Key Points
Question
Is cannabinoid agonist treatment, in combination with psychosocial services, a safe and efficacious approach to reducing illicit cannabis use in patients with cannabis dependence who are seeking treatment?
Findings
In this randomized clinical trial of 128 participants, a 12-week course of nabiximols, a combination of tetrahydrocannabinol and cannabidiol, resulted in significantly fewer days of illicit cannabis use compared with placebo, and was well tolerated by participants.
Meaning
The use of cannabinoid agonist medication appears to be a promising addition to the treatment of patients with cannabis dependence.
Abstract
Importance
There are no effective medications for treating dependence on cannabis.
Objective
To examine the safety and efficacy of nabiximols in the treatment of patients with cannabis dependence.
Design, Setting, and Participants
This parallel double-blind randomized clinical trial comparing nabiximols with placebo in a 12-week, multisite outpatient study recruited participants from February 3, 2016, to June 14, 2017, at 4 outpatient specialist alcohol and drug treatment services in New South Wales, Australia. Participants had cannabis dependence (as defined by the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision) and were seeking treatment, were nonresponsive to prior treatment attempts, were 18 to 64 years of age, had no other substance use disorder, had no severe medical or psychiatric conditions, were not pregnant, were not mandated by a court to undergo treatment, and provided informed consent. Results for primary efficacy measures and all secondary outcomes were obtained using a modified intention-to-treat data set.
Interventions
Participants received 12-week treatment involving weekly clinical reviews, structured counseling, and flexible medication doses—up to 32 sprays daily (tetrahydrocannabinol, 86.4 mg, and cannabidiol, 80 mg), dispensed weekly.
Main Outcomes and Measures
Primary outcome was self-reported number of days using illicit cannabis during the 12-week period. Other outcomes included alternate cannabis use parameters (periods of abstinence, withdrawal, cravings, and problems), safety parameters (adverse events and aberrant medication use), health status, other substance use, and treatment retention.
Results
A total of 128 participants (30 women and 98 men; mean [SD] age, 35.0 [10.9] years) were randomized and received at least 1 dose of study medication. Participants had used a mean (SD) of 2.3 (2.1) g of cannabis on a mean (SD) of 25.7 (4.5) days in the past 28 days. Treatment retention was comparable for the 2 groups (placebo, 30 of 67 participants [44.8%]; nabiximols, 30 of 61 participants [49.2%]), and both groups used similar mean (SD) doses (placebo, 18.5 [9.5] sprays daily; nabiximols, 17.6 [9.5] sprays daily, equivalent to a mean [SD] of 47.5 [25.7] mg of tetrahydrocannabinol and 44.0 [23.8] mg of cannabidiol). For the primary end point, the placebo group reported significantly more days using cannabis during the 12 weeks (mean [SD], 53.1 [33.0] days) than the nabiximols group (mean [SD], 35.0 [32.4] days; estimated difference, 18.6 days; 95% CI, 3.5-33.7 days; P = .02). Both groups showed comparable improvements in health status, with no substantial changes in other substance use. Medication was well tolerated with few adverse events.
Conclusions and Relevance
This study demonstrates that cannabinoid agonist treatment, in this case using nabiximols, in combination with psychosocial interventions is a safe approach for reducing cannabis use among individuals with cannabis dependence who are seeking treatment.
Trial Registration
anzctr.org.au Identifier: ACTRN12616000103460
This randomized clinical trial examines the safety and efficacy of nabiximols, an oromucosal tetrahydrocannabinol-cannabidiol medication vs placebo, in the treatment of adults with cannabis dependence.
Introduction
Apart from alcohol and tobacco, cannabis is the most widely used psychoactive substance and accounts for the largest number of people dependent on illicit drugs globally.1,2 In Australia, 10.4% of adults reported using cannabis in the past 12 months,3 of whom approximately 10% describe dependent patterns of use.4 Cannabis dependence is associated with a range of cognitive, psychiatric, and physical health problems1,4,5 and accounts for the second largest number of drug treatment episodes in Australia.6
The effectiveness of existing treatments for cannabis dependence is unsatisfactory. Approximately 80% of patients relapse to regular use within 1 to 6 months of either cannabis withdrawal7,8 or counseling (eg, cognitive behavioral therapy [CBT]) interventions.9 As with the treatment of other chronic addiction conditions, there is interest in combining long-term medication with psychosocial interventions,10 although no efficacious pharmacotherapies for cannabis dependence have been established.11
A promising approach is the use of cannabinoid agonist pharmacotherapies, akin to opioid or nicotine replacement treatment.12 The rationale is to provide a safer route of administration than smoking, reduce unsanctioned drug use by ameliorating withdrawal and cravings,7 and facilitate greater engagement in psychosocial interventions, leading to improved health and psychosocial functioning. However, cannabinoid agonist treatment may also be associated with adverse events (AEs) and aberrant medication use in people with a history of illicit cannabis use. Although short courses (eg, 5-7 days) of cannabinoid agonists for treating acute cannabis withdrawal successfully suppress withdrawal symptoms,7,13,14,15 the high rates of relapse after acute withdrawal indicate that longer-term treatment (eg, ≥12 weeks) may be required to achieve longer-term outcomes.10,11
The longer-term use of dronabinol, a synthetic oral tetrahydrocannabinol (THC) product, for cannabis dependence was examined in a 12-week randomized placebo-controlled trial in 122 patients with cannabis dependence.16 Although dronabinol, 60 mg daily, was well tolerated and reduced withdrawal symptoms, there was no advantage compared with placebo in achieving abstinence or reducing days of cannabis use. More recently, a 12-week, 40-participant, placebo-controlled feasibility randomized clinical trial examining nabiximols for cannabis dependence concluded that “nabiximols in combination with Motivational Enhancement Therapy/CBT was well tolerated and allowed for reduction of cannabis use,”17(p2) suggesting that larger trials are warranted.
Our study examined the efficacy and safety of nabiximols in the treatment of patients with cannabis dependence. The primary hypothesis for the study is that a 12-week treatment program with nabiximols will result in significantly less illicit cannabis use—as assessed by self-reported cannabis use days over the 12-week period—compared with placebo. Secondary hypotheses are that nabiximols treatment will result in significant improvements in a range of secondary cannabis treatment outcomes, including periods of abstinence, measures of cannabis withdrawal, cravings, and cannabis-related problems, compared with placebo; will have an acceptable AE and abuse liability profile in a population with cannabis dependence; and will result in significant improvements in general health and psychosocial measures compared with placebo.
