Introduction
Immunoglobulin G4–related diseases (IgG4-RD) are a group of immune-mediated disorders characterized by organ infiltration with lymphocytes and IgG4+ plasma cells. IgG4-RD has multiple clinical manifestations, affecting distant organs ranging from the orbit to the pancreas. Ulcerative colitis (UC) is an inflammatory bowel disease that causes chronic colonic mucosal inflammation, most likely due to a damaged epithelial barrier, an abnormal reaction to intestinal bacteria, and a dysregulated immune response.1 UC is also associated with extraintestinal manifestations including ocular complications. Here we present an unusual case of IgG4-related orbital disease (IgG4-ROD) arising in a patient with ulcerative colitis.
Case presentation
A 49-year-old woman with a history of UC for 29 years controlled on mesalamine presented for evaluation of bilateral orbital swelling. The patient first experienced sudden onset, painless, right orbital swelling 3 years prior but did not seek treatment. However, the symptoms continued to worsen, progressing to involve the left orbit. Her primary care physician ordered magnetic resonance imaging of the orbits, which was notable for enlargement and homogeneous enhancement of the right greater than left lacrimal glands with homogenous low T2 signal (concerning for lymphoma vs granulomatous disease). Initial workup was negative for antinuclear antibodies, rheumatoid factor, anti-Sjögren's syndrome type B antibody, angiotensin-converting enzyme, rapid plasma reagin, Lyme disease, and quantiferon gold. However, she was found to have elevated serum IgG4, of unknown significance.
One year later, because of persistent orbital swelling, she underwent lacrimal gland biopsy, which found fibrosis and a well-differentiated mixed T- and B-cell infiltrate. There were many plasma cells showing an elevated IgG4/IgG ratio at 0.65:1. Over the following year, she received several prednisone courses (40 mg/d orally) with initial decrease in orbital swelling but rebound swelling upon steroid taper. During this time, her UC symptoms remained stable, but colonoscopy was advised to investigate a possible role for underlying inflammation. Colonoscopy found active colitis, providing evidence of ongoing active disease despite symptomatic stability. Based on these findings, it was hypothesized that systemic inflammation might be contributing to orbital swelling. She was taken off mesalamine and received a trial of azathioprine (100 mg/d orally) with little improvement. She was then started on vedolizumab, a monoclonal antibody that binds to integrin α₄β₇ and has anti-inflammatory properties. Her UC symptoms improved, but orbital swelling did not decrease. A local eyelid steroid injection was attempted with short-lived and incomplete improvement of her symptoms. She was referred to us for further evaluation.
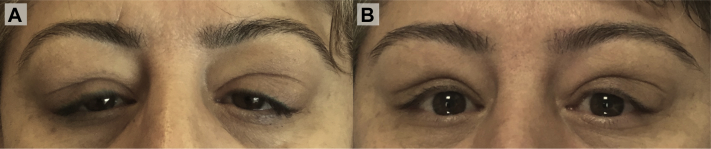
On physical examination, she had diffuse, bilateral orbital and eyelid swelling (Fig 1, A). Sclera were normal; pupils were equal, round, and reactive to light with intact accommodation; and her extraocular movements were intact. The patient denied fevers, chills, nausea, vomiting, night sweats, blurry vision, headaches, change in vision, pain, rashes, lymphadenopathy, and weight loss.
Fig 1.
Photos of IgG4-ROD before and after treatment. A, Before treatment with diffuse, painless, bilateral orbital and eyelid swelling. B, Three months later, after 2 rituximab infusions, a significant decrease in bilateral swelling.
