Abstract
Background:
The long-term predicted value of microvolt T-wave alternans (MTWA) for ventricular tachyarrhythmia in patients with arrhythmogenic right ventricular cardiomyopathy (ARVC) remains unclear. Our study explored the characteristics of MTWA and its prognostic value when combined with an electrophysiologic study (EPS) in patients with ARVC.
Methods:
All patients underwent non-invasive MTWA examination with modified moving average (MMA) analysis and an EPS. A positive event was defined as the first occurrence of sudden cardiac death, documented sustained ventricular tachycardia (VT), ventricular fibrillation, or the administration of appropriate implantable cardioverter defibrillator therapy including shock or anti-tachycardia pacing.
Results:
Thirty-five patients with ARVC (age 38.6 ± 11.0 years; 28 males) with preserved left ventricular (LV) function were recruited. The maximal TWA value (MaxValt) was 17.0 (11.0–27.0) μV. Sustained VT was induced in 22 patients by the EPS. During a median follow-up of 99.9 ± 7.7 months, 15 patients had positive clinical events. When inducible VT was combined with the MaxValt, the area under the curve improved from 0.739 to 0.797. The receiver operating characteristic curve showed that a MaxValt of 23.5 μV was the optimal cutoff value to identify positive events. The multivariate Cox regression model for survival showed that MTWA (MaxValt, hazard ratio [HR], 1.06; 95% confidence interval [CI], 1.01–1.11; P = 0.01) and inducible VT (HR, 5.98; 95% CI, 1.33–26.8; P = 0.01) independently predicted positive events in patients with ARVC.
Conclusions:
MTWA assessment with MMA analysis complemented by an EPS might provide improved prognostic ability in patients with ARVC with preserved LV function during long-term follow-up.
Keywords: Modified moving average analysis, Microvolt T-wave alternans, Electrophysiologic study, Ventricular tachyarrhythmia, Arrhythmogenic right ventricular cardiomyopathy
Introduction
Arrhythmogenic right ventricular cardiomyopathy (ARVC) is an inherited cardiomyopathy characterized by right ventricular (RV) dysfunction and ventricular arrhythmias.[1] Studies have shown that ARVC is present in up to 20% of individuals who experience sudden cardiac death (SCD) and is even more common among athletes who die suddenly.[2]
Prevention of SCD is the most important goal in the clinical management of patients with ARVC. According to the consensus guidelines, currently, the implantable cardioverter defibrillator (ICD) is the only effective strategy for the prevention of SCD.[3,4] More effective markers are needed to determine the long-term prognosis of patients with ARVC.
Microvolt T-wave alternans (MTWA) is a non-invasive test of arrhythmia vulnerability. Previous studies have shown that MTWA can predict ICD shocks and ventricular tachyarrhythmic events in diverse patient populations, including those with heart failure and ischemic cardiomyopathy.[5,6] Ambulatory electrocardiograph-based TWA was reported to exhibit prognostic ability in patients with ARVC.[7] Currently, electrophysiologic studies (EPSs) are also used to predict the prognosis in patients with ARVC. However, studies have shown mixed results.[8–12] Saguner et al[8] reported that inducible sustained monomorphic ventricular tachycardia (VT) might predict long-term adverse outcomes in patients with ARVC.
Therefore, the objective of this study was to explore the prognostic value of MTWA using modified moving average (MMA) analysis complemented by an EPS in patients with ARVC with preserved left ventricular (LV) function during long-term follow-up.
Methods
Ethical approval
The study protocol was approved by the institutional ethics committee of the First Affiliated Hospital of Nanjing Medical University. All participants provided written informed consent.
Patient recruitment
Between January 2007 and November 2008, all in-hospital patients with ARVC were consecutively recruited. The diagnosis of ARVC was established on the basis of the criteria set by the Task Force of the Working Group of Myocardial and Pericardial Disease of the European Society of Cardiology and the Scientific Council on Cardiomyopathies of the International Society and Federation of Cardiology.[1] All patients underwent MTWA tests and EPSs. Patients with acute infectious disease, acute myocardial ischemia, or uncontrolled heart failure or who were unable to complete the treadmill exercise test were excluded.
