Abstract
Background:
Seasonal influenza constitutes an enormous public health burden. The 2017-2018 influenza season was the most severe since the 2009 novel Influenza A (H1N1) pandemic. The State of Texas, like other states, experienced unusually high and persistent influenza activity.
Methods:
Data on confirmed cases of influenza and influenza-like illness (ILI) in Brazos County during December 2017 were collected by the Brazos County Health Department (BCHD) from medical records. Records of vaccine administered between January 1 and December 31, 2017 were collected from vaccination providers. The total number of influenza cases for 2017 was compiled from regular weekly influenza counts reported to BCHD by healthcare providers.
Results:
A total of 1651 cases of laboratory-confirmed influenza were reported in Brazos County residents in December 2017, 10 times more than that reported in December 2016. The highest rates of infection were in 2 ZIP codes where vaccination rates were also high. A total of 16 027 influenza vaccinations were given to individuals reporting a residential address in Brazos County in 2017. Vaccination coverage was lowest among adults aged 18 to 49, whereas those aged 65 or older and Hispanics were most likely to be hospitalized.
Discussion:
Overall, vaccination coverage in Brazos County, Texas is low, less than half of the Healthy People 2020 target. The development of health education materials and an increased use of social media, local television and radio, and communication methods that can reach parents, younger adults, and Hispanic residents are needed.
Keywords: Influenza, vaccines, public health practice, communicable diseases, disease outbreaks
Background
Influenza-like illness (ILI) is a respiratory infection characterized by a fever of ⩾100°F, cough, and a sore throat in the absence of a known cause. Influenza is a highly contagious acute infection of the respiratory tract caused by influenza viruses, which typically includes fever/chills, cough, sore throat, runny or stuffy nose, headache, general body or muscle pain, and fatigue; children’s symptoms may include diarrhea and vomiting.1 Influenza is spread mostly through large-particle virus-laden droplets and small aerosols from an infected person; people may also become infected by touching contaminated surfaces and later touching their eyes, mouth, or nose with their hands.2
The spread, rates, and severity of seasonal influenza vary widely from year to year, depending on many factors. These include the types and subtypes of the viruses causing disease and the immunity of the general population in the specific locality. Two major types of influenza viruses (A and B) cause disease in humans. Increased severity and higher rates of hospitalizations, complications, and deaths have been associated with certain subtypes of influenza (ie, the H3N2 subtype of Influenza A).3,4 People who are at the greatest risk of severe infection or complications include children, especially those younger than 2 years of age, those aged more than 65, pregnant women, and people with chronic or immunosuppressing medical conditions such as asthma, diabetes, heart disease, cancer, and HIV/AIDS. The highest rates of infection with seasonal influenza typically occur in these high-risk groups and in school-age children.2,5,6 Influenza-associated mortality also increases with age, pregnancy, and the presence of preexisting chronic medical conditions.7
Influenza viruses are in circulation globally year round and cause annual epidemics referred to as seasonal influenza as well as paroxysmal pandemics.8 In the United States, most cases of seasonal influenza occur between October and May, with the largest number of cases reported during December, January, and February. These regular seasonal influenza epidemics are in part due to mismatches between the annual vaccine and the circulating virus because of antigenic drift,9 social, psychological, and demographic factors associated with vaccine uptake,10 and willingness to use non-pharmaceutical interventions to mitigate infection and reduce transmission in the community.11
The Centers for Disease Control and Prevention (CDC) estimates that influenza has been responsible for 9.2 to 35.6 million medical visits, 140 000 to 710 000 hospitalizations, 12 000 to 56 000 deaths, and an economic burden of about US$90 billion each year since 2010.12 The direct medical costs of influenza in children alone, including medical and emergency room visits and hospitalizations, are estimated at US$44 to US$279 million annually.13
The prevention and control of ILI and influenza are based on pharmaceutical (eg, vaccination and treatment and prophylaxis with antiviral drugs) and non-pharmaceutical (eg, hand washing, cough etiquette, isolation of those who are ill, and frequent disinfection of surfaces) methods, with the main strategy for the prevention and control of seasonal influenza being annual vaccination.14–16 When the vaccine strains are well matched to the influenza virus strains circulating in the population, vaccine efficacy may be up to 70% to 90%; however, vaccine effectiveness is much lower for certain strains (H3N2) and when the vaccine is not well matched to the circulating strain.17,18 Early in the 2017-2018 influenza season, CDC reported an overall vaccine effectiveness of 36% (95% confidence interval [CI]: 27%, 44%). Effectiveness for specific strains was similar: 25% (CI: 13%, 36%) for Influenza A (H3N2), 67% (CI: 54%, 76%) for Influenza A (H1N1), and 42% (CI: 25%, 56%) for Influenza B.19 Vaccination coverage in the United States is generally low, with coverage through May 2017 for the 2016-2017 influenza season being only 46.8%, and lower in the southern and western states. For example, Texas had a coverage of 43.5%, whereas Nevada had the lowest coverage at 36.1%.20
The CDC described the 2017-2018 influenza season as one of “high severity.”21 Influenza activity across the United States increased sharply beginning in December 201722 and the 2017-2018 influenza season saw the largest percentage of outpatient visits for ILI (peaking at 7.5% during the week that ended February 5, 2018), influenza-related hospitalizations (106.6 per 100 000), and influenza-associated pediatric deaths (N = 171) in a non-pandemic year. Among the children who died, 79 of 154 had at least 1 underlying medical condition that put them at high risk for influenza-related complications and 80% were not fully vaccinated.23 In Brazos County, Texas, the location of this study, there was a 10-fold increase in ILI and influenza activity during the 2017-2018 season, as well as 2 confirmed institutional outbreaks. However, rates of vaccination coverage are unknown in Brazos County for this year and all prior years because data on influenza vaccination coverage are not tracked at the local health department level. In addition, the occurrence of ILI and influenza at the local level is typically underestimated for several reasons. Uncomplicated influenza illness is typically not reported by providers to public health authorities as part of regular public health surveillance, with requirements for reporting differing by state. For example, in Texas, only ILI and influenza outbreaks, influenza-associated pediatric deaths, and confirmed cases of novel Influenza A are reportable.24
In this study, we sought to identify determinants of influenza vaccination and infection among residents of Brazos County, Texas, and to map the geographic distribution of both vaccination and cases of influenza to improve the effectiveness of public health interventions to support influenza vaccination and prevention of infection.
