SUMMARY
The most severe effects of rheumatoid arthritis (RA) are loss of physical function and chronic pain, which may have a major impact on different areas of the person’s existence. The aim of this study was to get an insight into the quality of life (QOL) in subjects with RA in connection with pain perception and functional ability. The following instruments were used: the World Health Organization Quality of Life Questionnaire (WHOQOL-BREF), Short Form Health Survey (SF-36), Health Assessment Questionnaire Disability Index (HAQ-DI) and Visual Analog Scale for Pain (VAS Pain). The results indicated that there was no statistical difference in the QOL between subjects with RA and healthy population according to SF-36 Croatian norms. Also, the results showed that stronger pain experience was significantly associated with poorer social functioning assessment (SF36SF, Spearman’s rho=-0.463, p<0.05), poorer general health perception (SF36GH, Spearman’s rho=-0.432, p<0.05) and poorer physical functioning (WHOPH, Spearman’s rho=-0.688, p<0.01). Furthermore, the subjects evaluating their general functional state worse were found to have worse physical functioning (SF36PF, Spearman’s rho=-0.699 and WHOPH, Spearman’s rho=-0.769), poorer social functioning (SF36SF, Spearman’s rho=-0.580) and experienced greater pain intensity (SF36BP, Spearman’s rho=-0.652). Therefore, additional efforts should be invested to define a holistic and integrative model of treatment and rehabilitation of people with RA, focused on pain relief, improvement of functional ability, encouraging social interaction and supporting positive emotional responses.
Key words: Arthritis, rheumatoid; Quality of life; Health status; Pain; Activities of daily living
Introduction
Rheumatoid arthritis (RA) is an inflammatory chronic, progressive disease, which belongs to the systemic connective tissue diseases and affects mostly peripheral joints (1). Although progressive, the disease has its phases of high and low disease activity, which is translated into symptoms and functional ability. Any worsening of the disease leaves irreversible changes in the joints (2). The characteristic clinical features of RA usually involve the following problems: morning stiffness lasting for more than 1 hour, pain (usually more pronounced at rest), swelling of joints, deformities, limitation of physical activity, and consequently decreased quality of life (QOL) (1, 3). Fassbender (4) defines three different determinants that describe complete picture of RA: exudative inflammatory process, which causes swelling, pain and stiffness; proliferative-destructive process that affects joint destruction; and enzymatic collagenolytic process, which can cause primary necrotizing of, e.g., myocardial muscle, blood vessels, and sclera of the eye.
Rheumatoid arthritis affects approximately 1% of the world population (3). The leading symptom of rheumatic diseases is a sense of pain, and it is usually the main reason for seeking consultation (5). Pain can be considered as a complex dual phenomenon; one part is the perception of pain, and the other is the patient’s emotional reaction to it (6). Besides leading to unpleasant sensation, pain leads to the occurrence of depression in a number of patients (7, 8). According to Rezaei et al. (9), three illness perceptions significantly mediate the relationship between depression and pain: consequences, personal control, and emotional response. Pain is also brought into contact with a heightened sense of fatigue in this population. Thus, for example, Pollard et al. (10) state that high level of fatigue is often noticed in RA patients and is mostly associated with pain and depression.
Regarding pain perception, Lončarić-Katušin et al. (11) in their study, conducted on a sample of 1090 subjects with various causes of chronic pain, found that moderate and severe sleep quality disorders were significantly more frequent in subjects over 65 years of age, as well as in subjects with musculoskeletal, neuropathic and back pain. In the same group of subjects, the higher intensity of pain and poor sleep quality also were the leading cause of deterioration of the Patients’ Global Impression of Change Scale.
Quality of life in persons with rheumatoid arthritis
The World Health Organization (WHO) defines QOL as the individual’s perception of their position in life regarding culture and value systems in which they live, and in relation to their goals, expectations, standards and concerns. It is a wide concept that includes physical health, psychological state, level of independence, social relationships, personal beliefs and their relationship to salient features of their environment (12).
Because RA affects different areas of personal existence, determinants that could define QOL in this population have been constantly tested. Considering the results of different investigations, it appears that people with RA have significantly worse results in physical functioning in particular (13-15). However, RA also has a major impact on other areas of human life, e.g., social relationships, family life, and psychological well-being. Furthermore, because of RA, patients often are not able to perform everyday tasks in their private or professional life, and very often, they should change their profession or go to early retirement. Changes in self-perception in relation to painful stimuli, reduced functional ability, and labor and social inadequacy may also induce emotional and mental disorders. The overall negative effects of RA affect the patient QOL (16, 17). For this purpose, the aim of this research was to get an insight into the QOL in subjects with RA in connection with their functional ability and pain perception.
Subjects and Methods
Participants
The study included 25 patients suffering from RA (22 women and 3 men), median age 52 (range 21-88) years and medium disease duration 15 (range 1-30) years. The diagnosis was confirmed by an experienced rheumatologist and patients fulfilled the ACR/EULAR criteria (18). The study was carried out at the Department of Rheumatology, Physical Medicine and Rehabilitation, Sestre milosrdnice University Hospital Centre in Zagreb.
