Highlights
-
•
Forward head posture is not associated with muscular performance in either groups.
-
•
Forward head posture does not explain pain and disability in CNP patients.
-
•
The muscle size–endurance relationship is affected in CNP.
-
•
Deep cervical muscles are selectively affected in the presence of CNP.
Keywords: Chronic neck pain, Head posture, Extensor muscles, Flexor muscles, Muscle endurance, Ultrasonography
Abstract
Background
Forward head posture (FHP) and muscular dysfunction are likely contributing factors to chronic neck pain (CNP) but there are inconsistent findings on the relevance of these factors to clinical CNP characteristics.
Objective
To compare FHP, cervical muscles size and endurance between CNP and asymptomatic participants and to investigate their association with pain and disability and relative involvement of deep/superficial and flexor/extensor muscles.
Methods
Thirty-two patients with CNP and 35 asymptomatic participants were included in this case–control study. FHP in standing, extensor and flexor muscles endurance and dimensions were assessed using digital photography, clinical tests and ultrasonographic imaging, respectively. The visual analog scale and neck disability index were also used to evaluate CNP patients’ clinical characteristics.
Results
Deep flexor (mean difference = 0.06, 95% CI = 0.02–0.11) and extensor muscles size (mean difference = 0.07, 95% CI = 0.01–0.12) were found to be significantly smaller in CNP patients. CNP patients also demonstrated lower levels of flexor (mean difference = 14.68, 95% CI = 3.65–25.72) and global extensor endurance capacity. FHP was neither different between the groups nor correlated with any of the dependent variables. Neither FHP nor endurance was correlated with pain/disability. Extensor endurance in both groups and flexor endurance in the asymptomatic group showed significant correlations with muscles size.
Conclusions
FHP was found neither different between groups nor correlated with muscle performance or CNP clinical characteristics. While cervical endurance was found lower in CNP patients, it did not show any association with pain/disability. The muscular size–endurance relationship seems to become more complex in the presence of NP. While deep muscles seem to be differentially affected in the presence of CNP, the alterations do not seem to be uniform in the flexor and extensor groups.
Introduction
Optimal head and neck posture is important to minimize the need for muscular activity and the stress imposed on the cervical tissues.1 Forward head posture (FHP), defined as the forward displacement of the head on the cervical spine, has been commonly associated with neck pain.1, 2, 3, 4 This malalignment has been suggested to increase stress on the posterior cervical elements,1 affect the length–tension relationship in the cervical muscles,5 increase muscular activity level,6 restrict neck movement7, 8 and impair cervical proprioception.9
Chronic neck pain (CNP) is a highly prevalent and multifaceted disorder being associated with various dysfunctions both in the cervical region and other regions functionally associated with the neck.10, 11, 12 Janda13 has suggested reduced cervical muscles strength and endurance to be the result of sustained FHP by disturbing the optimal length–tension relationship.13 On the other hand, reduced muscular endurance has been proposed as a possible mechanism for losing the ability to maintain optimal posture, ultimately leading to FHP by some other authors.14 Despite the intuitive assumption that FHP is determining in CNP characteristics, controversial findings on the difference of head alignment in these patients and asymptomatic subjects question the relevance of FHP to CNP.15 On the other hand, superficial flexor muscles training in CNP patients has demonstrated a considerable level of clinical recovery without having modified FHP.16 Investigation of the correlation between FHP and muscular performance and clinical CNP characteristics may further elucidate how relevant FHP might be to CNP and it also provides some evidence on the possible mechanisms of the effect of FHP on the functioning of the cervical region.
Various levels of involvement have been attributed to deep and superficial groups of cervical muscles in the presence of CNP.17, 18, 19 Since exercise therapy selectively targets specific muscles,16 clear identification of the involved elements is a prerequisite for successful rehabilitation of CNP. While endurance capacity is believed to be provided by corresponding muscles activation,20 in a series of preliminary studies, this relationship was found to be affected in the presence of CNP.17, 21, 22 Neck disability index (NDI) and pain intensity were found to be merely correlated with extensor muscles endurance and size,17 respectively, while there were no correlations between the clinical characteristics of the CNP patients and any of the flexor group variables.21, 22, 23 The endurance scores of the flexor21, 22 and extensor17 muscles were also poorly correlated with their size especially in CNP cases. To the best of the authors’ knowledge, no study has yet compared the relative involvement of the flexor/extensor and superficial/deep muscle groups of the cervical region in CNP patients. The long-lasting presence of pain in these patients is believed to impose adaptive alterations in the motor control strategies of the cervical region.24 This might cause the relationships among the discrete components of the postural control system (namely muscle size, endurance and cervical posture) not to be simply explained by the biomechanical principles. In other words, the interactions between these elements might have become more complex by the neuromuscular adaptations to chronic pain. Investigation of these relationships in CNP patients and asymptomatic participants besides comparison of FHP between the two groups will shed light on this assumption.
The aims of this study were (1) to compare the cervical muscles size, endurance and posture and their relationships in CNP patients and asymptomatic participants, (2) to investigate the association of cervical muscles size, endurance and posture with clinical CNP characteristics and (3) to investigate the relative involvement of the deep vs. superficial and flexor vs. extensor neck muscles in CNP patients. We hypothesized that CNP patients will have smaller cervical muscles and reduced endurance and altered cervical posture in terms of FHP comparing the control group. The association between these factors was also hypothesized to be affected in the presence of CNP. The other hypothesis of the current study was that deep cervical muscles will be selectively affected by CNP.
Methods
Design
This is a cross-sectional correlational analysis study conducted from April to October 2016.
Participants
Thirty-two CNP patients and 35 pain-free adults participated in this study. Patients were all referred from outpatient orthopaedic clinics in Tehran. The control group participants were selected from university campus and hospitals students and employees. The sample size was calculated based on the mean and standard deviation of the FHP measure, as the primary outcome, in a pilot study on 15 participants from each group. To yield the power of 0.80 at a = 0.05 and the effect size of 0.75, we needed 30 participants in each group.