Methods
Due to the excess number of cases of influenza being reported in Brazos County in December 2017, the Brazos County Health Department (BCHD) partnered with the Texas A&M School of Public Health’s EpiAssist program to perform a 2-part study. First, a Community Assessment for Public Health Emergency Preparedness (CASPER) was conducted to assess knowledge of and attitudes toward influenza and influenza vaccination by residents of Brazos County.25 The CASPER was conducted on March 2 and 3, 2018. Second, data on each case of influenza or ILI reported to the health department as part of voluntary reporting by facilities (eg, hospitals, private clinics, laboratories, and school), as well as information about influenza vaccinations administered to county residents, were collected by BCHD. Between January and March 2018, medical records were collected from healthcare providers for both outpatient and emergency room visits and hospitalizations for influenza and ILI during December 2017, a period when 10 times more cases of ILI and influenza were reported to BCHD in weekly influenza activity reports than the prior year. The total number of influenza cases for the remainder of 2017 was compiled from the regular weekly influenza counts voluntarily reported to BCHD by healthcare providers.
Records of influenza vaccine administered between January 1 and December 31, 2017 were collected from healthcare providers and other vaccination centers, including pharmacies, as well as from the Texas Vaccines for Children Program (TVFC), which makes vaccines available to participating health care providers at no cost to immunize children who meet eligibility requirements.26 Some vaccination records were verified using the ImmTrac2 database. Inclusion criteria included having an influenza vaccination in 2017 and a residential address in Brazos County. Vaccination data were entered into Microsoft Excel 2013 (Redmond, WA) and imported into Stata Version 14 (College Station, TX) for analysis.
Medical records of reported cases of influenza or ILI were obtained from health care providers. Demographic data, including age, sex, race, and ZIP code, as well as influenza vaccination status (Yes/No), receipt of antiviral medications (ie, Oseltamivir [Tamiflu]) (Yes/No), and hospitalization for influenza (Yes/No) were extracted from the records, entered into Microsoft Excel 2013, and imported into Stata Version 14 for descriptive and multivariate regression analyses. Cases without a residential address in Brazos County, Texas, laboratory confirmation of influenza in December 2017, age, or sex were excluded. To assess for potential associations between demographic variables and the receipt of influenza vaccination, receipt of Tamiflu, or hospitalization, crude and adjusted odds ratios (ORs) and 95% CIs were calculated. Population estimates from the US Census Bureau were used to estimate the prevalence of influenza and vaccination among demographic groups. Spatial analyses of the distribution of influenza and ILI cases and vaccination were performed using ArcGIS Version 10.4 (ESRI, Redlands, CA). This study was reviewed by the Texas A&M Institutional Review Board and determined to be exempt; therefore, informed consent was waived (IRB2018-0059).
Results
The total number of weekly influenza cases voluntarily reported to the BCHD by healthcare providers between October and December 2016 was 256. However, between October and December 2017, 2096 cases were reported to the health department, with 1775 of 2096 (84.69%) reported in December alone. Between January and March 2018, an additional 4471 cases were reported, with 2023 of 4471 (45.45%) reported in January 2018 and 2062 or 4471 (46.12%) reported in February 2018.
Using medical records, a total of 3304 cases of laboratory-confirmed influenza were identified in December 2017; 1651 cases were Brazos County residents (Table 1). A slight majority of the cases were women (N = 899; 54.5%). The age of the cases ranged from 3 months to 98 years (mean = 25 years; median = 15 years). More than one-third of the cases (N = 589; 35.68%) were in the 5- to 17-year-old age group and cases were fairly evenly distributed among whites (N = 562; 34.04%), Hispanics (N = 521; 31.56%), and African-Americans (N = 337; 20.41%). Four in five confirmed cases were Influenza A (N = 1.327; 80.4%). About 10% (N = 180) had received the influenza vaccine during 2017, whereas 25% (N = 404) had not. The vaccination status of 64.43% (N = 1067) of the cases was unknown. Approximately 30% (N = 477) received Oseltamivir (Tamiflu), whereas approximately 20% were hospitalized (N = 338). The hospitalization status of 47.30% (N = 781) of cases was unknown. More than half of the confirmed cases were residents of 2 ZIP codes, 77803 (N = 416; 25.20%) and 77845 (N = 453; 27.44%).
