarino V, Badimon L, Bremner JD, Cenko E, Cubedo J, Dorobantu M, Duncker DJ, Koller A, Manfrini O, Milicic D, Padro T, Pries AR, Quyyumi AA, et al. , and ESC Scientific Document Group Reviewers. Depression and coronary heart disease: 2018 ESC position paper of the working group of coronary pathophysiology and microcirculation developed under the auspices of the ESC Committee for Practice Guidelines. Eur Heart J. 2019. 10.1093/eurheartj/ehy913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wu Y, Zhu B, Chen Z, Duan J, Luo A, Yang L, Yang C. New Insights Into the Comorbidity of Coronary Heart Disease and Depression. Curr Probl Cardiol. 2019. 10.1016/j.cpcardiol.2019.03.002 [DOI] [PubMed] [Google Scholar]
- 7.Jang HY, Song YK, Kim JH, Kim MG, Han N, Lee HY, Kim IW, Oh JM. Impact of depression on change in coronary heart disease risk status: the Korean Genome and Epidemiology Study (KoGES). Ther Clin Risk Manag. 2018; 14:121–28. 10.2147/TCRM.S149501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lahtinen M, Kiviniemi AM, Junttila MJ, Kääriäinen M, Huikuri HV, Tulppo MP. Depressive Symptoms and Risk for Sudden Cardiac Death in Stable Coronary Artery Disease. Am J Cardiol. 2018; 122:749–55. 10.1016/j.amjcard.2018.05.006 [DOI] [PubMed] [Google Scholar]
- 9.Fihn SD, Gardin JM, Abrams J, Berra K, Blankenship JC, Dallas AP, Douglas PS, Foody JM, Gerber TC, Hinderliter AL, King SB 3rd, Kligfield PD, Krumholz HM, et al. , and American College of Cardiology Foundation; American Heart Association Task Force on Practice Guidelines; American College of Physicians; American Association for Thoracic Surgery; Preventive Cardiovascular Nurses Association; Society for Cardiovascular Angiography and Interventions; Society of Thoracic Surgeons. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS Guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2012; 60:e44–164. 10.1016/j.jacc.2012.07.013 [DOI] [PubMed] [Google Scholar]
- 10.Montalescot G, Sechtem U, Achenbach S, Andreotti F, Arden C, Budaj A, Bugiardini R, Crea F, Cuisset T, Di Mario C, Ferreira JR, Gersh BJ, Gitt AK, et al. , and Document Reviewers. 2013 ESC guidelines on the management of stable coronary artery disease: the Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J. 2013; 34:2949–3003. 10.1093/eurheartj/eht296 [DOI] [PubMed] [Google Scholar]
- 11.Maarsingh OR, Heymans MW, Verhaak PF, Penninx BW, Comijs HC. Development and external validation of a prediction rule for an unfavorable course of late-life depression: A multicenter cohort study. J Affect Disord. 2018; 235:105–13. 10.1016/j.jad.2018.04.026 [DOI] [PubMed] [Google Scholar]
- 12.Schaakxs R, Comijs HC, Lamers F, Kok RM, Beekman AT, Penninx BW. Associations between age and the course of major depressive disorder: a 2-year longitudinal cohort study. Lancet Psychiatry. 2018; 5:581–90. 10.1016/S2215-0366(18)30166-4 [DOI] [PubMed] [Google Scholar]
- 13.Ng TP. Old age depression: worse clinical course, brighter treatment prospects? Lancet Psychiatry. 2018; 5:533–34. 10.1016/S2215-0366(18)30186-X [DOI] [PubMed] [Google Scholar]
- 14.Cooper C, Bebbington P, McManus S, Meltzer H, Stewart R, Farrell M, King M, Jenkins R, Livingston G. The treatment of Common Mental Disorders across age groups: results from the 2007 Adult Psychiatric Morbidity Survey. J Affect Disord. 2010; 127:96–101. 10.1016/j.jad.2010.04.020 [DOI] [PubMed] [Google Scholar]
- 15.Correll CU, Detraux J, De Lepeleire J, De Hert M. Effects of antipsychotics, antidepressants and mood stabilizers on risk for physical diseases in people with schizophrenia, depression and bipolar disorder. World Psychiatry. 2015; 14:119–36. 10.1002/wps.20204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fond G, Godin O, Brunel L, Aouizerate B, Berna F, Bulzacka E, Capdevielle D, Chereau I, Dorey JM, Dubertret C, Dubreucq J, Faget C, Gabayet F, et al. , and FACE-SZ (FondaMental Academic Centers of Expertise for Schizophrenia) group. Peripheral sub-inflammation is associated with antidepressant consumption in schizophrenia. Results from the multi-center FACE-SZ data set. J Affect Disord. 2016; 191:209–15. 10.1016/j.jad.2015.11.017 [DOI] [PubMed] [Google Scholar]
- 17.Himmerich H, Minkwitz J, Kirkby KC. Weight Gain and Metabolic Changes During Treatment with Antipsychotics and Antidepressants. Endocr Metab Immune Disord Drug Targets. 2015; 15:252–60. 10.2174/1871530315666150623092031 [DOI] [PubMed] [Google Scholar]
- 18.Kok RM, Reynolds CF 3rd. Management of Depression in Older Adults: A Review. JAMA. 2017; 317:2114–22. 10.1001/jama.2017.5706 [DOI] [PubMed] [Google Scholar]
