Highlights
-
•
Crepitus is not associated with higher odds of having total knee replacement.
-
•
Crepitus is associated with decreased quadriceps strength in patients with KOA.
-
•
Crepitus does not affect physical function and quality of life of patients with KOA.
Keywords: Knee osteoarthritis, Quality of life, Recovery of function, Knee
Abstract
Objective(s)
To investigate whether the presence of knee crepitus is associated with the occurrence of total knee replacement (TKR), quality of life and deficits in physical function at long-term.
Methods
Setting – This observational study uses longitudinal data (up to 4-year follow-up) from the Osteoarthritis Initiative (OAI). Participants – 4566 participants. Main Outcome Measure(s) – Logistic regression models were used to test if baseline knee crepitus is associated with the occurrence of TKR. Linear mixed models with adjustment for confounding variables (age, gender, BMI and Kellgren–Lawrence grade) were used to test the association between baseline knee crepitus and longitudinal changes in the pain, self-reported physical function, quality of life and performance-based function.
Results
The presence of knee crepitus at baseline does not predict the occurrence of TKR at 36 months (p = 0.58 and 0.67 for right and left knees, respectively). The crepitus group presented a slightly knee extension strength decline from baseline to 48 months (p = 0.03 for the right and 0.01 for the left knee; between group difference = 2% for both right [95%CI = −0.12; −0.01] and left knees [95%CI = −0.13; −0.02]).
Conclusion
The presence of knee crepitus is not associated with the occurrence of TKR in the following three years. Knee crepitus is associated with slightly declines in knee extension strength, but this does not seem to affect physical function and quality of life at long-term.
Introduction
Osteoarthritis (OA) is defined according to the Osteoarthritis Research Society International (OARSI) as a disorder involving joints characterized by cell stress and extracellular matrix degradation initiated by micro- and macro-injury that activates maladaptive repair responses including pro-inflammatory pathways of innate immunity.1 It is estimated that in 2020, OA will be the fourth leading cause of disability worldwide.2 Regarding the weight-bearing joints, the knee is most commonly affected by OA with high prevalence in people who are 60 years or older.3
Knee OA is a progressive disease that leads to the disuse of the painful extremity, deficits in knee strength,4, 5 functional disability4, 6 and low quality of life.7 Such poor clinical presentation may contribute to the high occurrence of total knee replacements (TKR) in individuals with knee OA.8 Nearly 500,000 TKRs, due to knee OA, were performed in the United States in 2011, which is estimated to increase to 3.5 million by 2030.9 High knee pain, poor physical function and age are clinical characteristics associated with worse post TKR outcomes in individuals with knee OA.8 However, there are clinical signs associated with knee OA, yet to be investigated prospectively, that could predict the occurrence of TKR. Knowing clinical predictors of TKR could potentially help clinicians and researchers to develop strategies and direct resources aiming to prevent TKR.
Crepitus is an objective and easy to perform clinical test defined as an audible grinding noise and/or palpable vibrations during joint movement.10, 11 The presence of knee crepitus is possibly the first symptom of patellofemoral OA12 and is associated with magnetic resonance imaging features of patellofemoral OA.13 Moreover, knee crepitus is one of the 5 clinical criteria that could be considered for diagnosing OA without the need for radiographic examination.14 Despite being associated with the development of knee OA and structural damage, it is unknown if knee crepitus is a clinical predictor of TKR or even if crepitus is associated with low physical function or poor quality of life in the future.
In this context, the primary aim of this study is to investigate longitudinally the association between knee crepitus and the occurrence of TKR. The secondary aim is to investigate if the presence of knee crepitus is longitudinally associated with decreased physical function and quality of life in individuals with knee OA. We hypothesized that the presence of knee crepitus at baseline will be associated with higher levels of pain which may result in decreased physical function and consequently poor quality of life. Therefore, we also hypothesized that knee crepitus would be a predictor of TKR.
Methods
Design
This is a longitudinal observational study reported according to STROBE guideline recommendations.15 This study is a secondary analysis of longitudinal data (up to 4-year follow-up) from the Osteoarthritis Initiative (OAI).
