History
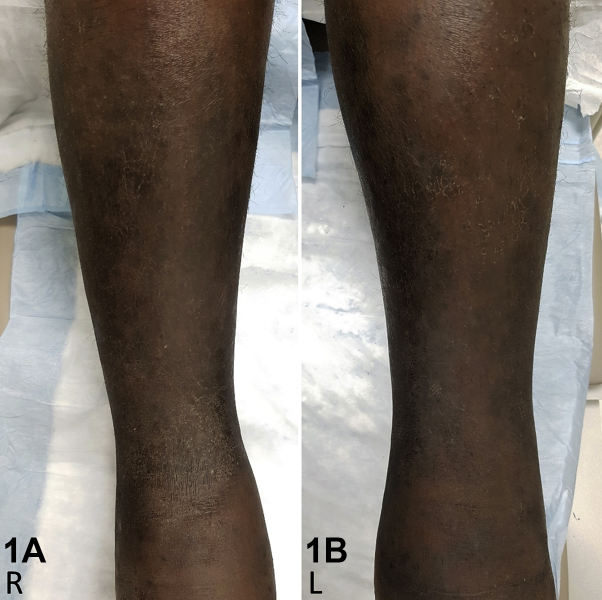
A 45-year-old Nigerian man presented with a 6-month history of hyperpigmentation and progressive edema to the lower legs. His medical history was significant for HIV/AIDS with a CD4 count of 20 and an HIV viral load of 58863 copies per milliliter. He denied any infectious symptoms, such as cough, fever, dyspnea, or rigors. On his lower legs, he had woody, indurated, nonpitting edema, with large hyperpigmented patches and minimally elevated plaques (Fig 1). At follow-up 5 months later, the edema of his legs now extended to his proximal thighs and he had a new, hyperpigmented, indurated plaque on his lateral left thigh (Fig 2).
Fig 1.
Fig 2.
Question 1: What is the best next step for the diagnosis of this patient?
-
A.
Punch biopsy for histologic diagnosis
-
B.
Initiation of intravenous vancomycin
-
C.
Potassium hydroxide preparation
-
D.
Calculate calcium-phosphate product
-
E.
Complete blood count with Sezary prep
Answers:
-
A.
Punch biopsy for histologic diagnosis – Correct. The differential diagnosis for a patient with bilateral lower leg edema accompanied with hyperpigmented patches and plaques includes lymphedema, lipodermatosclerosis, Kaposi sarcoma (KS), stasis dermatitis, chronic venous insufficiency, and many other entities.1 Our patient has poorly controlled HIV, and a biopsy is necessary to rule out KS.
-
B.
Initiation of intravenous vancomycin – Incorrect. Intravenous vancomycin is empiric treatment for cellulitis in a patient at risk for methicillin-resistant Staphylococcus aureus (HIV positive status).1 Bilateral lower leg cellulitis is rare, and our patient does not have other stigmata of acute infections, such as fever, pain, or malaise.1
-
C.
Potassium hydroxide preparation – Incorrect. A potassium hydroxide preparation is a useful diagnostic test when suspecting a superficial fungal infection. Although an argument may be made for an atypical presentation of superficial fungal infection in our immunocompromised patient, it would not explain the significant edema that developed, and our patient requires a biopsy to rule out KS.
-
D.
Calculate calcium-phosphate product – Incorrect. The calcium-phosphate product is a clinically relevant tool in predicting the risk of extra-skeletal calcification in a patient with renal disease. In our patient, there is no history of renal failure or cutaneous calcification.
-
E.
Complete blood count with Sezary prep – Incorrect. Sezary syndrome is a type of cutaneous T-cell lymphoma classically characterized by the triad of lymphadenopathy, erythroderma, and Sezary cells in the blood, lymph nodes, and skin. Our patient does not have erythroderma or lymphadenopathy; therefore, this test would be inappropriate.
Question 2: Based on the clinical presentation and histology, what is the most likely diagnosis?
-
A.
Lipodermatosclerosis
-
B.
Lymphedema
-
C.
Stasis dermatitis
-
D.
Kaposi sarcoma
-
E.
Bilateral lower leg cellulitis
Answers:
-
A.
Lipodermatosclerosis – Incorrect. Although lipodermatosclerosis is a diagnostic consideration in our patient's clinical presentation, CD31 and human herpes virus 8 (HHV-8) positivity indicate KS. Interestingly, there are increasing reports of KS mimicking other clinical and histologic entities including lymphangioma-like KS, pyogenic granuloma–like KS, lipodermatosclerosis–like KS, and ecchymotic KS.1, 2, 3
-
B.
