Dear Editor,
Minimally invasive glaucoma surgery (MIGS) is a less-invasive surgical alternative to filtering surgery for reducing intraocular pressure (IOP). This technique has been shown to offer long-term outcomes equivalent to filtering surgery[1]. The XEN gel implant (Allergan Inc., CA, USA) is one of MIGS procedures. This implant consists of a 6-mm tube of collagen-derived gelatin cross-linked with glutaraldehyde, preloaded in an injector. The XEN gel implant is implanted ab interno. It produces a drainage pathway between the anterior chamber and the subconjunctival space. The XEN® gel implant has been developed for the surgical management of refractory glaucoma. This simplified technique leads to less post-surgical complications, such as hypotony and choroidal detachment, than filtering surgery[1]. However, there are very few reports of complications following MIGS procedures, in particular for XEN gel implant[1]–[2].
Here, we report a total hyphema that occurred after an uncomplicated ab interno XEN gel stent surgery. Consent to publish the case report was not obtained. This report does not contain any personal information that could lead to identification of the patient. This report was performed in compliance with the Declaration of Helsinki.
A 72-year-old male was referred for an evaluation of ocular hypertension. His past medical history included a Bentall procedure, a graft replacement of the aortic valve, aortic root and ascending aorta and an atrial fibrillation. He was treated with acetylsalicylic acid (Kardegic® 75 mg/d), and fluindione (Previscan®) with a target international normalized ratio of between 2 and 3. His past ocular history included severe myopia (Figures 1 and 2), open-angle glaucoma, and cataract surgery in both eyes. He was under local treatment with bimatoprost 0.03% (Allergan, Inc., Irvine, California, USA) at bedtime, a dorzolamide/timolol combination 0.2%/0.5% (Merck Canada Inc., Kirkland, Quebec) twice daily in both eyes. On initial examination, the best corrected visual acuity was 20/20 in each eye. IOP was measured at 20 mm Hg in the right eye and 26 mm Hg in the left eye using Goldman applanation tonometer. As IOP in the left eye was poorly controlled with the maximally tolerated medications and there was evidence of progression in the visual fields, and therefore IOP-lowering surgery was recommended. After an informed discussion with the patient, he agreed to proceed with the XEN gel stent implant to his left eye in the superonasal quadrant. During the 3-month follow-up, IOP measurement was stable at 11 mm Hg in the operated eye without antiglaucoma medications. As the surgery to the left eye was effective, and the patient agreed to proceed with the XEN gel stent implant to his right eye after having been given an exhaustive information. The patient was initially referred to us by his ophthalmologist for a functional aggravation. There was no change of oral treatment regimen around the timing of the XEN gel stent surgery. The surgical procedure was performed with no complications. Three hours after surgery, the XEN gel stent was well placed with effective filtration and no blood in the anterior chamber or the subconjunctival space was observed. Two days postoperatively, the patient presented with a total hyphema (grade 4) in the right eye and IOP measurement was 10 mm Hg. The patient didn't report neither ocular traumatism, neither straining, Valsalva manoeuvre nor general body traumatism at the incident. The retina appeared to be attached on the B-Mode ultrasound imaging (Figure 3). No subconjunctival hemorrhage was observed post-operatively. The bleb was formed and its shape remained the same before and after the hyphema. Neither medical nor surgical treatment have been prescribed for the hyphema. The patient was asked to drink at least 1.5 liter of water a day and to sleep in a half-sitting position. Seven days post-operatively, the hyphema decreased markedly. The hyphema height was 3 mm and improved from grade 4 to grade 1 (less than 1/3 of the anterior chamber) without any additional treatment. IOP measurement was 15 mm Hg in this eye. One month after surgery, IOP of the right eye measurement was 11 mm Hg and the hyphema resolved spontaneously. The slit lamp examination was unremarkable. The XEN gel stent was well placed with effective filtration and the patient recovered a visual acuity of 20/20 with no other complications.
Figure 1. Infrared image of the right and left optic nerve heads showing a dysversion, a peripapillary atrophy and the staphyloma of both optic nerve heads.

Figure 2. Optic coherence tomography of the optic nerve head evaluating the retinal nerve fiber layer.
