SUMMARY
Intraventricular hemorrhage (IVH) is usually associated with premature infants; however, it has been estimated to occur in up to 5% of infants born at term and may be associated with different prenatal, perinatal and postnatal risk factors. The present retrospective study included toddlers aged 13-24 months, born at term (≥36 weeks), referred to the Department of Rheumatology, Physical Medicine and Rehabilitation in Zagreb, Croatia, because they had at least two risk factors for neurodevelopmental delay. A total of 63 patients without hemorrhage were control subjects, while 103 case patients were children with IVH. The ordinal logistic regression revealed that neurodevelopmental outcome in term infants was associated with IVH grade (p<0.05). Although more boys than girls suffered from severe IVH (grades III and IV), there were no statistically significant gender differences in the distribution of IVH or in neurodevelopmental outcomes (p>0.05).
Key words: Cerebral intraventricular hemorrhage; Developmental disabilities; Psychomotor disorders; Infant, premature; Infant, newborn; Risk factors
Introduction
Prenatal, perinatal and postnatal risk factors can result in intraventricular hemorrhage (IVH) as one of the most common forms of brain injury in infants. Prenatal risk factors include maternal genetic abnormalities, various medical conditions (e.g., gestational diabetes, herpes simplex), excessive alcohol consumption, smoking, etc. The most common perinatal risk factors are premature and obstructed labor, Apgar scores less than 7, perinatal asphyxia, and others. Postnatal risk factors include brain injuries, tumors, afebrile seizures, central nervous system infections, and others (1). The severity of IVH is usually classified by the system that was first reported by Papile et al., with grades ranging from I to IV (2).
Mostly found in preterm infants, IVH also appears in 3-5 percent of term newborns (3-6). Today, it is known that IVH can lead to delay in psychomotor development and reduction of motor repertoires, both in preterm and term neonates. These motor difficulties are often accompanied by difficulties in language, perception, thought, and others. Furthermore, they can affect academic and social functioning, as well as activities of daily living. Considering all of the above, early screening of newborns on maternity wards by a specialist in physical medicine and rehabilitation (physiatrist) specialized for children is very important as early interventions can enhance the individual’s potential (2, 7-10).
For more than 30 years, it has been known that male sex is associated with an increased prevalence of IVH, as many researchers have shown this in preterm infants. Additionally, numerous studies have found that IVH grades III and IV are major predictors of adverse neurodevelopmental outcome. The latter is usually measured either by screening tests or test batteries. While there are many motor coordination test batteries, most of them are not very useful for screening due to time and cost (9, 11-15).
The most commonly used test for rough estimation of psychomotor development of infants and toddlers in Croatia was designed in 1976 by the psychologist Nevenka Čuturić. Recent research has shown that this test is not sensitive enough to detect mild neurodevelopmental delay. Thus, we used another test, psychomotor developmental test, which was designed in 2015 by a physiatrist specialized in child rehabilitation to assess both motor and other accompanying difficulties in toddlers (7, 17).
The aim of the current study was to examine the association between IVH grade, gender and neurodevelopmental outcome in toddlers born at term, as well as to present the psychometric properties of the psychomotor developmental test.
Subjects and Methods
Participants
This retrospective study was conducted from April 2016 to August 2017 as part of a larger research project entitled Evaluation of Differences in the Effectiveness of Neurodevelopmental Stimulation in Medical Unit and Infirmary. The project has been approved by the Hospital Ethics Committee.
Toddlers were recruited from the Department of Rheumatology, Physical Medicine and Rehabilitation, Sestre milosrdnice University Hospital Centre, Zagreb, Croatia. They were referred to the Department because of prenatal, perinatal and postnatal risk factors; hence, they were at risk of neurodevelopmental delay.
Comprehensive interdisciplinary developmental evaluation included assessments by a physiatrist specialized in child rehabilitation, physical therapist, psychologist, speech pathologist and special education teacher.
Demographic, perinatal and postnatal data were retrieved from medical records including details on delivery and brain ultrasound. All ultrasound images were collected in the first 72 hours after birth.
Inclusion criteria were children aged 13 to 24 months. Non-inclusive criteria were data missing, toddlers born preterm (less than 36 weeks), chromosome abnormalities, and other medical conditions that may affect development (e.g., microcephaly). Exclusion criteria were respiratory or other infections in the last two weeks.
A total of 166 children were included in final analysis. Control group consisted of 63 children with no IVH on ultrasound, while experimental group included 103 children with IVH grades I-IV.