Methods
Study Design
This phase 3 multisite outpatient randomized, double-blind, parallel-design study compared a 12-week course of nabiximols with placebo. Medications were dispensed on a weekly basis, and both groups received standardized clinical care.18 All participants were followed up for confidential research interviews (irrespective of completion of the trial intervention) at weeks 0 (baseline), 4, 8, and 12. Recruitment began February 3, 2016, and ended June 14, 2017. Study procedures are described in greater detail elsewhere.18 The study was approved by the South East Sydney Local Health District Human Research Ethics Committee. Participants provided written informed consent.
Sites
The study was conducted across 4 specialist outpatient addiction treatment services in New South Wales, Australia: The Langton Centre, St George Hospital, Newcastle Community Health Services, and the Centre for Addiction Medicine (Western Sydney).
Participants
Previous studies of treatment for cannabis dependence have reported on abstinence rates, and this outcome (while not the primary end point in this study) was used to estimate a sample size of 142 participants (71 per group) to detect a doubling of abstinence rates at 12 weeks from 22% (placebo) to 44% (nabiximols) with 80% power (2-tailed) and α = 0.05. Inclusion criteria were age 18 to 65 years, cannabis dependence (as defined by the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision19), inability to stop cannabis use in previous quit attempts, and provision of informed consent and agreement to study procedures, including to not drive and to use reliable contraception. Exclusion criteria were another substance use disorder other than nicotine or caffeine; severe medical or psychiatric disorder, including history of epilepsy or psychosis; pregnant or lactating women or those planning pregnancy; inability to safely store medication; not available for follow-up; addiction treatment mandated by a court; and treatment for cannabis dependence within past month.
Recruitment
Individuals seeking treatment were screened by telephone for broad eligibility (eg, geographic location and age), with potentially eligible participants invited to attend a medical assessment after providing written informed consent. Eligible participants were referred to the researcher for study enrollment, after which randomization and study treatment were initiated within 3 to 7 days.
Randomization and Blinding
The randomization schedule was developed by an independent researcher, using a permuted 8-block randomization schedule with 1:1 random allocation per site.18 Participants, clinicians, and researchers were blind to allocation, with only trial pharmacists aware of group allocation.
Clinical Interventions
Study Medications
Each nabiximols spray delivers 0.1 mL, comprising 2.7 mg of THC and 2.5 mg of cannabidiol (CBD); matching placebo used the same carrier and flavoring, but without cannabinoids. Medication canisters were identically labeled and dispensed weekly. Doses were titrated at weekly clinical reviews to optimize clinical effect (reduce cravings, withdrawal, and illicit cannabis use) and safety (minimize AEs). After a 3-day dose induction period, the maximum daily dose (to end week 12) was 32 oromucosal sprays (86.4 mg of THC and 80 mg of CBD) in 4 divided doses.
Clinical Reviews and Counseling Intervention
Weekly clinical sessions enabled monitoring and review of medication use and dose adequacy, experience of withdrawal, cravings, and AEs. Participants were offered 6 structured CBT-based individual counseling sessions, delivered by counselors or nurses who had completed a standardized training program.20 Participants who did not attend clinical sessions for more than 2 consecutive weeks were discontinued from study treatment. More detail regarding interventions is provided in the trial protocol in Supplement 1.18
Outcomes and Measures
The primary end point was self-reported total days of illicit cannabis use during weeks 1 to 12 (maximum, 84 days). Illicit cannabis use was quantified as the self-reported number of days of cannabis use in the preceding 28 days using Time Line Follow Back21 techniques at 4-week research interviews (weeks 1-4, 5-8, and 9-12). This variable was also used to calculate the proportion of participants achieving abstinence in any of the three 4-week periods, and the number of participants who achieved 50% or greater reduction in cannabis use in the preceding 28 days from baseline (weeks –4 to 0) to week 12 (weeks 9-12) research interviews. Urine drug tests measuring THC and metabolites (11-OH and 11-nor-9-carboxy-Δ9-tetrahydrocannabinol [THC-COOH]) were performed at research interviews to validate self-reported cannabis use. Urine samples were analyzed as previously reported22,23; in brief, cannabinoid analytes were hydrolyzed with β-glucuronidase, extracted via supported liquid extraction, and quantified via liquid chromatography–tandem mass spectrometry. Creatinine was measured colorimetrically via the Jaffe method (eAppendices 11-14, eTables 11-13, and eFigure 3 in Supplement 2).
Adverse events were evaluated during clinical assessments at weeks 2, 4, 8, and 12 by a study medical officer (N.L., A.D., N.P., and M.M.). Potential mental health concerns were monitored using the Brief Psychiatric Rating Scale24 at 4-week medical reviews. Self-reported aberrant medication behaviors (eg, selling or giving medication to others or repeated unauthorized dose escalation) were assessed at the researcher interviews using the modified Opioid-Related Behaviours In Treatment scale.25
Several secondary outcomes were assessed at 4-week research interviews, including the Cannabis Withdrawal Scale,26 Marijuana Craving Questionnaire,27 Cannabis Problems Questionnaire,28 Alcohol Use Disorders Identification Test,29 Fagerström Test for Nicotine Dependence,30 general health status and psychosocial function (36-item Short Form Survey31), and self-reported participation in crime (Opioid Treatment Index–Crime subscale32). Global satisfaction was assessed by asking participants (yes or no) “Would you recommend this medication to a friend seeking treatment?”
Treatment process measures were extracted from clinical records, including treatment retention (days in protocol treatment); medication doses; participation in counseling, medical, and nursing sessions; and reasons for study termination. Study blinding was tested by asking participants to estimate which medication group they were assigned to at research interviews at weeks 4, 8, and 12, with the last available interview used for analysis.
Statistical Analysis
Results for the primary efficacy measures and all secondary outcomes were obtained using a modified intention-to-treat data set, comprising all participants who were allocated to a study group and received at least 1 dose of medication (details of participants who were randomized and did not receive study medication are provided in eTable 1 in Supplement 2, but excluded from further analyses). Site differences for key variables at baseline were tested using simple regression (eAppendix 1 in Supplement 2). All P values were from 2-sided tests and results were deemed statistically significant at P < .05.