Table 1.
Characteristics of influenza cases, Brazos County, Texas, December 2017 (N = 1651).
| Total (N = 1651) |
Vaccinated (N = 180) |
Unvaccinated (N = 404) |
Hospitalized (N = 338) |
|
|---|---|---|---|---|
| N (%) | N (%) | N (%) | N (%) | |
| Sex | ||||
| Male | 752 (45.55) | 88 (48.89) | 164 (40.59) | 160 (47.34) |
| Female | 899 (54.45) | 92 (51.11) | 240 (59.41) | 178 (52.66) |
| Age group | ||||
| 0-4 | 305 (18.47) | 52 (28.89) | 62 (15.34) | 80 (23.67) |
| 5-17 | 589 (35.68) | 55 (30.55) | 133 (32.92) | 74 (21.89) |
| 18-49 | 465 (28.16) | 32 (17.78) | 149 (36.88) | 88 (26.04) |
| 50-64 | 155 (9.39) | 16 (8.89) | 38 (9.41) | 39 (11.54) |
| 65 or older | 137 (8.30) | 25 (13.89) | 22 (5.45) | 57 (16.86) |
| Race/ethnicity | ||||
| African-American | 337 (20.41) | 25 (13.89) | 77 (19.06) | 66 (19.53) |
| White | 562 (34.04) | 89 (49.44) | 196 (48.51) | 114 (33.73) |
| Hispanic | 521 (31.56) | 42 (23.33) | 97 (24.01) | 144 (42.60) |
| Other | 53 (3.21) | 24 (13.33) | 34 (8.42) | 14 (4.14) |
| Missing | 178 (10.78) | – | – | – |
| Influenza strain | ||||
| A | 1327 (80.38) | 160 (88.89) | 374 (92.57) | 316 (93.49) |
| B | 123 (7.45) | 15 (8.33) | 25 (6.19) | 20 (5.92) |
| Not known | 201 (12.17) | 5 (2.78) | 5 (1.24) | 2 (0.59) |
| Vaccination status | ||||
| Yes | 180 (10.90) | – | – | 62 (18.34) |
| No | 404 (24.47) | – | – | 127 (37.58) |
| Unknown | 1067 (64.63) | – | – | 149 (44.08) |
| Received Tamiflu | ||||
| Yes | 477 (28.89) | 112 (62.22) | 231 (57.18) | 191 (56.51) |
| No | 367 (22.23) | 64 (35.56) | 163 (40.35) | 131 (38.76) |
| Unknown | 807 (48.88) | 4 (2.22) | 10 (2.47) | 16 (4.73) |
| Hospitalized | ||||
| Yes | 338 (20.47) | 62 (34.44) | 127 (31.44) | – |
| No | 532 (32.22) | 118 (65.56) | 277 (68.56) | – |
| Unknown | 781 (47.30) | – | – | – |
Of the 30 influenza vaccination facilities in Brazos County contacted by BCHD, 15 (50.0%) provided vaccination data on request, whereas two-thirds (20 of 30) of healthcare providers contacted provided records of both influenza vaccination and laboratory-confirmed cases. A total of 16 027 persons reporting a residential address in Brazos County received an influenza vaccine during 2017 (Table 2). The ages of those vaccinated ranged from 6 months to 101 years (mean = 33 years; median = 28 years). Approximately 30% of those vaccinated (N = 4635) were in the 18- to 49-year-old age group. About half of those receiving vaccine were women (N = 7481; 46.68%) and among those where a race was known, three-quarters were white (2952 of 3913; 75.44%). The largest proportion of vaccines were given to individuals with a residential address in ZIP codes 77803 (N = 3448; 21.51%) and 77845 (N = 4875; 30.42%).
Table 2.
Demographic characteristics of vaccinated persons, Brazos County, Texas, 2017 (N = 16 027).