Instruments
The following instruments were used, as described below.
The World Health Organization Quality of Life Questionnaire, Short Form (WHOQOL-BREF) is a shorter version of the original instrument, and is more appropriate for use in a large research or clinical research. It has 26 items and measures the following dimensions: physical health (WHOPH), psychological health (WHOPSY), social relationship (WHOSR) and environment (WHOENV). The WHOQOL-BREF has appropriate psychometric properties in people with RA and represents a valid outcome measure for interventions that aim to improve the QOL in people with this disease (19). High internal consistency and test-retest stability were established for the results in the Croatian version of the WHOQOL-BREF, i.e. Cronbach alpha coefficients were 0.82 for Physical Health, 0.75 for Psychological Health, 0.66 for Social Relations and 0.80 for Environment (20).
The Short Form Health Survey (SF-36) is a set of generic, coherent, and easily administered QOL measures with 36 questions. It is a generic measure and can be used in general and specific populations. SF-36 consists of 8 scales, as follows: 1) Physical Functioning (SF36PF), 2) Role Limitation due to Physical Problems (SF36RP), 3) Role Limitations due to Emotional Problems (SF36RE), 4) Vitality (SF36VT), 5) Mental Health (SF36ME), 6) Social Functioning (SF36SF), 7) Body Pain (SF36BP), and 8) General Health Perception (SF36GH). Maslić Seršić and Vuletić (21) showed that population norms for the Croatian version of SF-36 could be used as a valid and reliable instrument in research of QOL in Croatian population.
The Health Assessment Questionnaire Disability Index (HAQ-DI) has become one of the dominant self-reported instruments for measuring functional state (disability) in many disease areas, including arthritis. It assesses the following dimensions: 1) dressing and grooming, 2) arising, 3) eating, 4) walking, 5) hygiene, 6) reach, 7) grip, and 8) common daily activities. It has 20 questions and respondents are intended to note the level of difficulty they have in performing activities mentioned above. Each question asks on a scale ranging from 0 to 3 if the activities can be performed without any difficulty (scale 0) up to cannot be done at all (scale 3). This questionnaire also includes two visual scales (HAQ-DI VAS1 and HAQ-DI VAS2) for evaluating pain and general health. Linde et al. (22) showed that HAQ-DI could be used as a valid and reliable instrument in measuring health-related QOL in persons with RA.
Visual Analog Scale for Pain (VAS Pain) consists of a line length of 10 cm at the ends of which extreme values are marked, from no pain to the greatest possible pain. The respondent should note the spot on the line that corresponds to the pain intensity. The scale is scored by measuring the distance from the “absence of pain” to the point that the respondent has marked. Test-retest reliability has been shown to be good, but higher among literate (r=0.94, p<0.001) than illiterate patients (r=0.71, p<0.001) before and after attending a rheumatology outpatient clinic. The VAS Pain is easy for use but some respondents can have difficulty understanding the instructions. In that case, supervision during the use of the scale can minimize the errors (23).
Approvals were obtained from the authors and/or publishers for using these instruments.
Procedures
The research was approved by the institutional Ethics Committee and an informed consent was obtained from all study participants. Due to the small number of respondents and non-normality of the distribution of results, Spearman’s correlation coefficient was used on data processing to assess the relationship between the variables, and Mann-Whitney U test to determine differences among respondents. Statistical analysis was performed using the SPSS 20.0 software (IBM SPSS Statistics). The level of significance was set at p<0.01.
Results
According to the aim of this study that tried to get an insight into the impact of RA on the QOL and network of different determinants which can be predictors of better coping with the disease, the instruments of WHOQOL-BREF, SF-36, HAQ-DI and VAS Pain were used (Table 1). The instruments used in the study were chosen for not being time consuming and for allowing comparison of the results of this and other studies based on their frequent use in other researches.
Table 1. Descriptive analysis of the results.
