ABSTRACT
To establish the profile of patients who developed antiangiogenic agent-related osteonecrosis of the jaws, and identify the treatments currently used in dental management. We searched the PubMed®/Medline® and Scopus databases using the words “osteonecrosis AND antiangiogenic therapy”, with the following inclusion criteria: articles published in English, case reports, available online, and for an unlimited period. Of the 209 articles retrieved, 18 were selected, for a total of 19 case reports, since one article included two cases that met the inclusion criteria for this study. Medication-related osteonecrosis of the jaws is characterized by exposure of necrotic bone in the oral cavity that does not heal over a period of 8 weeks in patients with no previous history of radiation therapy. Antiangiogenic drugs are indicated in the treatment of certain tumors, since they stop the formation of new blood vessels, controlling tumor growth and the chance of metastasis. Dental prevention is essential in patients who will be put on antiangiogenic agents, to minimize the risk for osteonecrosis.
Keywords: Osteonecrosis, Dental care, Metastatic neoplasm, Angiogenesis inhibitors, Antineoplastic agents
RESUMO
Traçar o perfil dos pacientes que desenvolveram osteonecrose dos maxilares associada a agentes antiangiogênicos e identificar os tratamentos realizados atualmente no manejo odontológico. Foi realizada busca nas bases de dados PubMed®/Medline® e Scopus por meio dos descritores “osteonecrosis AND antiangiogenic therapy”, sendo utilizados os critérios de inclusão: artigos publicados em inglês, relato de caso, disponíveis on-line e por período ilimitado. Após análise dos 209 artigos encontrados, foram selecionados 18 artigos para este estudo, resultando em 19 relatos de caso, visto que um dos artigos apresentou dois casos que se enquadravam nos critérios de inclusão. A osteonecrose dos maxilares associada a medicamentos é caracterizada pela exposição de osso necrótico na cavidade oral que não cicatriza em um período de 8 semanas em pacientes que não foram submetidos à radioterapia. Os medicamentos antiangiogênicos são indicados no tratamento de alguns tumores, pois impedem o crescimento de novos vasos sanguíneos, controlando o crescimento do tumor e a chance de metastização. Torna-se imprescindível a realização de prevenção odontológica do paciente a ser submetido a uso de antiangiogênicos visando a minimizar as chances de desenvolvimento da osteonecrose.
Descritores: Osteonecrose, Assistência odontológica, Metástase neoplásica, Inibidores da angiogênese, Antineoplásicos
INTRODUCTION
Medication-related osteonecrosis of the jaws (MRONJ) is characterized by exposure of necrotic bone in the oral cavity that does not heal over a period of 8 weeks, in patients with no previous history of radiotherapy. According to the American Association of Oral and Maxillofacial Surgeons (AAOMS), to be diagnosed with MRONJ, patients must meet some criteria, such as previous/current treatment with bisphosphonates, antiresorptive or antiangiogenic agents.( 1 – 7 )
Angiogenesis is the formation of blood vessels, allowing for tumor growth and invasion of these vessels, which facilitates metastases.( 7 ) Antiangiogenic agents are indicated in the treatment of diseases that depend on vascular neoformation to grow and metastasize.( 7 ) The antiangiogenic agent-related osteonecrosis of the jaws (AARONJ) occurs due to an interference in the natural angiogenesis inherent to bone repair, leading to reduced blood supply to the jaws, and bacterial contamination of the exposed bone.( 1 , 2 , 4 , 5 , 7 , 8 )
Antiangiogenic agent-related osteonecrosis of the jaws is a relatively new complication, since these drugs are only now being used on a large scale.( 7 ) Therefore, we are still waiting for longitudinal studies aiming to investigate the main dental risk factors specific to this class of drugs.
OBJECTIVE
To establish the profile of patients with antiangiogenic agent-related osteonecrosis of the jaws, and identify the main risk factors through an integrative review.
METHODS
We searched the PubMed®/Medline® and Scopus databases using the words “osteonecrosis AND antiangiogenic therapy”. The inclusion criteria were articles published in English, case reports and/or case series, available online, and for an unlimited period. The exclusion criteria were patients treated with bisphosphonates and/or antiresorptive agents, patients irradiated in the region affected by osteonecrosis, osteonecrosis not involving the jaws, and animal studies.
RESULTS
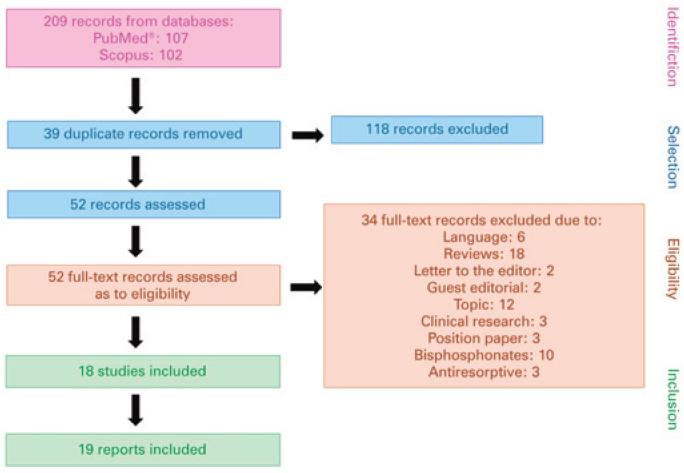
We found 209 articles in the databases, and selected 18 for our final sample, with a total of 19 case reports, since one of the papers included two cases that met our inclusion criteria.