Participants
The OAI is a multicenter study of knee OA since 2004, sponsored by the National Institutes of Health that combines clinical, serologic, and joint imaging data of 4796 individuals between 45 and 79 years of age at five centers (Baltimore, MD; Columbus, OH; Pittsburgh, PA; Pawtucket, RI and San Francisco, CA). This database is available for public access at http://www.oai.ucsf.edu. According to the definition of the OAI database we included participants with knee OA and participants at high risk of developing knee OA. Participants with frequent knee symptoms and symptomatic radiographic knee OA were consider as having knee OA. Participants presenting knee symptoms (pain, aching or stiffness), associated with, at least, one of other risk factors of OA such as age >45 years, overweight, knee injury or surgery and family history were considered as having high risk of developing knee OA (http://www.oai.ucsf.edu). However, the definition of “high risk” of developing knee OA used by OAI is currently accepted as a clinical diagnosis of knee OA without the need of imaging.14 We excluded participants who had a total knee replacement and those with missing data on crepitus and Kellgren–Lawrence (KL) grade in either knee at baseline. All participants provided written informed consent and this study received ethical approval from each OAI clinical site (Memorial Hospital of Rhode Island Institutional Review Board, The Ohio State University's Biomedical Sciences Institutional Review Board, University of Pittsburgh Institutional Review Board, and University of Maryland Baltimore – Institutional Review Board), and the OAI coordinating center (Committee on Human Research at University of California, San Francisco, California, United States of America. Number 10-00532).
Outcome measures
All assessments were conducted using a standardized protocol at all five centers of data collection. Participants underwent a knee examination by a trained clinician under the supervision of physician examiners. The assessment of knee crepitus was performed at baseline, the occurrence of TKR was assessed at 36 months and other outcomes such as self-reported knee pain and physical function, and objective physical function were assessed at baseline and at 24 and 48 months follow-ups.
According to the OAI guidelines, a clinician assessed crepitus by placing the palm of the hand over the patella to detect the presence of a continuous grinding sensation during passive knee flexion-extension movement in the supine position. The test was considered positive for crepitus when a continuous grinding, crackling or crunching sensation during knee extension or flexion was detected. One or two clicks or pops were not considered crepitus, however, it was not necessary for the crepitus to be felt throughout the entire range of motion. The same clinical test has been used in other studies.10, 11
The KL grade is a radiologic grading system for knee OA, which determines the severity of radiographic OA based of the presence and degree of osteophytes, joint-space narrowing (JSN), sclerosis, and deformity affecting the tibiofemoral joint, irrespective of clinical symptoms. KL defines OA in five grades (0 – normal to 4 – severe).16 The OAI used the KL grade only to define tibiofemoral OA, the patellofemoral OA was not evaluated. The occurrence of TKR was evaluated by the OAI radiologists with radiographs at 36 months and coded as “right/left knee, ever have replacement surgery where all or part of joint was replaced”.
Self-reported outcomes
The progression of pain and physical function were assessed by questionnaires and objective physical tests. The Western Ontario and McMaster Universities Osteoarthritis index (WOMAC) was used to assess pain (pain subscale) and physical function (physical function subscale) regarding knee-specific limitations in daily activities such as stair use, sit-to-stand movement, and getting in and out of a bath or bed. The WOMAC is a disease-specific, 3-dimensional and self-rated questionnaire. The five-point Likert version was used, item responses range from ‘none’ to ‘extreme’ and were summed to produce subscales (pain 0–20, functioning 0–68) with higher scores indicating worse health. Knee outcome in Osteoarthritis Survey (KOOS) was used as a complement to the WOMAC, because the KOOS assesses the difficulty of performing higher level physical activities such as squatting, running, jumping, twisting/pivoting on the injured knee, and kneeling (function in sport and recreation and knee related quality of life subscales).
The SF-12, an abbreviated version of the SF-36, is a self-administered, generic health related quality of life instrument used to assess general health status and function. It consists of twelve questions covering eight health domains (physical functioning, social functioning, role-physical, role-emotional, mental health, energy/vitality, pain and general health perception). For the SF-12, higher scores indicate better performance.