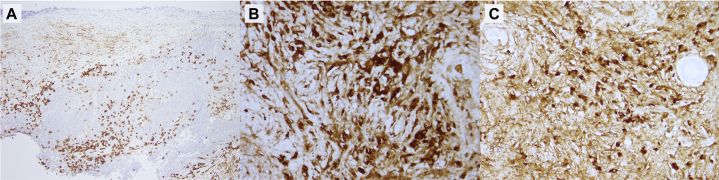
Repeat blood work was notable for elevated IgG4 (402; upper limit of normal [ULN], 123) and mildly elevated IgG3 (136; ULN, 134) and IgG2 (572; ULN, 549). Lactate dehydrogenase level was normal, serum protein electrophoresis result was negative, and basic autoimmune panel was negative. Repeat orbital magnetic resonance imaging was notable for bilateral lacrimal gland enlargement compatible with IgG4 disease, and intact optic nerves and extraocular muscles. Repeat lacrimal gland biopsy found dense storiform fibrosis and a dense infiltrate of polyclonal small lymphocytes including B and T cells (Fig 2). Similar to the previous biopsy, the IgG4 proportion of IgG plasma cells was high at 65%, on average. IgG immunostaining highlighted an increase of IgG4+ plasma cells to greater than 50 per high-power field (Fig 3). Considering recent steroid use, it was not unexpected that the number of IgG4+ cells was less than 100 per high-power field. However, her overall clinical presentation along with pathologic and laboratory findings were compatible with a diagnosis of IgG4-related orbital disease, a type of IgG4-RD that is characterized by painless bilateral orbital swelling. Therapy with rituximab was initiated. After 2 doses of immunotherapy, she had significant improvement of bilateral orbital swelling (Fig 1, B).
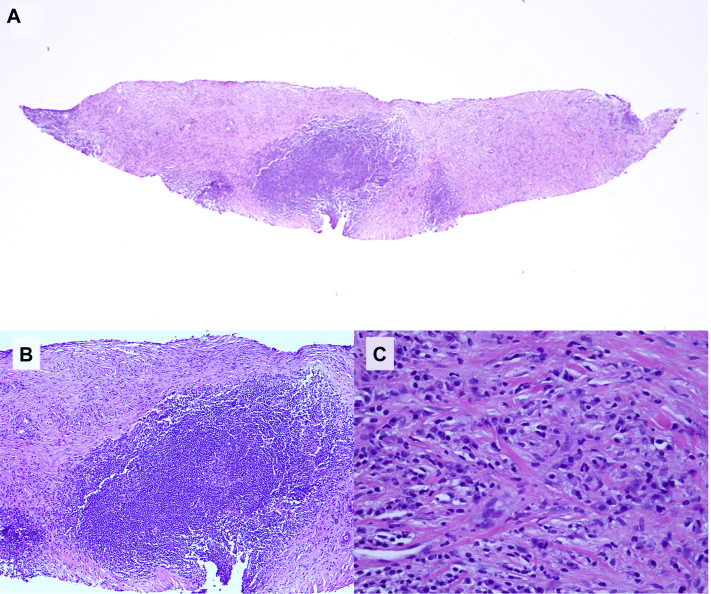
Fig 2.
Histopathology of lacrimal gland biopsy. A, Low-power image of the lacrimal gland shows a multinodular lymphocytic infiltrate amid a background of storiform fibrosis. B, High-power magnification shows a well-differentiated lymphocytic infiltrate predominated by small lymphocytes and plasma cells. Also note a densely sclerotic fibrous background. C, Higher-power magnification shows areas of sclerosis exhibiting patterned fibroplasia typical for IgG sclerosing disease. Numerous small lymphocytes and mature plasma cells are noted amid the sclerotic collagen bundles. (Hematoxylin- eosin stain; original magnifications: A, ×20; B, ×100; C, ×400.)
Fig 3.
Immunostaining of lacrimal gland biopsy. A, CD138 immunostaining highlights the many plasma cells that course through the infiltrate. B, The IgG stain highlights the many plasma cells that are observed in the infiltrate. C, In the same field, the IgG4 stain highlights a number of plasma cells, demonstrating an IgG4/IgG ratio of around 0.65:1. (Original magnifications: A, ×100; B and C, ×400.)