| N (%) | |
|---|---|
| Sex | |
| Male | 5795 (36.16) |
| Female | 7481 (46.68) |
| Missing | 2751 (17.16) |
| Age group | |
| 0-4 | 2770 (17.28) |
| 5-17 | 3590 (22.40) |
| 18-49 | 4635 (28.92) |
| 50-64 | 2211 (13.80) |
| 65 or older | 2821 (17.60) |
| Race/ethnicity | |
| African-American | 620 (15.84) |
| White | 2952 (75.44) |
| Hispanic | 134 (3.42) |
| Other | 207 (5.29) |
| Unknown | 12 114 (75.58) |
| ZIP code | |
| 77801 | 1191 (7.43) |
| 77802 | 1963 (12.25) |
| 77803 | 3448 (21.51) |
| 77805 | 119 (0.74) |
| 77806 | 70 (0.44) |
| 77807 | 974 (6.08) |
| 77808 | 1214 (7.57) |
| 77840 | 2017(12.59) |
| 77841 | 19 (0.12) |
| 77842 | 90 (0.56) |
| 77843 | 3 (0.02) |
| 77844 | 1 (0.01) |
| 77845 | 4875 (30.42) |
| 77862 | 2 (0.01) |
| 77866 | 29 (0.18) |
| 77881 | 12 (0.07) |
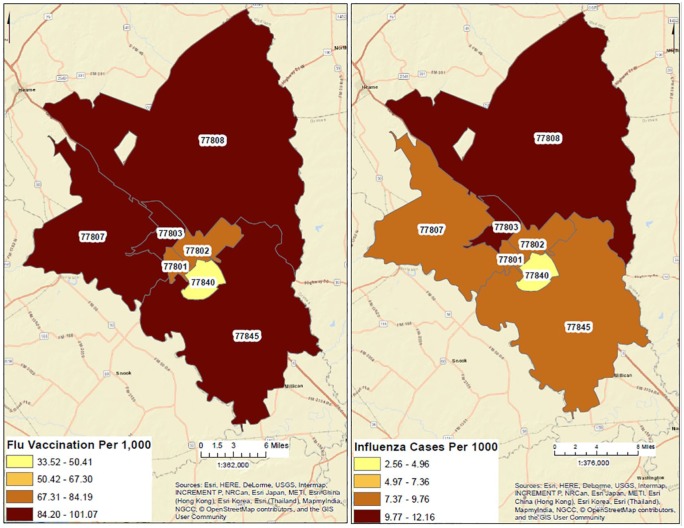
Based on the total population and the number of vaccinations in each ZIP code, the prevalence of influenza and vaccination coverage was calculated (Figure 1). The ZIP code 77840, which includes the areas of Brazos County that are adjacent to the campus of Texas A&M University, had the lowest prevalence of influenza cases with 2.56 per 1000 and the lowest prevalence of vaccination at 33.52 per 1000 (Figure 1). Two ZIP codes in the city of Bryan, Texas, 77803 and 77808, had the highest prevalence of influenza or ILI during December 2017 (12.16 per 1000 and 12.07 per 1000, respectively). Those 2 ZIP codes also had the highest prevalence of vaccination in 2017 (100.79 per 1000 and 101.07 per 1000, respectively).
Figure 1.
Influenza cases and vaccination rates by ZIP code, Brazos County, Texas, 2017.
In crude models, among influenza cases vaccination was significantly less likely among children aged 5 to 17 (OR = 0.49; 95% CI: 0.30, 0.80) and younger adults aged 18 to 49 (OR = 0.26; 95% CI: 0.15, 0.44) compared with the referent group that included children aged 6 months to 4 years (Table 3). Although those 65 years or older were more likely to have received vaccine, they were also more than 3 times as likely to have been hospitalized (OR = 3.33; 95% CI: 1.94, 5.69). Those aged 50 to 64 were also more likely to be hospitalized (OR = 1.76; 95% CI: 1.03, 3.00). Those who received Oseltamivir (Tamiflu), which has been shown in clinical trials and surveillance data to provide substantial benefits to children with influenza A and adults with influenza A (H1N1),27,28 were about twice as likely to have Influenza A, compared with Influenza B (OR = 0.48; 95% CI: 0.28, 0.83). Although there were no differences in vaccination or receipt of Oseltamivir (Tamiflu) by ethnicity, Hispanics were about 3 times as likely to be hospitalized compared with white, non-Hispanics (OR = 2.96; 95% CI: 2.12, 4.14).
Table 3.
Crude associations between demographic variables and receipt of influenza vaccination, receipt of Oseltamivir (Tamiflu), or hospitalization, Brazos County, Texas.
| Crude OR | 95% CI | |
|---|---|---|
| Receipt of influenza vaccine | ||
| Female | 0.71 | 0.50, 1.02 |
| Age group | ||
| 5-17 years | 0.49* | 0.30, 0.80 |
| 18-49 years | 0.26* | 0.15, 0.44 |
| 50-64 years | 0.50 | 0.25, 1.00 |
| 65 years or older | 1.35 | 0.69, 2.68 |
| Race/ethnicity | ||
| Hispanic | 0.95 | 0.61, 1.47 |
| Black/other | 0.70 | 0.43, 1.16 |
| ZIP code (College Station vs Bryan) | 0.87 | 0.60, 1.26 |
| Influenza strain (type B) | 1.40 | 0.72, 2.73 |
| Receipt of Oseltamivir (Tamiflu) | ||
| Female | 1.04 | 0.79, 1.37 |
| Age group | ||
| 5-17 years | 0.71 | 0.49, 1.02 |
| 18-49 years | 0.74 | 0.51, 1.09 |
| 50-64 years | 1.14 | 0.65, 2.02 |
| 65 years or older | 1.13 | 0.66, 1.92 |
| Race/ethnicity | ||
| Hispanic | 0.79 | 0.57, 1.10 |
| Black/other | 0.78 | 0.55, 1.11 |
| ZIP code (College Station vs Bryan) | 1.09 | 0.82, 1.46 |
| Influenza strain (type B) | 0.48* | 0.28, 0.83 |
| Hospitalization | ||
| Female | 0.93 | 0.71, 1.22 |
| Age group | ||
| 5-17 years | 0.58* | 0.39, 0.85 |
| 18-49 years | 0.97 | 0.66, 1.43 |
| 50-64 years | 1.76* | 1.03, 3.00 |
| 65 years or older | 3.33* | 1.94, 5.69 |
| Race/ethnicity | ||
| Hispanic | 2.96* | 2.12, 4.14 |
| Black/other | 1.13 | 0.78, 1.64 |
| ZIP code (College Station vs Bryan) | 0.38* | 0.28, 0.52 |
| Influenza strain (type B) | 0.76 | 0.44, 1.33 |
Abbreviations: CI, confidence interval; OR, odds ratio.