Participants in both groups were 20–55 years old. The inclusion criteria for the CNP group were as follows: experience of pain felt dorsally between the inferior margin of the occiput and the first thoracic spine, persistent or episodic pain not associated with any trauma or known pathology for at least 3 months with a frequency no less than once a week.25 The asymptomatic group had no history of neck pain within the year before the study. Participants would be excluded from either group if they reported any of the following conditions: a history of cervical trauma or surgery; congenital anomalies involving the spine (cervical, thoracic or lumbar); structural abnormalities such as scoliosis; systemic arthritis; positive Spurling test (to exclude radiculopathies26), diagnosis of fibromyalgia, or any disorder of the central nervous system and history of neck physical therapy within 6 months prior to our testing. All participants voluntarily took part in the study by signing the informed consent form approved by the Human Ethical Committee of the University of Social Welfare and Rehabilitation Sciences (Tehran, Iran) after being familiarized with the purpose and content of the study.
Outcome measures
Clinical pain characteristics
Pain intensity over the last week was measured using a blank 10-cm visual analog scale (VAS), where 0 anchored to ‘no pain at all’ and 10 to ‘the worst imaginable pain’. Neck pain-related disability was assessed by the Persian version of the neck disability index (NDI-P).27 NDI covers 10 items of daily living activities and is scored from 0 to 50, with higher scores corresponding to greater disability.
Forward head posture
For the assessment of FHP, a lateral view photo was captured from the participants in the relaxed standing posture by asking them to share their weight symmetrically on both lower extremities while standing barefoot with the feet shoulder width apart.28 We decided to assess FHP in the standing posture because it is more commonly used in the clinical setting29 and to make comparison of the results possible with those of other studies.1, 15, 29, 30, 31 FHP assessed in this posture has also been found to be more sensitive in discriminating CNP patients from healthy controls.32 Participants would flex and extend their head three times before assuming the comfortable neutral head position. A digital camera (Olympus, SP-590UZ, 12 megapixel, 26× optical wide zoom) was placed at a 2-m distance from the participant's right side and fixed on tripods. The lens of the camera was set at the height of the participant's shoulder. The spinous process of C7 and tragus of the ear were marked with round adhesive tapes as landmarks to be captured by photography. The images were processed offline by Photoshop software CS6. The cranio-cervical angle formed by intersection of the horizontal line passing through C7 and the line extending from the tragus of the ear to C7 marker was used to measure FHP33 (Fig. 1). This FHP measurement procedure has shown to be both reliable and valid against radiological measurements as the gold standard.34
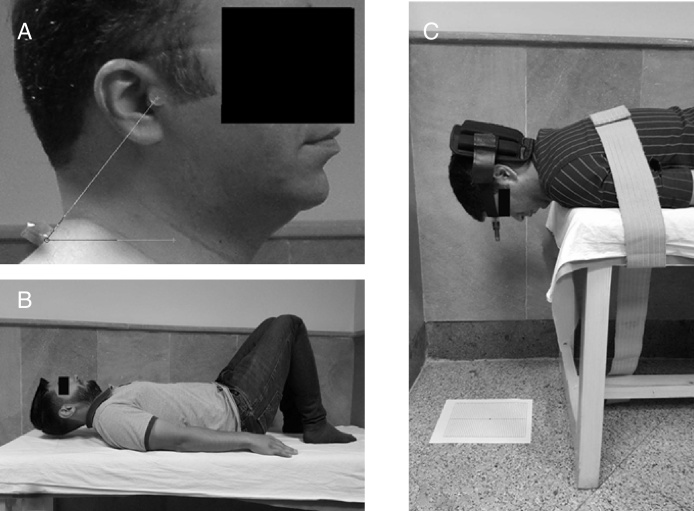
Figure 1.
An illustration of the assessment of the FHP defined as the cranio-cervical angle (A) and clinical flexor (B) and extensor (C) endurance tests performance.
Clinical endurance tests
To perform the flexor endurance test, participants were asked to lie in the crook lying position and to raise their head approximately 2 cm off the plinth while keeping their chins tucked in (cranio-cervical flexion posture) (Fig. 1). The time the participants could maintain this posture was measured in seconds.35 For extensor endurance, the participants were positioned prone with their head protruding from the plinth and instructed to assume the chin tuck position with an external load (2 kg for women and 4 kg for men) applied to the posterior aspect of the head. The external resistance magnitude was determined based on previous works.17, 36 Five seconds of at least 5° of deviation from the neutral position to cranio-cervical flexion or extension or five repetitions of less than 5° deviation was considered as test termination.37 For the purpose of real-time assessment of the head deviations, a laser beam and a graded paper were used as illustrated in Fig. 1. If the test was terminated in the cranio-cervical flexion position, the holding time was recorded as “global (superficial and deep) extensors endurance” while extended cervical spine at the end of test would yield “local (deep) extensors endurance”.38 The holding time regardless of representing deep or superficial muscles endurance was considered as the “total extensors endurance”.17, 21
Ultrasonography imaging (USI)
Neck muscles size was measured by a real-time ultrasonography device (SONOLINE G40™, Siemens, Germany) with an 8 MHz, 38.7 mm linear array transducer.
