Abstract
Osteosarcoma is the most common primary tumor of bone. Osteosarcomas are rare in humans, but occur more commonly in dogs. A comparative approach to studying osteosarcoma has highlighted many clinical and biologic aspects of the disease that are similar between dogs and humans; however, important species-specific differences are becoming increasingly recognized. In this review, we describe risk factors for the development of osteosarcoma in dogs and humans, including height and body size, genetics, and conditions that increase turnover of bone-forming cells, underscoring the concept that stochastic mutational events associated with cellular replication are likely to be the major molecular drivers of this disease. We also discuss adaptive, cancer-protective traits that have evolved in large, long-lived mammals, and how increasing size and longevity in the absence of natural selection can account for the elevated bone cancer risk in modern domestic dogs.
Keywords: bone cancer, osteosarcoma, dog, human, pediatric, comparative oncology, genetics, risk factors
1. Introduction
Osteosarcoma is the most common primary tumor of bone in both dogs and humans. Osteosarcomas are rare in humans, with fewer than 1,000 new cases diagnosed annually [1]. In contrast, osteosarcomas occur more commonly in dogs, although the precise incidence of canine osteosarcoma is not known. A national canine cancer registry does not exist in the United States, European registries are too recent to provide accurate estimates, and most cases of suspected osteosarcoma are not definitively diagnosed histopathologically. Nevertheless, the incidence of osteosarcoma seems to be greater in dogs than in any other species, possibly 10–50 times higher than in humans [1,2,3]. A comparative approach has contributed to our understanding of risk factors associated with osteosarcoma in humans and dogs and has clarified aspects of the disease that are different between the two species. The biological behavior and treatment of osteosarcoma have been the subjects of several recent reviews [4,5,6,7], and the reader is referred to those publications for more extensive coverage of these particular aspects of the disease. The purpose of this review is to highlight risk factors for the development of osteosarcoma in dogs and in humans, underscoring the concept that stochastic mutational events associated with cellular replication are likely to be the major molecular drivers of this disease.
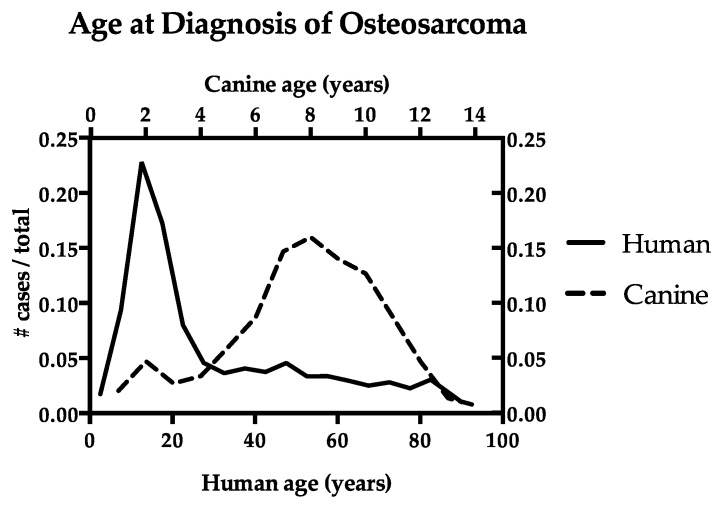
In both dogs and humans, osteosarcoma has a bimodal age distribution with incidence peaks at two distinct ages (Figure 1). Census-derived population data are available in humans, allowing for the calculation of osteosarcoma rates by age [8]. Comparable data are not available in dogs, and therefore numbers are more commonly presented as frequency among cases. In dogs, the largest incidence peak is observed in older adults [3,9,10], with 80% of cases occurring in animals over 7 years old, and more than 50% of cases occurring in animals over 9 years old. A second, smaller peak comprises approximately 6 to 8% of cases in dogs under 3 years of age (juveniles and young adults). Conversely, peak incidence of osteosarcoma in humans occurs in adolescents and young adults [11,12], with 53% of cases occurring in individuals under 24 years of age. A second, smaller peak occurs in the elderly [1,13], with many osteosarcoma cases in individuals over 60 years of age occurring as a second or later malignancy (24.3%) [1,13], or concomitantly with Paget’s disease (9.5%), which is characterized by abnormal bone turnover in the aging (>55 year old) skeleton [14]. Overall, osteosarcoma is an uncommon complication of Paget’s disease, occurring in an estimated 1 in 650 patients. However, this represents an approximately 30-fold increase compared to the general population >40 years old [15].
Figure 1.
Age at diagnosis of osteosarcoma in dogs and humans. The data are represented as the number of cases diagnosed at each age out of the total number of osteosarcoma cases. Human data (n = 4071) are compiled from the SEER 18 database [8]. Canine cases (n = 150) of histopathologically-confirmed appendicular osteosarcoma, complied from the authors’ database, are consistent with published data [16,17,18,19].
Osteosarcoma has been reported in every vertebrate class including a wide variety of mammals such as cats [20,21,22,23,24,25,26,27,28,29], horses [30,31,32,33], cows [34,35,36], African hedgehogs [37,38,39], baboons [40,41], guinea pigs [42,43], rabbits [44,45], and others [46,47,48,49], as well as birds [50,51,52,53], fish [54,55], a woma python [56], and two related spiny-tailed monitor lizards [57]. Primary tumors of bone-forming cells (osteoblastomas) have even been identified in dinosaur fossils [58], and osteosarcoma was recently described in a 240-million-year-old fossil of a shell-less stem-turtle [59]. Interestingly, the only published report of osteosarcoma in amphibians is a Russian abstract reporting the disease in an ancient amphibian fossil [60].
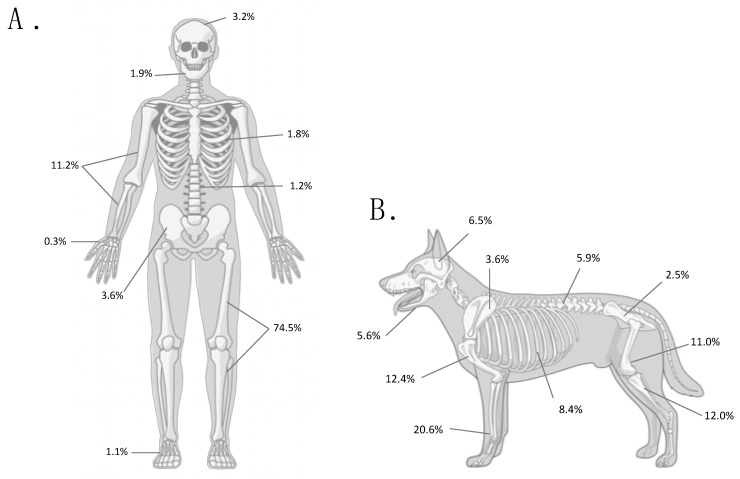
Osteosarcoma almost always originates in the skeletal system (Figure 2). It can affect either the appendicular or axial skeleton; however, osteosarcoma is most commonly diagnosed in the long bones of the extremities in both dogs (estimated at 56–86% of cases) [3,9,61] and humans (75.6–96.8% of cases) [1,12,62]. It is worth noting, however, that in species other than dogs and humans, osteosarcoma occurs most commonly in the axial skeleton.
Figure 2.
Anatomic distribution of osteosarcoma in humans (A) and in dogs (B). Numbers indicate the percentage of cases at each anatomic site out of all osteosarcomas in adolescent humans (<24 years old; n = 1855) [1], and the mean percentage at each anatomic site compiled from five canine studies (n = 1346) [3,9,16,63,64]. Only the most common skeletal sites are included; therefore, percentages do not add up to 100%.
Osteosarcomas of extraskeletal sites, including the skin and subcutaneous tissues [65,66,67,68,69], the liver [65,68,70,71], the lungs [67,72,73,74], and others, have been documented in dogs and humans; however, the frequency of extraskeletal osteosarcoma within all cases of canine osteosarcoma is not known. At a single institution over a 25-year period, Patnaik reported 11 cases of extraskeletal osteosarcoma, compared with approximately 1000 skeletal osteosarcoma cases [75]. The most common site of extraskeletal osteosarcoma documented in two other retrospective studies in dogs was the spleen [65,67], and, in a third study, it was the gastrointestinal tract and the mammary glands [68]. In humans, where there are robust data on osteosarcoma incidence from the Surveillance, Epidemiology, and End Results (SEER) program, extraosseous sites account for fewer than 6% of all osteosarcoma diagnoses, and the frequency increases with age [1]. Less than 1% of osteosarcoma tumors diagnosed in patients between the ages of 0–24 years are extraskeletal, compared with 7% between ages 25–59, and 18% in patients over 60 years old [1].
Cancers are caused by DNA mutations that (1) occur as the result of errors during DNA replication or DNA repair, (2) that develop after exposure to environmental carcinogens, or (3) that are inherited in the germline [76]. Recently, Tomasetti and Vogelstein demonstrated a correlation between the risk of cancer development in a particular tissue with the number of stem cell divisions within that tissue [77,78]. With the application of a machine-learning algorithm, they predicted that up to two-thirds of human cancers could potentially result from unavoidable replicative errors. In this model, the molecular etiology of osteosarcoma was almost entirely attributable to replicative errors, rather than environmental exposures or hereditary factors [77].
The remaining sections of this review will describe risk factors for the development of osteosarcoma in dogs and humans with particular attention to conditions that increase osteoblast turnover, as each replicative cycle has the potential to contribute to the cellular mutational burden and consequent malignant transformation.
2. Hormonal Influence
The peak incidence of age at osteosarcoma diagnosis in children is slightly different in boys (15–19 years) than in girls (10–14 years) [1,2]. This difference in peak age may represent hormonal differences in growth peaks between the two sexes. Males with osteosarcoma (n = 85) began their adolescent growth period and attained their final height earlier than male age-matched control subjects (n = 74) with non-neoplastic orthopedic conditions [79], suggesting that rapid growth could be a risk factor. Earlier onset of puberty was associated with a decreased risk of osteosarcoma in male adolescents in this study [79], suggesting that earlier cessation of growth was protective.
Sex hormones have known effects on bone density and growth [80,81]. Androgens, such as testosterone, increase longitudinal bone growth and stimulate cellular differentiation into osteoblasts. Estrogens, at higher concentrations, play the predominant role in closure of the growth plate. Testosterone may also contribute to growth plate closure through peripheral aromatization into estrogens, allowing binding to α-estrogen receptors (ERα) at the growth plate. A gender predisposition has been documented in humans, with osteosarcoma occurring more commonly in male adolescents (male:female ratio of 1.34:1) [1,11,12]. Gender predisposition has not been reproducibly documented in canine osteosarcoma; studies have reported a male predisposition (male:female ratio of 1.1:1) [16,17], a female predisposition (male:female ratio of 1:1.1) [18,19], or no significant difference in the proportion of male:female cases [3]. Similarly, associations between reproductive status and development of osteosarcoma have been inconsistent [17,18,19]. Although several reports suggest that spayed and/or neutered dogs have higher incidence of certain cancers [82,83], including osteosarcoma [84], the relationship between reproductive status and cancer risk may be confounded by other variables, such as the documented tendency toward increased adiposity and body condition in gonadectomized dogs [85]. Increased load combined with delayed physeal closure, a result of gonadectomy prior to skeletal maturity [86,87], could theoretically contribute to increased osteosarcoma risk in dogs. A recent, carefully controlled study confirmed a significant association between gonadectomy and longer lifespans in both male and female golden retrievers, as well as a significant difference in age between intact and spayed female golden retrievers that died of cancer, with spayed golden retrievers dying at an older age [82]. This study, which only included cancer cases with confirmed necropsy diagnoses, indicates that the loss of gonadal hormone influence does not increase the risk of cancer, at least in golden retrievers. Rather, the longer lifespan that is associated with gonadectomy might be the major factor that accounted for the previously reported increased risk of cancer in gonadectomized dogs [82].
