Abstract
Background
Timing and adequacy of peritoneal source control are the most important pillars in the management of patients with acute peritonitis. Therefore, early prognostic evaluation of acute peritonitis is paramount to assess the severity and establish a prompt and appropriate treatment. The objectives of this study were to identify clinical and laboratory predictors for in-hospital mortality in patients with acute peritonitis and to develop a warning score system, based on easily recognizable and assessable variables, globally accepted.
Methods
This worldwide multicentre observational study included 153 surgical departments across 56 countries over a 4-month study period between February 1, 2018, and May 31, 2018.
Results
A total of 3137 patients were included, with 1815 (57.9%) men and 1322 (42.1%) women, with a median age of 47 years (interquartile range [IQR] 28–66). The overall in-hospital mortality rate was 8.9%, with a median length of stay of 6 days (IQR 4–10). Using multivariable logistic regression, independent variables associated with in-hospital mortality were identified: age > 80 years, malignancy, severe cardiovascular disease, severe chronic kidney disease, respiratory rate ≥ 22 breaths/min, systolic blood pressure < 100 mmHg, AVPU responsiveness scale (voice and unresponsive), blood oxygen saturation level (SpO2) < 90% in air, platelet count < 50,000 cells/mm3, and lactate > 4 mmol/l. These variables were used to create the PIPAS Severity Score, a bedside early warning score for patients with acute peritonitis. The overall mortality was 2.9% for patients who had scores of 0–1, 22.7% for those who had scores of 2–3, 46.8% for those who had scores of 4–5, and 86.7% for those who have scores of 7–8.
Conclusions
The simple PIPAS Severity Score can be used on a global level and can help clinicians to identify patients at high risk for treatment failure and mortality.
Keywords: Acute peritonitis, Source control, Early warning score, Emergency surgery
Introduction
Peritonitis is an inflammation of the peritoneum. Depending on the underlying pathology, it can be infectious or sterile [1]. Infectious peritonitis is classified into primary peritonitis, secondary peritonitis, and tertiary peritonitis. Primary peritonitis is a diffuse bacterial infection (usually caused by a single organism) without loss of integrity of the gastrointestinal tract, typically seen in cirrhotic patients with ascites or in patients with a peritoneal dialysis catheter. It has a low incidence in surgical wards and is usually managed without any surgical intervention. Secondary peritonitis is an acute peritoneal infection resulting from loss of integrity of the gastrointestinal tract. Tertiary peritonitis is a recurrent infection of the peritoneal cavity that occurs > 48 h after apparently successful and adequate surgical source control of secondary peritonitis. Secondary peritonitis is the most common form of peritonitis. It is caused by perforation of the gastrointestinal tract (e.g. perforated duodenal ulcer) by direct invasion from infected intra-abdominal viscera (e.g. gangrenous appendicitis). It is an important cause of patient morbidity and is frequently associated with significant morbidity and mortality rates [2], despite development in diagnosis and management.
Timing and adequacy of peritoneal source control are the most important pillars in the management of patients with acute peritonitis, being determinant to control or interrupt the septic process [2, 3].
Many peritonitis-specific scoring systems have been designed and used to grade the severity of acute peritonitis [4–7].
Patients with acute peritonitis are generally classified into low risk and high risk. “High risk” is generally intended to describe patients at high risk for treatment failure and mortality [6]. In high-risk patients, the increased mortality associated with inappropriate management cannot be reversed by subsequent modifications. Therefore, early prognostic evaluation of acute peritonitis is important to assess the severity and decide the aggressiveness of treatment. Moreover, in emergency departments of limited-resource hospitals, diagnosis of acute peritonitis is mainly clinical, and supported only by basic laboratory tests [8], making some scoring systems impractical to a large part of the world’s population.
The objectives of this study were (a) to identify all clinical and laboratory predictors for in-hospital mortality in patients with acute peritonitis and (b) to develop a warning score system, based on easily recognizable and assessable variables, globally accepted, so as to provide the clinician with a simple tool to identify patients at high risk for treatment failure and mortality.
Methods
Study population
This worldwide multicentre observational study was performed across 153 surgical departments from 56 countries over a 4-month study period (February 1, 2018 – May 31, 2018). All consecutive patients admitted to surgical departments with a clinical diagnosis of acute peritonitis were included in the study. The following data were collected: age and gender; presence of comorbidities, namely primary or secondary immunodeficiency (chronic treatment with glucocorticoids, with immunosuppressive agents or chemotherapy, and patients with lymphatic diseases or with virus-related immunosuppression; solid or haematopoietic and lymphoid malignancy; severe cardiovascular disease (medical history of ischemic heart disease, history of heart failure, severe valvular disease [9]); diabetes with or without organ dysfunction; severe chronic kidney disease; and severe chronic obstructive pulmonary disease (COPD) [10]. Clinical findings were recorded at admission: abdominal findings (localized or diffuse abdominal pain, localized or diffuse abdominal rigidity); core temperature (defining fever as core temperature > 38.0 °C, and hypothermia as core temperature < 36.0 °C); heart rate (bpm); respiratory rate (breaths/min); systolic blood pressure (mmHg); alert/verbal/painful/unresponsive (AVPU) responsiveness scale [11]; and numerical rating scale (NRS) [12].
The following laboratory findings were also collected: blood oxygen saturation level (SpO2) (%) in air, white blood count (WBC) (cells/mm3), platelet count (cells/ mm3), international normalised ratio (INR), C-reactive protein (CRP) (mg/l), procalcitonin (ng/ml), and lactate (mmol/l). Quick Sequential Organ Failure Assessment (qSOFA) score upon admission was calculated [13]. The modality and setting of acquisition of radiological investigations (abdominal x-ray, ultrasound [US], computer tomography [CT] scan) was specified. Peritonitis was classified as community-acquired or healthcare-acquired. Peritonitis was considered healthcare-associated in patients hospitalized for at least 48 h during the previous 90 days; or those residing in skilled nursing or long-term care facility during the previous 30 days; or those who have received intravenous therapy, wound care, or renal replacement therapy within the preceding 30 days. Source of infection, extent of peritonitis (generalized or localized peritonitis/abscess), source control (conservative treatment, operative or non-operative interventional procedures), and its adequacy were noted. The adequacy of the intervention was defined by the establishment of the cause of peritonitis and the ability to control the source of the peritonitis [14]. Delay in the initial intervention (> 24 h of admission), and adequacy of antimicrobial therapy (if guided by antibiograms performed) were assessed. Reoperation during the hospital stay, re-laparotomy strategy (open abdomen, planned re-laparotomy, on demand re-laparotomy) and its timing, immediate (within 72 h) infectious post-operative complications, delayed infectious post-operative complications, length of hospital stay (LOS), and in-hospital mortality were determined. All patients were monitored until they were discharged or transferred to another facility.