P < .05.
Results were similar in adjusted models, with children aged 5 to 17 and adults aged 18 to 49 and 50 to 64 being less likely to be vaccinated, compared with the referent group that included children aged 6 months to 4 years (Table 4). Those with Influenza B were about half as likely to have received Tamiflu. In the adjusted models, those age 65 and older were only slightly more likely to receive vaccine (OR = 1.20; 95% CI: 0.58, 2.52) but remained at higher risk of hospitalization (OR = 5.18; 95% CI: 2.81, 9.55). Those aged 50 to 64 (OR = 2.60; 95% CI: 1.42, 4.77) and those of Hispanic ethnicity (OR = 3.03; 95% CI: 2.06, 4.47) were more likely to be hospitalized.
Table 4.
Adjusted associations between demographic variables and receipt of influenza vaccination, receipt of Tamiflu, or hospitalization, Brazos County, Texas.
| Adjusted OR | 95% CI | |
|---|---|---|
| Receipt of influenza vaccine | ||
| Female | 0.73 | 0.49, 1.09 |
| Age group | ||
| 5-17 years | 0.51* | 0.31, 0.86 |
| 18-49 years | 0.27* | 0.15, 0.49 |
| 50-64 years | 0.42* | 0.19, 0.93 |
| 65 years or older | 1.20 | 0.58, 2.52 |
| Race/ethnicity | ||
| Hispanic | 1.04 | 0.64, 1.72 |
| Black/other | 0.76 | 0.45, 1.29 |
| ZIP code (College Station vs Bryan) | 1.15 | 0.75, 1.78 |
| Influenza strain (type B) | 1.57 | 0.76, 3.23 |
| Receipt of Tamiflu | ||
| Female | 1.09 | 0.81, 1.46 |
| Age group | ||
| 5-17 years | 0.75 | 0.51, 1.10 |
| 18-49 years | 0.76 | 0.51, 1.17 |
| 50-64 years | 1.26 | 0.69, 2.32 |
| 65 years or older | 1.21 | 0.68, 2.14 |
| Race/ethnicity | ||
| Hispanic | 0.77 | 0.54, 1.11 |
| Black/other | 0.80 | 0.56, 1.16 |
| ZIP code (College Station vs Bryan) | 0.97 | 0.70, 1.34 |
| Influenza strain (type B) | 0.43* | 0.24, 0.76 |
| Hospitalization | ||
| Female | 1.00 | 0.74, 1.37 |
| Age group | ||
| 5-17 years | 0.62* | 0.41, 0.95 |
| 18-49 years | 1.28 | 0.83, 1.97 |
| 50-64 years | 2.60* | 1.42, 4.77 |
| 65 years or older | 5.18* | 2.81, 9.55 |
| Race/ethnicity | ||
| Hispanic | 3.03* | 2.06, 4.47 |
| Black/other | 1.32 | 0.88, 1.98 |
| ZIP code (College Station vs Bryan) | 0.44* | 0.31, 0.63 |
| Influenza strain (type B) | 0.75 | 0.40, 1.38 |
Abbreviation: CI, confidence interval; OR, odds ratio.
P < .05.
Although the CDC estimates influenza activity29 and vaccination coverage30 at the national, regional, and state levels, county-level data are not typically available. As this type of data can be important to health departments as they develop health education and vaccination campaigns, we calculated estimates of vaccination coverage for demographic groups (Table 5). During 2017, a total of 16 027 individuals with a Brazos County address received an influenza vaccine from a healthcare provider, pharmacy, or the TVFC, whereas the total population of Brazos County was 222 830. Using these totals, the estimated influenza vaccination coverage in Brazos County in 2017 was 71.92 per 1000 persons. Those between 18 and 49 years old had the lowest estimated coverage, likely because many in this age group who received a vaccine were not included in our data because they did not have a permanent address in Brazos County, which is home to Texas A&M University. However, Hispanics and those of other races had much lower estimated coverage than whites and African-Americans, perhaps highlighting the need to change approaches for reaching these populations with vaccinations for seasonal influenza.
Table 5.