3. Size, Height, and Body Weight
The association between appendicular osteosarcoma and size (height and mass) in both dogs [18,19,88,89] and children [12,79] has been shown in multiple studies. Large (25–45 kg) and giant (>45 kg) dogs have an increased risk of osteosarcoma [90] compared with smaller dogs (<10 kg), (odds ratio (OR) 4.2 and 5.6, respectively) [18]. Another study compared standard adult breed height (a variable created as a proxy measure of body height based on published breed standards) and body weight in German shepherd dogs (arbitrarily selected as the reference population) to those in dogs with osteosarcoma. Large (34–44 kg) and giant (>45 kg) breeds had an increased risk of osteosarcoma compared to their reference population (OR 10.3 and 22.8, respectively), as did breeds with increased standard height (>61 cm, OR 15.8) [19].
Similar associations have been well documented in humans with osteosarcoma. A recent meta-analysis evaluating published studies of osteosarcoma cases in humans <40 years old showed that high birth weight (defined as ≥4000 g) was associated with increased osteosarcoma risk [79]. Similarly, a pooled analysis of data from multiple studies showed that, compared with human subjects whose birth weight was between 2665 and 4045 g, individuals with high birth weights (≥4046 g) had an increased osteosarcoma risk [11]. Studies in this pooled analysis included all ages, although the majority of included cases (93.3%) were <24 years old. Increased birth weight was also shown to be associated with more advanced tumor stage at diagnosis [91] and an increased likelihood of the presence of metastatic disease at diagnosis [91,92]. Studies in humans have also shown that taller-than-average adolescents (individuals in the 51st – 89th percentiles of height for their age) and very tall individuals (≥90th percentile) have an increased risk of osteosarcoma (OR of 1.35 and 2.60, respectively) [11,93]. The majority (62%) of human osteosarcoma cases were above the median reference population height for their age. Cases tended to be approximately 0.26 standard deviations taller than the reference population, resulting in an average height difference of 2–3 cm [93].
4. Risks from Increased Cell Division/Turnover
The risk of developing osteosarcoma appears to be amplified under conditions that drive excess osteoblast proliferation. Osteosarcoma develops most commonly at or near the site of the growth plates, where cell turnover is highest [94,95]. In addition to overall body size, growth rate might contribute directly to osteosarcoma risk and other abnormalities in skeletal maturation [3,96]. Rapid bone growth results in increased bone remodeling and increased cell turnover. To minimize the risk of developmental bone disease, it is currently recommended to limit energy intake in large breed puppies to prevent rapid growth [96]. Rapid bone growth has been identified as a risk factor for osteosarcoma in humans as well. This is supported by the observations that male adolescents with osteosarcoma tend to have an earlier onset of the adolescent growth period and earlier attainment of final height [79].
Osteosarcoma risk also appears to increase in conditions that drive osteoblast proliferation, such as surgical fracture repair [21,97,98] and orthopedic implant surgery [99,100,101,102,103]. Interestingly, an observation has been stated that AKC-registered “show” greyhounds are at lower risk for developing osteosarcoma than racing greyhounds (G. Couto, unpublished observation, [104]). However, the frequencies of osteosarcoma in racing and show greyhounds have not been published in the peer-reviewed literature, and thus cannot be directly compared. If confirmed, this difference might be due to the effects of concussive forces during training and performance racing, with the potential to create micro-fractures and activate chronic repair processes. Further evidence to support microscopic trauma as a predisposing factor for osteosarcoma is the tendency for appendicular osteosarcoma to occur in weight-bearing bones. Canine appendicular osteosarcoma occurs more commonly in the long bones of forelimbs [19,105], which support approximately 60% of total body weight of the dog. Similarly, in humans, 74.6% of adolescent osteosarcomas occur in the weight-bearing lower limb bones compared with only 11.2% in the bones of the upper limb [1].
There are also anecdotal associations linking osteosarcoma and increased cell turnover due to inflammation. Visceral osteosarcoma secondary to retained surgical sponges has been reported in dogs [65,106], as has a case of osteosarcoma at the site of a previous subcutaneous injection [107]. Several cases of esophageal osteosarcoma are reported in dogs secondary to infection with the nematode parasite Spirocerca lupi [108,109,110,111]. There is a case report of orbital osteosarcoma in a cat, several years after enucleation for ocular melanoma, secondary to retention of conjunctival epithelium leading to cyst formation [24]. In humans, osteosarcoma has been diagnosed at the site of cutaneous scars resulting from dermal burn injury [112], following bone graft surgery [113], and at a site of previous electrodessication for actinic keratosis [114]. A case of primary hepatic osteosarcoma was diagnosed in a man with a history of hepatitis C infection and liver cirrhosis [71].
5. Germline and Somatic Driver Alterations
Unlike many other cancers that are characterized by simple predictable chromosomal rearrangements and relatively low mutation rates, osteosarcoma is a genetically diverse and karyotypically complex cancer [115], characterized by chromosomal instability, copy number alterations, and chromothripsis [116]. The chromosomal instability in osteosarcoma tumors does not necessarily lead to a high mutational burden [117]. There is a moderate mutational burden in osteosarcoma, comparable to many common forms of adult cancers [118], yet recurrent mutations, aside from TP53, are infrequent [119,120]. TP53 was the most commonly mutated gene in a whole exome sequencing (WES) study of matched tumor and normal tissues in dogs, with somatic TP53 mutations occurring in approximately 60% of tumor samples [121]. This study also found somatic mutations in SETD2 in 21% of canine tumor samples [121]. SETD2, a histone methyltransferase that functions as a tumor suppressor, is mutated in a variety of human cancers [122,123,124,125]; however, somatic SETD2 mutations occur in <2% of human osteosarcoma samples [126].
Osteosarcoma occurs more often in humans with Li-Fraumeni syndrome [127,128,129,130], familial retinoblastoma [131,132,133,134,135,136,137,138,139,140], and Paget’s disease [14,141,142,143,144,145]. It can also occur as a second or later malignancy [131,132,133,134,135,136,137,138,139,140,142]. However, these cases represent a small portion of all osteosarcoma diagnoses, and in approximately 88% of all cases there is no known predisposing condition [1]. The percentage of osteosarcoma cases associated with a predisposing condition varies with age. Only about 4% of osteosarcomas in young human subjects (≤24 years old) occur as a second malignancy or with Paget’s disease, compared with approximately 34% in subjects over 60 years of age [1]. This difference is likely due to the increased prevalence of Paget’s disease and higher likelihood of prior malignancies in older populations.
Osteosarcoma is one of the most common malignancies seen in patients with Li-Fraumeni syndrome, in which germline TP53 mutations occur in as many as 83% of cases [146,147]. Adolescent humans with osteosarcoma are more likely to have germline TP53 variants, with germline TP53 mutations occurring in 9.5% of young (<30 years old) osteosarcoma patients [148]. Pathogenic germline TP53 variants were recently reported in 3 out of 95 (3.2%) human osteosarcoma patients <20 years old; importantly, two of the three mutations were considered to be de novo [149].
In hereditary retinoblastoma, an uncommon disorder where people have germline mutations of the retinoblastoma (RB1) gene, affected individuals have a reported 69-fold increase in the risk of osteosarcoma, which then increases to greater than 400-fold after radiation therapy [150]. In sporadic (i.e., non-hereditary) cases of osteosarcoma, somatic mutations in the RB1 gene occur in 20–75% of tumors [119,151,152,153,154].
In addition to mutations in TP53 and RB1, a candidate gene association study identified several variants in growth or DNA repair genes that were significantly associated with osteosarcoma [155]. A second candidate gene study of osteosarcoma patients and their unaffected parent(s) discovered variants in estrogen-receptor signaling genes that were significantly associated with osteosarcoma incidence [156]. A genome-wide association study (GWAS) in humans identified two loci associated with the presence of osteosarcoma in a gene desert of chromosome 2, specifically in the glutamate receptor metabotropic 4 (GRM4) gene [157]. Additionally, a single, distinct locus in the NFIB gene was significantly associated with the presence of metastasis at diagnosis [158]. A trio GWAS study, evaluating pediatric osteosarcoma patients and their unaffected parents, identified genes that achieved significance related to TP53, estrogen-receptor signaling, and others [159].
GWAS data in three high-risk dog breeds (greyhounds, Rottweilers, and Irish wolfhounds) indicate that the patterns of heritable risk are complex and incompletely penetrant [104]. In that study, 33 loci were enriched in this population of osteosarcoma cases, including variants near CDKN2A/B. None of the risk loci were shared between the breeds, but this was due in part to fixed risk alleles for some of the genes in one or more breeds.
Another study, which evaluated whole exome sequencing of matched tumor and normal tissues in three dog breeds predisposed to osteosarcoma (golden retrievers, Rottweilers, and greyhounds), showed germline variants in genes previously associated with osteosarcoma in many of the samples. The most common genes affected were CDKN2A/B and GRM4 in 31.8% and 18.2% of cases, respectively [121]. Additional germline variants commonly seen in human osteosarcoma cases (RB, TP53, and NFIB) were uncommon in this canine cohort, occurring in only one case each [121].
Despite the identification of various germline and somatic mutations in cases of osteosarcoma, we should emphasize that the only recurrent alteration consistently identified in both human and canine osteosarcoma is mutation or copy number alteration of TP53. Additionally, it has been shown that the specific alterations affecting TP53 are not recurrent.
6. Canine Osteosarcoma Provides a Resolution to Peto’s Paradox
In 1977, epidemiologist Richard Peto noted that cancer incidence does not appear to correlate with the size of the organism. He expressed this observation, which came to be known as Peto’s Paradox, by comparing humans and mice: Although humans have 1000 times the number of cells as mice and typically live at least 30 times longer, cancer probability was not vastly different between the two species [160]. This paradox seemingly conflicted with the multistage model of carcinogenesis, proposed in 1954 by Peter Armitage and Richard Doll, which is based on the principle that cancer develops after a cell has accumulated a series of somatic mutations sufficient for carcinogenesis [161]. Based on the multistage model, organisms with increased cellular mass and/or longer lifespans (allowing for more cell divisions and increased exposure to potential DNA damaging agents) should have a higher incidence of cancer development.
Indeed, within a species, there is evidence for a correlation between increased cellular mass and osteosarcoma development. The increased risk of osteosarcoma in large and giant breed dogs, and in children who are in the higher percentiles of size for their age, can be partly explained by the fact that more cell divisions are needed for the formation and continuous remodeling of the long bones of the appendicular skeleton. Somatic mutations occurring during cell division can either undergo DNA repair, cause apoptosis of the cell, or potentially lead to carcinogenesis. Therefore, every replicative cycle of a cell, such as an osteoblast, has the potential to contribute to its mutational burden and transformation. Additionally, appendicular osteosarcoma tends to develop at or near the growth plates of long bones in both dogs and humans, suggesting an association with cell division [94,95].
There is also evidence for a correlation between longevity and cancer incidence within a given species. Many cancers are diseases of the aged, likely due to accumulation of a sufficient number or combination of cancer-initiating somatic mutations. The late age of osteosarcoma onset in dogs, although not in humans, is consistent with chronic selection for cells that accumulate a critical complement of mutations.