Study design
The centre coordinator of each participating medical institution collected data in an online case report database. Differences in local surgical practice of each centre were respected, and no changes were impinged on local management strategies. Each centre followed its own ethical standards and local rules. The study was monitored by a coordinating centre, which processed and verified any missing or unclear data submitted to the central database. The study did not attempt to change or modify the clinical practice of the participating physicians. Accordingly, informed consent was not needed and each hospital followed their ethical rules for formal research including an ethical approval if approval was needed. The data were completely anonymised. The study protocol was approved by the board of the World Society of Emergency Surgery (WSES), and the study was conducted under its supervision. The board of the WSES granted the proper ethical conduct of the study. The study met and conformed to the standards outlined in the Declaration of Helsinki and Good Epidemiological Practices.
Statistical analysis
The data were analysed in absolute frequency and percentage, in the case of qualitative variables. Quantitative variables were analysed as medians and interquartile range (IQR). Univariate analyses were performed to study the association between risk factors and in-hospital mortality using a chi-square test, or a Fisher’s exact test, if the expected value of a cell was < 5. All tests were two-sided, and p values of 0.05 were considered statistically significant.
To identify independent risk factors associated with in-hospital mortality, a multivariable logistic regression analysis was performed selecting independent variables that had p value < 0.05 in the univariate analysis. Then, a backward selection method was applied to select a limited number of variables, using a likelihood ratio test for comparing the nested models (α = 0.05). At each step, we removed from the previous model the variable with the highest p value greater than α, checking the fit of the obtained model, and then stopping when all p values were less than α. Then, we checked the global performance of the test calculating the area under the receiver operating characteristic (ROC) curve. All statistical analyses were performed using the Stata 11 software package (StataCorp, College Station, TX).
Results
Patients and diagnosis
During the study, 3137 patients from 153 hospitals worldwide were collected; these included 1815 (57.9%) men and 1322 (42.1%) women, with a median age of 47 years (IQR, 28–66). Considering World Health Organization regions, 1981 (63.1%) patients were collected in countries belonging to European region, 396 (12.6%) patients were from the African region, 275 (8.8%) from the region of the Americas, 239 (7.6%) from the South-East Asia region, 173 (5.5%) from the Eastern-Mediterranean region, and 73 (2.3%) from the Western Pacific region.
Forty-one (1.3%) patients were asymptomatic, while 990 (31.6%) reported localized abdominal pain, 665 (21.2%) localized abdominal rigidity, 797 (25.4%) diffuse abdominal pain, and 592 (18.9%) diffuse abdominal rigidity. In 52 (1.7%) patients, abdominal findings were not reported. Three hundred and thirty (10.5%) patients underwent abdominal x-ray, 756 (24.1%) patients had an US, 1016 (32.4%) abdominal CT scan, 189 (6.0%) patients had both abdominal x-ray and US, 76 (2.4%) had both abdominal x-ray scan and CT, 199 (6.3%) patients had both CT scan and US, 93 (3.0%) patients underwent abdominal x-ray scan, US and CT, and 445 (14.3%) patient did not undergo any radiological investigation. In 33 (1.1%) patients, radiological diagnosis was not specified.
Considering the setting of acquisition, 2826 (90.1%) patients were affected by community-acquired intra-abdominal infections (IAIs), while the remaining 311 (9.9%) suffered from healthcare-associated IAIs; moreover, 1242 patients (39.6%) were affected by generalized peritonitis, while 1895 (60.4%) suffered from localized peritonitis or abscesses. The cause of infection was acute appendicitis in 1321 (42.1%) patients, acute cholecystitis in 415 (13.2%), gastroduodenal perforation in 364 (11.6%) patients, small bowel perforation in 219 (7.0%), acute diverticulitis in 217 (6.9%), colonic perforation in 203 (6.5%), post-traumatic perforation in 79 (2.5%), acute infected pancreatitis in 40 (1.3%), pelvic inflammatory disease (PID) in 30 (1.0%), and other causes in 249 (7.9%).
Management
Among all patients enrolled in the PIPAS Study, 377 (12%) underwent non-operative procedures, and the other 2760 (88.0%) patients underwent operative interventional procedures as first-line treatment. Source control was considered inadequate in 247 (247/2834, 8.7%) patients who underwent surgical procedures. In 1630 (1630/2834, 57.5%) patients the initial intervention was delayed. Among 2159 patients who received antimicrobial therapy, in 336 (15.6%), it was considered inadequate. During the same hospitalization, 242 (242/2760, 8.8%) patients underwent a second procedure after 4 (IQR 2–7) days because of a postoperative complication or a worsening of the initial stage. In particular, 79 (2.9%) patients underwent an open abdomen surgery, 57 (2.1%) a planned relaparotomy, and 87 (3.2%) an on-demand relaparotomy, and in 19 (0.7%) patients, no specific procedure was specified.
Immediate post-operative complications were observed in 339 (339/2760, 12.3%) patients who underwent a surgical procedure; among them we observed ongoing peritonitis in 174 (6.3%) patients, multi-organ failure in 33 (1.2%), bleeding in 32 (1.2%), cardiovascular complications in 17 (0.6%), respiratory complications in 15 (0.5%), sepsis or septic shock in 13 (0.5%), and other complications in 55 (2.0%). Delayed post-operative complications were detected in 774 (774/2760, 28.0%) patients who underwent an interventional procedure; in particular, they suffered from surgical site infections in 343 (12.4%) patients, post-operative peritonitis in 132 (4.8%), post-operative abdominal abscess in 118 (4.3%), respiratory complications in 54 (2.0%),cardiovascular complications in 39 (1.4%), sepsis or septic shock in 33 (1.2%), ileus in 22 (0.8%), multi-organ failure in 18 (0.7%), renal complications in 13 (0.5%), and other complications in 79 (2.9%).
Outcome
The overall in-hospital mortality rate was 8.9%. The median duration of hospitalization was 6 days (IQR 4–10). Bivariate analyses were performed to analyse the association between risk factors and in-hospital mortality using a two-sided chi-square test or a two-sided Fisher’s exact test where appropriate. Distribution of clinical predictive variables of in-hospital mortality is reported in Table 1. Distribution of laboratory predictive variables of in-hospital mortality is reported in Table 2.
Table 1.