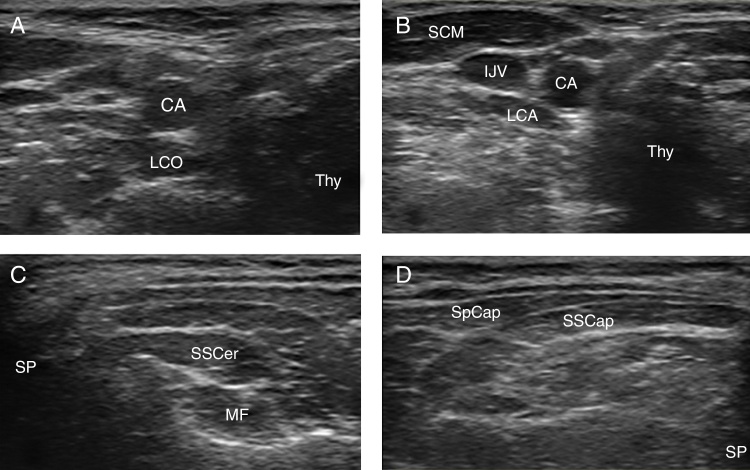
The flexor (longus colli/capitis, sternocleidomastoid) and extensor (Splenius capitis, Smispinalis capitis, Semispinalis cervicis and Multifidus) muscles were imaged in the crook lying and prone positions, respectively. The probe placement and landmark details have been fully described in previous studies17, 21 (Fig. 2). B-mode US images were captured and measurements of muscle dimensions were performed using on-screen-calipers. The antero-posterior (AP) dimension as the farthest distance from the anterior to posterior border of the muscle and the cross-section area (CSA) by tracing around the muscle border were used to identify the muscle size. The two ends of the splenius capitis and sternocleidomastoid muscles were rarely captured in the static USI which made CSA measurement impossible. In patients with bilateral CNP and asymptomatic participants, the mean values of US imaging measures of bilateral sides and in unilateral neck pain patients, the measures for the ipsilateral muscles were used for statistical analysis.
Figure 2.
A sample of US image of the cervical flexor and extensor muscles in one of the subjects from the CNP group: (A) LCO, longus colli; (B) SCM, sternocleidomastoid; LCA, longus capitis; (C) SSCer, semispinalis cervicis; MF, multifidus; (D) Sp Cap, splenius capitis; SSCap, semispinalis capitis. CA, carotid artery; IJV, internal jugular vein; Thy, thyroid gland; SP, spinous process.
Procedure
Demographic and anthropometric data were collected for both groups. All patients completed the NDI and VAS following familiarization with the test procedure. USI and head posture assessment were performed prior to endurance tests to avoid fatigue. The order of flexor and extensor muscles US imaging and endurance tests were randomized. Endurance tests were performed once to prevent pain exacerbation in patients. All tests were performed by a physical therapist with 11 years of clinical experience in the field of spine physical therapy who was trained in USI of the spinal muscles. To avoid bias, the examiner was unaware of the group to which the participants belonged.
Data analysis
Data distribution was verified by the Shapiro–Wilk test. Independent t-test and Mann–Whitney U-test were used for between-groups comparison of anthropometric data, FHP, flexor and extensor endurance scores and muscle size (thickness, CSA) for normally and non-normally distributed data, respectively. To assess the reliability of the endurance tests and FHP measurements, 20 participants (10 patients with CNP and 10 asymptomatic participants) were assessed in two sessions 5–7 days apart. Intra-class correlation coefficient (ICC) (2-way random, absolute agreement model) was used to determine the relative reliability of the measurements. The associations between FHP, endurance scores, muscle size, NDI and VAS scores were explored using Spearman and Pearson correlation coefficients. Correlations were classified as “little or no” (r < 0.25), “fair to moderate” (0.25 < r < 0.5), “moderate to good” (0.5 < r < 0.75) or “good to excellent” (0.75 < r).39 Statistical significance was set at p < 0.05. The statistical analyses were performed using statistical package SPSS software (version 21; SPSS Inc., Chicago, IL).
Results
No significant difference was found between the demographic characteristics of the two groups (Table 1). There were no dropouts or missing data. Between-sessions reliability analysis of the FHP (ICC3,1 = 0.85), flexor (ICC3,1 = 0.83) and extensor (ICC3,1 = 0.88) endurance tests were indicative of a “high” level of relative reliability (ICC3,1 = 0.70–0.89) according to Munrro's classification.40
Table 1.
Comparison of the demographic variables between the two groups.
| Characteristic | CNP (n = 32) | Asymptomatic (n = 35) | p-Value |
|---|---|---|---|
| Sex (% female) | 71 | 65 | 0.67 |
| Age (y) | 36.46 ± 9.40 | 37.31 ± 10.35 | 0.74 |
| Height (cm) | 166.06 ± 10.19 | 166.71 ± 8.20 | 0.62 |
| Weight (kg) | 69.09 ± 11.67 | 70.27 ± 11.68 | 0.71 |
| Past week pain intensity (VAS) | 3.95 ± 2.15 | NA | |
| Neck disability (score) | 11.06 ± 5.82 | NA |
Values are presented as mean ± SD. CNP, chronic neck pain; VAS, visual analog scale; NA, not applicable.
Between-groups comparisons revealed significant differences for semispinalis cervicis, multifidus and longus colli thickness (p = 0.003, p = 0.008, p = 0.003, respectively) and CSA (p = 0.006, p = 0.002, p = 0.001, respectively). The CNP patients also showed lower levels of flexor (p = 0.011), total extensor (p < 0.001) and global extensor (p = 0.001) endurance in comparison with the asymptomatic participants. The groups were not statistically different in the other measured variables (p > 0.05). The mean difference of the dependent variables between the two groups and the corresponding confidence intervals are presented in Table 2.
Table 2.