Objective physical function
To assess physical function objectively, we used the 20-meter walk test (20 m walk) which is commonly used to measure gait speed and monitor changes in patients’ physical function over time. In this test, the participants were timed as they walk down an unobstructed 20-m corridor at their usual walking speed.
Isometric muscle strength was measured bilaterally (in Newton) using the “Good Strength Chair” (Metitur Oy, Jyvaskyla, Finland). The participants sat on the chair with a knee angle of 60° flexion. There were two warm up trials with 50% effort and three measurement trials for each muscle group. The maximal strength produced during isometric contraction was measured during contraction of the right and left quadriceps and hamstring. All participants were encouraged for about 3 s with 30 s rest between trials.
Data analysis
The relationship between the presence of knee crepitus at baseline and the occurrence of TKR at 36 months was investigated using a logistic regression. Nine variables were inserted in the model (knee crepitus, WOMAC pain, KOOS QOL, WOMAC disability, KL grade, knee extensor isometric strength, age, BMI and gender). A logistic regression (forced entry) was performed for each knee (right and left) with associated odds ratios (OR) and 95% CI. The OR and 95% CI values greater than 1 indicate that as the predictor increases, the odds of the outcome occurring increase. Conversely, values lesser than 1 indicate that as the predictor increases, the odds of the outcome occurring decrease.17 Model calibration was checked using the Hosmer–Lemeshow goodness of fit statistic.17
Linear mixed models were used to evaluate the effect of knee crepitus on progression of physical function limitations. This was statistically tested by the interaction of time and group (based on the presence of crepitus) for WOMAC, KOOS, SF-12, 20-meter walk test and knee flexion and extension strength. Data for WOMAC and isometric muscle strength (flexion and extension) are provided separately for the left and right knee, thus, linear mixed models were used for each knee (right and left) for these variables. We analyzed continuous outcome measures using linear mixed models, including their age, gender, BMI and KL grade as covariates, participants as a random effect, knee crepitus as a fixed factor and outcomes measures assessed at baseline and at follow-up after 24 and 48 months as repeated factor. We analyzed the group*time interaction effect for all variables and when it was significant, we assessed the estimates of fixed effects and associated p-values to identify where the interaction occurred. Bonferroni's post hoc test was performed for multiple pairwise comparisons where appropriate. All analyses were performed using SPSS version 21 (IBM SPSS, Chicago, IL). The α level was set a priori at 0.05.
Results
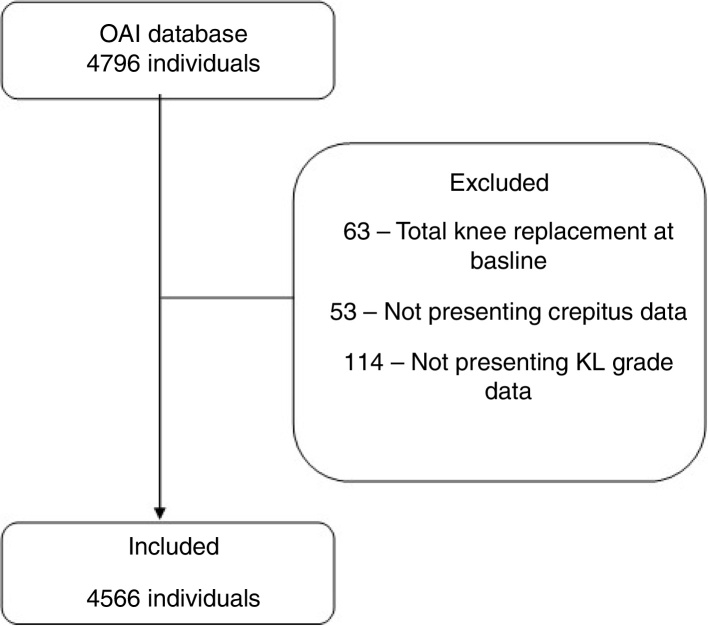
The OAI database was composed of 4796 individuals; however, 230 did not meet our inclusion/exclusion criteria, leaving 4566 for further analysis (Fig. 1). The main anthropometric characteristics are show in Table 1, presented separately for knee (right or left) and crepitus groups.