Therefore, it appears that achieving a large size relatively rapidly is a primary contributor to osteosarcoma risk. Why, then, do “giant” animals not commonly develop osteosarcoma (and other cancers)? If the probability of cancer development were constant across cells, one would expect a higher incidence of cancer in giant animals, such as elephants or whales. On the contrary, cancer incidence in humans and dogs is much higher than in these giant animals. Indeed, there appears to be no significant relationship between body size and cancer risk across different species. A comprehensive survey of necropsy data from captive zoo animals across 36 different mammalian species compared mortality due to any cancer by body size and lifespan [162]. With a minimum of 10 necropsies per species, animals ranged from the striped grass mouse, with a body weight of 51 g and a lifespan of 4.5 years, to the elephant, with a body weight of 4800 kg and a lifespan of 65 years. The authors found no significant relationship between body mass, lifespan, and cancer incidence [162]. The available literature on cancer incidence in large mammals is primarily based on captive animals held in zoos or wildlife sanctuaries; less is known about cancer incidence in wild mammals. Additionally, cancer incidence rates in large mammals typically do not take into account species population size.
Although the multistage model of carcinogenesis appears to remain true within a given species, as larger and longer-lived individuals have higher incidences of cancer, it does not hold true across different species. What, then, is the answer to Peto’s Paradox? It appears that the answer lies in the evolution of anti-cancer protective mechanisms in giant and long-lived species, reducing cancer risk and delaying cancer development beyond reproductive age and for the duration of the lifespan to which particular species have adapted in their unique evolutionary niche. Such mechanisms are unique to each species, conferring sufficient protection for their evolutionary lifespans.
There is a strong evolutionary pressure to delay cancer development until after the reproductive age in longer-lived animals that tend to reproduce later in life and that invest significant resources of time and energy rearing young. One mechanism that is protective against cancer in larger mammals (>10 kg) is replicative senescence due to telomere shortening. Most human somatic cells cease to express telomerase reverse transcriptase (TERT) after embryonic development leading to decreased telomerase production. With repeated cellular division, the telomeres of most somatic cells shorten. Replicative senescence occurs when telomeres reach a critically short length and the cell enters into a state of cell cycle arrest [163]. While most species with larger body mass have evolved the ability to undergo replicative senescence [164], smaller mammals such as rodents retain expression of telomerase and their cells do not undergo replicative senescence. Somatic mutations [165] and germline polymorphisms [166,167] in genes associated with increasing or maintaining telomere length have been documented in patients with various cancers, including a germline variant in OBFC1 significantly associated with pediatric osteosarcoma [167], providing further support for the role of replicative senescence in cancer protection. Maintaining or increasing telomere length may increase the risk of cancer development by allowing a cell to undergo more cell divisions, and therefore potentially accumulate more mutations before senescence.
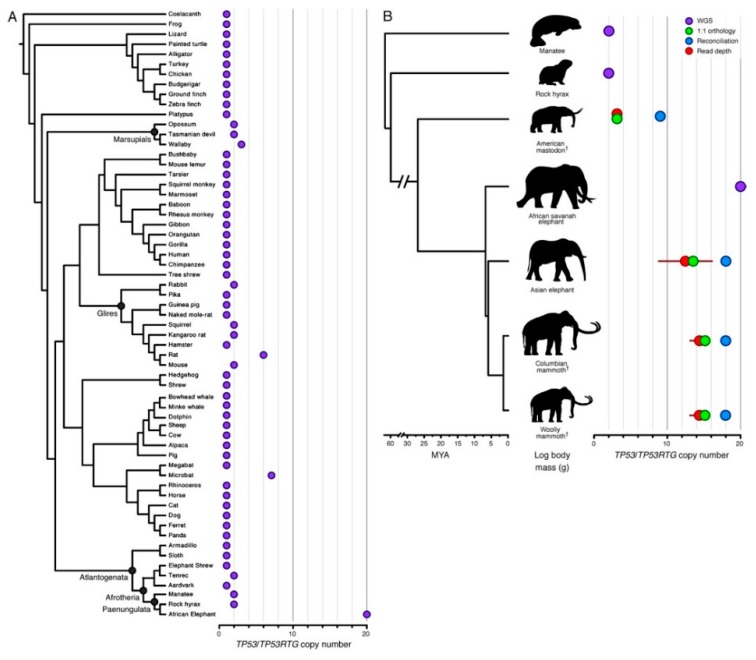
Elephants are the largest living land mammals, with an average body weight of 4800 kg and long lifespans (65 years) [162]; yet, cancer rates in elephants are quite low. The estimated cancer mortality rate in elephants, based on necropsy data from 644 captive African and Asian elephants, is about 5% [162], compared with up to 25% in humans [168]. Based on a mathematical model of carcinogenesis [169], it was determined that a 2.17-fold decrease in mutation rate would be necessary to provide sufficient protection against cancer development in elephants, given that their cellular mass is estimated to be 100 times that of humans [162]. It was recently discovered that in the elephant lineage, the TP53 gene underwent multiple duplication events after the split from a common ancestor that gave rise to hyraxes and manatees, but that preceded diversification into Proboscideans such as modern elephants and their extinct relatives, mastodons and mammoths (Figure 3) [170]. Humans and elephants each have one copy of TP53, but African elephants also have 19 TP53 duplication events, or retrogenes (TP53RTG) in their genome [162,170], 14 of which retain the potential to encode truncated p53 proteins [170]. Similarly, Asian elephants have 12–17 TP53RTG, and their extinct relatives, wooly mammoths and Columbian mammoths, also had 14 TP53RTGs. Each TP53RTG sequence is flanked on both sides by nearly identical transposable elements, which suggests that the copy number expansion was initiated by a single retrotransposition event, followed by repeated rounds of segmental duplication [170]. The expansion of the TP53RTG family in the Proboscidean lineage results in an enhanced p53-dependent DNA damage response leading to apoptosis, when compared to smaller relatives [162] such as hyraxes and aardvarks. Moreover, an elephant-specific leukemia inhibitory factor (LIF) pseudogene duplicate, Zombie LIF6, is upregulated by TP53 in response to DNA damage, leading to apoptosis [171]. This increased TP53-dependent apoptotic response in elephants may be protective against cancer development by removing cells with DNA damage from the dividing population before a cancerous state can develop. Despite its potentially protective role in elephants, we should note that TP53 duplication is neither necessary nor sufficient for cancer protection; other mammals (e.g., whales) have evolved cancer-protective mechanisms distinct from TP53 duplication, while still others (e.g., rats) have TP53 duplication, and yet are not known to experience dramatic cancer protection. However, combined with other selective pressures in elephants, amplification of p53 could serve as a protective mechanism for longevity without cancer.
Figure 3.
Expansion of the TP53RTG gene repertoire in Proboscideans. (A) TP53 copy number in 61 Sarcopterygian (Lobe-finned fish) genomes. Clade names are shown for lineages in which the genome encodes more than one TP53 gene or pseudogene. (B) Estimated TP53/TP53RTG copy number inferred from complete genome sequencing data (WGS, purple), 1:1 orthology (green), gene tree reconciliation (blue), and normalized read depth from genome sequencing data (red). Whiskers on normalized read depth copy number estimates show the 95% confidence interval of the estimate. Reproduced with permission from “TP53 copy number expansion is associated with the evolution of increased body size and an enhanced DNA damage response in elephants”, Sulak et al., 2016. https://doi.org/10.7554/eLife.11994.004.
Whales include the largest living animals, yet similar to elephants, they seem to have very low rates of cancer. The bowhead whale is the fifth largest whale species and is capable of living more than 200 years, the longest known lifespan of any mammal. Unlike elephants, the bowhead whale genome does not have extra copies of the TP53 gene. Rather, these animals have variants and copy number changes in multiple genes that seem to confer protection from cancer and aging, i.e., they are under positive selection [172]. Notably, bowhead whales were found to have increased ERCC1 (excision repair cross-complementing rodent repair deficiency, complementation group 1), and duplication of PCNA (proliferating cell nuclear antigen). Both are involved in DNA repair [172] and represent a distinct, albeit convergent, mechanism to confer cancer protection by decreasing the accumulation of mutations in dividing cells.
In addition to the large, long-lived species described, there are several smaller long-lived species that are known to have developed unique mechanisms of cancer prevention, such as the naked mole rat, a small rodent that, in captivity, can live more than 30 years. In contrast with other rodents that have high rates of tumor development, there have been only a few instances of cancer reported in the naked mole rat. Proposed cancer-protective mechanisms in this species include a slow cellular duplication rate, which is hypothesized to restrict malignant growth [173], and a reported hypersensitivity to contact inhibition [174]. Additionally, inactivation of either TP53 or RB alone in naked mole rat cells leads to apoptosis, rather than the cellular proliferation seen in other species [174,175].
It is apparent that these cancer-protective mechanisms are part of the evolutionary adaptation of each species to its own niche, including lifespan and body size, likely happening over tens or hundreds of millions of years (Figure 3). In addition, despite the fact that only a few of them have been characterized to date, it is likely that such protective mechanisms to prevent or reduce cancer-causing cellular mutations exist in every species, including humans and dogs. Concomitantly, it is likely that these adaptive solutions to enable large size with longevity are unique and specific to the evolutionary history of each species.
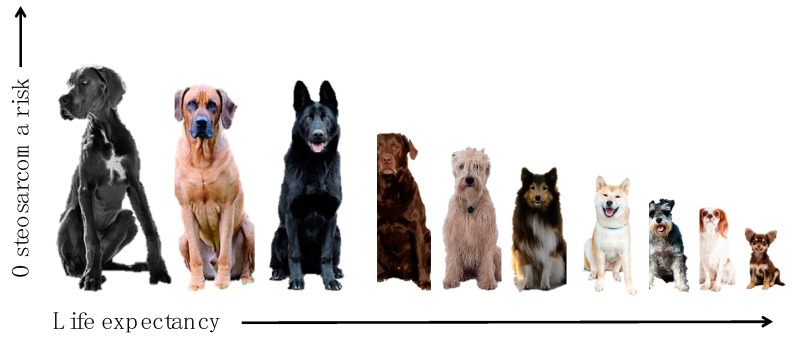
Viewed in this evolutionary context, Peto’s paradox disappears and allows us to conclude that the remarkably high rate of cancers in large and giant breed dogs is a result of artificial selection for large breeds without co-selection for cancer-protective mechanisms that would occur under conditions of truly natural selection. Selective breeding, especially for large size, has enriched risk alleles for osteosarcoma in certain populations that now appear to be fixed (Figure 4) [3,104,176]. The removal of natural selective pressures combined with increased longevity decreases the chances of adaptation across the rest of the genome. Consequently, the risks of mutation associated with normal processes of cell replication during development, growth, and maintenance into adulthood [77,78], are enhanced in large dogs, making it possible to explain their skewed risk of appendicular osteosarcoma by manipulation of their genomic plasticity with extreme selection for size. This explanation is also consistent with the observation that canine osteosarcoma is less common in the axial skeleton (similar to what is seen in other species) than in long bones, accounting for the effects of size and functional/mechanical stresses on bone.
Figure 4.
Risk of osteosarcoma and life expectancy are associated with body size in dogs. Large and giant breed dogs generally have shorter lifespans and an increased risk of osteosarcoma compared with smaller breed dogs.
