Abstract
Pressure ulcer interventions are commonly assessed with measures of seating interface pressure, such as peak pressure gradients (PPGs). Decreases in PPG magnitudes may reduce pressure ulcer risk by decreasing tissue deformation and increasing tissue perfusion of at-risk weight-bearing tissues. Changes in PPG directions, which have previously been overlooked in the seating pressure literature, may provide a transient increase in blood flow to at-risk tissues, even if the PPG magnitude and location remain the same. The purpose of this study was to assess both PPG components in response to combinations of wheelchair tilt and recline angles. Thirteen power wheelchair users were recruited into the study. Six combinations of wheelchair tilt (15°, 25°, and 35°) and recline (10° and 30°) were tested in random order. Each combination was tested with 5-min upright sitting, 5-min tilt and recline, and 5-min maximal pressure relief recovery. Changes in PPG magnitudes and PPG directions under the left ischial tuberosity were computed for the six angle combinations. The findings in this study suggested that when combining wheelchair tilt and recline, the recline function may be particularly useful in reducing PPG magnitudes, while the tilt function may be particularly useful in manipulating PPG directions.
Keywords: Peak Pressure Gradient, Pressure Ulcers, Recline, Seating Pressures, Spinal Cord Injury, Tilt, Wheelchair
Introduction
Spinal cord injury (SCI) affect more than a quarter-million people in the United States (National Spinal Cord Injury Statistical Center, 2012). Sitting-induced pressure ulcers are one of the most common secondary complications associated with SCI and impose excessive burdens on quality of life and healthcare costs (Oleson, de Zee, & Rasmussen, 2010). Each individual with SCI who has a pressure ulcer is estimated to cost $4,745 per month on average (Chan et al., 2013). Across the United States, treatment for SCI-related pressure ulcers is estimated to cost $1.2 billion per year, accounting for up to 60% of all pressure ulcer treatments (Byrne & Salzberg, 1996).
While mechanical loading is widely accepted as a prerequisite of pressure ulcers, there is no clear consensus on the mechanisms underlying the subsequent progression from tissue loading to tissue necrosis. The two leading hypotheses include tissue ischemia and tissue deformation (Liao, Burns, & Jan, 2013; Loerakker et al., 2011; Oleson et al., 2010). Under the ischemia hypothesis, mechanical loading leads to necrosis because arterial compression induces prolonged hypoxia by reducing the tissues’ supply of oxygen and nutrients. Under the deformation hypothesis, deformation or strain caused by either tensile, compressive and/or shear stress may trigger individual cell deaths. Because both hypotheses are rooted in mechanical loading, comprehensive pressure ulcer interventions incorporate both passive and active reductions of seating loads (Akins, Karg, & Brienza, 2011; Burns & Betz, 1999; Metring, Gaspar, Mateus-Vasconcelos, Gomes, & de Abreu, 2012; S. Sprigle & Schuch, 1993). Passive interventions include support surfaces that redistribute seating loads throughout the seating interface via immersion (i.e., how deep the buttocks sink below the interface) and envelopment (i.e., how well the interface conforms to the buttocks) (Jan & Brienza, 2006). Active interventions include manual and power-assisted maneuvers to shift the individual’s weight away from the seating interface. Manual maneuvers include wheelchair push-ups, side leaning, and forward leaning. Because people with SCI may not have the requisite motor function for manual weight shifts, power-assisted maneuvers are often recommended, including wheelchair tilt (i.e., changing the seat-to-ground angle while maintaining the seat-to-back angle) and wheelchair recline (i.e., changing the seat-to-back angle while maintaining the seat-to-ground angle) (Jan, Crane, Liao, Woods, & Ennis, 2013; Jan, Jones, Rabadi, Foreman, & Thiessen, 2010; Jan, Liao, Jones, Rice, & Tisdell, 2013).
Hobson (1992) was among the first to assess pressure ulcer interventions using seating interface pressures. Peak pressures were found to be significantly higher in people with SCI compared to people without SCI. Brienza, Karg, Geyer, Kelsey, and Trefler (2001) used an average of highest 4 pressures (not limited to adjacent sensors) to assess seating pressure distributions in a randomized controlled trial with 32 elderly wheelchair users over 12 months. The results indicated that higher interface pressure measurements were found to be significantly higher among participants who developed pressure ulcers than those who did not. Later, in order to increase the reliability and repeatability of seating interface pressure measurements, peak pressure index (PPI) was introduced as the sensel mean within a 9–10 cm2 area of the ischial tuberosity (Maurer & Sprigle, 2004). Chen et al. (2014) used PPI to investigate the relationship between ischial tuberosity and coccygeal pressures in six combinations of wheelchair tilt and recline. The results indicated that ischial tuberosity pressures appeared to be redistributed to the coccyx under the four smallest combinations of tilt and recline, while ischial tuberosity pressures appeared to be redistributed to the back support under the two largest combinations of tilt and recline.
In active interventions, dynamic repositioning of the body posture produces directional changes of forces acting on the buttock soft tissues. For example, as body weight is redistributed posteriorly from an upright posture, the normal and shear forces acting on the skin over the ischial tuberosity may significantly change. Thus, these changes in directional forces may be of particular interest for interventions such as tilt and recline, which inherently involve postural changes (Stephen Sprigle, Wootten, Bresler, & Flinn, 2002). In the literature, peak pressure gradients (PPGs) have been used to characterize these sitting-induced normal and shear forces (Aissaoui, Lacoste, & Dansereau, 2001; Hobson, 1992; S. Sprigle, Maurer, & Soneblum, 2010). Changes in PPG directions, which have previously been overlooked in the seating pressure literature, may provide a transient increase in blood flow to at-risk tissues (Lung, Hsiao-Wecksler, Burns, Lin, & Jan, 2016), even if the PPG magnitude and location remain the same (Figures 1 and 2).