Primary Analysis
Analysis of the primary outcome, total days of cannabis use across the 12-week trial, was performed using a modified intention-to-treat data set with no imputed data (excluding participants who did not initiate study medication after randomization). To address concerns of missing data, a modified intention-to-treat data set with multilevel multiple-imputation was also conducted. A per-protocol analysis (comprising only participants who completed the 12 weeks of study treatment) is also reported.
The primary analysis was an analysis of covariance, with total days of illicit cannabis use across the 12-week trial as the outcome, with 4 factors: treatment (2-level factor: placebo vs nabiximols), site (4-level factor: Langton, St. George, Western Sydney, and Newcastle), treatment × site interaction, and number of days cannabis was used in the 4 weeks prior to baseline. In the event of significant omnibus effects for treatment, site, or the treatment × site interaction, estimates of the difference between factor levels were obtained using covariate-adjusted means, with P values adjusted for multiple comparisons using the Benjamini-Hochberg procedure.33
To assess whether the assumptions of a linear model (analysis of variance) approach were met, residuals were examined (eAppendix 5 and eFigures 1 and 2 in Supplement 2). The departure from normality was small, and as analysis of variance is robust to nonnormality, the primary analysis presented used a linear model. The Wilcoxon Mann-Whitney test was also conducted to examine for similarity in results using a nonparametric analysis.
Urine drug tests were used to validate self-reported cannabis use. However, urinary THC markers cannot be used to detect illicit cannabis use (reliant on detection of THC and its metabolites) in patients who were prescribed a THC-based medicine such as nabiximols; thus, analysis of urinary THC markers for verification of self-report was restricted to the placebo group. Two approaches were used: (1) a multiple regression model with log-transformed, creatinine-adjusted cannabinoid levels as the outcome and self-reported days’ use of illicit cannabis, participant age, and sex as predictors, and (2) analysis of concordance between 2 binary variables—self-reported abstinence in the past 28 days and urinalysis estimate of abstinence based on creatinine-adjusted THC-COOH levels34—consisting of receiver operating characteristic curve analysis and logistic regression of urinary THC on self-reported abstinence (eAppendices 11-14, eTables 11-13, and eFigure 3 in Supplement 2).
Secondary Analyses
Logistic regression was used to test group differences in the odds of achieving the following binary outcomes: any 4-week periods of abstinence during the 12-week trial; reducing the number of days of cannabis use by 50% or more between baseline (weeks –4 to 0) and week 12 (weeks 9-12); correctly guessing treatment allocation; and intention to recommend treatment to a friend (from the last available research interview). For count variables (number of counseling sessions, AEs, and aberrant medication behaviors) either Poisson or negative binomial regressions were used, dependent on dispersion of scores. Change in 4-week scores for several secondary variables (Cannabis Withdrawal Scale, Marijuana Craving Questionnaire, Cannabis Problems Questionnaire, Fagerström Test for Nicotine Dependence, Alcohol Use Disorders Identification Test, and 36-item Short Form Survey) was tested using factorial mixed models for repeated measures regression (MMRM), with treatment and time (4-level factor: weeks 0 [baseline], 4, 8, and 12) as the fixed effects, and participant identification as the random effect. These MMRMs yielded omnibus main and interaction effects as well as estimates of group differences at each time point, with P values adjusted for multiple comparisons using the Benjamini-Hochberg method. Factorial logistic MMRM was used to analyze between-group differences in odds of committing a drug-related crime during the course of the study. Treatment retention was analyzed using a Kaplan-Meier plot and a Cox proportional hazards regression model. Dose of medication was quantified by averaging participants’ self-reported number of sprays per day across the maintenance phase of the study in weeks 2 to 12 (week 1 was dose titration), which was then analyzed for group differences using simple regression. All statistical analyses were performed in R, version 3.4.1,35 using lme4,36 tidyverse,37 survival,38 and mice39 packages.
Results
Study Recruitment and Retention
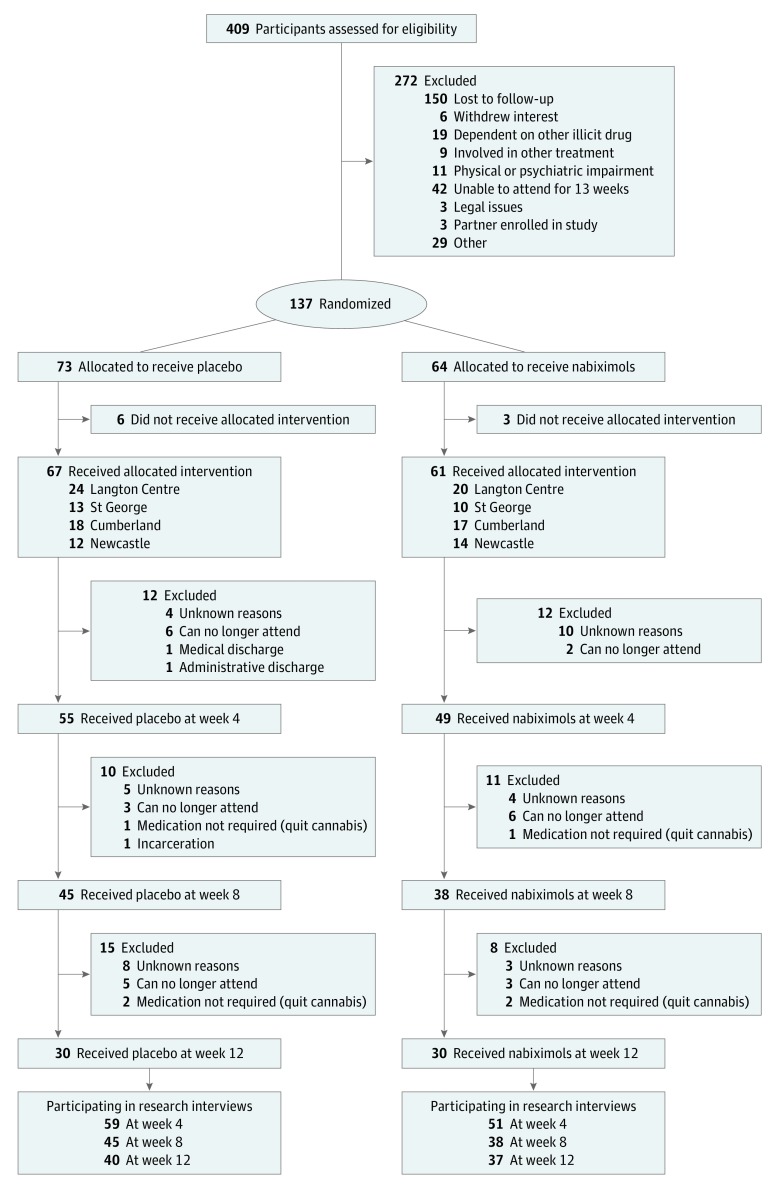
The CONSORT diagram is presented in Figure 1. A total of 409 individuals registered for screening and 272 (66.5%) were excluded, usually owing to being unable to be contacted, and were deemed lost to follow-up (n = 150) or unable to attend for treatment (n = 42). A total of 137 participants were enrolled, of whom 9 did not initiate treatment after randomization (6 placebo and 3 nabiximols; eAppendix 1 in Supplement 2), resulting in 128 participants for analysis (67 in the placebo group and 61 in the nabiximols group). Of these 128 participants, 77 (60.2%) completed the week 12 research interview (40 [59.7%] in the placebo group and 37 [60.7%] in the nabiximols group).