Between groups comparison of the dependent variables including FHP, US imaging measures and endurance test results.
| Mean ± SD |
Mean difference | 95% CI of the mean difference | p-value | Effect size | ||||
|---|---|---|---|---|---|---|---|---|
| CNP group | Asymptomatic group | |||||||
| Flexor muscles | LCO | AP | 0.46 ± 0.08 | 0.53 ± 0.09 | 0.06 ± 0.02 | 0.02, 0.11 | <0.01* | 0.82 |
| CSA | 0.42 ± 0.10 | 0.52 ± 0.13 | 0.10 ± 0.02 | 0.04, 0.16 | <0.01* | 0.86 | ||
| LCA | AP | 0.35 ± 0.08 | 0.39 ± 0.09 | 0.03 ± 0.02 | −0.00, 0.08 | 0.08 | 0.46 | |
| CSA | 0.33 ± 0.13 | 0.36 ± 0.09 | 0.02 ± 0.02 | −0.03, 0.08 | 0.36 | 0.26 | ||
| SCM | AP | 0.79 ± 0.13 | 0.86 ± 0.15 | 0.06 ± 0.03 | −0.00, 0.13 | 0.07 | 0.49 | |
| Extensor muscles | MF | AP | 0.29 ± 0.08 | 0.36 ± 0.12 | 0.07 ± 0.02 | 0.01, 0.12 | <0.01* | 0.68 |
| CSA | 0.21 ± 0.12 | 0.30 ± 0.20 | <0.01* | 0.54 | ||||
| SSCer | AP | 0.36 ± 0.07 | 0.43 ± 0.10 | 0.06 ± 0.02 | 0.02, 0.11 | <0.01* | 0.81 | |
| CSA | 0.42 ± 0.11 | 0.53 ± 0.20 | <0.01* | 0.68 | ||||
| SSCap | AP | 0.44 ± 0.07 | 0.47 ± 0.09 | 0.02 ± 0.02 | −0.01, 0.06 | 0.25 | 0.37 | |
| CSA | 0.72 ± 0.16 | 0.79 ± 0.21 | 0.06 ± 0.04 | −0.02, 0.16 | 0.14 | 0.37 | ||
| Sp Cap | AP | 0.42 ± 0.08 | 0.46 ± 0.13 | 0.04 ± 0.02 | −0.01, 0.09 | 0.16 | 0.37 | |
| Total extensor endurance | 166.21 ± 192.32 | 293.74 ± 184.93 | <0.01* | 0.67 | ||||
| Local extensor endurance | 204.166 ± 197.02 | 210.76 ± 93.23 | 0.32 | 0.04 | ||||
| Global extensor endurance | 92.72 ± 115.99 | 222.73 ± 130.05 | <0.01* | 1.05 | ||||
| Flexor endurance | 29.00 ± 17.88 | 43.68 ± 26.15 | 14.68 ± 5.52 | 3.65, 25.72 | 0.01* | 0.65 | ||
| FHP | 51.31 ± 6.29 | 49.80 ± 7.31 | 0.30 | 0.22 | ||||
CNP, chronic neck pain; LCO, longus colli; LCA, longus capitis; SCM, sternocleidomastoid; MF, multifidus; SSCer, semispinalis cervicis; SSCap, semispinalis capitis; Sp Cap, splenius capitis; AP, antero-posterior; CSA, cross-section area; FHP, forward head posture; CI, confidence interval.
The FHP, endurance test results, muscles thickness (AP) and CSA expressed in terms of degree, second, cm and cm2, respectively. 95% CI has not been reported for non-normally distributed variables.
Statistically significant difference.
In the CNP group, FHP was significantly correlated neither with VAS (r = 0.07, p = 0.67) nor with NDI (r = 0.15, p = 0.38). FHP was not significantly correlated with any of the endurance test results or muscle sizes (p > 0.05). Endurance capacity tests were not correlated with VAS or NDI (p > 0.05). The global extensor endurance showed a positive significant correlation with multifidus CSA (r = 0.51, p = 0.031) and thickness (r = 0.54, p = 0.013). The local extensor endurance scores were positively correlated with CSA of semispinalis capitis (r = 0.61, p = 0.032). There was no significant correlation between flexor endurance scores and flexor muscles dimensions (p > 0.05) (Table 3). There was no significant correlation between muscle sizes with VAS except a significant negative correlation between CSA of multifidus and VAS (r = −0.44, p = 0.013). Thickness of splenius capitis (r = 0.41, p = 0.011) and longus colli CSA (r = 0.48, p = 0.001) was positively correlated with NDI. In the asymptomatic participants, FHP was not correlated with flexor or extensor endurance tests and muscles sizes except thickness of splenius capitis (r = 0.38, p = 0.022). The flexor endurance scores showed significant positive correlation with longus capitis CSA (r = 0.38, p = 0.022), longus colli CSA (r = 0.40, p = 0.014) and thickness (r = 0.57, p = 0.001). There was a significant correlation between total extensor capacity scores with semispinalis capitis CSA (r = 0.41, p = 0.012) and thickness (r = 0.33, p = 0.044). The global extensor endurance test was correlated with CSA of multifidus (r = 0.52, p = 0.041) and semispinalis capitis (r = 0.61, p = 0.012) (Table 3).
Table 3.
Correlational analysis of the head posture, cervical endurance and muscle size in the CNP and asymptomatic groups.
