Introduction
Demodex folliculorum is a parasitic mite that is found in pilosebaceous units. Demodicosis, or an overgrowth of the mites, have been implicated in diseases such as blepharitis, scalp folliculitis, and nonspecific diffuse, pruritic papulopustular eruptions of the face and neck areas.1, 2, 3 Here we present a case of localized Demodex folliculitis mimicking perioral dermatitis in a pregnant woman and highlight the rapid onset of action of systemic ivermectin therapy.
Case report
A healthy 33-year-old pregnant woman presented previously for peri-alar seborrheic dermatitis that responded quickly to topical hydrocortisone 2.5% cream. At 36 weeks' gestation, she noted a worsening of her skin condition, despite continued hydrocortisone use. At this time, the patient presented with papules and pustules located periorally, in the absence of comedones, consistent with a diagnosis of perioral dermatitis. Her skin condition worsened despite stopping topical steroids and instituting topical calcineurin inhibitors, ketoconazole, azelaic acid, and metronidazole sequentially. Given the pregnancy, no tetracycline class antibiotics were prescribed. At a follow-up visit 2 weeks later, several days after her delivery of a healthy, full-term infant, her eruption evolved into perioral and lip erythema, swelling, confluent pustules, and scaling, with pronounced pruritus and burning sensations (Fig 1). Notably, there was sparing of the remainder of the face and neck. A differential diagnosis at this time included allergic contact dermatitis and lip licker's dermatitis, although the clinical findings of pustules mitigated against these, and the patient lacked a history of new facial cosmetic products or propensity for lip licking. A scraping of multiple pustules was performed and examined under light microscopy, revealing 6 Demodex mites in lower-power field (Fig 2). A diagnosis of Demodex folliculitis was made, and the patient was prescribed 2 doses of oral ivermectin, 200 μg/kg, spaced 1 week apart. All pustules, swelling, and erythema resolved 2 weeks after the start of the first dose of ivermectin (Fig 3), and all scaling resolved after an additional week without further treatment. She did not require use of any topical medications and did not have any further facial rashes after treatment.
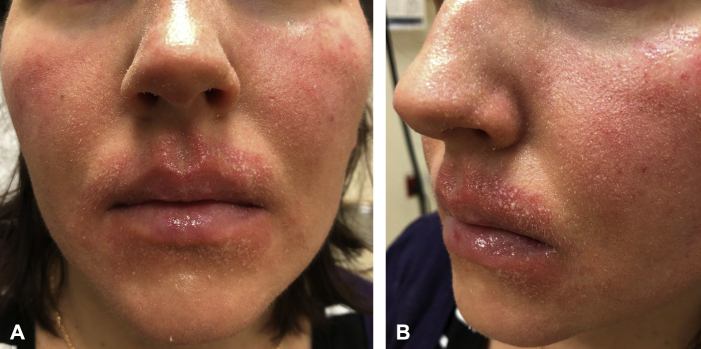
Fig 1.
A and B, Pinpoint pustules in a perioral distribution. Patient began applying plain petrolatum to the vermilion and cutaneous lips after dermatitis began.
Fig 2.

Demodex mite on light microscopy from scraping of a perioral pustule.
Fig 3.
A and B, Resolution of pustules after 1 dose of oral ivermectin.
Discussion
Demodicosis occurs when D folliculorum mites populate beyond a threshold. They are thought to induce an inflammatory response secondary to antigenic proteins produced by Bacillus oleronius, a bacterium that the mite harbors, although their role in inflammatory skin conditions remains controversial.4 Nevertheless, the mites have been implicated in rosacea, blepharitis, and folliculitis.1, 2, 3 Although it would be difficult to prove the causality of our patient's symptoms, we inferred that Demodex was underlying her disease because of 2 factors: (1) the high number of Demodex recovered through random scraping of pustules and (2) the rapid resolution of our patient's symptoms upon treatment with ivermectin, a medication that is known to have antiarthropod effects but not antifungal or antibacterial actions.
This case highlights the rapid therapeutic effect of oral ivermectin for Demodex folliculitis. The patient's symptoms essentially resolved after 2 doses of treatment spaced 1 week apart. Of note, the decision to treat with oral, as opposed to topical, ivermectin was due to the patient's concerns for accidentally smearing the topical agent onto her newborn.
There are little data regarding the safety of oral ivermectin use with breastfeeding. After extensive consultation with the patient and the patient's primary care provider, the decision was made to stop breastfeeding during the 2-week course. Because the half-life of systemic ivermectin is 18 hours,5 the treatment team felt it was safe to resume breastfeeding 5 days after her second dose of ivermectin. At follow-up 6 months after resolution of her symptoms, the patient remained symptom free, and both mother and child suffered no sequelae to the treatment regimen.
This case describes an atypical presentation of Demodex folliculitis that masqueraded as perioral dermatitis. In severe cases of perioral dermatitis that appear refractory to traditional approaches, including eliminating topical steroids and irritants, and instituting topical or systemic antibiotics or calcineurin inhibitors, one may need to consider Demodex folliculitis as the correct diagnosis, and institute ivermectin therapy for rapid resolution.
Footnotes
Funding sources: None.
Conflicts of interest: None disclosed.
References
- 1.Helou W., Avitan-Hersh E., Bergman R. Demodex folliculitis of the scalp: clinicopathological study of an uncommon entity. Am J Dermatopathol. 2016;38(9):658–663. doi: 10.1097/DAD.0000000000000512. [DOI] [PubMed] [Google Scholar]
- 2.Elston C.A., Elston D.M. Demodex mites. Clin Dermatol. 2014;32:739–743. doi: 10.1016/j.clindermatol.2014.02.012. [DOI] [PubMed] [Google Scholar]
- 3.English F.P., Nutting W.B. Demodicosis of ophthalmic concern. Am J Ophthalmol. 1981;91:362–372. doi: 10.1016/0002-9394(81)90291-9. [DOI] [PubMed] [Google Scholar]
- 4.Lacy N., Delaney S., Kavanagh K., Powell F.C. Mite-related bacterial antigens stimulate inflammatory cells in rosacea. Br J Dermatol. 2007;157:474–481. doi: 10.1111/j.1365-2133.2007.08028.x. [DOI] [PubMed] [Google Scholar]
- 5.Merck Stromectal Medication Package Insert. https://www.merck.com/product/usa/pi_circulars/s/stromectol/stromectol_pi.pdf