Figure 1. CONSORT Flow Diagram.
Baseline Characteristics
Baseline characteristics were similar between the intervention groups and are shown in Table 1. Participants had used a mean (SD) of 2.3 (2.1) g of cannabis per day on a mean (SD) of 25.7 (4.5) days in the past 28 days. All participants reported using cannabis flower and usually smoked using devices known as bongs (94 [73.4%]) or cigarettes known as joints (30 [23.4%]). There were no significant differences across sites at baseline except that 1 site had significantly higher age and duration of regular cannabis use than the other sites (eAppendix 1 in Supplement 2).
Table 1. Demographic and Baseline Characteristics of Participants.
| Characteristic | Participants, No. (%) | ||
|---|---|---|---|
| Placebo (n = 67) | Nabiximols (n = 61) | Total (N = 128) | |
| Age, mean (SD), y | 33.8 (10.3) | 36.2 (11.5) | 35.0 (10.9) |
| Female sex | 14 (20.9) | 16 (26.2) | 30 (23.4) |
| Born in Australia | 56 (83.6) | 51 (83.6) | 107 (83.6) |
| Aboriginal or Torres Strait Islander | 6 (9.0) | 4 (6.6) | 10 (7.8) |
| Tertiary education | 22 (32.8) | 27 (44.3) | 49 (38.3) |
| Employment as main source of income | 36 (53.7) | 35 (57.4) | 71 (55.5) |
| In a relationship | 27 (40.3) | 18 (29.5) | 45 (35.2) |
| Have ≥1 child | 23 (34.3) | 21 (34.4) | 44 (34.4) |
| Current legal problems | 6 (9.0) | 2 (3.3) | 8 (6.2) |
| Baseline cannabis use | |||
| No. of days cannabis used in last 28, mean (SD) | 25.6 (4.5) | 25.9 (4.6) | 25.7 (4.5) |
| Amount of cannabis used, mean (SD), g/d | 2.6 (2.5) | 2.0 (1.4) | 2.3 (2.1) |
| Age at first cannabis use, mean (SD), y (range, 5-40 y) | 15.0 (4.3) | 16.0 (3.4) | 15.5 (3.9) |
| Duration since first regular cannabis use, mean (SD), y | 15.2 (9.8) | 16.2 (9.9) | 15.7 (9.8) |
| ICD-10 score, mean (SD) (maximum = 8) | 7.2 (1.1) | 6.9 (1.2) | 7.1 (1.2) |
| Other variables | |||
| Fagerström nicotine dependence score, mean (SD) (maximum = 10)a | 2.1 (2.4) | 3.4 (2.8) | 2.7 (2.7) |
| AUDIT score, mean (SD) (maximum = 50) | 4.4 (5.1) | 4.7 (4.3) | 4.5 (4.7) |
| BPRS-18 score, mean (SD) (maximum = 128 | 23.6 (11.5) | 24.1 (12.0) | 23.8 (11.7) |
| Sheehan disability scale score, mean (SD) (maximum = 30) | 14.1 (8.2) | 12.9 (7.4) | 13.5 (7.8) |
| SF-36 score, mean (SD) (maximum = 100) | |||
| Physical functioning | 87.2 (18.4) | 86.2 (20.7) | 86.71 (19.4) |
| Role limitations owing to physical health | 36.6 (42.3) | 34.4 (41.4) | 35.57 (41.7) |
| Role limitations owing to emotional problems | 48.3 (44.7) | 48.1 (45.8) | 48.18 (45.0) |
| Energy or fatigue | 43.4 (18.3) | 40.8 (19.3) | 42.19 (18.8) |
| Emotional well-being | 56.1 (20.2) | 54.7 (18.1) | 55.06 (19.2) |
| Social functioning | 54.9 (30.6) | 59.1 (26.7) | 56.60 (28.8) |
| Pain | 69.8 (26.2) | 70.5 (25.6) | 70.12 (25.8) |
| General health | 49.3 (19.7) | 53.9 (21.6) | 51.48 (20.6) |
| OTI crime | |||
| Committed any drug-related crime in last month | 24 (35.8) | 21 (34.4) | 45 (35.2) |
| Committed any nondrug-related crime in the last monthb | 3 (4.6) | 1 (1.6) | 4 (3.2) |
Abbreviations: AUDIT, Alcohol Use Disorders Identification Test; BPRS, Brief Psychiatric Rating Scale; ICD-10, International Statistical Classification of Diseases and Related Health Problems, Tenth Revision; OTI, Opioid Treatment Index; SF-36, 36-item Short Form Survey.
Fagerström nicotine dependence score only for participants who identified as smokers (total, 106 [82.8%]; placebo, 58 [86.6%]; and nabiximols, 48 [78.7%]).
Refers to crimes related to selling cannabis to others. Does not include use or possession for personal use.
Participation in Treatment
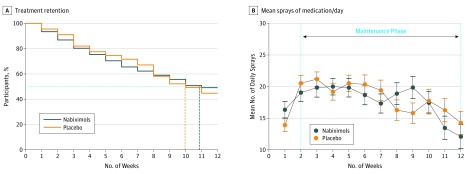
Treatment retention is shown in Figure 2A. A total of 60 participants (46.9%) completed the 12-week treatment protocol: 30 participants (44.8%) in the placebo group and 30 participants (49.2%) in the nabiximols group. There were no significant between-group differences.