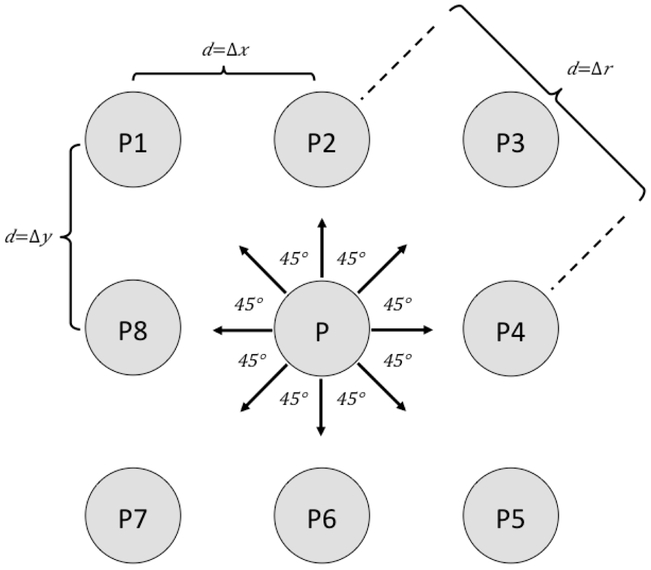
Figure 1.
Pressure gradients refer to the pressure change (i.e., P–Pi for i = {1,2,…,8}) per unit of distance (i.e., d) between orthogonally and diagonally adjacent sensels. The peak pressure gradient (PPG) refers to the maximal pressure gradient (i.e., for i = {1,2,…,8}). The PPG directional change refers to the angle between two vectors (e.g., ). The largest PPG magnitude belongs to a PPG vector in a single pressure frame. The angle of the PPG direction can be computed from the dot product of the two vectors from two consecutive pressure frames.
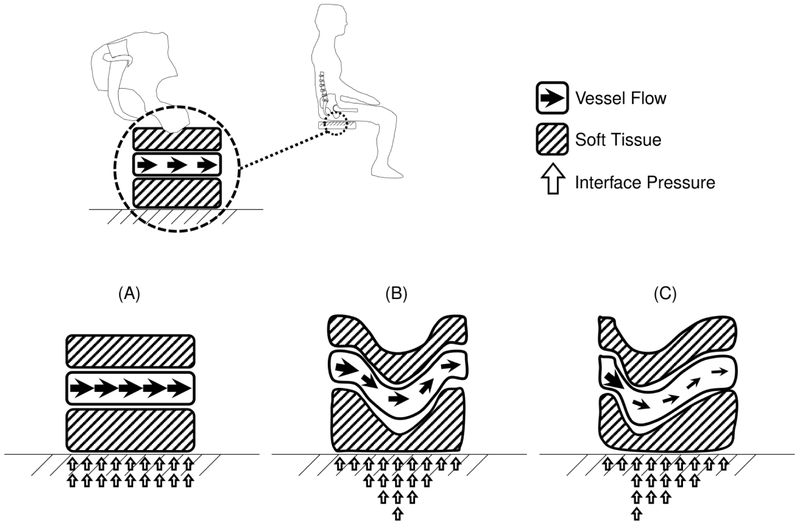
Figure 2.
A conceptual schematic of three ischial tuberosity pressure distributions. Although these distributions have similar average pressures, they have distinct peak pressure gradients: (A) zero, (B) medium, and (C) high. Peak pressure gradients may affect pressure ulcer development by impacting blood flow, as well as localized tensile and shear stresses.
With respect to the magnitude component, PPG magnitudes may potentially uncover localized risk factors masked by PPIs. Under the ischemia hypothesis, high PPG magnitudes may serve as an indicator of excessive blood flow blockades that are capable of inducing prolonged hypoxia. Under the deformation hypothesis, high PPG magnitudes may serve as an indicator of excessive tensile and shear stresses that are capable of inducing necrosis. In the literature, seating PPG magnitudes have been shown to be higher in people with SCI compared to those without SCI (Hobson, 1992). Just as PPG magnitudes may be of particular interest when PPIs are similar, PPG directions may be of interest when other variables are similar. Even when other variables differ, PPG directions may still be of interest due to the dynamic changes of directional forces in the buttock soft tissues during active interventions, such as tilt and recline. Theoretically, during different active interventions, such as tilt and recline, may induce different changes of PPG directions. Although small changes of PPG directions have been previously investigated in the risk of plantar ulcers (Lung et al., 2016), they have not yet been investigated in seating interface pressure.
The purpose of this study was to investigate seating PPG in response to postural changes from six combinations of wheelchair tilt and recline angles. This study assessed seating PPG not only in terms of magnitude, but also in terms of direction, which had not been previously investigated in the literature. By comparing commonly used tilt and recline angles, the goal was to better understand the effect of wheelchair tilt and recline on both PPG magnitudes and directions. Depending on the sensitivity of PPG magnitudes and directions in response to wheelchair postures, future work may be able to utilize these PPG components for pressure ulcer prevention.
Methods
This study used a treatment-outcomes, repeated-measures research design.
Participants
Thirteen wheelchair users with SCI were recruited via research flyers and hospital referrals. Inclusion criteria included having traumatic SCI between the levels of C4 and T5, being at least 6 months after spinal injury, using a power wheelchair as the primary means of mobility, and using a wheelchair seat with a width between 43 cm and 53 cm. Exclusion criteria included diagnoses of cardiovascular diseases, skeletal deformities (e.g., scoliosis, pelvic obliquity, and hip and knee contractures), or active pressure ulcers. All participants provided informed consent to this study, which was approved by an institutional review board for human subject research (IRB #14448).
The demographic data of the participants were as follows (values are mean ± SD): age 36.2 ± 10.0 years, body mass index 24.6 ± 4.6 kg/m2, and duration of injury 5.8 ± 5.9 years. The 13 participants included 4 women and 9 men: 3 African Americans, 1 Asian American, 8 Caucasian Americans, and 1 multiracial American. Four participants had sensory complete injury (American Spinal Injury Association Impairment Scale (AIS) A), 2 participants had motor complete injury (AIS B), and 7 participants had incomplete injury (AIS C).