| CNP group |
Asymptomatic group |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| FHP | Flexor end | Total Ext end | Global Ext end | Local Ext end | FHP | Flexor end | Total Ext end | Global Ext end | Local Ext end | ||
| SpCap (AP) | r (p) | 0.21 (0.24) | −0.39 (0.02*) | −0.08 (0.63) | 0.01 (0.94) | 0.18 (0.56) | 0.38 (0.02*) | 0.33 (0.05) | 0.23 (0.18) | 0.38 (0.15) | −0.05 (0.85) |
| SSCap (AP) | r (p) | −0.03 (0.85) | 0.44 (0.01*) | 0.11 (0.52) | −0.10 (0.68) | 0.16 (0.60) | 0.16 (0.33) | 0.40 (0.01*) | 0.33 (0.04*) | 0.47 (0.07) | 0.34 (0.24) |
| SSCap (CSA) | r (p) | 0.10 (0.56) | 0.42 (0.01*) | 0.27 (0.12) | 0.16 (0.51) | 0.61 (0.03*) | 0.21 (0.20) | 0.42 (0.01*) | 0.41 (0.01*) | 0.61 (0.01*) | 0.37 (0.20) |
| SSCer (AP) | r (p) | −0.34 (0.050 | 0.44 (0.01*) | 0.13 (0.45) | 0.43 (0.07) | −0.09 (0.77) | 0.17 (0.31) | 0.62 (<0.01*) | 0.09 (0.59) | 0.17 (0.54) | 0.32 (0.27) |
| SSCer (CSA) | r (p) | −0.20 (0.27) | 0.26 (0.15) | 0.09 (0.59) | 0.40 (0.09) | −0.22 (0.94) | −0.01 (0.93) | 0.09 (0.60) | 0.10 (0.54) | 0.27 (0.32) | 0.26 (0.37) |
| MF (AP) | r (p) | −0.11 (0.53) | 0.00 (0.96) | 0.06 (0.74) | 0.54 (0.01*) | 0.18 (0.57) | 0.17 (0.32) | 0.53 (<0.01*) | 0.30 (0.08) | 0.42 (0.11) | 0.48 (0.09) |
| MF (CSA) | r (p) | −0.03 (0.85) | 0.10 (0.58) | 0.04 (0.82) | 0.51 (0.03*) | 0.08 (0.78) | 0.16 (0.34) | 0.53 (<0.01*) | 0.25 (0.14) | 0.52 (0.04*) | 0.22 (0.45) |
| LCO (AP) | r (p) | 0.07 (0.70) | 0.13 (0.45) | 0.05 (0.77) | −0.19 (0.43) | 0.48 (0.11) | 0.18 (0.29) | 0.57 (<0.01*) | 0.16 (0.34) | 0.42 (0.11) | 0.23 (0.43) |
| LCO (CSA) | r (p) | 0.26 (0.14) | −0.27 (0.12) | 0.02 (0.89) | −0.14 (0.55) | 0.32 (0.30) | 0.23 (0.16) | 0.40 (0.04*) | −0.17 (0.30) | 0.37 (0.17) | 0.03 (0.90) |
| LCA (AP) | r (p) | 0.07 (0.67) | −0.17 (0.32) | 0.08 (0.66) | 0.00 (0.99) | 0.18 (0.56) | −0.10 (0.56) | 0.13 (0.45) | 0.57 (<0.01*) | 0.31 (0.25) | 0.53 (0.05) |
| LCA (CSA) | r (p) | 0.01 (0.94) | −0.32 (0.07) | −0.03 (0.83) | 0.07 (0.75) | 0.03 (0.90) | 0.03 (0.82) | 0.38 (0.02*) | 0.46 (<0.01*) | 0.46 (0.08) | 0.41 (0.16) |
| SCM (AP) | r (p) | 0.09 (0.62) | 0.23 (0.20) | 0.16 (0.36) | −0.29 (0.23) | 0.33 (0.29) | −0.05 (0.74) | 0.05 (0.76) | 0.38 (0.02*) | 0.11 (0.68) | −0.04 (0.87) |
CNP, chronic neck pain; FHP, forward head posture; End, endurance; SpCap, splenius capitis; SSCap, semispinalis capitis; SSCer, semispinalis cervicis; MF, multofidus; LCO, longus colli; LCA, longus capitis; SCM, sternocleidomastoid; AP, antero-posterior; CSA, cross-section area. r: Pearson or Spearman correlation of coefficients.
The FHP, endurance test results, muscles thickness (AP) and CSA expressed in terms of degree, second, cm and cm2, respectively.
Statistically significant correlation.
Discussion
The findings of the present study demonstrated that the cranio-cervical angle (defining FHP) was not different between the CNP and the asymptomatic groups. The results also showed that FHP was neither associated with the clinical neck pain characteristics nor with neck muscles endurance capacity and size except for SpCap thickness in the asymptomatic group. Investigations comparing FHP in patients with neck pain and asymptomatic participants have yielded inconsistent findings.41 Oliveira and Silva15 found the cranio-cervical angle to be smaller in adolescents with neck pain with no correlation between FHP and flexor or extensor endurance capacities in either neck pain or asymptomatic groups.15 Bokaee et al.42 failed to demonstrate any significant difference in the cervical muscles thickness except SCM of participants with or without FHP.42 Only 10–15% of the pain and disability intensities were reported to be explained by FHP.1 Pain and disability amelioration in response to cervical endurance training in patients with neck pain has been found as independent from FHP correction.16 Overall, the findings of our study and those of others may suggest immediate FHP assessment (not accompanying any functional task or after a sustained posture) not to be as relevant to CNP as thought before. The alterations of the FHP might become discriminative in CNP patients following prolonged postures or while being concomitant with cognitively or physically loading tasks.43 These issues need to be further investigated in future studies.
Our results showed less flexor, total and global extensor endurance capacity in the patients with CNP comparing those of the asymptomatic participants. The patients had also smaller deep flexor and extensor muscles. But the noticeable finding was that these factors were barely correlated with pain intensity or disability. This suggests that cervical muscles endurance reduction in CNP patients may not be simply explained by pain in this region. Although not investigated in the current study, factors such as pain avoidance and kinesophobia44 might have affected the time the patients would hold the tests position against gravity. This issue might also be viewed from the range of the existing associations between muscle size and endurance test scores. A noticeably broader range of variables in the asymptomatic group elicited a significant correlation regarding the muscular size and endurance parameters. Limitation of these associations in the CNP group might have implications identifying the motor control adaptations in these patients. It seems that these connections become interrupted in the presence of neck pain but determination of the intervening factors governing this relationship and identification of the control system priorities needs further investigations.