Figure 2. Treatment Retention and Mean Number of Sprays of Medication per Day.
A, Treatment retention. The risk set at initiation of the study was 67 participants receiving placebo and 61 participants receiving nabiximols. Vertical broken lines indicate estimated median lifetime: the estimated time when half the original sample had discontinued treatment. B, Daily mean (SD) doses of medication used during the 12-week period. Maintenance phase excludes the first week when dose was being titrated.
Medication use is shown in Figure 2B. There was no significant between-group difference in the mean (SD) number of sprays per day during weeks 2 to 12 (placebo, 18.5 [9.5] sprays; nabiximols, 17.6 [9.5] sprays, equivalent to a mean [SD] of 47.5 [25.7] mg of THC and 44.0 [23.8] mg of CBD). Similarly, there were no significant between-group differences in the mean (SD) number of CBT sessions attended (2.4 [2.2] in the placebo group and 2.6 [2.3] in the nabiximols group).
Cannabis Use
Primary End Point: Frequency of Cannabis Use
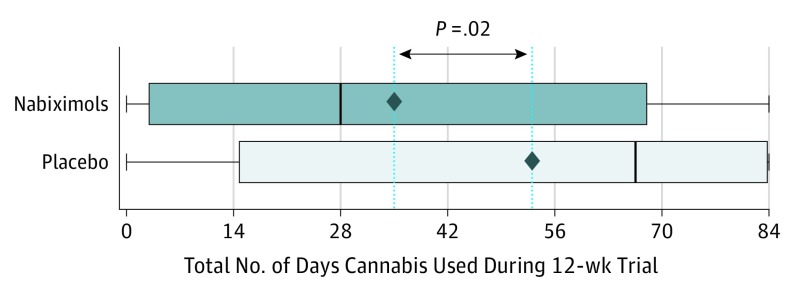
Figure 3 shows the means and distribution of days used during the trial for each group. The placebo group used illicit cannabis a mean (SD) of 53.1 [33.0] days (of 84 days) across the 12-week trial, compared with 35.0 [32.4] days in the nabiximols group, a significant difference of 18.6 days after adjusting for baseline cannabis use (95% CI, 3.5-33.7 days; P = .02).
Figure 3. Frequency of Cannabis Use During the 12-Week Trial.
Dotted vertical lines and diamonds indicate the mean number of days used for each group. The P value indicates the significance level of the treatment group coefficient from the regression of 84-day cannabis use on (1) treatment, (2) site, (3) treatment × site, and (4) baseline cannabis use, rounded to 2 decimal places. The solid vertical lines represent the median number of days used.
The effect of treatment when controlling for site, treatment × site interaction, and baseline use was similar irrespective of statistical approach (eAppendix 4 and eTable 3 in Supplement 2). With multilevel multiple-imputation, the estimated difference was 10.6 days (95% CI, 1.0-20.2 days; P = .04) and in the per-protocol analysis, the estimated difference was 20.3 days (95% CI, 3.2-37.4 days; P = .02) (eAppendices 2 and 3 and eTable 2 in Supplement 2). A nonparametric Wilcoxon-Mann-Whitney rank sum test estimated a 16.0-day difference in the location of the distributions of the treatment groups (U = 722; P = .04). Although there were differences in cannabis use across sites, the omnibus interaction between treatment and site was nonsignificant (eAppendix 4 and eTable 3 in Supplement 2).
Secondary Outcomes
Of the 104 participants who were still participating in the study at the 12-week research interview, 23 (22.1%) had 1 or more 4-week periods of abstinence during the trial: 10 of 55 (18.2%) in the placebo group and 13 of 49 (26.5%) in the nabiximols group, a nonsignificant difference (odds ratio, 1.63; 95% CI, 0.55-4.90; P = .31). A significantly lower proportion of the placebo group (11 of 38 [28.9%]) reduced their cannabis use by 50% or more from baseline to week 12 than the nabiximols group (20 of 37 [54.1%]) (odds ratio, 0.35; 95% CI, 0.13-0.90; P = .03; number needed to treat, 4; 95% CI, 2-29). Cannabis-related problems (Cannabis Problems Questionnaire), withdrawal (Cannabis Withdrawal Scale), and cravings (Marijuana Craving Questionnaire) improved in both groups over time, but with no significant between-group differences (Table 2).
Table 2. Raw Mean (SD) Values, Main and Interaction Effects, and Simple Effects for Secondary Variables Across the 12-Week Trial.