Distribution of clinical predictive variables of in-hospital mortality
| Variables | Total patients | Dead | Survivors | RR | p value |
|---|---|---|---|---|---|
| n 3137 | n 280 | n 2857 | |||
| (100%) | (8.9%) | (91.1%) | |||
| Age > 80 years | 246 (7.8) | 72 (25.7) | 174 (6.1) | 4.07 (3.22–5.14) | < 0.001 |
| Immunodeficiency | 240 (7.7) | 56 (20.0) | 184 (6.4) | 3.02 (2.32–3.92) | < 0.001 |
| Malignancy | 333 (10.6) | 83 (29.6) | 250 (8.8) | 3.55 (2.82–4.46) | < 0.001 |
| Severe cardiovascular disease | 406 (12.9) | 106 (37.9) | 300 (10.5) | 4.10 (3.30–5.10) | < 0.001 |
| Diabetes | 400 (12.8) | 76 (27.1) | 324 (11.3) | 2.55 (2.00–3.25) | < 0.001 |
| Severe CKD | 141 (4.5) | 52 (18.6) | 89 (3.1) | 4.85 (3.78–6.22) | < 0.001 |
| Severe COPD | 186 (5.9) | 60 (21.4) | 126 (4.4) | 4.33 (3.39–5.52) | < 0.001 |
| Core temperature (°C) | |||||
| < 36.0 | 85 (2.7) | 23 (8.2) | 62 (2.2) | 3.21 (2.22–4.64) | < 0.001 |
| 36.0–38.0 | 2292 (73.1) | 185 (66.1) | 2107 (73.7) | 0.72 (0.57–0.91) | < 0.05 |
| > 38.0 | 760 (24.2) | 72 (25.7) | 688 (24.1) | 1.08 (0.84–1.40) | 0.54 |
| Hearth rate (bpm) | |||||
| < 60 | 8 (0.3) | 1 (0.4) | 7 (0.2) | 1.40 (0.22–8.80) | 0.72 |
| 60–100 | 1919 (61.2) | 117 (41.8) | 1802 (63.1) | 0.46 (0.36–0.57) | < 0.001 |
| > 100 | 1210 (38.6) | 162 (57.9) | 1048 (36.7) | 2.19 (1.74–2.74) | < 0.001 |
| Systolic blood pressure (mmHg) | |||||
| < 90 | 138 (4.4) | 49 (17.5) | 89 (3.1) | 4.61 (3.57–5.96) | < 0.001 |
| 90–100 | 388 (12.4) | 70 (25.0) | 318 (11.1) | 2.36 (1.84–3.03) | < 0.001 |
| > 100 | 2610 (83.2) | 161 (57.5) | 2449 (85.7) | 0.27 (0.22–0.34) | < 0.001 |
| Respiratory rate (breaths/min) | |||||
| < 22 | 2244 (71.5) | 124 (44.3) | 2120 (74.2) | 0.32 (0.25–0.40) | < 0.001 |
| 22–29 | 684 (21.8) | 97 (34.6) | 587 (20.5) | 1.90 (1.50–2.39) | < 0.001 |
| 30–35 | 154 (4.9) | 39 (13.9) | 115 (4.0) | 3.13 (2.33–4.21) | < 0.001 |
| > 35 | 55 (1.8) | 20 (7.1) | 35 (1.2) | 4.31 (2.98–6.23) | < 0.001 |
| AVPU responsiveness scale | |||||
| Alert | 2917 (93.0) | 187 (66.8) | 2730 (95.6) | 0.15 (0.12–0.19) | < 0.001 |
| Voice | 123 (3.9) | 54 (19.3) | 69 (2.4) | 5.85 (4.62–7.41) | < 0.001 |
| Pain | 74 (2.4) | 23 (8.2) | 51 (1.8) | 3.70 (2.59–5.30) | < 0.001 |
| Unresponsive | 23 (0.7) | 16 (5.7) | 7 (0.2) | 8.21 (6.12–11.01) | < 0.001 |
| NRS | |||||
| 0–3 | 80 (2.6) | 16 (5.7) | 64 (2.2) | 2.32 (1.47–3.64) | < 0.001 |
| 4–6 | 1512 (48.2) | 112 (40.0) | 1400 (49.0) | 0.72 (0.57–0.90) | < 0.05 |
| 7–10 | 1112 (35.4) | 128 (45.7) | 984 (34.4) | 1.53 (1.23–1.92) | < 0.001 |
| Not reported | 433 (13.8) | 24 (8.6) | 409 (14.3) | NA | NA |
| qSOFA score | |||||
| 0 | 1367 (43.6) | 37 (13.2) | 1330 (46.6) | 0.20 (0.14–0.28) | < 0.001 |
| 1 | 1323 (42.2) | 109 (38.9) | 1214 (42.5) | 0.87 (0.96–1.10) | 0.25 |
| 2 | 353 (11.3) | 84 (30.0) | 269 (9.4) | 3.38 (2.68–4.26) | < 0.001 |
| 3 | 94 (3.0) | 50 (17.9) | 44 (1.5) | 7.04 (5.61–8.82) | < 0.001 |
All p values calculated using two-sided chi-square test
RR: risk ratio, NA: not applicable, CKD: chronic kidney disease, COPD: chronic obstructive pulmonary disease, AVPU: alert/verbal/painful/unresponsive, NRS: numerical rating scale, qSOFA: Quick Sequential Organ Failure Assessment
Table 2.
Distribution of laboratory predictive variables of in-hospital mortality
| Variables | Total patients | Dead | Survivors | RR | p value |
|---|---|---|---|---|---|
| n 3137 | n 280 | n 2857 | |||
| (100%) | (8.9%) | (91.1%) | |||
| Blood oxygen saturation level (SpO2) (%) in air | |||||
| > 92 | 2782 (88.7) | 152 (54.3) | 2630 (92.1) | 0.15 (0.12–0.19) | < 0.001 |
| 90–91 | 198 (6.3) | 66 (23.6) | 132 (4.6) | 4.58 (3.62–5.79) | < 0.001 |
| 85–89 | 99 (3.1) | 41 (14.6) | 58 (2.0) | 5.26 (4.04–6.85) | < 0.001 |
| < 85 | 21 (0.7) | 9 (3.2) | 12 (0.4) | 4.93 (2.97–8.18) | < 0.001 |
| Not reported | 37 (1.2) | 12 (4.3) | 25 (0.9) | NA | NA |
| WBC (cells/mm3) | |||||
| > 12,000 | 1950 (62.2) | 182 (65.0) | 1768 (61.9) | 1.13 (0.89–1.43) | 0.30 |
| 4000–12,000 | 1043 (33.2) | 63 (22.5) | 980 (34.3) | 0.58 (0.44–0.76) | < 0.001 |
| < 4000 | 94 (3.0) | 29 (10.4) | 65 (2.3) | 3.74 (2.70–5.18) | < 0.001 |
| Not reported | 50 (1.6) | 6 (2.1) | 44 (1.5) | NA | NA |
| Platelet count (cells/ mm3) | |||||
| > 150,000 | 2606 (83.1) | 183 (65.4) | 2423 (84.8) | 0.38 (0.31–0.49) | < 0.001 |
| 50,000–1,500,000 | 387 (12.3) | 73 (26.1) | 314 (11.0) | 2.51 (1.96–3.20) | < 0.001 |
| < 50,000 | 32 (1.0) | 18 (6.4) | 14 (0.5) | 6.67 (4.81–9.24) | < 0.001 |
| Not reported | 112 (3.6) | 6 (2.1) | 106 (3.7) | NA | NA |
| INR | |||||
| > 3 | 23 (0.7) | 12 (4.3) | 11 (0.4) | 6.06 (4.03–9.11) | < 0.001 |
| 1.2–3 | 296 (9.4) | 72 (25.7) | 224 (7.8) | 3.32 (2.61–4.22) | < 0.001 |
| < 1.2 | 1954 (62.3) | 149 (53.2) | 1805 (63.2) | 0.69 (0.55–0.86) | 0.001 |
| Not reported | 864 (27.5) | 47 (16.8) | 817 (28.6) | NA | NA |
| CRP (mg/l) | |||||
| > 200 | 450 (14.3) | 70 (25.0) | 380 (13.3) | 1.99 (1.55–2.56) | < 0.001 |
| 101–200 | 462 (14.7) | 51 (18.2) | 411 (14.4) | 1.29 (0.97–1.72) | 0.08 |
| 5–100 | 946 (30.2) | 69 (24.6) | 877 (30.7) | 0.76 (0.58–0.98) | 0.04 |
| < 5 | 258 (8.2) | 3 (1.1) | 255 (8.9) | 0.12 (0.04–0.37) | < 0.001 |
| Not reported | 1471 (46.9) | 157 (56.1) | 1314 (46.0) | NA | NA |
| Procalcitonin (ng/ml) | |||||
| > 10 | 85 (2.7) | 31 (11.1) | 54 (1.9) | 4.47 (3.30–6.06) | < 0.001 |
