Abstract
Objective:
Very few controlled trials have evaluated targeted treatment methods for childhood selective mutism (SM); the availability of evidence-based services remains limited. This study is the first controlled trial to evaluate an Intensive Group Behavioral Treatment (IGBT) for children with SM.
Method:
Twenty-nine children with SM (5–9 years; 76% female; 35% ethnic minority) were randomized to immediate SM 5-day IGBT or to a 4-week waitlist with psychoeducational resources (WLP), and were assessed at Week 4 and again 8 weeks into the following school year.
Results:
IGBT was associated with high satisfaction and low perceived barriers to treatment participation. At Week 4, 50% of the immediate IGBT condition and 0% of the WLP condition were classified as “clinical responders.” Further, Time×Condition interactions were significant for social anxiety severity, verbal behavior in social situations, and global functioning (but not for SM severity, verbal behavior in home settings, or overall anxiety). School-year follow-up assessments revealed significant improvements across all outcomes. Eight weeks into the following school year, 46% of IGBT-treated children were free of an SM diagnosis. In addition, teachers in the post-IGBT school year rated less school impairment and more classroom verbal behavior relative to teachers in the pre-IGBT school year.
Conclusions:
Findings provide the first empirical support for the efficacy and acceptability of IGBT for SM. Further study is needed to examine mechanisms of IGBT response, and other effective SM treatment methods, in order to clarify which treatment formats work best for which affected children.
Keywords: selective mutism, child anxiety, intensive treatment, RCT
Introduction
Selective mutism (SM) is a relatively rare, but highly impairing, childhood anxiety disorder characterized by a failure to speak in certain social situations (e.g., school), despite fluent speech in more familiar settings (e.g., home) (Bergman, Piacentini, & McCracken, 2002; Elizur & Perednik, 2003; Furr, Sanchez, Hong, & Comer, in press; Muris & Ollendick, 2015). Such persistent failure to speak in certain situations, especially in the school setting, can have profound negative impacts on functioning (e.g., Carbone et al., 2010). Further, SM is associated with the presence of other internalizing problems, notably social anxiety disorder (SocAD), social skills deficits, and considerable functional impairment (Carbone et al., 2010; Cunningham, McHolm, & Boyle, 2006; Scott & Beidel, 2011). The mean age of SM onset is between 2 and 5 years of age (Muris & Ollendick, 2015). Although the reported prevalence of SM is relatively low (i.e., less than 2%), prevalence estimates are expected to rise with improved identification and awareness (e.g., Bergman et al., 2002; Elizur & Perednik, 2003; Muris & Ollendick, 2015).
A very small, but growing, body of research has begun to examine how to most effectively treat SM and related impairments, with cognitive behavioral treatment (CBT) strategies showing the strongest preliminary support (Cohan, Chavira, & Stein, 2006; Furr et al., in press; Muris & Ollendick, 2015). Prior to 2013, the majority of SM treatment studies were case studies or open trials that demonstrated preliminary support for CBT interventions for SM (see Cohan et al., 2006 for review). For example, Manassis and Tannock (2008) naturalistically examined non-randomized outcomes across youth with SM (N = 17) who were treated with various intervention methods, and in a case series (N = 5), Sharkey and colleagues (2008) demonstrated the preliminary feasibility and utility of a group treatment format for children with SM. To date, only a handful of controlled evaluations of SM treatment have been conducted. In the first randomized controlled trial of a psychosocial intervention for childhood SM, Bergman and colleagues (2013) demonstrated the efficacy of a 6-month weekly outpatient CBT intervention that involved parents, children, and their teachers. A second randomized trial conducted by Oerbeck and colleagues (2014) evaluated a 21-session weekly behavioral intervention implemented in home and school settings, and observed treatment-related improvements in parent- and teacher-reported speaking behavior. Treatment gains were maintained up to five years following treatment, particularly among younger children, underscoring the importance of early intervention (Oerbeck, Overgaard, Stein, Pripp, & Kristensen, 2018; Oerbeck, Stein, Pripp, & Kristensen, 2015).
Importantly, both Bergman and colleagues’ (2013) and Oerbeck and colleagues’ (2014) studies found, using a 3-month waitlist control condition, that SM symptoms did not naturally remit over this amount of time. Although some literature suggests that as many as half of SM cases may remit within 13 years, this is a very long period of development, and untreated SM is associated with the development of other internalizing problems that often persist into young adulthood (Steinhausen, Wachter, Laimböck, & Metzke, 2006). Weekly interventions that take up to a half of a year to complete may occupy a considerable portion of the academic year during which time symptoms may still be interfering. Indeed, for the treatment of some children with SM, there may be a need for more efficient treatment formats that are shorter in length, and that can be completed in the summer months, when school is not in session.
Moreover, weekly treatment programs exclude families who do not have access to local expertise in the clinical management of SM. Some have argued that low base rate disorders such as SM may not afford sufficient practice opportunities for the majority of clinicians to develop an adequate skillset to effectively treat these conditions (Comer & Barlow, 2014). Although there has been some uncontrolled evidence supporting standard CBT for the common child anxiety disorders in the treatment of childhood SM (Fisak, Oliveros & Ehrenreich, 2006; Suveg, Comer, Furr, & Kendall, 2006), unique symptoms of SM (e.g., failure to speak with unfamiliar adults, limited verbal responses to questions) may limit the extent to which therapists can directly engage children in the traditional interactive communication, reciprocal discussion, and Socratic dialogues that are central to CBT for the more common child anxiety disorders (Furr et al., in press). Therapists must also be careful not to inadvertently reinforce non-verbal communication patterns early in treatment (e.g., accepting child head nods and other gestures as forms of child communication) in a misguided effort to move treatment along (see Furr et al., in press). Accordingly, although empirical investigations are needed, it may be that therapists working with youth with SM require a level of specialized training that therapists with expertise in standard treatment for other child anxiety disorders do not traditionally receive. This leaves many affected families, especially those in parts of the country with limited access to SM specialty clinics, without effective treatment options. As is the case for many low base rate conditions requiring specialized treatment methods (see Comer & Barlow, 2014), the majority of SM specialty centers are concentrated in major metropolitan regions or academic hubs.
Given potential limits in the acceptability and accessibility of SM treatment options—including few research-supported treatments, prolonged durations associated with the few evaluated treatments, and potential limited regional expertise in SM (see Comer & Barlow, 2014)—in recent years Intensive Group Behavioral Treatment (IGBT) formats have grown in popularity (e.g., Petersen, 2015; Saint Louis, 2015). IGBT for SM provides a full course of intervention in a condensed period of time (e.g., 1 week), allowing families dwelling in regions lacking local SM expertise to receive expert care at a specialty clinic within a shortened time frame. Summer intensive treatment programs have shown success for treating a range of childhood problems (e.g., Fabiano, Schatz, & Pelham, 2014; Gallo, Cooper-Vince, Hardway, Pincus, & Comer, 2014; Pelham & Hoza, 1996; Rice, Kostek, Gair, & Rojas, 2017), and destination intensive CBT programs, in particular, have shown promise for treating child anxiety disorders (e.g., Ehrenreich & Santucci, 2009; Gallo et al., 2014; Ollendick, 2014). A growing literature has anecdotally commented that IGBT for SM is becoming an increasingly common clinical referral for youth with SM, with initial evidence documenting the preliminary promise of IGBT for reducing symptoms of SM (Carpenter, Puliafico, Kurtz, Pincus, & Comer, 2014; Furr et al., in press). However, to date there has not been a controlled evaluation of IGBT for SM.
The present waitlist-controlled study is the first randomized trial to evaluate the preliminary efficacy of a 1-week summer IGBT as an acceptable treatment format for delivering specialized care to children with SM regardless of their proximity to an SM specialty center and regardless of their ability to sustain participation in prolonged weekly treatment. Participating children were followed from baseline (Week 0) through Week 4, and then followed up again 8 weeks into the following school year in order to examine the maintenance and generalizability of gains. Given the reported overlap in symptom presentations between SM and social anxiety disorder (SocAD), familial links between SM and SocAD (Chavira, Shipon-Blum, Hitchcock, Cohan & Stein, 2007), and questions as to whether SM is truly its own diagnostic entity, or whether it is simply a severe subtype or developmental variant of SocAD (Bogels et al., 2010; Martinez et al., 2015), we examined the impact of IGBT on SM symptoms as well as on social anxiety. It was hypothesized that IGBT would be a feasible and acceptable treatment option for families of children with SM, that IGBT would be associated with significant improvements in SM, social anxiety, overall anxiety, and global functioning, and that improvements would be maintained into the following school year.
Method
Participants
Participants were 29 children between the ages of 5 and 9 years (M = 6.6, SD = 1.3), and their parents who were seeking services for their child at an SM specialty treatment center in a large metropolitan region in the southeastern United States. Families were typically referred by other programs or professionals in the field, their school, or by reading about the program online or in national media coverage of IGBT. For study eligibility, children in the study age range needed to meet DSM-5 criteria for SM, and were excluded if: 1) they were identified as having any mental health condition more impairing than SM; or 2) they were nonverbal with both of their parents (given necessity of verbal interaction with at least one adult prior to starting treatment to facilitate stimulus fading and other treatment skills as described below). For generalizability, children with comorbid anxiety disorders and other disorders were included. Further, children taking stable doses of psychotropic medication (i.e., no starting/stopping medication, no dose changes for at least 6 weeks prior to baseline assessment) were also included if the family committed to remain on this stable dose through the post-treatment assessment. Families were required to cease non-study psychotherapeutic activities from the start of the study (i.e., before baseline assessment) through the post-treatment assessment, but were allowed to participate in non-study therapeutic activities after their post-treatment assessment procedures.