Figure 1 shows a flow chart with results from the articles found. Data obtained from the selected publications are presented in tables 1 and 2, organized by chronological order.
Figure 1. Flow chart of articles found in PubMed® and Scopus databases.
Table 1. Diagnostic features of antiangiogenic agent-related osteonecrosis of the jaws, types of antiangiogenic agents, and their mechanism of action in the articles selected.
| Article (country) | Sex, age | Location | Signs and symptoms | Imaging findings | Histological features | Drug/dose |
|---|---|---|---|---|---|---|
| Estilo et al.( 1 ) (United States) Case 1 | Female, 51 | Left mandible (lingual) | EB (1x1mm), normal ST, no evidence of infection, discomfort | NR | Devitalized bone, bacteria (Actinomyces) and inflammatory cells | Bevacizumab (inhibitor -VEGF), 15mg/kg, 3 weeks, total of 8 doses |
| Dişel et al.( 2 ) (Turkey) | Male, 51 | Right mandible | EB (3×3mm), ulcerated and necrotic ST, no evidence of infection, fistula and abscess, pain, difficulty masticating | PR and CT: sclerotic bone lesion | Osteonecrosis, bacteria (Actinomyces) | Bevacizumab (inhibitor -VEGF) 5mg/kg, 6 cycles/2 weeks |
| Brunamoti Binello et al.( 3 ) (Italy) | Male, 47 | Left mandible (lingual) | EB, edema with moderate mucosal exudate, trismus, pain, left-sided lower lip paresthesia | PR: no significant findings; CT: bone loss; BS: increased uptake | NR | Bevacizumab (inhibitor -VEGF),15mg/kg/ 6 months/8 doses |
| Erovigni et al.( 4 ) (Italy) Case 1 | Male, 79 | Left mandible (mylohyoid line) | EB (3×1m), ulcerated and necrotic ST, fistula, asymptomatic | CBCT: sclerotic lesion in the cortical bone, and alveolar residue with no sequestration images | NR | Bevacizumab (inhibitor-VEGF), dose NR |
| Erovigni et al.( 4 ) (Italy) Case 2 | Male, 60 | Left mandible (lingual) | EB (1cm), pain and gingival lesion | PR: no signs of osteolysis, only the alveolar profile; CT: 7mmx4mm cortical bone lesion | NR | Bevacizumab (inhibitor -VEGF), 5mg/kg/day/14 days (8 cycles/4 months) |
| Ponzetti et al.( 5 ) (Italy) | Female, 64 | Right mandible | Non-traumatic avulsion of two teeth with purulent secretion, symptoms NR | PR and CT: multiple foci of osteonecrosis of the jaws | NR | Aflibercept (inhibitor -VEGF), dose NR |
| Jung( 6 ) (Korea) | Female, 62 | Right and left mandible | EB around implants on the right and left sides, with pus drainage, gingival bleeding and edema, pain | PR and CT: fracture lines/bone sequestration in both regions; BS: bilateral uptake compatible with osteomyelitis | Acute osteomyelitis | Pazopanib (TKi), 6 months |
| Pakosch et al.( 8 ) (Germany) | Female, 53 | Left mandible (lingual) | EB (15×3 mm), fistula due to B and L, inflamed and ulcerated ST, abscess, pain and edema | PR and CBCT: osteolysis with two punctiform radiodense areas, due to foreign bodies, ST emphysema, fragmented cancellous bone, opacity of the right maxillary sinus | Chronic osteomyelitis with bone marrow fibrosis and necrotic bone | Bevacizumab (inhibitor -VEGF) and sorafenib (MKi), dose NR |
| Greuter et al.( 9 ) (Switzerland) | Female, 63 | Left maxilla | Fistula, pain, trigeminal neuralgia | PR and CT: sinusitis and osteonecrosis | Osteonecrosis | Bevacizumab (inhibitor -VEGF), dose NR |
| Serra et al.( 10 ) (Italy) | Male, 64 | Left mandible | EB in the alveolar region, pain | PR and CT: area of bone necrosis | Necrotic bone, bacteria and inflammatory cells | Bevacizumab (inhibitor -VEGF), 7.5mg/kg, 8g |