Figure 1.
Flow diagram.
Table 1.
Anthropometric characteristics of the participants at baseline.
| Right knee |
Left knee |
|||
|---|---|---|---|---|
| No crepitus | Crepitus | No crepitus | Crepitus | |
| Male (n) | 1184 | 726 | 1208 | 702 |
| Female (n) | 1523 | 1133 | 1509 | 1147 |
| Age (year) | 60.70 (9.25) | 61.79 (9.00) | 60.61 (9.22) | 61.94 (9.02) |
| Height (m) | 1.68 (0.10) | 1.69 (0.09) | 1.68 (0.08) | 1.68 (0.09) |
| Weight (kg) | 80.29 (16.33) | 82.77 (16.19) | 80.21 (16.33) | 82.90 (16.18) |
| BMI (kg/m2) | 28.17 (4.75) | 29.28 (4.81) | 28.12 (4.70) | 29.37 (4.86) |
Abbreviations: BMI, body mass index; m, meter; kg, kilogram; age, height, weight and BMI are presented in mean (standard deviation).
Logistic regression outputs indicated that the presence of knee crepitus at baseline is not related with the occurrence of TKR at 36 months (p = 0.58 and 0.67 for right and left knees, respectively). The quality of life (OR = 0.98; 95% CI = 0.96–0.99; p = 0.02 for right knee and OR = 0.98; 95% CI = 0.96–0.99; p = 0.04) and KL grade (OR = 4.43; 95% CI = 2.99–6.57; p < 0.001 for right knee and OR = 3.55; 95% CI = 2.42–5.21; p < 0.001) are associated with the occurrence of TKR at 36 months. The p-value (>0.05) in the Hosmer–Lemeshow test indicated a good fit to the models. We had missing data on TKR for 120 participants at 36 months; therefore, for this analysis data from 4446 participants were used (Table 2).
Table 2.
Amount of participants undergone TKR presented by presence of knee crepitus and KL grade at baseline.
| KL grade | Right knee |
Total | |
|---|---|---|---|
| No crepitus | Crepitus | ||
| 0 | 2/1165 (0.17%) | 2/468 (0.43%) | 4/1633 (0.24%) |
| 1 | 3/526 (0.57%) | 0/288 (0.00%) | 3/814 (0.37%) |
| 2 | 7/619 (1.13%) | 6/618 (0.97%) | 13/1237 (1.05%) |
| 3 | 6/266 (2.26%) | 12/338 (3.55%) | 18/604 (2.98%) |
| 4 | 5/57 (8.77%) | 21/101 (20.79%) | 26/158 (16.46%) |
| Total | 23/2633 (0.87%) | 41/1813 (2.26%) | 64/4446 (1.44%) |
| Left knee | |||
| 0 | 2/1245 (0.16%) | 2/482 (0.41%) | 4/1727 (0.23%) |
| 1 | 1/507 (0.20%) | 2/290 (0.69%) | 3/797 (0.38%) |
| 2 | 6/572 (1.05%) | 9/574 (1.57%) | 15/1146 (1.31%) |
| 3 | 10/268 (3.73%) | 14/358 (3.91%) | 24/626 (3.83%) |
| 4 | 5/44 (11.36%) | 21/106 (19.81%) | 26/150 (17.33%) |
| Total | 24/2636 (0.91%) | 48/1810 (2.65%) | 72/4446 (1.62%) |
Abbreviations: KL grade, Kellgren–Lawrence grade; TRK, total knee replacement. The values are presented by number of participants undergone TKR/total of participants in each group (percentage of the participants undergone TKR in each group).