Lymphedema – Incorrect. Our patient has woody, nonpitting edema, which is characteristic of lymphedema, but the findings of CD31 and HHV-8 positivity in the neoplastic capillaries are diagnostic of KS. Therefore, our patient's lymphedema is a complication of his KS.
-
C.
Stasis dermatitis – Incorrect. Stasis dermatitis is an intensely pruritic, eczematous disorder related to chronic venous insufficiency. Our patient does not complain of significant pruritus, and CD31 and HHV-8 should not be positive in stasis dermatitis. Interestingly, there are several reports of KS arising in the setting of arterial, venous, or lymphatic insufficiency with associated stasis dermatitis–like changes.3
-
D.
Kaposi sarcoma – Correct. The development of a new patch on the thigh at 6-month follow-up and the histologic findings of a patchy capillary proliferation in a tiered distribution are suggestive of KS. CD31 and HHV-8 immunohistochemical stains are positive in the neoplastic capillaries, and HHV-8 also demonstrates a focally strong positivity throughout the dermis in a tiered distribution, which confirms the diagnosis of KS (Fig 3).
-
E.
Bilateral lower leg cellulitis – Incorrect. Clinically, the patient does not have other stigmata of acute infection such as fever, pain, or malaise, and histology does not show a dense neutrophilic infiltrate to support an acute infectious process.
Fig 3.
Question 3. Based on the AIDS Clinical Trial Group, our patient has stage T1I1S0 Kaposi sarcoma. Of the treatment options below, choose the best option for treatment of this individual.
-
A.
No pharmacologic management indicated
-
B.
Combination antiretroviral therapy (cART)
-
C.
cART and liposomal daunorubicin
-
D.
cART and paclitaxel
-
E.
cART and topical alitretinoin
Answers:
-
A.
No pharmacologic management indicated – Incorrect. According to the AIDS Clinical Trial Group, our patient has stage T1I1S0 KS, which is considered poor risk prognostically.4 Pharmacologic management is indicated to prevent progression of the patient's KS and alleviate his extensive edema.
-
B.
cART – Incorrect. cART is recommended in essentially all patients with AIDS-related KS, and the importance of strict compliance with cART should be emphasized in this patient.5 However, our patient has more advanced stage KS as a result of his tumor-related edema, and he requires systemic chemotherapy to help control his disease.
-
C.
cART and liposomal daunorubicin – Correct. Our patient has extensive tumor-related edema, which carries a poor prognosis. Systemic chemotherapy is indicated to help prevent progression of his KS and hopefully alleviate his edema. First-line systemic chemotherapy is either liposomal daunorubicin or pegylated liposomal doxorubicin, in addition to strict compliance with cART.4
-
D.
cART and paclitaxel – Incorrect. Paclitaxel is considered a second-line systemic chemotherapy option in more advanced KS because of increased potential for toxicity compared with liposomal anthracyclines.4 Although this is an appropriate treatment strategy for our patient, it is not the best management option.
-
E.
cART and topical alitretinoin – Incorrect. Topical alitretinoin is a gel that may be used for local symptomatic treatment of KS. However, our patient has more advanced KS and requires systemic chemotherapy. Furthermore, this gel may result in inflammation and subsequent postinflammatory hyperpigmentation in our patient.
Footnotes
Dr Tompkins is currently affiliated with the Department of Pathology and Laboratory Medicine, University of Alberta, Edmonton, AB, Canada.
Funding sources: None.
Conflicts of interest: None disclosed.
References
- 1.Batra V., Baras A. Bilateral cellulitis. BMJ Case Rep. 2015;2015 doi: 10.1136/bcr-2015-211117. bcr2015211117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dean S.M., Kaffenberger B.H., Lustberg M.E. Kaposi sarcoma: an unconventional cause of lower extremity lymphedema. Vasc Med. 2017;22(6):544. doi: 10.1177/1358863X17729031. [DOI] [PubMed] [Google Scholar]
- 3.Johnson E.L., Pierpont Y.N., Donate G. Clinical challenge: cutaneous Kaposi's sarcoma of the lower extremity*. Int Wound J. 2011;8(2):163–168. doi: 10.1111/j.1742-481X.2010.00763.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schneider J.W., Dittmer D.P. Diagnosis and treatment of Kaposi sarcoma. Am J Clin Dermatol. 2017;18(4):529–539. doi: 10.1007/s40257-017-0270-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gonçalves P.H., Uldrick T.S., Yarchoan R. HIV-associated Kaposi sarcoma and related diseases. AIDS. 2017;31(14):1903–1916. doi: 10.1097/QAD.0000000000001567. [DOI] [PMC free article] [PubMed] [Google Scholar]