| Koch et al.( 11 ) (Sweden) | Male, 59 | Left mandible | EB (10mm), normal ST, pain | DVT: area of hypodense bone with no sequestration | Necrotic bone, bacteria (Actinomyces) | Sorafenib (TKi), sunitinib (TKi) 50mg/day |
| Bettini et al.( 12 ) (Italy) | Female, 57 | Left mandible | EB (6x3cm) reaching basal bone; severe periodontal disease, periodontal abscess in the right posterior region, pain and halitosis | BS: focal and persistent uptake suggestive of bone infection. CT: bone sequestration | Osteonecrosis, inflammatory infiltrate and few blood vessels | Bevacizumab (inhibitor -VEGF), 945mg IV/21 days |
| Nicolatou-Galitis et al.( 13 ) (Greece) Case 2 | Female, 64 | Left mandible (lingual) | EB, inflamed ST, superior central incisors present with periodontal disease, pain | PR: no obvious radiological changes or bone disease | NR | Sunitinib (TKi), 50mg/day |
| Hopp et al.( 14 ) (Brazil) | Male, 58 | Left mandible (lingual) | EB (5x5mm), normal ST, regional teeth with no pulp/periodontal abnormalities, pain | EX: absence of periapical/periodontal problems | Necrotic bone and bacteria | Bevacizumab (inhibitor -VEGF), 2.5mg (intravitreal) |
| Fleissig et al.( 15 ) (Israel) | Male, 58 | Right mandible | EB (small area), inflamed ST, limited pus drainage, enlarged submandibular lymph nodes; pain and limited mouth opening | PR: incomplete bone remodeling in the alveolar region; CT: irregular alveolar cortical margin at 38 | Necrotic bone and bacteria | Sunitinib (TKi), 50mg, once a day/4 consecutive weeks followed by 2 weeks off drugs |
| Magremanne et al.( 16 ) (Belgium) | Male, 49 | Left mandible | EB from the angle to the midline of the mandible, submandibular edema reaching the clavicle, partial necrosis of the mental nerve and facial artery, pain | PR: absence of periapical/periodontal lesions; CT: infiltration; ST, no evidence of necrosis | Necrotic tissues, inflammatory infiltrate, hemorrhagic necrosis and local thrombosis | Bevacizumab inhibitor -VEGF), 10mg/kg, single dose |
| Santos-Silva et al.( 17 ) (Brazil) | Male, 61 | Left mandible (lingual) | EB (1x1cm), normal ST, pain | PR: area of destroyed bone with discontinuity of the external oblique line; CT: lesion-associated loss of integrity and erosion of the underlying cortical bone | NR | Bevacizumab(inhibitor -VEGF) IV (10mg/kg every other week) |
| Marino et al.( 18 ) (Italy) | Female, 51 | Left mandible | Inflammation, infection with pus drainage, asymptomatic | PR: incomplete bone remodeling; CT: cortical irregularity and sclerotic reaction | Atypical bone necrosis | Cabozantinib (TKi), 175mg/day |
| Garuti et al.( 19 ) (Italy) | Male, 74 | Right mandible (body region) | EB with no infection/sequestration, gingival lesion | CBCT: lytic area in the contralateral mandibular body (right side), at the site of prior tooth extraction (October 2014) | NR | Sorafenib (TKi), 400mg/day |
EB: exposed bone; ST: soft tissue; NR: not reported; VEGF: vascular endothelial growth factor; PR: panoramic radiograph; CT: computed tomography; BS: bone scintigraphy; CBCT: cone beam CT scan; TKi: tyrosine kinase inhibitor; B: buccal; L: lingual; MKi: multikinase inhibitor; DVT: digital volume tomography; IV: intravenous; EX: unspecified radiographic examination.
Table 2. Local and systemic factors, and management of antiangiogenic agent-related osteonecrosis of the jaw.
