Abstract
Objective
To describe school-level and area-level factors that influence coverage of the school-delivered human papillomavirus (HPV) and meningococcal A, C, W and Y (MenACWY) programmes among adolescents.
Design
Ecological study.
Setting and participants
Aggregated 2016/2017 data from year 9 pupils were received from 1407 schools for HPV and 1432 schools for MenACWY. The unit of analysis was the school.
Primary and secondary outcome measures
Outcome measures were percentage point (pp) difference in vaccine coverage by schools’ religious affiliation, school type, urban/rural, single sex/mixed and region. A subanalysis of mixed-sex, state-funded secondary schools also included deprivation, proportion of population from black and ethnic minorities, and school size.
Results
Muslim and Jewish schools had significantly lower coverage than schools of no religious character for HPV (24.0 (95% CI −38.2 to −9.8) and 20.5 (95% CI −30.7 to −10.4) pp lower, respectively) but not for MenACWY. Independent, special schools and pupil referral units had increasingly lower vaccine coverage compared with state-funded secondary schools for both HPV and MenACWY. For both vaccines, coverage was 2 pp higher in rural schools than in urban schools and lowest in London. Compared with mixed schools, HPV coverage was higher in male-only (3.7 pp, 95% CI 0.2 to 7.2) and female-only (4.8 pp, 95% CI 2 to 7.6) schools. In the subanalysis, schools located in least deprived areas had the highest coverage for both vaccines (3.8 (95% CI 0.9 to 6.8) and 10.4 (95% CI 7.0 to 13.8) pp for HPV and MenACWY, respectively), and the smallest schools had the lowest coverage (−10.4 (95% CI −14.1 to −6.8) and −7.9 (95% CI −12 to −3.8) for HPV and MenACWY, respectively).
Conclusions
Tailored approaches are required to improve HPV vaccine coverage in Muslim and Jewish schools. In addition, better ways of reaching pupils in smaller specialist schools are needed.
Keywords: public health, infection control, epidemiology
Strengths and limitations of this study.
This study is the first school-level analysis of factors influencing the coverage of school-delivered vaccines among adolescents in England.
The data set includes a large number of schools across the country, and the school-level variables collected allow determination of associations between vaccine coverage and previously unstudied factors, such as school type or faith affiliation.
The voluntary nature of the school-level data return means the data set is not complete.
For some types of schools, the data set only includes a small number of schools, limiting the precision of some of the results.
The analysis of socioeconomic factors was restricted to mixed-sex, state-funded secondary schools only, based on the assumption that they were more likely to represent pupils from their immediate geographical area.
Introduction
Offering vaccination at school enables large numbers of children to be vaccinated without requiring individual appointments. School vaccination achieves higher coverage than primary care for adolescent vaccines.1 2 There are four school-based vaccination programmes in the UK, which protect against human papillomavirus (HPV vaccine, girls only), meningococcal A, C, W and Y (MenACWY vaccine), diphtheria, tetanus and polio (Td/IPV vaccine), and seasonal influenza.3
HPV vaccine was introduced for girls only in the UK in 2008, initially as a three-dose schedule offered in year 8 (children aged 12–13 years). In September 2014 this changed to a two-dose schedule.4 The recommendation, for operational ease, is for the first (priming) dose to be offered in year 8 and the second (completing) dose in year 9 (age 13–14 years), but NHS England (the agency responsible for commissioning the services) can choose to offer both doses in year 8. In 2015/2016, 85 of 152 (56%) local authorities (LAs) offered both doses within year 8.5 HPV vaccine coverage by the end of year 9 is the final year of assessment for both delivery models. In 2016/2017, national year 9 coverage for HPV was 83.1%.6 MenACWY vaccine was introduced in August 2015 in response to the rising number of MenW cases.7 From autumn 2013 adolescent MenC booster had been offered in school year 9 or 10 (age 14–15 years), but increasingly LAs were aligning to all offer MenC vaccine in year 9.8 In 2016/2017, 82% (124/152) of LAs offered MenACWY routinely in year 9 through the school-based programme.9 The Td/IPV (‘school leaver booster’) vaccine is usually offered alongside MenACWY vaccine. In 2016/2017, MenACWY vaccine coverage nationally by the end of year 9 was 83.6%.9
Previous studies of the national immunisation programme in England have identified inequalities in terms of geography, ethnicity and deprivation for vaccines delivered in primary care.10 11 A previous analysis of vaccine coverage data for the primary school-based seasonal influenza programme in England using population-level characteristics at the Lower Super Output Area level (LSOA, small areas with an average of approximately 1500 residents or 650 households12) in which the school was located identified deprivation, non-white ethnicity, religious beliefs and urban areas to be associated with lower coverage.13–15 2016/2017 is the first year that school-level data were available nationally for the adolescent vaccination programmes, delivered in secondary schools. This study aims to determine whether school-level and other local area factors are associated with vaccine coverage for those adolescent programmes.
Methods
In England, school-based vaccination is delivered by a variety of public and private healthcare providers and commissioned and coordinated through screening and immunisation teams (SITs). Data are routinely collected in each school through tally sheets, aggregated at the local LA level and submitted to Public Health England (PHE). Therefore prior to 2016/2017, school-level data, although collected, were not routinely available at the national level. In September 2017, the 14 SITs in England were asked to voluntarily submit school-level vaccine coverage data for 2016/2017 for all schools in their area using a standardised Microsoft Excel data collection tool. Reminders to submit school-level data were sent out as each submission of LA-level data was received and validated.