Table 1 presents baseline sample characteristics. Roughly three-quarters of the sample were female, and roughly one-third were Hispanic/Latino. Families came from a diverse range of economic backgrounds, with 55.2% earning less than $100,000 per year. All participating children met DSM-5 criteria for SM. Comorbid diagnoses included SocAD (72.4%), separation anxiety disorder (27.6%), generalized anxiety disorder (24.1%), specific phobia (10.3%), obsessive compulsive disorder (6.9%), enuresis (6.9%), and attention-deficit/hyperactivity disorder (6.8%). Seventeen percent (17.2%) of parents reported that their child was taking a stable dose of psychotropic medication. Fifty-two percent of families were from “out of town,” defined as >3 hours driving distance from the treatment center (Mdistance = 716 miles), with 44.8% of the full sample living more than 500 miles from the clinic.
Table 1.
Baseline characteristics across full sample, and by condition
| Full sample (N=29) |
Treatment Condition | Significance test | |||||
|---|---|---|---|---|---|---|---|
| IGBT (n=14) |
WLP (n=15) |
||||||
| N | % | N | % | N | % | ||
| Gender | χ2(1,N=29) = 0.29 , p = .591 | ||||||
| Female | 22 | 75.9 | 10 | 71.4 | 12 | 80.0 | |
| Male | 7 | 24.1 | 4 | 28.6 | 3 | 20.0 | |
| Ethnicity | χ2(1,N=29) = .02 , p = .893 | ||||||
| Hispanic/Latino | 10 | 34.5 | 5 | 35.7 | 5 | 33.3 | |
| Non-Hispanic/Latino | 19 | 65.5 | 9 | 64.3 | 10 | 66.7 | |
| Race | χ2(3,N=29) = 1.13 , p = .769 | ||||||
| White | 24 | 82.7 | 11 | 78.5 | 13 | 86.7 | |
| Black/African American | 2 | 6.9 | 1 | 7.1 | 1 | 6.7 | |
| Asian | 2 | 6.9 | 1 | 7.1 | 1 | 6.7 | |
| Other | 1 | 3.4 | 1 | 7.1 | 0 | 6.7 | |
| Household income | χ2(1,N=28) = 1.20, p = .274 | ||||||
| <$100,000 | 16 | 55.2 | 6 | 42.9 | 10 | 66.7 | |
| ≥$100,000 | 12 | 41.4 | 7 | 50.0 | 5 | 33.3 | |
| Parent Education Level | χ2(4,N=29) = 5.33, p = .255 | ||||||
| High school | 1 | 3.4 | 0 | 0 | 1 | 6.7 | |
| Some college | 6 | 20.7 | 4 | 28.6 | 2 | 13.3 | |
| Associate degree | 1 | 3.4 | 0 | 0 | 1 | 6.7 | |
| Bachelors degree | 8 | 27.6 | 2 | 14.3 | 6 | 40.0 | |
| Graduate degree | 13 | 44.8 | 8 | 57.1 | 5 | 33.3 | |
| Mean | SD | Mean | SD | Mean | SD | ||
| Age | 6.6 | 1.3 | 6.4 | 1.4 | 6.7 | 1.4 | t(27) = −1.07, p = .294; 95% CI [−1.44, .44] |
| Annual Household Income, $ | 88,303 | 51,184 | 90,422 | 41,698 | 86,467 | 59,619 | t(27) = .20, p = .843; 95% CI [−36,640, 44,551] |
| SM CSR | 4.9 | 0.7 | 4.9 | 0.8 | 4.9 | 0.6 | t(27) = −.04, p = .971; 95% CI [−.55, .53] |
IGBT: Intensive group behavioral therapy; WLP: Waitlist with psychoeducation; SM: Selective mutism; CSR: Clinical severity rating
Procedures
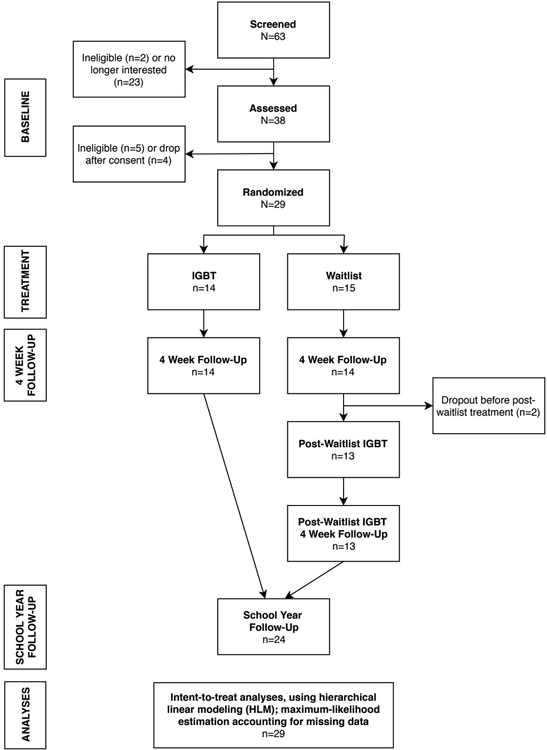
Study procedures were approved by the Florida International University Institutional Review Board and informed consent was obtained from all primary caregivers prior to study participation. Figure 1 presents the flow of study participants through all phases of the study. Several assessments and study procedures were conducted via remote mechanisms (e.g., phone), given the high number of participating families from out of state and/or >3 hours travel distance to the clinic. All consenting families completed a pre-summer semi-structured diagnostic interview and a battery of questionnaires (Baseline; Mean = 2.8 weeks prior to IGBT start), during which time each child’s respective teacher was asked to also complete a brief battery of questionnaires. Eligible families were then randomly assigned to IGBT or to a 4-week waitlist with psychoeducational materials (WLP). All participating families again completed a semi-structured diagnostic interview and a battery of questionnaires in a post-IGBT/WLP Week 4 assessment (roughly 4 weeks following their Baseline assessment), after which WLP families were given the opportunity to participate in post-WLP IGBT. WLP families then participated in a second post assessment after completing IGBT, again consisting of a semi-structured diagnostic interview and questionnaires. All families were again contacted 8 weeks into their child’s academic year to conduct a school-year follow-up (SYF; Mean = 14.7 weeks following IGBT) assessment consisting of a semi-structured diagnostic interview, parent questionnaires, and teacher questionnaires. Parents were compensated $40 for completing post-treatment assessment procedures and $40 for completing SYF assessment procedures; teachers were compensated $15 for completing SYF questionnaires. All participating families were offered treatment at a sliding scale discounted rate dependent on household income, ranging from $375 to $775 (Mean cost = $13/hour).
Figure 1.
Flow of participants across study phase
Study conditions
IGBT.
IGBT is an intensive group CBT program centered around graduated exposure to verbal communication that draws heavily on the early child format and advances of Parent-Child Interaction Therapy (PCIT; Funderburk & Eyberg, 2011). PCIT—originally developed to treat early child externalizing problems—is designed to reshape adult-child interaction patterns and social reinforcers associated with the maintenance of child symptoms. Treatment is delivered in a developmentally sensitive manner that does not engage young children in therapeutic tasks that may be beyond their cognitive developmental capacities. Recent years have witnessed an increasing number of researchers and practitioners flexibly adapting PCIT to effectively treat early child internalizing problems (e.g., Carpenter et al., 2014; Chronis-Tuscano et al., 2015; Comer et al., 2012; Luby, Lenze, & Tillman, 2012; Pincus, Santucci, Ehrenreich, & Eyberg, 2008; Puliafico, Comer & Pincus, 2012).
The structure of the IGBT evaluated in this trial entailed 5 consecutive days of 6–8-hour daily treatment: Monday through Friday child group treatment sessions were held from 9am to 3pm; Monday through Thursday group parent training sessions were held from 3pm to 5pm. Each IGBT classroom contained roughly 10 children of similar ages. IGBT entailed a ratio of one counselor (i.e., trained volunteer or therapist) to one child, and at least one masters-level therapist supervised each classroom under the higher supervision of a licensed clinical psychologist. To simulate a classroom/camp setting, the IGBT daily structure included activities typical of an early child school setting (e.g., daily morning meeting, lunch, recess, art, field trips to the community). On each of the first four treatment days, parents participated in 2 hours of group parent training in which they received psychoeducation about SM, were taught interaction strategies for optimizing positive adult-child relationships and eliciting verbal behavior from their child (further described below), and guided through role-plays of these strategies. Further, parents were coached in-vivo with their child by a therapist in the implementation of these skills in real-life situations (e.g., ordering from a store, asking to call a parent from the school main office).
Staff were trained to use two specific sets of skills to interact with and elicit verbal behavior from children throughout treatment. The first set of skills—Child Directed Interaction (CDI) skills—focused on positive attending skills, and were drawn directly from standard PCIT (Funderburk & Eyberg, 2011) to break negative reinforcement patterns and to promote a positive therapist-child relationship. As in standard PCIT, CDI-based interactions have the child lead play while the adult uses labeled praise (e.g., “Thank you for answering me”), behavioral description (e.g., “I see you pointing to the blocks”), and verbal reflection (e.g., child says “I want to draw”; adult says “you said you want to draw”) skills to reinforce appropriate and desired child behavior. When treating SM, these desired child behaviors include participation, interaction, or incidental and/or spontaneous verbal behavior. During CDI, adults also fully avoid asking any questions of the child, avoid any critical or negative statements, and practice active ignoring of unwanted child behaviors—when treating SM, such unwanted behaviors include hiding, clinging, behavioral inhibition, miming, whining, and other displays of anxious, or withdrawn behavior. CDI skills are used exclusively when a staff member initially meets a child, so as to let the child lead the interactions and build a positive relationship without placing initial pressure on the child to speak/interact, and are then interwoven throughout the staff’s remaining time interacting with the child.