| Variables | N | Minimum | Maximum | M | SD | |
|---|---|---|---|---|---|---|
| HAQ-DI Scales | HAQ-DI TOTAL | 25 | 0.000 | 3.000 | 1.45000 | 0.951288 |
| HAQ-DI VAS1 | 25 | 0.1200 | 1.7600 | 1.075200 | 0.4100927 | |
| HAQ-DI VAS2 | 25 | 0.0000 | 1.9200 | 1.178400 | 0.3936547 | |
| Visual Analog Scale for Pain | VAS Pain | 25 | 0.1400 | 1.8800 | 1.068800 | 0.4134441 |
| SF-36 Scales | SF36PF | 25 | 0 | 100 | 35.40 | 29.542 |
| SF36RP | 25 | 0 | 100 | 25.00 | 33.850 | |
| SF36RE | 25 | 0.0000 | 100.0000 | 52.000000 | 48.1894410 | |
| SF36VT | 25 | 5 | 75 | 45.20 | 20.791 | |
| SF36ME | 25 | 8 | 96 | 66.24 | 22.718 | |
| SF36SF | 25 | 0.0 | 100.0 | 52.000 | 29.0205 | |
| SF36BP | 25 | 0.0 | 90.0 | 40.100 | 24.2113 | |
| SF36GH | 25 | 10 | 100 | 37.60 | 20.922 | |
| WHOQOL – BREF Scales | WHOPH | 25 | 19.0000 | 88.0000 | 49.400000 | 19.3326149 |
| WHOPSY | 25 | 31.0000 | 94.0000 | 67.360000 | 17.5496439 | |
| WHOSR | 25 | 25.0000 | 100.0000 | 67.800000 | 19.6022958 | |
| WHOENV | 25 | 44.0 | 94.0 | 67.160 | 12.5621 | |
HAQ-DI = Health Assessment Questionnaire Disability Index; HAQ-DI TOTAL = Health Assessment Questionnaire Disability Index-Total score; HAQ-DI VAS1 = Health Assessment Questionnaire Disability Index-Visual Analog Scale 1; HAQ-DI VAS2 = Health Assessment Questionnaire Disability Index-Visual Analog Scale 2; VAS = Visual Analog Scale for Pain; SF-36 = Short Form Health Survey; SF36PF = Short Form Health Survey-Physical Functioning; SF36RP = Short Form Health Survey-Role Limitation due to Physical Problems; SF36RE = Short Form Health Survey-Role Limitations due to Emotional Problems; SF36VT = Short Form Health Survey-Vitality; SF36ME = Short Form Health Survey-Mental Health; SF36SF = Short Form Health Survey-Social Functioning; SF36BP = Short Form Health Survey-Body Pain; SF36GH = Short Form Health Survey-General Health Perception; WHOQOL-BREF = World Health Organization Quality of Life Questionnaire-BREF; WHOPH = World Health Organization Quality of Life Questionnaire-BREF-Physical Health; WHOSR = World Health Organization Quality of Life Questionnaire-BREF-Social Relationship; WHOPSY = World Health Organization Quality of Life Questionnaire-BREF-Psychological; WHOENV = World Health Organization Quality of Life Questionnaire-BREF-Environment
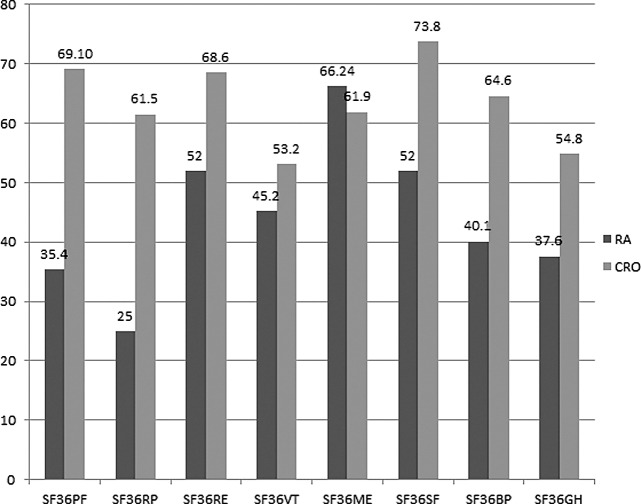
Figure 1 shows mean values of the results obtained on the SF-36 questionnaire scales in study participants (subjects with RA) and in the general population in Croatia (CRO). Standards for the general population in Croatia were established in the study by Maslić Seršić and Vuletić (21). The graph shows that on all SF-36 scales except for the SF36ME scale, general population evaluated QOL better than study subjects with RA. However, using the Mann-Whitney U test, it appeared that differences between these two groups were not statistically significant (Table 2).
Fig. 1.
Mean values of results obtained on the SF36 in the sample of RA patients and in the general population (CRO). RA = patients with RA (current research); CRO = general population of Croatia; SF-36 = Short Form Health Survey; SF36PF = Short Form Health Survey-Physical Functioning; SF36RP = Short Form Health Survey-Role Limitation Due to Physical Problems; SF36RE = Short Form Health Survey-Role Limitations due to Emotional Problems; SF36VT = Short Form Health Survey-Vitality; SF36ME = Short Form Health Survey-Mental Health; SF36SF = Short Form Health Survey-Social Functioning; SF36BP = Short Form Health Survey-Body Pain; SF36GH = Short Form Health Survey-General Health Perception
Table 2. Differences between the results of study subjects (RA patients) and the general population.