Instrumentation
Seating interface pressures were recorded with an interface pressure mat (CONFORMat 5330; Tekscan, South Boston, MA). The mat contains a 32 × 32 grid-based array of extremely thin (0.35 mm), flexible tactile sensels. The sensel array can measure an area of up to 47.1 × 47.1 cm, with each sensel measuring approximately 1.47 × 1.47 cm. The mat system was calibrated before each participant’s data collection, based on manufacturer guidelines. A power wheelchair (C300 Corpus; Permobil, Lebanon, TN) with tilt and recline seating functions was used in this study. The seat width was 48 cm. A standard high-density precontoured foam seat cushion (Corpus seating system; Permobil, Lebanon, TN) was used in this study.
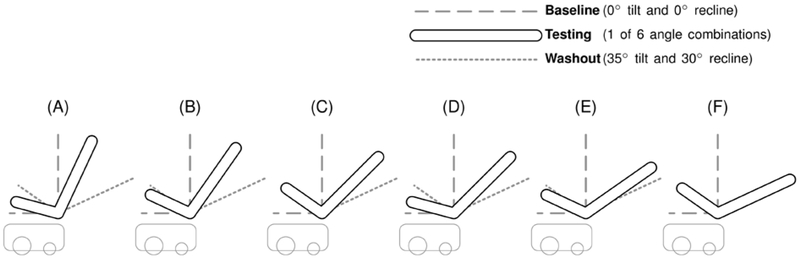
Configurations of tilt and recline are shown in Figure 3 and described in the author’s previous studies with the exception of the recline angle notation (Jan, Crane, et al., 2013; Jan et al., 2010; Jan, Liao, et al., 2013). Previously, recline values were reported as the angle between the seat and backrest. In keeping with current clinical practice, recline values in this paper were modified to denote the sagittal angle of the backrest from the vertical (Waugh & Crane, 2013). That is to say, the previously reported recline angle of 100° and 120° were updated to 10° and 30°, respectively, although the actual recline configurations were not changed. Two digital angle gauges (WR300; Wixey, online-based company) were used to measure the wheelchair tilt and recline angles.
Figure 3.
A schematic illustration of the six combinations of wheelchair tilt and recline angles: (A) 15° tilt and 10° recline, (B) 25° tilt and 10° recline, (C) 35° tilt and 10° recline, (D) 15° tilt and 30° recline, (E) 25° tilt and 30° recline, and (F) 35° tilt and 30° recline.
Protocols
The wheelchair configuration protocol is described in the authors’ previous studies, which were conducted in parallel to assess skin perfusion and seating pressure response to wheelchair tilt and recline (Jan, Crane, et al., 2013; Jan et al., 2010; Jan, Liao, et al., 2013). We selected 5-min upright sitting (the ischemic period), 5-min tilt and recline (the partial pressure relief period), and 5-min maximal pressure relief recovery (the washout period) in the entire protocol (Figure 3).
Procedures
Before the experiment, participants provided informed consent and acclimated to the room temperature (23°C ± 2°C) for 30 minutes. During the acclimation period, they were asked to empty their bladders, and the interface pressure mapping mat was placed atop the standard precontoured seat cushion of the test power wheelchair. Upon completion of the acclimation period, the participant was transferred to a mat table to affix a thin laser Doppler flowmetry (LDF) sensor placed at the skin over the right ischial tuberosity. The LDF probe was used to measure skin perfusion for the authors’ study regarding skin blood flow response to tilt and recline (Jan, Crane, et al., 2013; Jan, Liao, et al., 2013). The participant was then transferred to the test power wheelchair, which contained a pressure mapping mat at the interface between the cushion and the buttocks. The participant was asked to place his or her hands in the lap and to sit as far back as possible while remaining comfortable. The foot support was adjusted to ensure that the femurs were parallel to the floor. The ischial tuberosity and coccygeal areas were palpated to ensure that they were positioned over the pressure mapping mat. After a 6-min settling period to reduce the effects of creep (Crawford, Stinson, Walsh, & Porter-Armstrong, 2005), the pressure mapping mat was calibrated to the given participant according to manufacturer instructions.
Each experiment began with a washout configuration of 35° tilt and 30° recline. During the experiment, pressure mapping samples were recorded at 10 Hz, and the angle tolerance was ±3 degrees. To minimize operator effects, the same research assistant performed the tilt and recline adjustments for all experiments in this study. To minimize sequence effects, a balanced design with randomized testing protocols was used. To minimize carry-over effects, every testing condition was ended with a washout configuration of 35° tilt and 30° recline. In addition, the washout configuration served as a recovery period for the buttock soft tissue. The duration of reactive hyperemia is proportional to the time of occlusion (Jan et al., 2010). For partial pressure relief, recovery is supposed to be longer; thus, the additional 5-min washout period ensured an adequate reactive hyperemic response to the protocol’s occlusion periods (Jan et al., 2010). Each participant spent approximately 100 minutes in completing the entire protocol.
Data Analysis
Localized sensel averages (e.g., the PPI metric) have been widely used to compensate for reliability issues in modern interface pressures sensels (Hobson, 1992; Maurer & Sprigle, 2004). Thus, rather than computing PPG from raw sensel values, the interface pressure data were preprocessed using a 2-dimensional moving average filter with a window size of 3 sensels × 3 sensels (Wininger & Crane, 2014). Ischial tuberosity pressure was quantified as the PPI under the ischial tuberosity during the upright-sitting period (0° tilt, 0° recline) and was used as the baseline for comparisons among various tilt and recline angles. Because up to 30 seconds were needed to complete the tilt and recline angle adjustments, data obtained during the first 30 seconds of each 5-min testing period were excluded from analysis. PPG magnitudes and PPG directional changes were then computed within a 3 × 3 sensel window under the left ischial tuberosity. The thin LDF sensor placed at the skin over the right ischial tuberosity may affect the pressure distributions; thus, we only analyze the PPG parameters at the skin over the left ischial tuberosity. To compute the PPG magnitudes, the PPG magnitudes for the six testing conditions were divided by their corresponding upright-sitting baseline periods (0° tilt and 0° recline). The PPG magnitude of ischial pressure (P) was defined as follows,
| (Equation 1) |
where i = {1,2, …..8} and Pi refers to the set of eight sensels surrounding a given sensel P (Figure 1). The d was defined as the distance between the Pi and P.