School-level data for the 2016/2017 academic year include vaccines given up to and including 31 August 2017. For HPV the data will have included some doses given in the previous academic year (2015/2016).
Queries on data were sent back to providers if:
Denominators or numerators were missing for particular schools. For the small number of schools where denominators were unavailable from the provider, nationally published school roll data were used instead.16
A numerator was greater than a denominator (coverage >100%).
Coverage was 100% for schools with >20 pupils in the denominator.
All schools in an LA were queried if substantial changes were made to any individual schools queried above, and/or if total numerators, denominators or coverage differed by more than 5% from published statistics for LA coverage.6 9
School delivery of the MenACWY and Td/IPV vaccines is generally organised concurrently and given on the same day, so only MenACWY data were used and the findings relating to MenACWY should be generalisable to Td/IPV.
Data were analysed for school year 9 pupils (aged 13–14 years old), born 1 September 2002–31 August 2003. Vaccine coverage of a completed course was calculated by dividing the number of year 9 girls receiving two doses of HPV vaccine and the number of year 9 pupils receiving one dose of MenACWY vaccine by the total number of girls and adolescents, respectively, in the school year.
School characteristics (table 1) were obtained from the Department for Education16 school census and were linked to vaccine coverage using each school’s unique reference number. The LSOA-level geographical factors (table 1), based on the location of each school, were assigned to mixed-sex, state-funded secondary schools only, as these schools were considered most likely to represent pupils from their immediate geographical area. All schools were assigned a National Health Service (NHS) commissioning region (South of England, London, Midlands and East of England, North of England) based on their geographical location. We described the geographical distribution of schools included in the study and compared state-funded secondary schools in the study with all state-funded secondary schools in terms of distribution by school size, graphically and using χ2 test. It was not possible to compare the distribution of the sample with all schools in England because the Department for Education’s school data set does not report the number of independent and special schools or pupil referral units separately between primary and secondary education.
Table 1.
School and geographical characteristics included in the analysis
| Type of characteristics | Categories | Notes |
| Religious affiliation* | No religious character | |
| Church of England/other Christian faith excluding Roman Catholic | Includes Anglican, Free Church, Methodist, other Anglican faith, other Christian faith, Plymouth Brethren Christian Church. | |
| Roman Catholic | ||
| Jewish | ||
| Islam/Muslim | ||
| Other | Includes Hindu, Sikh and other. | |
| School type* | State-funded secondary | |
| Independent | ||
| Special school | Combines state-funded and non-maintained schools for children with special educational needs. | |
| Pupil referral unit | Schools for children excluded from mainstream education because of behaviour, sickness or other reasons. | |
| Urban/Rural* | Urban | |
| Rural | ||
| Single sex/mixed* | Mixed | |
| Female | ||
| Male | ||
| School size (number of pupils)† | Up to 400 (small) | Mean headcount was 728 pupils (range 1–2945). |
| >400 to 1000 (average) | ||
| >1000 (large) | ||
| % of population classifying themselves as black or minority ethnic‡ | <5% | Includes any ethnic group other than ‘White: English/Welsh/Scottish/Northern Irish/British, based on 2011 census categories.26 The thresholds are aligned with those used for influenza vaccine coverage school-level analyses in England.13 27 |
| ≥5% and <12% | ||
| ≥12% and <34% | ||
| ≥34% | ||
| Index of Multiple Deprivation 2015‡ | Quintiles | 1 represents the most deprived, 5 the least deprived. Quintiles were obtained by combining published deciles which rank the 32 844 LSOAs in England from most deprived to least deprived and dividing them into 10 equal groups.28 |
*School characteristics.
†School characteristics only used in the mixed-sex, state-funded school-only subanalysis.
‡Lower Super Output Area (LSOA) characteristics.
Statistical analyses
To take account of school variability and size, individual coverage was calculated for each school, and the analysis was weighted by the denominator of each school.
Unadjusted regression models were used for each school-level factor (except school size, which was adjusted for by weighting) and region to explore differences in coverage from the baseline for each factor (religious affiliation, school type, urban/rural, single sex/mixed). In addition to school-level factors, the association between ethnicity and deprivation LSOA-level factors (proportion of black or minority ethnic (BME) in school LSOA, deprivation) and vaccine coverage was explored for mixed-sex, state-funded secondary schools, using the same model. To ascertain the effect of school size, we opted to include school size as a variable, rather than weighting, in the mixed-sex, state-funded-only subanalysis. We restricted the analysis of school size to this subanalysis because all pupil referral units and special schools were small and had less than 400 pupils. An adjusted linear regression model was then used, presenting differences in coverage from the baseline for each factor, adjusting for all other school-level factors. Area-level factors (proportion of BME in school LSOA, deprivation) were adjusted for all other factors in the subanalysis restricted to mixed-sex, state-funded secondary schools.
This analysis was undertaken using aggregated data routinely collected as part of the ongoing monitoring of the vaccination programme.
Analyses were undertaken in STATA SE V.13.1 statistical software.
Patient and public involvement
This study used routinely collected aggregated data and patients were not involved.
Results
Representativeness of data set
HPV vaccine coverage school-level data for year 9 was received from 41 of 152 LAs. One LA was excluded because their programme was run in primary care during 2015/2016. The final HPV analysis therefore included 40 of 152 (26.3%) LAs and 1407 schools.
MenACWY vaccine coverage school-level data for year 9 was received from 50 LAs. Two were excluded: one ran a selective (boys only) vaccination programme and the other delivered their programme through primary care. In total, 48 of 152 (31.6%) LAs representing 1432 schools were included in the MenACWY analysis.