Measurements
Psychomotor development was assessed using the psychomotor development test (Appendix 1), developed in 2015 by the child physiatrist Matijević for children aged 13-24 months. It consists of two tests: test 1 (11 questions) examines motor development, while test 2 (10 questions) examines early development of communication, language and speech, spontaneous play and child socialization. Child physiatrists evaluate a toddler with rating 0 – not present or 1 – present on both tests.
The author proposed the following rating system: on test 1, 4 or less points indicate severe, 5 to 7 points moderate, and 8 or 9 points mild developmental delay, while 10 or more points denote normal development. On test 2, severe delay is scored 4 or less points, moderate delay 5 or 6 points, mild delay 7 or 8 points, and normal development 9 or 10 points. We evaluated this rating system whether it was sensitive enough to detect mild neurodevelopmental disorder.
The severity of IVH was graded according to the classification system developed by Papile et al., as follows: grade I IVH includes germinal matrix hemorrhage only, while grade II is IVH without ventricular dilatation. Severe IVH usually refers to grade III hemorrhage, i.e. the one that fills the ventricular system, and grade IV is IVH with parenchymal extension (2).
Statistical analysis
Statistical analysis was performed with the use of SPSS 23.0. Means and standard deviations were calculated for continuous variables and frequencies for categorical variables. Student’s t-test was used for comparison of two groups and χ2-test for categorical data.
To estimate the association between gender, IVH grade and neurodevelopmental outcome, we used ordinal logistic regression analysis. The receiver operating characteristic curve (ROC curve) was used to assess the sensitivity (true positive rate) and specificity (true negative rate) of our data. The level of statistical significance was set at p≤0.05.
Results
Study results are shown in Tables 1-5 and Figures 1-2.
Table 1. Descriptive data and t-test for case patients (N=103) and control subjects (N=63).
| Case patients | Control subjects | |||||
|---|---|---|---|---|---|---|
| Male (N=51) | Female (N=52) | p | Male (N=34) | Female (N=29) | p | |
| Age (months) | 17.27±3 | 18.12±3 | 0.188 | 17.62±3 | 18.03±3 | 0.629 |
| Birth weight (g) | 3172±608 | 3276±632 | 0.397 | 3205±492 | 3203±444 | 0.986 |
| Week of birth | 38.80±2 | 39.00±1 | 0.523 | 39.25±1 | 38.67±1 | 0.127 |
Table 2. Distribution of psychomotor development test 1 and test 2 results in girls and boys and χ2-test for gender differences.
| Case patients (N) | Control subjects (N) | Intraventricular hemorrhage | |||||
|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | |||
| Male | 51 | 34 | 34 | 12 | 17 | 18 | 6 |
| Female | 52 | 29 | 29 | 20 | 18 | 6 | 6 |
| χ2=3.869; p=0.424 | |||||||
Table 3. χ2-test and distribution of psychomotor development test 1 and test 2 results.
| Result | Test 1 | Test 2 | ||
|---|---|---|---|---|
| Case patients | Control subjects | Case patients | Control subjects | |
| Normal development | 27 (26%) | 34 (54%) | 43 (42%) | 49 (78%) |
| Mild delay | 35 (34%) | 13 (21%) | 30 (29%) | 12 (19%) |
| Moderate delay | 30 (29%) | 12 (19%) | 18 (17%) | 1 (1.5%) |
| Severe delay | 11 (11%) | 4 (6%) | 12 (12%) | 1 (1.5%) |
| χ2=44.551; p<0.001 | χ2=91.610; p<0.001 | |||
Table 4. Ordinal logistic regression for gender and IVH grade versus neurodevelopmental outcome on psychomotor development tests.
| Test 1 | Test 2 | ||||
|---|---|---|---|---|---|
| n | OR | 95% CI | OR | 95% CI | |
| Gender | |||||
| Female | 81 | 0.45 | (0.01-1.04) | 1.46 | (0.67-2.24) |
| Male | 85 | Ref | Ref | ||
| IVH | |||||
| 0 | 63 | 3.15 | (1.90-4.41) | 3.63 | (2.23-4.96) |
| 1 | 32 | 3.12 | (1.78-4.45) | 3.98 | (2.41-5.55) |
| 2 | 35 | 2.03 | (0.75-3.31) | 2.76 | (1.42-4.09) |
| 3 | 24 | 1.67 | (0.33-3.02) | 2.50 | (1.10-3.89) |
| 4 | 12 | Ref | Ref | ||
IVH = intraventricular hemorrhage; OR = odds ratio; 95% CI = 95% confidence interval; Ref = reference
Table 5. Neurodevelopmental outcomes on psychomotor development test according to IVH grade.
