Abstract
Background
To explore the immediate effects and mechanism of acupuncture on craving after tobacco cessation based on the fractional amplitude of low-frequency fluctuation (fALFF).
Methods
This was a functional magnetic resonance imaging (fMRI) study. Forty participants were recruited and divided into a smoking group and a non-smoking group, 20 cases in each one. The smoking participants were requested to quit smoking 24 hours before the fMRI scan. The scan process was scan – acupuncture – scan. Between the two scans, acupuncture was applied at Lieque (LU 7), Hegu (LI 4), Baihui (GV 20), Zusanli (ST 36), Sanyinjiao (SP 6) and Taichong (LR 3) in two groups.
Results
After acupuncture, self-made craving for smoking, Minnesota Nicotine Withdrawal Scale (MNWS) and Questionnaire of Smoking Urges (QSU) were all reduced (P<0.05). The fMRI results indicated the immediate effects of acupuncture on smoking craving were significant, and identified salience network (SN) consisted of anterior cingulate cortex and insula, prefrontal cortex, visual cortex and cerebellum as key brains area. Correlation analysis indicated that NWNS scores were positively correlated with the mean fALFF in the ACC (P<0.05) and negatively correlated with the mean fALFF in the insula (P<0.05) in the smoking group.
Conclusions
This was the first study in China to explore the neural mechanisms of acupuncture for smoking craving. The results indicated that the effects of acupuncture on smoking craving were significant, and the SN played a critical role in the process.
Keywords: Tobacco dependence, acupuncture, functional magnetic resonance imaging (fMRI), salience network (SN)
Introduction
Tobacco use is a significant threat to human health and social development, which is estimated to cause approximately 7 million global deaths each year (1). It is one of the main risk factors driving the growing epidemic of non-communicable diseases (NCDs), especially in China. Currently, a staggering 44% of the world’s cigarettes are smoked in China (2), and one million people die of tobacco-related diseases every year (3), many of them in the prime of their productive years.
Acupuncture, as one of the ancient non-pharmaceutical therapies, is widely accepted in China and is used for pain, stroke, neuropsychiatric diseases, etc. for more than 2000 years. In 1973, acupuncture was firstly used for tobacco cessation in Hong Kong (4). Following this inspiration, a large number of studies explored the efficacy of acupuncture on tobacco cessation. Our previous study has recruited more than 8000 smokers who were treated with acupuncture at Baihui (GV 20), Lieque (LU 7), Hegu (LI 4), Zusanli (ST 36), Sanyinjiao (SP 6), and Taichong (LR 3) for 8 weeks; the self-reported 7-day point abstinence rate was 34.00% at 8 weeks and 18.40% at 52 weeks, indicating acupuncture was safe and effective for smoking cessation (5). The other previous study was Chinese Acupuncture for Tobacco Cessation Research (C-ATCR) (6), which was the most rigorous randomized controlled trial to date; the 24-h point abstinence rate verified by carbon monoxide was 43.00% at 24 weeks in the acupuncture group, which was similar to 44.00% in the NRT group; it provided stronger evidence to support the safety and efficacy of acupuncture for smoking cessation.
However, despite its acceptance and efficacy, the neural mechanisms underlying acupuncture for tobacco cessation have not been well understood and still need to be further investigated. Fortunately, functional neuroimaging technologies have provided a new perspective to improve our understanding of the acupuncture mechanisms by measuring associated changes in blood flow, and emerging evidence suggests that the acupuncture effect was mediated by the central nervous system in humans (7). However, there is little high-quality data about the mechanisms of acupuncture for smoking cessation in China and elsewhere. In the only study reported to date (8), it showed “acupuncture alleviates cue-induced cravings through the regulation of activity in brain regions,” but this study was limited by small sample size and inappropriate methods for acupuncture.
Therefore, built on our previous clinical trials and fMRI studies (9), we designed this study to aimed to (I) observe the immediate effects of acupuncture on smoking craving, and (II) to analyze the resting-state brain function in the participants with 24-h tobacco abstinence by using the fractional amplitude of low-frequency fluctuation (fALFF) approach (10). We hypothesized that acupuncture might relieve the smoking craving through regulation on the reward system.
Methods
Participants
The study was approved by the China Ethics Committee of Registering Clinical Trials (ChiECTCT-2013014) and registered in the Chinese Clinical Trial Registry (ChiCTR-TRC-13003544). All the participants signed the consent forms after informing the purpose and protocol of this study. The scanning site was Guang’anmen Hospital of China Academy of Chinese Medical Sciences (Beijing, China).
