Abstract
Objective
The updated guidelines of 2015 for cardiopulmonary resuscitation (CPR) do not recommend the routine use of atropine for cardiopulmonary arrest.
Methods
The study population included out-of-hospital cardiac arrest (OHCA) patients with non-shockable rhythm who were encountered at a Japanese community hospital between October 1, 2012 and April 30, 2017.
Results
At the outcome, the epinephrine with atropine and epinephrine-only groups had a similar survival rate to that at hospital admission (28.7% vs. 26.7%: p=0.723). The odds ratio (OR) for the survival to hospital admission after the administration of atropine with epinephrine was 1.33 (95% CI 1.09-1.62; p<0.01), while that after the administration of epinephrine was 0.64 (95% CI: 0.55-0.74, p<0.01). The ORs for the survival to hospital admission for patients with pulseless electrical activity in the epinephrine-alone group and the atropine with epinephrine group were 0.62 (95% CI 0.49-0.78; p<0.01) and 1.35 (95% CI 0.99-1.83; p=0.06), respectively, and those for such patients with asystole in the epinephrine-alone group and the atropine with epinephrine group were 0.64 (95% CI 0.53-0.76; p<0.01) and 1.39 (95% CI 1.10-1.77; p<0.01), respectively. The OR for the survival to hospital admission after the administration of atropine sulfate (1 mg) was 2.91 (95% CI 1.49-5.67; p<0.01), while that for the survival to hospital admission after the administration of 0, 2 and ≥3 mg atropine sulfate was 0.38 (95% CI 0.29-0.50; p<0.01), 1.54 (95% CI 0.58-4.08; p=0.38) and 0.23 (95% CI 0.09-0.60; p<0.01), respectively.
Conclusion
The addition of atropine (within 2 mg) following epinephrine was a comprehensive independent predictor of the survival to hospital admission for non-shockable (especially asystole) OHCA adults.
Keywords: atropine sulfate, adult out-of-hospital cardiac arrest, non-shockable rhythm, survival to hospital admission
Introduction
Available evidence suggests that the routine use of atropine during cardiopulmonary resuscitation (CPR) is unlikely to have any therapeutic benefit (Class IIb, LOE B) (1, 2), and the SOS-KANTO study in 2011 concluded that the administration of atropine had no long-term neurological benefit in adults with out-of-hospital cardiac arrest (OHCA) due to non-shockable rhythm. In addition, atropine has been shown to not be useful for adults with pulseless electrical activity (PEA) (3). However, the evidence thus far is insufficient to allow comment on critical outcomes, such as the survival to hospital admission and to discharge with a good neurologic outcome with either epinephrine alone or epinephrine with atropine, due to the low number of prospective or randomized controlled studies. Even though the routine use of atropine for cardiopulmonary arrest has not been recommended since the publication of the 2010 American Heart Association (AHA) Guidelines for CPR and Emergency Cardiovascular Care (ECC), the two selected emergency medical physicians in our emergency center have always routinely used atropine following epinephrine during CPR because they believe that the use of atropine facilitates a vagolytic effect that might be consistent with a physiologic approach to treating asystole or bradycardic PEA rhythm. In addition, atropine is inexpensive, safe and easy to administer. The actual changes in atropine use and the critical outcomes in clinical situations after 2010 are thus unclear.
In the present study, we assessed the efficacy of atropine in out-of-hospital non-traumatic cardiac arrest patients with non-shockable rhythm (PEA or asystole) following the guideline revision in 2010.
Materials and Methods
This study was approved by the Research Ethics Board of our hospital, and the requirement for informed consent was waived according to Japanese government guidelines (4).
Study setting and population
This study was conducted at a tertiary-care suburban community hospital with over 3,000 emergency department (ED) visits annually and nearly 350 inpatient beds. This hospital is now the only emergency and cardiovascular care center in Nobeoka City, which is located in the northern region of Miyazaki Prefecture in the southern part of Japan with a population of over 120,000 and an area of 86,800 km2. The emergency medical service (EMS) system in Nobeoka City is located at a fire station with a dispatch center and is managed by municipal governments. EMS providers in Japan are trained in basic life support (BLS) according to the Japanese CPR guidelines (5); they are not permitted to terminate resuscitation in the field. Some emergency medical technicians (EMTs) are qualified to perform advanced airway management as well as intravenous drug administration during CPR.
Subjects
We conducted a retrospective observational study of non-traumatic OHCA patients between October 1, 2012, and April 30, 2017. Patients were excluded if they were younger than 18 years old or achieved sustained return of spontaneous circulation (ROSC) before ED arrival, the initial cardiac rhythm at ED was shockable, the precise drug dose was not available, epinephrine was not given or the patient had a do-not-resuscitate order. BLS and advanced cardiovascular life support (ACLS) were performed in accordance with the ACLS guidelines of 2010 (6). A 1-mg dose of epinephrine every 3-5 minutes was administered intravenously if cardiac arrest persisted. Although the use of atropine was not standardized, the dose of atropine for asystole or PEA arrest was 1 mg intravenously, which could be repeated every 3-5 minutes (maximum total of 3 mg) if asystole or PEA arrest persisted. The use of other resuscitation drugs (e.g. vasopressins, antiarrhythmics and buffers), inclusive of high-dose epinephrine, was not standardized if the initial administration of 1 mg epinephrine failed. Extracorporeal CPR and hypothermia for post-resuscitation care were also not standardized. It was up to the attending physicians to stop the ACLS efforts.