Estimated vaccination coverage, Brazos County, Texas, 2017.
| County population (N = 222 830) |
Influenza vaccinations (N = 16 027) |
Vaccinations/1000 | |
|---|---|---|---|
| N | N (%) | ||
| Sex | |||
| Male | 112 775 | 5795 (36.16) | 51.39 |
| Female | 110 055 | 7481 (46.68) | 67.98 |
| Missing | 2751 (17.16) | – | |
| Age group | |||
| 0-4 | 13 921 | 2770 (17.28) | 198.98 |
| 5-17 | 32 262 | 3590 (22.40) | 111.28 |
| 18-49 | 128 578 | 4635 (28.92) | 36.05 |
| 50-64 | 28 348 | 2211 (13.80) | 77.99 |
| 65 or older | 19 721 | 2821 (17.60) | 143.05 |
| Race/ethnicity | |||
| African-American | 24 511 | 620 (3.87) | 25.29 |
| White | 124 562 | 2952 (18.42) | 23.70 |
| Hispanic | 57 490 | 134 (0.84) | 2.33 |
| Other | 16 267 | 207 (1.29) | 12.73 |
| Missing | 12 114 (75.58) | – | |
Discussion
Local health departments serve as the first line of defense against infectious disease outbreaks, including seasonal and pandemic influenza.31 However, little data related to trends in seasonal influenza or influenza vaccination coverage are available at the local health department level. Therefore, to assess influenza activity and vaccination coverage at the local health department level, agencies need to use voluntary reporting data from healthcare providers, which is likely incomplete as influenza and ILI are not reportable conditions, or dedicate limited epidemiologic resources to the active collection and analysis of data from healthcare and vaccine providers. When local-level data are available as part of local passive surveillance and reporting systems, there is rarely capacity or expertise at the local level to analyze these data and use them for the development of interventions or other programs.32 In addition, as federal funding accounts for more than three-quarters of the funding for epidemiologic activities in the states, federal priorities—such as a novel pandemic strain of influenza—may drive epidemiologic activities, with little funding being available on a year-to-year basis to analyze trends or develop and evaluate programs addressing seasonal influenza.33
Since 2010, annual vaccination for seasonal influenza has been recommended for all individuals 6 months of age or older in the United States.17 However, in some influenza seasons, and among some age groups, the level of protection offered by the vaccine is low.34 Our study provides some evidence that this may have been the case during December, 2017, in Brazos County, Texas. Those aged more than 65 were more likely to receive the influenza vaccine but were also more likely to be hospitalized due to complications resulting from their infection. In another aspect of this study published elsewhere,25 a CASPER survey was conducted among households in Brazos County. Most respondents who did not receive the vaccine reported no barriers to vaccination (71 of 99; 71.8%); however, African-Americans were less likely to receive a vaccine, whereas, in addition to those aged more than 65, those who believed the vaccine to be effective were more likely to be vaccinated. Among those reporting an objection to the vaccine, the most frequent objection was that the vaccine was not effective (19 of 35; 54.3%). In a spatial analysis, ZIP codes 77808 and 77803 both had higher rates of influenza vaccination per 1000 population but also reported numbers of cases of influenza per 1000 population during December 2017. The ZIP code 77840 had the lowest prevalence of influenza cases and vaccination, which was likely due to a large population of university students whose permanent home address is outside of Brazos County and were therefore not included in the data.
Our study also provides some evidence for the role that schools and school-aged children play in the transmission of seasonal influenza. In this study, 36% (589 of 1651) of the cases of laboratory-confirmed influenza in December 2017 were among children aged 5 to 17. Several studies of school-age children in Japan have demonstrated correlations between high vaccination coverage and reductions in the severity of influenza epidemics, particularly during influenza seasons in which vaccine efficacy is low.35 In addition, in this instance, about one-third of the residents of the Bryan-College Station Metropolitan Area are university students who belong to the least vaccinated age group in this study (18-49 years). A special emphasis on the vaccination of university students, in addition to school children, may be effective in reducing the transmission of influenza in this community.
Part of the reason for the increase in the number of influenza cases in December 2017 was that the vaccine being used for the 2017-2018 influenza season was widely reported to be a poor match for the predominantly circulating strain, which was Influenza A (H3N2).36 Studies from the influenza season in Australia, which occurs prior to the major US influenza season during the southern hemisphere winter months, showed that the vaccine was only 10% effective against H3N2, although higher vaccine effectiveness was reported later from Canada (17%), the United States (25%), and Spain (29%).37 Another reason that Brazos County and public health departments across the United States were seeing an elevated number of cases of influenza in December 2017 was that national vaccination coverage was only 38.6%, the lowest early season coverage since 2014-2015.38
This study has several important limitations. Not all vaccination facilities and healthcare providers in Brazos County provided vaccination data and data about laboratory-confirmed cases to the BCHD on request. However, those providing data did include 3 of the 5 major pharmacy chains and the 5 largest healthcare providers in Brazos County, providing some level of confidence that, although the data are incomplete, they are representative. The geographic location of vaccination and healthcare facilities also covered the entire county, including rural communities outside of the College Station-Bryan Metropolitan Area. Of those that did provide data, some facilities did not include data on the vaccinated persons’ age, sex, or ZIP code; therefore, these records were not able to be included in all of our analyses. Of the total number of reported vaccinations administered during 2017, only 20% (16 027 of 75 520) had a verifiable address that met the inclusion criteria for this study. The remainder reported a residential address outside of Brazos County. This is reasonable given that Brazos County is home to Texas A&M University, a public university with an enrollment of more than 68 000 students, many of whom use their family’s home address as their “official address” on documents such as their driver’s license or health insurance cards. This study used vaccination data for the time period of January 1 through December 31, 2017, which included some vaccinations for the 2016-2017 season as well as the 2017-2018 influenza season. We were required to include all 2017 vaccinations because 76% of the records provided (57 293 of 75 520) did not include data for the date variable beyond the year. Only 35% (584 of 1651) of influenza cases had a known vaccination status, whereas data on influenza cases and vaccination status were not able to be obtained from local long-term care facilities.