All the participants were recruited via a local newspaper, community events, hospital websites, and recommendation from other medical institutions. The participants were included into a smoking group if they voluntarily participated in this study, right-handed, aged between 30 to 70 years, smoked more than ten cigarettes per day in last ten years and had not undergone smoking abstinence longer than three months in the past year. The participants were included in a non-smoking group if they voluntarily participated in this study, right-handed, aged between 18 to 70 years, not smoked during the past ten years. The participants were excluded if they had mental diseases, severe cardiovascular diseases, apoplexy or nervous system diseases, had disturbances of blood coagulation or were pregnant.
Study procedure
This study consisted of the recruitment period, preparation period, and scanning period. In the recruitment period, the participants who met the criteria above were recruited. After signing the consent forms, they received a 1-hour preliminary evaluation and waited for scanning date.
In the preparation period, firstly, the study team scheduled the scan date with the fMRI technology team and then told all the participants. Secondly, the smoking participants were required to quit smoking 24 hours before the scan date. Finally, all the participants were measured with exhaled breath CO machine (purchased from Bedfont Scientific Company, Maidstone, British) with the result <6 ppm as the qualification for fMRI scan on the scan day.
In the scan period, the scan process was scan – acupuncture – scan. During the scan, the participants were in supine position; a foam pillow was used to minimize head movement, and rubber headphones were used to reduce the noise. The participants were required to rest with closed eyes and quiet breathing, not deliberately think. Acupuncture was applied between two scans. After two scans, fMRI data were collected.
Acupuncture treatment
Selection of acupoints
Baihui (GV 20), Lieque (LU 7), Hegu (LI 4), Zusanli (ST 36), Sanyinjiao (SP 6) and Taichong (LR 3), according to the Acupuncture point locations in the Western Pacific Region by World Health Organization (Figure S1) (11).
Figure S1.
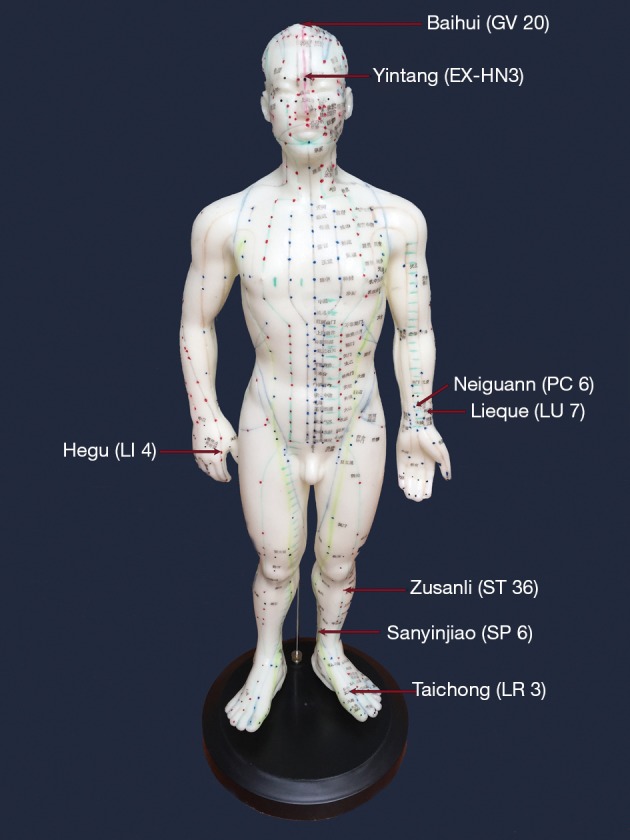
Location of acupoints for tobacco cessation.
Body position
Subjects were in supine to expose the body acupoints.
Needle specification
0.25 mm × 40 mm disposable sterile needles were used (Purchased from Suzhou Medical Appliance Factory, Jiangsu Province, China).
Manipulation of acupuncture
Routine fertilization was given on the selected acupoints with 75% medicinal alcohol before acupuncture. Needles were horizontally inserted at Baihui (GV 20) while vertically inserted at other acupoints with a depth of 25 to 50 mm. The mild reinforcing and reducing technique were applied at all acupoints. The arrival of qi (needle sensation) was required, and needles were required to stay at the acupoints for 30 min. Meanwhile, electroacupuncture device (HuaTuo SDZ-III type) was used and connected at Lieque (LU 7) and Zusanli (ST 36) with continuous wave (15 Hz) for 30 min. The needles were withdrawn quickly to avoid bleeding or hematoma.