Data
Demographic data and baseline characteristics were obtained from EMS reports and medical records, which included the following data: age, sex, cause of cardiac arrest (cardiogenic or not), witnessed cardiopulmonary arrest (CPA), bystander administration of CPR (BSCPR), public access defibrillation (PAD), prehospital tracheal intubation by EMT, implementation of automated chest compression cardiopulmonary resuscitation (ACC-CPR), time interval from call receipt to ED arrival and initial electrocardiogram rhythm at ED.
Outcomes
The primary outcome was the survival to hospital admission, which means the survival until admission after ROSC. Additional outcomes included the 30-day survival and a favorable neurological outcome at 30 days after cardiac arrest according to the Glasgow-Pittsburgh cerebral-performance category of 1 (good performance) or 2 (moderate disability) on a 5-point scale; the other categories were 3 (severe disability), 4 (a vegetative state) and 5 (death).
Statistical analyses
Continuous variables are expressed as the mean±standard deviation (SD) when normally distributed and as the median with the interquartile range (IQR) when non-normally distributed. Variables were tested for a normal distribution using the Kolmogorov-Smirnov test. Categorical data are presented as absolute numbers and percent frequencies. Student's t-test was used to compare the values of normally distributed continuous variables, and the Mann-Whitney U test was used to compare the values of non-normally distributed continuous variables. Baseline characteristics between the epinephrine-only group and the epinephrine with atropine group were first compared using the chi-squared test or Fisher's exact test for categorical variables and Student's t-test or the Mann-Whitney U test for continuous variables, as appropriate.
Of the earlier reported variables, the age, gender, witnessed CPA, BSCPR, PAD and cardiogenic arrest were candidates for the multivariable model. A multiple logistic-regression analysis was carried out to identify independent predictors of the current study outcomes, including these candidate factors, prehospital tracheal intubation by EMT, ACC-CPR, time interval from call receipt to ED arrival, initial electrocardiogram rhythm at scene and the administration of epinephrine with or without atropine.
We changed the doses of epinephrine and atropine to categorical data for assessing independent predictors. Epinephrine was classified into 3 different categories (1, 2 and ≥3 mg) and atropine sulfate into 4 different categories (0, 1, 2 and ≥3 mg) according to the total administered dose. An interaction analysis was performed between epinephrine and atropine for the survival to hospital admission, and we conducted a binominal logistic regression analysis for the survival to hospital admission using these categorized variables according to the total administered dose of atropine or epinephrine.
The results of the multivariate logistic regression analyses were summarized by estimating the odds ratios (ORs) and the respective 95% confidence intervals (CIs). A 2-tailed p value of <0.05 was considered statistically significant.
All statistical analyses were performed with EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan), which is a graphical user interface for R, ver. 3.3.2 (The R Foundation for Statistical Computing, Vienna, Austria).
Results
During the study period, 453 non-traumatic cardiac arrest patients arrived in our ED. Of these, 86 were excluded for the following reasons: 8 were below 18 years old, 15 achieved prehospital ROSC, 26 demonstrated shockable rhythm at ED, 8 had no available drug data, and 31 were not administered epinephrine during CPR This left 367 patients for the analysis (Fig. 1).
Figure 1.
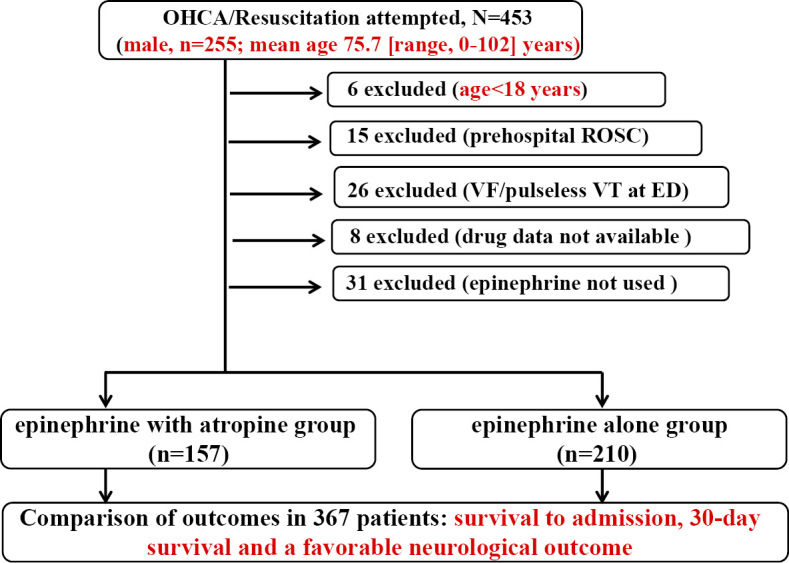
Study profile. Non-traumatic out-of-hospital cardiac arrest patients and study participants in the emergency center of Miyazaki Prefectural Nobeoka Hospital (between October 1, 2012, and April 30, 2017).