7. Conclusions
In summary, the extremely high risk of appendicular osteosarcoma in large and giant breed dogs may often be the result of replicative mutations caused by normal processes of cell division required to create longer bones, with only modest contributions from heritable or environmental factors. Although a comparative approach enhances our understanding of osteosarcoma, we should also acknowledge that in addition to the many similarities between canine and human osteosarcoma, there are important species-specific differences. This recognition is essential to design innovative comparative studies that will maximize the potential for developing safer and more effective strategies to prevent and treat osteosarcoma in both dogs and people. Additionally, insights from large mammals that have evolved cancer-protective mechanisms to adapt to their species-specific niche, including lifespan and body size, can help elucidate distinct undiscovered mechanisms of cancer protection in other species, such as dogs and humans.
Acknowledgments
The authors would like to acknowledge Mitzi Lewellen for reviewing this manuscript.
Author Contributions
Conceptualization, K.M.M., L.J.M, A.L.S., M.S.H., L.G.S., and J.F.M.; Methodology, L.J.M. and A.L.S.; Validation, L.J.M. and A.L.S.; Investigation, K.M.M., J.F.M.; Resources, K.M.M., L.G.S., J.F.M.; Data Curation, K.M.M., L.G.S., J.F.M.; Writing—Original Draft Preparation, K.M.M., J.F.M.; Writing—Review & Editing, K.M.M., L.J.M, A.L.S., M.S.H., L.G.S., S.N., J.F.M.; Visualization, K.M.M., L.J.M, A.L.S., M.S.H., L.G.S., S.N., and J.F.M.; Supervision, J.F.M.; Project Administration, J.F.M.; Funding Acquisition, K.M.M., J.F.M.
Funding
K.M.M. would like to acknowledge support from an NIH Cancer Biology Training Grant, T32 CA009138. J.F.M. is supported by the Alvin and June Perlman Chair in Animal Oncology. A.L.S. is supported by an NIH NCI R50 grant, CA211249. This work was supported in part by the Zach Sobiech Osteosarcoma Fund of the Children’s Cancer Research Fund, Minneapolis, MN. The authors gratefully acknowledge support from donors to the Animal Cancer Care and Research Program of the University of Minnesota that helped support this work.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Mirabello L., Troisi R.J., Savage S.A. Osteosarcoma incidence and survival rates from 1973 to 2004: Data from the Surveillance, Epidemiology, and End Results Program. Cancer. 2009;115:1531–1543. doi: 10.1002/cncr.24121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anfinsen K.P., Devesa S.S., Bray F., Troisi R., Jonasdottir T.J., Bruland O.S., Grotmol T. Age-period-cohort analysis of primary bone cancer incidence rates in the United States (1976–2005) Cancer Epidemiol. Biomark. Prev. 2011;20:1770–1777. doi: 10.1158/1055-9965.EPI-11-0136. [DOI] [PubMed] [Google Scholar]
- 3.Anfinsen K.P., Grotmol T., Bruland O.S., Jonasdottir T.J. Breed-specific incidence rates of canine primary bone tumors—A population based survey of dogs in Norway. Can. J. Vet. Res. 2011;75:209–215. [PMC free article] [PubMed] [Google Scholar]
- 4.Simpson S., Dunning M.D., de Brot S., Grau-Roma L., Mongan N.P., Rutland C.S. Comparative review of human and canine osteosarcoma: Morphology, epidemiology, prognosis, treatment and genetics. Acta Vet. Scand. 2017;59:71. doi: 10.1186/s13028-017-0341-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fenger J.M., London C.A., Kisseberth W.C. Canine osteosarcoma: A naturally occurring disease to inform pediatric oncology. ILAR J. 2014;55:69–85. doi: 10.1093/ilar/ilu009. [DOI] [PubMed] [Google Scholar]
- 6.Mueller F., Fuchs B., Kaser-Hotz B. Comparative biology of human and canine osteosarcoma. Anticancer Res. 2007;27:155–164. [PubMed] [Google Scholar]
- 7.Wycislo K.L., Fan T.M. The immunotherapy of canine osteosarcoma: A historical and systematic review. J. Vet. Intern. Med. 2015;29:759–769. doi: 10.1111/jvim.12603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National Cancer Institute . SEER 18 Research Data: Incidence (2000–2015) National Cancer Institute; Bethesda, MD, USA: 2018. Surveillance, Epidemiology, and End Results (SEER) Program (www.seer.cancer.gov. ) [Google Scholar]
- 9.Al-Khan A.A., Gunn H.J., Day M.J., Tayebi M., Ryan S.D., Kuntz C.A., Saad E.S., Richardson S.J., Danks J.A. Immunohistochemical Validation of Spontaneously Arising Canine Osteosarcoma as a Model for Human Osteosarcoma. J. Comp. Pathol. 2017;157:256–265. doi: 10.1016/j.jcpa.2017.07.005. [DOI] [PubMed] [Google Scholar]
- 10.Withers S.S., Skorupski K.A., York D., Choi J.W., Woolard K.D., Laufer-Amorim R., Sparger E.E., Rodriguez C.O., McSorley S.J., Monjazeb A.M., et al. Association of macrophage and lymphocyte infiltration with outcome in canine osteosarcoma. Vet. Comp. Oncol. 2018 doi: 10.1111/vco.12444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mirabello L., Pfeiffer R., Murphy G., Daw N.C., Patino-Garcia A., Troisi R.J., Hoover R.N., Douglass C., Schuz J., Craft A.W., et al. Height at diagnosis and birth-weight as risk factors for osteosarcoma. Cancer Causes Control. 2011;22:899–908. doi: 10.1007/s10552-011-9763-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Longhi A., Pasini A., Cicognani A., Baronio F., Pellacani A., Baldini N., Bacci G. Height as a risk factor for osteosarcoma. J. Pediatr. Hematol. Oncol. 2005;27:314–318. doi: 10.1097/01.mph.0000169251.57611.8e. [DOI] [PubMed] [Google Scholar]
- 13.Mirabello L., Troisi R.J., Savage S.A. International osteosarcoma incidence patterns in children and adolescents, middle ages and elderly persons. Int. J. Cancer. 2009;125:229–234. doi: 10.1002/ijc.24320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hansen M.F., Seton M., Merchant A. Osteosarcoma in Paget’s disease of bone. J. Bone Miner. Res. 2006;21:P58–P63. doi: 10.1359/jbmr.06s211. [DOI] [PubMed] [Google Scholar]
- 15.Price C.H. The incidence of osteogenic sarcoma in South-West England and its relationship to Paget’s disease of bone. J. Bone Joint Surg. Br. 1962;44-B:366–376. doi: 10.1302/0301-620X.44B2.366. [DOI] [PubMed] [Google Scholar]
- 16.Egenvall A., Nodtvedt A., von Euler H. Bone tumors in a population of 400 000 insured Swedish dogs up to 10 y of age: Incidence and survival. Can. J. Vet. Res. 2007;71:292–299. [PMC free article] [PubMed] [Google Scholar]
- 17.Hillers K.R., Dernell W.S., Lafferty M.H., Withrow S.J., Lana S.E. Incidence and prognostic importance of lymph node metastases in dogs with appendicular osteosarcoma: 228 cases (1986–2003) J. Am. Vet. Med. Assoc. 2005;226:1364–1367. doi: 10.2460/javma.2005.226.1364. [DOI] [PubMed] [Google Scholar]
- 18.Sapierzynski R., Czopowicz M. The animal-dependent risk factors in canine osteosarcomas. Pol. J. Vet. Sci. 2017;20:293–298. doi: 10.1515/pjvs-2017-0035. [DOI] [PubMed] [Google Scholar]
- 19.Ru G., Terracini B., Glickman L.T. Host related risk factors for canine osteosarcoma. Vet. J. 1998;156:31–39. doi: 10.1016/S1090-0233(98)80059-2. [DOI] [PubMed] [Google Scholar]
- 20.Dimopoulou M., Kirpensteijn J., Moens H., Kik M. Histologic prognosticators in feline osteosarcoma: A comparison with phenotypically similar canine osteosarcoma. Vet. Surg. 2008;37:466–471. doi: 10.1111/j.1532-950X.2008.00409.x. [DOI] [PubMed] [Google Scholar]
- 21.Sonnenschein B., Dickomeit M.J., Bali M.S. Late-onset fracture-associated osteosarcoma in a cat. Vet. Comp. Orthop. Traumatol. 2012;25:418–420. doi: 10.3415/VCOT-11-10-0143. [DOI] [PubMed] [Google Scholar]
- 22.Taulescu M.A., Carlson C.S., Amorim I.F., De Fatima Gartner M., Farcas L., Gal A.F., Catoi C. Pathology in practice. Productive osteoblastic osteosarcoma of the left humerus with unilateral eye, cervical muscle, pulmonary, renal, jejunal mesentery, and liver metastases. J. Am. Vet. Med. Assoc. 2014;245:1103–1105. doi: 10.2460/javma.245.10.1103. [DOI] [PubMed] [Google Scholar]
- 23.Griffith J.W., Dubielzig R.R., Riser W.H., Jezyk P. Parosteal osteosarcoma with pulmonary metastases in a cat. Vet. Pathol. 1984;21:123–125. doi: 10.1177/030098588402100123. [DOI] [PubMed] [Google Scholar]
- 24.Groskopf B.S., Dubielzig R.R., Beaumont S.L. Orbital extraskeletal osteosarcoma following enucleation in a cat: A case report. Vet. Ophthalmol. 2010;13:179–183. doi: 10.1111/j.1463-5224.2010.00774.x. [DOI] [PubMed] [Google Scholar]
- 25.Heldmann E., Anderson M.A., Wagner-Mann C. Feline osteosarcoma: 145 cases (1990–1995) J. Am. Anim. Hosp. Assoc. 2000;36:518–521. doi: 10.5326/15473317-36-6-518. [DOI] [PubMed] [Google Scholar]
- 26.Nakata K., Miura H., Sakai H., Mori T., Shibata S., Nishida H., Maeda S., Kamishina H. Vertebral replacement for the treatment of vertebral osteosarcoma in a cat. J. Vet. Med. Sci. 2017;79:999–1002. doi: 10.1292/jvms.17-0142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Negrin A., Bernardini M., Diana A., Castagnaro M. Giant cell osteosarcoma in the calvarium of a cat. Vet. Pathol. 2006;43:179–182. doi: 10.1354/vp.43-2-179. [DOI] [PubMed] [Google Scholar]
- 28.Stimson E.L., Cook W.T., Smith M.M., Forrester S.D., Moon M.L., Saunders G.K. Extraskeletal osteosarcoma in the duodenum of a cat. J. Am. Anim. Hosp. Assoc. 2000;36:332–336. doi: 10.5326/15473317-36-4-332. [DOI] [PubMed] [Google Scholar]
- 29.Yuki M., Nitta M., Omachi T. Parathyroid hormone-related protein-induced hypercalcemia due to osteosarcoma in a cat. Vet. Clin. Pathol. 2015;44:141–144. doi: 10.1111/vcp.12224. [DOI] [PubMed] [Google Scholar]