Acupuncture duration
Thirty minutes.
Quality control of acupuncture
All the acupuncturists participated in this study were certified by the China Administration of Traditional Chinese Medicine, with the collective acupuncture experience of ten years to guarantee the consistency of acupuncture treatment. A study researcher and an acupuncturist performed the acupuncture treatment. The acupuncturist was responsible for the clinical treatment while the study researcher recorded data to maintain the accuracy and consistency of this study.
fMRI data acquisition
The fMRI data were acquired on a 1.5 Tesla GE Signa MRI scanner (GE Healthcare, Buckinghamshire, United Kingdom) equipped with the standard two-channel birdcage head coil. T1-weighted high-resolution structural images were acquired with the three-dimensional fast spoiled gradient-echo sequence (matrix was 256×192, the field of view was 200 mm, the flip angle was 15 degrees, slice thickness was 1.4 mm). T2-weighted functional images were acquired with the gradient echo echoplanar imaging sequence (echo time was 30 msec, repetition time was 2,500 msec, the matrix was 64×64, FOV was 240 mm, the flip angle was 90 degrees, slice thickness was 3.0 mm, voxel size was 3 mm × 3 mm ×3 mm, the gap was 0.5 mm, 43 slices. Image collection was preceded by four dummy scans to allow for equilibration of the MRI signal.
Data Processing Assistant for Resting-State fMRI (DPARSF) (12) software developed by State Key Laboratory of Cognitive Neuroscience and Learning of Beijing Normal University was used for fMRI data processing and calculating fALFF under the Matlab 12.0 platform. Data preprocessing includes DICOM data format conversion, the removal of the first ten time points, slice timing, realign, normalize, smoothing, detrend, and regress out nuisance covariates. Resting-state fMRI Data Analysis Toolkit (REST) software was used to calculate the value of fALFF in each participant. The P value was set at <0.05, with AlphaSim corrected.
Measures of craving for smoking
A self-made one-item ten-point scale, a 9-item version of Minnesota Nicotine Withdrawal Scale (MNWS) and a 9-item version of Questionnaire of Smoking Urges (QSU) were used to measure the pre-scan and post-scan craving for smoking. High score of the three scales indicated intense craving for smoking. Each subject completed the three measures before the beginning of the 1st scanning session and after the end of the 2nd scanning session.
Statistical analysis
SPSS 19.0 statistical software was used for statistical analysis. The measurement data were represented with means ± standard deviation (x±s). T-test was used for comparison which met Gaussian distribution and homogeneity of variance, while the non-parametric test was used for comparison which did not meet homogeneity of variance. Chi-square test was used for enumeration data. P<0.05 was taken as statistical significance. The authors had no access to information that could identify individual participant during or after data collection.
Results
Study flow and description of participants
From September to December of 2017, 52 participants were recruited. Twenty participants in the smoking group and 20 participants in the non-smoking group finished the study and included in the analysis (Figure S2). Moreover, no adverse events were observed during the acupuncture treatment.
Figure S2.
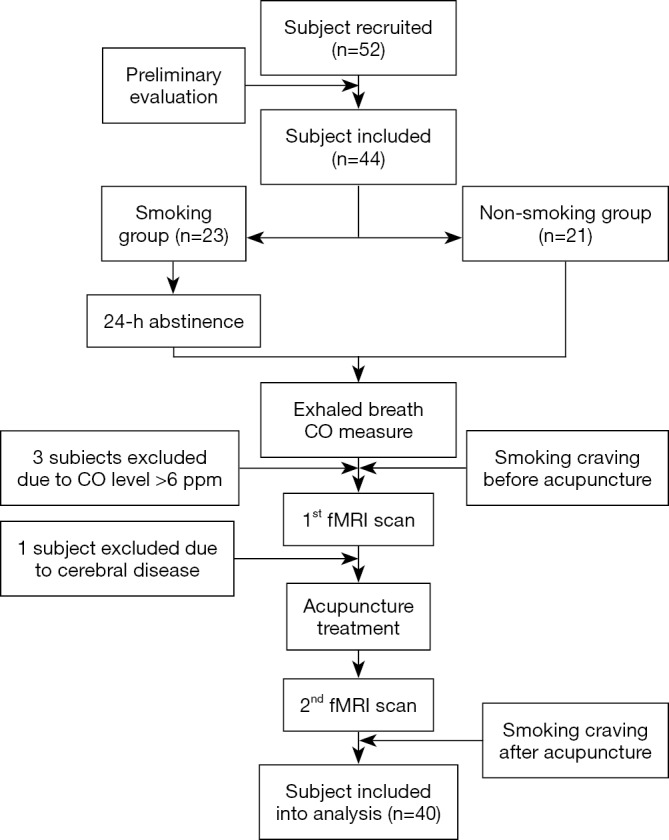
Flow chart of the participants.