Treadmill exercise test and measurement of microvolt T-wave alternans
The exercise test was performed using a treadmill ergometer after enrollment. Continuous electrocardiograms (ECGs) were digitally recorded at 500 Hz with a CardioSoft exercise ECG system (version 4.0; GE Healthcare, Boston, MA, USA) and analyzed fully automatically by the GE Healthcare version of the MMA method using an incremental update factor of 1/32. Using a modified Bruce protocol in the treadmill exercise test, the heart rate of patients could be smoothly increased to 90 to 120 beats/min and maintained for at least 3 min. The treadmill was suspended if VT, syncope, ST-segment depression >0.2 mV, or weakness occurred in patients. The TWA values were calculated continuously during the entire exercise test from rest to recovery using all chest leads (V1–V6). The maximal TWA value at heart rate <120 beats/min among all pre-cordial leads of each subject was derived and designated the MaxValt. The MTWA value was independently analyzed by two blinded experts.
Electrocardiographic characteristics
All patients underwent ECG at rest (25 mm/s, 10 mm/mV) with standard lead positions. The ECGs were independently analyzed by two blinded experienced doctors. Differences in electrocardiographic interpretation were adjudicated by a third experienced doctor, and a final conclusion was made by consensus. QRS duration, epsilon wave, T-wave inversions in inferior or pre-cordial leads, and T-wave inversions beyond leads V1 to V3 were measured according to current practice.
Electrophysiologic studies
All the enrolled patients participated in the EPS. The endpoints of the EPS were the induction of sustained VT or ventricular fibrillation (VF) or the lack of induction of any tachyarrhythmias. Intravenous isoproterenol (1–4 μg/min) was administered if sustained VT was not induced by the baseline EPS. Programmed stimulation consisting of up to three extra stimuli was performed at the right ventricular apex and right outflow tract by delivering current at twice the diastolic threshold. Coupling intervals were progressively shortened until a response was no longer elicited or to a minimum of 200 ms.
Follow-up
All patients received follow-up with electrocardiography, 24-h ambulatory electrocardiography, and ICD interrogation during clinical visits, which were scheduled every 3 to 6 months. The positive endpoint was the first occurrence of any of the following events: SCD, documented sustained VT, VF, or the administration of appropriate ICD therapy. SCD was defined as death within 1 h of the onset of symptoms or during sleep without any other identified cause. Appropriate ICD therapies were shock or anti-tachycardia pacing delivered for persistent ventricular tachyarrhythmia.
Statistical analyses
Categorical variables are expressed as frequencies (percentages). Continuous variables are expressed as the mean ± standard deviation (SD). Variables with skewed distributions are expressed as medians (interquartile range [IQR], range). Clinical characteristics were compared with the t test or Pearson Chi-squared test as appropriate. Univariate and multivariate Cox regression analyses were performed to analyze associations between follow-up events and clinical variables. The results of the event-free analyses are presented with hazard ratios (HRs) and 95% confidence intervals (CIs). Event-free survival curves were plotted according to the Kaplan-Meier method with statistical significance examined by the log-rank test. All statistical analyses were performed with SPSS statistical software (version 20.0; IBM Co., NY, USA). A P value <0.05 was considered statistically significant.
Results
Patient characteristics
The study population consisted of 35 patients with ARVC (mean age 38.6 ± 11.0 years; 28 males). The baseline characteristics are shown in Table 1. The echocardiography of all these patients showed the characteristic manifestations of RV abnormalities, such as wide RV outflow tract, local hypokinesia, local bulging, or local thinning [Table 2]. All patients had LV ejection fractions (LVEFs) >50%, and their heart function was better than the New York Heart Association (NYHA) II class.
Table 1.
Clinical characteristics of patients with and without clinical events at baseline.

Table 2.
Characteristic right ventricle echocardiographic manifestations in patients with arrhythmogenic right ventricular cardiomyopathy.

Among the 35 patients with ARVC, 28 had experienced sustained VT, four had syncope, and three had implanted ICD devices.
Analysis of MMA-TWA
All enrolled patients with ARVC successfully underwent the MWTA test with treadmill exercise. The MaxValt was 17.0 (11.0–27.0) μV in 35 patients. The MaxValt values were 25.0 (12.5–28.0) μV in 15 patients with positive events and 17.0 (9.25–19) μV in 20 patients without positive events.
Fifteen patients were using anti-arrhythmic drugs (AADs) when the MTWA test was performed, including seven patients using beta-blockers, five using sotalol, one using propafenone, one using a beta-blocker and propafenone, and one using a beta-blocker and amiodarone. The MaxValt of the 15 patients who used AADs was similar to that of the other 20 patients who did not use AADs (median: 16 vs. 17.5, P = 0.36).