Recent studies have shown smaller size and lower endurance capacity in both flexor and extensor muscles in patients with CNP compared to asymptomatic participants.15, 17, 21 Pain inhibition behaviour is attributed to the smaller size in deep muscles of CNP patients in many studies.45 The superficial muscles, in contrast, have been proposed to become overactive to compensate for the lost cervical stability.46 However, there are inconsistent findings on the alteration of the superficial muscles size in CNP patients. The superficial neck muscles have been inconsistently reported to be smaller,47 larger48 and not different17, 21 between CNP and asymptomatic groups in different studies. It thus seems that the superficial muscles size is not as sensitive to CNP as the alterations of the electrical activity of these muscles.46, 49 Lower endurance capacity in the presence of CNP is attributed to poor function of the deep muscles to keep the cervical spine in an optimal posture while a vicious cycle of pain–weakness is established.50 The lack of association found in the present study between the endurance capacity and muscles size in the CNP group is an important finding that merits consideration in clinical practice. In the CNP patients, the flexor endurance was correlated with neither deep nor superficial flexor muscles size. Meanwhile there was an unexpected association between the global extensor endurance and local muscles size and between the local extensor endurance and global muscles size in these patients. These associations seem contrary to what is expected as the role of these muscles groups.38 It should be noted that the validity of the clinical cervical extensor tests is a concern being addressed in our previous study,17 having extra intervening factors which cannot be identified within the current study.
The findings of our study are indicative of a differential involvement of the flexor and extensor muscles in the presence of CNP. While the flexor muscles endurance lost their correlation with the size of these muscles (such as that found in asymptomatic participants) in CNP patients, this relationship was still evident within the extensor group but not the same way as in the control group. Loss of the relationship between muscular size and endurance in the flexor group and alteration of this relationship in the extensor cervical muscles warrants further investigation into the relative involvement and differential consequences of these alterations. The clinical implications of these findings might be an emphasis on the need to identify involved muscle groups before prescription of exercise therapies since the local and superficial and the flexor and extensor muscle groups were found not to be uniformly affected by CNP. The other clinical point is lack of considerable association between muscles size, endurance and head posture with the clinical CNP characteristics. The results suggest that emphasis should be put on activating the cervical muscles rather than enhancing their force generating capacity by having larger muscles.
Limitations
Muscle state was evaluated by measuring its size in this investigation. Although the CSA and thickness of the muscles have been shown as correlated with their performance,20 they might not fully describe the activation of the muscles. Comparing the results of this study with those investigating muscular activation patterns such as those measuring the electromyographic activity of the muscles might give further insights. Head posture might be altered during sustained postures and affected by the cognitive context of the concurrent task. While we made the assessments at the initial stage of a simple standing task, investigation of the head posture after maintaining a prolonged posture or while performing a cognitively loading concurrent task might further elucidate the motor control adaptations in the presence of CNP from a functional perspective.
Conclusion
The findings of the current study revealed that FHP is neither different between CNP and asymptomatic participants nor correlated with either muscles size or endurance and clinical characteristics of these patients. While muscle size and endurance were correlated in the control group participants, their relationship was interrupted in the CNP patients. It seems that the muscular size–endurance relationship becomes more complex in the presence of CNP. The nature of the alterations in this relationship was not the same for the flexor and extensor groups of cervical muscles. It could thus be postulated that deep vs. superficial and flexor vs. extensor groups of muscles may not be uniformly and comparatively affected in the presence of CNP. This finding has important implications for the assessment and rehabilitation of these patients.
Conflicts of interest
The authors report no conflicts of interest.
Acknowledgement
The authors express their appreciation for the support received from the Rofeideh Rehabilitation Hospital Clinical Research Development Center.
References
- 1.Yip C.H.T., Chiu T.T.W., Poon A.T.K. The relationship between head posture and severity and disability of patients with neck pain. Man Ther. 2008;13(2):148–154. doi: 10.1016/j.math.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 2.Chiu T., Ku W., Lee M. A study on the prevalence of and risk factors for neck pain among university academic staff in Hong Kong. J Occup Rehabil. 2002;12(2):77–91. doi: 10.1023/a:1015008513575. [DOI] [PubMed] [Google Scholar]
- 3.Peterson-Kendall F., Kendall-McCreary E., Geise-Provance P., McIntyre-Rodgers M., Romani W. Lippincott Williams & Wilkins; Baltimore: 2005. Muscles testing and function with posture and pain. [Google Scholar]