| Article (country) | Time to lesion onset | Underlying disease | Triggering factor | Treatment | Associated treatments | Comorbidities | Outcome |
|---|---|---|---|---|---|---|---|
| Estilo et al.( 1 ) (United States) Case 1 | 1 week | Breast cancer, ST metastasis | Spontaneous | EB smoothing, 0.12% CLXMW, discontinuation of bevacizumab and capecitabine | Doxorubicin, cyclophosphamide, letrozole, paclitaxel, chest X-ray and capecitabine | NR | A few weeks later: CH |
| Disel et al.( 2 ) (Turkey) | 2 weeks | Sigmoid colon cancer, metastasis | Spontaneous | Curettage and dressing | Fluorouracil, leucovorin and oxaliplatin | NR | NR |
| Brunamonti Binello et al.( 3 ) (Italy) | 10 months | Cancer of the parotid gland, bone metastasis | Eruption | EB removal, antibiotic therapy (amoxicillin + clavulanate) | Epirubicin, cisplatin | NR | Death |
| Erovigni et al.( 4 ) (Italy) Case 1 | 3 years | Colon cancer, lung metastasis | Tooth extraction | LPLT, antibiotic therapy (amoxicillin + clavulanate and meropenem) and 0.2% CLXMW | Capecitabine, oxaliplatin, leucovorin, oxaliplatin, RT in the lung region, mitomycin and bisphosphonates (after BRONJ) | HTN and prostatic hyperplasia | 6 months later: CH |
| Erovigni et al.( 4 ) (Italy) Case 2 | 8 months | Renal cancer, lung and brain metastases | Tooth extraction | Antibiotic therapy (amoxicillin + clavulanate and meropenem) and 0.12% CLXMW | Leucovorin, oxaliplatin and pelvic RT | NR | Death |
| Ponzetti et al.( 5 ) (Italy) | After cycle 11 | Colon cancer, liver metastasis | Atraumatic avulsion of 2 teeth | LPLT and discontinuation of chemotherapy | Cetuximab, capecitabine, oxaliplatin, raltitrexed and leucovorin | HTN and chronic periodontitis | Death |
| Jung( 6 ) (Korea) | 7 weeks | Kidney cancer | NR | Removal of implants and bone sequestration, placement of a fixation plate, antibiotic therapy (3rd generation cefalexin), discontinuation of everolimus (treatment with pazopanib had already finished) | Everolimus | NR | Interrupted follow-up |
| Pakosch et al.( 8 ) (Germany) | During the 3-month treatment | Pancreatic cancer | Abscess | Removal of EB, abscess drainage, antibiotic therapy (amoxicillin + clavulanate), chemotherapy discontinuation, 0.12% CLXMW. NGT to prevent trauma | Gemcitabine, erlotinib, folinic acid, 5-FU, oxaliplatin and paclitaxel | NR | 2 months later: CH |
| Greuter et al.( 9 ) (Switzerland) | 1 month | Breast cancer | Tooth extraction | Removal of EB, maxillary sinus drainage | Liposomal doxorubicin | NR | 3 weeks later: CH |
| Serra et al.( 10 ) (Italy) | 1 week | Lung cancer, bone metastasis | Tooth extraction | Removal of EB, antibiotic therapy (amoxicillin + clavulanate), 0.2% CLXMW | Cisplatin and gemcitabine | NR | 2 weeks later: initiated treatment with zoledronic acid. PH |
| Koch et al.( 11 ) (Sweden) | 1.5 year | Kidney cancer, ST metastasis | Tooth extraction | Removal of EB | Interferon, viblastin, ramipril, HCT, metoprolol and hyroxin | HTN and hyperthyroidism | Healing |
| Bettini et al.( 12 ) Italy | 1 month | Lung cancer, lymph node metastasis | Atraumatic avulsion of 2 teeth | Removal of implants, antibiotic therapy (amoxicillin + clavulanate, lincomycin) | Gemcitabine, cisplatin and corticosteroids | No comorbidities | 2 weeks later: healing |
| Nicolatou-Galitis et al.( 13 ) (Greece) Case 2 | 4 years | Kidney cancer, lung metastasis | Potential trauma of the inferior dental implant | Antibiotic therapy: amoxicillin, CLXMW, discontinuation of sunitinib | Prednisolone | Hypothyroidism and cutaneous vasculitis | 3 months later: CH |
| Hopp et al.( 14 ) (Brazil) | 2 years | Retinal vein thrombosis | Spontaneous | Bone curettage, antibiotic therapy (clindamycin), 0.12% CLXMW | NR | HTN, gout and retinal vein thrombosis | 3 weeks later: CH |
| Fleissig et al.( 15 ) (Israel) | 6 months | Kidney cancer | Tooth extraction | Antibiotic therapy: (amoxicillin + clavulanate) temporary discontinuation of sunitinib | NR | Hypothyroidism and osteoporosis | 6 weeks later: PH |
| Magremanne et al.( 16 ) (Belgium) | 2 weeks | Glioblastoma | Tooth extraction | Antibiotic therapy (clindamycin, meropenem), CLXMW, ST debridement, facial artery ligation; dressing: gauze with povidone. Use of NET for feeding | Temozolomide, RT and corticosteroids | NR | 4 weeks later: CH |
| Santos-Silva et al.( 17 ) (Brazil) | 55 weeks | Kidney cancer, lymph node metastasis | Spontaneous | Temporary discontinuation of bevacizumab and tensirolimus, 0.12% CLXMW | Tensirolimus IV (25 mg/week) | HTN | 3 months later: CH |
| Marino et al.( 18 ) (Italy) | 3 months | Thyroid cancer, liver metastasis | Tooth extraction | Segmental ostectomy, debridement, antibiotic therapy, 0.2% CLXMW. | 5-FU, dacarbazine, RT, levothyroxine, calcitriol, vitamin D3, duloxetine propranolol, lansoprazol and loperamide | NR | 4-year control: CH |
| Garuti et al.( 19 ) (Italy) | 1 month | Liver cancer, recurrence | Tooth extraction | Discontinuation of sorafenib | Furosemide, potassium canrenoate, bisoprolol, allopurinol, tamsulosin, hydroxychloroquine, vitamin D and sertraline | Hepatitis C and aortic artery stenosis | Death |
ST: soft tissue; EB: exposed bone; CLXMW: chlorhexidine mouthwash; RT: radiation therapy; NR: not reported; CH: complete healing; LPLT: low-power laser therapy; BRONJ: biphosphonate-related osteonecrosis of the jaws; HTN: hypertension; NGT: nasogastric tube; 5-FU: irinotecan; HCT: hydrochlorothiazide; PH: partial healing; IV: intravenously; NET: nasoenteral tube.