Electrophysiologic studies
All 35 patients underwent EPSs. Among them, 22 patients had induced VT, with 13 exhibiting one type of induced monomorphic sustained VT, and nine exhibiting two or more types. Sixteen of 22 patients underwent ablation, with an acute success rate of 6/16.
Follow-up
During a median follow-up period of 99.9 ± 7.7 months, 15 patients had positive clinical events, including one SCD and 14 ventricular tachyarrhythmias. During the follow-up period, all 15 event-positive patients continued taking anti-arrhythmic drugs, two of them suffered syncope due to VT, and two ICD patients received shocks for fast VT/VF. Six patients underwent a second ablation for frequent sustained VT recurrence, and five more patients underwent implantation of ICDs during the follow-up period.
Predictors of clinical events
Compared with patients without positive events, patients with positive events had a higher proportion of male gender (15/15 vs. 13/20, P = 0.03) and a higher proportion of VT inducible by EPS (13/15 vs. 9/20, P = 0.02) [Table 1].
Survival analysis with the univariate Cox regression model indicated that inducible VT (HR, 5.23; 95% CI, 1.17–23.24; P = 0.02) and MaxValt (HR, 1.06; 95% CI, 1.00–1.12; P = 0.02) were risk factors for positive events. The multivariate Cox regression model for survival showed that inducible VT (HR, 5.98; 95% CI, 1.33–26.8; P = 0.01) and MaxValt (HR, 1.06; 95% CI, 1.01–1.11; P = 0.01) independently predicted positive clinical events [Table 3].
Table 3.
Cox regression analysis of variables and events in patients with arrhythmogenic right ventricular cardiomyopathy.

To evaluate the predictive power of MTWA and inducible VT for the occurrence of ventricular arrhythmias, the receiver operating characteristic (ROC) curve and the area under the curve (AUC) were used. When inducible VT was combined with MTWA, the AUC improved from 0.739 to 0.797 [Figure 1]. The ROC curve showed that a MaxValt of 23.5 μV was the optimal cutoff value to identify positive events. Patients with MaxValt values >23.5 μV had worse event-free survival according to the Kaplan-Meier analysis (log-rank P = 0.015) [Figure 2]. The Kaplan-Meier survival curve analysis of patients categorized by MaxValt and inducible VT showed that patients with both a MaxValt >23.5 μV and inducible VT had the worst prognosis (P = 0.002) [Figure 3]. The positive predictive value (PPV) was 85.71% (odds ratio [OR], 9; P = 0.027). In contrast, patients with a MaxValt ≤23.5 μV and non-inducible VT had the highest cumulative survival rate, with a negative predictive value (NPV) of 100% (P = 0.0015).
Figure 1.
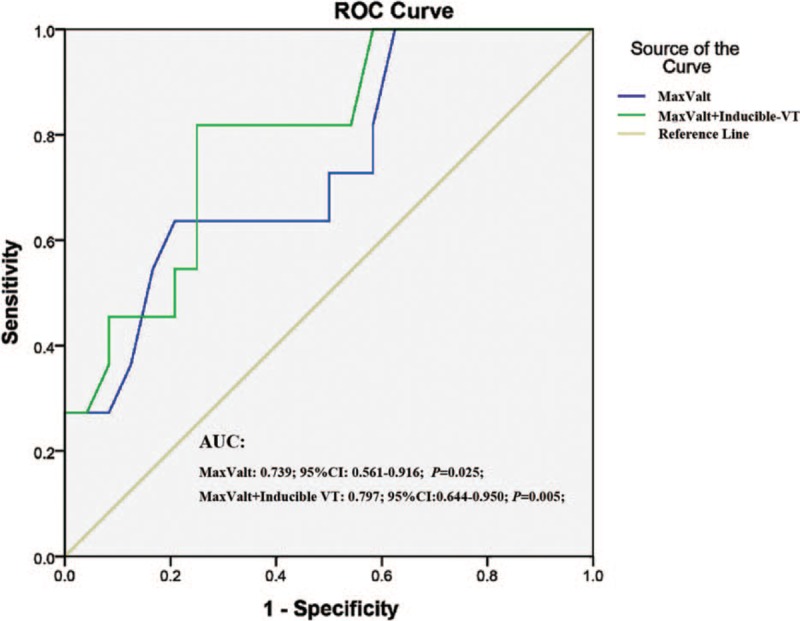
Receiver operating characteristic curve for MaxValt and MaxValt+inducible VT to predict positive events in patients with arrhythmogenic right ventricular cardiomyopathy. The area under the curve values were 0.739 and 0.797 for MaxValt and MaxValt+inducible VT, respectively. The MaxValt was obtained from the maximal value of TWA in any pre-cordial lead from V1 to V6. AUC: Area under the curve; MaxValt: Maximal TWA value; ROC: Receiver operating characteristic curve; TWA: T-wave alternans; VT: Ventricular tachycardia.