The second set of skills—Verbal Directed Interaction (VDI) skills (see Carpenter et al., 2014)—were used to directly prompt for and reinforce child verbalizations in ways that optimize the likelihood of eliciting a verbal response. In VDI, IGBT staff fully refrain from asking questions that can be answered non-verbally, such as yes/no questions (which can be answered with a head nod). When directly eliciting speech from the child, staff are trained to ask forced-choice questions (e.g., “Do you want to play with blocks or crayons?”) and/or give direct commands to verbally respond, leaving ample opportunity for response (i.e., at least 5 seconds), and differentially following through with either reinforcement for verbal behavior (e.g., labeled praise, sticker) or with re-prompting if the child is non-verbal or gestures his/her response. Children are graduated to more challenging question types (e.g., open-ended) as they progress through treatment. For more in-depth coverage of CDI and VDI sequences for children with SM, please see Furr and colleagues (in press).
Throughout the treatment week, exposure-based strategies focused on verbalizations and social situations (e.g., asking to go to the bathroom, speaking to peers at recess) were woven into classroom activities in a graduated fashion, with exposure demands becoming more challenging each day. The following treatment techniques were employed: reinforcement (rewarding target behaviors, such as verbalizing, with tangible reinforcements, such as checks on a chart or stickers), prompting (giving child cues to use speech in certain situations), shaping (gradually training the child to use speech by breaking down target situations into multiple steps), stimulus fading (gradually introducing new individuals to promote child speech with new people), graduated exposure (gradually increasing difficulty of each exposure throughout the week), social skills training (teaching children appropriate social skills to use with other peers and adults), cognitive strategies (providing psychoeducation about anxiety, teaching children how to identify maladaptive thinking patterns and generate more adaptive coping thoughts in a developmentally sensitive way), relaxation training, and modeling (having other children and adults display appropriate, adaptive verbal behavior).
WLP.
WLP participants were assigned to a 4-week waitlist. On the first day of the initial IGBT, WLP parents received (via email) the same psychoeducational information that IGBT parents received on their first day of IGBT. Specifically, parents were provided with a one-page psychoeducational informational brochure on the nature of SM (e.g., prevalence, diagnostic information). Four weeks following the initial IGBT, a second IGBT was offered for WLP families.
Staff Training
Program staff consisted of a licensed clinical psychologist, multiple doctoral- or masters-level clinicians, and undergraduate or post-baccalaureate volunteers. All staff underwent two 6-hour didactic trainings led by the licensed clinical psychologist and participated in five 1.5-hour weekly group meetings during the pre-treatment months to practice IGBT skills in role-plays. Before being paired with a child and participating as a counselor in the treatment program, each treatment staff member was required to demonstrate proficient CDI and VDI skill use (i.e., at least five labeled praises, five behavioral descriptions, five reflections and two or fewer commands, negative talk, or questions in a 2.5-minute time frame; and at least 80% effective questions/commands for verbalization sequences in a second 2.5-minute time frame). IGBT staff members were each coded at random once during the treatment week to assess adherence to the IGBT treatment protocol; adherence checks were conducted by the study PI and the clinical director of the program. All staff met pre-study fidelity criteria, as well as the IGBT-week fidelity check—i.e., using treatment skills for >80% of child-focused verbalizations and using non-skills for <20% of child-focused verbalizations (Mskills = 93.11%, SDskills = 7.15%; Mnon-skills = 6.87%, SDnon-skills = 7.16%).
Assessments
Diagnostic information.
Child diagnoses were determined using the Anxiety Disorders Interview Schedule for Children-Parent Version (ADIS; Silverman & Albano, 1997), a widely used semi-structured diagnostic interview administered to parents to assess present-state DSM-5-based internalizing and externalizing disorders. The ADIS has demonstrated strong reliability, validity, and sensitivity to change (Silverman & Ollendick, 2005; Wood, Piacentini, Bergman, McCracken, & Barrios, 2002). Independent evaluators (IEs) were trained according to ADIS training standards reported elsewhere (see Albano & Silverman, 1996). For each diagnosis, IEs assigned a clinical severity rating (CSR) ranging from 0 (no symptoms) to 8 (extremely severe symptoms). CSRs ≥4 indicate that diagnostic criteria for a particular disorder have been met. ADIS diagnostic profiles were generated at Baseline, Week 4, and SYF; at Week 4 these profiles were generated by IEs masked to whether youth participated in IGBT or WLP. All ADIS assessments following the Baseline ADIS only consisted of administration of diagnostic sections that were initially assigned a CSR of 1 or greater. Consistent parent informants participated across time points. Clinic reliability checks on ADIS assessments have yielded high interrater reliability (κ>.80).
Treatment responder status.
The Clinical Global Impression-Improvement Scale (CGI-I; Guy & Bonato, 1970) is a widely used generic clinician-rated measure of treatment-related change. The CGI-I rates improvement on a 7-point Likert scale ranging from 1 (“very much improved”) to 7 (“very much worse”), where 4 represents “no change.” Consistent with the child literature (e.g., Comer et al., 2017; Walkup et al., 2008), children assigned a CGI-I score of 1 (“very much improved”) or 2 (“much improved”) were classified as “treatment responders.” CGI-I scores were assigned at Week 4, and SYF; at Week 4, these scores were assigned by IEs masked to whether youth participated in IGBT or WLP.
Child SM symptoms and verbal behavior.
SM symptoms were assessed using the Selective Mutism Questionnaire (SMQ; Bergman, Keller, Piacentini, & Bergman, 2008), a 23-item parent-report measure of SM symptoms and verbal behavior across settings. The SMQ Home, Social and School subscales were used in this study. Items are rated on a 4-point scale ranging from 0 (never) to 3 (always); subscale scores represent the mean response across items in that subscale (range: 0–3). The SMQ has shown good reliability, validity, and sensitivity to treatment-related change (Bergman et al., 2008; Bergman, Gonzalez, PIacentini, & Keller, 2013; Letamendi et al., 2008; α = .80 in present sample). The SMQ was administered at Baseline, Week 4, and SYF. Given that IGBT occurred over the summer break, parents could not report on children’s school verbal behavior immediately following treatment. Accordingly, the SMQ School subscale was only examined at Baseline and SYF in the pooled sample of treated youth.
The School Speech Questionnaire (SSQ; Bergman et al., 2002) is an 8-item teacher-report of child verbal behavior in the school setting, adapted from the SMQ. Only the severity items were used for the purpose of this study; items are also rated on a 4-point Likert-style scale ranging from 0 (never) to 3 (always); a total score reflects the mean response across all SSQ items (range: 0–3). The SSQ has demonstrated acceptable reliability and sensitivity to treatment-related change (Bergman et al., 2002; Bergman et al., 2013; Oerbeck et al., 2014; α = .81 in present sample). The SSQ was administered to teachers during the pre-treatment school year and at the SYF assessment. Given that Baseline and SYF data were collected across two different school years, reporting teachers were different for these two assessments.
Child anxiety.
The Child Behavior Checklist (CBCL; Achenbach & Rescorla, 2001) is a standardized parent-report assessing child behavioral and emotional problems. Parents rate each item on a 3-point Likert-style scale ranging from 0 (not true) to 2 (very true or often true). Scores are normed by age and sex to yield subscale T-scores reflecting a range of psychopathology domains. For the present study, CBCL Anxiety Problems T-scores were used to measure overall child anxiety at Baseline, Week 4, and SYF. Depending on the age of the child, parents completed the CBCL 1.5–5 (Achenbach & Rescorla, 2000; for children <6 years) or the CBCL 6–18 (Achenbach & Rescorla, 2001; for children ≥6 years). The CBCL Anxiety Problems subscale has demonstrated strong reliability and validity in previous literature (e.g., Achenbach, Dumenci, & Rescorla, 2003; Nakamura, Ebesutani, Bernstein & Chorpita, 2009; CBCL 1.5–5 α = .90 and CBCL 6–18 α = .79 in present sample).
Global functioning.
Overall functioning was measured using the Children’s Global Assessment Scale (CGAS; Shaffer et al., 1983). The CGAS is a widely used clinician-rated measure rating global child functioning, impairment, and life disturbance on a scale of 0 to 100, with lower scores indicating greater functional impairments and higher scores indicating better functioning. The CGAS has been successfully used with child populations in this age range (e.g., Comer et al., 2014). CGAS scores were assigned at Baseline, Week 4, and SYF; at Week 4 scores were assigned by IEs masked to whether youth were in IGBT or WLP.
School/academic impairment.
The Impairment Rating Scale (IRS; Fabiano et al., 2006) teacher-version was used to measure child impairment and academic functioning as a function of their current problem (i.e., SM) in the school setting. The IRS was originally developed to measure impairment in youth with ADHD, however items are worded non-specifically so that teachers can report on other child “problems.” Sample items include “How does this child’s problems affect his or her relationship with other children?” and “How does this child’s problems affect his or her academic progress?” Seven of the 8 items are rated on a 7-point Likert-style scale ranging from 0 (No Problem) to 6 (Extreme Problem). The 8-item measure has demonstrated good concurrent, convergent, and discriminant validity in children with ADHD (Fabiano et al., 2006; α = .77 in present sample).