- 4.Silva A.G., Punt T.D., Sharples P., Vilas-Boas J.P., Johnson M.I. Head posture and neck pain of chronic nontraumatic origin: a comparison between patients and pain-free persons. Arch Phys Med Rehabil. 2009;90(4):669–674. doi: 10.1016/j.apmr.2008.10.018. [DOI] [PubMed] [Google Scholar]
- 5.Lindfors P., Von Thiele U., Lundberg U. Work characteristics and upper extremity disorders in female dental health workers. J Occup Health. 2006;48(3):192–197. doi: 10.1539/joh.48.192. [DOI] [PubMed] [Google Scholar]
- 6.Kumar S., Narayan Y., Amell T., Ferrari R. Electromyography of superficial cervical muscles with exertion in the sagittal, coronal and oblique planes. Eur Spine J. 2002;11(1):27–37. doi: 10.1007/s005860100318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.American Thoracic Society/European Respiratory Society ATS/ERS statement on respiratory muscle testing. Am J Respir Crit Care Med. 2002;166(4):518–624. doi: 10.1164/rccm.166.4.518. [DOI] [PubMed] [Google Scholar]
- 8.Chen X., O’Leary S., Johnston V. Modifiable individual and work-related factors associated with neck pain in 740 office workers: a cross-sectional study. Braz J Phys Ther. 2018 doi: 10.1016/j.bjpt.2018.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee M.-Y., Lee H.-Y., Yong M.-S. Characteristics of cervical position sense in subjects with forward head posture. J Phys Ther Sci. 2014;26(11):1741–1743. doi: 10.1589/jpts.26.1741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Falla D., Farina D. Neuromuscular adaptation in experimental and clinical neck pain. J Electromyogr Kines. 2008;18(2):255–261. doi: 10.1016/j.jelekin.2006.11.001. [DOI] [PubMed] [Google Scholar]
- 11.Kahlaee A.H., Ghamkhar L., Arab A.M. The association between neck pain and pulmonary function: a systematic review. Am J Phys Med Rehabil. 2017;96(3):203–210. doi: 10.1097/PHM.0000000000000608. [DOI] [PubMed] [Google Scholar]
- 12.Genebra C.V.D.S., Maciel N.M., Bento T.P.F., Simeão S.F.A.P., De Vitta A. Prevalence and factors associated with neck pain: a population-based study. Braz J Phys Ther. 2017;21(4):274–280. doi: 10.1016/j.bjpt.2017.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Janda V. Churchill Livingstone; New York: 1994. Muscles and motor control in cervicogenic disorders: assessment and management physical therapy of the cervical and thoracic spine; pp. 195–216. [Google Scholar]
- 14.Jull G., Falla D., Treleaven J., Hodges P., Vicenzino B. Retraining cervical joint position sense: the effect of two exercise regimes. J Orthop Res. 2007;25(3):404–412. doi: 10.1002/jor.20220. [DOI] [PubMed] [Google Scholar]
- 15.Oliveira A.C., Silva A.G. Neck muscle endurance and head posture: a comparison between adolescents with and without neck pain. Man Ther. 2016;22:62–67. doi: 10.1016/j.math.2015.10.002. [DOI] [PubMed] [Google Scholar]
- 16.Falla D., Jull G., Russell T., Vicenzino B., Hodges P. Effect of neck exercise on sitting posture in patients with chronic neck pain. Phys Ther. 2007;87(4):408–417. doi: 10.2522/ptj.20060009. [DOI] [PubMed] [Google Scholar]
- 17.Kahlaee A.H., Rezasoltani A., Ghamkhar L. Is the clinical cervical extensor endurance test capable of differentiating the local global muscles? Spine J. 2017;17:913–921. doi: 10.1016/j.spinee.2017.01.014. [DOI] [PubMed] [Google Scholar]
- 18.O’Leary S., Falla D., Elliott J.M., Jull G. Muscle dysfunction in cervical spine pain: implications for assessment and management. J Ortho Sport Phys. 2009;39(5):324–333. doi: 10.2519/jospt.2009.2872. [DOI] [PubMed] [Google Scholar]
- 19.Falla D., Jull G., Edwards S., Koh K., Rainoldi A. Neuromuscular efficiency of the sternocleidomastoid and anterior scalene muscles in patients with chronic neck pain. Disabil Rehabil. 2004;26(12):712–717. doi: 10.1080/09638280410001704287. [DOI] [PubMed] [Google Scholar]
- 20.Stokes M., Hides J., Nassiri D.K. Musculoskeletal ultrasound imaging: diagnostic and treatment aid in rehabilitation. Phys Ther Rev. 1997;2(2):73–92. [Google Scholar]
- 21.Ghamkhar L., Kahlaee A. Are ultrasonographic measures of cervical flexor muscles correlated with flexion endurance in chronic neck pain and asymptomatic participants? Am J Phys Med Rehabil. 2017;96(12):874–880. doi: 10.1097/PHM.0000000000000778. [DOI] [PubMed] [Google Scholar]
- 22.Amiri Arimi S., Ghamkhar L., Kahlaee A.H. The relevance of proprioception to chronic neck pain: a correlational analysis of flexor muscle size and endurance, clinical neck pain characteristics and proprioception. Pain Med. 2018 doi: 10.1093/pm/pnx331. [DOI] [PubMed] [Google Scholar]
- 23.Ghamkhar L., Kahlaee A.H., Nourbakhsh M.R., Ahmadi A., Arab A.M. Relationship between proprioception and endurance functionality of the cervical flexor muscles in chronic neck pain and asymptomatic participants. J Manipulative Physiol Ther. 2018;12(2):129–136. doi: 10.1016/j.jmpt.2017.08.006. [DOI] [PubMed] [Google Scholar]
- 24.Parker R.S., Lewis G.N., Rice D.A., McNair P.J. Is motor cortical excitability altered in people with chronic pain? A systematic review and meta-analysis. Brain Stimul. 2016;9(4):488–500. doi: 10.1016/j.brs.2016.03.020. [DOI] [PubMed] [Google Scholar]
- 25.Misailidou V., Malliou P., Beneka A., Karagiannidis A., Godolias G. Assessment of patients with neck pain: a review of definitions, selection criteria, and measurement tools. J Chiropr Med. 2010;9(2):49–59. doi: 10.1016/j.jcm.2010.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.De Hertogh W.J., Vaes P.H., Vijverman V., De Cordt A., Duquet W. The clinical examination of neck pain patients: the validity of a group of tests. Man Ther. 2007;12(1):50–55. doi: 10.1016/j.math.2006.02.007. [DOI] [PubMed] [Google Scholar]