Figure 2.

Kaplan-Meier survival analyses of patients with arrhythmogenic right ventricular cardiomyopathy with a MaxValt >23.5 μV and a MaxValt ≤23.5 μV. At a cutoff value of MaxValt >23.5 μV, MTWA could predict ventricular tachyarrhythmia events in patients with ARVC. Patients with a MaxValt >23.5 μV had worse event-free survival than those with a MaxValt ≤23.5 μV. The MaxValt was obtained from the maximal value of TWA in any pre-cordial lead from V1 to V6. ARVC: Arrhythmogenic right ventricular cardiomyopathy; MaxValt: Maximal TWA value; MTWA: microvolt T-wave alternans; TWA: T-wave alternans.
Figure 3.

Kaplan-Meier survival analyses of patients with arrhythmogenic right ventricular cardiomyopathy categorized by MaxValt and inducible VT. Patients with both a MaxValt >23.5 μV and inducible VT had the worst prognosis; similarly, patients with a MaxValt ≤23.5 μV and non-inducible VT had the highest cumulative survival rate. The MaxValt was obtained from the maximal value of TWA in any pre-cordial lead from V1 to V6. MaxValt: Maximal TWA value; TWA: T-wave alternans.
Discussion
The major findings of this study were as follows: (1) MTWA measured using MMA analysis could have prognostic value in patients with ARVC with preserved LV function during long-term follow-up. (2) A MaxValt >23.5 μV and inducible VT independently predicted life-threatening ventricular tachyarrhythmias, appropriate ICD therapy and SCD in this cohort.
Exercise-induced MMA-TWA as a high-risk marker for cardiovascular events
Exercise, such as on a treadmill or bicycle, is one of the most important methods to increase the heart rate to the critical level needed to detect TWA.[13] The MTWA test using the spectral method and exercise can sometimes be affected by noise or artifacts. The MTWA test is improved when the MMA method is used.[14] Moreover, exercise-induced MTWA by the MMA method has been shown to be a marker of increased risk for cardiovascular events in patients with or without heart diseases. In the Finnish Cardiovascular Study (FINCAVAS),[15] the largest TWA study conducted to date, consecutive patients (n = 3598, 2164 males) underwent a clinically indicated exercise test with a bicycle ergometer, and their MMA-TWA was analyzed from the pre-cordial leads. The results demonstrated that the maximal TWA monitored from pre-cordial lead V5 was the strongest predictor of cardiovascular mortality and SCD, and higher TWA values indicated greater cardiovascular mortality and SCD risk.
Predictors of ventricular tachyarrhythmia and SCD in patients with ARVC
ARVC is a genetically determined disease that often pre-disposes patients to life-threatening ventricular tachyarrhythmias, which may occur as the first manifestation of the disease in young people without previous symptoms. The main goal of ARVC therapy is the prevention of SCD.
Previous studies showed that a number of clinical characteristics were associated with an increased risk of major arrhythmic events in patients with ARVC, such as male gender, proband status, cardiac arrest, syncope, LV dysfunction, inducible VT/VF, T-wave inversion in inferior or pre-cordial leads, T-wave inversions beyond right pre-cordial leads (V1–V3), and QRS fragmentation. However, these studies were based on smaller samples of patients who were followed for relatively short periods.
In the present study, we explored the predictive value of the previous indices of history of syncope and cardiac arrest, T-wave inversion in inferior or pre-cordial leads, T-wave inversion beyond leads V1 to V3, QRS duration, epsilon waves, inducible VT, and the new index, MTWA. Using Cox regression analysis, only the MaxValt and inducible VT could independently predict major tachyarrhythmic events. Patients with both a MaxValt >23.5 μV and inducible VT had the worst prognosis. The PPV was 85.71%. However, patients with a MaxValt ≤23.5 μV and non-inducible VT had the highest cumulative survival rate, with an NPV of 100%. Therefore, the MTWA test using MMA analysis in this cohort was more powerful for predicting prognosis than the previous indices.