Conclusions
Influenza vaccination coverage in Brazos County, Texas, is likely less than half the Healthy People 2020 target of 70%. Additional data on influenza cases and vaccination coverage are needed by local public health authorities who are typically responsible for the implementation of health education and vaccination campaigns to limit the public health impact of both seasonal and pandemic influenza. Data must be used to inform the development of new messages and dissemination of these messages to specific groups at higher risk of infection, hospitalization, and other complications. Increased use of social media, local television and radio, and other communication methods that can reach parents, older adults, and Hispanics is particularly needed.
Footnotes
Funding:The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of Conflicting Interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: YA and JA conceived of the study. IK and OM conducted the data analysis. JAH drafted the manuscript. All authors contributed edits to the manuscript.
ORCID iDs: Osaro Mgbere  https://orcid.org/0000-0002-2863-6284
https://orcid.org/0000-0002-2863-6284
Jennifer A Horney  https://orcid.org/0000-0003-3060-0894
https://orcid.org/0000-0003-3060-0894
References
- 1. Centers for Disease Control and Prevention. Clinical signs and symptoms of influenza. https://www.cdc.gov/flu/professionals/acip/clinical.htm. Updated May 26, 2016. Accessed January 4, 2018.
- 2. World Health Organization. Manual for the Laboratory Diagnosis and Virological Surveillance of Influenza. http://www.who.int/influenza/gisrs_laboratory/manual_diagnosis_surveillance_influenza/en/. Updated 2011.
- 3. Thompson WW, Shay DK, Weintraub E, et al. Mortality associated with influenza and respiratory syncytial virus in the united states. JAMA. 2003;289:179–186. [DOI] [PubMed] [Google Scholar]
- 4. Zucs P, Buchholz U, Haas W, Uphoff H. Influenza associated excess mortality in Germany, 1985–2001. Emerg Themes Epidemiol. 2005;2:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Izurieta HS, Thompson WW, Kramarz P, et al. Influenza and the rates of hospitalization for respiratory disease among infants and young children. N Engl J Med. 2000;342:232–239. [DOI] [PubMed] [Google Scholar]
- 6. Brammer TL, Izurieta HS, Fukuda K, et al. Surveillance for influenza–United States, 1994–95, 1995–96, and 1996–97 seasons. MMWR CDC Surveill Summ. 2000;49:13–28. [PubMed] [Google Scholar]
- 7. Barker WH, Mullooly JP. Pneumonia and influenza deaths during epidemics: implications for prevention. Arch Intern Med. 1982;142:85–89. [PubMed] [Google Scholar]
- 8. Centers for Disease Control and Prevention. Pandemic influenza. https://www.cdc.gov/flu/pandemic-resources/. Updated March 5, 2018.
- 9. Carrat F, Flahault A. Influenza vaccine: the challenge of antigenic drift. Vaccine. 2007;25:6852–6862. [DOI] [PubMed] [Google Scholar]
- 10. Bish A, Yardley L, Nicoll A, Michie S. Factors associated with uptake of vaccination against pandemic influenza: a systematic review. Vaccine. 2011;29:6472–6484. [DOI] [PubMed] [Google Scholar]
- 11. Aiello AE, Coulborn RM, Aragon TJ, et al. Research findings from nonpharmaceutical intervention studies for pandemic influenza and current gaps in the research. Am J Infect Control. 2010;38:251–258. [DOI] [PubMed] [Google Scholar]
- 12. Centers for Disease Control and Prevention. Disease burden of influenza. https://www.cdc.gov/flu/about/disease/burden.htm. Updated May 22, 2018. Accessed January 4, 2018.
- 13. Fairbrother G, Cassedy A, Ortega-Sanchez IR, et al. High costs of influenza: direct medical costs of influenza disease in young children. Vaccine. 2010;28: 4913–4919. [DOI] [PubMed] [Google Scholar]
- 14. Osterholm MT, Kelley NS, Sommer A, Belongia EA. Efficacy and effectiveness of influenza vaccines: a systematic review and meta-analysis. Lancet Infect Dis. 2012;12:36–44. [DOI] [PubMed] [Google Scholar]
- 15. Fiore AE, Fry A, Shay D, et al. ; Centers for Disease Control and Prevention (CDC). Antiviral agents for the treatment and chemoprophylaxis of influenza—recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Surveill Summ. 2011;60:1–24. [PubMed] [Google Scholar]
- 16. Harper SA, Bradley JS, Englund JA, et al. Seasonal influenza in adults and children-diagnosis, treatment, chemoprophylaxis, and institutional outbreak management: clinical practice guidelines of the Infectious Diseases Society of America. Clin Infect Dis. 2009;48:1003–1032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Fiore AE, Uyeki TM, Broder K, et al. Prevention and control of influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices (ACIP), 2010. MMWR Recomm Rep. 2010;59:1–62. [PubMed] [Google Scholar]
- 18. Jefferson T, Di Pietrantonj C, Rivetti A, Bawazeer GA, Al-Ansary LA, Ferroni E. Vaccines for preventing influenza in healthy adults. Cochrane Database Syst Rev. 2010;7:CD001269. [DOI] [PubMed] [Google Scholar]
- 19. Centers for Disease Control and Prevention. Seasonal influenza vaccine effectiveness, 2005–2018. https://www.cdc.gov/flu/professionals/vaccination/effectiveness-studies.htm. Updated February 15, 2018. Accessed May 5, 2018.