To compute the PPG directional changes by the upright-sitting baseline periods, the angle between the baseline PPG direction and testing PPG direction was computed for each testing condition. The PPG directional change was defined as follows,
| (Equation 2) |
where represents the vector from sensel P to sensel Pm and represents the vector from sensel P to sensel Pn; Pm and Pnare the peak pressures at two consecutive frames (Figure 1). Since each angle could be represented by either of two conjugate angles, the reflex angle was discarded; that is, the angle that was less than or equal to 180° was always selected. For example, in Figure 1. All PPG computations were performed using MATLAB R2015a (MathWorks, South Boston, MA).
Paired samples t tests were used to compare the PPG magnitudes and PPG directional changes between two recline angles (10° and 30°) under each tilt angle (15°, 25°, and 35°). One-way analysis of variance (ANOVA) with Fisher’s least significant difference correction was used for pairwise comparisons of PPG magnitudes and directional changes between three tilt angles (15°, 25°, and 35°) under each recline angle (10° and 30°). All statistical tests were performed using SPSS 22 (IBM, Somers, NY) at a significance level of .05.
Results
The values were presented as the mean ± standard errors in Figure 4-7.
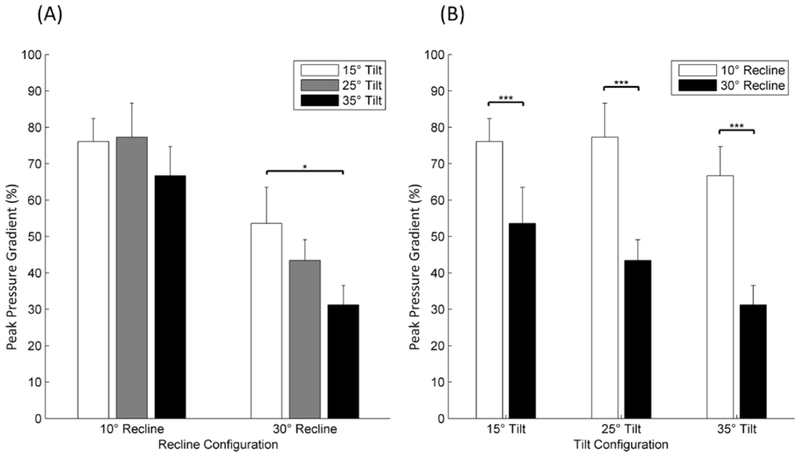
Figure 4.:
Comparison of peak pressure gradient (PPG) magnitudes: (A) two recline angles (10° and 30°) in response to three tilt angles (15°, 25°, and 35°), (B) three tilt angles (15°, 25°, and 35°) in response to two recline angles (10° and 30°). *A significant difference (p<.05). ***A significant difference (p<.001).
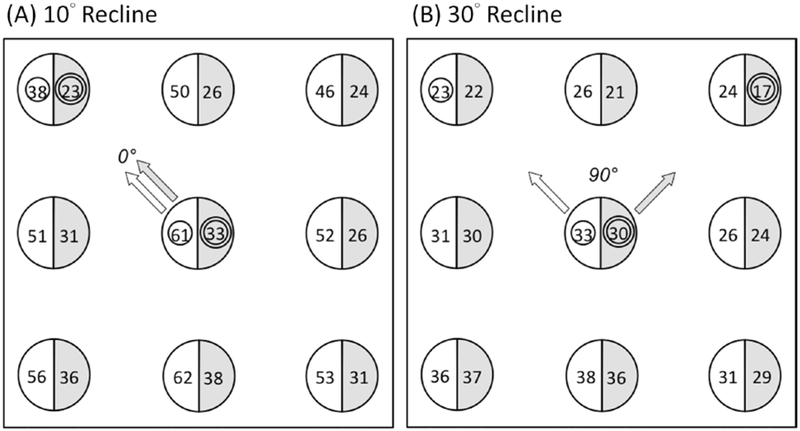
Figure 7.
Ischial tuberosity pressure distributions from a sample participant: (A) no directional change was observed between the testing condition of 15° tilt and 10° recline (light) and the testing condition of 25° tilt and 10° recline (dark); (B) a directional change of 90° was observed between the testing condition of 15° tilt and 30° recline (light) and the testing condition of 25° tilt and 30° recline (dark).
Peak Pressure Gradient Magnitude Changes
Tilt Angle Effect
Under 10° recline, there were no significant pairwise differences in PPG magnitudes between 15° tilt, 25° tilt, and 35° tilt (Figure 4A).
Under 30° recline, there was a significant decrease in PPG magnitudes between 15° tilt and 35° tilt (p<.05), whereas there were no significant differences in PPG magnitudes between 15° tilt and 25° tilt and between 25° tilt and 35° tilt (Figure 4A).
Recline Angle Effect
Under every tilt angle (15°, 25°, and 35°), there was a significant decrease (p<.001) in PPG magnitudes between 10° recline and 30° recline (Figure 4B).
Peak Pressure Gradient Direction Changes
Tilt Angle Effect
Under 10° recline, there was a significant increase (p<.05) in PPG directional changes between 15° tilt and 35° tilt, whereas there were no significant differences in PPG directions between 15° tilt and 25° tilt and between 25° tilt and 35° tilt (Figure 5A).
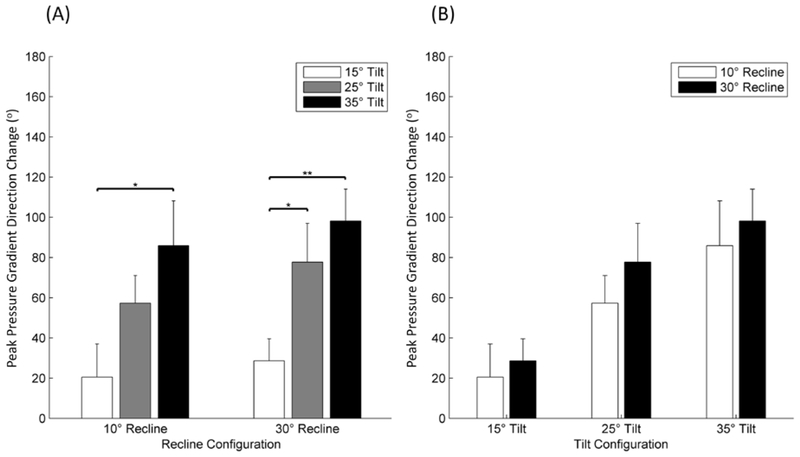
Figure 5.