| Variable | Mean (SD) Valuea | Omnibus Effectb | Adjusted P Valuec | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Week 0 | Week 4 | Week 8 | Week 12 | |||||||
| Placebo | Nabiximols | Placebo | Nabiximols | Placebo | Nabiximols | Placebo | Nabiximols | |||
| Cannabis Withdrawal Scale score | 65.1 (37.0) | 64.8 (43.5) | 47.5 (37.5) | 44.7 (27.7) | 44.2 (41.0) | 42.6 (32.7) | 43.6 (37.3) | 30.7 (28.9) | Treatment | .56 |
| Time | <.001 | |||||||||
| Estimated difference (95% CI)d | −0.4 (−13.3 to 12.6) | −6.4 (−20.7 to 8.0) | −2.2 (−18.1 to 13.7) | −14.1 (−31.4 to 3.2) | Treatment × time | .60 | ||||
| Marijuana Craving Questionnaire score | 48.2 (16.4) | 46.7 (17.9) | 36.8 (15.8) | 34.3 (13.8) | 34.0 (14.0) | 27.7 (13.8) | 31.2 (15.2) | 27.2 (18.9) | Treatment | .29 |
| Estimated difference (95% CI) | −1.5 (−7.0 to 4.1) | −1.4 (−7.6 to 4.9) | −5.7 (−12.6 to 1.1) | −3.4 (−10.3 to 3.5) | Time | <.001 | ||||
| Treatment × time | .56 | |||||||||
| Cannabis Problems Questionnaire score | 118.1 (44.5) | 112.0 (52.8) | 81.8 (50.3) | 81.3 (48.9) | 70.2 (48.5) | 61.6 (54.2) | 52.0 (43.4) | 42.4 (49.8) | Treatment | .56 |
| Estimated difference (95% CI) | −6.0 (−23.2 to 11.1) | 1.6 (−16.7 to 19.8) | −6.3 (−26.5 to 14.0) | −4.4 (−24.7 to 15.9) | Time | <.001 | ||||
| Treatment × time | .91 | |||||||||
| Fagerström Test for Nicotine Dependence score | 1.9 (2.4) | 2.8 (2.8) | 1.7 (2.4) | 2.9 (3.1) | 2.0 (2.6) | 2.6 (3.0) | 1.6 (2.3) | 2.8 (3.2) | Treatment | .31 |
| Estimated difference (95% CI) | 0.9 (−0.1 to 1.8) | 0.0 (−0.6 to 0.6) | −0.3 (−1.0 to 0.3) | −0.1 (−0.7 to 0.6) | Time | .89 | ||||
| Treatment × time | .85 | |||||||||
| AUDIT score | 4.4 (5.1) | 4.7 (4.3) | 5.3 (5.3) | 3.6 (3.6) | 4.6 (4.2) | 4.7 (5.8) | 5.1 (5.4) | 4.1 (5.0) | Treatment | .69 |
| Time | .91 | |||||||||
| Estimated difference (95% CI) | 0.3 (−1.3 to 2.0) | −1.7 (−3.1 to 0.3) | −0.2 (−1.7 to 1.4) | −1.2 (−2.8 to 0.4) | Treatment × time | .28 | ||||
| SF-36 score | ||||||||||
| Physical | 87.2 (18.4) | 86.2 (20.7) | 86.5 (19.4) | 89.9 (17.3) | 86.6 (19.1) | 88.0 (18.6) | 90.9 (15.4) | 92.4 (13.2) | Treatment | .69 |
| Estimated difference (95% CI) | −1.08 (−7.5 to 5.4) | 4.7 (−1.8 to 11.2) | 3.11 (−4.1 to 10.3) | 2.89 (−4.3 to 10.1) | Time | .28 | ||||
| Treatment × time | .69 | |||||||||
| Role limitation–physical | 36.6 (42.3) | 34.4 (41.4) | 35.5 (41.0) | 28.1 (39.1) | 36.6 (46.1) | 20.7 (34.0) | 25.0 (40.0) | 27.0 (41.8) | Treatment | .56 |
| Time | .43 | |||||||||
| Estimated difference (95% CI) | −2.1 (−16.4 to 12.2) | −6.3 (−22.5 to 10.0) | −14.4 (−32.4 to 3.6) | 5.2 (−12.8 to 23.3) | Treatment × time | .48 | ||||
| Role limitation–emotional | 48.3 (44.7) | 48.1 (45.8) | 42.4 (43.3) | 43.5 (44.2) | 43.4 (44.6) | 28.6 (38.9) | 29.9 (41.0) | 36.1 (46.0) | Treatment | .85 |
| Estimated difference (95% CI) | −0.2 (−15.5 to 15.1) | −0.0 (−15.5 to 15.5) | −14.5 (−31.8 to 2.8) | 6.2 (−11.3 to 23.7) | Time | .001 | ||||
| Treatment × time | .43 | |||||||||
| Energy | 43.4 (18.3) | 40.8 (19.3) | 48.4 (18.0) | 47.8 (16.9) | 47.8 (19.6) | 48.6 (18.9) | 54.4 (19.0) | 48.8 (23.3) | Treatment | .56 |
| Estimated difference (95% CI) | −2.6 (−9.2 to 3.9) | 2.4 (−4.2 to 9.0) | 1.3 (−6.0 to 8.6) | −4.7 (−12.0 to 2.7) | Time | <.001 | ||||
| Treatment × time | .56 | |||||||||
| Emotional well-being | 56.1 (20.2) | 54.7 (18.1) | 61.8 (20.3) | 61.5 (17.6) | 62.4 (19.9) | 62.6 (19.0) | 65.1 (22.7) | 64.1 (20.4) | Treatment | .69 |
| Estimated difference (95% CI) | −1.5 (−8.3 to 5.3) | 1.4 (−5.6 to 8.3) | −0.6 (−8.3 to 7.2) | −2.1 (−9.9 to 5.6) | Time | <.001 | ||||
| Treatment × time | .91 | |||||||||
| Social | 54.9 (30.6) | 59.1 (26.7) | 62.1 (29.5) | 63.7 (27.2) | 68.0 (28.5) | 64.3 (25.4) | 71.6 (28.0) | 68.0 (29.7) | Treatment | .97 |
| Estimated difference (95% CI) | 4.3 (−5.6 to 14.1) | −2.0 (−12.5 to 8.5) | −7.4 (−19.1 to 4.8) | −8.2 (−20.0 to 3.6) | Time | .001 | ||||
| Treatment × time | .61 | |||||||||
| Pain | 69.8 (26.2) | 70.5 (25.6) | 73.7 (26.7) | 81.5 (22.4) | 79.7 (27.8) | 76.9 (26.2) | 77.8 (24.0) | 82.7 (22.4) | Treatment | .61 |
| Estimated difference (95% CI) | 0.6 (−8.1 to 9.4) | 7.2 (−2.0 to 16.4) | −1.3 (−11.5 to 8.9) | 3.3 (−6.9 to 13.5) | Time | <.001 | ||||
| Treatment × time | .56 | |||||||||
| General | 49.3 (19.7) | 53.9 (21.6) | 54.7 (19.5) | 54.6 (23.6) | 52.6 (22.5) | 60.0 (24.0) | 55.8 (22.2) | 58.4 (22.4) | Treatment | .60 |
| Estimated difference (95% CI) | 4.5 (−3.0 to 12.0) | −3.7 (−10.5 to 3.1) | 1.6 (−6.0 to 9.2) | −4.5 (−12.1 to 3.1) | Time | .45 | ||||
| Treatment × time | .56 | |||||||||
| OTI drug-related crime, No. (%)e,f | 24 (35.8) | 21 (34.4) | 12 (20.3) | 6 (11.8) | 13 (28.9) | 8 (21.1) | 13 (32.5) | 4 (10.8) | Treatment | .28 |
| Odds ratio (95% CI) | 0.9 (0.1 to 7.2) | 0.3 (0.0 to 2.0) | 0.4 (0.1 to 3.4) | 0.1 (0.0 to 0.6) | Time | .001 | ||||
| Treatment × time | .40 | |||||||||
Abbreviations: AUDIT, Alcohol Use Disorders Identification Test; OTI, Opioid Treatment Index; Pl, Placebo; SF-36, 36-item Short Form Survey.