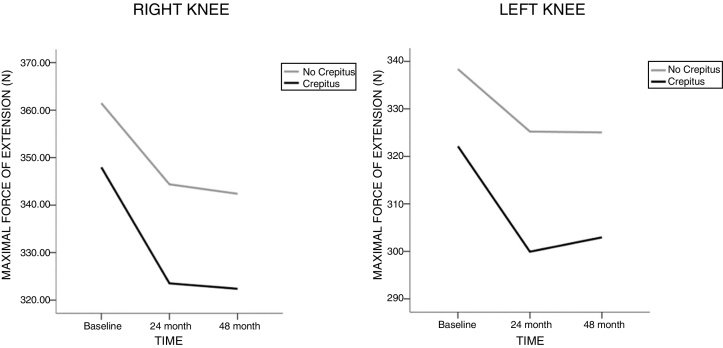
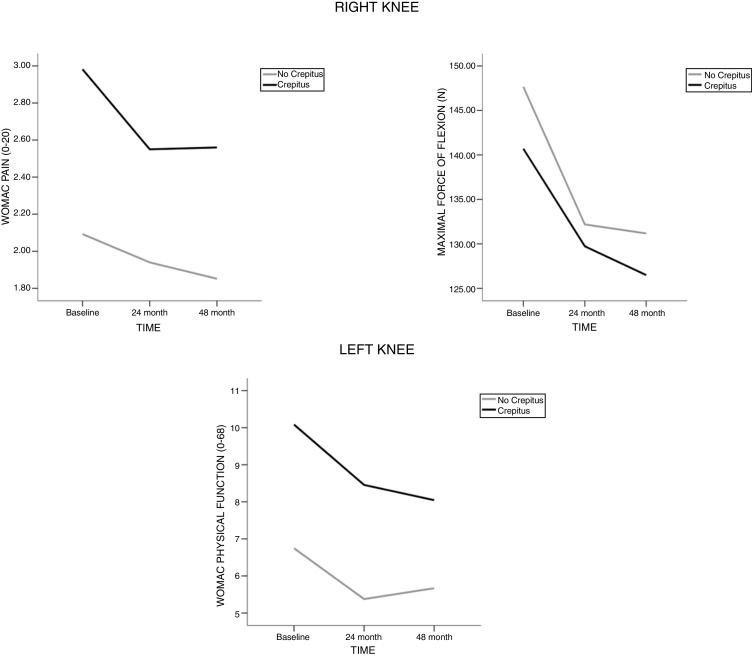
There were no Time*Group interaction effects for walking speed, quality of life and self-reported function (KOOS FSR). There were Time*Group interaction effects for knee extension strength in the right (F(2;3700.723) = 5.085; p = 0.006) and left knee (F(2;3719.161) = 5.584; p = 0.004) with the crepitus group experiencing a more rapid strength decline from baseline to 48 months (p = 0.03 for the right and 0.01 for the left knee; between group difference = 2% for both right [95%CI = −0.12; −0.01] and left knees [95%CI = −0.13; −0.02]) (Fig. 2). Interaction effects were also identified for right knee WOMAC pain (F(2;4214.777) = 3.807; p = 0.02), and maximal knee flexor strength (F(2;3754.612) = 3.222; p = 0.04) but the post hoc tests indicated no statistical difference (Fig. 3, Table 3). A significant interaction was identified for left knee WOMAC physical function (F(2;4231.125) = 3.550; p = 0.03) with both groups experiencing improvements from baseline to 48 months, however, the improvements for both groups were trivial (less than 2 points in a 0–68 point scale).
Figure 2.
Mean values over time for maximal force of extension in the right and left knees.
Figure 3.
Mean values over time for variables whose presented overall interaction Time*Groups in the right and left knees.
Table 3.
Interactions and mean (standard deviation) values of the variables with significant interaction.