| SF36PF | SF36RP | SF36RE | SF36VT | SF36ME | SF36SF | SF36BF | SF36GH | |
|---|---|---|---|---|---|---|---|---|
| Mann-Whitney U | 4.000 | 4.000 | 12.000 | 11.000 | 11.000 | 8.000 | 3.000 | 3.000 |
| Wilcoxon W | 329.000 | 329.000 | 337.000 | 336.000 | 12.000 | 333.000 | 328.000 | 328.000 |
| Z | -1.140 | -1.237 | -0.073 | -0.201 | -0.201 | -0.605 | -1.282 | -1.284 |
| p | 0.254 | 0.216 | 0.942 | 0.841 | 0.841 | 0.545 | 0.200 | 0.199 |
SF-36 = Short Form Health Survey; SF36PF = Short Form Health Survey-Physical Functioning; SF36RP = Short Form Health Survey-Role Limitation due to Physical Problems; SF36RE = Short Form Health Survey-Role Limitations due to Emotional Problems; SF36VT = Short Form Health Survey-Vitality; SF36ME = Short Form Health Survey-Mental Health; SF36SF = Short Form Health Survey-Social Functioning; SF36BP = Short Form Health Survey-Body Pain; SF36GH = Short Form Health Survey-General Health Perception
Table 3 shows Spearman’s correlation coefficients between VAS Pain and HAQ-DI. The results showed a significant negative correlation between the intensity of pain and QOL in patients with RA. The VAS Pain and VAS1 scales showed high correlation, which means that the scales measure the same constructs. The results showed stronger pain experience to be significantly associated with poorer social functioning assessment (SF36SF, Spearman’s rho=-0.463, p<0.05), greater pain (SF36BP, Spearman’s rho=-0.554, p<0.01), poorer general health perception (SF36GH, Spearman’s rho=-0.432, p<0.05) and poorer physical functioning (WHOPH, Spearman’s rho=-0.688, p<0.01).
Table 3. Correlation of results obtained on the Visual Analogue Scales for Pain (HAQ-DI VAS1; VAS Pain) and SF-36, WHOQOL and HAQ-DI.
| HAQ-DI VAS1 | VAS Pain | |
|---|---|---|
| HAQ-DI VAS1 | 1.000 | 0.972** |
| VAS Pain | 0.972** | 1.000 |
| SF36PF | -0.262 | -0.318 |
| SF36RP | -0.337 | -0.429* |
| SF36RE | -0.131 | -0.185 |
| SF36VT | -0.133 | -0.121 |
| SF36ME | -0.073 | -0.105 |
| SF36SF | -0.433* | -0.463* |
| SF36BP | -0.553** | -0.554** |
| SF36GH | -0.442* | -0.432* |
| WHOPH | -0.627** | -0.688** |
| WHOPSY | -0.239 | -0.280 |
| WHOSR | -0.205 | -0.283 |
| WHOENV | -0.332 | -0.366 |
*Correlation significant at the 0.05 level; **correlation significant at the 0.01 level; HAQ-DI = Health Assessment Questionnaire Disability Index; HAQ-DI VAS1 = Health Assessment Questionnaire Disability Index-Visual-Analog Scale 1; VAS Pain = Visual Analog Scale for Pain; SF-36 = Short Form Health Survey; SF36PF = Short Form Health Survey-Physical Functioning; SF36RP = Short Form Health Survey-Role Limitation due to Physical Problems; SF36RE = Short Form Health Survey-Role Limitations due to Emotional Problems; SF36VT = Short Form Health Survey-Vitality; SF36ME = Short Form Health Survey-Mental Health; SF36SF = Short Form Health Survey-Social Functioning; SF36BP = Short Form Health Survey-Body Pain; SF36GH = Short Form Health Survey-General Health Perception; WHOQOL-BREF = World Health Organization Quality of Life Questionnaire-BREF; WHOPH = World Health Organization Quality of Life Questionnaire-BREF-Physical Health; WHOSR = World Health Organization Quality of Life Questionnaire-BREF-Social Relationship; WHOPSY = World Health Organization Quality of Life Questionnaire-BREF-Psychological; WHOENV = World Health Organization Quality of Life Questionnaire-BREF-Environment
Correlation between the QOL and functional capacity in RA patients showed a significant negative correlation (at p<0.01 level) obtained on the HAQ-DI and SF36PF, SF36SF, SF36BP and WHOPH scales (Table 4). The results indicated that subjects evaluating their general functional state worse had poorer physical functioning (SF36PF, Spearman’s rho=-0.699 and WHOPH, Spearman’s rho=-0.769) and social functioning (SF36SF, Spearman’s rho=-0.580), and experienced greater pain intensity (SF36BP, Spearman’s rho=-0.652). Similar results were obtained in other studies (15, 24).
Table 4. Spearman’s rank correlation coefficients among the HAQ-DI, SF-36 and WHOQOL-BREF.