Treatment satisfaction.
Parent satisfaction was measured using the Client Satisfaction Questionnaire (CSQ; Larsen, Attkisson, Hargreaves, & Nguyen, 1979), a frequently used measure of satisfaction with treatment services. The CSQ contains 8-items, each rated on a 4-point scale, and has demonstrated good validity with a variety of clinical populations (Larsen et al., 1979; Atkisson & Zwick, 1982), including parents of children with mental health needs (Byalin, 1993).
Barriers to treatment participation.
Barriers to treatment participation were measured using the Barriers to Treatment Participation Scale (BTPS, Kazdin et al., 1997), a 58-item parent-report inquiring about how often various potential barriers were a problem for parents participating in a particular treatment service. Items are each rated on a 5-point Likert-style scale ranging from 1 (never a problem) to 5 (very often a problem). Four subscales are generated from the BTPS: Stressors and obstacles that compete with treatment, Treatment demands and issues, Perceived relevance of treatment, and Relationship with the therapist. The BTPS has demonstrated good reliability and validity (Colonna-Pydyn, Giesfield, & Greeno, 2007; Kazdin et al., 1997; α = .62 in present sample).
Recent service use.
Given the naturalistic follow-up component of this study, a brief measure to assess service use between the post-treatment assessment and SYF assessment was administered to parents. Parents reported if they received any of the following services post-treatment targeting their child’s SM: starting or change in medication, family therapy, child therapy, parent-focused therapy, group therapy. Any service use (i.e., “Has your family received mental health services for your child’s behavior or anxiety since August 16th, 2017? Yes or No?”) was controlled for in follow-up analyses.
Data Analyses
Descriptive statistics characterized baseline demographic and clinical characteristics of the sample, as well as feasibility, satisfaction, barriers to treatment participation, diagnostic remission, and response rates. T-tests and chi-square analyses tested for baseline differences between conditions in order to confirm successful randomization, as well as to compare diagnostic remission and treatment response rates between conditions. To examine between-group changes on continuous measures from Baseline to Week 4, two-way mixed analyses of variance (ANOVAs) examined changes between conditions (IGBT vs. WLP) and across time. Specifically 2 (Time, within-subjects) × 2 (Condition, between-subjects) factorial ANOVAs were conducted for each continuous outcome. The effects of Time, Condition, and Time×Condition interactions were evaluated, with significant Time×Condition interactions reflecting that symptom changes from baseline to Week 4 were not uniform across children in IGBT versus WLP.
To examine relatively longer lasting treatment-related changes that extended into the following school year, data were pooled together across conditions (as both conditions had completed IGBT by the following school year). For outcomes measured at three time points (i.e., baseline, post-treatment, and SYF), hierarchical linear modeling (HLM) was used to examine changes. HLM uses maximum-likelihood estimation of parameters in order to account for missing data. For each model, the Akaike Information Criterion (AIC) value was used to determine which of three tested trajectory shapes (linear, quadratic, logarithmic) was the best-fitting trajectory type; lower AIC values indicate better fit. In these pooled analyses, Condition assignment was controlled for, as a level 1 covariate, to account for differential timing associated with immediate IGBT versus post-waitlist IGBT. Recent service use was also controlled for as a level 1 covariate. To examine changes in school speech behavior and academic/social impairment as reported by teachers and parents, two-way mixed analyses of variance (ANOVAs) examined changes across time controlling for Condition effect and controlling for the interaction effect, Time×Condition. Specifically 2 (Time, within-subjects) × 2 (Condition, between-subjects) factorial ANOVAs were conducted for parent-reported verbal behavior in school and teacher-reported verbal behavior and academic/social impairment.
Results
Feasibility & Satisfaction
IGBT Feasibility.
100% of families randomized to IGBT completed treatment, and 86.7% of WLP families participated in IGBT after the 4-week waitlist period (2 WLP families declined to participate in IGBT after the 4-week waitlist). Families across both conditions who participated in IGBT (whether before or after the waitlist) had a 100% attendance rate, with zero no-shows or missed treatment days across participants.
Parents reported minimal barriers to IGBT participation. Specifically, IGBT-treated parents reported a mean Total barriers score of 50.54 (SD=4.64) on the BTPS (range of possible Total BTPS scores: 47 – 220). Scores were also very low on each of the BTPS subscales: Stressors and obstacles that compete with treatment (M = 28.83, SD = 2.91; range of possible scores: 20 –100), Treatment demands and issues (M = 11.33, SD = 1.46; range of possible scores: 10 – 50), Problems in perceived relevance of treatment (M = 9.25, SD = 1.36; range of possible scores: 8 – 40), and Problems in relationship with the therapist(s) (M = 6.13, SD = .34; range of possible scores: 6 – 30).
Satisfaction.
Parents reported very high rates of satisfaction with IGBT (including IGBT parents and WLP parents who filled out CSQ post-treatment) – mean post-IGBT Total CSQ-8 score was 30.46 out of a total possible 36. Of the parents who filled out the CSQ-8 (n = 26), 96.2% of parents rated the quality of the services they received as “excellent” and the remaining 3.8% of parents rated the quality of the services they received as “good.” One hundred percent of parents reported that they received the kind of services they wanted. All parents reported “most” or “almost all” of their needs had been met, and 100% reported that they would recommend IGBT if a friend were in need of similar help. Roughly three-fourths of parents (i.e., 76.9%) reported they were “very satisfied” with IGBT and 19.2% reported they were “mostly satisfied.” All parents reported that they would participate again in IGBT if they needed further help for their child in the future.
Outcomes Through Week 4
Table 2 presents baseline and Week 4 outcome data, broken down by condition.
Table 2.
Details of IE-assigned and parent-reported outcomes at Baseline and Week 4
| IGBT (n=14) | WLP (n=15) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | Week 4 | Baseline | Week 4 | |||||||
| % | N | % | N | % | N | % | N | Significance test | Effect Size | |
| Treatment responder1 | Fisher’s exact test: p = .006** | Phi = −.58 | ||||||||
| Yes | 0.0 | 0 | 50.0 | 7 | 0.0 | 0 | 0.0 | 0 | ||
| No | 100.0 | 14 | 50.0 | 7 | 100.0 | 15 | 100.0 | 15 | ||
| SM diagnostic criteria met | Fisher’s exact test: p = 1.00 | Phi = .19 | ||||||||
| Yes | 100.0 | 14 | 92.9 | 13 | 100.0 | 15 | 100.0 | 15 | ||
| No | 0.0 | 0 | 7.1 | 1 | 0.0 | 0 | 0 | 0 | ||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Time × Condition Interaction Effect | Effect Size | |
| SM CSR | 4.9 | 0.8 | 4.2 | 0.9 | 4.9 | 0.7 | 4.6 | 0.7 | F(1,26) = 2.31 | d = −.50 |
| Social anxiety CSR | 4.8 | 1.2 | 4.0 | 0.8 | 3.6 | 1.6 | 3.6 | 1.5 | F(1,26) = 5.37* | d = −.50 |
| Parent-report SMQ | ||||||||||
| SM Home Subscale | 2.0 | 0.7 | 2.2 | 0.4 | 1.9 | 0.8 | 1.7 | 0.7 | F(1,25) = 3.47 | d = .36 |
| SM Social Subscale | 0.8 | 0.5 | 1.2 | 0.6 | 0.6 | 0.7 | 0.7 | 0.7 | F(1,25) = 5.35* | d = .58 |
| Parent-report CBCL | ||||||||||
| Anxiety Problems T-score | 65.7 | 8.9 | 61.6 | 7.7 | 60.9 | 9.8 | 59.4 | 11.2 | F(1,25) = .99 | d = −.28 |
| Global functioning (CGAS score) | 48.9 | 5.5 | 53.6 | 4.6 | 51.5 | 4.7 | 52.5 | 4.9 | F(1,26) = 12.64** | d = .73 |
Note: IGBT = intensive group behavior treatment; WLP = 4-week waitlist with psychoeducational resources; SM= selective mutism; CSR = clinical severity rating, assigned via the Anxiety Disorders Interview Schedule (ADIS) for Children-Parent Version; SMQ = Selective Mutism Questionnaire; CBCL = Child Behavior Checklist; CGAS = Children’s Global Assessment Scale (0–100; lower scores indicating greater functional impairments).
“Treatment responder” = Score of 1 or 2 on the CGI-I as rated by masked independent evaluator (IE)
p<.05,
p<.01
Responder status and diagnostic outcomes.
At Week 4, a significantly greater proportion of IGBT children than WLP children were classified as “responders” (i.e., CGII = 1 or 2) by an IE masked to treatment condition. Specifically, 50% of children in the IGBT condition were classified as “responders,” whereas 0% of WLP children were classified as “responders” (see Table 2). That said, full SM diagnostic remission by Week 4 was rare, with only 7.1% of IGBT children and 0% of WLP children classified as “SM diagnosis free” at Week 4; diagnostic remission rates at Week 4 did not significantly differ between conditions (see Table 2).
Continuous outcomes.
Two-way mixed ANOVAs examined the extent to which Time (within-subjects), Condition (between-subjects), and Time×Condition (mixed) interactions predicted continuous outcomes measured at both baseline and Week 4. Parent-reported SM symptoms in social settings (i.e., SMQ Social), IE-rated social anxiety severity (i.e., social anxiety CSR), and IE-rated global functioning (i.e., CGAS) all showed significantly greater improvement from baseline to Week 4 among IGBT-treated children relative to WLP children (see Table 2). At Week 4, there were no observed effects of IGBT, relative to WLP, on SM CSR, SMQ Home subscale, and CBCL Anxiety subscale.