| Test 1 | Test 2 | |||||||
|---|---|---|---|---|---|---|---|---|
| Normal development | Mild delay | Moderate delay | Severe delay | Normal development | Mild delay | Moderate delay | Severe delay | |
| IVH | ||||||||
| 0 | 34 (54%) | 13 (21%) | 12 (19%) | 4 (6%) | 49 (77%) | 12 (19%) | 1 (2%) | 1 (2%) |
| 1 | 15 (47%) | 13 (41%) | 4 (12%) | 0 | 24 (75%) | 5 (16%) | 2 (6%) | 1 (3%) |
| 2 | 8 (23%) | 13 (37%) | 11 (31%) | 3 (9%) | 23 (65%) | 6 (17%) | 3 (9%) | 3 (9%) |
| 3 | 4 (17%) | 7 (29%) | 10 (42%) | 3 (12%) | 12 (50%) | 7 (29%) | 4 (17%) | 1 (4%) |
| 4 | 0 | 2 (16%) | 5 (42%) | 5 (42%) | 1 (9%) | 3 (25%) | 4 (33%) | 4 (33%) |
| χ2=44.235; p<0.001 | ?χ2=50.639; p<0.001 | |||||||
IVH = intraventricular hemorrhage
Fig. 1.
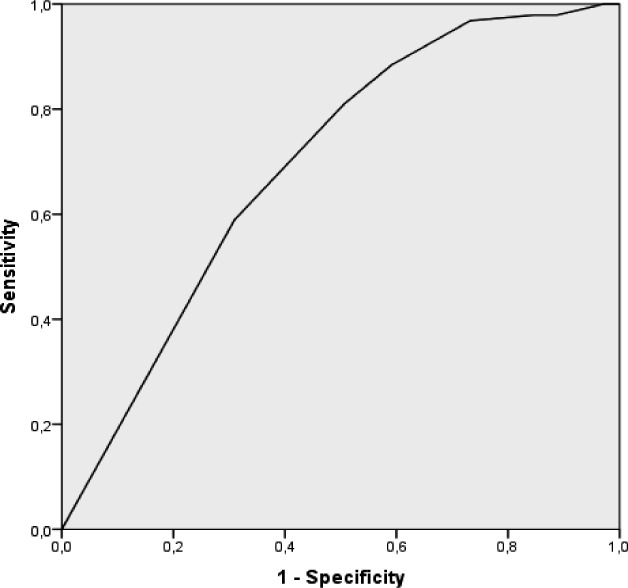
ROC curve – test 1 (AUC=0.726).
Fig. 2.
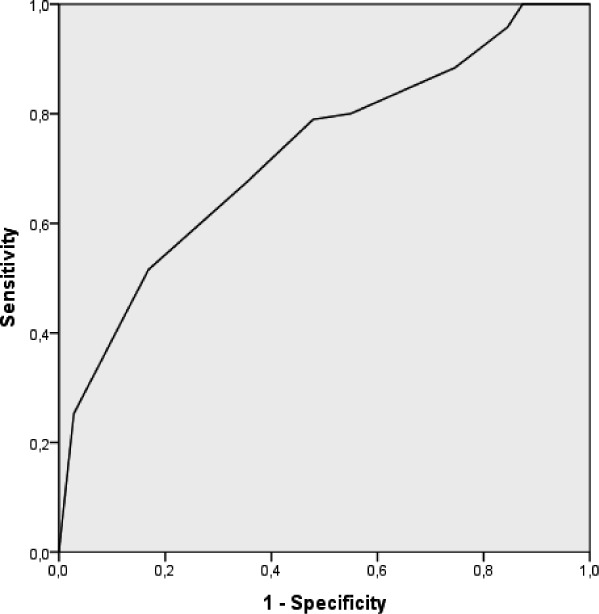
ROC curve – test 2 (AUC=0.701).
Discussion
The main goal of this study was to determine the association between gender, IVH grade and neurodevelopmental outcome in toddlers born at gestational age ≥36 weeks and to present the psychometric properties of screening by use of the psychomotor development test.
The groups of case patients and control subjects were matched by all relevant data, i.e. gender, age (at the time of test administration), week of birth and birth weight. Additionally, there was no statistically significant difference between boys and girls, or within the groups of case patients or control subjects.
Although male gender is associated with a greater risk of IVH grades III-IV and more boys than girls in our sample had severe IVH, the difference was not statistically significant. One of the possible explanations is that our subjects were not recruited based on their birth weight, as in many other studies. Furthermore, our sample consisted of toddlers that were born at term while most studies that found difference between males and females were conducted in preterm children (13-16, 18).