- 30.Bush J.M., Fredrickson R.L., Ehrhart E.J. Equine osteosarcoma: A series of 8 cases. Vet. Pathol. 2007;44:247–249. doi: 10.1354/vp.44-2-247. [DOI] [PubMed] [Google Scholar]
- 31.Cesar F.B., Joiner K.S., Albanese V., Groover E.S., Waguespack R.W. Pathology in Practice. Poorly productive, osteoblastic osteosarcoma of the left paranasal sinuses in a 1-year-old colt. J. Am. Vet. Med. Assoc. 2016;248:773–775. doi: 10.2460/javma.248.7.773. [DOI] [PubMed] [Google Scholar]
- 32.Jenner F., Solano M., Gliatto J., Lavallee S., Kirker-Head C. Osteosarcoma of the tarsus in a horse. Equine Vet. J. 2003;35:214–216. doi: 10.2746/042516403776114090. [DOI] [PubMed] [Google Scholar]
- 33.Zaruby J.F., Williams J.W., Lovering S.L. Periosteal osteosarcoma of the scapula in a horse. Can. Vet. J. 1993;34:742–744. [PMC free article] [PubMed] [Google Scholar]
- 34.Nagamine E., Matsuda K., Ishii C., Koiwa M., Taniyama H. Primary ischial osteosarcoma occupying the pelvic cavity in a Japanese Black cow. J. Vet. Med. Sci. 2014;76:891–894. doi: 10.1292/jvms.13-0491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Plumlee K.H., Haynes J.S., Kersting K.W., Thompson J.R. Osteosarcoma in a cow. J. Am. Vet. Med. Assoc. 1993;202:95–96. [PubMed] [Google Scholar]
- 36.Prins D.G., Wittek T., Barrsett D.C. Maxillary osteosarcoma in a beef suckler cow. Ir. Vet. J. 2012;65:15. doi: 10.1186/2046-0481-65-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Benoit-Biancamano M.O., D’Anjou M.A., Girard C., Langlois I. Rib osteoblastic osteosarcoma in an African hedgehog (Atelerix albiventris) J. Vet. Diagn. Invest. 2006;18:415–418. doi: 10.1177/104063870601800420. [DOI] [PubMed] [Google Scholar]
- 38.Reyes-Matute A., Mendez-Bernal A., Ramos-Garduno L.A. Osteosarcoma in African Hedgehogs (Atelerix albiventris): Five Cases. J. Zoo Wildl. Med. 2017;48:453–460. doi: 10.1638/2016-0260R.1. [DOI] [PubMed] [Google Scholar]
- 39.Rhody J.L., Schiller C.A. Spinal osteosarcoma in a hedgehog with pedal self-mutilation. Vet. Clin. North Am. Exot. Anim. Pract. 2006;9:625–631. doi: 10.1016/j.cvex.2006.05.016. [DOI] [PubMed] [Google Scholar]
- 40.Mezzles M.J., Dick E.J., Jr., Owston M.A., Bauer C. Osteosarcoma in Baboons (Papio spp.) Comp. Med. 2015;65:144–149. [PMC free article] [PubMed] [Google Scholar]
- 41.Russell S.W., Jenson F.C., Vanderlip J.E., Alexander N.L. Osteosarcoma of the mandible of a baboon (Papio papio): Morphological and virological (oncornavirus) studies, with a review of neoplasms previously described in baboons. J. Comp. Pathol. 1979;89:349–360. doi: 10.1016/0021-9975(79)90024-0. [DOI] [PubMed] [Google Scholar]
- 42.Brunetti B., Bo P., Sarli G. Pathology in practice. Productive osteoblastic osteosarcoma with metastases in a guinea pig. J. Am. Vet. Med. Assoc. 2013;243:801–803. doi: 10.2460/javma.243.6.801. [DOI] [PubMed] [Google Scholar]
- 43.Cojean O., Langlois I., Begin-Pepin M., Helie P. Chondroblastic osteosarcoma of the middle ear in a guinea pig (Cavia porcellus) Can. Vet. J. 2018;59:855–859. [PMC free article] [PubMed] [Google Scholar]
- 44.Ishikawa M., Kondo H., Onuma M., Shibuya H., Sato T. Osteoblastic osteosarcoma in a rabbit. Comp. Med. 2012;62:124–126. [PMC free article] [PubMed] [Google Scholar]
- 45.Kondo H., Ishikawa M., Maeda H., Onuma M., Masuda M., Shibuya H., Koie H., Sato T. Spontaneous osteosarcoma in a rabbit (Oryctolagus cuniculus) Vet. Pathol. 2007;44:691–694. doi: 10.1354/vp.44-5-691. [DOI] [PubMed] [Google Scholar]
- 46.Dadone L.I., Whiteside D.P., Black S.R., Remedios A., Raverty S. Nasal osteosarcoma and interstitial cell tumor in a Vancouver Island marmot (Marmota vancouverensis) J. Zoo Wildl. Med. 2011;42:330–334. doi: 10.1638/2010-0159.1. [DOI] [PubMed] [Google Scholar]
- 47.de Oliveira Conrado F., Bruno S.F., de Alencar N.X. What is your diagnosis? Scapular mass in a Chinese hamster. Vet. Clin. Pathol. 2013;42:533–534. doi: 10.1111/vcp.12083. [DOI] [PubMed] [Google Scholar]
- 48.Johnson J.G., 3rd, Kim K., Serio J., Paulsen D., Rademacher N., Pirie G. Mandibular osteosarcoma in a nutria (Myocastor coypus) J. Zoo Wildl. Med. 2014;45:723–726. doi: 10.1638/2014-0032R.1. [DOI] [PubMed] [Google Scholar]
- 49.Rodriguez-Ramos Fernandez J., Thomas N.J., Dubielzig R.R., Drees R. Osteosarcoma of the maxilla with concurrent osteoma in a southern sea otter (Enhydra lutris nereis) J. Comp. Pathol. 2012;147:391–396. doi: 10.1016/j.jcpa.2012.01.017. [DOI] [PubMed] [Google Scholar]
- 50.Churgin S.M., Steinberg H., Ravi M., Hartup B.K. Sternal osteosarcoma in a blue crane (Anthropoides paradiseus) J. Zoo Wildl. Med. 2013;44:1075–1078. doi: 10.1638/2012-0199R.1. [DOI] [PubMed] [Google Scholar]
- 51.De Luca Bossa L.M., Mennonna G., Meomartino L., Paciello O., Ciccarelli F., De Biase D., Raia P., Caputo V., Fioretti A., Dipineto L. Polyostotic Chondroblastic Osteosarcoma in a Kestrel (Falco tinnunculus) J. Avian Med. Surg. 2015;29:336–339. doi: 10.1647/2014-052. [DOI] [PubMed] [Google Scholar]
- 52.Lamb S., Reavill D., Wojcieszyn J., Sitinas N. Osteosarcoma of the tibiotarsus with possible pulmonary metastasis in a ring-necked dove (Streptopelia risoria) J. Avian Med. Surg. 2014;28:50–56. doi: 10.1647/2012-064. [DOI] [PubMed] [Google Scholar]
- 53.Sladakovic I., Sangster C.R., Allan G.S., Portas T.J., Howlett C.R., Blas-Machado U. Calvarial Osteosarcoma with Cerebral Compression in a Free-Ranging Powerful Owl (Ninox strenua) J. Zoo Wildl. Med. 2017;48:208–212. doi: 10.1638/2013-0285.1. [DOI] [PubMed] [Google Scholar]
- 54.Manera M., Biavati S. Branchial osteogenetic neoplasm in barbel Barbus barbus plebejus. Dis Aquat Organ. 1999;37:231–236. doi: 10.3354/dao037231. [DOI] [PubMed] [Google Scholar]
- 55.Rahmati-Holasoo H., Shokrpoor S., Masoudifard M., Davudypoor S., Vaseghi M. Telangiectatic osteosarcoma and renal adenocarcinoma in an Oscar (Astronotus ocellatus, Agassiz): Diagnostic imaging and immunohistochemical study. J. Fish. Dis. 2018;41:1165–1172. doi: 10.1111/jfd.12788. [DOI] [PubMed] [Google Scholar]
- 56.Cowan M.L., Monks D.J., Raidal S.R. Osteosarcoma in a woma python (Aspidites ramsayi) Aust. Vet. J. 2011;89:520–523. doi: 10.1111/j.1751-0813.2011.00853.x. [DOI] [PubMed] [Google Scholar]
- 57.Needle D.M., McKnight C.A., Kiupel M. Chondroblastic osteosarcoma in two related spiny-tailed monitor lizards (Varanus acanthurus) J. Exotic Pet. Med. 2013;22:265–269. doi: 10.1053/j.jepm.2013.08.013. [DOI] [Google Scholar]
- 58.Rothschild B.M., Tanke D.H., Helbling M., 2nd, Martin L.D. Epidemiologic study of tumors in dinosaurs. Naturwissenschaften. 2003;90:495–500. doi: 10.1007/s00114-003-0473-9. [DOI] [PubMed] [Google Scholar]
- 59.Haridy Y., Witzmann F., Asbach P., Schoch R.R., Frobisch N., Rothschild B.M. Triassic Cancer-Osteosarcoma in a 240-Million-Year-Old Stem-Turtle. JAMA Oncol. 2019 doi: 10.1001/jamaoncol.2018.6766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gubin Iu M., Petrovichev N.N., Solov’ev Iu N., Kochergina N.V., Luk’ianchenko A.B., Markov S.M. Cranial bone neoplasm in early triassic amphibia. Vopr. Onkol. 2001;47:449–455. [PubMed] [Google Scholar]
- 61.Leeper H., Viall A., Ruaux C., Bracha S. Preliminary evaluation of serum total cholesterol concentrations in dogs with osteosarcoma. J. Small Anim. Pract. 2017;58:562–569. doi: 10.1111/jsap.12702. [DOI] [PubMed] [Google Scholar]
- 62.Aljubran A.H., Griffin A., Pintilie M., Blackstein M. Osteosarcoma in adolescents and adults: Survival analysis with and without lung metastases. Ann. Oncol. 2009;20:1136–1141. doi: 10.1093/annonc/mdn731. [DOI] [PubMed] [Google Scholar]
- 63.Kirpensteijn J., Kik M., Rutteman G.R., Teske E. Prognostic significance of a new histologic grading system for canine osteosarcoma. Vet. Path. 2002;39:240–246. doi: 10.1354/vp.39-2-240. [DOI] [PubMed] [Google Scholar]
- 64.Wolke R.E., Nielsen S.W. Site incidence of canine osteosarcoma. J. Small Anim. Pract. 1966;7:489–492. doi: 10.1111/j.1748-5827.1966.tb04475.x. [DOI] [PubMed] [Google Scholar]
- 65.Duffy D., Selmic L.E., Kendall A.R., Powers B.E. Outcome following treatment of soft tissue and visceral extraskeletal osteosarcoma in 33 dogs: 2008–2013. Vet. Comp. Oncol. 2017;15:46–54. doi: 10.1111/vco.12141. [DOI] [PubMed] [Google Scholar]
- 66.Fiegen A.P., Tjarks B.J., Jassim A.D. Primary Cutaneous Osteosarcoma. SD Med. 2018;71:164–166. [PubMed] [Google Scholar]
- 67.Kuntz C.A., Dernell W.S., Powers B.E., Withrow S. Extraskeletal osteosarcomas in dogs: 14 cases. J. Am. Anim. Hosp. Assoc. 1998;34:26–30. doi: 10.5326/15473317-34-1-26. [DOI] [PubMed] [Google Scholar]
- 68.Langenbach A., Anderson M.A., Dambach D.M., Sorenmo K.U., Shofer F.D. Extraskeletal osteosarcomas in dogs: A retrospective study of 169 cases (1986–1996) J. Am. Anim. Hosp. Assoc. 1998;34:113–120. doi: 10.5326/15473317-34-2-113. [DOI] [PubMed] [Google Scholar]
- 69.Llamas-Velasco M., Rutten A., Requena L., Mentzel T. Primary cutaneous osteosarcoma of the skin: A report of 2 cases with emphasis on the differential diagnoses. Am. J. Dermatopathol. 2013;35:e106–e113. doi: 10.1097/DAD.0b013e31827f0a6f. [DOI] [PubMed] [Google Scholar]
- 70.Jiang L., Luan L., Yun H., Hou Y., Shi H. Extraosseous Osteosarcoma of the Liver Demonstrated on 18F-FDG PET/CT Imaging. Clin. Nucl. Med. 2016;41:650–653. doi: 10.1097/RLU.0000000000001210. [DOI] [PubMed] [Google Scholar]