| SF36PF | SF36RP | SF36RE | SF36VT | SF36ME | SF36SF | SF36BP | SF36GH | WHOPH | WHOPSY | WHOSR | WHOENV | HAQ-TOTAL | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SF36PF | 1.000 | 0.423* | 0.276 | 0.205 | 0.261 | 0.307 | 0.307 | 0.395 | 0.531** | 0.149 | 0.317 | 0.466* | -0.699** |
| SF36RP | 0.423* | 1.000 | 0.497* | 0.270 | 0.412* | 0.453* | 0.416* | 0.477* | 0.423* | 0.299 | 0.092 | 0.417* | -0.334 |
| SF36RE | 0.276 | 0.497* | 1.000 | .459* | 0.657** | 0.714** | 0.562** | 0.566** | 0.488* | 0.689** | 0.297 | 0.423* | -0.322 |
| SF36VT | 0.205 | 0.270 | 0.459* | 1.000 | 0.749** | 0.327 | 0.145 | 0.526** | 0.338 | 0.480* | 0.169 | 0.307 | -0.030 |
| SF36ME | 0.261 | 0.412* | 0.657** | 0.749** | 1.000 | 0.521** | 0.313 | 0.577** | 0.389 | 0.788** | 0.379 | 0.560** | -0.148 |
| SF36SF | 0.307 | 0.453* | 0.714** | 0.327 | 0.521** | 1.000 | 0.904** | 0.749** | 0.766** | 0.739** | 0.273 | 0.496* | -0.580** |
| SF36BP | 0.307 | 0.416* | 0.562** | 0.145 | 0.313 | 0.904** | 1.000 | 0.623** | 0.718** | 0.556** | 0.186 | 0.375 | -0.652** |
| SF36GH | 0.395 | 0.477* | 0.566** | 0.526** | 0.577** | 0.749** | 0.623** | 1.000 | 0.510** | 0.621** | 0.041 | 0.573** | -0.409* |
| WHOPH | 0.531** | 0.423* | 0.488* | 0.338 | 0.389 | 0.766** | 0.718** | 0.510** | 1.000 | 0.511** | 0.381 | 0.498* | -0.769** |
| WHOPSY | 0.149 | 0.299 | 0.689** | 0.480* | 0.788** | 0.739** | 0.556** | 0.621** | 0.511** | 1.000 | 0.407* | 0.499* | -0.252 |
| WHOSR | 0.317 | 0.092 | 0.297 | 0.169 | 0.379 | 0.273 | 0.186 | 0.041 | 0.381 | 0.407* | 1.000 | 0.273 | -0.403* |
| WHOENV | 0.466* | 0.417* | 0.423* | 0.307 | 0.560** | 0.496* | 0.375 | 0.573** | 0.498* | 0.499* | 0.273 | 1.000 | -0.490* |
| HAQ-DI TOTAL | -0.699** | -0.334 | -0.322 | -0.030 | -0.148 | -0.580** | -0.652** | -0.409* | -0.769** | -0.252 | -0.403* | -0.490* | 1.000 |
*Correlation significant at the 0.05 level; **correlation significant at the 0.01 level; SF-36 = Short Form Health Survey; SF36PF = Short Form Health Survey-Physical Functioning; SF36RP = Short Form Health Survey-Role Limitation due to Physical Problems; SF36RE = Short Form Health Survey-Role Limitations due to Emotional Problems; SF36VT = Short Form Health Survey-Vitality; SF36ME = Short Form Health Survey-Mental Health; SF36SF = Short Form Health Survey-Social Functioning; SF36BP = Short Form Health Survey-Body Pain; SF36GH = Short Form Health Survey-General Health Perception; WHOQOL-BREF = World Health Organization Quality of Life Questionnaire-BREF; WHOPH = World Health Organization Quality of Life Questionnaire-BREF-Physical Health; WHOSR = World Health Organization Quality of Life Questionnaire-BREF-Social Relationship; WHOPSY = World Health Organization Quality of Life Questionnaire-BREF-Psychological; WHOENV = World Health Organization Quality of Life Questionnaire-BREF-Environment; HAQ-DI TOTAL = Health Assessment Questionnaire Disability Index-Total score
Positive correlations between similar scales used in this study indicated that there was a correlation between the constructs measured by the scales. Thus, for example, lower pain experience assessed on the SF36BP scale was statistically significantly associated (at p=0.01 level) with improved QOL in the role limitations due to emotional problems (SF36RE, Spearman’s rho=0.056), social functioning (SF36SF, Spearman’s rho=0.904), general health perception (SF36GH, Spearman’s rho=0.623), physical (WHOPH, Spearman’s rho=0.718) and psychological functioning (WHOPSY, Spearman’s rho=0.566).
Discussion
Comparing the results obtained on the SF-36 questionnaire between RA patients and subjects from the general population reveals that the two groups differed on almost all scales, particularly in limitations due to physical functioning, social functioning, and pain; however, by using Mann Whitney U test, this difference was not statistically significant. In other words, the QOL in the RA patients included in this study and that from the general population had no statistically significant differences.