More than 50% of control subjects without IVH had normal development on test 1 and more than 75% had no delays on test 2. These results were similar to those recorded in the group with grade I IVH. Most of the children with grade II IVH had mild or moderate delay on test 1 and normal development on test 2. Children with grades III and IV hemorrhage had higher rates of moderate and severe delay on test 1. On the other hand, 50% of the infants with grade III hemorrhage were evaluated as having normal development on test 2. Considering that more than two-thirds of our subjects, both control and case, were estimated as having normal development on test 2, the possible ceiling effect should be taken in consideration (19).
Psychometric properties of the psychomotor development test mostly were very good. To estimate internal consistency of the reliability of our tests, we calculated Cronbach’s alpha coefficients and they were very good (20), 0.824 for test 1 and 0.803 for test 2. To check the stability of the test, we conducted test-retest reliability on 45 children. All the children were retested in 3-6 months after first administration. Correlation between initial and repeated testing was strong both for test 1 (r=0.769; p<0.001) and test 2 (r=0.752; p<0.001), yielding appropriate stability (21).
The results of our study suggested that neurodevelopmental outcome was similar in control subjects and case patients with grade I IVH (χ2=2.251; p=0.522), therefore, we merged them into one group. This is consistent with some other studies on premature infants that also showed that absence of IVH and grade 1 hemorrhage had comparable outcome (22). In order to examine the sensitivity and specificity of the psychomotor development test, we performed ROC curve analysis of both tests. The area under the curve (AUC) was slightly above 0.7 in both tests, suggesting that there is more than 70% chance that psychomotor development test will be able to distinguish between children with normal development and children with developmental delay (23).
Conclusion
Intraventricular hemorrhage may occur in term infants and carries a risk of adverse neurodevelopmental delay. Suspicion of IVH should include not only premature infants, but also infants born at term that have risk factors for neurodevelopmental delay. In many cases, early intervention can minimize delay in motor and other accompanying difficulties (e.g., language, perception). Therefore, we emphasize the importance of screening for general movements immediately at maternity wards by a specialist in physical medicine and rehabilitation.
Appendix 1. Psychomotor development test
| Test 1 | Test 2 |
|---|---|
| 1) Proper walking kinematics | 1) Knows his name |
| 2) Proper posture in standing position | 2) Exploring the environment |
| 3) Walking backwards | 3) Know functions of several objects |
| 4) Walking up the stairs | 4) Imitates activities |
| 5) Kicking the ball with their feet | 5) Understands basic/simple instructions |
| 6) Climbing on the furniture | 6) On request points the pictures in the book |
| 7) Bending to reach the toy | 7) Pronounces 5 and more words with meaning |
| 8) Taking off (clothes) socks, cap/hat | 8) Plays by himself |
| 9) Turning pages in the book | 9) On request points the parts of body (head, nose, ear) |
| 10) Building tower from 3 to 4 cubes | 10) Looking forward to be accompanied with other children |
| 11) Scribbles with pen |
References
- 1.Matijević M, Marunica Karsaj J. Neurorizično dijete. Fiz Rehabil Med. 2015;27(1-2):133–42. [Google Scholar]
- 2.Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. 1978;92(4):529–34. 10.1016/S0022-3476(78)80282-0 [DOI] [PubMed] [Google Scholar]
- 3.Afsharkhas L, Khalessi N, Karimi Panah M. Intraventricular hemorrhage in term neonates: sources, severity and outcome. Iran J Child Neurol. 2015;9(3):34–9. [PMC free article] [PubMed] [Google Scholar]
- 4.Mitchell W, O’Tuama L. Cerebral intraventricular hemorrhages in infants: a widening age spectrum. Pediatrics. 1980;65(1):35–9. 10.22037/ijcn.v9i3.7414 [DOI] [PubMed] [Google Scholar]