- 71.Tamang T.G., Shuster M., Chandra A.B. Primary Hepatic Osteosarcoma: A Rare Cause of Primary Liver Tumor. Clin. Med. Insights Case Rep. 2016;9:31–33. doi: 10.4137/CCRep.S38384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Dhumeaux M.P., Haudiquet P.R. Primary pulmonary osteosarcoma treated by thoracoscopy-assisted lung resection in a dog. Can. Vet. J. 2009;50:755–758. [PMC free article] [PubMed] [Google Scholar]
- 73.Karfis E.A., Karaiskos T., Cheva A., Drossos G.E. Primary extraosseous osteosarcoma of the lung. Acta Oncol. 2010;49:114–116. doi: 10.3109/02841860902953864. [DOI] [PubMed] [Google Scholar]
- 74.Wajstaub S., Bezjak A., Howarth D., King M.H., Catton C.N. A radio-sensitive primary osteosarcoma in the lung. Int. J. Clin. Oncol. 2011;16:67–70. doi: 10.1007/s10147-010-0113-2. [DOI] [PubMed] [Google Scholar]
- 75.Patnaik A.K. Canine extraskeletal osteosarcoma and chondrosarcoma: A clinicopathologic study of 14 cases. Vet. Pathol. 1990;27:46–55. doi: 10.1177/030098589002700107. [DOI] [PubMed] [Google Scholar]
- 76.Hanahan D., Weinberg R.A. Hallmarks of cancer: The next generation. Cell. 2011;144:646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 77.Tomasetti C., Vogelstein B. Cancer etiology. Variation in cancer risk among tissues can be explained by the number of stem cell divisions. Science. 2015;347:78–81. doi: 10.1126/science.1260825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Tomasetti C., Li L., Vogelstein B. Stem cell divisions, somatic mutations, cancer etiology, and cancer prevention. Science. 2017;355:1330–1334. doi: 10.1126/science.aaf9011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Troisi R., Masters M.N., Joshipura K., Douglass C., Cole B.F., Hoover R.N. Perinatal factors, growth and development, and osteosarcoma risk. Br. J. Cancer. 2006;95:1603–1607. doi: 10.1038/sj.bjc.6603474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Clarke B.L., Khosla S. Androgens and bone. Steroids. 2009;74:296–305. doi: 10.1016/j.steroids.2008.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Emons J., Chagin A.S., Savendahl L., Karperien M., Wit J.M. Mechanisms of growth plate maturation and epiphyseal fusion. Horm Res. Paediatr. 2011;75:383–391. doi: 10.1159/000327788. [DOI] [PubMed] [Google Scholar]
- 82.Kent M.S., Burton J.H., Dank G., Bannasch D.L., Rebhun R.B. Association of cancer-related mortality, age and gonadectomy in golden retriever dogs at a veterinary academic center (1989–2016) PLoS ONE. 2018;13:e0192578. doi: 10.1371/journal.pone.0192578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Hoffman J.M., Creevy K.E., Promislow D.E. Reproductive capability is associated with lifespan and cause of death in companion dogs. PLoS ONE. 2013;8:e61082. doi: 10.1371/journal.pone.0061082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Cooley D.M., Beranek B.C., Schlittler D.L., Glickman N.W., Glickman L.T., Waters D.J. Endogenous gonadal hormone exposure and bone sarcoma risk. Cancer Epidemiol. Biomark. Prev. 2002;11:1434–1440. [PubMed] [Google Scholar]
- 85.Lefebvre S.L., Yang M., Wang M., Elliott D.A., Buff P.R., Lund E.M. Effect of age at gonadectomy on the probability of dogs becoming overweight. J. Am. Vet. Med. Assoc. 2013;243:236–243. doi: 10.2460/javma.243.2.236. [DOI] [PubMed] [Google Scholar]
- 86.Salmeri K.R., Bloomberg M.S., Scruggs S.L., Shille V. Gonadectomy in immature dogs: Effects on skeletal, physical, and behavioral development. J. Am. Vet. Med. Assoc. 1991;198:1193–1203. [PubMed] [Google Scholar]
- 87.Root M.V., Johnston S.D., Olson P.N. The effect of prepuberal and postpuberal gonadectomy on radial physeal closure in male and female domestic cats. Vet. Radiol. Ultrasound. 1997;38:42–47. doi: 10.1111/j.1740-8261.1997.tb01601.x. [DOI] [PubMed] [Google Scholar]
- 88.Tjalma R.A. Canine bone sarcoma: Estimation of relative risk as a function of body size. J. Natl. Cancer Inst. 1966;36:1137–1150. [PubMed] [Google Scholar]
- 89.Gruntzig K., Graf R., Boo G., Guscetti F., Hassig M., Axhausen K.W., Fabrikant S., Welle M., Meier D., Folkers G., et al. Swiss Canine Cancer Registry 1955–2008: Occurrence of the Most Common Tumour Diagnoses and Influence of Age, Breed, Body Size, Sex and Neutering Status on Tumour Development. J. Comp. Pathol. 2016;155:156–170. doi: 10.1016/j.jcpa.2016.05.011. [DOI] [PubMed] [Google Scholar]
- 90.Withrow S.J., Powers B.E., Straw R.C., Wilkins R.M. Comparative aspects of osteosarcoma. Dog versus man. Clin. Orthop. Relat. Res. 1991;270:159–168. [PubMed] [Google Scholar]
- 91.Endicott A.A., Morimoto L.M., Kline C.N., Wiemels J.L., Metayer C., Walsh K.M. Perinatal factors associated with clinical presentation of osteosarcoma in children and adolescents. Pediatr. Blood Cancer. 2017;64 doi: 10.1002/pbc.26349. [DOI] [PubMed] [Google Scholar]
- 92.Diessner B.J., Spector L.G. Birthweight and site of osteosarcoma development. Pediatr. Blood Cancer. 2017;64 doi: 10.1002/pbc.26443. [DOI] [PubMed] [Google Scholar]
- 93.Arora R.S., Kontopantelis E., Alston R.D., Eden T.O., Geraci M., Birch J.M. Relationship between height at diagnosis and bone tumours in young people: A meta-analysis. Cancer Causes Control. 2011;22:681–688. doi: 10.1007/s10552-011-9740-9. [DOI] [PubMed] [Google Scholar]
- 94.Jesus-Garcia R., Seixas M.T., Costa S.R., Petrilli A.S., Laredo Filho J. Epiphyseal plate involvement in osteosarcoma. Clin. Orthop. Relat. Res. 2000;373:32–38. doi: 10.1097/00003086-200004000-00006. [DOI] [PubMed] [Google Scholar]
- 95.Kirpensteijn J., Timmermans-Sprang E.P., van Garderen E., Rutteman G.R., Lantinga-van Leeuwen I.S., Mol J.A. Growth hormone gene expression in canine normal growth plates and spontaneous osteosarcoma. Mol. Cell. Endocrinol. 2002;197:179–185. doi: 10.1016/S0303-7207(02)00269-1. [DOI] [PubMed] [Google Scholar]
- 96.Larsen J. Feeding large-breed puppies. Compend. Contin. Educ. Vet. 2010;32:E1–E4. [PubMed] [Google Scholar]
- 97.Gilley R.S., Hiebert E., Clapp K., Bartl-Wilson L., Nappier M., Werre S., Barnes K. Long-term Formation of Aggressive Bony Lesions in Dogs with Mid-Diaphyseal Fractures Stabilized with Metallic Plates: Incidence in a Tertiary Referral Hospital Population. Front. Vet. Sci. 2017;4:3. doi: 10.3389/fvets.2017.00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Arthur E.G., Arthur G.L., Keeler M.R., Bryan J.N. Risk of Osteosarcoma in Dogs After Open Fracture Fixation. Vet. Surg. 2016;45:30–35. doi: 10.1111/vsu.12416. [DOI] [PubMed] [Google Scholar]
- 99.Atherton M.J., Arthurs G. Osteosarcoma of the tibia 6 years after tibial plateau leveling osteotomy. J. Am. Anim. Hosp. Assoc. 2012;48:188–193. doi: 10.5326/JAAHA-MS-5730. [DOI] [PubMed] [Google Scholar]
- 100.Burton A.G., Johnson E.G., Vernau W., Murphy B.G. Implant-associated neoplasia in dogs: 16 cases (1983–2013) J. Am. Vet. Med. Assoc. 2015;247:778–785. doi: 10.2460/javma.247.7.778. [DOI] [PubMed] [Google Scholar]
- 101.Murphy S.T., Parker R.B., Woodard J.C. Osteosarcoma following total hip arthroplasty in a dog. J. Small Anim. Pract. 1997;38:263–267. doi: 10.1111/j.1748-5827.1997.tb03365.x. [DOI] [PubMed] [Google Scholar]
- 102.Sartor A.J., Ryan S.D., Sellmeyer T., Withrow S.J., Selmic L.E. Bi-institutional retrospective cohort study evaluating the incidence of osteosarcoma following tibial plateau levelling osteotomy (2000–2009) Vet. Comp. Orthop. Traumatol. 2014;27:339–345. doi: 10.3415/VCOT-14-01-0006. [DOI] [PubMed] [Google Scholar]
- 103.Selmic L.E., Ryan S.D., Boston S.E., Liptak J.M., Culp W.T., Sartor A.J., Prpich C.Y., Withrow S.J. Osteosarcoma following tibial plateau leveling osteotomy in dogs: 29 cases (1997–2011) J. Am. Vet. Med. Assoc. 2014;244:1053–1059. doi: 10.2460/javma.244.9.1053. [DOI] [PubMed] [Google Scholar]
- 104.Karlsson E.K., Sigurdsson S., Ivansson E., Thomas R., Elvers I., Wright J., Howald C., Tonomura N., Perloski M., Swofford R., et al. Genome-wide analyses implicate 33 loci in heritable dog osteosarcoma, including regulatory variants near CDKN2A/B. Genome Biol. 2013;14:R132. doi: 10.1186/gb-2013-14-12-r132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Duffy M.E., Anderson C.L., Choy K., Fidel J.L. Metronomic administration of lomustine following palliative radiation therapy for appendicular osteosarcoma in dogs. Can. Vet. J. 2018;59:136–142. [PMC free article] [PubMed] [Google Scholar]
- 106.Slovak J.E., Kieves N.R., Haynes J. Extraskeletal Osteosarcoma Induced by a Foreign Body Granuloma. J. Am. Anim. Hosp. Assoc. 2015;51:315–319. doi: 10.5326/JAAHA-MS-6224. [DOI] [PubMed] [Google Scholar]
- 107.Selmic L.E., Griffin L.R., Rector M.H., Lafferty M., Pool R., Ehrhart N.P. Treatment of extraskeletal osteosarcoma at a previous injection site resulting in prolonged survival in 1 dog. Can. Vet. J. 2016;57:950–954. [PMC free article] [PubMed] [Google Scholar]
- 108.Thrasher J.P., Barrett R.B., Tyler D.E. Osteogenic carcinoma of the canine esophagus (Spirocerca lupi?) Vet. Med. Small Anim. Clin. 1968;63:333–336. [PubMed] [Google Scholar]
- 109.Thrasher J.P., Ichinose H., Pitot H.C. Osteogenic sarcoma of the canine esophagus associated with spirocerca lupi infection. Am. J. Vet. Res. 1963;24:808–818. [PubMed] [Google Scholar]
- 110.Ranen E., Lavy E., Aizenberg I., Perl S., Harrus S. Spirocercosis-associated esophageal sarcomas in dogs. A retrospective study of 17 cases (1997–2003) Vet. Parasitol. 2004;119:209–221. doi: 10.1016/j.vetpar.2003.10.023. [DOI] [PubMed] [Google Scholar]