Of these, 157 were administered epinephrine with atropine (epinephrine with atropine group), and 210 were administered epinephrine alone (epinephrine-only group). Baseline characteristics and outcomes of these patients are presented in Table 1. At baseline, significant differences were seen between the epinephrine with atropine group and the epinephrine-only group in the proportions of cardiogenic cause [53.5% (n=84) vs. 36.2% (n=76); p=0.001] and the time from call receipt to ED arrival [25 (20-33) min vs. 27 (23-35) min; p=0.0494]. Regarding the patient outcomes, the 2 groups had similar rates of surviving to hospital admission [28.7% (45/157) vs. 26.7% (56/210); p=0.723]. The total number of survivors to admission after ROSC was 101, and we selected 10 variables, including the baseline characteristics, epinephrine and atropine, for the binominal multivariate logistic analysis (>1 variable/10 samples). The rates of availability of PAD, ACCR and medications other than epinephrine and atropine were below 10%, so we excluded these factors from the multivariate analysis.
Table 1.
Baseline Characteristics and Outcomes of Out-of-hospital Cariac Arrest Patients with Non-shockable Rhythm at ED.
| Total (n=367) | Epinephrine with atropine group (n=157) | Epinephrine-only group (n=210) | p | |
|---|---|---|---|---|
| Baseline characteristics | ||||
| Age (years) | 79 (70.5-86.5) | 80 (72-87) | 79 (70-86) | 0.663 |
| Sex (male) | 204 (55.6%) | 89 (56.7%) | 115 (54.8%) | 0.751 |
| Etiology | ||||
| Cardiogenic | 160 (43.6%) | 84 (53.5%) | 76 (36.2%) | 0.001 |
| Witnessed | 170 (46.3%) | 82 (52.2%) | 88 (41.9%) | 0.057 |
| BSCPR | 235 (63.7%) | 100 (63.7%) | 135 (64.3%) | 0.913 |
| PAD | 11 (2.98%) | 5 (3.2%) | 6 (2.9%) | 1 |
| Initial rhythm at ED arrival | ||||
| Pulseless electrical activity(PEA) | 115 (31.2.%) | 49 (31.2%) | 66 (31.4%) | 1 |
| Time from call receipt to ED arrival (min) | 27 (22-33) | 25 (20-33) | 27 (23-35) | 0.0494 |
| Prehospital intubation | 68 (18.4%) | 25 (15.9%) | 43 (20.5%) | 0.281 |
| ACC-CPR | 33 (8.9%) | 5 (4.3%) | 7 (4.7%) | 1 |
| Outcomes | ||||
| Survival to hospital admission | 101 (27.4%) | 45 (28.7%) | 56 (26.7%) | 0.723 |
| 30-day survival | 11 (2.98%) | 6 (3.8%) | 5 (2.4%) | 0.54 |
| Favorable neurologic outcome at 1 month (CPC score 1 or 2) | 1 (0.27%) | 1 (0.6%) | 0 (0%) | 0.48 |
Quantitative values are expressed as the mean±SD or median (IQR). Categorical variables are expressed as the number (percentage).
When comparing the non-ROSC achievement group and the ROSC achievement group, p values of <0.05 were considered significant.
BSCPR: bystander cardiopulmonary resuscitation, PAD: public access defibrillation, ACC-CPR: automated chest compression cardiopulmonary resuscitation, CPC: cerebral performance category, CPR: cardiopulmonary resuscitation, ED: emergency department, ROSC: return of spontaneous circulation, IQR: interquartile range
Table 1-2.
Baseline Characteristics of Out-of-hospital Cariac Arrest Patients with Pulseless Electrical Activity.
| Total (n=115) | Epinephrine with atropine group (n=49) | Epinephrine-only group (n=66) | p | |
|---|---|---|---|---|
| Age (years) | 76.9 (74.6-79.1) | 77.8 (±10.9) | 76.2 (±13.1) | 0.48 |
| Sex (male) | 65 (56.5%) | 26 (53.1%) | 39 (59.1%) | 0.571 |
| Etiology | ||||
| Cardiogenic | 50 (43.5%) | 22 (44.9%) | 28 (42.4%) | 0.85 |
| Witnessed | 89 (77.4%) | 38 (77.6%) | 51 (77.3%) | 1 |
| BSCPR | 61 (53%) | 27 (55.1%) | 34 (51.5%) | 0.711 |
| PAD | 11 (2.98%) | 5 (3.2%) | 6 (2.9%) | 1 |
| Time from call receipt to ED arrival (min) | 28.2 (25.9-30.5) | 26.9 (±13.4) | 29.1 (±11.8) | 0.36 |
| Prehospital intubation | 11 (2.98%) | 4 (8.2%) | 7 (10.6%) | 0.756 |
| ACC-CPR | 6 (5.2%) | 1 (2%) | 5 (7.6%) | 0.238 |
| Survival to hospital admission | 45 (39.1%) | 19 (38.8%) | 26 (39.4%) | 1 |
| 30-day survival | 9 (7.8%) | 5 (10.2%) | 4 (6.1%) | 0.493 |
| Favorable neurologic outcome at 1 month (CPC score 1 or 2) | 1 (0.87%) | 1 (2%) | 0 (0%) | 0.426 |
Quantitative values are expressed as the mean±SD or median (IQR). Categorical variables are expressed as the number (percentage).