Combined with other indices, such as heart rate turbulence or heart rate variability, the MMA-TWA test has been shown to be effective in identifying post-myocardial infarction patients at high risk of arrhythmic events. Furthermore, TWA testing could provide high NPVs for the primary endpoint of arrhythmia-free survival (appropriate ICD therapy, documented VT/VF, or all-cause mortality), as well as programmed ventricular stimulation.[16] Our present study has provided comparable outcomes.
Measurement and clinical implication of MMA-MTWA in patients with ARVC
The spectral and MMA methods are the only two techniques approved by the United States Food and Drug Administration to measure microvolt levels of TWA for risk stratification for arrhythmic death. Tests with TWA levels ≥1.9 μV and a signal-to-noise ratio of K = 3 sustained for 2 min are classified as positive in the spectral protocol. However, a high incidence (approximately 20–40%) of “indeterminate” test results often occurs due to many factors, such as excessive ectopy, HR <105 beats/min, unsustained MTWA, or noise.
As a promising time-domain analytical technique, MMA-TWA allows TWA analysis during routine exercise stress testing and 24-h ambulatory ECG monitoring without requiring special electrodes or a target heart rate. MMA-based TWA analyses on ambulatory ECG have been found to predict cardiovascular mortality and SCD in thousands of patients with coronary artery disease, myocardial infarction, heart failure, and ischemic and non-ischemic cardiomyopathy[17] with varying extents of LV dysfunction.[18] MMA-TWA has also been found to be elevated in ambulatory ECG recordings in other disease states associated with the risk of ventricular arrhythmias, including sleep apnea patients with congestive heart failure, epilepsy, chronic renal disease, hemodialysis, Brugada syndrome, and long QT syndrome.
In the ambulatory ECG-based TWA test, TWA ≥47 μV in standard pre-cordial leads is considered abnormal, and TWA ≥60 μV is considered severely abnormal.[19] These cutoff points are based on algorithms that used an update factor of 1/8.
However, MMA-TWA characteristics and cutoff values based on the exercise stress test in patients with ARVC have not been previously reported. In our previous study,[20] we found that TWA values in all pre-cordial leads and the MaxValt in patients with ARVC were much higher than those in healthy controls (MaxValt: 17.0 μV vs. 7 μV), using an update factor value of 1/32. In our present study, the cutoff value was proposed to be >23.5 μV, which was different from that suggested in the study by Chung et al.[7] Chung et al used the protocol of ambulatory ECG-based TWA and an update factor value of 1/8. Their study showed that compared with patients without tachyarrhythmic events, those with tachyarrhythmic events had higher TWA within the modified V5 and V1 channels. These channels suggested a cutoff value of >66 μV, which is approximately two times our cutoff value.
MTWA combined with EPS has a greater prognostic value in patients with ARVC
MTWA has been reported to be a strong independent predictor of spontaneous ventricular arrhythmias, death, and programmed ventricular stimulation. MTWA was shown to be better than signal-averaged electrocardiography for the risk stratification of patients with regard to life-threatening arrhythmias.[6] The Alternans Before Cardioverter Defibrillator study[21] (566 patients, median follow-up 1.9 years) was the first clinical trial to use MTWA measured with the spectral method with a graded exercise protocol to guide prophylactic ICD insertion in patients with ischemic cardiomyopathy and low LVEF. The results demonstrated that TWA testing appeared to be comparable to EPSs for guiding ICD implantation and that the two methods may be complementary, especially with a high NPV to identify the subset of patients least likely to benefit from ICD insertion. In our present study, we also combined MMA-TWA and EPS to predict the prognosis in patients with AVRC with preserved LVEF. Our results showed that MaxValt and inducible VT independently predicted life-threatening ventricular tachyarrhythmias. Furthermore, the NPV was 100% when MMA-TWA was combined with EPS in a long-term follow-up study.
Study limitations
Despite a follow-up period as long as 8 years, our study was limited by a small sample size affiliated with a single center. ICD implantation was limited in our recruited patients. Furthermore, in this study, we used an update factor of 1/32 when analyzing TWA, which was less sensitive than the recommended update factor of 1/8.[19] As a result, the TWA values obtained were substantially lower than expected, and the capacity to predict VT might also be reduced.