Comparison of peak pressure gradient (PPG) directions change: (A) two recline angles (10° and 30°) in response to three tilt angles (15°, 25°, and 35°), (B) three tilt angles (15°, 25°, and 35°) in response to two recline angles (10° and 30°). *A significant difference (p<.05). **A significant difference (p<.005).
Under 30° recline, there was a significant increase (p<.05) in PPG directional changes between 15° tilt and 25° tilt and a significant increase (p<.005) between 15° tilt and 35° tilt, whereas there was no significant difference in PPG directions between 25° tilt and 35° tilt (Figure 5A).
Recline Angle Effect
Under every tilt angle (15°, 25°, and 35°), there were no significant differences in PPG directional changes between 10° recline and 30° recline (Figure 5B).
Discussion
In this study, we analyzed seating pressure gradients as vectors, rather than only magnitudes, to encapsulate directional information that had not previously been addressed in the seating pressure literature. At the plantar interface, Lung et al. (2016) were interested in PPG directions during walking because plantar tissues are subjected to dynamic changes in directional forces throughout the gait cycle. They proposed the analysis of PPG directions as an additional variable to consider for diabetic foot ulcer risk. At the seating interface, changes in directional forces are also present, especially during active interventions such as wheelchair tilt and recline. During tilt and recline maneuvers, normal and tangential component forces at the seating interface will change in response to body weight redistribution. For example, Hobson (1992) reported a 25% increase in tangential forces in response to 20° recline maneuvers. Pelvic rotation will also modify the directional forces surrounding the pelvis. In altering the load-bearing structures of the buttock region, these positional and rotational changes of the pelvis have the potential to increase pressure ulcer risk (Stephen Sprigle et al., 2002). Because active interventions, such as tilt and recline, can induce these types of changes in the buttock tissues, changes in directional forces may be of particular interest during assessment. While interface pressure mats do not directly measure internal forces within the tissues, it is reasonable to assume a relationship between interface pressure gradients and internal tissue shear stresses (Hobson, 1992). Shear stress plays an important role within both major hypotheses of pressure ulcer etiology (Oleson et al., 2010). Under the deformation hypothesis, the relationship between shear stress and tissue necrosis is direct, in that interface shear stress can directly induce individual cell deaths. Under the ischemia hypothesis, the relationship between shear stress and tissue necrosis involves the occlusion of blood flow. Seating interface shear stress has been shown to be approximately three times higher in people with SCI than people without SCI (Bennett, Kavner, Lee, & Trainor, 1979; Bennett, Kavner, Lee, Trainor, & Lewis, 1984). Furthermore, interface shear stress has been shown to reduce blood flow at a greater rate than interface pressure of the same magnitude (Zhang & Roberts, 1993).
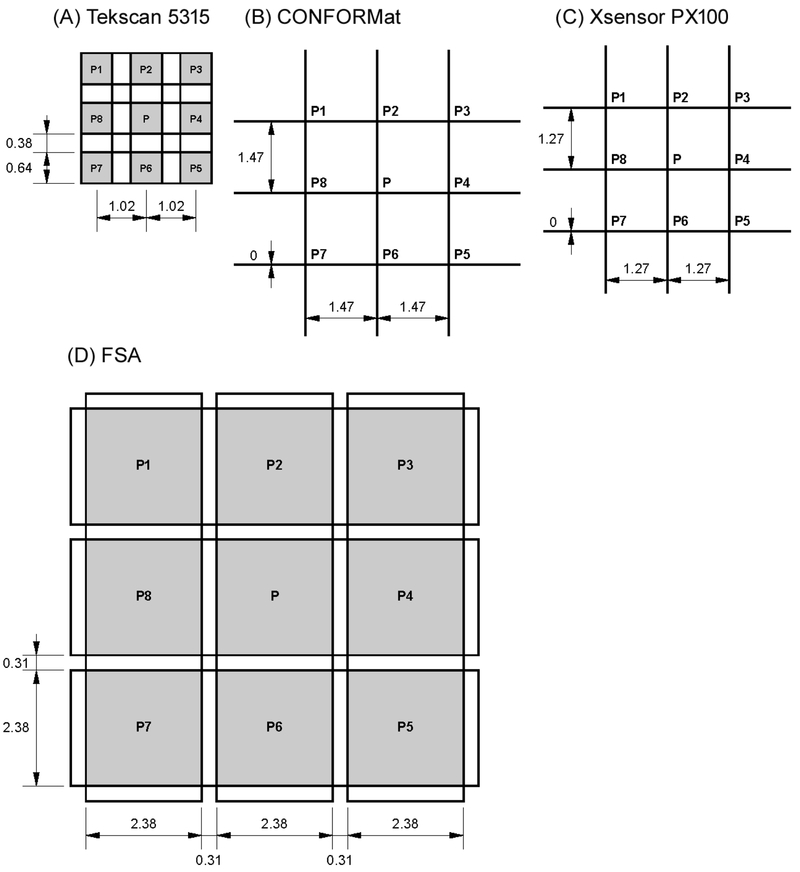
Due to current technological limitations, it is more difficult to measure seating shear stress than seating pressure without significantly altering the seating interface properties. Thus, seating pressure-based measures for shear stress are desirable. Zou and colleagues demonstrated that the PPG was highly correlated with the maximal shear stress (Zou, Mueller, & Lott, 2007). For example, seating interface displacement has been proposed as one such surrogate measure for shear stress (Lung et al., 2014). Lung et al. (2014) observed between 3 cm and 7 cm of seating displacement in response to tilt and recline angle combinations, which supported previous laboratory tests of dynamic seating conditions (e.g., tilt, recline, and forward flexion), in which sliding displacements of between 1.5 cm and 6 cm were observed (Aissaoui et al., 2001; Cooper, Dvorznak, Rentschler, & Boninger, 2000; Hobson, 1992; Hobson & Tooms, 1992; Tam, Mak, Lam, Evans, & Chow, 2003). Thus, Lung et al. (2014) proposed the use of sliding displacement as a secondary indicator of tangential shear stress at the seating interface. In contrast to the tangential shear stress approximated by interface displacement, PPG magnitudes may represent a more localized measure of internal tissue shear stress (Hobson, 1992). Given various ischial tuberosity pressure distributions with similar PPIs, the distributions with higher PPG magnitudes would hypothetically result in disproportionately greater blood flow occlusion surrounding the ischial tuberosity. As long as a given interface pressure mat’s sensel resolution is reasonable, interface pressure gradients can be conveniently measured and computed. In Figure 6, the dimensional specifications of 9-sensel regions from four commonly used interface pressure mats are illustrated. While the sensel resolution differs between each mat, PPG values can still be reasonably compared between different mats because the magnitudes are already standardized by distance. That is, because the sensel distance (d) is in the PPG denominator, the PPG magnitudes inherently adjust for the resolutional differences between dense and sparse sensel arrays. However, the differences in the inherent filtering of pressure mats may affect the noise level of PPG data.