The analysis is not reliable because of the optic nerve heads' conformation.
Figure 3. B-mode ultrasound imaging of right eye two days postoperatively.
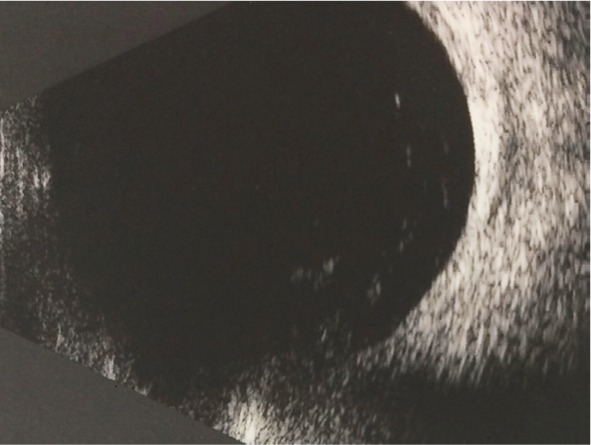
The retina appeared to be attached. Neither choroidal detachment nor choroidal hemorrhage was noted.
The aims of MIGS are to provide an alternative and less invasive surgical treatment for reducing IOP to filtering surgery. The XEN gel stent has the potential to keep the patient off IOP-lowering treatment unlike other MIGS procedures[2]–[3].
Recently, De Gregorio et al[4] prospectively studied the implantation of XEN gel stents in 41 patients. Intraoperative complications included subconjunctival hemorrhage in 36.5% patients, transient anterior chamber hyphema in 24.3% patients, and stent malpositioning requiring repositioning in 12.2% patients were reported. Schlenker et al[1] performed a retrospective cohort study of 354 patients who underwent XEN gel stent procedure or trabeculectomy. Among the most common complication in the XEN gel stent group, malignant glaucoma (n=4) conjunctival wound leak (n=3), hyphema (n=2), vitreous hemorrhage (n=2), hypotony maculopathy (n=2), choroidal effusion (n=1), stent obstruction (n=1) or exposed stent (n=1), and Dellen formation (n=2) were reported.
In our case, the surgical procedure was performed with no complications. The immediate postoperative exam did not reveal any intraocular or subconjunctival bleeding. Indeed, three hours after surgery, the XEN gel stent was well placed with effective filtration and no blood in the anterior chamber or the subconjunctival space. The total hyphema was reported two days after the surgery. Perhaps a slow trickle intraoperative hyphema would have been observed if the patient had been examined at day 1. In our case, the time delay might be explained by the onset of a delayed and transient hypotony[5]. Indeed, hyphema can be produced by postoperative hypotony with inherent reversal of the pressure gradient between episcleral venous pressure and intraocular pressure. In MIGS, the physiologic outflow system is restored. Hence, the hyphema might represent blood refluxed from the episcleral venous system through the XEN gel stent[6]. However, no hypotony has been noted. IOP was measured at 10 mm Hg in this eye. Most hyphemas following intraocular surgery occur at the time or in the immediate post-operative period. The source of the bleeding appears to be the iris root[7]. Furthermore, eyes with larger hyphema may have a more rapid wash-out than eyes with smaller hyphema, possibly due to the increased permeability and patency of the trabecular meshwork induced by XEN gel stent. One can hypothesize that a subconjunctival hemorrhage would have been observed if the patient had been examined between the seven-day visit and the one-month visit.
The patient was treated with a vitamin K antagonist associated with an antiplatelet therapy that increases the risk of bleeding. Systemic anticoagulation and antiplatelet therapy are widely used for the treatment and prevention of thromboembolic events[8]. Stopping these treatments may increase the risk of life-threatening systemic complications such as cerebrovascular accidents or embolic disease. Ophthalmologists are currently dealing with larger numbers of patients undergoing anticoagulant and antiplatelet treatment and requiring ophthalmic surgery and this trend is set to continue. According to the French Glaucoma Society, no systematic approach can be recommended. Any decision to discontinue or modify an antiplatelet therapy or an anticoagulant treatment before glaucoma surgery must be made after the careful evaluation of the benefits and risks with patients, anesthesiologists and cardiologists. Our patient was considered to have a high risk of thromboembolic events because of a graft replacement of the aortic valve and an atrial fibrillation. Discontinuing his treatment would have been life-threatening[9].