In conclusion, MTWA assessment using MMA analysis complemented with an EPS could improve the ability to predict the prognosis in patients with ARVC with preserved LV function during long-term follow-up.
Acknowledgements
The authors thank professor Zhao Yang of the Department of Biostatistics, School of Public Health, Nanjing Medical University, for his assistance in statistical analyses.
Funding
This work was supported by grants from the National Natural Science Foundation of China (No. 81470457) and the Frontier Technology of Jiangsu Provincial Science and Technology Department (No. BE2016764).
Conflicts of interest
None.
Footnotes
How to cite this article: Xue SL, Hou XF, Sun KY, Wang Y, Qian ZY, Wang QP, Shen SP, Yin HL, Zhang R, Yin HP, Zou JG. Microvolt T-wave alternans complemented with electrophysiologic study for prediction of ventricular tachyarrhythmias in patients with arrhythmogenic right ventricular cardiomyopathy: a long-term follow-up study. Chin Med J 2019;00:00–00. doi: 10.1097/CM9.0000000000000239
References
- 1.McKenna WJ, Thiene G, Nava A, Fontaliran F, Blomstrom-Lundqvist C, Fontaine G, et al. Diagnosis of arrhythmogenic right ventricular dysplasia/cardiomyopathy. Task Force of the Working Group Myocardial and Pericardial Disease of the European Society of Cardiology and of the Scientific Council on Cardiomyopathies of the International Society and Federation of Cardiology. Br Heart J 1994; 71:215–218. doi: 10.1136/hrt.71.3.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Corrado D, Basso C, Thiene G. Arrhythmogenic right ventricular cardiomyopathy: diagnosis, prognosis, and treatment. Heart 2000; 83:588–595. doi: 10.1136/heart.83.5.588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zorzi A, Rigato I, Bauce B, Pilichou K, Basso C, Thiene G, et al. Arrhythmogenic right ventricular cardiomyopathy: risk stratification and indications for defibrillator therapy. Curr Cardiol Rep 2016; 18:57.doi: 10.1007/s11886-016-0734-9. [DOI] [PubMed] [Google Scholar]
- 4.Corrado D, Wichter T, Link MS, Hauer RN, Marchlinski FE, Anastasakis A, et al. Treatment of arrhythmogenic right ventricular cardiomyopathy/dysplasia: an International Task Force Consensus Statement. Circulation 2015; 132:441–453. doi: 10.1161/CIRCULATIONAHA.115.017944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gehi AK, Stein RH, Metz LD, Gomes JA. Microvolt T-wave alternans for the risk stratification of ventricular tachyarrhythmic events: a meta-analysis. J Am Coll Cardiol 2005; 46:75–82. doi: 10.1016/j.jacc.2005.03.059. [DOI] [PubMed] [Google Scholar]
- 6.Gold MR, Bloomfield DM, Anderson KP, El-Sherif NE, Wilber DJ, Groh WJ, et al. A comparison of T-wave alternans, signal averaged electrocardiography and programmed ventricular stimulation for arrhythmia risk stratification. J Am Coll Cardiol 2000; 36:2247–2253. doi: 10.1016/S0735-1097(00)01017-2. [DOI] [PubMed] [Google Scholar]
- 7.Chung FP, Lin YJ, Chong E, Chang SL, Lo LW, Hu YF, et al. The application of ambulatory electrocardiographically-based t-wave alternans in patients with arrhythmogenic right ventricular dysplasia/cardiomyopathy. Can J Cardiol 2016; 32:1355.e15–1355.e22. doi: 10.1016/j.cjca.2016.01.035. [DOI] [PubMed] [Google Scholar]
- 8.Saguner AM, Medeiros-Domingo A, Schwyzer MA, On CJ, Haegeli LM, Wolber T, et al. Usefulness of inducible ventricular tachycardia to predict long-term adverse outcomes in arrhythmogenic right ventricular cardiomyopathy. Am J Cardiol 2013; 111:250–257. doi: 10.1016/j.amjcard.2012.09.025. [DOI] [PubMed] [Google Scholar]
- 9.Corrado D, Leoni L, Link MS, Della Bella P, Gaita F, Curnis A, et al. Implantable cardioverter-defibrillator therapy for prevention of sudden death in patients with arrhythmogenic right ventricular cardiomyopathy/dysplasia. Circulation 2003; 108:3084–3091. doi: 10.1161/01.CIR.0000103130.33451.D2. [DOI] [PubMed] [Google Scholar]