National HPV vaccine coverage in year 9 in 2016/2017 was 83.1%6 compared with 82.1% among schools included in the study. National MenACWY vaccine coverage in year 9 in 2016/2017 was 83.6%9 compared with 83% among schools included in the study. Schools from each of the four NHS England regions were included, and LAs from all four quartiles of nationally published LA-level HPV vaccine coverage were represented for both HPV and MenACWY.
Compared with all state-funded secondary schools in England, small state-funded secondary schools were under-represented (p=0.03). Distribution was otherwise graphically comparable (figure 1). London schools were under-represented, in particular for HPV where they comprised 3.3% of included schools, whereas 14.6% of all England state-funded secondary schools are in London.
Figure 1.
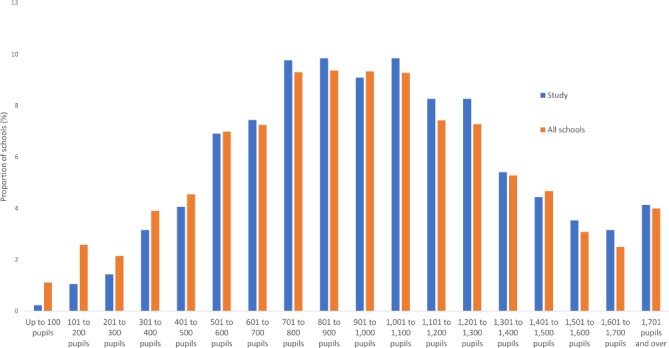
Distribution of state-funded secondary schools by number of pupils, England, 2017.
School type
In the HPV vaccine coverage data set, there were 952 state-funded secondary schools, 235 independent schools, 179 special schools and 41 pupil referral units. HPV vaccine coverage was >80% in 67.1% of state-funded secondary schools, 40.4% of independent schools, 33.5% of special schools and 19.5% of pupil referral units (figure 2).
Figure 2.
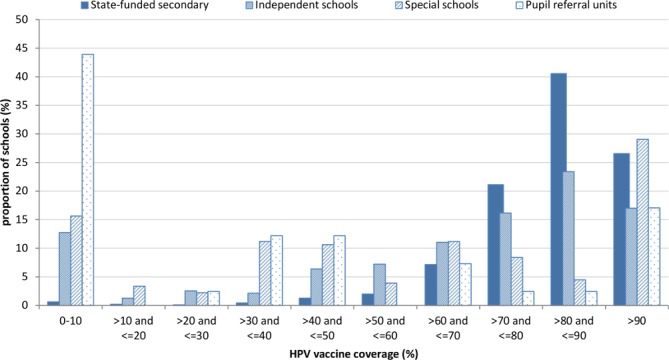
Human papillomavirus (HPV) vaccine coverage distribution by school type, 2016/2017.
In the MenACWY vaccine coverage data set, there were 903 state-funded secondary schools, 263 independent schools, 208 special schools and 58 pupil referral units. MenACWY vaccine coverage was >80% in 68.0% of state-funded secondary schools, 55.1% of independent schools, 26.9% of special schools and 20.7% of pupil referral units (figure 3).
Figure 3.
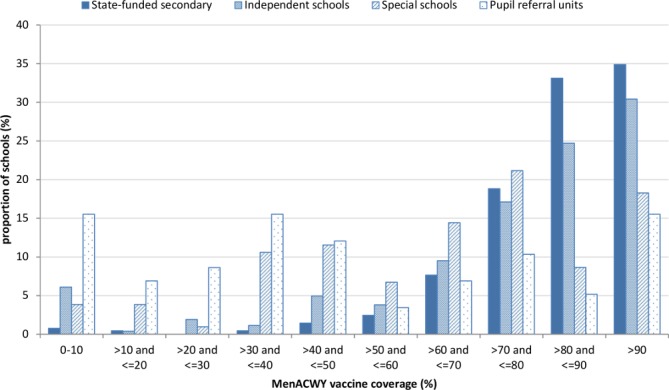
Meningococcal A, C, W and Y (MenACWY) vaccine coverage distribution by school type, 2016/2017.
Factors associated with HPV and MenACWY vaccine uptake
In the adjusted analysis, Muslim and Jewish schools had significantly lower HPV coverage than schools of no religious character (24 and 20.5 percentage points (pp) lower, respectively; table 2), but this was not the case for MenACWY vaccine coverage (table 3).
Table 2.