School Year Follow-Up Results
By 8 weeks into the start of the following school year (after which children in both conditions had participated in IGBT and thus data across conditions were pooled), 45.8% of children (n = 11) who completed SYF assessments (n = 24; 5 participating parents lost to follow-up) were free of an SM diagnosis and 62.5% of children (n = 15) were considered “treatment responders.” Forty-two percent of youth were free of a SocAD diagnosis (compared to only 27.5% at baseline and 37% at post-treatment). Twenty-eight percent of participating families received services between completion of treatment (i.e., following their post-treatment assessment) and SYF. Accordingly, interim service use was controlled for in all HLMs.
Table 3 presents baseline to SYF data among the pooled sample of IGBT-treated youth (combining the data of IGBT youth with the data of WLP youth who participated in IGBT following a 4-week waitlist).
Table 3.
Baseline to School-Year Follow-Up (SYF) data among pooled sample of IGBT-treated youth (N=29)
| Baseline (n=29) | Post-Treatment1 (n=27) | SYF (n=24) | ||||
|---|---|---|---|---|---|---|
| % | N | % | N | % | N | |
| T reatment responder2 | ||||||
| Yes | 0 | 0 | 55.1 | 16 | 62.5 | 15 |
| No | 100 | 29 | 37.9 | 11 | 37.5 | 9 |
| SM diagnostic criteria met | ||||||
| Yes | 100 | 29 | 81.5 | 22 | 45.8 | 11 |
| No | 0 | 0 | 18.5 | 5 | 54.2 | 13 |
| SocAD diagnostic criteria met | ||||||
| Yes | 72.5 | 21 | 63.0 | 17 | 58.3 | 14 |
| No | 27.5 | 8 | 37.0 | 10 | 41.7 | 10 |
| Mean | SD | Mean | SD | Mean | SD | |
| SM CSR | 4.7 | 0.7 | 4.4 | 1.0 | 3.6 | 1.1 |
| Social anxiety CSR | 4.2 | 1.5 | 3.7 | 1.2 | 3.5 | 1.2 |
| Parent-report SMQ | ||||||
| SM Home Subscale | 1.9 | 0.7 | 2.2 | 0.4 | 2.2 | 0.6 |
| SM Social Subscale | 0.7 | 0.6 | 1.2 | 0.7 | 1.5 | 0.8 |
| Parent-report CBCL | ||||||
| Anxiety Problems T-score | 62.7 | 10.4 | 59.8 | 7.6 | 58.6 | 7.2 |
| Teacher-report SSQ Total3 | 1.1 | 0.7 | - | - | 1.6 | 0.7 |
| Teacher-report IRS Total score3 | 3.1 | 1.0 | - | - | 1.5 | 1.3 |
| Global functioning (CGAS score) | 50.7 | 5.5 | 55.1 | 4.7 | 57.3 | 4.3 |
Note: SYF = School year follow-up (8 weeks into following school year); IGBT = intensive group behavior treatment; SM = selective mutism; CSR = clinical severity rating, assigned via the Anxiety Disorders Interview Schedule (ADIS) for Children-Parent Version; SocAD = Social Anxiety Disorder; SMQ = Selective Mutism Questionnaire; CBCL = Child Behavior Checklist; SSQ = School Speech Questionnaire (higher scores = more verbal behavior); IRS = Impairment Rating Scale (higher scores = more impairment); CGAS = Children’s Global Assessment Scale (0–100; lower scores indicating greater functional impairments).
In this pooled sample of IGBT-treated youth, Post-Treatment data refers to post-IGBT data (i.e., Week 4 data for IGBT youth; Week 8 data for WLP youth)
“Treatment responder” = Score of 1 or 2 on the CGI-I as rated by masked independent evaluator (IE)
Based on sample subset with teacher-report data (baseline n = 25; SYF n = 16)
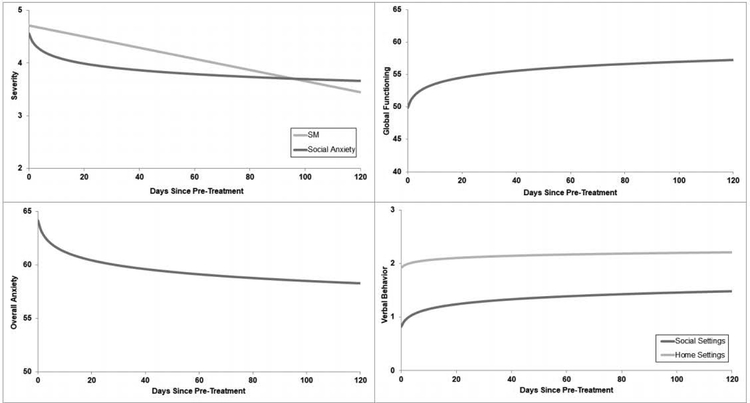
HLMs controlling for Condition (immediate IGBT or post-waitlist IGBT) and recent service use examined changes from pre-treatment through post-treatment and into SYF in SM severity (CSR), SocAD CSR, global functioning (CGAS), overall anxiety (CBCL Anxiety Problems), verbal behavior in “home” settings (SMQ Home), and verbal behavior in social settings (SMQ Social). Linear, quadratic, and logarithmic slopes were tested for each outcome, with the AIC (lower = better fit) used to determine which slope was the best fitting slope to the data. The best-fitting models, according to AIC, showed: (a) significant linear decrease over time in SM severity (AIC = 178.01; b(44.27) = −.01, p < .001; 95% CI [−.013, −.007]); (b) significant logarithmic decrease over time in social anxiety severity (AIC = 192.19; b(44.04) = −.19, p < .001; 95% CI [−.28, −.09]); (c) significant logarithmic improvement over time in global functioning (AIC = 399.93; b(44.06) = 1.54, p < .001; 95% CI [1.06, 2.00]); (d) significant logarithmic decrease over time in overall anxiety symptoms (AIC = 434.80; b(42.57) = −1.22, p = .001; 95% CI [−1.92, −.52]); (e) significant logarithmic improvement over time in verbal behavior in “home” settings (AIC = 95.72; b(41.80) = .06, p = .005; 95% CI [.010, .102]); and (f) significant logarithmic improvement in verbal behavior in social settings (AIC = 117.75; b(41.26) = .14, p < .001; 95% CI [.084, .191]). Figure 2 graphically presents all of these significant trajectories.
Figure 2.
Trajectories of change from pre-treatment through SYF
SM: Selective mutism
Notes: SM and Social Anxiety severity measured by masked Independent Evaluator (IE)-rated Clinical Severity Rating; Global Functioning measured by masked IE-rated Children’s Global Assessment Scale; Overall Anxiety, measured by Parent-report CBCL Anxiety Problems T-score; Verbal Behavior in “home” and “social” settings measured by the parent-reported Selective Mutism Questionnaire.
Two-way mixed ANOVAs examined the extent to which Time (within-subjects), controlling for Condition (between-subjects) and Time×Condition (mixed) interaction, predicted parent-reported verbal behavior in school measured at both baseline and SYF. Results indicated a significant effect of Time (F(1,20) = 18.62, p < .001), suggesting that parent-reported verbal behavior in school improved across children treated in both immediate and post-WLP IGBT from baseline to SYF. There was no Time×Condition effect (F(1,20) = .05, p = .832), suggesting that the timing of IGBT (i.e., early versus later in the summer) did not differentially predict SYF parent-reported verbal behavior in school.
Regarding teacher-reported change, two-way mixed ANOVAs examined the extent to which Time (within-subjects), controlling for Condition (between-subjects) and Time×Condition (mixed) interactions, predicted teacher-reported verbal behavior in school and teacher-reported academic/social impairment measured at both baseline and SYF. Results indicated a significant effect of Time (F(1,10) = 6.06, p = .034), on teacher-reported verbal behavior, suggesting that teacher-reported verbal behavior in school improved across children treated in both immediate and post-WLP IGBT from baseline to SYF. There was no Time×Condition effect (F(1,10) = .22, p = .65), suggesting that the timing of IGBT (i.e., early versus later in the summer) did not differentially predict SYF teacher-reported verbal behavior in school. Similarly, there was a significant effect of Time (F(1,10) = 18.82, p = .001) on teacher-reported academic/social impairment, suggesting that teacher-reported academic/social impairment in school improved across children treated in both immediate and post-WLP IGBT from baseline to SYF. Again, there was no Time×Condition effect (F(1,10) = 2.81, p = .125), suggesting that the timing of IGBT (i.e., early versus later in the summer) did not differentially predict SYF teacher-reported academic/social impairment in school.
Discussion
Whereas recent years have witnessed a very small handful of controlled trials evaluating weekly treatment for childhood SM (e.g., Bergman et al., 2013; Bunnell, Mesa, & Beidel, 2018; Oerbeck et al., 2014), the present study offers the first randomized controlled trial to evaluate an intensive treatment format for children with SM. Results provide promising support for the feasibility, acceptability, and preliminary efficacy of a 5-day IGBT for children with SM aged 5–9. Whereas 50% of children randomized to participate in IGBT were classified four weeks later by an IE as a “responder,” no child randomized to waitlist with self-directed psychoeducation was classified as such. These findings are consistent with a growing body of literature supporting the very favorable role brief intensive treatment formats can play in broadening the portfolio of treatment options for a range of child anxiety and related problems (Gallo et al., 2014; Ollendick, 2014; Öst & Ollendick, 2017; Santucci et al., 2009; Storch et al., 2007). The continued improvements observed into the following school year are also consistent with Öst and Ollendick’s recent meta-analysis (2017) which reported that remission rates for intensive treatment programs for anxiety-related problems tend to rise even higher at follow-ups relative to post-treatment assessments. The present findings are especially encouraging given the lack of available, evidence-based SM treatment options.