| 0.5–10 | 260 (8.3) | 42 (15.0) | 218 (7.6) | 1.96 (1.44–2.64) | < 0.001 |
| < 0.5 | 100 (3.2) | 3 (1.1) | 97 (3.4) | 0.33 (0.11–1.01) | 0.03 |
| Not reported | 2692 (85.8) | 204 (72.9) | 2488 (87.1) | NA | NA |
| Lactate (mmol/l) | |||||
| >4 | 139 (4.4) | 61 (21.8) | 78 (2.7) | 6.01 (4.79–7.54) | < 0.001 |
| 1–4 | 615 (19.6) | 86 (30.7) | 529 (18.5) | 1.82 (1.43–2.31) | < 0.001 |
| < 1 | 136 (4.3) | 6 (2.1) | 130 (4.6) | 0.48 (0.22–1.07) | 0.06 |
| Not reported | 2247 (71.6) | 127 (45.4) | 2120 (74.2) | NA | NA |
All p values calculated using two-sided chi-square test
RR: risk ratio, NA: not applicable, WBC: white blood count, INR: international normalised ratio, CRP; C-reactive protein
Independent variables associated with in-hospital mortality according to the multivariable logistic regression are reported in Table 3. The model was highly significant (p < 0.0001), and the global performance of the test is explained by the area under the ROC curve, which is equals to 0.84 (95% CI).
Table 3.
Results of multinomial logistic regression for the analysis of variables associated with in-hospital mortality
| Variables | OR | 95% CI | p value |
|---|---|---|---|
| Age > 80 years | 2.11 | 1.43–3.10 | < 0.001 |
| Malignancy | 3.02 | 2.15–4.24 | < 0.001 |
| Severe cardiovascular disease | 2.76 | 1.97–3.87 | < 0.001 |
| Severe chronic kidney disease | 3.33 | 2.12–5.23 | < 0.001 |
| Respiratory rate ≥ 22 breaths/min | 3.38 | 2.23–5.13 | < 0.001 |
| Systolic blood pressure < 100 mmHg | 2.18 | 1.58–3.00 | < 0.001 |
| AVPU responsiveness scale voice or unresponsive | 3.07 | 2.10–4.51 | < 0.001 |
| Blood oxygen saturation level (SpO2) < 90% in air | 2.67 | 1.64–4.32 | < 0.001 |
| Platelet count < 50,000 cells/ mm3 | 4.81 | 2.07–11.20 | < 0.001 |
| Lactate > 4 mmol/l | 4.00 | 2.58–6.23 | < 0.001 |
CI: confidence interval, OR: odds ratio, AVPU: alert/verbal/painful/unresponsive
Developing the severity score
The second aim of the study was to develop a severity score for patients with a clinical diagnosis of acute peritonitis that is simple and globally acceptable with a good prognostic value. Only the significant clinical variables associated with in-hospital mortality obtained from the multivariable logistic regression model were included, excluding the lactate, and platelet count. This modification was done for three reasons: (a) to simplify the score, (b) to make it more universal and globally acceptable, and (c) because of lack of facilities to obtain lactate in low-income countries. The coefficients of the variables were used to develop the score, and not the Odds Ratio. The significant clinical variables were subjected to different direct logistic regression models using either simple binomial variables or ordinal data, to arrive at a simplified and acceptable model. Direct logistic regression model of the clinical variables affecting mortality which were used to develop the score is reported in Table 4. The score would have become complicated if we had to follow the model proposed by Moons et al. [15], whereby the coefficient would have to be multiplied by 10 and the value approximated to the nearest integral to get a score. This meant that the scores derived from the model would be 10, 11, 9, 12, 8, 9, 9, and 14, making it very complex. Hence, it was decided to approximate the coefficient to the nearest integral number and test the model. Since the coefficients were approximated to 1, each of these variables could have a score of 1 or 0 with a maximum score of 8 and a range of 0–8. The simplified and finalized the PIPAS Severity Score is shown in the Appendix.
Table 4.
Direct logistic regression model with clinical variables affecting mortality of patients used to develop the score
| Variable | Estimate | SE | Wald test | P | OR | 95% CI | |
|---|---|---|---|---|---|---|---|
| LL | UL | ||||||
| Age > 80 years | 0.97 | 0.19 | 25.91 | < 0.0001 | 2.63 | 1.81 | 3.89 |
| Malignancy | 1.13 | 0.17 | 42.43 | < 0.0001 | 3.11 | 2.21 | 4.37 |
| Severe CVD | 0.88 | 0.17 | 26.09 | < 0.0001 | 2.41 | 1.72 | 3.38 |
| Severe CKD | 1.2 | 0.23 | 26.23 | < 0.0001 | 3.32 | 2.1 | 5.26 |
| RR ≥ 22 breaths/min | 0.75 | 0.16 | 22.61 | < 0.0001 | 2.11 | 1.55 | 2.87 |
| SBP < 100 mmHg | 0.86 | 0.17 | 27.29 | < 0.0001 | 2.37 | 1.71 | 3.27 |
| AVPU responsiveness scale: not completely alert. | 1.35 | 0.2 | 47.98 | < 0.0001 | 3.86 | 2.63 | 5.65 |
| Blood oxygen saturation level: SpO2 < 90% in air | 0.87 | 0.25 | 12.15 | < 0.0001 | 2.39 | 1.46 | 3.89 |
| Constant | − 3.79 | 0.13 | 834.77 | < 0.0001 | 0.023 | – | – |
SE: standard error, OR: odds ratio, CI: confidence interval, LL: lower limit, UL: upper limit, CVD: cardiovascular disease, CKD: chronic kidney disease, RR: respiratory rate, SBP: systolic blood pressure, AVPU: alert/verbal/painful/unresponsive
The PIPAS Severity Score had a very good ability of distinguishing those who survived from those who died (Fig. 1). The ROC curve showed that the best cutoff point for predicting mortality was a PIPAS Severity Score of 1.5 having a sensitivity of 74.3%, a specificity of 82.2% (Fig. 2) and an area under the curve of 85.1%. The overall mortality was 2.9% for the patients who had scores of 0 and 1, 22.7% for those who had scores of 2 and 3, 46.8% for those who had scores 4 and 5, and 86.7% for those who have scores 7–8.