When comparing the non-ROSC achievement group and the ROSC achievement group, p values of <0.05 were considered significant.
BSCPR: bystander cardiopulmonary resuscitation, PAD: public access defibrillation, ACC-CPR: automated chest compression cardiopulmonary resuscitation, CPC: cerebral performance category, CPR: cardiopulmonary resuscitation, ED: emergency department, ROSC: return of spontaneous circulation, IQR: interquartile range
Table 1-3.
Baseline Characteristics of Out-of-hospital Cariac Arrest Patients with Asystole.
| Total (n=252) | Epinephrine with atropine group (n=108) | Epinephrine-only group (n=144) | p | |
|---|---|---|---|---|
| Age (years) | 77.0 (75.3-78.7) | 77.1 (±14.0) | 77.0 (±13.6) | 0.95 |
| Sex (male) | 139 (55.2%) | 63 (58.3%) | 76 (52.8%) | 0.443 |
| Etiology | ||||
| Cardiogenic | 110 (43.7%) | 62 (57.4%) | 48 (33.3%) | <0.01 |
| Witnessed | 81 (32.1%) | 44 (40.7%) | 37 (25.7%) | 0.01 |
| BSCPR | 174 (69%) | 73 (67.6%) | 101 (70.1%) | 0.682 |
| PAD | 4 (1.59%) | 2 (1.9%) | 2 (1.4%) | 1 |
| Time from call receipt to ED arrival (min) | 31.2 (29.4-33.0) | 30.1 (±14.0) | 32.1 (±15.0) | 0.29 |
| Prehospital intubation | 57 (22.6%) | 21 (19.4%) | 36 (25%) | 0.362 |
| ACC-CPR | 27 (10.7%) | 8 (7.4%) | 19 (13.2%) | 0.156 |
| Survival to hospital admission | 56 (22.2%) | 26 (24.1%) | 30 (20.8%) | 0.545 |
| 30-day survival | 8 (0.8%) | 1 (0.9%) | 1 (0.7%) | 1 |
| Favorable neurologic outcome at 1 month (CPC score 1 or 2) | 0 | 0 | 0 |
Quantitative values are expressed as the mean±SD or median (IQR). Categorical variables are expressed as the number (percentage).
When comparing the non-ROSC achievement group and the ROSC achievement group, p values of <0.05 were considered significant.
BSCPR: bystander cardiopulmonary resuscitation, PAD: public access defibrillation, ACC-CPR: automated chest compression cardiopulmonary resuscitation, CPC: cerebral performance category, CPR: cardiopulmonary resuscitation, ED: emergency department, ROSC: return of spontaneous circulation, IQR: interquartile range
In the multiple logistic regression analysis (Table 2), the OR after the administration of atropine with epinephrine was 1.33 (95% CI 1.09-1.62; p<0.01) for the survival to hospital admission, while that after the administration of epinephrine was 0.64 (95% CI: 0.55-0.74, p<0.01). A multivariate regression receiver operating characteristic (ROC) curve including the baseline characteristics, epinephrine and atropine for the survival to hospital admission (n=101) revealed the area under the ROC curve to be 0.807 (95% CI: 0.756-0.858) (Fig. 2). The square root of the variance inflation factor indicates how much larger the standard error is than what it would be if that variable were uncorrelated with the other predictor variables in the model. Since the variation inflation factor of each predictor was not inflated (1.03-2.20), there was little multicollinearity among these predictors. Other independent predictors for the survival to hospital admission were the age (OR 0.98; 95% CI 0.96-1.00; p=0.033), witnessed arrest (OR 3.17; 95% CI 1.74-5.78; p<0.01) and time from call receipt to ED arrival (OR 0.98; 95% CI 0.95-1.00; p=0.029).
Table 2.