Figure 6.
Dimensional specifications of 9-sensel regions from four commonly used interface pressure mats: (A) Tekscan 5315 (Tekscan, South Boston, MA), (B) CONFORMat (Tekscan, South Boston, MA), (C) Xsensor PX100 (XSENSOR Technology, Calgary, Alberta, Canada), (D) FSA UT100 (Vista Medical, Winnipeg, Manitoba, Canada)
In this study, PPG magnitudes were more affected by wheelchair recline than wheelchair tilt. Among all pairwise tilt comparisons, only one pair resulted in a significant decrease in PPG magnitudes, whereas all pairwise recline comparisons resulted in a significant decrease in PPG magnitudes. Furthermore, PPG magnitudes were found to be significantly lower when repositioning from 10° recline to 30° recline while maintaining the same level of tilt. While Hobson (1992) found that wheelchair recline typically caused an increase in overall surface shear stress, the findings in the current study suggest that the recline function may still be useful in reducing localized stresses at the ischial tuberosity when combined with tilt. These findings were also supported by Aissaoui et al. (2001), which found decreases in PPG magnitudes for all tested combinations of tilt and recline, except in the case of 30° recline without any tilt.
Conversely, PPG directions were more affected by tilt than recline. While maintaining the same level of tilt, PPG directions did not change significantly when repositioning from 10° recline to 30° recline; however, under both recline conditions, PPG directions changed significantly when repositioning from 15° tilt to 35° tilt. Additionally, PPG directions changed significantly when repositioning from 15° tilt to 25° tilt under 30° recline, but not under 10° recline. In Figures 7, ischial tuberosity pressure distributions during 10° recline and 30° recline, respectively, from a sample participant are shown as an illustrative example. No change in the PPG direction was observed when repositioning from 15° tilt to 25° tilt while under 10° recline (Figure 7A), whereas a change in the PPG direction was observed while under 30° recline (Figure 7B). In this example, the PPG magnitude under 25° tilt and 10° recline was the same as the PPG magnitude under 25° tilt and 30° recline. However, while the magnitudes were identical under both recline conditions, a directional change was observed only under the 30° recline condition.
Although PPG directional changes may be beneficial for tissue viability, the potential benefits have yet to be investigated. A potential benefit of assessing PPG directional changes may be to recognize reductions in pressure gradient duration. Under the traditional view of seating gradients, the PPG exists as a scalar at the location of the vector tail. For example, the PPGs in Figure 7B are both scalar values located at the ischial tuberosity for 10 minutes total. However, by including the PPG direction along with the magnitude, they would actually be considered two gradient vectors starting at the ischial tuberosity and pointing in distinct directions for 5 minutes each. This view of PPGs may be useful for situations in which existing metrics cannot easily explain individual differences in physiological responses (e.g., skin blood flow characteristics, pressure ulcer development, etc.) to pressure ulcer interventions, particularly active interventions involving directional changes of force within the soft tissues. While there is existing evidence that ulcer risk decreases as pressure duration decreases, studies have not yet investigated the effect of gradient duration on ulcer risk. Future work should attempt to uncover potential relationships between gradient duration and ulcer risk.
The direction component of PPGs may also provide insight into the localized stresses experienced at the ischial tuberosity. Given various ischial tuberosity pressure distributions with similar PPG magnitudes, pressure ulcer risk may nevertheless be affected by the directions of those PPGs. Under the deformation hypothesis, stresses imposed on the tissues can cause direct cell death. Because the duration of tissue stress remains a significant factor in the deformation hypothesis, changing the PPG direction may serve as a protective mechanism by temporarily redirecting tissue stresses from one area of the ischia to another area before cell death occurs. Under the ischemia hypothesis, PPG redirection may facilitate a localized increase in blood flow to hypoxic tissues. For example, changing a posterior PPG to an anterior PPG may provide a transient increase in blood flow to the posterior compressed tissues at the ischial tuberosity, even if the PPG magnitude remains the same. If PPG directional variance can indeed be shown to lower the risk of ulceration, then PPG directions could increase the locational precision of ulceration diagnosis. For example, rather than identifying a risk of ulceration at the general location of the ischial tuberosity, a stagnant anterior PPG direction could inform clinicians to pay increased attention to the anterior soft tissues at the ischial tuberosity. Future work should investigate the effects of manipulating PPG directions on skin blood flow.