Fig. 1.
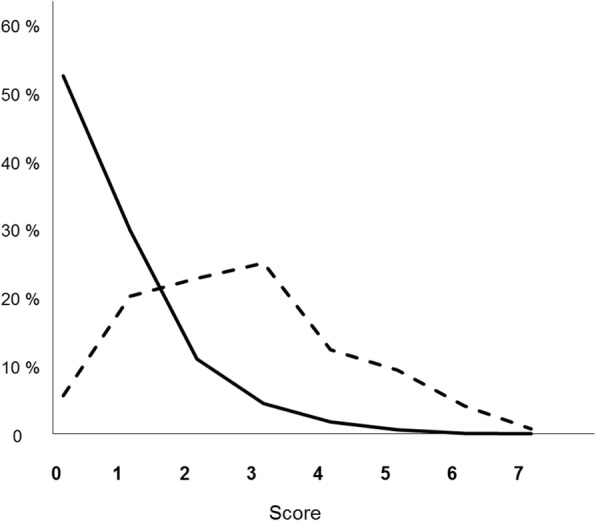
Distribution of the percentile PIPAS Severity Score of hospitalized peritonitis patients for those who survived (continuous line) (n = 2832) and those who died (interrupted line) (n = 268). Global data from 153 worldwide surgical departments in 56 countries, over a 4-month study period (February 1, 2018–May 31, 2018). Thirty-seven patients (1.2%) had missing data in whom the score could not be computed
Fig. 2.
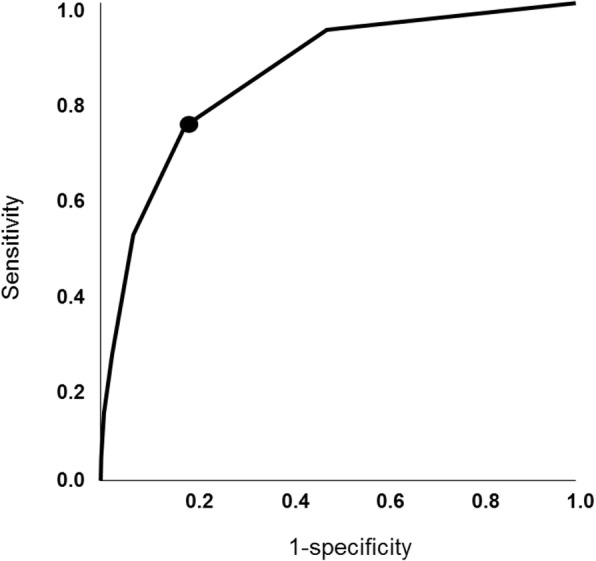
Receiver operating characteristic (ROC) curve for the best PIPAS Severity Score (1.5, black circle) that predicted mortality in peritonitis patients. Global data from 153 worldwide surgical departments in 56 countries, over a 4-month study period (February 1, 2018–May 31, 2018)
Discussion
Using the multivariable logistic regression, ten independent variables associated with in-hospital mortality were identified. The model was highly significant, with a good global performance of the test. Excluding platelet count and lactate, eight bedside easy-to-measure parameters were recognized to develop an early warning score, the PIPAS Severity Score, assessing anamnestic data (age > 80 years, malignancy, severe cardiovascular disease, severe chronic kidney disease), and physiological functions (respiratory rate ≥ 22 breaths/min, systolic blood pressure < 100 mmHg, AVPU responsiveness scale voice or unresponsive, blood oxygen saturation level (SpO2) < 90% in air).
The PIPAS Severity Score, taking into account physiological parameters recognizable on hospital admission, immediately allows clinicians to assess the severity and decide the aggressiveness of treatment. Particularly for clinicians working in low- and middle-income countries, where diagnostic imaging is often insufficient, and in some instances completely lacking, the utility of this score system is remarkable [16].
Sometimes, the atypical clinical presentation of acute peritonitis may be responsible for a delay in diagnosis and treatment. Therefore, a triage system that quickly recognizes patients at high risk for mortality and allows to transfer them immediately to an acute care unit is a vital component of the emergency services. As a consequence, any process of improving the quality of emergency care globally should focus on simple diagnostic criteria based on physical examination findings that can recognize patients needing critical care. From a global perspective, a feasible, low-cost method of rapidly identifying patients requiring critical care is crucial. Early warning system scores utilize physiological, easy-to-measure parameters, assessing physiological parameters such as systolic blood pressure, pulse rate, respiratory rate, temperature, oxygen saturations, and level of consciousness [17].
The statistical analysis shows that the PIPAS Severity Score has a very good ability of distinguishing those who survived from those who died. The overall mortality was 2.9% for the patients who had scores of 0 and 1, 22.7% for those who had scores of 2 and 3, 46.8% for those who had scores of 4 and 5, and 86.7% for those who have scores of 7–8.
PIPAS Study has strengths and limitations. It is an observational multicentre study involving a large, but probably not representative, number of hospitals worldwide, since the majority of patients were collected in countries belonging to the WHO European region. Moreover, its validity needs to be tested in future large prospective series before potentially serving as a template for future database and research into patient outcomes. Finally, a potential limitation may be the high rate of patients with acute appendicitis enrolled in the study (42.1%). Some authors [18], after excluding patients with perforated appendicitis, found that the cure rate among patients who had peritonitis and were enrolled in clinical trials, was much higher than that of patients who were not enrolled and that the mortality rate was much lower. Although, delineating the source of infection as accurately as possible prior to surgery is described as the primary aim and the first step in managing acute peritonitis, in emergency departments of limited-resource hospitals, diagnosis of acute peritonitis is mainly clinical, and supported only by basic laboratory tests, and excluding acute appendicitis in the pre-operative phase would make the score impractical to a large part of the world’s population.