Multivariate Analysis of Factors Predicting Survival to Hospital Admission.
| Variable | OR (95% CI) | p | Variance inflation factors |
|---|---|---|---|
| Age (years) | 0.98 (0.96-1.00) | 0.033 | 1.18 |
| Sex (male) | 1.08 (0.63-1.87) | 0.78 | 1.06 |
| Etiology | |||
| Cardiogenic | 0.59 (0.34-1.03) | 0.062 | 1.03 |
| Witnessed | 3.17 (1.74-5.78) | <0.01 | 1.26 |
| BSCPR | 1.09 (0.62-1.93) | 0.76 | 1.07 |
| Initial rhythm at ED arrival | |||
| Pulseless electrical activity | 1.46 (0.79-2.71) | 0.23 | 1.27 |
| Time from call receipt to ED arrival (min) | 0.98 (0.95-1.00) | 0.029 | 1.29 |
| Prehospital intubation | 1.17 (0.52-2.63) | 0.7 | 1.4 |
| Atropine sulfate | 1.33 (1.09-1.62) | <0.01 | 2.13 |
| Epinephrine | 0.64 (0.55-0.74) | <0.01 | 2.2 |
OR: odds ratio, CI: confidence interval, BSCPR: bystander cardiopulmonary resuscitation, ED: emergency department
Figure 2.
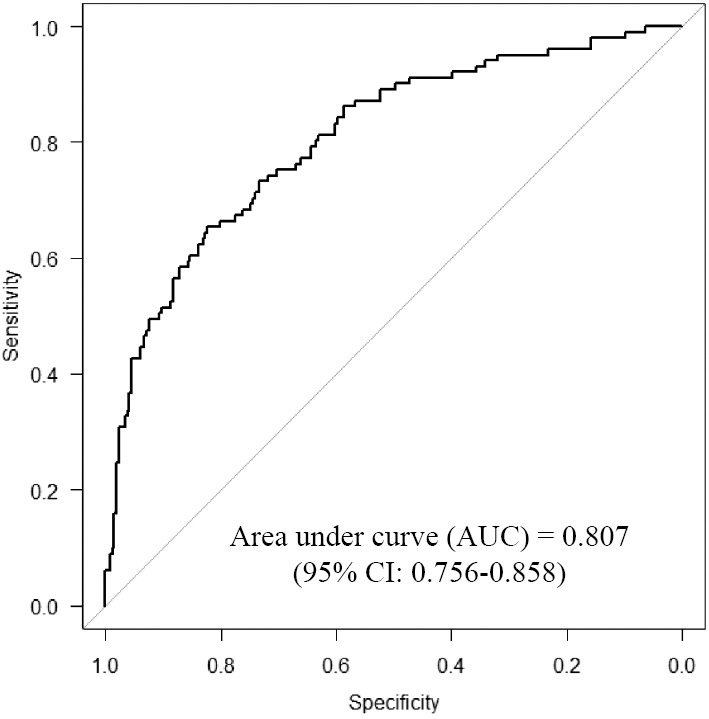
A multivariate regression receiver operating characteristic (ROC) curve including baseline characteristics, epinephrine and atropine for the survival to hospital admission (n=101).
Eleven patients demonstrated a 30-day survival, including 1 with a favorable 30-day neurological outcome. However, the sample size was too small to perform a binominal multivariate logistic regression analysis with this variable.
In the subgroup of patients with PEA (Table 1-2), no significant differences were seen between the epinephrine with atropine group and the epinephrine-only group, including in the rate of the survival to hospital admission [38.8% (19/49) vs. 39.4% (26/66); p=1]. In the subgroup of patients with asystole (Table 1-3), significant differences were seen between the 2 groups in the rate of cardiogenic cause [54.7% (n=62/108) vs. 33.3% (n=48/144); p<0.01] and witnessed arrest [40.7% (n=44/108) vs. 25.7% (n=37/144); p=0.01], while no significant differences were seen in other factors, including the rate of the survival to hospital admission [24.1% (26/108) vs. 20.8% (30/144); p=0.545].
The total number of survivors to admission in each subgroup after ROSC was 45 and 56, respectively, and we selected 4 variables, including the age, gender, epinephrine and atropine, for the binominal multivariate logistic analysis (>1 variable/10 samples). In the multiple logistic regression analysis (Table 2-2) for the subgroup of patients with PEA, the ORs of the epinephrine-alone and atropine with epinephrine groups were 0.62 (95% CI 0.49-0.78; p<0.01) and 1.35 (95% CI 0.99-1.83; p=0.06) for the survival to hospital admission (45 cases), respectively. In the multiple logistic regression analysis (Table 2-3) for the subgroup of patients with asystole, the ORs of the epinephrine-alone and atropine with epinephrine groups were 0.64 (95% CI 0.53-0.76; p<0.01) and 1.39 (95% CI 1.10-1.77; p<0.01) for the survival to hospital admission (56 cases), respectively.
Table 2-2.
Multivariate Analysis of Factors Predicting Survival to Hospital Admission of Out-of-hospital Cariac Arrest Patients with Pulseless Electrical Activity.
| Variable | OR (95% CI) | p | Variance inflation factors |
|---|---|---|---|
| Age (years) | 0.96 (0.93-1.00) | 0.051 | 1.09 |
| Sex (male) | 0.77 (0.32-1.84) | 0.56 | 1.01 |
| Atropine sulfate | 1.35 (0.99-1.83) | 0.059 | 2.08 |
| Epinephrine | 0.62 (0.49-0.78) | <0.01 | 2.16 |
OR: odds ratio, CI: confidence interval, BSCPR: bystander cardiopulmonary resuscitation, ED: emergency department
Table 2-3.