Despite half of the IGBT-treated sample being classified as a “responder” at Week 4 by an IE masked to treatment condition, a relatively low percentage of children (i.e., 7.1%) was free of SM diagnosis at Week 4. This finding, when considered against the large effect sizes in measures of parent-reported SM symptoms and other IE-rated measures (e.g., global functioning), underscores how meaningfully symptoms can improve while a child still meets diagnostic criteria for SM. Importantly, almost half of treated children were free of an SM diagnosis by the follow-up assessment conducted 8 weeks into the following school year. This may reflect the extent to which a 4-week time period may be too brief of a period of time in which to exhibit or detect full remission of SM diagnosis. On the other hand, it is possible that more substantial remission in symptoms can only occur as children and parents apply treatment skills after intensive treatment in their own natural environments and particularly in the school setting.
The present study observed broad improvements in social anxiety severity as a result of participating in IGBT. At the Week 4 assessment, IGBT demonstrated an effect on social anxiety severity, as rated by a masked IE, but no effect on masked IE-rated SM severity. This finding was surprising given that IGBT is designed to directly target SM symptoms, with social anxiety symptoms expected to improve collaterally. The present pattern of findings may highlight the potential obstinacy of SM symptomology relative to social anxiety symptoms. The definition of SocAD is inherently fear-centric, whereas the definition of SM is behavior-centric. Specifically, DSM-5 requires fear to be present in order for an individual to meet diagnostic criteria for SocAD, whereas diagnostic criteria for SM only requires that behavior (i.e., extreme verbal avoidance), but not necessarily fear, be present (American Psychiatric Association, 2013). It is possible that improvements in child fear occur at a faster rate than improvements in associated child behavior. Alternatively, it may be challenging to fully appreciate children’s improvements in verbal behavior over the summer when children are not in the settings in which their verbal behavior, or lack thereof, may be most pronounced (i.e., school).
Parent reports of child verbal behavior in school and teacher reports of child verbal behavior and social/academic functioning indicated significant improvements from the school year that preceded the summer IGBT to the school year that followed the IGBT. Specifically, there were significant differences across the two school years in regards to verbal child behavior and social/academic functioning. An important limitation of these findings based on teacher-reports is that, out of necessity, different teachers reported on each child in the years before and following IGBT. That said, many anxious children may experience more severe anxiety in the early months—relative to later months—of a school year as they become acclimated to a new environment, peers, and teachers. Accordingly, one might actually expect that, in the absence of intervention, teacher-reported child anxiety in the early months of a school year would be higher than teacher-reported child anxiety in the later months of a school year; indeed the presently documented teacher-reported improvements in treated children’s classroom verbal behavior from spring to fall may be particularly encouraging. Nonetheless, it is possible that a new school year may simply presented an opportunity for children with SM to have a “fresh start” for speaking in a new setting.
In addition to positive symptom improvements and functional outcomes associated with IGBT, the present study also observed family satisfaction to be very high and perceived barriers to treatment participation to be very low. These findings are consistent with the growing body of literature documenting high satisfaction with intensive treatment formats for a range of child mental health problems, including anxiety (e.g., Jensen et al., 2001; Ollendick et al., 2009, 2015; Santucci et al., 2009).
Although the present study speaks to many positive outcomes associated with IGBT for SM, including high family satisfaction, it is important to note that participation in a destination intensive treatment program can entail considerable out-of-pocket costs associated with travel and lodging. The present sample had a relatively high mean household income (M = $88,303) and reported very low barriers to treatment participation. Despite the efficacy and satisfaction associated with IGBT, the added costs associated with this unique treatment format (both financial costs and other potential barriers) may be prohibitive for some families in need. Although the present study did not have funding to offer assistance (e.g., housing, travel support) to families, intensive treatment programs could be developed in creative ways in order to help bring down associated out-of-pocket costs (e.g., holding intensive programs on academic campuses that can offer families temporary housing in dormitory space). There is also a need to simultaneously explore other innovative treatment formats that can also address geographic and cost limitations in quality care options.
In recent years, an increasing body of work has examined the merits of leveraging remote technologies to improve the reach of quality mental health care (Comer & Barlow, 2014; Comer et al., 2017; Doss, Feinberg, Rothman, Roddy, & Comer, 2017; Kazdin & Blase, 2011), and some recent work has begun to examine the role of technology in the specific treatment of childhood SM. For example, Bunnell and colleagues (2018) demonstrated support for the use of mobile apps to promote verbalizations in children with SM, and Ooi and colleagues (2016) showed that web-based intervention strategies, where children interact with a therapist via videoteleconferencing, can also be beneficial in reducing symptoms. As a portfolio of alternative treatment options showing support for the treatment of SM unfold, future work should consider sequential, multiple assignment, randomized trial (SMART) designs to determine which innovative treatment strategies and formats (e.g., traditional weekly treatments, intensive formats, videoteleconferencing, apps) work for which children affected by SM, and in which sequences.
The present study has several limitations that warrant comment. First, our sample size was relatively small, prohibiting the evaluation of mediators and moderators that could help identify causal accounts of IGBT effects, uncover key mechanisms of IGBT-related change, and clarify for whom IGBT may be most well-suited. Second, because Week 4 assessments occurred during the summer months, it was not possible to evaluate the acute effects of IGBT on school-based verbal behavior, performance, and anxiety. Relatedly, at Week 4 it is possible that parents and children did not have an adequate amount of time to re-immerse themselves in regular social activities (e.g., camp, extracurriculars, playdates) after attending the program, and thus parents may not have been able to observe and accurately report on IGBT-related improvements. Future work might do well to examine IGBT during school breaks (e.g., winter break, spring break), which would allow treated children to still participate without missing school days, but would allow them to immediately apply and demonstrate their new skills in the most relevant and impairing settings. Third, given that WLP families were offered IGBT after completing the 4-week waitlist period, it was not possible to evaluate between-group effects into the following school year. Accordingly it is possible that some of the improvements between Week 4 and SYF were related to the passage of time rather than to IGBT specifically, although the work of Bergman and colleagues (2013) and Oerbeck and colleagues (2014) suggests that SM remission would be unlikely across this time frame in the absence of intervention. Fourth, waitlist-randomized trials control for the passage of time and patient expectancies, but future evaluations incorporating more rigorous comparison groups are needed. Fifth, behavioral observations were not included in the present analysis. Sixth, the IRS has been previously evaluated in youth with ADHD, but its psychometric properties in anxious youth have not been tested; moreover the internal consistency for the BTPS was somewhat low. Seventh, the present study did not collect qualitative data which could have captured richer information about satisfaction and acceptability from the patient/family perspective. Future mixed-methods evaluations will be informative on this front. Lastly, children in the present study participated in treatment in different classrooms (i.e., determined by age), with each classroom having its own staff and peers. The present study was not powered to accommodate multi-level modeling approaches that would account for potential effects nested within classrooms.
Despite these limitations, the present study offers the first controlled data supporting the promise of IGBT for the treatment of childhood SM. In the context of this initial waitlist-controlled trial, the present study found children treated with one week of IGBT showed significant improvements one month later relative to children on a four-week waitlist whose parents received psychoeducational resources. Treated families participation, and IGBT-related child outcomes continued to improve into the following school year. Research is now needed to further evaluate IGBT against increasingly rigorous comparison conditions (e.g., 1-week group summer camp programs that do not explicitly focus on promoting child verbal behavior; or weekly CBT), and to incorporate additional controlled follow-up assessments to examine longer-term maintenance of IGBT-related gains. Future efforts are needed to standardize IGBT training materials and procedures in order to best disseminate IGBT to community settings. With continued support, IGBT may prove to be an important evidence-based strategy in the portfolio of treatment options for children with SM, with the ability to extend the availability and acceptability of quality care for affected families who may lack SM treatment expertise in their local area.
Public health significance:
This is the first controlled trial evaluating intensive group behavioral treatment (IGBT) for selective mutism. Results suggest IGBT may be an effective and acceptable treatment option for children with selective mutism. In particular, IGBT may be a feasible “destination” treatment option for affected children dwelling in regions lacking local selective mutism expert care.
Acknowledgments:
The authors would like to thank Dr. Jeremy Pettit, Dr. Katie Hart, and Dr. Elizabeth Cramer for their guidance on and contributions to this research.