Negative estimates indicate nabiximols scoring lower than placebo.
Treatment = main effect of treatment group averaged across time points; time = main effect of time averaged across treatment groups; treatment × time = interaction between treatment group and time.
For omnibus main and interaction effects adjusted for multiple comparisons using the Benjamini-Hochberg procedure for controlling the false discovery rate.
Estimated difference between nabiximols and placebo groups at the time point in question. 95% CIs within each regression model are uncorrected.
Number who committed 1 or more drug-related crimes in the previous 4 weeks.
Omnibus statistics obtained from type 3 Wald χ2 tests.
Validation of Self-reported Cannabis Use
Urinalysis indicated that the self-reported number of days using cannabis was significantly positively associated with urinary THC-COOH levels (eAppendix 11, eTable 11, and eFigure 3 in Supplement 2). The odds of having a negative test result for THC-COOH after self-reported abstinence were 8 times higher than after self-reported use (odds ratio, 7.9; 95% CI, 2.5-26.0; P < .001), confirming the validity of self-reported cannabis use (eAppendices 13 and 14 and eTables 12 and 13 in Supplement 2).
AEs and Aberrant Medication Use
Study medications were generally well tolerated, with no significant between-group differences in AEs (eAppendix 6 and eTables 4-6 in Supplement 2). A total of 32 participants (25.0%) reported an AE (placebo, 17 of 67 [25.4%]; and nabiximols, 15 of 61 [24.6%]), with 14 participants (10.9%) reporting 2 or more AEs. Headache was the only AE reported by more than 5% of participants (total, 7 of 128 [5.5%]; placebo, 2 of 67 [3.0%]; and nabiximols, 5 of 61 [8.2%]). One serious AE was reported by a participant in the placebo group who was hospitalized for suicidal ideation in the first week in the study and subsequently discontinued treatment. Brief Psychiatric Rating Scale scores were stable across the 2 groups over time, with no significant main effects of treatment or time, nor treatment × time interaction.
A total of 21 of all 70 participants who completed the Opioid-Related Behaviours In Treatment scale at week 14 (30.0%; placebo, 14 of 37 [37.8%]; nabiximols, 7 of 33 [21.2%]) reported any aberrant medication behaviors (eAppendices 7 and 8 and eTables 7 and 8 in Supplement 2), with no significant group differences. The most common behaviors were giving or selling medication to someone else (12 of 70 [17.1%]) and altering the dose in some other way (10 of 70 [14.3%]), referring to unauthorized dose escalation.
General Health and Patient Satisfaction Outcomes
Data on summary general health and psychosocial functional outcomes, other substance use, and crime are shown in Table 2. Omnibus tests revealed that, across both groups, there was general improvement in several outcomes (36-item Short Form Survey and Opioid Treatment Index–Crime subscale), with significant main effects of time, but no between-group differences, nor interactions between treatment and time. There were no significant changes over time in other substance use (Fagerström Test for Nicotine Dependence and Alcohol Use Disorders Identification Test), nor any between-group differences or interactions.
There were high levels of global satisfaction with the medication, with most participants indicating they would recommend the medication to a friend seeking treatment (placebo, 41 of 55 [74.5%]; nabiximols, 42 of 51 [82.4%]).
Testing the Study Blinding
The proportion of participants who correctly guessed their treatment allocation was significantly lower in the placebo group (27 of 55 [49.1%]) than the nabiximols group (42 of 51 [82.4%; odds ratio, 0.21; 95% CI, 0.08-0.50; P = .001).
Discussion
Our study demonstrates that cannabinoid agonist treatment, in combination with psychosocial interventions, reduced illicit cannabis use in patients with cannabis dependence who were seeking treatment. Participants who received nabiximols used illicit cannabis on two-thirds as many days (mean, 35 of 84 days [41.7%]) as those allocated to placebo (mean, 53 of 84 days [63.1%]), an estimated mean difference of 18.6 days, representing both a statistically and clinically meaningful reduction. This treatment effect was consistent across study sites, suggesting that the benefits of nabiximols are generalized across different treatment settings. The reductions in illicit cannabis use, and a safer route of administration (compared with smoked cannabis using bongs or joints that are associated with chronic respiratory problems4,5) suggest the harm reduction benefits of cannabinoid agonist treatment.
Limitations
Our findings also highlight some limitations of this treatment: only half of the participants were retained in treatment during the 12-week period, illicit cannabis was still used on 41.7% of possible days, and abstinence from illicit cannabis was achieved by only a minority of patients. Although our treatment retention of 46.9% at 12 weeks is comparable with prior randomized clinical trials of cannabinoid agonist treatment (55% at 11 weeks16 and 67% at 12 weeks17), the limited treatment retention across these studies highlights the fact that cannabinoid agonist treatment is not effective for or acceptable to all patients. Further research is required to better understand the reasons for treatment dropout from trials40—for example, some participants in both groups thought they were receiving placebo, which may undermine treatment retention—and/or whether improvements in the model of care (eg, treatment duration, cannabinoid preparation, dose, psychosocial interventions, or better targeting of patients) can enhance future treatment outcomes. For example, our findings of reduced cannabis use with nabiximols is in contrast with findings from a trial of fixed-dose dronabinol that suggested no benefit vs placebo.16 It remains unclear whether our flexible dose schedule, the pharmacokinetic profile of nabiximols (higher bioavailability and more rapid onset of action), and/or the combination of THC with CBD (anticraving41,42 and neuroprotective43,44 properties in cannabis users), conveys advantages vs dronabinol.
In our study, as in previous studies, high doses of THC-based medications were well tolerated in this patient group, reflecting their pharmacologic tolerance to THC. Patients with severe mental health problems, such as psychosis or bipolar affective disorder, were excluded from the study, and caution should remain regarding the use of THC-based medicines in such patients.
Despite the nabiximols group reporting significantly less illicit cannabis use than the control group, participants in both groups improved to a comparable degree on a range of secondary cannabis-related (withdrawal and cravings) and general health and psychosocial outcomes (eg, cannabis-related problems and the 36-item Short Form Survey). The interpretation of withdrawal and cannabis scores is difficult in the context of an outpatient study in which most participants in the control group used cannabis on most days throughout the study.