Multivariate Analysis of Factors Predicting Survival to Hospital Admission of Out-of-hospital Cariac Arrest Patients with Asystole.
| Variable | OR (95% CI) | p | Variance inflation factors |
|---|---|---|---|
| Age (years) | 0.99 (0.97-1.01) | 0.42 | 1.07 |
| Sex (male) | 1.20 (0.63-2.32) | 0.58 | 1.05 |
| Atropine sulfate | 1.39 (1.10-1.77) | <0.01 | 2.09 |
| Epinephrine | 0.64 (0.53-0.76) | <0.01 | 2.11 |
OR: odds ratio, CI: confidence interval, BSCPR: bystander cardiopulmonary resuscitation, ED: emergency department
An interaction analysis showed that epinephrine and atropine had no effect modification (OR 0.98; p=0.53) with each other for the survival to hospital admission. We performed a binominal logistic-regression analysis for the survival to hospital admission using the categorized variables according to the total administered dose of atropine or epinephrine (Table 3). The OR for the survival to hospital admission after the administration of 1 mg atropine sulfate was 2.91 (95% CI 1.49-5.67; p<0.01), while those for the survival to hospital admission after the administration of 0, 2 and ≥3 mg atropine sulfate were 0.38 (95% CI 0.29-0.50; p<0.01), 1.54 (95% CI 0.58-4.08; p=0.38) and 0.23 (95% CI 0.09-0.60; p<0.01), respectively. The ORs for the survival to hospital admission after the administration of 1, 2 and ≥3 mg epinephrine were 1.15 (95% CI 0.68-1.95; p=0.59), 0.69 (95% CI 0.33-1.43; p=0.39) and 0.19 (95% CI 0.10-0.34; p<0.01), respectively.
Table 3.
Logistic Regression Analysis for Survival to Hospital Admission according to the Categorized Dose of Atropine and Epinephrine.
| Variable | OR (95% CI) | p |
|---|---|---|
| Atropine sulfate | ||
| Atro-0 mg (atropine sulfate 0 mg: n=244) | 0.38 (0.29-0.50) | <0.01 |
| Atro-1 mg (atropine sulfate 1 mg: n=42) | 2.91 (1.49-5.67) | <0.01 |
| Atro-2 mg (atropine sulfate 2 mg: n=19) | 1.54 (0.58-4.08) | 0.38 |
| Atro≥3 mg (atropine sulfate ≥3 mg: n=62) | 0.23 (0.09-0.60) | <0.01 |
| Epinephrine | ||
| Epi-1 mg (epinephrine 1 mg: n=56) | 1.15 (0.68-1.95) | 0.59 |
| Epi-2 mg (epinephrine 2 mg: n=61) | 0.69 (0.33-1.43) | 0.32 |
| Epi≥3 mg (epinephrine ≥3 mg: n=250) | 0.19 (0.10-0.34) | <0.01 |
OR: odds ratio, CI: confidence interval
Discussion
This was the first single-rural-center retrospective observational study in Japan concerning the administration of atropine during ACLS in adult patients with OHCA due to non-shockable rhythm (asystole or PEA) since the recommendation of the routine use of atropine for CPA was stopped in 2010, a move whose wisdom we questioned at the time.
For decades, no specific drug therapy has been shown to improve the survival to hospital discharge after cardiac arrest, and only a few drugs have been proven to benefit the short-term survival (7). In 1979, Brown et al. (8) noted the possible role of the parasympathetic nervous system in cardiac arrest and reported that atropine was beneficial during cardiac arrest; subsequently, the AHA included atropine as a recommended treatment for asystole. Despite its historic use and widespread acceptance for application during CPR, few studies have demonstrated any real benefit associated with the administration of atropine in cases of out-of-hospital asystole or PEA (7, 9). Furthermore, only a few reports have shown that patients who received atropine demonstrated better ROSC rates at the ED or showed an improved short-term survival without favorable neurological outcomes than those receiving epinephrine alone (3, 10). CPR is an attempt to restore spontaneous circulation. Since CPA victims with a non-shockable rhythm constitute a heterogeneous subgroup that is separate from victims of shockable-rhythm CPA, pharmacological intervention, such as atropine injection during CPR, will likely benefit their short-term survival.
In the present study, in the 367 adults with non-shockable rhythm at ED, although the epinephrine with atropine group had favorable conditions for resuscitation (e.g., a shorter time from call receipt to ED arrival) than the epinephrine-only group, and the resuscitation outcomes for survival to hospital admission, expressed as the short-term survival, did not differ significantly between the two groups (Table 1-1). In contrast, a multiple logistic-regression analysis showed that the administration of atropine was an independent predictor of the survival to hospital admission (Table 2-1). This result suggests that the clinical importance of atropine use is small in this study sample because the logistic regression model demonstrated statistically significant results with a smaller sample size. The administration of atropine with epinephrine may significantly improve the rate of the survival to admission of non-shockable OHCA cases in a larger sample size, concurring with the findings of previous studies (3).