Funding: This work was supported by the National Institute of Health (F31 MH112296) zand the American Psychological Association Division 53 Society for Clinical Child and Adolescent Psychology
References
- Achenbach TM, Dumenci L, & Rescorla LA (2003). DSM-oriented and empirically based approaches to constructing scales from the same item pools. Journal of clinical child and adolescent psychology, 32(3), 328–340. 10.1207/S15374424JCCP3203_02 [DOI] [PubMed] [Google Scholar]
- Achenbach TM, & Rescorla LA (2000). Manual for the ASEBA preschool forms and profiles. Burlington, VT: University of Vermont, Research center for children, youth, & families. [Google Scholar]
- Achenbach TM, Rescorla LA (2001). Manual for the ASEBA school-age forms & profiles. Burlington, VM: University of Vermont, Research Center for Children, Youth, and Families. [Google Scholar]
- Albano AM, & Silverman WK (1996). Anxiety Disorders Interview Schedule for DSM-IV-Child Version: Clinician Manual. Psychological Corporation. [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author; 10.1176/appi.books.9780890425596 [DOI] [Google Scholar]
- Attkisson CC, & Zwick R (1982). The Client Satisfaction Questionnaire: Psychometric properties and correlations with service utilization and psychotherapy outcome. Evaluation and program planning, 5(3), 233–237. 10.1016/0149-7189(82)90074-X [DOI] [PubMed] [Google Scholar]
- Bergman RL, Gonzalez A, Piacentini J, & Keller ML (2013). Integrated behavior therapy for selective mutism: A randomized controlled pilot study. Behaviour Research and Therapy, 51(10), 680–689. 10.1016/j.brat.2013.07.003 [DOI] [PubMed] [Google Scholar]
- Bergman RL, Keller ML, Piacentini J, & Bergman AJ (2008). The development and psychometric properties of the selective mutism questionnaire. Journal of Clinical Child & Adolescent Psychology, 37(2), 456–464. 10.1080/15374410801955805 [DOI] [PubMed] [Google Scholar]
- Bergman RL, Piacentini J, & McCracken JT (2002). Prevalence and description of selective mutism in a school-based sample. Journal of the American Academy of Child & Adolescent Psychiatry, 41(8), 938–946. 10.1097/00004583-200208000-00012 [DOI] [PubMed] [Google Scholar]
- Bogels SM, Alden L, Beidel DC, Clark LA, Pine DS, Stein MB, &Voncken M. (2010). Social anxiety disorder: Questions and answers for the DSM-V. Depression and Anxiety, 27, 168–189. 10.1002/da.20670 [DOI] [PubMed] [Google Scholar]
- Bunnell BE, Mesa F, & Beidel DC (2018). A Two-Session Hierarchy for Shaping Successive Approximations of Speech in Selective Mutism: Pilot Study of Mobile Apps and Mechanisms of Behavior Change. Behavior Therapy. 10.1016/j.beth.2018.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byalin K (1993). Assessing parental satisfaction with children’s mental health services: A pilot study. Evaluation and Program Planning, 16(2), 69–72. 10.1016/0149-7189(93)90018-4 [DOI] [Google Scholar]
- Carbone D, Schmidt LA, Cunningham CC, McHolm AE, Edison S, Pierre JS, & Boyle MH (2010). Behavioral and socio-emotional functioning in children with selective mutism: A comparison with anxious and typically developing children across multiple informants. Journal of abnormal child psychology, 38(8), 1057–1067. 10.1007/s10802-010-9425-y [DOI] [PubMed] [Google Scholar]
- Carpenter AL, Puliafico AC, Kurtz SM, Pincus DB, & Comer JS (2014). Extending Parent–Child interaction therapy for early childhood internalizing problems: New advances for an overlooked population. Clinical Child and Family Psychology Review, 17(4), 340–356. 10.1007/s10567-014-0172-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chavira DA, Shipon-Blum E, Hitchcock C, Cohan S, & Stein MB (2007). Selective mutism and social anxiety disorder: all in the family?. Journal of the American Academy of Child & Adolescent Psychiatry, 46(11), 1464–1472. 10.1097/chi.0b013e318149366a [DOI] [PubMed] [Google Scholar]
- Chronis-Tuscano A, Rubin KH, O’Brien KA, Coplan RJ, Thomas SN, Dougherty LR, … & Wimsatt M (2015). Preliminary evaluation of a multimodal early intervention program for behaviorally inhibited preschoolers. Journal of Consulting and Clinical Psychology, 85, 534–540. 10.1037/a0039043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohan SL, Chavira DA, & Stein MB (2006). Practitioner review: Psychosocial interventions for children with selective mutism: A critical evaluation of the literature from 1990–2005. Journal of Child Psychology and Psychiatry, 47(11), 1085–1097. 10.1111/j.1469-7610.2006.01662.x [DOI] [PubMed] [Google Scholar]
- Colonna-Pydyn C, Gjesfjeld CD, & Greeno CG (2007). The factor structure of the Barriers to Treatment Participation Scale (BTPS): Implications for future barriers scale development. Administration and Policy in Mental Health and Mental Health Services Research, 34(6), 563–569. 10.1007/s10488-007-0139-6 [DOI] [PubMed] [Google Scholar]
- Comer JS, & Barlow DH (2014). The occasional case against broad dissemination and implementation: Retaining a role for specialty care in the delivery of psychological treatments. American Psychologist, 69(1), 1 10.1037/a0033582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comer JS, Furr JM, Cooper-Vince CE, Kerns CE, Chan PT, Edson AL, … Freeman JB. (2014). Internet-delivered, family-based treatment for early-onset OCD: A preliminary case series. Journal of Clinical Child & Adolescent Psychology, 43(1), 74–87. 10.1080/15374416.2013.855127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comer JS, Furr JM, Miguel E, Cooper-Vince CE, Carpenter AL, Elkins RM, Kerns C, Cornacchio D, Chou T, Coxe S, DeSerisy M, Sanchez AL, Golik A, Martin J, Myers K, & Chase R (2017). Remotely delivering real-time parent training to the home: An initial randomized trial of Internet-delivered Parent-Child Interaction Therapy (I-PCIT). Journal of Consulting and Clinical Psychology, 85, 909–917. 10.1037/ccp0000230 [DOI] [PubMed] [Google Scholar]
- Comer JS, Puliafico AC, Aschenbrand SG, McKnight K, Robin JA, Goldfine M, & Albano AM (2012). A pilot feasibility evaluation of the CALM Program for anxiety disorders in early childhood. Journal of Anxiety Disorders, 26, 40–49. 10.1016/j.janxdis.2011.08.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham CE, McHolm AE, & Boyle MH (2006). Social phobia, anxiety, oppositional behavior, social skills, and self-concept in children with specific selective mutism, generalized selective mutism, and community controls. European child & adolescent psychiatry, 15(5), 245–255. 10.1007/s00787-006-0529-4 [DOI] [PubMed] [Google Scholar]
- Doss BD, Feinberg LK, Rothman K, Roddy MK, & Comer JS (2017). Using technology to enhance and expand interventions for couples and families: Conceptual and methodological considerations. Journal of Family Psychology, 31(8), 983 10.1037/fam0000349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehrenreich JT, & Santucci LC (2009). Special series: Intensive cognitive-behavioral treatments for child and adolescent anxiety disorders. Cognitive and Behavioral Practice, 16(3), 290–293. 10.1016/j.cbpra.2009.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elizur Y, & Perednik R (2003). Prevalence and description of selective mutism in immigrant and native families: A controlled study. Journal of the American Academy of Child & Adolescent Psychiatry, 42(12), 1451–1459. 10.1097/00004583-200312000-00012 [DOI] [PubMed] [Google Scholar]
- Fabiano GA, Schatz NK, & Pelham WE (2014). Summer treatment programs for youth with ADHD. Child and adolescent psychiatric clinics of North America, 23(4), 757–773. 10.1016/j.chc.2014.05.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fabiano GA, Pelham J, William E, Waschbusch DA, Gnagy EM, Lahey BB, Chronis AM, … Burrows-MacLean L. (2006). A practical measure of impairment: Psychometric properties of the impairment rating scale in samples of children with attention deficit hyperactivity disorder and two school-based samples. Journal of Clinical Child and Adolescent Psychology, 35(3), 369–385. 10.1207/s15374424jccp3503_3 [DOI] [PubMed] [Google Scholar]
- Fisak BJ Jr, Oliveros A, & Ehrenreich JT (2006). Assessment and behavioral treatment of selective mutism. Clinical Case Studies, 5(5), 382–402. 10.1177/1534650104269029 [DOI] [Google Scholar]
- Funderburk BW, & Eyberg S (2011). Parent–child interaction therapy In Norcross JC, VandenBos GR, & Freedheim DK (Eds.), History of psychotherapy: Continuity and change (pp. 415–420). Washington, DC, US: American Psychological Association; 10.1037/12353-021 [DOI] [Google Scholar]
- Furr JM, Sanchez AL, Hong N, & Comer JS (in press). Exposure therapy for childhood selective mutism: principles, practices, and procedures In McGuire J, Peris T, & Storch E (Eds), A Clinicians’ Guide to Exposure Therapy with Children and Adolescents. New York, NY: Elsevier. [Google Scholar]
- Gallo KP, Cooper-Vince CE, Hardway CL, Pincus DB, & Comer JS (2014). Trajectories of change across outcomes in intensive treatment for adolescent panic disorder and agoraphobia. Journal of Clinical Child & Adolescent Psychology, 43(5), 742–750. 10.1080/15374416.2013.794701 [DOI] [PubMed] [Google Scholar]
- Guy W, & Bonato R (1970). Clinical global impression scale (CGI). ECDEU Assessment Manual for Psychopharmacology Revised, pp. 217–222. [Google Scholar]