Discussion
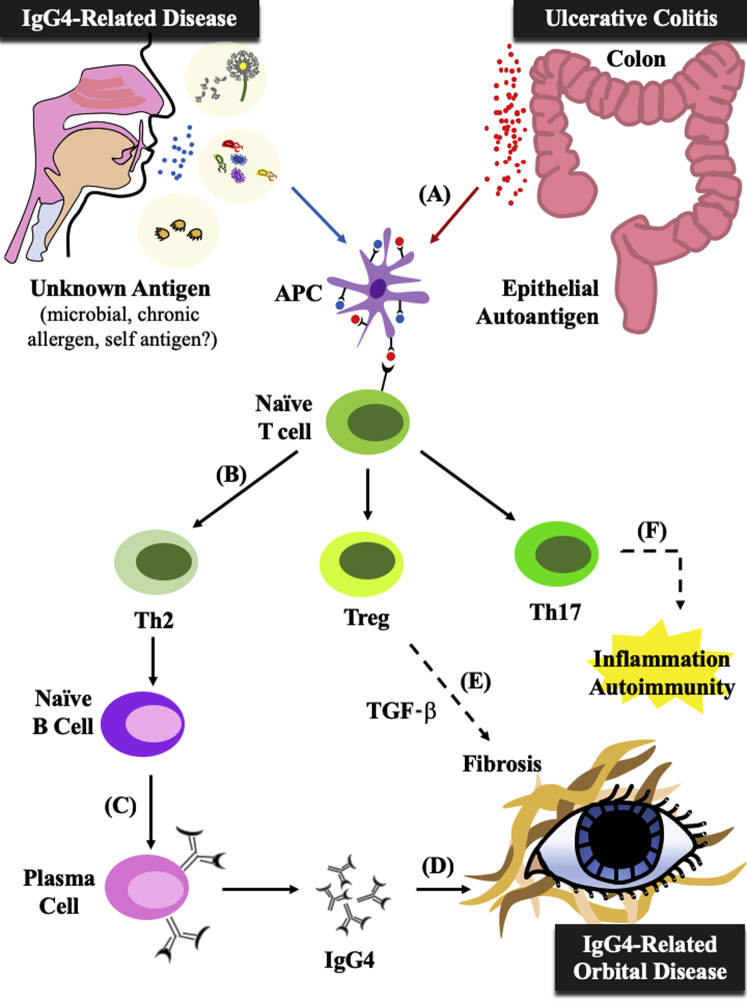
The pathogenesis of UC has historically been attributed to an imbalance of T helper (Th) type 1/type 2 cells with a Th2-dominant immune response, initially induced in response to an epithelial colonic antigen. Recently, mounting evidence suggests that UC also induces elevated levels of Th17 cells and Th17-associated cytokines, contributing to autoimmunity and chronic inflammation.2 Likewise, IgG4-RD, which is characterized by a fibrosis-associated inflammatory response and IgG4-plasma cell infiltration of organs, is thought to be related to a Th2-dominant response,3 even in cases not associated with other inflammatory conditions. Th2 cells produce interleukin (IL)-4 (along with IL-5 and IL-13), and IL-4 in turn acts on plasma cells and promotes immunoglobulin isotype switching to IgG4 and IgE.4 IgG4-RD has also been associated with a T-cell shift toward the Th17 cell phenotype, contributing to autoimmunity.5 In addition, the number of regulatory T (Treg) cells is elevated in IgG4-RD, but it is suspected that the severity of inflammation may be too extreme for Treg control or that the Tregs themselves are dysfunctional.6
Studies have frequently linked ulcerative colitis with type I autoimmune pancreatitis, the most common manifestation of IgG4-related disease, suggesting a shared role for inflammation in their pathogenesis. The presence of IgG4 in UC patients is associated with higher levels of UC disease activity, whereas the absence is linked to a milder disease phenotype. Likewise, more severe gastrointestinal inflammation is linked to a greater degree of IgG4-positive plasma cell infiltration in the colonic mucosa.7
Notably, UC can also present with extra-intestinal manifestations including various ocular complications in up to 5% of UC patients.8 However, UC has not been associated previously with IgG4-ROD. Possibly, the same epithelial colonic autoantigen that triggers an inflammatory reaction in the bowel may also present in other tissues, like the orbit, causing an extraintestinal antibody-mediated immune response.9 Although our patient had no documented ocular complications previously, it is likely that her UC induced low levels of chronic ocular inflammation.