The results of this research differ from the results obtained in some other studies. Namely, according to them, patients with RA assessed their QOL worse than the general population. For example, Yacooub et al. (14) examined the disease related parameters affecting QOL on a sample of 250 Moroccan individuals with RA. Their results showed that the QOL was dramatically changed in RA patients. Disease duration, pain intensity, disease activity, immune status and functional disability were the main determinants linked with disruption of the QOL. A similar research was conducted by Haroon et al. (15) and the authors concluded that the QOL in individuals with RA was significantly lower compared with healthy populations, as well as that functional disability was the most important factor affecting their QOL. Salaffi et al. (16) compared the QOL in patients with RA, psoriatic arthritis and ankylosing spondylitis, and found that functional impairment, limitations due to physical functioning and physical pain had a significant impact on the QOL in patients with RA as compared to those related to mental health, restrictions arising from emotional health, social functioning and vitality. Roma et al. (13) analyzed and compared the QOL in 99 adults and elderly patients with RA. Adults were subjects aged 18 to 59 years, while those over 60 were considered elderly. Elderly RA patients were found to have lower mean values than adults in the following areas of SF-36: physical functioning, social functioning, and emotional aspects. Regarding pain, physical appearance, general health, vitality and mental aspects, elderly patients had better results. The authors concluded that the QOL and functional capacity were reduced in RA patients, but the results did not show significant differences between the two study groups. Garip et al. (17) also evaluated variables associated with QOL in RA patients and found pain to have the greatest negative impact on the QOL and functional status.
Similarly, in our study, a negative correlation was obtained between the intensity of pain on SF-36 and the constraints arising from emotional health, social functioning and overall health assessment obtained on SF-36 and physical functioning and psychological functioning on WHOQOL-BREF. Also, a significant positive correlation was obtained between the VAS Pain scale and HAQ-DI. This means that the stronger pain experience leads to worse functional state. Garip et al. (17) and Macejova et al. (25) also report on a high correlation between pain and HAQ-DI, thus confirming the validity of the results of this research. We can say that pain has great impact on different domains of the QOL. It can also be a major cause of negative emotional responses connected with depression, anxiety, anger, helplessness, and social isolation. For example, results of a systematic review and meta-analysis performed by Dickens et al. (8) showed that depression was more common in RA patients than in healthy individuals, and it was supposed that the intensity of depression depended in part on the levels of pain experience. Rezaei et al. (9) report on 66% of RA patients to have a clinically significant level of depression. In their study including 120 patients, Gibson and Clark (26) aimed to determine what the patients ranked first as the goal of treatment; almost half of the respondents (47%) ranked pain relief as the most desirable aim of their treatment, 20% gave priority to preventing deformity, and 21% preferred enabling better physical activity. Reducing stiffness (10%) and swelling (2%) were not defined as highly desirable benefits. Concerning the results obtained, the authors concluded that a substantial number of RA patients wanted pain relief above all other benefits.
An additional factor that may adversely affect the QOL and psychological status of RA patients is lower socioeconomic status. For example, Molina et al. (27) concluded that lower socioeconomic status correlated with long clinician waiting times and delay in disease-modifying anti-rheumatic drugs. Therefore, we can notice an urgent need for reducing treatment delay, along with lifestyle modification, improving low socioeconomic status and low educational status in RA patients (28).
Difference in the results of QOL comparison between RA patients and healthy population recorded in the present study and some other studies may be due to the small number of respondents included in the study. However, it may also reflect different experience of many parameters that define QOL in an individual. In addition, acquiring some compensatory functional skills and/or supportive psycho-emotional environment can reduce the negative impact of pain and functional disability on QOL in some RA patients (29, 30).
Results of this and other similar studies indicate that the QOL in RA patients should be seriously considered and is therefore assessed in many investigations. Taking this problem area in consideration could provide valuable contribution to defining a comprehensive treatment in persons with RA because, as emphasized by Matcham et al. (31), “assessing clinical state exclusively in terms of narrow disease activity may not characterize the health outcomes of primary concern to patients”.
In Croatia, several studies on the QOL in RA patients have been conducted to date. For example, the results obtained in the study by Vuger-Kovačić et al. (32) showed that patients with RA considered pain (98%) and reduced functional ability as a major problem. Also, fear of existential difficulties, disease deterioration, physical disability and family problems were stressed. It could lead to emotional problems such as anxiety, depression, and difficulties of adjustment to disease. The study by Žagar et al. (33) revealed positive correlation of pain experience, fatigue and disease activity with the level of depression in RA patients.
The present study was conducted in an attempt to add to the important problem area in persons with RA. A limitation of the study was the small number and inhomogeneity of respondents, as well as interpretation of results regardless of age, clinical features, disease duration and activity, thus reducing the generalizability of the results obtained. However, as in some other similar researches, this study highlighted the idea that self-experience and desirable benefits should be integrated in the treatment protocol for each individual patient. The QOL is an individual category and its improvement should imply personal experience of the individual. Furthermore, the integrative therapeutic model should include psychosocial support, activities to improve functional abilities, professional counseling, and using medical and complementary therapies to alleviate the symptoms of RA. In this way, the results of this study indicated the need for further research that would include a larger number of respondents homogenized by age, gender, comorbidities, sociodemographic parameters, duration of disease, etc. Assessing the impact of different interventions on the QOL should also be an important task that can help define a holistic and integrative model of treatment and rehabilitation for RA patients.