- 10.Corrado D, Calkins H, Link MS, Leoni L, Favale S, Bevilacqua M, et al. Prophylactic implantable defibrillator in patients with arrhythmogenic right ventricular cardiomyopathy/dysplasia and no prior ventricular fibrillation or sustained ventricular tachycardia. Circulation 2010; 122:1144–1152. doi: 10.1161/CIRCULATIONAHA.109.913871. [DOI] [PubMed] [Google Scholar]
- 11.Bhonsale A, James CA, Tichnell C, Murray B, Gagarin D, Philips B, et al. Incidence and predictors of implantable cardioverter-defibrillator therapy in patients with arrhythmogenic right ventricular dysplasia/cardiomyopathy undergoing implantable cardioverter-defibrillator implantation for primary prevention. J Am Coll Cardiol 2011; 58:1485–1496. doi: 10.1016/j.jacc.2011.06.043. [DOI] [PubMed] [Google Scholar]
- 12.Link MS, Laidlaw D, Polonsky B, Zareba W, McNitt S, Gear K, et al. Ventricular arrhythmias in the North American multidisciplinary study of ARVC: predictors, characteristics, and treatment. J Am Coll Cardiol 2014; 64:119–125. doi: 10.1016/j.jacc.2014.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Turitto G, Caref EB, El-Attar G, Helal M, Mohamed A, Pedalino RP, et al. Optimal target heart rate for exercise-induced T-wave alternans. Ann Noninvasive Electrocardiol 2001; 6:123–128. doi: 10.1111/j.1542-474X.2001.tb00096.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nearing BD, Verrier RL. Modified moving average analysis of T-wave alternans to predict ventricular fibrillation with high accuracy. J Appl Physiol 2002; 92:541–549. doi: 10.1152/japplphysiol.00592.2001. [DOI] [PubMed] [Google Scholar]
- 15.Leino J, Verrier RL, Minkkinen M, Lehtimaki T, Viik J, Lehtinen R, et al. Importance of regional specificity of T-wave alternans in assessing risk for cardiovascular mortality and sudden cardiac death during routine exercise testing. Heart Rhythm 2011; 8:385–390. doi: 10.1016/j.hrthm.2010.11.004. [DOI] [PubMed] [Google Scholar]
- 16.Narayan SM. Is T-wave alternans as good or better than programmed ventricular stimulation? Heart Rhythm 2007; 4:913–915. doi: 10.1016/j.hrthm.2007.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sakaki K, Ikeda T, Miwa Y, Miyakoshi M, Abe A, Tsukada T, et al. Time-domain T-wave alternans measured from Holter electrocardiograms predicts cardiac mortality in patients with left ventricular dysfunction: a prospective study. Heart Rhythm 2009; 6:332–337. doi: 10.1016/j.hrthm.2008.12.011. [DOI] [PubMed] [Google Scholar]
- 18.Verrier RL, Sroubek J. Quantitative T-wave alternans analysis for sudden cardiac death risk assessment and guiding therapy: answered and unanswered questions: For: Proceedings of ICE2015 Comandatuba, Brazil, Sudden Death Symposium. J Electrocardiol 2016; 49:429–438. doi: 10.1016/j.jelectrocard.2016.02.013. [DOI] [PubMed] [Google Scholar]
- 19.Verrier RL, Klingenheben T, Malik M, El-Sherif N, Exner DV, Hohnloser SH, et al. Microvolt T-wave alternans physiological basis, methods of measurement, and clinical utility–consensus guideline by International Society for Holter and Noninvasive Electrocardiology. J Am Coll Cardiol 2011; 58:1309–1324. doi: 10.1016/j.jacc.2011.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Xue SL, Hou XF, Xu DJ, Shan QJ, Chen ML, Chen C, et al. The features and clinical significance of microvolt T-wave alternans in patients with right ventricular tachycardia [in Chinese]. Chin J Cardiac Arrhyth 2009; 13:117–120. [Google Scholar]
- 21.Costantini O, Hohnloser SH, Kirk MM, Lerman BB, Baker JH, 2nd, Sethuraman B, et al. The ABCD (alternans before cardioverter defibrillator) trial: strategies using T-wave alternans to improve efficiency of sudden cardiac death prevention. J Am Coll Cardiol 2009; 53:471–479. doi: 10.1016/j.jacc.2008.08.077. [DOI] [PubMed] [Google Scholar]