- 27.Mousavi S.J., Parnianpour M., Montazeri A. Translation and validation study of the Iranian versions of the neck disability index and the Neck Pain and Disability Scale. Spine. 2007;32(26):E825–E831. doi: 10.1097/BRS.0b013e31815ce6dd. [DOI] [PubMed] [Google Scholar]
- 28.Fortin C., Ehrmann Feldman D., Cheriet F., Labelle H. Clinical methods for quantifying body segment posture: a literature review. Disabil Rehabil. 2011;33(5):367–383. doi: 10.3109/09638288.2010.492066. [DOI] [PubMed] [Google Scholar]
- 29.Silva A.G., Punt T.D., Sharples P., Vilas-Boas J.P., Johnson M.I. Head posture assessment for patients with neck pain: is it useful. Int J Ther Rehabil. 2009;16(1):43–53. [Google Scholar]
- 30.Quek J., Pua Y.-H., Clark R.A., Bryant A.L. Effects of thoracic kyphosis and forward head posture on cervical range of motion in older adults. Manual Ther. 2013;18(1):65–71. doi: 10.1016/j.math.2012.07.005. [DOI] [PubMed] [Google Scholar]
- 31.Salahzadeh Z., Maroufi N., Ahmadi A. Assessment of forward head posture in females: observational and photogrammetry methods. J Back Musculoskelet Rehabil. 2014;27(2):131–139. doi: 10.3233/BMR-130426. [DOI] [PubMed] [Google Scholar]
- 32.Ahmadi A., Maroufi N., Sarrafzadeh J. Evaluation of forward head posture in sitting and standing positions. Eur Spine J. 2016;25(11):3577–3582. doi: 10.1007/s00586-015-4254-x. [DOI] [PubMed] [Google Scholar]
- 33.Raine S., Twomey L.T. Head and shoulder posture variations in 160 asymptomatic women and men. Arch Phys Med Rehabil. 1997;78(11):1215–1223. doi: 10.1016/s0003-9993(97)90335-x. [DOI] [PubMed] [Google Scholar]
- 34.van Niekerk S.-M., Louw Q., Vaughan C., Grimmer-Somers K., Schreve K. Photographic measurement of upper-body sitting posture of high school students: a reliability and validity study. BMC Musculoskelet Disord. 2008;9(1):113. doi: 10.1186/1471-2474-9-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cleland J.A., Childs J.D., Fritz J.M., Whitman J.M. Interrater reliability of the history and physical examination in patients with mechanical neck pain. Arch Phys Med Rehabil. 2006;87(10):1388–1395. doi: 10.1016/j.apmr.2006.06.011. [DOI] [PubMed] [Google Scholar]
- 36.Edmondston S.J., Wallumrød M.E., MacLéid F., Kvamme L.S., Joebges S., Brabham G.C. Reliability of isometric muscle endurance tests in subjects with postural neck pain. J Manip Physiol Ther. 2008;31(5):348–354. doi: 10.1016/j.jmpt.2008.04.010. [DOI] [PubMed] [Google Scholar]
- 37.Lee H., Nicholson L.L., Adams R.D. Neck muscle endurance, self-report, and range of motion data from subjects with treated and untreated neck pain. J Manipulative Physiol Ther. 2005;28(1):25–32. doi: 10.1016/j.jmpt.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 38.Sebastian D., Chovvath R., Malladi R. Cervical extensor endurance test: a reliability study. J Bodyw Mov Ther. 2015;19(2):213–216. doi: 10.1016/j.jbmt.2014.04.014. [DOI] [PubMed] [Google Scholar]
- 39.Chiu T.T., Lam T.-H., Hedley A.J. Correlation among physical impairments, pain, disability, and patient satisfaction in patients with chronic neck pain. Arch Phys Med Rehabil. 2005;86(3):534–540. doi: 10.1016/j.apmr.2004.02.030. [DOI] [PubMed] [Google Scholar]
- 40.Domholdt E. WB Saunders; Philadelphia, PA: 2005. Rehabilitation research: principles and applications. [Google Scholar]
- 41.Silva A.G., Sharples P., Johnson M.I. Studies comparing surrogate measures for head posture in individuals with and without neck pain. Phys Ther Rev. 2010;15(1):12–22. [Google Scholar]
- 42.Bokaee F., Rezasoltani A., Manshadi F.D., Naimi S.S., Baghban A.A., Azimi H. Comparison of cervical muscle thickness between asymptomatic women with and without forward head posture. Braz J Phys Ther. 2017;21(3):206–211. doi: 10.1016/j.bjpt.2017.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Szeto G.P., Straker L., Raine S. A field comparison of neck and shoulder postures in symptomatic and asymptomatic office workers. Appl Ergon. 2002;33(1):75–84. doi: 10.1016/s0003-6870(01)00043-6. [DOI] [PubMed] [Google Scholar]
- 44.Edmondston S., Björnsdóttir G., Pálsson T., Solgård H., Ussing K., Allison G. Endurance and fatigue characteristics of the neck flexor and extensor muscles during isometric tests in patients with postural neck pain. Man Ther. 2011;16(4):332–338. doi: 10.1016/j.math.2010.12.005. [DOI] [PubMed] [Google Scholar]
- 45.De Pauw R., Coppieters I., Kregel J., De Meulemeester K., Danneels L., Cagnie B. Does muscle morphology change in chronic neck pain patients? A systematic review. Man Ther. 2016;22:42–49. doi: 10.1016/j.math.2015.11.006. [DOI] [PubMed] [Google Scholar]
- 46.Schomacher J., Falla D. Function and structure of the deep cervical extensor muscles in patients with neck pain. Man Ther. 2013;18(5):360–366. doi: 10.1016/j.math.2013.05.009. [DOI] [PubMed] [Google Scholar]
- 47.Rezasoltani A., Ali-Reza A., Khosro K.-K., Abbass R. Preliminary study of neck muscle size and strength measurements in females with chronic non-specific neck pain and healthy control subjects. Man Ther. 2010;15(4):400–403. doi: 10.1016/j.math.2010.02.010. [DOI] [PubMed] [Google Scholar]
- 48.Oksanen A., Erkintalo M., Metsähonkala L. Neck muscles cross-sectional area in adolescents with and without headache—MRI study. Eur J Pain. 2008;12(7):952–959. doi: 10.1016/j.ejpain.2008.01.006. [DOI] [PubMed] [Google Scholar]
- 49.Falla D., Bilenkij G., Jull G. Patients with chronic neck pain demonstrate altered patterns of muscle activation during performance of a functional upper limb task. Spine. 2004;29(13):1436–1440. doi: 10.1097/01.brs.0000128759.02487.bf. [DOI] [PubMed] [Google Scholar]
- 50.Mayoux-Benhamou M., Revel M., Vallee C., Roudier R., Barbet J., Bargy F. Longus colli has a postural function on cervical curvature. Surg Radiol Anat. 1994;16(4):367–371. doi: 10.1007/BF01627655. [DOI] [PubMed] [Google Scholar]