In the subgroup of PEA (115 patients), the epinephrine with atropine group had no favorable conditions for resuscitation compared with the epinephrine-only group, and outcomes were similar between the 2 groups (Table 1-2). A multiple logistic-regression analysis failed to show that the administration of atropine for PEA victims was an independent predictor of the survival to hospital admission (Table 2-2). In the subgroup of asystole (252 patients), the epinephrine with atropine group had favorable conditions for resuscitation (e.g., a higher proportion of witnessed arrest) than the epinephrine-only group, with similar outcomes between the 2 groups (Table 1-3). A multiple logistic-regression analysis showed that the administration of atropine for asystole victims was an independent predictor of the survival to hospital admission (Table 2-3). Although the results of the present study were based on the findings of a statistical analysis using a small sample size, the efficacy of atropine for asystole was found to be in line with that of previous studies (3). A retrospective review of patients with asystole found that 6 of 43 patients (14%) treated with atropine survived to hospital admission compared to 0 of 41 patients (0%) who did not receive atropine (p<0.04) (10). A case series of adults in cardiac arrest documented conversion from asystole to sinus rhythm in 7 of 8 patients within 30 seconds of the administration of the last dose of atropine (1 to 2 mg, intravenous). Five patients (62.5%) lived 12 hours, and 3 patients (37.5%) were discharged from the hospital (8). A prospective controlled non-randomized study of out-of-hospital arrest found that 2 of 11 patients with asystole or pulseless idioventricular rhythms treated with atropine survived to hospital admission compared with 2 of 10 patients who did not receive atropine (9). These previous findings were obtained in a small case series or a non-randomized study of OHCA with a small sample size and suggest that data on patients with OHCA due to asystole are insufficient at present. Our study showed that the administration of atropine during ACLS for adults with asystole was associated with a short-term survival benefit, thus demonstrating that a number of asystole cases due to high parasympathetic tone or reflex vagal stimulation could be included in our study.
In the present study, we failed to demonstrate statistically significant short-term survival benefits of atropine during ACLS for adults with PEA. Although we were unable to determine whether the QRS complexes of PEA was wide or narrow and the heart rate fast or slow, we did conclude that heterogenous wide QRS complexes might account for a majority of cases of PEA, due to their poor response to atropine. Those rhythms often indicate the malfunction of the myocardium or the cardiac conduction system below the bundle of His, where atropine did not exert an effect, such as in cases of massive acute myocardial infarction, severe hyperkalemia, hypothermia, hypoxia, preexisting acidosis and overdose of a number of drugs. PEA is caused by reversible conditions and can be treated if those conditions are identified and corrected (11). Therefore, more clinical studies in patients with PEA who have wide or narrow QRS complexes are needed.
Based on the ORs for the survival to hospital admission according to different doses of atropine or epinephrine, the addition of 1 mg atropine sulfate following 1 mg epinephrine seems to have a beneficial effect on the survival to hospital admission, while epinephrine alone and ≥3 mg of atropine sulfate and/or epinephrine did not. We also showed the optimal dose of epinephrine and atropine as well as their upper-limit dose in the present study. A major challenge in managing non-shockable rhythm OHCA is the immediate recognition and treatment of the underlying causes of OHCA; therefore, instead of increasing the dose of atropine sulfate and/or epinephrine to 3 mg, other strategies besides pharmacological intervention should be considered, such as extracorporeal support (12, 13). We showed that the 1-month survival rate of non-shockable cases was 2.98%, while the same value in the SOS-KANTO data was 2% (3).
Limitations
Several limitations associated with the present study warrant mention. First, it is difficult to conduct a randomized controlled trial for patients with out-of-hospital cardiac arrest in Japan, and we performed a retrospective observational study, which cannot derive decisive conclusions. Second, this study included several sources of bias including 1) selection bias, while epinephrine was administered within 4 minutes from ED arrival in both groups, the two selected, most experienced and skillful emergency physicians have always routinely used atropine following epinephrine during CPR and they could contribute to the better odds ratio for ROSC that was observed in the atropine addition group and 2) resuscitation time bias, as because the 2 groups had a mean call-to-ER arrival interval of longer than 20 minutes (Table 1-1), the time interval from cardiac arrest to administration of epinephrine and atropine was a long and unmeasured variable, as a result, the resuscitation outcomes might have changed if the drugs with epinephrine and atropine had been administered during the circulatory phase (from approximately 4 to 10 minutes after cardiac arrest). “Resuscitation time bias” is very important to consider when evaluating the effect of treatment options in patients with OHCA (14), and adjusting for this bias in a retrospective study is thought to be very difficult. Third, regarding the statistical analyses, we were unable to evaluate the effect of additionally used atropine using propensity score matching instead of logistic regression and therefore could not validate the prediction model due to technical issues. Fourth, the decision to stop ACLS efforts was left to the attending physician's discretion.