This study had limitations. First, a small, thin laser Doppler probe was placed under the right ischial tuberosity to facilitate the collection of skin perfusion readings for a parallel study (Jan et al., 2010). Thus, we only analyzed the PPG parameters at the left ischial tuberosity. The purpose of the sensor was for the long-term goal of incorporating both interface pressure and skin perfusion in developing a comprehensive model on the effects of wheelchair tilt and recline. Second, only 13 wheelchair users with SCI were recruited. Future work should target a larger sample size to corroborate the current findings. A larger-scale study will also facilitate the testing of the relationship between PPG magnitudes, PPG directions, and pressure ulcer risk. Third, the participants used the same precontoured cushion rather than their everyday cushions. By standardizing the support surface, it was more possible to isolate the effects of tilt and recline on PPG magnitudes and directions. Nevertheless, support surfaces are known to affect interface pressure characteristics. Future work should consider the interactions between PPG, postural changes, as well as support surfaces.
Finally, despite advancements in pressure mapping technologies, modern interface pressure sensels remain somewhat unreliable, which has led to the common practice of replacing peak pressures with sensel averages (e.g., PPI) to increase reliability (Maurer & Sprigle, 2004). PPI provides greater reliability in measurement over maximum single sensor values (Giesbrecht, Ethans, & Staley, 2011). In addition, it has been recommended in the ISO standards and demonstrates good stability in the within and between sessions (S. Sprigle, Dunlop, & Press, 2003). Our method of PPG direction adopting the PPI method as the basis for subsequent calculations. Because the calculation of a gradient involves the subtraction of sensel values, PPG calculations are also affected by sensel reliability. In traditional PPG calculations, original sensel values are used, in spite of these reliability concerns. In this study, we mitigated the sensel reliability limitation by first applying a moving average filter over the sensel values. Thus, the PPG calculations were effectively performed on two PPI values, rather than two sensel values. In this way, our PPG calculation followed the same philosophy as the PPI metric: to increase reliability at the potential cost of sensitivity.
Conclusion
Seating PPG was investigated in response to wheelchair tilt and recline. In the literature, PPG has only been assessed with respect to its magnitude. However, for active interventions such as tilt and recline, dynamic repositioning of the body produces directional changes of force acting on the buttock soft tissues. Thus, while previous studies have only considered magnitudes when assessing PPG, this study also included the directional component. The findings suggested that when combining wheelchair tilt and recline, the recline function may be particularly useful in reducing PPG magnitudes, while the tilt function may be particularly useful in manipulating PPG directions. Furthermore, significant changes in PPG magnitudes did not always correspond to significant changes in PPG directions, suggesting that PPG directional changes may provide additional information for the assessment of interface pressure in response to tilt and recline. Further work is needed to investigate the relationship between PPG directional characteristics and tissue viability.
Acknowledgement
This work was supported by a Campus Research Board Grant (#13288) from the University of Illinois at Urbana-Champaign and the National Institutes of Health (R03HD060751).
Footnotes
Conflict of interest statement: The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be considered as a potential conflict of interest.
References
- Aissaoui R, Lacoste M, & Dansereau J (2001). Analysis of sliding and pressure distribution during repositioning of persons in a simulator chair. IEEE Transactions on Neural Systems and Rehabilitation Engineering, 9(2), 215–223. [DOI] [PubMed] [Google Scholar]
- Akins JS, Karg PE, & Brienza DM (2011). Interface shear and pressure characteristics of wheelchair seat cushions. Journal of Rehabilitation Research and Development, 48(3), 225. doi: 10.1682/jrrd.2009.09.0145 [DOI] [PubMed] [Google Scholar]
- Bennett L, Kavner D, Lee BK, & Trainor FA (1979). Shear vs pressure as causative factors in skin blood flow occlusion. Archives of Physical Medicine and Rehabilitation, 60(7), 309–314. [PubMed] [Google Scholar]
- Bennett L, Kavner D, Lee BY, Trainor FS, & Lewis JM (1984). Skin stress and blood flow in sitting paraplegic patients. Archives of Physical Medicine and Rehabilitation, 65, 186–190. [PubMed] [Google Scholar]
- Brienza DM, Karg P, Geyer MJ, Kelsey S, & Trefler E (2001). The relationship between pressure ulcer incidence and buttock-seat cushion interface pressure in at-risk elderly wheelchair users. Archives of Physical Medicine and Rehabilitation, 82, 529–533. [DOI] [PubMed] [Google Scholar]
- Burns SP, & Betz KL (1999). Seated pressures with conventional and dynamic wheelchair cushions in tetraplegia. Archives of Physical Medicine and Rehabilitation, 80, 566–571. [DOI] [PubMed] [Google Scholar]
- Byrne DW, & Salzberg CA (1996). Major risk factors for pressure ulcers in the spinal cord disabled: A literature review. Spinal Cord, 34(5), 255–263. [DOI] [PubMed] [Google Scholar]
- Chan BC, Nanwa N, Mittmann N, Bryant D, Coyte PC, & Houghton PE (2013). The average cost of pressure ulcer management in a community dwelling spinal cord injury population. Int Wound J, 10(4), 431–440. doi: 10.1111/j.1742-481X.2012.01002.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y, Wang J, Lung CW, Yang TD, Crane BA, & Jan Y-K (2014). Effect of tilt and recline on ischial and coccygeal interface pressures in people with spinal cord injury. American Journal of Physical Medicine and Rehabilitation, 93(12), 1019–1030. [DOI] [PubMed] [Google Scholar]
- Cooper RA, Dvorznak MJ, Rentschler AJ, & Boninger ML (2000). Displacement between the seating surface and hybrid test dummy during transitions with a variable configuration wheelchair: A technical note. J Rehabil Res Dev, 37(3), 297–303. [PubMed] [Google Scholar]