| Variable | Group | Baseline mean (SD) | 24 month mean (SD) | 48 month mean (SD) | Time*Group interaction p-values |
Post hoc tests |
|---|---|---|---|---|---|---|
| Right knee WOMAC pain |
No crepitus | 2.09 (0.06) | 1.96 (0.06) | 1.87 (0.06) | 0.02* | No significant post hoc effect |
| Crepitus | 2.98 (0.07) | 2.60 (0.07) | 2.62 (0.07) | |||
| Right knee Maximal strength of extension |
No crepitus | 357.91 (2.61) | 343.49 (2.50) | 337.09 (2.52) | 0.006* | Greater strength decline in the crepitus group from baseline to 48 months (p = 0.03) |
| Crepitus | 346.27 (3.15) | 322.28 (3.04) | 318.36 (3.05) | |||
| Right knee Maximal strength of flexion |
No Crepitus | 145.93 (1.39) | 131.49 (1.27) | 128.92 (1.26) | 0.04* | No significant post hoc effect |
| Crepitus | 139.51 (1.68) | 129.35 (1.55) | 124.46 (1.52) | |||
| Left knee WOMAC physical function |
No crepitus | 6.74 (0.21) | 5.52 (0.20) | 5.68 (0.20) | 0.03* | Greater improvement in the crepitus group from baseline to 48 months (p = 0.01) |
| Crepitus | 10.11 (0.26) | 8.52 (0.24) | 8.18 (0.25) | |||
| Left knee Maximal strength of extension |
No Crepitus | 335.11 (2.52) | 324.25 (2.42) | 320.73 (2.43) | 0.004* | Greater strength decline in the crepitus group from baseline to 48 months (p = 0.01) |
| Crepitus | 319.88 (3.06) | 299.33 (2.95) | 297.57 (2.94) |
Abbreviations: WOMAC pain range is from 0 to 20 (more details are presented in the methods section); Maximal strength of extension and flexion were measured in Newton (N); WOMAC physical function range from 0 to 68.
p < 0.05.
Discussion
The presence of knee crepitus is not associated with the occurrence of TKR in the following 36 months. However, lower quality of life and higher KL grade are associated with the occurrence of TKR in the following 36 months in individuals with knee OA. Individuals with knee crepitus presented slightly higher declines in knee extension strength (2%) than individuals without knee crepitus, but this does not seem to affect physical function and quality of life at long-term (4 years).
Individuals with higher scores in KL grade and poorer quality of life are more likely to undergone TKR after 36 months. The radiographic severity is one of the key factors considered by clinicians in selecting patients for TKR,8 which may explain this finding. However, the radiographic severity is not associated with improvement in knee pain, physical function nor level of patient satisfaction after TKR.8 Surgeons should pay more attention to the clinical presentation of patients with knee OA such as higher levels of knee pain, lower physical function and patient age before recommending surgical procedures instead of rely their decision-making solely on radiographical findings.8
Our findings indicate that knee extensor strength declined faster in individuals with knee crepitus compared to individuals without knee crepitus within the first 4 years. Despite the statistical difference between individuals with and without knee crepitus, this difference may not be clinically relevant. Knee extensor strength deficits by 22–30% are commonly observed in patients with knee OA compared to pain-free populations,18, 19 which is much higher than the 2% difference found between crepitus versus no crepitus groups.20, 21 More specifically, in 4 years, individuals with knee crepitus reduced their knee extensor strength in 7% whereas individuals without knee crepitus reduced 5%. Ruhdorfer et al.22 highlighted the importance of knee extensor strength to individuals with knee OA by identifying that deficits higher than 4% in knee extensor strength are associated with a clinically important difference in WOMAC functional disability. However, knee crepitus seems not be clinically important to knee extensor strength as the between groups difference found in our study was only 2%. Additionally, the presence of knee crepitus had no effect on knee flexor strength or in objective function. In other words, even with slightly knee extensor strength deficits, physical function was stable over time, regardless the presence of knee crepitus.
Knee crepitus is a common sign of young10, 11 and elderly individuals with knee pain as well as in asymptomatic individuals.23 In most cases, the noise around the knee is physiological and is not associated with knee pain and physical function, as evidenced by our findings in a OA population and by a recent study with women with patellofemoral pain.10 Knee crepitus is a poorly understood symptom that creates negative emotions and leads to altered behavior in attempts to avoid the noise.24 Therefore, providing education to patients about the non-association of crepitus with poor clinical outcomes seems to be important.24
Limitations
Some limitations of this research should be acknowledged: (1) Knee strength was determined under isometric conditions, and not isokinetically. Isometric strength may be less related to individual's daily-basis functional tasks25; (2) The OAI participants could have undergone conservative treatments prior to or during the follow-up visits and we do not know what kind of treatment each one chose or how it influenced the results of TKR at 36 months; (3) We could not identify if individuals with knee crepitus were more likely to visit a surgeon or a GP compared to individuals with knee OA without crepitus. This information could indicate a threatening behavior by individuals with knee crepitus.