- 5.Gupta SN, Kechli AM, Kanamalla US. Intracranial hemorrhage in term newborns: management and outcomes. Pediatr Neurol. 2009. Jan;40(1):1–12. 10.1016/j.pediatrneurol.2008.09.019 [DOI] [PubMed] [Google Scholar]
- 6.Fink S. Intraventricular hemorrhage in the term infant. Neonatal Netw. 2000;19(7):13–8. 10.1891/0730-0832.19.7.13 [DOI] [PubMed] [Google Scholar]
- 7.Matijević V, Marunica Karsaj J. (Re)habilitation guidelines for children with neurodevelopmental disorders. Fiz Rehabil Med. 2015;27(3-4):302–29. [Google Scholar]
- 8.Futagi Y, Toribe Y, Ogawa K, Suzuki Y. Neurodevelopmental outcome in children with intraventricular hemorrhage. Pediatr Neurol. 2006;34(3):219–24. 10.1016/j.pediatrneurol.2005.08.011 [DOI] [PubMed] [Google Scholar]
- 9.Blank R, Smits-Engelsman B, Polatajko H, Wilson P. European Academy for Childhood Disability (EACD): recommendations on the definition, diagnosis and intervention of developmental coordination disorder (long version). Dev Med Child Neurol. 2012;54(1):54–93. 10.1111/j.1469-8749.2011.04171.x [DOI] [PubMed] [Google Scholar]
- 10.Lang Morović M, Matijević V, Divljaković K, Kraljević M, Dimić Z. Drawing skills in children with neurodevelopmental delay aged 2-5 years. Acta Clin Croat. 2015;54:119–26. [PubMed] [Google Scholar]
- 11.Bolisetty S, Dhawan A, Abdel-Latif M, Bajuk B, Stack J, Lui K. Intraventricular hemorrhage and neurodevelopmental outcomes in extreme preterm infants. Pediatrics. 2014;133(1):55–62. 10.1542/peds.2013-0372 [DOI] [PubMed] [Google Scholar]
- 12.Vohr BR, Allan WC, Westerveld M, Schneider KC, Katz KH, Makuch RW, et al. School-age outcomes of very low birth weight infants in the indomethacin intraventricular hemorrhage prevention trial. Pediatrics. 2003;111(4 Pt 1):e340–6. 10.1542/peds.111.4.e340 [DOI] [PubMed] [Google Scholar]
- 13.Tioseco JA, Aly H, Essers J, Patel K, El-Mohandes AA. Male sex and intraventricular hemorrhage. Pediatr Crit Care Med. 2006;7(1):40–4. 10.1097/01.PCC.0000192341.67078.61 [DOI] [PubMed] [Google Scholar]
- 14.Mohamed MA, Aly H. Male gender is associated with intraventricular hemorrhage. Pediatrics. 2010;125(2):e333–9. 10.1542/peds.2008-3369 [DOI] [PubMed] [Google Scholar]
- 15.Kent AL, Wright IM, Abdel-Latif ME. Mortality and adverse neurologic outcomes are greater in preterm male infants. Pediatrics. 2012;129(1):124–31. 10.1542/peds.2011-1578 [DOI] [PubMed] [Google Scholar]
- 16.Frondas-Chauty A, Simon L, Branger B, Gascoin G, Flamant C, Ancel PY, et al. Early growth and neurodevelopmental outcome in very preterm infants: impact of gender. Arch Dis Child Fetal Neonatal Ed. 2014;99(5):F366–72. 10.1136/archdischild-2013-305464 [DOI] [PubMed] [Google Scholar]
- 17.Radmilović G, Matijević V, Zavoreo I. Comparison of psychomotor development screening test and clinical assessment of psychomotor development. Acta Clin Croat. 2016;55:600–6. 10.20471/acc.2016.55.04.10 [DOI] [PubMed] [Google Scholar]
- 18.Suneja U, Gadiparthi R, Standish L, Rajegowda B, Prokhorov S. Intraventricular hemorrhage in full term newborn: a rare phenomenon. Arch Med. 2016;8:4 10.21767/1989-5216.1000156 [DOI] [Google Scholar]
- 19.Kaplan C. Ceiling effects in assessing high-IQ children with the WPPSI-R. J Clin Child Psychol. 1992;21(4):403–6. 10.1207/s15374424jccp2104_11 [DOI] [Google Scholar]
- 20.George D, Mallery P. SPSS for Windows step by step: a simple guide and reference, 4th edn. Boston: Allyn & Bacon; 2003. [Google Scholar]
- 21.Duff K. Evidence-based indicators of neuropsychological change in the individual patient: relevant concepts and methods. Arch Clin Neuropsychol. 2012;27(3):248–61. 10.1093/arclin/acr120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee JY, Kim HS, Jung E, Kim ES, Shim GH, Lee HJ, et al. Risk factors for periventricular-intraventricular hemorrhage in premature infants. J Korean Med Sci. 2010;25(3):418–24. 10.3346/jkms.2010.25.3.418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vanagas G. Receiver operating characteristic curves and comparison of cardiac surgery risk stratification systems. Interact Cardiovasc Thorac Surg. 2004;3(2):319–22. 10.1016/j.icvts.2004.01.008 [DOI] [PubMed] [Google Scholar]