HPV vaccine coverage and unadjusted/adjusted impact on coverage determined through linear regression, weighted by school size, of school-level predictors and children aged 13–14 years old, England, 2016/2017
| Variable (significance) | Schools (n) | Children (n) | Crude vaccine coverage* (%) | SD of school-level coverage | Unadjusted difference in coverage from baseline (95% CI) | Adjusted difference in coverage from baseline (95% CI)† |
| Denomination of school (p<0.001) | ||||||
| No religious character | 1140 | 73 834 | 82.4 | 25.4 | Baseline | Baseline |
| Church of England/other Christian faith excluding Roman Catholic | 164 | 9201 | 79.8 | 21.8 | −2.5 (−4.7 to 0.4) | −0.7 (−2.9 to 1.5) |
| Roman Catholic | 90 | 6736 | 84.3 | 12.2 | 2.0 (−0.6 to 4.5) | 1.9 (−0.6 to 4.3) |
| Islam/Muslim | 7 | 178 | 56.7 | 24.7 | −25.6 (−40.5 to 10.7) | −24 (−38.2 to −9.8) |
| Jewish | 5 | 356 | 59.6 | 33.6 | −22.8 (−33.4 to 12.3) | −20.5 (−30.7 to −10.4) |
| Other (Hindu, Sikh, Other) | 1 | 48 | 93.8 | – | 11.4 (−17.3 to 40.0) | 10.4 (−16.9 to 37.7) |
| Type of school (p<0.001) | ||||||
| State-funded secondary | 952 | 83 741 | 83.1 | 13.0 | Baseline | Baseline |
| Independent school | 235 | 5693 | 72.8 | 30.9 | −10.3 (−12.9 to 7.7) | −10.3 (−13.0 to −7.5) |
| Special school | 179 | 819 | 56.7 | 35.6 | −26.4 (−33.2 to 19.7) | −26.1 (−32.7 to −19.4) |
| Pupil referral unit | 41 | 100 | 42.0 | 38.9 | −41.1 (−60.3 to 21.8) | −41.1 (−60.0 to −22.2) |
| Urban/Rural classification of school (p=0.03) | ||||||
| Urban | 1165 | 77 645 | 82.0 | 24.4 | Baseline | |
| Rural | 242 | 12 708 | 83.1 | 25.2 | 1.1 (−0.8 to 3.0) | 2.0 (0.1 to 3.9) |
| Sex of school pupils (p=0.07) | ||||||
| Mixed | 1289 | 78 114 | 82.2 | 25.0 | Baseline | Baseline |
| Male | – | – | – | – | – | – |
| Female | 118 | 12 239 | 81.7 | 19.8 | −0.5 (−2.5 to 1.4) | 1.8 (−0.1 to 3.7) |
| Region (p<0.001) | ||||||
| South of England | 580 | 36 855 | 81.0 | 24.8 | Baseline | Baseline |
| London | 47 | 3416 | 77.0 | 14.7 | −4.0 (−7.6 to 0.4) | −3.3 (−6.8 to 0.1) |
| Midlands and East of England | 572 | 36 669 | 82.8 | 24.0 | 1.8 (0.4 to 3.3) | 2.0 (0.6 to 3.4) |
| North of England | 208 | 13 413 | 84.6 | 26.7 | 3.6 (1.6 to 5.6) | 3.6 (1.6 to 5.5) |
| Proportion of BME in school LSOA‡ (p<0.001) | ||||||
| <5% | 243 | 20 210 | 85.5 | 13.3 | Baseline | |
| ≥5% and <12% | 302 | 25 210 | 83.7 | 12.1 | −1.8 (−3.7 to 0.1) | −1.6 (−3.8 to 0.6) |
| ≥12% and <34% | 233 | 19 614 | 81.8 | 13.3 | −3.7 (−5.6 to 1.7) | −4.2 (−6.8 to −1.6) |
| ≥34% | 109 | 8742 | 78.0 | 12.9 | −7.5 (−10.0 to 5.0) | −7.1 (−10.8 to −3.3) |
| Deprivation quintile of school LSOA‡ (p<0.001) | ||||||
| 1 (most deprived) | 149 | 11 295 | 78.6 | 15.3 | Baseline | Baseline |
| 2 | 157 | 12 318 | 84.0 | 11.4 | 5.3 (2.8 to 7.9) | 3.2 (0.2 to 6.0) |
| 3 | 171 | 14 177 | 82.3 | 13.1 | 3.7 (1.2 to 6.2) | 1.5 (−1.3 to 4.4) |
| 4 | 218 | 18 892 | 83.3 | 13.1 | 4.6 (2.3 to 7.0) | 2.6 (−0.2 to 5.4) |
| 5 (least deprived) | 192 | 17 094 | 85.5 | 11.6 | 6.9 (4.5 to 9.3) | 3.8 (0.9 to 6.8) |
| School size (number of pupils)‡ (p<0.001) | ||||||
| >400 to 1000 | 409 | 26 601 | 82.7 | 13.2 | Baseline | Baseline |
| Up to 400 | 50 | 1397 | 74.9 | 21.7 | −10.6 (−14.3 to 6.8) | −10.4 (−14.1 to −6.8) |
| >1000 | 428 | 45 778 | 83.4 | 10.8 | 1.3 (−0.4 to 3.0) | 1.4 (−0.3 to 3.1) |
| Total | 1407 | 90 353 | 82.1 | 24.6 | ||
Estimates are in bold if p<0.05. Estimates were adjusted for all variables.
*Crude coverage calculated as total numerators divided by total denominators.
†School-level factors (denomination, type of school, urban/rural, sex of school pupils, region) are adjusted for other school-level factors only.
‡Based on a subset of mixed-sex, state-funded secondary schools (n=887).
BME, black or minority ethnic; HPV, human papillomavirus; LSOA, Lower Super Output Area.
Table 3.