Conclusions
This worldwide multicentre observational study was performed in 153 surgical departments from 56 countries over a 4-month study period (February 1, 2018–May 31, 2018). All consecutive patients admitted to surgical departments with clinical diagnosis of acute peritonitis were included in the study. The most significant independent variables associated with in-hospital mortality were adjusted to clinical criteria and were used to create a new bedside early warning score for patients with acute peritonitis. The simple PIPAS Severity Score for patients with acute peritonitis can be used on the global level and can help clinicians to assess patients with acute peritonitis at high risk for treatment failure and mortality. The authors created an acronym for the PIPAS Severity Score to help remember the variables “Scores Must Be Simple For Sepsis Risk Assessment” (severe cardiovascular disease, malignancy, blood oxygen saturation level, severe chronic kidney disease, fully alert, systolic blood pressure, respiratory rate, age).
Acknowledgements
Not applicable.
Funding.
Not applicable.
Abbreviations
- AVPU
Alert/verbal/painful/unresponsive
- COPD
Chronic obstructive pulmonary disease
- CRP
C-reactive protein
- CT
Computer tomography
- INR
International normalised ratio
- IQR
Interquartile range
- LOS
Length of hospital stay
- NRS
Numerical rating scale
- PID
Pelvic inflammatory disease. IAIs: intra-abdominal infections
- qSOFA
Quick Sequential Organ Failure Assessment
- ROC
Receiver operating characteristic
- US
Ultrasound
- WBC
White blood count
- WSES
World Society of Emergency Surgery
Apenndix
Table 5.
PIPAS Severity Score for patients with acute peritonitis (range 0–8)
| Variables | Score |
|---|---|
| Age (years) | |
| 80 or more | 1 |
| Less than 80 | 0 |
| Malignancy | |
| Yes | 1 |
| No | 0 |
| Severe cardiovascular disease | |
| Yes | 1 |
| No | 0 |
| Severe chronic kidney disease | |
| Yes | 1 |
| No | 0 |
| Respiratory rate ≥ 22 breaths/min | |
| Yes | 1 |
| No | 0 |
| Systolic blood pressure < 100 mmHg | |
| Yes | 1 |
| No | 0 |
| Blood oxygen saturation level (SpO2) < 90% in air | |
| Yes | 1 |
| No | 0 |
| AVPU responsiveness scale full alert | |
| No | 1 |
| Yes | 0 |
Authors’ contributions
M Sartelli designed the study and wrote the manuscript. FM Abu-Zidan developed the severity score. FM Labricciosa performed the statistical analysis. All authors participated in the study. All authors read and approved the final manuscript.
Availability of data and materials
The authors are responsible for the data described in the manuscript and assure full availability of the study material upon request to the corresponding author.
Ethics approval and consent to participate
The data was completely anonymised, and no patient or hospital information was collected in the database. The study protocol was approved by the board of the WSES, and the study was conducted under its supervision. The board of the WSES granted the proper ethical conduct of the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Massimo Sartelli, Email: massimosartelli@gmail.com.
Fikri M. Abu-Zidan, Email: fabuzidan@uaeu.ac.ae
Francesco M. Labricciosa, Email: labricciosafrancesco@gmail.com
Yoram Kluger, Email: y_kluger@rambam.health.gov.il.
Federico Coccolini, Email: federico.coccolini@gmail.com.
Luca Ansaloni, Email: aiace63@gmail.com.
Ari Leppäniemi, Email: ari.leppaniemi@hus.fi.
Andrew W. Kirkpatrick, Email: Andrew.Kirkpatrick@albertahealthservices.ca
Matti Tolonen, Email: matti.tolonen@hus.fi.
Cristian Tranà, Email: trana.cristian@gmail.com.
Jean-Marc Regimbeau, Email: regimbeau.jean-marc@chu-amiens.fr.
Timothy Hardcastle, Email: hardcastle@ukzn.ac.za.
Renol M. Koshy, Email: renolkoshy@gmail.com
Ashraf Abbas, Email: ashrafabbaas@hotmail.com.
Ulaş Aday, Email: ulasaday@gmail.com.
A. R. K. Adesunkanmi, Email: adesunkanmi@yahoo.com
Adesina Ajibade, Email: ajifada2@gmail.com.
Lali Akhmeteli, Email: laliakhmeteli@gmail.com.
Emrah Akın, Email: emrahakindr@gmail.com.
Nezih Akkapulu, Email: akkapulu@gmail.com.
Alhenouf Alotaibi, Email: dr.h.alnashmi@live.com.
Fatih Altintoprak, Email: fatihaltintoprak@yahoo.com.
Dimitrios Anyfantakis, Email: danyfantakis@med.uoc.gr.
Boyko Atanasov, Email: doktor_boiko@abv.bg.
Goran Augustin, Email: augustin.goran@gmail.com.
Constança Azevedo, Email: azevedo.constanca91@gmail.com.
Miklosh Bala, Email: rbalam@hadassah.org.il.
Dimitrios Balalis, Email: dbalalis@gmail.com.
Oussama Baraket, Email: oubaraket@gmail.com.
Suman Baral, Email: brylsuman.sur@gmail.com.
Or Barkai, Email: orbarkai0902@gmail.com.
Marcelo Beltran, Email: beltran_01@yahoo.com.
Roberto Bini, Email: re.bini@libero.it.
Konstantinos Bouliaris, Email: kwstisbool@yahoo.com.
Ana B. Caballero, Email: anabelen0604@gmail.com
Valentin Calu, Email: drcalu@gmail.com.
Marco Catani, Email: marco.catani@uniroma1.it.
Marco Ceresoli, Email: marco.ceresoli89@gmail.com.
Vasileios Charalampakis, Email: vasileios.charalampakis@swft.nhs.uk.
Asri Che Jusoh, Email: asricj@yahoo.com.
Massimo Chiarugi, Email: massimo.chiarugi@med.unipi.it.
Nicola Cillara, Email: ncillara@gmail.com.
Raquel Cobos Cuesta, Email: raquelcoboscuesta@hotmail.com.
Luigi Cobuccio, Email: l.cobuccio@tiscali.it.
Gianfranco Cocorullo, Email: gianfranco.cocorullo@unipa.it.
Elif Colak, Email: elifmangancolak@hotmail.com.
Luigi Conti, Email: dr.luigiconti@gmail.com.
Yunfeng Cui, Email: yunfengcuidoctor@aliyun.com.
Belinda De Simone, Email: desimone.belinda@gmail.com.
Samir Delibegovic, Email: sam.delibey@gmail.com.
Zaza Demetrashvili, Email: zdemetr@yahoo.com.
Demetrios Demetriades, Email: Demetrios.Demetriades@med.usc.edu.
Ana Dimova, Email: Anamajsecb@gmail.com.
Agron Dogjani, Email: agrondogjani@yahoo.com.
Mushira Enani, Email: menani@kfmc.med.sa.
Federica Farina, Email: f.farina@uslnordovest.toscana.it.