Our patient's unusual presentation can be explained by the significant overlap between the pathogenesis of UC and IgG4-related disease—both are characterized by a Th2-dominant immune response, overexpression of Th2-related cytokines, and upregulation of Th17 cells (Fig 4). Indeed, confirmed presence of active colitis soon after the onset of eyelid swelling suggests that despite symptomatic stability, her UC was ongoing and active, likely causing inflammation both locally and systemically. Thus, through chronic extraintestinal inflammation, a proinflammatory cytokine milieu, and a dysregulated Th2 response, we posit that our patient's ulcerative colitis promoted and contributed to the development of her IgG4-related orbital disease.
Fig 4.
Parallels and intersection of UC and IgG4-related disease pathways. A, An unknown antigen in the IgG4 pathway and an epithelial autoantigen in the UC pathway both stimulate antigen-presenting cells. B, Antigen-presenting cells activate naïve T cells and lead to a Th2-dominant response, with increases in the number of Tregs and Th17 cells. C, Th2 cells release IL-4, which promotes naïve B-cell differentiation into plasma cells and immunoglobulin isotype switching to IgG4. D, IgG4 infiltration of orbits leads to fibrosis and IgG4-ROD. E, Tregs release IL-10 and transforming growth factor-β, which contribute to fibrosis. F, Th17 cells and Th17-related cytokines induce autoimmunity and promote inflammation.
Footnotes
Funding sources: None.
Conflicts of interest: None disclosed.
References
- 1.Cioffi M., Rosa A.D., Serao R., Picone I., Vietri M.T. Laboratory markers in ulcerative colitis: current insights and future advances. World J Gastrointest Pathophysiol. 2015;6(1):13–22. doi: 10.4291/wjgp.v6.i1.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liu Z.J., Yadav P.K., Su J.L., Wang J.S., Fei K. Potential role of Th17 cells in the pathogenesis of inflammatory bowel disease. World J Gastroenterol. 2009;15(46):5784–5788. doi: 10.3748/wjg.15.5784. Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moriyama M., Nakamura S. Th1/Th2 immune balance and other T helper subsets in IgG4-related disease. Curr Top Microbiol Immunol. 2017;401:75–83. doi: 10.1007/82_2016_40. [DOI] [PubMed] [Google Scholar]
- 4.Punnonen J., Aversa G., Cocks B.G. Interleukin 13 induces interleukin 4-independent IgG4 and IgE synthesis and CD23 expression by human B cells. Proc Natl Acad Sci U S A. 1993;90(8):3730–3734. doi: 10.1073/pnas.90.8.3730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grados A., Ebbo M., Piperoglou C. T cell polarization toward T(H)2/T(FH)2 and T(H)17/T(FH)17 in patients with IgG4-related disease. Front Immunol. 2017;8:235. doi: 10.3389/fimmu.2017.00235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Uchida K., Okazaki K. Roles of regulatory T and B cells in IgG4-related disease. Curr Top Microbiol Immunol. 2017;401:93–114. doi: 10.1007/82_2016_41. [DOI] [PubMed] [Google Scholar]
- 7.Kuwata G., Kamisawa T., Koizumi K. Ulcerative colitis and immunoglobulin G4. Gut Liver. 2014;8(1):29–34. doi: 10.5009/gnl.2014.8.1.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Troncoso L.L., Biancardi A.L., de Moraes H.V., Jr., Zaltman C. Ophthalmic manifestations in patients with inflammatory bowel disease: a review. World J Gastroenterol. 2017;23(32):5836–5848. doi: 10.3748/wjg.v23.i32.5836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Halstensen T.S., Das K.M., Brandtzaeg P. Epithelial deposits of immunoglobulin G1 and activated complement colocalise with the M(r) 40 kD putative autoantigen in ulcerative colitis. Gut. 1993;34(5):650–657. doi: 10.1136/gut.34.5.650. [DOI] [PMC free article] [PubMed] [Google Scholar]