Conclusion
Knee crepitus is not associated with the occurrence of TKR in the following 36 months in individuals with knee OA. Individuals with knee crepitus presented slightly higher declines with small or trivial effect size in knee extensor strength compared to individuals without crepitus. Additionally, knee crepitus does not seem to affect physical function or quality of life at long-term.
Funding source
The authors would like to acknowledge the Fundação de Amparo a Pesquisa do Estado de São Paulo (scholarships process numbers: 2015/10631-3 and 2015/11534-1). The financial sponsor played no role in the design, execution, analysis and interpretation of data, or writing of the study.
Conflicts of interest
The authors declare no conflicts of interest.
References
- 1.Kraus V.B., Blanco F.J., Englund M., Karsdal M.A., Lohmander L.S. Call for standardized definitions of osteoarthritis and risk stratification for clinical trials and clinical use. Osteoarthr Cartil. 2015;23(8):1233–1241. doi: 10.1016/j.joca.2015.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Woolf A.D., Pfleger B. Burden of major musculoskeletal conditions. Bull World Health Organ. 2003;81(9):646–656. doi:S0042-96862003000900007 [pii] [PMC free article] [PubMed] [Google Scholar]
- 3.Pereira D., Peleteiro B., Araújo J., Branco J., Santos R.a., Ramos E. The effect of osteoarthritis definition on prevalence and incidence estimates: a systematic review. Osteoarthr Cartil. 2011;19(11):1270–1285. doi: 10.1016/j.joca.2011.08.009. [DOI] [PubMed] [Google Scholar]
- 4.Ruhdorfer A.S., Dannhauer T., Wirth W. Thigh muscle cross-sectional areas and strength in knees with early vs knees without radiographic knee osteoarthritis: a between-knee, within-person comparison. Osteoarthr Cartil. 2014;22(10):1634–1638. doi: 10.1016/j.joca.2014.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Francis P., McCormack W., Toomey C., Lyons M., Jakeman P. Muscle strength can better differentiate between gradations of functional performance than muscle quality in healthy 50–70 y women. Braz J Phys Ther. 2017;21(6):457–464. doi: 10.1016/j.bjpt.2017.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eckstein F., Hitzl W., Duryea J., Kent Kwoh C., Wirth W. Baseline and longitudinal change in isometric muscle strength prior to radiographic progression in osteoarthritic and pre-osteoarthritic knees – data from the Osteoarthritis Initiative. Osteoarthr Cartil. 2013;21(5):682–690. doi: 10.1016/j.joca.2013.02.658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Briani R.V., Ferreira A.S., Pazzinatto M.F., Pappas E., De Oliveira Silva D., Azevedo F.M.de. What interventions can improve quality of life or psychosocial factors of individuals with knee osteoarthritis?. A systematic review with meta-analysis of primary outcomes from randomised controlled trials. Br J Sports Med. 2018;52(16):1031–1038. doi: 10.1136/bjsports-2017-098099. [DOI] [PubMed] [Google Scholar]
- 8.Chang C.B., Yoo J.H., Koh I.J., Kang Y.G., Seong S.C., Kim T.K. Key factors in determining surgical timing of total knee arthroplasty in osteoarthritic patients: age, radiographic severity, and symptomatic severity. J Orthop Traumatol. 2010;11(1):21–27. doi: 10.1007/s10195-010-0086-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kurtz S., Ong K., Lau E., Mowat F., Helpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Jt Surg Am. 2007;89(4):780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 10.De Oliveira Silva D., Pazzinatto M.F., Priore L.B., Del Knee crepitus is prevalent in women with patellofemoral pain, but is not related with function, physical activity and pain. Phys Ther Sport. 2018;33:7–11. doi: 10.1016/j.ptsp.2018.06.002. [DOI] [PubMed] [Google Scholar]