- Crawford SA, Stinson MD, Walsh DM, & Porter-Armstrong AP (2005). Impact of sitting time on seat-interface pressure and on pressure mapping with multiple sclerosis patients. Arch Phys Med Rehabil, 86(6), 1221–1225. doi: 10.1016/j.apmr.2004.08.010 [DOI] [PubMed] [Google Scholar]
- Giesbrecht EM, Ethans KD, & Staley D (2011). Measuring the effect of incremental angles of wheelchair tilt on interface pressure among individuals with spinal cord injury. Spinal Cord, 49(7), 827–831. doi: 10.1038/sc.2010.194 [DOI] [PubMed] [Google Scholar]
- Hobson DA (1992). Comparative effects of posture on pressure and shear at the body-seat interface. Journal of Rehabilitation Research and Development, 29(4), 21–31. [DOI] [PubMed] [Google Scholar]
- Hobson DA, & Tooms RE (1992). Seated lumbar/pelvic alignment: A comparison between spinal cord-injured and noninjured groups. Spine, 17(3), 293–298. [PubMed] [Google Scholar]
- Jan YK, & Brienza DM (2006). Technology for pressure ulcer prevention. Topics in Spinal Cord Injury Rehabilitation, 11(4), 30–41. [Google Scholar]
- Jan YK, Crane BA, Liao F, Woods JA, & Ennis WJ (2013). Comparison of muscle and skin perfusion over the ischial tuberosities in response to wheelchair tilt-in-space and recline angles in people with spinal cord injury. Archives of Physical Medicine and Rehabilitation, 94(10), 1990–1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jan YK, Jones MA, Rabadi MH, Foreman RD, & Thiessen A (2010). Effect of wheelchair tilt-in-space and recline angles on skin perfusion over the ischial tuberosity in people with spinal cord injury. Archives of Physical Medicine and Rehabilitation, 91(11), 1758–1764. doi: 10.1016/j.apmr.2010.07.227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jan YK, Liao F, Jones MA, Rice LA, & Tisdell T (2013). Effect of Durations of Wheelchair Tilt-in-Space and Recline on Skin Perfusion Over the Ischial Tuberosity in People With Spinal Cord Injury. Archives of Physical Medicine and Rehabilitation, 94(4), 667–672. doi: 10.1016/j.apmr.2012.11.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liao F, Burns S, & Jan YK (2013). Skin blood flow dynamics and its role in pressure ulcers. Journal of Tissue Viability, 22(2), 25–36. doi: 10.1016/j.jtv.2013.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loerakker S, Manders E, Strijkers GJ, Nicolay K, Baaijens FP, Bader DL, & Oomens CW (2011). The effects of deformation, ischemia, and reperfusion on the development of muscle damage during prolonged loading. Journal of Applied Physiology, 111(4), 1168–1177. [DOI] [PubMed] [Google Scholar]
- Lung CW, Hsiao-Wecksler ET, Burns S, Lin F, & Jan YK (2016). Quantifying Dynamic Changes in Plantar Pressure Gradient in Diabetics with Peripheral Neuropathy. Front Bioeng Biotechnol, 4, 54. doi: 10.3389/fbioe.2016.00054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lung CW, Yang TD, Crane BA, Elliott J, Dicianno BE, & Jan YK (2014). Investigation of peak pressure index parameters for people with spinal cord injury using wheelchair tilt-in-space and recline: Methodology and preliminary report. BioMed Research International, 2014, 1–9. doi: 10.1155/2014/508583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maurer CL, & Sprigle S (2004). Effect of seat inclination on seated pressures of individuals with spinal cord injury. Physical Therapy, 84, 255–261. [PubMed] [Google Scholar]
- Metring NL, Gaspar MI, Mateus-Vasconcelos EC, Gomes MM, & de Abreu DC (2012). Influence of different types of seat cushions on the static sitting posture in individuals with spinal cord injury. Spinal Cord, 50(8), 627–631. doi: 10.1038/sc.2012.7 [DOI] [PubMed] [Google Scholar]
- National Spinal Cord Injury Statistical Center. (2012). Spinal cord injury facts and figures at a glance. Journal of Spinal Cord Medicine, 35(6), 480–481. doi: 10.1179/1079026812z.000000000124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oleson CG, de Zee M, & Rasmussen J (2010). Missing links in pressure ulcer research - an interdisciplinary review. Journal of Applied Physiology, 108, 1458–1464. doi: 10.1152/japplphysiol.01006.2009.-This [DOI] [PubMed] [Google Scholar]
- Sprigle S, Dunlop W, & Press L (2003). Reliability of bench tests of interface pressure. Assist Technol, 15(1), 49–57. doi: 10.1080/10400435.2003.10131889 [DOI] [PubMed] [Google Scholar]
- Sprigle S, Maurer C, & Soneblum SE (2010). Load redistribution in variable position wheelchairs in people with spinal cord injury. Journal of Spinal Cord Medicine, 33(1), 58–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sprigle S, & Schuch JZ (1993). Using seat contour measurements during seating evaluations of individuals with SCI. Assistive Technology, 5(1), 24–35. [DOI] [PubMed] [Google Scholar]
- Sprigle S, Wootten M, Bresler M, & Flinn N (2002). Development of a noninvasive measure of pelvic and hip angles in seated posture. Archives of Physical Medicine and Rehabilitation, 83(11), 1597–1602. doi: 10.1053/apmr.2002.35468 [DOI] [PubMed] [Google Scholar]
- Tam EW, Mak AF, Lam WN, Evans JH, & Chow YY (2003). Pelvic movement and interface pressure during manual wheelchair propulsion. Archives of Physical Medicine and Rehabilitation, 84, 1466–1472. doi: 10.1016/S0003-9993(03)00269-7 [DOI] [PubMed] [Google Scholar]
- Waugh K, & Crane B (2013). A clinical application guide to standardized wheelchair seating measures of the body and seating support surfaces. Retrieved from Aurora, CO: [Google Scholar]
- Wininger M, & Crane B (2014). Effect of interpolation on parameters extracted from seating interface pressure arrays. Journal of Rehabilitation Research and Development, 51(9), 1365–1375. doi: 10.1682/JRRD.2014.04.0101 [DOI] [PubMed] [Google Scholar]
- Zhang M, & Roberts VC (1993). The effect of shear forces externally applied to skin surface on underlying tissues. Journal of Biomedical Engineering, 15, 451–456. [DOI] [PubMed] [Google Scholar]
- Zou D, Mueller MJ, & Lott DJ (2007). Effect of peak pressure and pressure gradient on subsurface shear stresses in the neuropathic foot. J Biomech, 40(4), 883–890. doi: 10.1016/j.jbiomech.2006.03.005 [DOI] [PubMed] [Google Scholar]