However, although the use of short-term outcomes, such as ROSC and the survival to hospital admission, as the primary outcomes in our study was not optimal, and despite long-term outcomes such as the survival to discharge or the 30-day/90-day neurological outcome generally being preferred as more clinically relevant and important, these short-term outcomes are able to more realistically reflect the effect of CPR interventions for two reasons. First, post-resuscitation care can markedly affect the incidence of good recovery, and the care regimens were not standardized in our study. Second, the use of atropine during CPR in our current study significantly influenced the short-term survival but not the long-term survival due to very low prevalence of favorable neurological outcomes, which was comparable to the SOS-KANTO data (approximately 2%) (3).
Conclusion
The addition of atropine (within 2 mg) following epinephrine was a comprehensive independent predictor of the survival to hospital admission for non-shockable (especially asystole) OHCA adults. These preliminary results need to be confirmed in a larger population for further evaluations.
This current study was approved by the ethics committee of Miyazaki Prefectural Nobeoka Hospital.
The authors state that they have no Conflict of Interest (COI).
References
- 1. Robert WN, Charles WO, Mark SL, et al. Part 8: Adult Advanced Cardiovascular Life Support 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 122: S729-S767, 2010. [DOI] [PubMed] [Google Scholar]
- 2. Mark SL, Lauren CB, Peter JK, et al. Part 7: Adult Advanced Cardiovascular Life Support 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 132: S444-S464, 2015. [DOI] [PubMed] [Google Scholar]
- 3. Survey of Survivors After Out-of-hospital Cardiac Arrest in KANTO Area, Japan (SOS-KANTO) Study Group Atropine sulfate for patients with out-of-hospital cardiac arrest due to asystole and pulseless electrical activity. Circ J 75: 580-588, 2011. [DOI] [PubMed] [Google Scholar]
- 4. The Ministry of Health, Labor and Welfare in Japan. The guideline of ethics for the epidemiological survey [Internet]. [cited 2009 July 19]. Available from: http://www.mhlw.go.jp/general/seido/kousei/i-kenkyu/index.html (in Japanese).
- 5. Japan Resuscitation Council Resuscitation Guidelines 2015, Chapter 1: BLS; Basic Life Support [Internet]. [cited 2018 Aug. 4]. Available from: http://www.japanresuscitationcouncil.org/wp-content/uploads/2016/04/1327fc7d4e9a5dcd73732eb04c159a7b.pdf (in Japanese).
- 6. Japan Resuscitation Council Resuscitation Guidelines 2015, Chapter 2: ALS; Advanced Life Support [Internet]. [cited 2018 Aug. 4]. Available from: http://www.japanresuscitationcouncil.org/wp-content/uploads/2016/04/0e5445d84c8c2a31aaa17db0a9c67b76.pdf (in Japanese) .
- 7. Stiell IG, Wells GA, Field B, Ontario Prehospital Advanced Life Support Study Group, et al. Advanced cardiac life support in out-of-hospital cardiac arrest. N Engl J Med 351: 647-656, 2004. [DOI] [PubMed] [Google Scholar]
- 8. Brown DC, Lewis AJ, Criley JM. Asystole and its treatment: the possible role of the parasympathetic nervous system in cardiac arrest. JACEP 8: 448-452, 1979. [DOI] [PubMed] [Google Scholar]
- 9. Coon GA, Clinton JE, Ruiz E. Use of atropine for brady asystolic prehospital cardiac arrest. Ann Emerg Med 10: 462-467, 1981. [DOI] [PubMed] [Google Scholar]
- 10. Stueven HA, Tonsfeldt DJ, Thompson BM, Whitcomb J, Kastenson E, Aprahamian C. Atropine in asystole: human studies. Ann Emerg Med 13: 815-817, 1984. [DOI] [PubMed] [Google Scholar]
- 11. American Heart Association in collaboration with international Liaison Committee on Resuscitation Guidelines 2000 for cardiopulmonary resuscitation and emergency cardiovascular care: international consensus on science. Circulation 102 (Suppl): I1-I384, 2000. [PubMed] [Google Scholar]
- 12. Nagao K, Hayashi N, Kanmatsuse K, et al. Cardiopulmonary cerebral resuscitation using emergency cardiopulmonary bypass, coronary reperfusion therapy and mild hypothermia in patients with cardiac arrest outside the hospital. J Am Coll Cardiol 36: 776-783, 2000. [DOI] [PubMed] [Google Scholar]
- 13. Nagao K, Kikushima K, Watanabe K, et al. Early induction of hypothermia during cardiac arrest improves neurological outcomes in patients with out-of-hospital cardiac arrest who undergo emergency cardiopulmonary bypass and percutaneous coronary intervention. Circ J 74: 77-85, 2010. [DOI] [PubMed] [Google Scholar]
- 14. Sawyer KN, Elmer J. Measuring and improving outcomes that matter to patients after cardiac arrest. Resuscitation 125: 79-82, 2018. [DOI] [PubMed] [Google Scholar]