The baseline characteristics were well balanced between the two groups (Table 1). The only imbalance noted was a self-reported health score on a scale of 0–100 points (P<0.05). Also, the smoking pattern indicated moderate tobacco dependence in smoking participants, while the three craving scales indicated an intense craving for smoking before acupuncture.
Table 1. Baseline characteristics of subjects.
| Baseline data | Smoking group (n=20) | Non-smoking group (n=20) |
|---|---|---|
| Gender | ||
| Male | 19 | 18 |
| Female | 1 | 2 |
| Age (years) | 40.50±12.72 | 39.54±6.24 |
| 30–40 | 11 | 13 |
| 41–60 | 8 | 7 |
| 61 and above | 1 | 0 |
| Ethnicity | ||
| Han | 19 | 19 |
| Others | 1 | 1 |
| Marriage | ||
| Yes | 17 | 18 |
| No | 3 | 2 |
| Education | ||
| College | 16 | 17 |
| Below College | 4 | 3 |
| BMI | 24.46±4.17 | 23.60±2.91 |
| Self-reported health score | 83.89±15.77 | 86.15±10.44 |
| Drinking | ||
| Yes | 3 | 5 |
| No | 17 | 15 |
| Smoking duration (years) | 20.28±12.64 | NA |
| Cigarettes smoked per day | 21.44±9.93 | NA |
| FTND | 4.72±2.72 | NA |
| Craving before acupuncture | ||
| Self-made scale | 6.33±2.09 | NA |
| MNWS | 11.83±10.40 | NA |
| QSU | 38.50±19.71 | NA |
FTND, Fagerstrom Test for Nicotine Dependence; MNWS, Minnesota Nicotine Withdrawal Scale; QSU, Questionnaire of Smoking Urges; NA, not applicable.
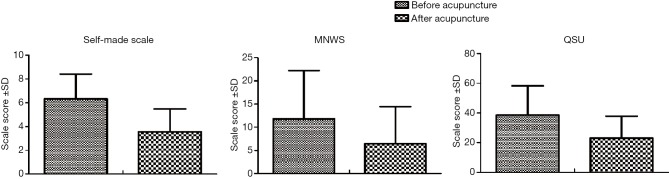
Smoking craving measures results
As was shown in Figure 1, in the smoking group, 24-hour abstinence from smoking resulted in significant smoking craving; after acupuncture, the smoking craving was significantly reduced as measured by three types of scales (P<0.05).
Figure 1.
Three types of scales for craving before and after acupuncture. MNWS, Minnesota Nicotine Withdrawal Scale; QSU, Questionnaire of Smoking Urges.
fMRI results
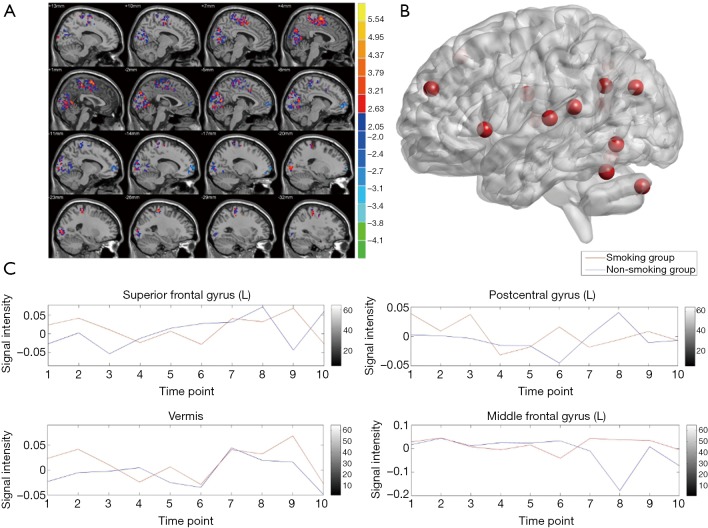
fALFF before acupuncture in the smoking group and non-smoking group
As was shown in Figure 2 and Table S1, before acupuncture, compared between smoking group and non-smoking group, significant activation was observed in the left calcarine (BA 17), left cuneus (BA 18), vermis and right postcentral gyrus (BA 3), while the deactivation was observed in left superior frontal gyrus (BA 11) and middle frontal gyrus (BA 44).