Conclusion
Upon reviewing the results of this and similar researches, it is concluded that pain and functional ability may have an important impact on QOL in RA patients through restrictions and unpleasant physical sensations they cause. Although the results of this study showed that there was no statistical difference in the QOL between RA patients and healthy population according to SF-36 Croatian norms, it was obvious that negative pain experience was significantly associated with poorer social functioning, general health perception and physical functioning. In addition, the patients who evaluated their general functional state worse, had poorer physical functioning, social functioning and pain experience. Knowledge about the impact of various parameters on the QOL in RA patients is important in the context of considering the predictors of QOL and planning of therapeutic and rehabilitation interventions, which should be focused on pain relief, improving functional ability, encouraging social interaction, and supporting positive emotional responses.
References
- 1.Majithia V, Geraci SA. Rheumatoid arthritis: diagnosis and management. Am J Med. 2007;120(11):936–9. 10.1016/j.amjmed.2007.04.005 [DOI] [PubMed] [Google Scholar]
- 2.Jajić I. Reumatologija. Priručnik za liječnike specijaliste reumatologije, specijaliste drugih graničnih struka i studente medicine. Zagreb: Medicinska knjiga, 1995. (in Croatian)
- 3.Gibofsky A. Overview of epidemiology, pathophysiology, and diagnosis of rheumatoid arthritis. Am J Manag Care. 2012. Dec 18; 13(Suppl):S295–302. [PubMed] [Google Scholar]
- 4.Fassbender HG. The clinical presentation of rheumatoid arthritis: the results from three separate pathogenetic mechanisms in adults and children. Acta Clin Croat. 2008;47(1):50–5. [Google Scholar]
- 5.Vlak T. Utjecaj reumatoidnog artritisa na radnu sposobnost bolesnika. Reumatizam. 2001;48(1):12–8. [in Croatian] [PubMed] [Google Scholar]
- 6.Grazio S, Nemčić T, Grubišić F. Bol u reumatoidnom artritisu i ostalim upalnim neinfektivnim artritisima. In: Jukić M, Majerić Kogler V, Fingler M, eds. Bol – uzroci i liječenje. Zagreb: Medicinska naklada; 2011; p. 122-34. (in Croatian) [Google Scholar]
- 7.Štambuk B. Reumatske bolesti i bol. Fizikalna medicina i rehabilitacija. 2002;17(1-2):47-53. (in Croatian)
- 8.Dickens C, McGowan L, Clark-Carter D, Creed F. Depression in rheumatoid arthritis: a systematic review of the literature with meta-analysis. Psychosom Med. 2002;64(1):52–60. 10.1097/00006842-200201000-00008 [DOI] [PubMed] [Google Scholar]
- 9.Rezaei F, Doost HTN, Molavi H, Abedi MR, Karimifar M. Depression and pain in patients with rheumatoid arthritis: mediating role of illness perception. Egypt Rheumatol. 2014;36(2):57–64. 10.1016/j.ejr.2013.12.007 [DOI] [Google Scholar]
- 10.Pollard LC, Choy EH, Gonzales J, Khoshaba B, Scott DL. Fatigue in rheumatoid arthritis reflects pain, not disease activity. Rheumatology. 2006;45(7):885–9. 10.1093/rheumatology/kel021 [DOI] [PubMed] [Google Scholar]
- 11.Lončarić-Katušin M, Milošević M, Žilić A, Mišković P, Majerić-Kogler V, Žunić J. Practical chronic pain assessment tools in clinical practice. Acta Clin Croat. 2016;55 Suppl 1:19–26. 10.20471/acc.2016.55.s1.02 [DOI] [PubMed] [Google Scholar]
- 12.Skevington SM, Lotfy M, O’Connell KA. The World Health Organization’s WHOQOL-BREF quality of life assessment: psychometric properties and results of the international field trial. A report from the WHOQOL Group. Qual Life Res. 2004;13:299–310. 10.1023/B:QURE.0000018486.91360.00 [DOI] [PubMed] [Google Scholar]
- 13.Roma I, Lourenco de Almeida M, Mansano N. Arruda Viani, Assis MR, Barbosa PMK. Quality of life in adults and elderly patients with rheumatoid arthritis. Rev Bras Reumatol. 2014;54(4):279–86. 10.1016/j.rbr.2014.03.025 [DOI] [PubMed] [Google Scholar]
- 14.Ibn Yacoub Y, Amine B, Laatiris A, Hajjaj-Hassoun N. Health-related quality of life in Moroccan patients with rheumatoid arthritis. Clin Rheumatol. 2012;31:1471–7. 10.1007/s10067-012-2037-x [DOI] [PubMed] [Google Scholar]
- 15.Haroon N, Aggarwall A, Lawrence VA, Misra R. Impact of rheumatoid arthritis on quality of life. Mod Rheumatol. 2007;17:290–5. 10.3109/s10165-007-0604-9 [DOI] [PubMed] [Google Scholar]