Francesco Ferrara, Email: frr.fra@gmail.com.
Domitilla Foghetti, Email: domitilla.foghetti@gmail.com.
Tommaso Fontana, Email: tommasofontana2@virgilio.it.
Gustavo P. Fraga, Email: fragagp2008@gmail.com
Mahir Gachabayov, Email: gachabayovmahir@gmail.com.
Grelpois Gérard, Email: Grelpois.Gerard@chu-amiens.fr.
Wagih Ghnnam, Email: wghnnam@gmail.com.
Teresa Giménez Maurel, Email: teresagm87@gmail.com.
Georgios Gkiokas, Email: georgiokas@yahoo.com.
Carlos A. Gomes, Email: caxiaogomes@gmail.com
Ali Guner, Email: draliguner@yahoo.com.
Sanjay Gupta, Email: sandiv99@yahoo.co.uk.
Andreas Hecker, Email: andreas.hecker@chiru.med.uni-giessen.de.
Elcio S. Hirano, Email: hiranoes@gmail.com
Adrien Hodonou, Email: hodasm98@gmail.com.
Martin Hutan, Email: martin.hutan@yahoo.com.
Igor Ilaschuk, Email: lsmd@ukr.net.
Orestis Ioannidis, Email: telonakos@hotmail.com.
Arda Isik, Email: kararda@yahoo.com.
Georgy Ivakhov, Email: ivakhovsurg@yandex.ru.
Sumita Jain, Email: sumitajain@gmail.com.
Mantas Jokubauskas, Email: mantas910317@gmail.com.
Aleksandar Karamarkovic, Email: alekara@sbb.rs.
Robin Kaushik, Email: robinkaushik@yahoo.com.
Jakub Kenig, Email: jkenig@cm-uj.krakow.pl.
Vladimir Khokha, Email: vladimirkhokha@gmail.com.
Denis Khokha, Email: ionseed@gmail.com.
Jae Il Kim, Email: erythrokim@paik.ac.kr.
Victor Kong, Email: victorywkong@yahoo.com.
Dimitris Korkolis, Email: dkorkolis_2000@yahoo.com.
Vitor F. Kruger, Email: vitorfkruger@gmail.com
Ashok Kshirsagar, Email: kshirsagarashok007@gmail.com.
Romeo Lages Simões, Email: romeolagessimoes@gmail.com.
Andrea Lanaia, Email: andrea.lanaia@ausl.re.it.
Konstantinos Lasithiotakis, Email: kwstaslasith@gmail.com.
Pedro Leão, Email: pedroleao@med.uminho.pt.
Miguel León Arellano, Email: miguel.leon.arellano@gmail.com.
Holger Listle, Email: holger.listle@uni-greifswald.de.
Andrey Litvin, Email: aalitvin@gmail.com.
Aintzane Lizarazu Pérez, Email: aintzanelizarazu@hotmail.com.
Eudaldo Lopez-Tomassetti Fernandez, Email: dretomassetti@gmail.com.
Eftychios Lostoridis, Email: e.lostoridis@gmail.com.
Davide Luppi, Email: dl.davideluppi@gmail.com.
Gustavo M. Machain V, Email: gmmachain@yahoo.com
Piotr Major, Email: majorpiotr@gmail.com.
Dimitrios Manatakis, Email: dmanatak@yahoo.gr.
Marianne Marchini Reitz, Email: reitzmm@gmail.com.
Athanasios Marinis, Email: drmarinis@gmail.com.
Daniele Marrelli, Email: daniele.marrelli@unisi.it.
Aleix Martínez-Pérez, Email: aleix.martinez.perez@gmail.com.
Sanjay Marwah, Email: drsanjay.marwah@gmail.com.
Michael McFarlane, Email: michaelm500@yahoo.com.
Mirza Mesic, Email: meshakmmm@gmail.com.
Cristian Mesina, Email: mesina.cristian@doctor.com.
Nickos Michalopoulos, Email: nickos.michalopoulos@gmail.com.
Evangelos Misiakos, Email: misiakos@med.uoa.gr.
Felipe Gonçalves Moreira, Email: fgmoreira@gmail.com.
Ouadii Mouaqit, Email: mouaqit3001@gmail.com.
Ali Muhtaroglu, Email: alimuhtarogluu@gmail.com.
Noel Naidoo, Email: Noel.naidoo@gmail.com.
Ionut Negoi, Email: negoiionut@gmail.com.
Zane Nikitina, Email: tu.un.es@inbox.lv.
Ioannis Nikolopoulos, Email: inikolopoulos@gmail.com.
Gabriela-Elisa Nita, Email: GabrielaElisa.Nita@ausl.re.it.
Savino Occhionorelli, Email: savino.occhionorelli@unife.it.
Iyiade Olaoye, Email: tunde_olaoye_dr@yahoo.com.
Carlos A. Ordoñez, Email: ordonezcarlosa@gmail.com
Zeynep Ozkan, Email: drzeynepozkan@yahoo.com.
Ajay Pal, Email: akpal.jnmc@yahoo.com.
Gian M. Palini, Email: palinigm@yahoo.it
Kyriaki Papageorgiou, Email: kypapage@gmail.com.
Dimitris Papagoras, Email: dpapagoras@hotmail.com.
Francesco Pata, Email: francesco.pata@gmail.com.
Michał Pędziwiatr, Email: mpedziwiatr@gmail.com.
Jorge Pereira, Email: docjota@netcabo.pt.
Gerson A. Pereira Junior, Email: gersonapj@gmail.com
Gennaro Perrone, Email: gennaro.perrone82@gmail.com.
Tadeja Pintar, Email: tadeja.pintar@kclj.si.
Magdalena Pisarska, Email: magdalenapisarska@interia.pl.
Oleksandr Plehutsa, Email: plehutsa@ukr.net.
Mauro Podda, Email: mauropodda@ymail.com.
Gaetano Poillucci, Email: gaetano.poillucci@gmail.com.
Martha Quiodettis, Email: traumahst@gmail.com.
Tuba Rahim, Email: dr.tooba@live.com.
Daniel Rios-Cruz, Email: jobzon@hotmail.com.
Gabriel Rodrigues, Email: gabyrodricks@gmail.com.
Dmytry Rozov, Email: ddocmail@gmail.com.
Boris Sakakushev, Email: bsakakushev@gmail.com.
Ibrahima Sall, Email: sall_i17@yahoo.fr.
Alexander Sazhin, Email: sazhin-av@yandex.ru.
Miguel Semião, Email: migsemiao@hotmail.com.
Taanya Sharda, Email: taanya.sharda19@gmail.com.
Vishal Shelat, Email: vgshelat@rediffmail.com.
Giovanni Sinibaldi, Email: giovanni.sinibaldi@gmail.com.
Dmitrijs Skicko, Email: d.skicko@gmail.com.