Figure 2.
Brain areas with altered fALFF before acupuncture between two groups. (A) areas in blue indicated brain areas where fALFF was significantly decreased while areas in red indicated brain areas where fALFF was significantly increased, sagittal view, Alphasim corrected, P<0.05; (B) red sphere indicated areas where fALFF was significantly changed, sagittal view, Alphasim corrected, P<0.05; (C) time-course of signal change within 4 different brain areas between smoking group and non-smoking group. fALFF, fractional amplitude of low-frequency fluctuation.
Table S1. Brain areas with altered fALFF before acupuncture between two groups.
| Brain area | MNI coordinates | Intensity | Voxel size | Anatomy | Side | BA | ||
|---|---|---|---|---|---|---|---|---|
| X | Y | Z | ||||||
| Frontal lobe | −18 | 69 | 0 | −4.52 | 73 | Superior frontal gyrus | L | 11 |
| −51 | 18 | 42 | −3.60 | 77 | Middle frontal gyrus | L | 44 | |
| Occipital lobe | −1 | −78 | 7 | 1.16 | 80 | Calcarine | L | 17 |
| −6 | −82 | 31 | 3.35 | 112 | Cuneus | L | 18 | |
| Others | −3 | −60 | 0 | 4.43 | 609 | Vermis | ||
| 57 | −6 | 36 | 6.12 | 1,168 | Postcentral gyrus | R | 3 | |
fALFF, fractional amplitude of low-frequency fluctuation.
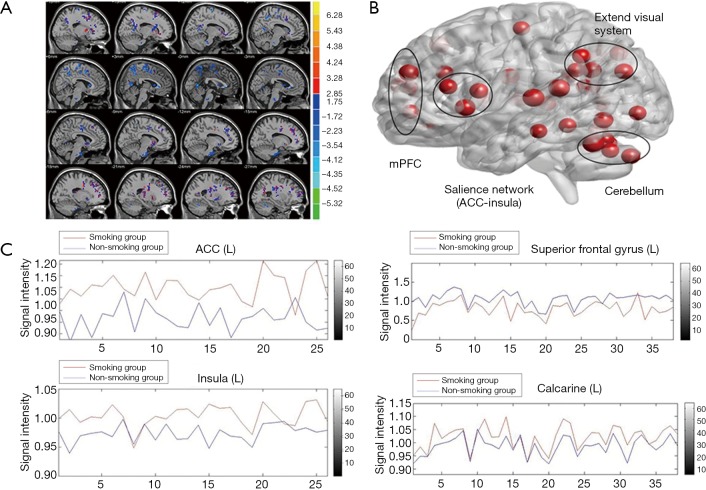
fALFF before and after acupuncture in the smoking group
As was shown in Figure 3 and Table S2, after acupuncture, in smoking group the areas with significantly increased fALFF included bilateral postcentral gyrus (BA 4), right middle frontal gyrus (BA 9), right dorsal lateral prefrontal cortex (DLPFC, BA 8), right middle occipital gyrus (BA 19), right calcarine (BA 17), left insula (BA 48) and right pallidum; the areas with significantly decreased fALFF included left middle occipital gyrus (BA 18), left precuneus, left middle temporal gyrus (BA 21), right anterior cingulate gyrus (BA 11) and right supplementary motor area (BA 6).
Figure 3.
Brain areas with altered fALFF after acupuncture between two groups. (A) areas in blue indicated brain areas where fALFF was significantly decreased while areas in red indicated brain areas where fALFF was significantly increased, sagittal view, Alphasim corrected, P<0.05; (B) red sphere indicated areas where fALFF was significantly changed, sagittal view, Alphasim corrected, P<0.05; (C) time-course of signal change within 4 different brain areas between smoking group and non-smoking group. fALFF, fractional amplitude of low-frequency fluctuation.