- 20. Centers for Disease Control and Prevention. 2016-17 influenza season vaccination coverage report. www.cdc.gov/flu/fluvaxview/reportshtml/reporti1617/reporti/index.html. Updated September 28, 2017. Accessed January 4, 2018.
- 21. Centers for Disease Control and Prevention. How CDC classifies flu severity. https://www.cdc.gov/flu/professionals/classifies-flu-severity.htm. Updated May 4, 2018. Accessed July 17, 2018.
- 22. Budd AP, Wentworth DE, Blanton L, et al. Update: influenza activity—United States, October 1, 2017-February 3, 2018. MMWR Morb Mortal Wkly Rep. 2018;67:169–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Garten R, Blanton L, Elal AIA, et al. Update: influenza activity in the United States during the 2017–18 season and composition of the 2018–19 influenza vaccine. MMWR Morb Mortal Wkly Rep. 2018;67:634–642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Texas Department of State Health Services. Notifiable conditions. https://www.dshs.texas.gov/idcu/investigation/conditions/. Updated April 2, 2018. Accessed July 17, 2018.
- 25. Stone KH, Akpalu Y, Horney JA. Use of the Community Assessment for Public Health Response (CASPER) method to assess influenza vaccination and activity in Brazos County, Texas. Vaccine. 2018;36:6001–6006. [DOI] [PubMed] [Google Scholar]
- 26. Texas Department of State Health Services. Texas Vaccines for Children Program—Immunization Unit. https://www.dshs.texas.gov/immunize/tvfc/. Updated May 15, 2018. Accessed July 25, 2018.
- 27. Heinonen S, Silvennoinen H, Lehtinen P, et al. Early oseltamivir treatment of influenza in children 1-3 years of age: a randomized controlled trial. Clin Infect Dis. 2010;51:887–894. [DOI] [PubMed] [Google Scholar]
- 28. Hall RJ, Peacey MP, Ralston JC, et al. Pandemic Influenza A (H1N1) viruses currently circulating in New Zealand are sensitive to Oseltamivir. Eurosurveillance. 2009;14:19282. [DOI] [PubMed] [Google Scholar]
- 29. Centers for Disease Control and Prevention. FluView. https://www.cdc.gov/flu/weekly/. Updated September 15, 2018. Accessed September 21, 2018.
- 30. Centers for Disease Control and Prevention. FluVaxView. https://www.cdc.gov/flu/fluvaxview/index.htm. Updated April 4, 2018. Accessed September 21, 2018.
- 31. Balicer RD, Omer SB, Barnett DJ, Everly GS., Jr. Local public health workers’ perceptions toward responding to an influenza pandemic. BMC Public Health. 2006;6:99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Nsubuga P, White ME, Thacker SB, et al. Public health surveillance: a tool for targeting and monitoring interventions. In: Jamison DT, Breman JG, Measham AR, et al., eds. Disease Control Priorities in Developing Countries. Washington, DC: World Bank; 2006:997–1018. [Google Scholar]
- 33. Council of State and Territorial Epidemiologists. 2017. Epidemiology Capacity Assessment Report. https://cdn.ymaws.com/www.cste.org/resource/resmgr/eca/2017_ECA_Report_Web_final.pdf. Accessed July 25, 2018. [DOI] [PMC free article] [PubMed]
- 34. Flannery B, Chung JR, Belongia EA, et al. Interim estimates of 2017–18 seasonal influenza vaccine effectiveness—United States, February 2018. Am J Transplant. 2018;18:1020–1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Uchida M, Kaneko M, Hidaka Y, et al. High vaccination coverage is associated with low epidemic level of seasonal influenza in elementary schools: an observational study in Matsumoto City, Japan. BMC Infect Dis. 2018;18:128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Paules CI, Sullivan SG, Subbarao K, Fauci AS. Chasing seasonal influenza-the need for a universal influenza vaccine. N Engl J Med. 2018;378:7–9. [DOI] [PubMed] [Google Scholar]
- 37. Sullivan SG, Chilver MB, Carville KS, et al. Low interim influenza vaccine effectiveness, Australia, 1 May to 24 September 2017. Euro Surveill. 2017. October 26;22(43):17–00707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Centers for Disease Control and Prevention. National Early-Season Flu Vaccination Coverage, United States, November 2017. https://www.cdc.gov/flu/fluvaxview/nifs-estimates-nov2017.htm. Updated December 9, 2017. Accessed January 18, 2018.