DISCUSSION
Medication-related osteonecrosis of the jaws is an uncommon disease that can result in significantly reduced quality of life, and requires all of the following features: current or previous treatment with antiresorptive or antiangiogenic agents; exposed bone or bone that can be probed through an intra- or extraoral fistula in the maxillofacial region, persisting for more than 8 weeks; no history of radiotherapy in the affected bones or evidence of metastatic disease in the region.( 7 )
Historically, the first drugs associated with the condition were bisphosphonates, which led to coining of the term “biphosphonate-related osteonecrosis of the jaws” (BRONJ). However, there was a need to include other drugs in the etiopathogeny of osteonecrosis, such as other antiresorptive and antiangiogenic agents. The cases reported of antiangiogenic agent-related osteonecrosis have been accumulating over the years and, therefore, the most appropriate term for the condition is AARONJ.( 2 , 7 , 20 )
Medication-related osteonecrosis of the jaws was first reported by Marx, in 2003,( 21 ) and, although it has been studied for nearly two decades now, the pathophysiology of the condition has not been fully clarified. The processes of inhibition of bone resorption and osteoclastic remodeling, inflammation and infection, and inhibition of angiogenesis are the most widely accepted hypotheses.( 7 , 20 , 22 )
Angiogenesis allows for growth and formation of new blood vessels, which are critical to disease progression, particularly in cancer. This step is mediated by chemical signallings in the body, and the vascular endothelial growth factor (VEGF) is the most relevant in this process. This signalling binds to receptors on endothelial cells that line the internal wall of blood vessels, stimulating angiogenesis and affecting the balance of bone neoformation.( 7 , 23 , 24 )
The mechanism of action of antiangiogenic agents is, in simple terms, blocking the direct or indirect action of VEGF. Some drugs act by preventing VEGF from binding onto endothelial cells, such as bevacizumab, which is considered a monoclonal antibody. Sunitinib, another antiangiogenic agent, acts endogenously, preventing VEGF receptors from sending signallings to endothelial cells, and therefore is known as a tyrosine-kinase inhibitor.( 24 , 25 )
In this review, we observed that antiangiogenic agents were prescribed for metastatic cancer in 63.2% (n=12) of cases,( 1 – 5 , 10 – 13 , 17 , 18 ) whereas kidney cancer was the most prevalent diagnosis (n=6; 31.6%),( 4 , 6 , 11 , 13 , 15 , 17 ) followed by colon cancer, with 15.8% (n=3).( 2 , 4 , 5 ) Antiangiogenic agent-related osteonecrosis of the jaws was also described in a non-cancer case of retinal vein thrombosis.( 14 )
The most commonly found antiangiogenic agent was bevacizumab, in 58% of cases (n=11),( 1 – 4 , 9 , 10 , 12 , 14 , 16 , 17 ) followed by sunitinib, in 11% (n=2),( 13 , 15 ) and the other 31% used aflibercept (n=1),( 5 ) sorafenib (n=1),( 20 ) cabozantinib (n=1),( 18 ) pazopanib (n=1),( 6 ) sorafenib + sunitinib (n=1),( 11 ) and bevacizumab + sorafenib (n=1).( 8 )
In the selected articles, most were published in Italy,( 3 – 6 , 10 , 12 , 18 , 19 ) i.e, 39% (n=7), followed by Brazil,( 14 , 17 ) with 11% (n=2), and the United States( 1 ) (n=1), Sweden( 11 ) (n=1), Turkey( 2 ) (n=1), Greece( 13 ) (n=1), Israel( 15 ) (n=1), Belgium( 16 ) (n=1), Germany( 8 ) (n=1), Korea( 6 ) (n=1), and Switzerland( 9 ) (n=1), accounting altogether for 50% (n=9) of articles. Based on this evidence, there is no effect of geographies or economies on patients affected by AARONJ.
The mean age of patients with AARONJ was 59.7 years, and the median, 60 years, with minimum age of 47 years( 3 ) and maximum age of 79 years.( 4 ) In respect to sex, 11 patients were male (58%)( 2 – 4 , 10 , 14 – 17 , 19 ) and 8 were female (42%);( 1 , 5 , 6 , 8 , 9 , 12 , 13 , 16 , 18 ) different from what the AAOMS reported in 2014.( 7 ) The race of patients was not described in the articles and, therefore, was excluded from the final result table.