- 16.Salaffi F, Carotti M, Gasparini S, Intorcia M, Grassi W. The health-related quality of life in rheumatoid arthritis, ankylosing spondylitis, and psoriatic arthritis: a comparison with a selected sample of healthy people. Health Qual Life Outcomes. 2009;7:25. 10.1186/1477-7525-7-25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Garip Y, Eser F, Bodur H. Health-related quality of life in rheumatoid arthritis: comparison of RAQoL with other scales in terms of disease activity, severity of pain, and functional status. Rheumatol Int. 2011;31(6):769–72. 10.1007/s00296-009-1353-1 [DOI] [PubMed] [Google Scholar]
- 18.Aletaha D, Neogi T, Silman AJ, et al. Rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Ann Rheum Dis. 2010;69:1580–8. 10.1136/ard.2010.138461 [DOI] [PubMed] [Google Scholar]
- 19.Taylor WJ, Myers J, Simpson RT, McPherson KM, Weatherall M. Quality of life of people with rheumatoid arthritis as measured by the World Health Organization Quality of Life instrument, short form (WHOQOL-BREF): score distributions and psychometric properties. Arthritis Rheum. 2004;51(3):350–7. 10.1002/art.20398 [DOI] [PubMed] [Google Scholar]
- 20.Radošević-Vidaček B, Macan J, Koščec A. Stres i alergija. Arh Hig Rada Toksikol. 2004;55:205–11. [in Croatian] [PubMed] [Google Scholar]
- 21.Maslić Seršić D, Vuletić G. Psychometric evaluation and establishing norms of Croatian SF-36 Health Survey: framework for subjective health research. Croat Med J. 2006;47:95–102. [PMC free article] [PubMed] [Google Scholar]
- 22.Linde L, Sorensen J, Ostergaard M, Horslev-Petersen K, Hetland ML. Health-related quality of life: validity, reliability, and responsiveness of SF-36, 15D, EQ-5D (corrected) RAQoL, and HAQ in patients with rheumatoid arthritis. J Rheumatol. 2008;35:1528–37. [PubMed] [Google Scholar]
- 23.Hawker GA, Samra M, Kendzerska T, French M. Measures of adult pain. Arthritis Care Res (Hoboken). 2011;63 S11:S240–52. 10.1002/acr.20543 [DOI] [PubMed] [Google Scholar]
- 24.ten Klooster PM, Vonkeman HE, Taal E, Siemons L, Hendriks L, de Jong AJL, et al. Performance of the Dutch SF-36 version 2 as a measure of health-related quality of life in patients with rheumatoid arthritis. Health Qual Life Outcomes. 2013;11:77. 10.1186/1477-7525-11-77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Macejová Z, Nagyova I, Szilasiova A, Kovarova M, Spisak B. Pain and rheumatoid arthritis. Vnitr Lek. 1999;45(6):359–63. [PubMed] [Google Scholar]
- 26.Gibson T, Clark B. Use of simple analgesics in rheumatoid arthritis. Ann Rheum Dis. 1985;44:27–9. 10.1136/ard.44.1.27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Molina E, del Rincon I, Restrepo JF, Battafarano DF, Escalante A. Association of socioeconomic status with treatment delays, disease activity, joint damage, and disability in rheumatoid arthritis. Arthritis Care Res (Hoboken). 2015;67(7):940–6. 10.1002/acr.22542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Callahan LF, Corday DS, Wells G, Pincus T. Formal education and five-year mortality in rheumatoid arthritis: mediation by helplessness scale scores. Arthritis Care Res. 1996;9(6):463–72. 10.1002/art.1790090608 [DOI] [PubMed] [Google Scholar]
- 29.Englbrecht M, Kruckow M, Araujo E, Rech J, Schett G. The interaction of physical function and emotional well-being in rheumatoid arthritis – what is the impact on disease activity and coping? Semin Arthritis Rheum. 2013;42(5):482–91. 10.1016/j.semarthrit.2012.09.003 [DOI] [PubMed] [Google Scholar]
- 30.Dures E, Almeida C, Caesley J, et al. Patient preferences for psychological support in inflammatory arthritis: a multicentre survey. Ann Rheum Dis. 2016;75(1):142–7. 10.1136/annrheumdis-2014-205636 [DOI] [PubMed] [Google Scholar]
- 31.Matcham F, Scott IC, Rayner L, Hotopf M, Kingsley GH, Norton S, et al. The impact of rheumatoid arthritis on quality-of-life assessed using the SF-36: a systematic review and meta-analysis. Semin Arthritis Rheum. 2014;44(2):123–30. 10.1016/j.semarthrit.2014.05.001 [DOI] [PubMed] [Google Scholar]
- 32.Vuger-Kovačić D, Kovačić D, Budišin V, Slijepčević B, Bitar Z. Emocionalne reakcije u oboljelih od reumatoidnog artritisa. Reumatizam. 2010;57(2):134 [in Croatian] [Google Scholar]
- 33.Žagar I, Babić-Naglić Đ, Ćurković B, Kovač Durmiš K. Depresija i reumatoidni artritis. Reumatizam. 2010;58(2):147 [in Croatian] [Google Scholar]