Table S2. Brain areas with altered fALFF before and after acupuncture in smoking group.
| Brain area | MNI coordinates | Intensity | Voxel size | Anatomy | Side | BA | ||
|---|---|---|---|---|---|---|---|---|
| X | Y | Z | ||||||
| Frontal lobe | 48 | −12 | 33 | 4.28 | 109 | Postcentral gyrus | R | 4 |
| 36 | −27 | 72 | 4.07 | 65 | Precentral gyrus | R | 4 | |
| 42 | 15 | 45 | 4.15 | 91 | Middle frontal gyrus | R | 9 | |
| 15 | 15 | 57 | 3.77 | 121 | DLPFC | R | 8 | |
| Occipital lobe | −36 | −93 | 3 | −3.20 | 41 | Middle occipital gyrus | L | 18 |
| 42 | −69 | 33 | 3.75 | 97 | Middle occipital gyrus | R | 19 | |
| 0 | −51 | 66 | −4.17 | 138 | Precuneus | L | ||
| 15 | −102 | 0 | 5.29 | 116 | Calcarine | R | 17 | |
| Temporal lobe | −51 | −33 | 0 | −3.68 | 79 | Middle temporal gyrus | L | 21 |
| Others | 6 | 41 | 0 | −4.19 | 87 | ACC | R | 24 |
| 12 | −15 | 72 | −4.13 | 195 | Supplementary motor area | R | 6 | |
| −30 | 27 | 12 | 3.80 | 134 | Insula | L | 48 | |
| 6 | −57 | −48 | −3.75 | 63 | Cerebellum | R | ||
| 18 | 9 | 0 | 5.83 | 295 | Pallidum | R | ||
fALFF, fractional amplitude of low-frequency fluctuation; MNI, Montreal Neurological Institute; DLPFC, dorsal lateral prefrontal cortex; ACC, anterior cingulate cortex.
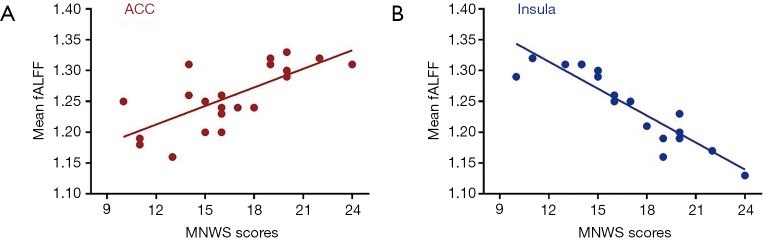
Correlation analysis result
The correlation analysis results indicated that the NWNS scores were positively correlated with the mean fALFF in the ACC (P<0.05) and negatively correlated with the mean fALFF in the insula (P<0.05) in the smoking group (Figure S3).
Figure S3.
Correlation analysis of acupuncture for tobacco cessation. Correlation between the mean fALFF and MNWS scores in the smoking group. (A) Significant positive correlations between the fALFF in the ACC and MNWS scores (P<0.05); (B) significant negative correlations between the fALFF in the insula and with MNWS scores (P<0.05). fALFF, fractional amplitude of low-frequency fluctuation; MNWS, Minnesota Nicotine Withdrawal Scale; ACC, anterior cingulate cortex.
Discussion
According to our knowledge, this was the first study in China to explore the neural mechanisms of acupuncture for smoking craving. The results indicated that the immediate effects of acupuncture on smoking craving were significant and identified ACC, insula, PFC, visual cortex, and cerebellum as key brains area. Consistent with the previous study, these changes might be related to decreasing salience of smoking and increasing the ability to resist the craving, respectively.
Nicotine-addicted individuals are known to exhibit deficits in central neural systems. A review by Jasinska (13) summarized that nicotine had a dual action in the brain: it promoted addiction, and it modulated cognition. Nicotine’s role in addiction was associated primarily with mesolimbic DA pathways connecting the VTA with the amygdala, whereas its effect on cognition was mediated by the mesocortical DA pathways connecting the VTA with the cortical regions. From the anatomical and fMRI evidence, ACC was the final projections of the mesocorticolimbic dopamine system and was known to control the urge to smoke (14). The insula played a critical role in tobacco dependence. Smokers with damage to insula were reported to more likely to quit and remain abstinent (15). More importantly, salience network (SN) (16), consisted of ACC and insula, was a switch between default mode network (DMN) and central executive network (CEN), and was thought to facilitate the processing of relevant stimuli arising from internal or external sources. Furthermore, the results showed that MNWS scores in the smoking group were negatively correlated with the fALFF in the insula and positively correlated with fALFF in the ACC. As such, on the contrary to our hypothesis that acupuncture might relieve the smoking craving through regulation on the reward system, we speculated the immediate effects of acupuncture on smoking craving was to improve the cognition function through ACC and insula circuit, leading to better executive function and impulsivity control.