The most affected region was the mandible (95% of cases), and the left side was involved in 69% of individuals (n=13),( 1 , 3 , 4 , 8 , 10 – 14 , 16 – 18 ) the right side in 21% (n=4),( 2 , 5 , 15 , 19 ) and both sides simultaneously in 5%.( 6 ) The left maxillary sinus was reported in 5% of cases.( 9 ) This predilection for the mandibular region is explained by it being formed by compacted bone, which means less blood supply within its structure when compared with the maxilla,( 4 , 7 , 8 ) and it also has portions of thinner mucosa lining bony protuberances, such as the mylohyoid line.( 4 , 8 )
The most frequent clinical signs were bone exposure in 84.2% of cases (n=16),( 1 – 4 , 6 , 8 , 10 – 17 , 19 ) followed by: suppuration (n=4)( 5 , 6 , 15 , 18 ) and inflamed soft tissue (n=4)( 8 , 13 , 15 , 18 ) (21% each), fistula (n=3)( 4 , 8 , 9 ) and ulcer (n=3),( 2 , 4 , 8 ) (15.8% each), soft tissue necrosis (n=2),( 2 , 4 ) abscess (n=2),( 8 , 12 ) periodontal disease (n=2)( 12 , 13 ) (10.5% each) and atraumatic avulsion (n=1),( 5 ) trismus (n=1),( 10 ) and enlarged lymph nodes (n=1)( 11 ) and nerve necrosis (n=1)( 16 ) (5.3% each). The most frequently found symptoms were pain in 73.7% of cases (n=14),( 2 – 4 , 6 , 8 – 17 ) followed by edema (n=4),( 3 , 6 , 8 , 16 ) in 21%, gingival lesion (n=2)( 4 , 19 ) and asymptomatic patients (n=2)( 4 , 18 ) (10.5% each). Other symptoms reported included discomfort (n=1),( 1 ) difficulty masticating (n=1),( 2 ) halitosis (n=1),( 1 ) lower lip paresthesia (n=1),( 3 ) limited mouth opening (n=1),( 15 ) gingival bleeding (n=1),( 6 ) pus drainage (n=1)( 6 ) and neuralgia (n=1)( 9 ) − each representing 5.3% of sample. One of the articles did not report the signs and symptoms found.( 5 )
The most frequently requested supplemental diagnostic tests were panoramic radiographs,( 2 – 6 , 9 – 18 ) CT scans( 2 – 6 , 8 – 12 , 15 – 19 ) and bone scintigraphy.( 3 , 6 ) The panoramic radiographs and CT scans showed that, in early cases, there were no obvious changes on the images;( 13 , 14 ) however, as the condition progresses, it is possible to visualize areas of rarefaction/hypodense bone, bone sequestration, and cortical bone rupture,( 2 – 6 , 8 – 12 , 15 – 19 ) and, on scintigraphy images, in the regions of osteonecrosis, increased contrast uptake can be seen.( 3 , 6 ) One of the articles did not describe the imaging modality used.( 1 )
The time to lesion onset varies with the type, dose and duration of antiangiogenic agent use - and the longer the duration of the therapy and the older the patient, the greater the chance of AARONJ.( 4 , 7 , 12 , 16 ) The shortest time to lesion onset was 1 week( 1 ) and the longest, 4 years.( 13 )
The major risk factors for onset of AARONJ were invasive dental procedures with manipulation of bone tissue, such as tooth extractions and periapical/periodontal surgery, in addition to local trauma, periodontal disease, and periapical infection, among others.( 1 – 5 , 7 , 10 – 19 ) Antiangiogenic agent-related osteonecrosis of the jaws can also develop spontaneously.( 7 , 10 , 16 , 17 ) In consonance with what the literature describes, the main risk/triggering factors found were tooth extractions, in 50% of cases (n=9),( 4 , 9 – 11 , 15 , 16 , 18 , 19 ) atraumatic avulsion in 11.1% of cases (n=2);( 5 , 12 ) and trauma (n=1),( 13 ) eruption (n=1)( 3 ) and abscess (n=1)( 8 ) in 15.8%. Antiangiogenic agent-related osteonecrosis of the jaws developed spontaneously in 22.2% of cases (n=4).( 1 , 2 , 14 , 17 ) In one of the articles, the triggering factor was not reported.( 6 )
Antiangiogenic agent-related osteonecrosis of the jaws cases must be managed according to the AAOMS recommendations,( 7 ) i.e., taking staging into account. In this review, we found that the most commonly used treatments were antibiotic therapy in 63.2% of cases (n=12),( 3 , 4 , 6 , 8 , 10 , 12 – 16 , 18 ) antimicrobial mouth wash in 52.6% (n=10),( 1 , 4 , 8 , 9 , 13 , 14 , 16 – 18 ) discontinuation of antiangiogenic therapy in 42.1% (n=8),( 1 , 5 , 6 , 8 , 13 , 15 , 19 ) removal of exposed bone in 42.1% (n=8),( 1 , 3 , 8 – 11 , 14 , 18 ) followed by soft tissue debridement (n=2),( 16 , 18 ) dressings (n=2),( 2 , 16 ) laser therapy (n=2),( 4 , 5 ) and nasogastric tube to stop oral intake (n=2),( 8 , 16 ) representing 10.5% each. Curettage (n=1),( 2 ) removal of complete dentures (n=1),( 12 ) abscess drainage (n=1),( 8 ) maxillary sinus drainage (n=1)( 9 ) and removal of implants (n=1)( 6 ) accounted for 26.3% of the remaining cases. In earlier stages, treatment can be more conservative, however for more severe cases, surgical intervention is required, aiming to stabilize AARONJ.( 7 , 15 , 17 )
Some authors believe that predisposing factors can increase the risk of onset of AARONJ, such as smoking and diabetes,( 5 , 7 , 11 , 12 ) alcohol use,( 5 ) and anemia, among others. According to the AAOMS, standardized studies, with concrete evidence, must be conducted to prove the influence of other comorbidities and/or predisposing factors in the onset of AARONJ.( 7 )
In two case reports,( 1 , 18 ) patients were subjected to radiation therapy, but in a region other than that affected by AARONJ, and were, therefore, included in this review. In one case report,( 10 ) the patient was currently on treatment for AARONJ and initiated therapy with zoledronic acid. Because AARONJ was diagnosed before treatment with bisphosphonates, the case report was included for analysis.