- 111.Yas E., Kelmer G., Shipov A., Ben-Oz J., Segev G. Successful transendoscopic oesophageal mass ablation in two dogs with Spirocerca lupi associated oesophageal sarcoma. J. Small Anim. Pract. 2013;54:495–498. doi: 10.1111/jsap.12076. [DOI] [PubMed] [Google Scholar]
- 112.Lee M.A., Yi J., Chae J.M. Cutaneous osteosarcoma arising from a burn scar. Skelet. Radiol. 2017;46:547–551. doi: 10.1007/s00256-016-2565-6. [DOI] [PubMed] [Google Scholar]
- 113.Park S.G., Song J.Y., Song I.G., Kim M.S., Shin B.S. Cutaneous extraskeletal osteosarcoma on the scar of a previous bone graft. Ann. Dermatol. 2011;23:S160–S164. doi: 10.5021/ad.2011.23.S2.S160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Santos-Juanes J., Galache C., Miralles M., Curto J.R., Sanchez del Rio J., Soto J. Primary cutaneous extraskeletal osteosarcoma under a previous electrodessicated actinic keratosis. J. Am. Acad. Dermatol. 2004;51:S166–S168. doi: 10.1016/j.jaad.2004.04.021. [DOI] [PubMed] [Google Scholar]
- 115.Savage S.A., Mirabello L. Using epidemiology and genomics to understand osteosarcoma etiology. Sarcoma. 2011;2011:548151. doi: 10.1155/2011/548151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Smida J., Xu H., Zhang Y., Baumhoer D., Ribi S., Kovac M., von Luettichau I., Bielack S., O’Leary V.B., Leib-Mosch C., et al. Genome-wide analysis of somatic copy number alterations and chromosomal breakages in osteosarcoma. Int. J. Cancer. 2017;141:816–828. doi: 10.1002/ijc.30778. [DOI] [PubMed] [Google Scholar]
- 117.Wedekind M.F., Wagner L.M., Cripe T.P. Immunotherapy for osteosarcoma: Where do we go from here? Pediatr. Blood Cancer. 2018;65:e27227. doi: 10.1002/pbc.27227. [DOI] [PubMed] [Google Scholar]
- 118.Rickel K., Fang F., Tao J. Molecular genetics of osteosarcoma. Bone. 2017;102:69–79. doi: 10.1016/j.bone.2016.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Lorenz S., Baroy T., Sun J., Nome T., Vodak D., Bryne J.C., Hakelien A.M., Fernandez-Cuesta L., Mohlendick B., Rieder H., et al. Unscrambling the genomic chaos of osteosarcoma reveals extensive transcript fusion, recurrent rearrangements and frequent novel TP53 aberrations. Oncotarget. 2016;7:5273–5288. doi: 10.18632/oncotarget.6567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Ribi S., Baumhoer D., Lee K., Edison, Teo A.S., Madan B., Zhang K., Kohlmann W.K., Yao F., Lee W.H., et al. TP53 intron 1 hotspot rearrangements are specific to sporadic osteosarcoma and can cause Li-Fraumeni syndrome. Oncotarget. 2015;6:7727–7740. doi: 10.18632/oncotarget.3115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Sakthikumar S., Elvers I., Kim J., Arendt M.L., Thomas R., Turner-Maier J., Swofford R., Johnson J., Schumacher S.E., Alfoldi J., et al. SETD2 Is Recurrently Mutated in Whole-Exome Sequenced Canine Osteosarcoma. Cancer Res. 2018;78:3421–3431. doi: 10.1158/0008-5472.CAN-17-3558. [DOI] [PubMed] [Google Scholar]
- 122.Fahey C.C., Davis I.J. SETting the Stage for Cancer Development: SETD2 and the Consequences of Lost Methylation. Cold Spring Harb. Perspect. Med. 2017;7 doi: 10.1101/cshperspect.a026468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Huang K.K., McPherson J.R., Tay S.T., Das K., Tan I.B., Ng C.C., Chia N.Y., Zhang S.L., Myint S.S., Hu L., et al. SETD2 histone modifier loss in aggressive GI stromal tumours. Gut. 2016;65:1960–1972. doi: 10.1136/gutjnl-2015-309482. [DOI] [PubMed] [Google Scholar]
- 124.Li J., Kluiver J., Osinga J., Westers H., van Werkhoven M.B., Seelen M.A., Sijmons R.H., van den Berg A., Kok K. Functional Studies on Primary Tubular Epithelial Cells Indicate a Tumor Suppressor Role of SETD2 in Clear Cell Renal Cell Carcinoma. Neoplasia. 2016;18:339–346. doi: 10.1016/j.neo.2016.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Zhu X., He F., Zeng H., Ling S., Chen A., Wang Y., Yan X., Wei W., Pang Y., Cheng H., et al. Identification of functional cooperative mutations of SETD2 in human acute leukemia. Nat. Genet. 2014;46:287–293. doi: 10.1038/ng.2894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Behjati S., Tarpey P.S., Haase K., Ye H., Young M.D., Alexandrov L.B., Farndon S.J., Collord G., Wedge D.C., Martincorena I., et al. Recurrent mutation of IGF signalling genes and distinct patterns of genomic rearrangement in osteosarcoma. Nat. Commun. 2017;8:15936. doi: 10.1038/ncomms15936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Carnevale A., Lieberman E., Cardenas R. Li-Fraumeni syndrome in pediatric patients with soft tissue sarcoma or osteosarcoma. Arch. Med. Res. 1997;28:383–386. [PubMed] [Google Scholar]
- 128.Garcia Garcia A., Barros F., Bouzas M.L., Penaranda J.M. Li-Fraumeni syndrome and osteosarcoma of the maxilla. J. Oral. Maxillofac. Surg. 1998;56:1106–1109. doi: 10.1016/S0278-2391(98)90267-1. [DOI] [PubMed] [Google Scholar]
- 129.Porter D.E., Holden S.T., Steel C.M., Cohen B.B., Wallace M.R., Reid R. A significant proportion of patients with osteosarcoma may belong to Li-Fraumeni cancer families. J. Bone Joint Surg. Br. 1992;74:883–886. doi: 10.1302/0301-620X.74B6.1447251. [DOI] [PubMed] [Google Scholar]
- 130.Yoshida G.J., Fuchimoto Y., Osumi T., Shimada H., Hosaka S., Morioka H., Mukai M., Masugi Y., Sakamoto M., Kuroda T. Li-Fraumeni syndrome with simultaneous osteosarcoma and liver cancer: Increased expression of a CD44 variant isoform after chemotherapy. BMC Cancer. 2012;12:444. doi: 10.1186/1471-2407-12-444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Pratt C.B., Michalkiewicz E.N., Rao B.N., Lipson M., Cain A., Kaste S. Multifocal osteosarcoma following retinoblastoma. Ophthalmic Genet. 1999;20:23–29. doi: 10.1076/opge.20.1.23.2296. [DOI] [PubMed] [Google Scholar]
- 132.Potepan P., Luksch R., Sozzi G., Testi A., Laffranchi A., Danesini G.M., Parafioriti A., Giardini R., Spagnoli I. Multifocal osteosarcoma as second tumor after childhood retinoblastoma. Skelet. Radiol. 1999;28:415–421. doi: 10.1007/s002560050540. [DOI] [PubMed] [Google Scholar]
- 133.Agarwal G., Kochar H.S., Julka P.K., Bahadur S. Osteosarcoma as a second malignant disease in a case of bilateral retinoblastoma. Indian J. Otolaryngol. Head Neck Surg. 2011;63:115–117. doi: 10.1007/s12070-011-0254-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Chauveinc L., Mosseri V., Quintana E., Desjardins L., Schlienger P., Doz F., Dutrillaux B. Osteosarcoma following retinoblastoma: Age at onset and latency period. Ophthalmic Genet. 2001;22:77–88. doi: 10.1076/opge.22.2.77.2228. [DOI] [PubMed] [Google Scholar]
- 135.Fujiwara T., Fujiwara M., Numoto K., Ogura K., Yoshida A., Yonemoto T., Suzuki S., Kawai A. Second primary osteosarcomas in patients with retinoblastoma. Jpn. J. Clin. Oncol. 2015;45:1139–1145. doi: 10.1093/jjco/hyv140. [DOI] [PubMed] [Google Scholar]
- 136.Lee J.A., Choi S.Y., Kang H.J., Lee J.W., Kim H., Kim J.H., Sung K.W., Shin H.Y., Ahn H.S., Park K.D. Treatment outcome of osteosarcoma after bilateral retinoblastoma: A retrospective study of eight cases. Br. J. Ophthalmol. 2014;98:1355–1359. doi: 10.1136/bjophthalmol-2014-305116. [DOI] [PubMed] [Google Scholar]
- 137.MacCarthy A., Bayne A.M., Brownbill P.A., Bunch K.J., Diggens N.L., Draper G.J., Hawkins M.M., Jenkinson H.C., Kingston J.E., Stiller C.A., et al. Second and subsequent tumours among 1927 retinoblastoma patients diagnosed in Britain 1951–2004. Br. J. Cancer. 2013;108:2455–2463. doi: 10.1038/bjc.2013.228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Okada K., Hasegawa T., Tateishi U., Itoi E. Second primary osteosarcoma with rosette-like structure in a patient with retinoblastoma. Virchows Arch. 2004;445:421–424. doi: 10.1007/s00428-004-1082-5. [DOI] [PubMed] [Google Scholar]
- 139.Stine K.C., Saylors R.L., Saccente S., Becton D.L. Long-term survival in osteosarcoma patients following retinoblastoma using doxorubicin, cisplatin, and methotrexate. Med. Pediatr. Oncol. 2003;41:77–78. doi: 10.1002/mpo.10311. [DOI] [PubMed] [Google Scholar]
- 140.Wong F.L., Boice J.D., Jr., Abramson D.H., Tarone R.E., Kleinerman R.A., Stovall M., Goldman M.B., Seddon J.M., Tarbell N., Fraumeni J.F., Jr., et al. Cancer incidence after retinoblastoma. Radiation dose and sarcoma risk. JAMA. 1997;278:1262–1267. doi: 10.1001/jama.1997.03550150066037. [DOI] [PubMed] [Google Scholar]
- 141.Hansen M.F., Nellissery M.J., Bhatia P. Common mechanisms of osteosarcoma and Paget’s disease. J. Bone Miner. Res. 1999;14:39–44. doi: 10.1002/jbmr.5650140209. [DOI] [PubMed] [Google Scholar]
- 142.Dray M.S., Miller M.V. Paget’s osteosarcoma and post-radiation osteosarcoma: Secondary osteosarcoma at Middlemore Hospital, New Zealand. Pathology. 2008;40:604–610. doi: 10.1080/00313020802320663. [DOI] [PubMed] [Google Scholar]
- 143.McNairn J.D., Damron T.A., Landas S.K., Ambrose J.L., Shrimpton A.E. Inheritance of osteosarcoma and Paget’s disease of bone: A familial loss of heterozygosity study. J. Mol. Diagn. 2001;3:171–177. doi: 10.1016/S1525-1578(10)60669-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Brenton D.P., Isenberg D.A., Bertram J. Osteosarcoma complicating familial Paget’s disease. Postgrad. Med. J. 1980;56:238–243. doi: 10.1136/pgmj.56.654.238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Frassica F.J., Sim F.H., Frassica D.A., Wold L.E. Survival and management considerations in postirradiation osteosarcoma and Paget’s osteosarcoma. Clin. Orthop. Relat. Res. 1991;270:120–127. [PubMed] [Google Scholar]