Apart from ACC and insula of SN, PFC, which covers the front part of the frontal lobe, was prominent in addictive behavior, and was considered as the command and control center of brain (17); and it was implicated in decision making and planning selection, which may contribute to withdrawal symptoms, tobacco craving, and cognitive impairments. This was consistent with our results, indicating that smokers with 24-h abstinence had impaired execution function and impulsivity control. Unlike cue-reactivity fMRI studies, no obvious smoking cues were provided during our study. However, smokers with 24-h abstinence still showed vision-related activity in the brain (calcarine and cuneus). The reasons may be the increased allocation of attention to the smoking signal due to smoking withdrawal. Also, the cerebellum is one of the brain areas of NAChRs in the brain (18). In the present study, the activity of cerebellar nerve in the smoking group was reduced after acupuncture. This might show that the regulation of acupuncture on cerebellum is one of the critical neurological points for the basis of acupuncture for stopping smoking.
The strengths of our study included biochemical verification of smoking status, verified acupuncture treatment procedure, and resting-state fMRI design. Firstly, we used biochemical verification in this study not only because it was highly specific, simple and relatively inexpensive (19), but also it guaranteed 24 h-abstinence from smoking so the effects of acupuncture on smoking craving could be investigated. Secondly, the acupuncture treatment adopted in this study was built on our previous literature research (4) and clinical studies (5,6). Lastly, acupuncture could induce sustained effects or even after needling manipulation being suspended (20), and the neural responses to acupuncture stimulation have carryover effects. In consideration of these characteristics, although task state was used as a classical method of acupuncture research, this study applied a resting-state type to simplify the fMRI protocol, avoid head movement during the scan period and accurately collect the data.
Our study had several limitations. Firstly, our study only investigated the short-term mechanism of acupuncture on smoking craving so the result might not reflect the overall efficacy of acupuncture. Secondly, the relatively small sample size was another limitation. Thirdly, the participants were mainly male, and the effects on female were still unclear. Finally, fMRI was an indirect method to measure blood oxygen saturation and the changes in blood flow, which could not directly display the function of nerve activity.
Conclusions
This was the first study in China to explore the neural mechanisms of acupuncture for smoking craving. The results indicated that the effects of acupuncture on smoking craving were significant, where SN played a critical role in the process. Prospective studies are needed to explore the neural mechanisms of long-term acupuncture on tobacco dependence.
Acknowledgments
Funding: This paper is supported by the Special Scientific Research Fund of Traditional Chinese Medicine of China (Project No. 201307014) and the Fundamental Research Funds for National Natural Science Foundation of China (81774433).
Ethical Statement: The study was approved by the China Ethics Committee of Registering Clinical Trials (ChiECTCT-2013014) and registered in the Chinese Clinical Trial Registry (ChiCTR-TRC-13003544). All the participants signed the consent forms after informing the purpose and protocol of this study.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Ministry of Health of People’s Republic of China. China Report on the Health Hazards of Smoking. Beijing: People‘s Medical Publishing House, 2012. [Google Scholar]
- 2.World Health Organization. The bill China cannot afford: health, economic and social costs of China’s tobacco epidemic. Manila, Philippines: World Health Organization Regional Office for the Western Pacific, 2017. [Google Scholar]
- 3.Chen Z, Peto R, Zhou M, Iona A, Smith M, Yang L, Guo Y, Chen Y, Bian Z, Lancaster G, Sherliker P, Pang S, Wang H, Su H, Wu M, Wu X, Chen J, Collins R, Li L, China Kadoorie Biobank (CKB) collaborative group Contrasting male and female trends in tobacco-attributed mortality in China: evidence from successive nationwide prospective cohort studies. Lancet 2015;386:1447-56. 10.1016/S0140-6736(15)00340-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liu Z, Wang Y, Wu Y, Yang J. Condition and effectiveness evaluation of acupuncture for smoking cessation. Zhongguo Zhen Jiu 2015;35:851-7. [PubMed] [Google Scholar]