The outcomes of the cases reported in this review show that, after the treatments used, AARONJ may remain stable, i.e. with no infection, no symptoms and no progression; however, it does not completely disappear.( 7 ) The time to AARONJ stability varies based on the patient's age, the stage of evolution, and duration of use of antiangiogenic agent.( 7 , 12 )
CONCLUSION
It is extremely important that patients scheduled to initiate treatment with antiangiogenic agents previously undergo a rigorous dental evaluation aiming to clear the oral cavity, avoiding infections and the need for invasive procedures, and thus preventing osteonecrosis of the jaws.
REFERENCES
- 1.Estilo CL, Fornier M, Farooki A, Carlson D, Bohle G, 3rd, Huryn JM. Osteonecrosis of the jaw related to bevacizumab. J Clin Oncol. 2008;26(24):4037–4038. doi: 10.1200/JCO.2007.15.5424. [DOI] [PubMed] [Google Scholar]
- 2.Dişel U, Beşen AA, Özyılkan Ö, Er E, Canpolat T. A case report of bevacizumab-related osteonecrosis of the jaw: old problem, new culprit. Oral Oncol. 2012;48(2):e2–e3. doi: 10.1016/j.oraloncology.2011.07.030. [DOI] [PubMed] [Google Scholar]
- 3.Brunamonti Binello P, Bandelloni R, Labanca M, Buffoli B, Rezzani R, Rodella LF. Osteonecrosis of the jaws and bevacizumab therapy: a case report. Int J Immunopathol Pharmacol. 2012;25(3):789–791. doi: 10.1177/039463201202500328. [DOI] [PubMed] [Google Scholar]
- 4.Erovigni F, Gambino A, Cabras M, Fasciolo A, Bianchi SD, Bellini E, et al. Delayed Diagnosis of Osteonecrosis of the Jaw (ONJ) Associated with Bevacizumab Therapy in Colorectal Cancer Patients: Report of Two Cases. Dent J (Basel) 2016;4(4):E39. doi: 10.3390/dj4040039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ponzetti A, Pinta F, Spadi R, Mecca C, Fanchini L, Zanini M, et al. Jaw osteonecrosis associated with aflibercept, irinotecan and fluorouracil: attention to oral district. Tumori. 2016;102(Suppl 2):S74–S77. doi: 10.5301/tj.5000405. Review. [DOI] [PubMed] [Google Scholar]
- 6.Jung TY. Osteonecrosis of jaw after antiangiogenic agent administration in a renal cell carcinoma patient. Oral and Maxillofacial Surgery Cases. 2017;3(2):27–33. [Google Scholar]
- 7.Ruggiero SL, Dodson TB, Fantasia J, Goodday R, Aghaloo T, Mehrotra B, et al. American Association of Oral and Maxillofacial Surgeons position paper on medication-related osteonecrosis of the jaw - 2014 update. J Oral Maxillofac Surg. 2014;72(10):1938–1956. doi: 10.1016/j.joms.2014.04.031. Erratum in: J Oral Maxillofac Surg. 2015;73(9):1879. Erratum in: J Oral Maxillofac Surg. 2015;73(7):1440. [DOI] [PubMed] [Google Scholar]
- 8.Pakosch D, Papadimas D, Munding J, Kawa D, Kriwalsky MS. Osteonecrosis of the mandible due to anti-angiogenic agent, bevacizumab. Oral Maxillofac Surg. 2013;17(4):303–306. doi: 10.1007/s10006-012-0379-9. [DOI] [PubMed] [Google Scholar]
- 9.Greuter S, Schmid F, Ruhstaller T, Thuerlimann B. Bevacizumab-associated osteonecrosis of the jaw. Ann Oncol. 2008;19(12):2091–2092. doi: 10.1093/annonc/mdn653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Serra E, Paolantonio M, Spoto G, Mastrangelo F, Tete S, Dolci M. Bevacizumab-related osteneocrosis of the jaw. Int J Immunopathol Pharmacol. 2009;22(4):1121–1123. doi: 10.1177/039463200902200429. [DOI] [PubMed] [Google Scholar]
- 11.Koch FP, Walter C, Hansen T, Jager E, Wagner W. Osteonecrosis of the jaw related to sunitinib. Oral Maxillofac Surg. 2011;15(1):63–66. doi: 10.1007/s10006-010-0224-y. [DOI] [PubMed] [Google Scholar]