- 146.Olivier M., Goldgar D.E., Sodha N., Ohgaki H., Kleihues P., Hainaut P., Eeles R.A. Li-Fraumeni and related syndromes: Correlation between tumor type, family structure, and TP53 genotype. Cancer Res. 2003;63:6643–6650. [PubMed] [Google Scholar]
- 147.Mai P.L., Best A.F., Peters J.A., DeCastro R.M., Khincha P.P., Loud J.T., Bremer R.C., Rosenberg P.S., Savage S.A. Risks of first and subsequent cancers among TP53 mutation carriers in the National Cancer Institute Li-Fraumeni syndrome cohort. Cancer. 2016;122:3673–3681. doi: 10.1002/cncr.30248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Mirabello L., Yeager M., Mai P.L., Gastier-Foster J.M., Gorlick R., Khanna C., Patino-Garcia A., Sierrasesumaga L., Lecanda F., Andrulis I.L., et al. Germline TP53 variants and susceptibility to osteosarcoma. J. Natl. Cancer Inst. 2015;107 doi: 10.1093/jnci/djv101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Spector L., Lock I., Lane J., Sarver A., Krailo M., Nagarajan R., Pankratz N. Abstract A37: De novo and transmitted germline TP53 variation in pediatric osteosarcoma: A report from the Children’s Oncology Group. Cancer Res. 2016;76:A37. doi: 10.1158/1538-7445.Pedca15-a37. [DOI] [Google Scholar]
- 150.Kleinerman R.A., Tucker M.A., Tarone R.E., Abramson D.H., Seddon J.M., Stovall M., Li F.P., Fraumeni J.F., Jr. Risk of new cancers after radiotherapy in long-term survivors of retinoblastoma: An extended follow-up. J. Clin. Oncol. 2005;23:2272–2279. doi: 10.1200/JCO.2005.05.054. [DOI] [PubMed] [Google Scholar]
- 151.Chen X., Bahrami A., Pappo A., Easton J., Dalton J., Hedlund E., Ellison D., Shurtleff S., Wu G., Wei L., et al. Recurrent somatic structural variations contribute to tumorigenesis in pediatric osteosarcoma. Cell Rep. 2014;7:104–112. doi: 10.1016/j.celrep.2014.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Perry J.A., Kiezun A., Tonzi P., Van Allen E.M., Carter S.L., Baca S.C., Cowley G.S., Bhatt A.S., Rheinbay E., Pedamallu C.S., et al. Complementary genomic approaches highlight the PI3K/mTOR pathway as a common vulnerability in osteosarcoma. Proc. Natl. Acad. Sci. USA. 2014;111:E5564–E5573. doi: 10.1073/pnas.1419260111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Belchis D.A., Meece C.A., Benko F.A., Rogan P.K., Williams R.A., Gocke C.D. Loss of heterozygosity and microsatellite instability at the retinoblastoma locus in osteosarcomas. Diagn. Mol. Pathol. 1996;5:214–219. doi: 10.1097/00019606-199609000-00011. [DOI] [PubMed] [Google Scholar]
- 154.Benassi M.S., Molendini L., Gamberi G., Ragazzini P., Sollazzo M.R., Merli M., Asp J., Magagnoli G., Balladelli A., Bertoni F., et al. Alteration of pRb/p16/cdk4 regulation in human osteosarcoma. Int. J. Cancer. 1999;84:489–493. doi: 10.1002/(SICI)1097-0215(19991022)84:5<489::AID-IJC7>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- 155.Mirabello L., Yu K., Berndt S.I., Burdett L., Wang Z., Chowdhury S., Teshome K., Uzoka A., Hutchinson A., Grotmol T., et al. A comprehensive candidate gene approach identifies genetic variation associated with osteosarcoma. BMC Cancer. 2011;11:209. doi: 10.1186/1471-2407-11-209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Musselman J.R., Bergemann T.L., Ross J.A., Sklar C., Silverstein K.A., Langer E.K., Savage S.A., Nagarajan R., Krailo M., Malkin D., et al. Case-parent analysis of variation in pubertal hormone genes and pediatric osteosarcoma: A Children’s Oncology Group (COG) study. Int. J. Mol. Epidemiol. Genet. 2012;3:286–293. [PMC free article] [PubMed] [Google Scholar]
- 157.Savage S.A., Mirabello L., Wang Z., Gastier-Foster J.M., Gorlick R., Khanna C., Flanagan A.M., Tirabosco R., Andrulis I.L., Wunder J.S., et al. Genome-wide association study identifies two susceptibility loci for osteosarcoma. Nat. Genet. 2013;45:799–803. doi: 10.1038/ng.2645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Mirabello L., Koster R., Moriarity B.S., Spector L.G., Meltzer P.S., Gary J., Machiela M.J., Pankratz N., Panagiotou O.A., Largaespada D., et al. A Genome-Wide Scan Identifies Variants in NFIB Associated with Metastasis in Patients with Osteosarcoma. Cancer Discov. 2015;5:920–931. doi: 10.1158/2159-8290.CD-15-0125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Yang Y., Basu S., Mirabello L., Spector L., Zhang L. A Bayesian Gene-Based Genome-Wide Association Study Analysis of Osteosarcoma Trio Data Using a Hierarchically Structured Prior. Cancer Inform. 2018;17 doi: 10.1177/1176935118775103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Peto R., Roe F.J., Lee P.N., Levy L., Clack J. Cancer and ageing in mice and men. Br. J. Cancer. 1975;32:411–426. doi: 10.1038/bjc.1975.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Armitage P., Doll R. The age distribution of cancer and a multi-stage theory of carcinogenesis. Br. J. Cancer. 1954;8:1–12. doi: 10.1038/bjc.1954.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Abegglen L.M., Caulin A.F., Chan A., Lee K., Robinson R., Campbell M.S., Kiso W.K., Schmitt D.L., Waddell P.J., Bhaskara S., et al. Potential Mechanisms for Cancer Resistance in Elephants and Comparative Cellular Response to DNA Damage in Humans. JAMA. 2015;314:1850–1860. doi: 10.1001/jama.2015.13134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Campisi J., Robert L. Cell senescence: Role in aging and age-related diseases. Interdiscip. Top. Gerontol. 2014;39:45–61. doi: 10.1159/000358899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Gomes N.M., Ryder O.A., Houck M.L., Charter S.J., Walker W., Forsyth N.R., Austad S.N., Venditti C., Pagel M., Shay J.W., et al. Comparative biology of mammalian telomeres: Hypotheses on ancestral states and the roles of telomeres in longevity determination. Aging Cell. 2011;10:761–768. doi: 10.1111/j.1474-9726.2011.00718.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Valentijn L.J., Koster J., Zwijnenburg D.A., Hasselt N.E., van Sluis P., Volckmann R., van Noesel M.M., George R.E., Tytgat G.A., Molenaar J.J., et al. TERT rearrangements are frequent in neuroblastoma and identify aggressive tumors. Nat. Genet. 2015;47:1411–1414. doi: 10.1038/ng.3438. [DOI] [PubMed] [Google Scholar]
- 166.Telomeres Mendelian Randomization C., Haycock P.C., Burgess S., Nounu A., Zheng J., Okoli G.N., Bowden J., Wade K.H., Timpson N.J., Evans D.M., et al. Association Between Telomere Length and Risk of Cancer and Non-Neoplastic Diseases: A Mendelian Randomization Study. JAMA Oncol. 2017;3:636–651. doi: 10.1001/jamaoncol.2016.5945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Walsh K.M., Whitehead T.P., de Smith A.J., Smirnov I.V., Park M., Endicott A.A., Francis S.S., Codd V., Group E.C.T., Samani N.J., et al. Common genetic variants associated with telomere length confer risk for neuroblastoma and other childhood cancers. Carcinogenesis. 2016;37:576–582. doi: 10.1093/carcin/bgw037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Ferlay J., Soerjomataram I., Dikshit R., Eser S., Mathers C., Rebelo M., Parkin D.M., Forman D., Bray F. Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012. Int. J. Cancer. 2015;136:E359–E386. doi: 10.1002/ijc.29210. [DOI] [PubMed] [Google Scholar]
- 169.Calabrese P., Shibata D. A simple algebraic cancer equation: Calculating how cancers may arise with normal mutation rates. BMC Cancer. 2010;10:3. doi: 10.1186/1471-2407-10-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Sulak M., Fong L., Mika K., Chigurupati S., Yon L., Mongan N.P., Emes R.D., Lynch V.J. TP53 copy number expansion is associated with the evolution of increased body size and an enhanced DNA damage response in elephants. eLife. 2016;5 doi: 10.7554/eLife.11994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Vazquez J.M., Sulak M., Chigurupati S., Lynch V.J. A Zombie LIF Gene in Elephants Is Upregulated by TP53 to Induce Apoptosis in Response to DNA Damage. Cell Rep. 2018;24:1765–1776. doi: 10.1016/j.celrep.2018.07.042. [DOI] [PubMed] [Google Scholar]
- 172.Keane M., Semeiks J., Webb A.E., Li Y.I., Quesada V., Craig T., Madsen L.B., van Dam S., Brawand D., Marques P.I., et al. Insights into the evolution of longevity from the bowhead whale genome. Cell Rep. 2015;10:112–122. doi: 10.1016/j.celrep.2014.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Seluanov A., Chen Z., Hine C., Sasahara T.H., Ribeiro A.A., Catania K.C., Presgraves D.C., Gorbunova V. Telomerase activity coevolves with body mass not lifespan. Aging Cell. 2007;6:45–52. doi: 10.1111/j.1474-9726.2006.00262.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Seluanov A., Hine C., Azpurua J., Feigenson M., Bozzella M., Mao Z., Catania K.C., Gorbunova V. Hypersensitivity to contact inhibition provides a clue to cancer resistance of naked mole-rat. Proc. Natl. Acad. Sci. USA. 2009;106:19352–19357. doi: 10.1073/pnas.0905252106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Rangarajan A., Hong S.J., Gifford A., Weinberg R.A. Species- and cell type-specific requirements for cellular transformation. Cancer Cell. 2004;6:171–183. doi: 10.1016/j.ccr.2004.07.009. [DOI] [PubMed] [Google Scholar]
- 176.Phillips J.C., Stephenson B., Hauck M., Dillberger J. Heritability and segregation analysis of osteosarcoma in the Scottish deerhound. Genomics. 2007;90:354–363. doi: 10.1016/j.ygeno.2007.05.001. [DOI] [PubMed] [Google Scholar]