- Jensen PS, Hinshaw SP, Swanson JM, Greenhill LL, Conners CK, Arnold LE, … & March JS. (2001). Findings from the NIMH Multimodal Treatment Study of ADHD (MTA): implications and applications for primary care providers. Journal of Developmental & Behavioral Pediatrics, 22(1), 60–73. [DOI] [PubMed] [Google Scholar]
- Kazdin AE, & Blase SL (2011). Rebooting psychotherapy research and practice to reduce the burden of mental illness. Perspectives on psychological science, 6(1), 21–37. 10.1177/1745691610393527 [DOI] [PubMed] [Google Scholar]
- Kazdin AE, Holland L, Crowley M, & Breton S (1997). Barriers to treatment participation scale: Evaluation and validation in the context of child outpatient treatment. Journal of Child Psychology and Psychiatry, 38(8), 1051–1062. 10.1111/j.1469-7610.1997.tb01621.x [DOI] [PubMed] [Google Scholar]
- Larsen DL, Attkisson CC, Hargreaves WA, & Nguyen TD (1979). Assessment of client/patient satisfaction: Development of a general scale. Evaluation and Program Planning, 2(3), 197–207. 10.1016/0149-7189(79)90094-6 [DOI] [PubMed] [Google Scholar]
- Letamendi AM, Chavira DA, Hitchcock CA, Roesch SC, Shipon-Blum E, & Stein MB (2008). Selective mutism questionnaire: Measurement structure and validity. Journal of the American Academy of Child & Adolescent Psychiatry, 47(10), 1197–1204. 10.1097/CHI.0b013e3181825a7b [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luby J, Lenze S, & Tillman R (2012). A novel early intervention for preschool depression: Findings from a pilot randomized controlled trial. Journal of Child Psychology and Psychiatry, 53, 313–322. 10.1111/j.1469-7610.2011.02483.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manassis K, & Tannock R (2008). Comparing interventions for selective mutism: A pilot study. Canadian Journal of Psychiatry, 53, 700–703. 10.1177/070674370805301010 [DOI] [PubMed] [Google Scholar]
- Martinez YJ, Tannock R, Manassis K, Garland EJ, Clark S, & McInnes A (2015). The teachers’ role in the assessment of selective mutism and anxiety disorders. Canadian Journal of School Psychology, 30(2), 83–101. 10.1177/0829573514566377 [DOI] [Google Scholar]
- Muris P, & Ollendick TH (2015). Children who are anxious in silence: A review on selective mutism, the new anxiety disorder in DSM-5. Clinical child and family psychology review, 18(2), 151–169. 10.1007/s10567-015-0181-y [DOI] [PubMed] [Google Scholar]
- Nakamura BJ, Ebesutani C, Bernstein A, & Chorpita BF (2009). A psychometric analysis of the child behavior checklist DSM-oriented scales. Journal of Psychopathology and Behavioral Assessment, 31(3), 178–189. 10.1007/s10862-008-9119-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oerbeck B, Overgaard KR, Stein MB, Pripp AH, & Kristensen H (2018). Treatment of selective mutism: A 5-year follow-up study. European Child and Adolescent Psychiatry, 27, 997–1009. 10.1007/s00787-018-1110-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oerbeck B, Stein MB, Pripp AH, & Kristensen H (2015). Selective mutism: Follow-up study 1 year after end of treatment. European Child and Adolescent Psychiatry, 24, 757–766. 10.1007/s00787-014-0620-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oerbeck B, Stein MB, Wentzel-Larsen T, Langsrud Ø, & Kristensen H (2014). A randomized controlled trial of a home and school-based intervention for selective mutism–defocused communication and behavioural techniques. Child and Adolescent Mental Health, 19(3), 192–198. 10.1111/camh.12045 [DOI] [PubMed] [Google Scholar]
- Ooi YP, Sung SC, Raja M, Kwan C, Koh JBK, & Fung D (2016). Web-based CBT for the Treatment of Selective Mutism: Results from a Pilot Randomized Controlled Trial in Singapore. Journal of Speech Pathology and Therapy, 1(2), 112 10.4172/2472-5005.1000112 [DOI] [Google Scholar]
- Ollendick TH (2014). Brief, high intensity interventions with children and adolescents with anxiety disorders: Introductory comments. Psychopathology Review, 1, 169–174. 10.5127/pr.034813 [DOI] [Google Scholar]
- Ollendick TH, Halldorsdottir T, Fraire MG, Austin KE, Noguchi RJP, Lewis KM, Jarrett MA, Cunningham NR, Canavera K, Allen KB, & Whitmore MJ (2015). Specific phobias in youth: A randomized controlled trial comparing one-session treatment to a parent-augmented one-session treatment. Behavior Therapy, 46, 141–155. 10.1016/j.beth.2014.09.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ollendick TH, Öst LG, Reuterskiöld L, Costa N, Cederlund R, Sirbu C, … & Jarrett MA. (2009). One-session treatment of specific phobias in youth: a randomized clinical trial in the United States and Sweden. Journal of consulting and clinical psychology, 77(3), 504 10.1037/a0015158 [DOI] [PubMed] [Google Scholar]
- Öst LG, & Ollendick TH (2017). Brief, intensive and concentrated cognitive behavioral treatments for anxiety disorders in children: A systematic review and meta-analysis. Behaviour research and therapy, 97, 134–145. 10.1016/j.brat.2017.07.008 [DOI] [PubMed] [Google Scholar]
- Pelham WE Jr, & Hoza B (1996). Intensive treatment: A summer treatment program for children with ADHD In Hibbs ED & Jensen PS (Eds.), Psychosocial treatments for child and adolescent disorders: Empirically based strategies for clinical practice (pp. 311–340). Washington, DC: American Psychological Association; 10.1037/10196-013 [DOI] [Google Scholar]
- Petersen A (2015, August 17). When a child doesn’t speak: Treating selective mutism. Wall Street Journal. [Google Scholar]
- Pincus DB, Santucci LC, Ehrenreich JT, & Eyberg SM (2008). The implementation of modified Parent-Child Interaction Therapy for youth with separation anxiety disorder. Cognitive and Behavioral Practice, 15, 118–125. [Google Scholar]
- Puliafico AC, Comer JS, & Pincus DB (2012). Adapting parent-child interaction therapy to treat anxiety disorders in young children. Child and Adolescent Psychiatric Clinics, 21(3), 607–619. 10.1016/j.chc.2012.05.005 [DOI] [PubMed] [Google Scholar]
- Rice TR, Kostek NT, Gair SL, & Rojas A (2017). Summer Camp Program for Children With Obsessive–Compulsive Disorder: Description and Preliminary Observations. Cognitive and Behavioral Practice, 24(2), 142–151. 10.1016/j.cbpra.2016.03.006 [DOI] [Google Scholar]
- Saint Louis C (2015, August 18). Scared into silence, little voices learn to speak. New York Times, pp. D1. [Google Scholar]
- Santucci LC, Ehrenreich JT, Trosper SE, Bennett SM, & Pincus DB (2009). Development and preliminary evaluation of a one-week summer treatment program for separation anxiety disorder. Cognitive and Behavioral Practice, 16(3), 317–331. 10.1016/j.cbpra.2008.12.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott S, & Beidel DC (2011). Selective mutism: an update and suggestions for future research. Current psychiatry reports, 13(4), 251–257. 10.1007/s11920-011-0201-7 [DOI] [PubMed] [Google Scholar]
- Shaffer D, Gould MS, Brasic J, Ambrosini P, Fisher P, Bird H, & Aluwahlia S (1983). A children’s global assessment scale (CGAS). Archives of General Psychiatry, 40(11), 1228–1231. 10.1001/archpsyc.1983.01790100074010 [DOI] [PubMed] [Google Scholar]
- Sharkey L, Mc Nicholas F, Barry E, Begley M, & Ahern S (2008). Group therapy for selective mutism–A parents’ and children’s treatment group. Journal of Behavior Therapy and Experimental Psychiatry, 39(4), 538–545. 10.1016/j.jbtep.2007.12.002 [DOI] [PubMed] [Google Scholar]
- Silverman WK, Albano AM. The Anxiety Disorders Interview Schedule for Children for DSM-IV: Child and Parent Versions. San Antonio, TX: Psychological Corporation; 1997. [Google Scholar]
- Silverman WK, & Ollendick TH (2005). Evidence-based assessment of anxiety and its disorders in children and adolescents. Journal of Clinical Child and Adolescent Psychology, 34(3), 380–411. 10.1207/s15374424jccp3403_2 [DOI] [PubMed] [Google Scholar]
- Steinhausen H, Wachter M, Laimböck K, & Metzke CW (2006). A long term outcome study of selective mutism in childhood. Journal of Child Psychology and Psychiatry, 47(7), 751–756. 10.1111/j.1469-7610.2005.01560.x [DOI] [PubMed] [Google Scholar]
- Storch EA, Geffken GR, Merlo LJ, Mann G, Duke D, Munson M, … & Goodman WK. (2007). Family-based cognitive-behavioral therapy for pediatric obsessive-compulsive disorder: Comparison of intensive and weekly approaches. Journal of the American Academy of Child & Adolescent Psychiatry, 46(4), 469–478. 10.1097/chi.0b013e31803062e7 [DOI] [PubMed] [Google Scholar]
- Suveg C, Comer JS, Furr JM, & Kendall PC (2006). Adapting manualized CBT for a cognitively delayed child with multiple anxiety disorders. Clinical Case Studies, 5, 488–510. 10.1177/1534650106290371 [DOI] [Google Scholar]
- Walkup JT, Albano AM, Piacentini J, Birmaher B, Compton SN, Sherrill JT, … Kendall PC (2008). Cognitive behavioral therapy, sertraline, or a combination in childhood anxiety. New England Journal of Medicine, 359, 2753–2766. 10.1056/NEJMoa0804633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood JJ, Piacentini JC, Bergman RL, McCracken J, & Barrios V (2002). Concurrent validity of the anxiety disorders section of the Anxiety Disorders Interview Schedule for DSM-IV: Child and Parent Versions. Journal of Clinical Child and Adolescent Psychology, 31(3), 335–342. 10.1056/NEJMoa0804633 [DOI] [PubMed] [Google Scholar]