XEN gel stent is generally well tolerated, but not without risks, in particular for patients under antiplatelet or anticoagulant therapy. Although hyphema usually resolves spontaneously, patients must be provided with comprehensive information on the benefits and risks.
Acknowledgments
Conflicts of Interest: Rezkallah A, None; Mathis T, None; Denis P is consultant for Alcon, Allergan, Novartis and Théa; Kodjikian L is consultant for Abbvie, Allergan, Alimera, Bayer, Novartis, Roche and Théa.
REFERENCES
- 1.Schlenker MB, Gulamhusein H, Conrad-Hengerer I, Somers A, Lenzhofer M, Stalmans I, Reitsamer H, Hengerer FH, Ahmed IIK. Efficacy, safety, and risk factors for failure of standalone ab interno gelatin microstent implantation versus standalone trabeculectomy. Ophthalmology. 2017;124(11):1579–1588. doi: 10.1016/j.ophtha.2017.05.004. [DOI] [PubMed] [Google Scholar]
- 2.Widder RA, Dietlein TS, Dinslage S, Kühnrich P, Rennings C, Rössler G. The XEN45 Gel Stent as a minimally invasive procedure in glaucoma surgery: success rates, risk profile, and rates of re-surgery after 261 surgeries. Graefes Arch Clin Exp Ophthalmol. 2018;256(4):765–771. doi: 10.1007/s00417-018-3899-7. [DOI] [PubMed] [Google Scholar]
- 3.Gonnermann J, Bertelmann E, Pahlitzsch M, Maier-Wenzel AB, Torun N, Klamann MK. Contralateral eye comparison study in MICS & MIGS: Trabectome® vs. iStent inject®. Graefes Arch Clin Exp Ophthalmol. 2017;255(2):359–365. doi: 10.1007/s00417-016-3514-8. [DOI] [PubMed] [Google Scholar]
- 4.De Gregorio A, Pedrotti E, Russo L, Morselli S. Minimally invasive combined glaucoma and cataract surgery: clinical results of the smallest ab interno gel stent. Int Ophthalmol. 2018;38(3):1129–1134. doi: 10.1007/s10792-017-0571-x. [DOI] [PubMed] [Google Scholar]
- 5.Koch JM, Heiligenhaus A, Heinz C. Canaloplasty and transient anterior chamber haemorrhage: a prognostic factor? Klin Monbl Augenheilkd. 2011;228(5):465–467. doi: 10.1055/s-0029-1245486. [DOI] [PubMed] [Google Scholar]
- 6.Grieshaber MC, Schoetzau A, Flammer J, Orgül S. Postoperative microhyphema as a positive prognostic indicator in canaloplasty. Acta Ophthalmol. 2013;91(2):151–156. doi: 10.1111/j.1755-3768.2011.02293.x. [DOI] [PubMed] [Google Scholar]
- 7.Sharan S, Painter G, Grigg JR. Total hyphema following postoperative enoxaparin (Clexane) Eye (Lond) 2005;19(7):827–828. doi: 10.1038/sj.eye.6701664. [DOI] [PubMed] [Google Scholar]
- 8.Kakkos SK, Kirkilesis GI, Tsolakis IA. Editor's Choice-efficacy and safety of the new oral anticoagulants dabigatran, rivaroxaban, apixaban, and edoxaban in the treatment and secondary prevention of venous thromboembolism: a systematic review and meta-analysis of phase III trials. Eur J Vasc Endovasc Surg. 2014;48(5):565–575. doi: 10.1016/j.ejvs.2014.05.001. [DOI] [PubMed] [Google Scholar]
- 9.Recommandations SFG/SFO: Gestion des traitements anticoagulants et anti-aggrégants dans la chirurgie du glaucome. http://www.leglaucome.fr/2014/recommandations-sfgsfo-gestion-des-traitements-anticoagulants-et-anti-aggregants-dans-la-chirurgie-du-glaucome/.