MenACWY vaccine coverage and unadjusted/adjusted impact on coverage determined through linear regression, weighted by school size, of school-level predictors and children aged 13–14 years old, England, 2016/2017
| Variable (significance) | Schools (n) | Children (n) | Crude vaccine coverage* (%) | SD of school-level coverage | Unadjusted difference in coverage from baseline (95% CI) | Adjusted difference in coverage from baseline (95% CI)† |
| Denomination of school (p=0.685) | ||||||
| No religious character | 1170 | 140 011 | 83.1 | 22.4 | Baseline | Baseline |
| Church of England/other Christian faith excluding Roman Catholic | 158 | 17 765 | 82.8 | 15.8 | −0.3 (−2.6 to 2.0) | −0.3 (−2.6 to 1.9) |
| Roman Catholic | 91 | 13 374 | 83.0 | 14.1 | −0.1 (−2.7 to 2.5) | −0.3 (−2.7 to 2.2) |
| Islam/Muslim | 6 | 60 | 56.7 | 34.2 | −26.4 (−63.4 to 10.5) | −23.3 (−58.4 to 11.8) |
| Jewish | 5 | 605 | 79.3 | 13.4 | −3.7 (−15.4 to 7.9) | 1.2 (−9.9 to 12.3) |
| Other (Hindu, Sikh, Other) | 2 | 153 | 92.8 | 30.7 | 9.7 (−13.4 to 32.9) | 17.6 (−4.4 to 39.6) |
| Type of school (p<0.001) | ||||||
| State-funded secondary | 903 | 155 760 | 83.6 | 14.3 | Baseline | Baseline |
| Independent school | 263 | 13 238 | 81.0 | 25.4 | −2.6 (−5.1 to 0.1) | −2.8 (−5.4 to −0.2) |
| Special school | 208 | 2402 | 65.3 | 25.7 | −18.2 (−23.9 to 12.4) | −18.0 (−23.6 to −12.4) |
| Pupil referral unit | 58 | 568 | 43.7 | 33.0 | −40.0 (−51.7 to 28.3) | −39.6 (−51.0 to −28.2) |
| Urban/Rural classification of school (p=0.003) | ||||||
| Urban | 1162 | 144 682 | 82.6 | 20.7 | Baseline | |
| Rural | 270 | 27 286 | 85.4 | 24.2 | 2.8 (0.9 to 4.7) | 2.0 (0.1 to 3.8) |
| Sex of school pupils (p=0.599) | ||||||
| Mixed | 1268 | 154 500 | 82.9 | 21.5 | Baseline | Baseline |
| Male | 63 | 6452 | 83.3 | 24.2 | 0.4 (−3.2 to 4.0) | 3.7 (0.2 to 7.2) |
| Female | 101 | 11 016 | 84.4 | 18.0 | 1.4 (−1.4 to 4.3) | 4.8 (2.0 to 7.6) |
| Region (p<0.001) | ||||||
| South of England | 569 | 66 632 | 83.2 | 21.5 | Baseline | Baseline |
| London | 168 | 21 097 | 76.2 | 22.6 | −7.1 (−9.3 to 4.8) | −7.8 (−10.0 to −5.5) |
| Midlands and East of England | 298 | 36 382 | 83.7 | 19.9 | 0.5 (−1.4 to 2.3) | 0.6 (−1.2 to 2.4) |
| North of England | 397 | 47 857 | 85.3 | 21.5 | 2.1 (0.4 to 3.7) | 2.3 (0.6 to 3.9) |
| Proportion of BME in school LSOA‡ (p<0.001) | ||||||
| <5% | 274 | 45 727 | 84.9 | 14.9 | Baseline | Baseline |
| ≥5% and <12% | 263 | 47 521 | 84.9 | 13.7 | 0.1 (−2.0 to 2.1) | 0.4 (−2.1 to 2.9) |
| ≥12% and <34% | 182 | 32 394 | 83.6 | 13.0 | −1.3 (−3.6 to 1.0) | 1.1 (−1.8 to 4.2) |
| ≥34% | 100 | 16 853 | 75.6 | 17.4 | −9.3 (−12.1 to 6.5) | −1.1 (−5.9 to 3.8) |
| Deprivation quintile of school LSOA‡ (p<0.001) | ||||||
| 1 (most deprived) | 108 | 17 574 | 76.0 | 15.3 | Baseline | Baseline |
| 2 | 148 | 23 107 | 82.8 | 16.8 | 6.8 (3.7 to 9.9) | 5.2 (1.8 to 8.7) |
| 3 | 161 | 26 006 | 82.0 | 16.3 | 6.0 (3.0 to 9.0) | 3.9 (0.4 to 7.3) |
| 4 | 206 | 37 777 | 83.6 | 14.3 | 7.6 (4.7 to 10.4) | 5.1 (1.7 to 8.4) |
| 5 (least deprived) | 196 | 38 031 | 88.2 | 8.8 | 12.2 (9.4 to 15.0) | 10.4 (7.0 to 13.8) |
| School size (number of pupils)‡ (p<0.001) | ||||||
| >400 to 1000 | 378 | 51 249 | 82.1 | 14.2 | Baseline | Baseline |
| Up to 400 | 49 | 2720 | 76.9 | 25.5 | −7.5 (−11.9 to 3.2) | −7.9 (−12 to −3.8) |
| >1000 | 392 | 88 526 | 84.5 | 12.7 | 3.2 (1.1 to 5.3) | 2.6 (0.6 to 4.6) |
| Total | 1432 | 171 968 | 83.0 | 21.4 | ||
Estimates are in bold if p<0.05. Estimates were adjusted for all variables.
*Crude coverage calculated as total numerators divided by total denominators.
†School-level factors (denomination, type of school, urban/rural, sex of school pupils, region) are adjusted for other school-level factors only.
‡Based on a subset of mixed-sex, state-funded secondary schools (n=887).
BME, black or minority ethnic; LSOA, Lower Super Output Area; MenACWY, meningococcal A, C, W and Y.
Independent, special schools and pupil referral units had increasingly lower vaccine coverage than state-funded secondary schools for both HPV and MenACWY. This ranged from 10.3 pp lower for independent schools to 41.1 pp lower for pupil referral units for HPV (table 2), and from 2.8 pp lower for independent schools to 39.6% lower for pupil referral units for MenACWY (table 3).
Rural schools had 2.0 pp higher coverage than urban schools for both HPV and MenACWY (tables 2 and 3).