- 11.De Oliveira Silva D., Barton C., Crossley K. Implications of knee crepitus to the overall clinical presentation of women with and without patellofemoral pain. Phys Ther Sport. 2018;33:89–95. doi: 10.1016/j.ptsp.2018.07.007. [DOI] [PubMed] [Google Scholar]
- 12.Schiphof D., Van Middelkoop M., De Klerk B.M. Crepitus is a first indication of patellofemoral osteoarthritis (and not of tibiofemoral osteoarthritis) Osteoarthr Cartil. 2014;22(5):631–638. doi: 10.1016/j.joca.2014.02.008. [DOI] [PubMed] [Google Scholar]
- 13.Crema M.D., Guermazi A., Sayre E.C. The association of magnetic resonance imaging (MRI)-detected structural pathology of the knee with crepitus in a population-based cohort with knee pain: the MoDEKO study. Osteoarthr Cartil. 2011;19(12):1429–1432. doi: 10.1016/j.joca.2011.09.003. [DOI] [PubMed] [Google Scholar]
- 14.Zhang W., Doherty M., Peat G. EULAR evidence-based recommendations for the diagnosis of knee osteoarthritis. Ann Rheum Dis. 2010;69(3):483–489. doi: 10.1136/ard.2009.113100. [DOI] [PubMed] [Google Scholar]
- 15.Von Elm E., Altman D.G., Pocock S.J., Gotzsche P.C., Vandenbroucke J.P. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Br Med J. 2007;335:806–808. doi: 10.1136/bmj.39335.541782.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kellgren J.H., Lawrence J.S. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1956;16(3):494–503. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Field A. 4th ed. London. 2013. Discovering Statistics Using IBM SPSS Statistics. [Google Scholar]
- 18.Judd D.L., Thomas A.C., Dayton M.R., Stevens-Lapsley J.E. Strength and functional deficits in individuals with hip osteoarthritis compared to healthy, older adults. Disabil Rehabil. 2014;36(4):307–312. doi: 10.3109/09638288.2013.790491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Palmieri-Smith R.M., Thomas A.C., Karvonen-Gutierrez C., Sowers M.F. Isometric quadriceps strength in women with mild, moderate, and severe knee osteoarthritis. Am J Phys Med Rehabil. 2012;89(7):541–548. doi: 10.1097/PHM.0b013e3181ddd5c3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dias J.M., Cisneros L., Dias R. Hydrotherapy improves pain and function in older women with knee osteoarthritis: a randomized controlled trial. Brazilian J Phys Ther. 2017;21(6):449–456. doi: 10.1016/j.bjpt.2017.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ruhdorfer A., Wirth W., Hitzl W., Nevitt M., Eckstein F. Thigh muscle strength is associated with knee symptoms but not with radiographic disease stage of osteoarthritis – data from the Osteoarthritis Initiative. Arthritis Care Res (Hoboken) 2014;66(9):1344–1353. doi: 10.1002/acr.22317. [DOI] [PubMed] [Google Scholar]
- 22.Ruhdorfer A., Wirth W., Eckstein F. Relationship between isometric thigh muscle strength and minimum clinically important differences in knee function in osteoarthritis: data from the osteoarthritis initiative. Arthritis Care Res (Hoboken) 2015;67(4):509–518. doi: 10.1002/acr.22488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McCoy G.F., McCrea J.D., Beverland D.E., Kernohan W.G., Mollan R.A.B. Vibration arthrography as a diagnostic aid in diseases of the knee. J Bone Jt Surg. 1987;69(2):288–293. doi: 10.1302/0301-620X.69B2.3818762. [DOI] [PubMed] [Google Scholar]
- 24.Song S.J., Park C.H., Liang H., Kim S.J. Noise around the knee. CiOS Clin Orthop Surg. 2018;10(1):1–8. doi: 10.4055/cios.2018.10.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Briani R.V., Pazzinatto M.F., De Oliveira Silva D., Azevedo F.M. Different pain responses to distinct levels of physical activity in women with patellofemoral pain. Braz J Phys Ther. 2017;21(2):138–143. doi: 10.1016/j.bjpt.2017.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]