- 5.Wang YY, Liu Z, Wu Y, Zhang O, Chen M, Huang LL, He XQ, Wu GY, Yang JS. Acupuncture for Smoking Cessation in Hong Kong: A Prospective Multicenter Observational Study. Evid Based Complement Alternat Med 2016;2016:2865831. 10.1155/2016/2865831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang YY, Liu Z, Wu Y, Yang L, Guo LT, Zhang HB, Yang JS, Chinese Acupuncture for Tobacco Cessation Research Team Efficacy of Acupuncture Is Noninferior to Nicotine Replacement Therapy for Tobacco Cessation: Results of a Prospective, Randomized, Active-Controlled Open-Label Trial. Chest 2018;153:680-8. 10.1016/j.chest.2017.11.015 [DOI] [PubMed] [Google Scholar]
- 7.He T, Zhu W, Du SQ, Yang JW, Li F, Yang BF, Shi GX, Liu CZ. Neural mechanisms of acupuncture as revealed by fMRI studies. Auton Neurosci 2015;190:1-9. 10.1016/j.autneu.2015.03.006 [DOI] [PubMed] [Google Scholar]
- 8.Kang OS, Kim SY, Jahng GH, Kim H, Kim JW, Chung SY, Kim JW, Yang SI, Park HJ, Lee H, Chae Y. Neural substrates of acupuncture in the modulation of cravings induced by smoking-related visual cues: an fMRI study. Psychopharmacology (Berl) 2013;228:119-27. 10.1007/s00213-013-3015-y [DOI] [PubMed] [Google Scholar]
- 9.Fang J, Egorova N, Rong P, Liu J, Hong Y, Fan Y, Wang X, Wang H, Yu Y, Ma Y, Xu C, Li S, Zhao J, Luo M, Zhu B, Kong J. Early cortical biomarkers of longitudinal transcutaneous vagus nerve stimulation treatment success in depression. Neuroimage Clin 2016;14:105-11. 10.1016/j.nicl.2016.12.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang JJ, Chen X, Sah SK, Zeng C, Li YM, Li N, Liu MQ, Du SL. Amplitude of low-frequency fluctuation (ALFF) and fractional ALFF in migraine patients: a resting-state functional MRI study. Clin. Radiol 2016;71:558-64. 10.1016/j.crad.2016.03.004 [DOI] [PubMed] [Google Scholar]
- 11.WHO Regional Office for the Western Pacific, Acupuncture Point Locations in the Western Pacific Region, World Health Organization. Western Pacific Region, Beijing, China, 2008. [Google Scholar]
- 12.Chao-Gan Y, Yu-Feng Z. DPARSF: A MATLAB Toolbox for ‘Pipeline’ Data Analysis of Resting-State fMRI. Front Syst Neurosci 2010;4:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jasinska AJ, Zorick T, Brody AL, Stein EA. Dual role of nicotine in addiction and cognition: a review of neuroimaging studies in humans. Neuropharmacology 2014;84:111-22. 10.1016/j.neuropharm.2013.02.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Janes AC, Farmer S, Peechatka AL, Frederick Bde B, Lukas SE. Insula-dorsal anterior cingulate cortex coupling is associated with enhanced brain reactivity to smoking cues. Neuropsychopharmacology 2015;40:1561-8. 10.1038/npp.2015.9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moran LV, Sampath H, Stein EA, Hong LE. Insular and anterior cingulate circuits in smokers with schizophrenia. Schizophr Res 2012;142:223-9. 10.1016/j.schres.2012.08.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bonnelle V, Ham TE, Leech R, Kinnunen KM, Mehta MA, Greenwood RJ, Sharp DJ. Salience network integrity predicts default mode network function after traumatic brain injury. Proc Natl Acad Sci U S A 2012;109:4690-5. 10.1073/pnas.1113455109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Janes AC, Pizzagalli DA, Richardt S, deB Frederick B, Chuzi S, Pachas G, Culhane MA, Holmes AJ, Fava M, Evins AE, Kaufman MJ. Brain reactivity to smoking cues prior to smoking cessation predicts ability to maintain tobacco abstinence. Biol Psychiatry 2010;67:722-9. 10.1016/j.biopsych.2009.12.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hahn B, Ross TJ, Yang Y, Kim I, Huestis MA, Stein EA. Nicotine enhances visuospatial attention by deactivating areas of the resting brain default. J Neurosci 2007;27:3477-89. 10.1523/JNEUROSCI.5129-06.2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hughes JR, Keely JP, Niaura RS, Ossip-Klein DJ, Richmond RL, Swan GE. Measures of abstinence in clinical trials: issues and recommendations. Nicotine Tob Res 2003;5:13-25. 10.1080/1462220031000070552 [DOI] [PubMed] [Google Scholar]
- 20.Cai RL, Shen GM, Wang H, Guan YY. Brain functional connectivity network studies of acupuncture: a systematic review on resting-state fMRI. J Integr Med 2018;16:26-33. 10.1016/j.joim.2017.12.002 [DOI] [PubMed] [Google Scholar]