- 19.Borza T, Engedal K, Bergh S, Benth JS, Selbæk G. The course of depression in late life as measured by the Montgomery and Asberg Depression Rating Scale in an observational study of hospitalized patients. BMC Psychiatry. 2015; 15:191. 10.1186/s12888-015-0577-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jamieson A, Goodwill AM, Termine M, Campbell S, Szoeke C. Depression related cerebral pathology and its relationship with cognitive functioning: A systematic review. J Affect Disord. 2019; 250:410–18. 10.1016/j.jad.2019.03.042 [DOI] [PubMed] [Google Scholar]
- 21.Kopin L, Lowenstein C. Dyslipidemia. Ann Intern Med. 2017; 167:ITC81–96. 10.7326/AITC201712050 [DOI] [PubMed] [Google Scholar]
- 22.Wang HH, Garruti G, Liu M, Portincasa P, Wang DQ. Cholesterol and Lipoprotein Metabolism and Atherosclerosis: Recent Advances In reverse Cholesterol Transport. Ann Hepatol. 2017. (Suppl. 1: s3-105.); 16:s27–42. 10.5604/01.3001.0010.5495 [DOI] [PubMed] [Google Scholar]
- 23.Shin HY, Kang G, Kang HJ, Kim SW, Shin IS, Yoon JS, Kim JM. Associations between serum lipid levels and depressive symptom in a Korean older population. Int J Geriatr Psychiatry. 2016; 31:1087–89. 10.1002/gps.4429 [DOI] [PubMed] [Google Scholar]
- 24.Shin HY, Kang G, Kang HJ, Kim SW, Shin IS, Yoon JS, Kim JM. Relationships between high-density lipoprotein cholesterol and depressive symptoms: Findings of the Korean National Health and Nutrition Examination Survey (KNHANES). Psychiatry Res. 2016; 241:172–74. 10.1016/j.psychres.2016.05.003 [DOI] [PubMed] [Google Scholar]
- 25.Persons JE, Robinson JG, Coryell WH, Payne ME, Fiedorowicz JG. Longitudinal study of low serum LDL cholesterol and depressive symptom onset in postmenopause. J Clin Psychiatry. 2016; 77:212–20. 10.4088/JCP.14m09505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Devantier TA, Nørgaard BL, Øvrehus KA, Marwan M, Poulsen MK, Achenbach S, Dey D, Videbech P. Coronary plaque volume and composition assessed by computed tomography angiography in patients with late-onset major depression. Psychosomatics. 2014; 55:243–51. 10.1016/j.psym.2013.09.001 [DOI] [PubMed] [Google Scholar]
- 27.Troisi A. Cholesterol in coronary heart disease and psychiatric disorders: same or opposite effects on morbidity risk? Neurosci Biobehav Rev. 2009; 33:125–32. 10.1016/j.neubiorev.2008.09.003 [DOI] [PubMed] [Google Scholar]
- 28.Peng YF, Zhong SM, Qin YH. The relationship between major depressive disorder and glucose parameters: A cross-sectional study in a Chinese population. Adv Clin Exp Med. 2017; 26:665–69. 10.17219/acem/63023 [DOI] [PubMed] [Google Scholar]
- 29.Delanaye P, Cavalier E, Pottel H. Serum Creatinine: Not So Simple! Nephron. 2017; 136:302–08. 10.1159/000469669 [DOI] [PubMed] [Google Scholar]
- 30.Levey AS, Eckfeldt JH. Estimating Glomerular Filtration Rate Using Serum Creatinine. Clin Chem. 2017; 63:1161–62. 10.1373/clinchem.2016.262352 [DOI] [PubMed] [Google Scholar]
- 31.Brand-Gothelf A, Leor S, Apter A, Fennig S. The impact of comorbid depressive and anxiety disorders on severity of anorexia nervosa in adolescent girls. J Nerv Ment Dis. 2014; 202:759–62. 10.1097/NMD.0000000000000194 [DOI] [PubMed] [Google Scholar]
- 32.Whited MC, Schneider KL, Appelhans BM, Ma Y, Waring ME, DeBiasse MA, Busch AM, Oleski JL, Merriam PA, Olendzki BC, Crawford SL, Ockene IS, Lemon SC, Pagoto SL. Severity of depressive symptoms and accuracy of dietary reporting among obese women with major depressive disorder seeking weight loss treatment. PLoS One. 2014; 9:e90361. 10.1371/journal.pone.0090361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hackett RA, Steptoe A. Psychosocial factors in diabetes and cardiovascular risk. Curr Cardiol Rep. 2016; 18:95. 10.1007/s11886-016-0771-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Doi-Kanno M, Fukahori H. Predictors of depression in patients diagnosed with myocardial infarction after undergoing percutaneous coronary intervention: a literature review. J Med Dent Sci. 2016; 63:37–43. 10.11480/jmds.630301 [DOI] [PubMed] [Google Scholar]
- 35.Domingueti CP, Dusse LM, Carvalho M, de Sousa LP, Gomes KB, Fernandes AP. Diabetes mellitus: the linkage between oxidative stress, inflammation, hypercoagulability and vascular complications. J Diabetes Complications. 2016; 30:738–45. 10.1016/j.jdiacomp.2015.12.018 [DOI] [PubMed] [Google Scholar]
- 36.Suzuki T, Shiga T, Kuwahara K, Kobayashi S, Suzuki S, Nishimura K, Suzuki A, Omori H, Mori F, Ishigooka J, Kasanuki H, Hagiwara N. Depression and outcomes in hospitalized Japanese patients with cardiovascular disease. - Prospective single-center observational study-. Circ J. 2011; 75:2465–73. 10.1253/circj.CJ-11-0140 [DOI] [PubMed] [Google Scholar]
- 37.Wang L, Song R, Chen Z, Wang J, Ling F. Prevalence of depressive symptoms and factors associated with it in type 2 diabetic patients: a cross-sectional study in China. BMC Public Health. 2015; 15:188. 10.1186/s12889-015-1567-y [DOI] [PMC free article] [PubMed] [Google Scholar]