- 12.Bettini G, Blandamura S, Saia G, Bedogni A. Bevacizumab-related osteonecrosis of the mandible is a self-limiting disease process. BMJ Case Rep. 2012;2012:pii–pii. doi: 10.1136/bcr-2012-007284. bcr2012007284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nicolatou-Galitis O, Migkou M, Psyrri A, Bamias A, Pectasides D, Economopoulos T, et al. Gingival bleeding and jaw bone necrosis in patients with metastatic renal cell carcinoma receiving sunitinib: report of 2 cases with clinical implications. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113(2):234–238. doi: 10.1016/j.tripleo.2011.08.024. [DOI] [PubMed] [Google Scholar]
- 14.Hopp RN, Pucci J, Santos-Silva AR, Jorge J. Osteonecrosis after administration of intravitreous bevacizumab. J Oral Maxillofac Surg. 2012;70(3):632–635. doi: 10.1016/j.joms.2011.02.104. [DOI] [PubMed] [Google Scholar]
- 15.Fleissig Y, Regev E, Lehman H. Sunitinib related osteonecrosis of jaw: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113(3):e1–e3. doi: 10.1016/j.tripleo.2011.06.023. [DOI] [PubMed] [Google Scholar]
- 16.Magremanne M, Lahon M, De Ceulaer J, Reychler H. Unusual bevacizumab-related complication of an oral infection. J Oral Maxillofac Surg. 2013;71(1):53–55. doi: 10.1016/j.joms.2012.03.022. [DOI] [PubMed] [Google Scholar]
- 17.Santos-Silva AR, Belizário GA, Castro GD, Júnior, Dias RB, Prado Ribeiro AC, Brandão TB. Osteonecrosis of the mandible associated with bevacizumab therapy. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;115(6):e32–e36. doi: 10.1016/j.oooo.2013.02.001. [DOI] [PubMed] [Google Scholar]
- 18.Marino R, Orlandi F, Arecco F, Gandolfo S, Pentenero M. Osteonecrosis of the jaw in a patient receiving cabozantinib. Aust Dent J. 2015;60(4):528–531. doi: 10.1111/adj.12254. [DOI] [PubMed] [Google Scholar]
- 19.Garuti F, Camelli V, Spinardi L, Bucci L, Trevisani F. Osteonecrosis of the jaw during sorafenib therapy for hepatocellular carcinoma. Tumori. 2016;102(Suppl 2):S69–S70. doi: 10.5301/tj.5000504. [DOI] [PubMed] [Google Scholar]
- 20.Ruggiero SL, Dodson TB, Assael LA, Landesberg R, Marx RE, Mehrotra B, American Association of Oral and Maxillofacial Surgeons American Association of Oral and Maxillofacial Surgeons position paper on bisphosphonate-related osteonecrosis of the jaws--2009 update. J Oral Maxillofac Surg. 2009;67(5 Suppl):2–12. doi: 10.1016/j.joms.2009.01.009. [DOI] [PubMed] [Google Scholar]
- 21.Marx RE. Pamidronate (Aredia) and zoledronate (Zometa) induced avascular necrosis of the jaws: a growing epidemic. J Oral Maxillofac Surg. 2003;61(9):1115–1117. doi: 10.1016/s0278-2391(03)00720-1. [DOI] [PubMed] [Google Scholar]
- 22.Ruggiero SL, Mehrotra B, Rosenberg TJ, Engroff SL. Osteonecrosis of the jaws associated with the use of bisphosphonates: a review of 63 cases. J Oral Maxillofac Surg. 2004;62(5):527–534. doi: 10.1016/j.joms.2004.02.004. [DOI] [PubMed] [Google Scholar]
- 23.Vasudev NS, Reynold AR. Anti-angiogenic therapy for cancer: current progress, unresolved questions and future directions. Angiogenesis. 2014;17(3):471–494. doi: 10.1007/s10456-014-9420-y. Review. Erratum in: Angiogenesis. 2014;17(3):495-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Folkman J. Tumor angiogenesis: therapeutic implications. N Engl J Med. 1971;285(21):1182–1186. doi: 10.1056/NEJM197111182852108. Review. [DOI] [PubMed] [Google Scholar]
- 25.Jayson GC, Kerbel R, Ellis LM, Harris AL. Antiangiogenic therapy in oncology: current status and future directions. Lancet. 2016;388(10043):518–529. doi: 10.1016/S0140-6736(15)01088-0. Review. [DOI] [PubMed] [Google Scholar]