Single-sex schools had higher coverage than mixed schools for MenACWY (3.7 pp higher for boys, 4.8 pp higher for girls; table 2), but there was no difference between mixed and female-only schools for HPV (table 2).
There was regional variation in vaccine coverage for both HPV and MenACWY, but this was most marked for MenACWY, where coverage in London was 7.8 pp lower than in the South of England (table 3).
Mixed-sex, state-funded secondary schools located in LSOAs with the largest BME populations (≥34%) had HPV vaccine coverage 7.1 pp below those located in LSOAs with BME populations of <5% (table 2). In contrast, there was no association between MenACWY vaccine coverage and BME population proportion within the school LSOA (table 3). There was no clear trend in vaccination coverage by school LSOA deprivation quintiles, although schools located in the least deprived LSOAs had the highest coverage for both HPV and MenACWY (3.8 pp and 10.4 pp higher than schools located in the most deprived LSOAs for HPV and MenACWY, respectively; tables 2 and 3). Among mixed-sex, state-funded schools, compared with average-sized schools, small schools (up to 400 pupils) had lower coverage for HPV and MenACWY (−10.4 pp and −7.9 pp, respectively), and for MenACWY only larger schools had higher coverage (2.6 pp).
Discussion
Interpretation of key findings
Although national HPV and MenACWY vaccine coverage is high, this first school-level analysis has identified important school-level factors associated with wide variations in vaccine coverage.
The lower coverage in Jewish schools for HPV but not for MenACWY suggests that there are no issues with vaccination acceptance or access in general, but there may be less acceptance of the need for HPV vaccine particularly within this religious community. In Muslim schools, coverage was lower for MenACWY and HPV; the difference was only significantly lower for HPV. In contrast, coverage for both vaccines in Roman Catholic schools was similar or higher than coverage in schools of no religious character. These findings suggest that issues around vaccination may be specific to each religious community and that different vaccines may be perceived differently within a given community. Factors underlying these differences require further investigation.
The vast majority of schools in England participate in the school-based vaccination programmes. A survey of SITs undertaken by PHE’s national immunisation team highlighted that only a small number of minority faith/anthroposophic (Steiner) schools in specific areas declined to allow immunisation teams access. In these instances, it is sometimes possible for immunisation teams to provide letters and/or leaflets directing pupils to external clinics, although uptake is likely to be lower in these settings than in school-based sessions.
The marked variation in coverage across school types is likely to be multifactorial. Our analysis has shown that school size is a factor, with smaller schools achieving lower coverage; state-funded secondary schools are the largest, followed by independent, special schools and pupil referral units. Identifying and reaching eligible pupils in referral units, where the number of pupils is likely to be small and change throughout the year, with possibly only one eligible child in a particular year, is more challenging than in larger schools. Immunisation teams may also find it more resource-efficient to visit and offer mop-up sessions in larger schools, where a greater number of pupils can be reached at any one visit. Pupils in special schools in particular may have specific health needs that are typically managed by their general or specialist practitioner, and children with medical conditions are less likely to be immunised.17 Information about vaccines given by other health practitioners may not always get back to the immunisation teams responsible for providing vaccine coverage data to PHE. In addition, the independent school category may include some small schools that cater to children with special educational or health needs, so there could be some overlap between categories. Steiner schools, identified by several SITs as not offering vaccination, are typically independent schools and could not be identified separately in our analysis (they are categorised as having no religious character).
There was no difference in HPV coverage between mixed and female-only schools. The reason behind the higher MenACWY coverage in single-sex schools is unclear, although in the case of female-only schools it may partly be because MenACWY can be offered alongside the existing HPV programme. It could also be that in mixed schools, boys have lower coverage than girls, although this cannot be verified because gender-specific coverage is not collected.
Coverage was lower for London compared with other areas, as seen across other childhood immunisation programmes.18 Participation from London was low in this study particularly for HPV. Lack of statistical power with the London HPV sample may partly explain why HPV coverage for London was not lower than the baseline after adjusting for other factors.
The ability to study school-specific factors was a major strength of this study. Although we did a restricted, mixed-sex, state-funded secondary schools-only subanalysis (ie, schools most likely to have pupil catchment areas in the immediate locality) to determine the association between coverage and deprivation and ethnicity factors, the influence of these factors on vaccine coverage is less clear. However, the fact that schools in the most deprived areas had lowest coverage across both programmes suggests that even within a school-based programme, deprivation has an influence on coverage. These findings may be less reliable in London as students may travel in other parts of the city to attend school.
The lower HPV coverage in schools located in areas with the highest BME proportion could relate to the school-level finding of particular religious schools having lower coverage for HPV. These results suggest some religious and possibly ethnic groups have objections to offering or receiving the HPV vaccine in particular. These results were not observed for the MenACWY vaccination programme.
Limitations of the data
This data set relied on voluntary submissions of school-level data. Although the data set contained schools from only 26% and 32% of LAs for HPV and MenACWY, respectively, overall coverage aligned well with national coverage, so the data set appeared to be broadly representative. Because the school census does not allow to easily distinguish primary and secondary schools, we could not ascertain whether the proportion of religious, independent and special schools was similar in our sample compared with all schools in England. This may affect the precision of the findings and may lead to failing to detect associations between particular characteristics and uptake for school types that are under-represented.
Although the numerator for each school should include any vaccine given up to and including 31 August 2017, it could be underestimated as some schools/areas may only include vaccines given in the particular academic year, which ends in July in most schools. The extent to which this is an issue is unclear, but likely small as only a limited number of individuals in these age groups receive HPV and MenACWY through general practice.