Matej Skrovina, Email: matej.skrovina@nnj.agel.cz.
Dimitrios Stamatiou, Email: jpstamatiou@yahoo.gr.
Marco Stella, Email: m.stel@libero.it.
Marcin Strzałka, Email: marcin.strzalka@uj.edu.pl.
Ruslan Sydorchuk, Email: rsydorchuk@ukr.net.
Ricardo A. Teixeira Gonsaga, Email: novo02@uol.com.br
Joel Noutakdie Tochie, Email: joeltochie@gmail.com.
Gia Tomadze, Email: giatomadze@gmail.com.
Lara Ugoletti, Email: Lara.Ugoletti@ausl.re.it.
Jan Ulrych, Email: Jan.Ulrych@vfn.cz.
Toomas Ümarik, Email: toomas.ymarik@regionaalhaigla.ee.
Mustafa Y. Uzunoglu, Email: drmyuzunoglu@gmail.com
Alin Vasilescu, Email: vasilescu.alin@gmail.com.
Osborne Vaz, Email: osborne.vaz@mft.nhs.uk.
Andras Vereczkei, Email: vereczkei.andras@pte.hu.
Nutu Vlad, Email: nutu.vlad@gmail.com.
Maciej Walędziak, Email: maciej.waledziak@gmail.com.
Ali I. Yahya, Email: aliyahyaz60@hotmail.com
Omer Yalkin, Email: omeryalkin@gmail.com.
Tonguç U. Yilmaz, Email: utku.yilmaz@acibadem.edu.tr
Ali Ekrem Ünal, Email: info@wses.org.uk.
Kuo-Ching Yuan, Email: traumayuan@gmail.com.
Sanoop K. Zachariah, Email: skzach@yahoo.com
Justas Žilinskas, Email: justas.zilinskas@gmail.com.
Maurizio Zizzo, Email: zizzomaurizio@gmail.com.
Vittoria Pattonieri, Email: infonew@wses.org.uk.
Gian Luca Baiocchi, Email: gianluca.baiocchi@unibs.it.
Fausto Catena, Email: faustocatena@gmail.com.
References
- 1.Sartelli M, Catena F, Abu-Zidan FM, Ansaloni L, Biffl WL, Boermeester MA, et al. Management of intra-abdominal infections: recommendations by the WSES 2016 consensus conference. World J Emerg Surg. 2017;12:22. doi: 10.1186/s13017-017-0132-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sartelli M, Catena F, Di Saverio S, Ansaloni L, Malangoni M, Moore EE, et al. Current concept of abdominal sepsis: WSES position paper. World J Emerg Surg. 2014;9:22. doi: 10.1186/1749-7922-9-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Angus DC, van der Poll T. Severe sepsis and septic shock. N Engl J Med. 2013;369:840–851. doi: 10.1056/NEJMra1208623. [DOI] [PubMed] [Google Scholar]
- 4.Wacha H, Linder MM, Feldman U, Wesch G, Gundlach E, Steifensand RA. Mannheim peritonitis index – prediction of risk of death from peritonitis: construction of a statistical and validation of an empirically based index. Theor Surg. 1987;1:169–177. [Google Scholar]
- 5.Bosscha K, Reijnders K, Hulstaert PF, Algra A, van der Werken C. Prognostic scoring systems to predict outcome in peritonitis and intra-abdominal sepsis. Br J Surg. 1997;84:1532–1534. [PubMed] [Google Scholar]
- 6.Sartelli M, Abu-Zidan FM, Catena F, Griffiths EA, Di Saverio S, Coimbra R, et al. Global validation of the WSES sepsis severity score for patients with complicated intra-abdominal infections: a prospective multicenter study (WISS study) World J Emerg Surg. 2015;10:61. doi: 10.1186/s13017-015-0055-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chatterjee AS, Renganathan DN. POSSUM: A Scoring System for Perforative Peritonitis. J Clin Diagn Res. 2015;9:PC05–PC09. doi: 10.7860/JCDR/2015/12720.5854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sartelli M, Chichom-Mefire A, Labricciosa FM, Hardcastle T, Abu-Zidan FM, Adesunkanmi AK, et al. The management of intra-abdominal infections from a global perspective: 2017 WSES guidelines for management of intra-abdominal Infections. World J Emerg Surg. 2017;12:29. doi: 10.1186/s13017-017-0141-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fleisher LA, Beckman JA, Brown KA, Calkins H, Chaikof E, Fleischmann KE, et al. ACC/AHA 2007 Guidelines on Perioperative Cardivascular Evaluation and Care for Noncardiac Surgery: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines on Perioperative Cardiovascular Evaluation for Noncardiac Surgery): Developed in Collaboration With the American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Rhythm Society, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, and Society for Vascular Surgery. Circulation. 2007;116:1971–1996. doi: 10.1161/CIRCULATIONAHA.107.185700. [DOI] [PubMed] [Google Scholar]
- 10.Vestbo J, Hurd SS, Agustí AG, Jones PW, Vogelmeier C, Anzueto A, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2013;187:347–365. doi: 10.1164/rccm.201204-0596PP. [DOI] [PubMed] [Google Scholar]
- 11.Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;2:81–84. doi: 10.1016/S0140-6736(74)91639-0. [DOI] [PubMed] [Google Scholar]
- 12.Farrar JT, Young JP, Jr, LaMoreaux L, Werth JL, Poole RM. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94:149–158. doi: 10.1016/S0304-3959(01)00349-9. [DOI] [PubMed] [Google Scholar]
- 13.Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) JAMA. 2016;315:801–810. doi: 10.1001/jama.2016.0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sartelli M. A focus on intra-abdominal infections. World J Emerg Surg. 2010;5:9. doi: 10.1186/1749-7922-5-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bickler SW, Spiegel D. Improving surgical care in low- and middle-income countries: a pivotal role for the World Health Organization. World J Surg. 2010;34:386–390. doi: 10.1007/s00268-009-0273-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moons KG, Harrell FE, Steyerberg EW. Should scoring rules be based on odds ratios or regression coefficients? J Clin Epidemiol. 2002;55:1054–1055. doi: 10.1016/S0895-4356(02)00453-5. [DOI] [PubMed] [Google Scholar]
- 17.Kruisselbrink R, Kwizera A, Crowther M, Fox-Robichaud A, O’Shea T, Nakibuuka J, et al. Modified early warning score (MEWS) identifies critical illness among ward patients in a resource restricted setting in Kampala. Uganda: a prospective observational study. PLoS One. 2016;11:e0151408. doi: 10.1371/journal.pone.0151408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Merlino JI, Malangoni MA, Smith CM, Lange RL. Prospective randomized trials affect the outcomes of intraabdominal infection. Ann Surg. 2001;233:859–866. doi: 10.1097/00000658-200106000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors are responsible for the data described in the manuscript and assure full availability of the study material upon request to the corresponding author.