Similarity/difference from the results of other studies
HPV vaccine uptake by school denomination has previously been studied in Scotland, although no difference in uptake was found between denominational and non-denominational schools.19 This may be because the denomination category did not allow the detail of individual types of denominational schools to be explored, and because the number of non-Christian faith schools is small. Similar to our findings, the Scottish study found that those in schools with the highest deprivation quintile (as measured by the percentage of pupils eligible for free school meals) had a significantly lower uptake than those in schools with the lowest percentage of pupils eligible for free school meals,19 and deprivation was also significantly associated with lower vaccine coverage for the influenza programme.15 A previous study in South West England found no evidence of an association of HPV vaccination and deprivation (assigned by LSOA of residence), but did find an association by ethnicity (individual level), and that young women attending non-mainstream educational settings were less likely to initiate vaccination.20 A systematic review of factors associated with HPV vaccine initiation and completion in teenage girls found that having a Caucasian ethnic background was associated with higher rates of vaccine initiation and completion.21 Another systematic review mainly including studies from the USA also found inequalities with regard to ethnicity, and more specifically that, compared with white women, black women were less likely to be vaccinated against HPV.22 Although these findings are not directly comparable with our ecological analysis of the role of ethnicity, the results are nonetheless compatible.
Vaccine uptake for the school-based influenza programme by area-level (LSOA) factors has identified variation by religious beliefs, with adjusted uptake in children aged 4–11 years old in the highest Muslim population tertile 8% lower than the lowest Muslim population tertile, but this could be specific to the influenza vaccine because of the porcine origin gelatine component.13 Similarly to MenACWY and HPV, influenza vaccine uptake in schools was higher in rural areas than in urban areas, and similarly to HPV coverage decreased with increasing proportion of BME population in the LSOA, although the association was stronger with the influenza vaccine.13 The school-based influenza vaccine programme targets a much younger age group, and there may be other factors influencing uptake, such as perceptions and attitudes to each disease.23
Finally, in addition to school-based programmes, variation in uptake by ethnicity, deprivation and geography is also found in primary care-based programme,10 11 and while some factors influencing uptake are school-specific, others may be more closely related to characteristics of the population attending these schools.
Conclusions
Although school delivery programmes achieve high coverage for adolescent vaccine programmes overall, there are particular types of schools that have lower coverage and where alternative approaches to improve coverage might be beneficial. This includes particular religious schools, where further understanding of acceptance of particular vaccinations would be helpful. Tailored approaches, such as the WHO’s ‘Tailoring immunization programmes’, which aim to understand barriers that are context-specific,24 could help improve uptake in these schools. Because factors influencing uptake are likely to be a mix of school-based and community-based factors, tailored strategies addressing both aspects are most likely to succeed. In addition, it could be helpful to share best practice regarding the best ways of reaching pupils in small specialist schools and pupil referral centres. It is important to bear in mind that as well as considering school-level factors, the individual relationship between a school and immunisation nursing teams must be mutually supportive for successful vaccine delivery.25 It is hoped that, given these findings, submission of school-level data returns will improve to enable continued monitoring of these influences on vaccine coverage.
Supplementary Material
Acknowledgments
The authors would like to thank all screening and immunisation teams that provided data for this analysis, Ashley Makwana for his assistance with data validation, and Bryony Cook in the Geographical Information Systems Department of Public Health England for the production of maps.
Footnotes
Contributors: KT, JW, ME and MR designed the study. KT, ME and NA designed the analytical plan. KT and ET managed and analysed the data. All authors contributed to writing the manuscript.
Funding: This analysis was undertaken using aggregated data routinely collected as part of the ongoing monitoring of the vaccination programme.
Competing interests: None declared.
Ethics approval: No formal ethical approval was required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: The school-level data set (anonymised to prevent school-level disclosure) can be requested by emailing the corresponding author.
Patient consent for publication: Not required.
References
- 1. Crocker J, Porter-Jones G, McGowan A, et al. . Teenage booster vaccine: factors affecting uptake. J Public Health 2012;34:498–504. 10.1093/pubmed/fds047 [DOI] [PubMed] [Google Scholar]
- 2. Rehn M, Uhnoo I, Kühlmann-Berenzon S, et al. . Highest vaccine uptake after school-based delivery - a county-level evaluation of the implementation strategies for hpv catch-up vaccination in Sweden. PLoS One 2016;11:e0149857 10.1371/journal.pone.0149857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Public Health England. The complete routine immunisation schedule. 2018. https://www.gov.uk/government/publications/the-complete-routine-immunisation-schedule (Accessed Dec 2018).
- 4. Public Health England, Department of Health, NHS England. HPV vaccination programme: change from 3 to 2 doses. 2014. https://www.gov.uk/government/publications/schedule-change-from-3-to-2-doses-in-the-hpv-vaccination-programme (Accessed Dec 2018).
- 5. Public Health England. Annual HPV vaccine coverage 2015 to 2016: by local authority and area team. 2016. https://www.gov.uk/government/statistics/annual-hpv-vaccine-coverage-2015-to-2016-by-local-authority-and-area-team (Accessed Dec 2018).
- 6. Public Health England. Human Papillomavirus (HPV) vaccination coverage in adolescent females in England: 2016/17. 2017. https://www.gov.uk/government/statistics/annual-hpv-vaccine-coverage-2016-to-2017-by-local-authority-local-team-and-area-team.
- 7. Public Health England. MenACWY vaccine introduction. 2015. https://www.gov.uk/government/publications/menacwy-vaccine-introduction (Accessed Dec 2018).
- 8. Public Health England. Changes to the meningococcal C conjugate (MenC) vaccine schedule 2013-2015. 2014. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/336171/MenC_information_for_healthcare_professionals_V7_.pdf (Accessed Dec 2018).
- 9. Public Health England. Vaccine coverage estimates for the school based meningococcal ACWY (MenACWY) adolescent vaccination programme in England. 31 August 2017 2018. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/677839/hpr0318_men-acwy-schl.pdf.
- 10. Tiley KS, White JM, Andrews N, et al. . Inequalities in childhood vaccination timing and completion in London. Vaccine 2018;36:6726–35. 10.1016/j.vaccine.2018.09.032 [DOI] [PubMed] [Google Scholar]
- 11. Byrne L, Ward C, White JM, et al. . Predictors of coverage of the national maternal pertussis and infant rotavirus vaccination programmes in England. Epidemiol Infect 2018;146:197–206. 10.1017/S0950268817002497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Office for National Statistics. Census geography, Output Area (OA) https://www.ons.gov.uk/methodology/geography/ukgeographies/censusgeography (Accessed Dec 2018).
- 13. Green HK, Andrews N, Letley L, et al. . Phased introduction of a universal childhood influenza vaccination programme in England: population-level factors predicting variation in national uptake during the first year, 2013/14. Vaccine 2015;33:2620–8. 10.1016/j.vaccine.2015.03.049 [DOI] [PubMed] [Google Scholar]
- 14. Public Health England. Seasonal influenza vaccine uptake in children of primary school age: winter season 2015 to 2016. 2017. https://www.gov.uk/government/statistics/seasonal-flu-vaccine-uptake-in-children-of-primary-school-age-winter-season-2015-to-2016 (Accessed Dec 2018).
- 15. Public Health England. Seasonal influenza vaccine uptake in children of primary school age: winter season 2016 to 2017. 2017. https://www.gov.uk/government/statistics/seasonal-flu-vaccine-uptake-in-children-of-primary-school-age-winter-season-2016-to-2017 (Accessed Dec 2018).
- 16. Department for Education. Schools, pupils and their characteristics: Jan 2017. 2017. https://www.gov.uk/government/statistics/schools-pupils-and-their-characteristics-january-2017 (Accessed Dec 2018).
- 17. Aigbogun NW, Hawker JI, Stewart A. Interventions to increase influenza vaccination rates in children with high-risk conditions--a systematic review. Vaccine 2015;33:759–70. 10.1016/j.vaccine.2014.12.013 [DOI] [PubMed] [Google Scholar]
- 18. Public Health England. Vaccine uptake guidance and the latest coverage data, Cover of vaccination evaluated rapidly programme. 2018. https://www.gov.uk/government/collections/vaccine-uptake#cover-of-vaccination-evaluated-rapidly-programme (Accessed Dec 2018).
- 19. Sinka K, Kavanagh K, Gordon R, et al. . Achieving high and equitable coverage of adolescent HPV vaccine in Scotland. J Epidemiol Community Health 2014;68:57–63. 10.1136/jech-2013-202620 [DOI] [PubMed] [Google Scholar]
- 20. Fisher H, Audrey S, Mytton JA, et al. . Examining inequalities in the uptake of the school-based HPV vaccination programme in England: a retrospective cohort study. J Public Health 2014;36:36–45. 10.1093/pubmed/fdt042 [DOI] [PubMed] [Google Scholar]
- 21. Kessels SJ, Marshall HS, Watson M, et al. . Factors associated with HPV vaccine uptake in teenage girls: a systematic review. Vaccine 2012;30:3546–56. 10.1016/j.vaccine.2012.03.063 [DOI] [PubMed] [Google Scholar]
- 22. Fisher H, Trotter CL, Audrey S, et al. . Inequalities in the uptake of human papillomavirus vaccination: a systematic review and meta-analysis. Int J Epidemiol 2013;42:896–908. 10.1093/ije/dyt049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Brabin L, Roberts SA, Farzaneh F, et al. . Future acceptance of adolescent human papillomavirus vaccination: a survey of parental attitudes. Vaccine 2006;24:3087–94. 10.1016/j.vaccine.2006.01.048 [DOI] [PubMed] [Google Scholar]
- 24. World Health Organization. Guide to tailoring immunization programmes. 2013. http://www.euro.who.int/en/health-topics/communicable-diseases/measles-and-rubella/publications/2013/guide-to-tailoring-immunization-programmes (Accessed Dec 2018).
- 25. Brabin L, Stretch R, Roberts SA, et al. . The school nurse, the school and HPV vaccination: a qualitative study of factors affecting HPV vaccine uptake. Vaccine 2011;29:3192–6. 10.1016/j.vaccine.2011.02.038 [DOI] [PubMed] [Google Scholar]
- 26. Office for National Statistics. Ethnic group by sex and age, nomis, official labour market statistics 2011. http://www.nomisweb.co.uk/census/2011/lc2101ew (Accessed Dec 2018).
- 27. Tessier E, Warburton F, Tsang C, et al. . Population-level factors predicting variation in influenza vaccine uptake among adults and young children in England, 2015/16 and 2016/17. Vaccine 2018;36:3231–8. 10.1016/j.vaccine.2018.04.074 [DOI] [PubMed] [Google Scholar]
- 28. Ministry of Housing Communities and Local Government. English indices of deprivation. 2015. https://www.gov.uk/government/statistics/english-indices-of-deprivation-2015 (Accessed Dec 2018).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