There are several possible explanations for the comparable improvements in general health outcomes: (1) the treatment elements consistent to both groups (counseling, case management, medical and nursing reviews, and therapeutic rapport) were associated with improved general health; (2) the reductions in illicit cannabis use in the control group, while not as great as in the nabiximols group, were nevertheless sufficient to lead to improvements in general health; and (3) participants experienced a possible therapeutic placebo effect related to expectancy issues (particularly as half of the participants in the placebo group thought they were receiving nabiximols). Just as important, nabiximols—even at high doses—does not appear to prevent improvements in areas such as mental health, addressing potential concerns that a THC-based medication may contribute to persistent mental health problems.
Other limitations are worth noting, particularly the low (60.2%) follow-up of participants completing week 12 research interviews. Although statistical analysis (multilevel multiple-imputation) that imputed for missing data resulted in similar findings to nonimputed and per-protocol analyses, the 60.2% research follow-up rate suggests that some caution is warranted in interpreting our findings.
Another limitation is our reliance on self-reported measures of illicit cannabis use, as we are unable to differentiate prescribed from unsanctioned THC use in urine test results at this time. Although the urine drug screening results in the placebo arm indicate adequate validity of self-report in this study, further research is required to develop objective markers of illicit use, for both clinical and research purposes. Finally, our study examined a 12-week medication period, and open-label follow-up studies of longer duration (eg, 6 or 12 months) are needed to establish the safety and effectiveness under real-world conditions.
Conclusions
Cannabinoid agonist treatment is unlikely to be an approach relevant to all cannabis users seeking treatment, as evidenced by the large numbers of individuals who did not complete the study screening process, and the modest 12-week treatment retention rates. Whereas nicotine-agonist and opioid-agonist treatments are considered front-line therapies, our findings suggest a more cautious approach for cannabinoid agonist treatment at this time. The control group demonstrated some benefits from treatment, confirming previous research that psychosocial interventions (CBT and case management) without medication can be effective for some patients. Although further research is required to replicate our findings and to refine how cannabinoid agonist treatment is delivered, our study suggests cannabinoid agonist treatment to be a promising approach for treating patients with cannabis dependence, particularly for those who cannot sustain reductions in illicit cannabis use with counseling-only interventions, in a stepped care approach.
Trial Protocol
eTable 1. Comparison of Characteristics of Participants Who Were Randomized but Received No Medication to Those Who Were Randomized and Commenced Treatment
eAppendix 1. Site Comparisons of Biohistorical Values at Baseline
eAppendix 2. Primary Analysis: Effect of Treatment on Total Days of Cannabis Use Across the 12-Week Trial
eTable 2. Effect of Treatment on Total Days Used From Three Different Datasets, Controlling for Site, Treatment x Site Interaction, and Baseline Use
eAppendix 3. Note on Multiple-Imputation Analysis
eTable 3. Mean Days Used Across the 12-Week Trial by Site and Treatment Group
eAppendix 4. Interpretation
eFigure 1. QQ-Plots of Residuals for 12-Week Cannabis Use
eAppendix 5. Analysis
eFigure 2. Histogram of Model Residuals for 12-Week Cannabis Use
eTable 4. Adverse Event Reported by Group
eTable 5. Comparison of Numbers of Each Type of Adverse Event and Total Adverse Events
eTable 6. Group Difference in Incidence Rate of AEs
eAppendix 6. Analysis and Interpretation
eTable 7. Incidence Rates of Aberrant Behaviours by Group (ORBIT)
eAppendix 7. Analysis
eTable 8. Comparison of Incidence Rate of Aberrant Behaviours Between Groups
eAppendix 8. Interpretation
eTable 9. Comparison of Incidence Rate of Aberrant Behaviours Across Groups
eAppendix 9. Analysis
eTable 10. Pearson’s Chi-Square Test of Between-Group Difference in Rate of Aberrant Behaviours
eAppendix 10. Interpretation
eAppendix 11. Analysis 1: Testing the Ability of Self-Reported Days Use to Predict Urinary Cannabinoid Concentration
eTable 11. Results of Regressing Three Cannabinoids on Self-Reported Days Use of Illicit Cannabis, Age, and Gender at Four Different Timepoints in the Placebo Group
eFigure 3. Results of Regressing Three Cannabinoids on Self-Reported Days Use of Illicit Cannabis, Age, Gender, and Age First Used Cannabis, at Four Different Timepoints in the Placebo Group
eAppendix 12. Interpretation
eAppendix 13. Method 2
eTable 12. Confusion Matrix of Numbers in the Placebo Group With Self-Reported Cannabis Use or Abstinence Versus Numbers Who Met Threshold Urinary THC-COOH Levels (Left) and Receiver Operating Characteristics Analysis (Right)
eTable 13. Relationship Between Self-Reported Cannabis Use and Urinary THC-COOH Levels
eAppendix 14. Interpretation
Data Sharing Statement
References
- 1.UN Office on Drugs and Crime World Drug Report 2013. Vienna, Austria: UN Office on Drugs and Crime; 2013. [Google Scholar]
- 2.UN Office on Drugs and Crime World Drug Report 2015. Vienna, Austria: UN Office on Drugs and Crime; 2015. [Google Scholar]
- 3.Australian Institute of Health and Welfare 2016 National Drug Strategy Household Survey: Preliminary Findings. Canberra, Australia: Australian Institute of Health and Welfare; 2017. [Google Scholar]
- 4.Hall W, Degenhardt L. Adverse health effects of non-medical cannabis use. Lancet. 2009;374(9698):1383-1391. doi: 10.1016/S0140-6736(09)61037-0 [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization The Health and Social Effects of Nonmedical Cannabis Use. Geneva, Switzerland: World Health Organization; 2016. [Google Scholar]
- 6.Roffman RA, Stephens RS. Cannabis Dependence: Its Nature, Consequences, and Treatment. Cambridge, UK: Cambridge University Press; 2006. doi: 10.1017/CBO9780511544248 [DOI] [Google Scholar]
- 7.Allsop DJ, Copeland J, Lintzeris N, et al. Nabiximols as an agonist replacement therapy during cannabis withdrawal: a randomized clinical trial. JAMA Psychiatry. 2014;71(3):281-291. doi: 10.1001/jamapsychiatry.2013.3947 [DOI] [PubMed] [Google Scholar]
- 8.Johnston J, Lintzeris N, McGregor I, Allsop DJ, Helliwell D, Winstock A. A double blind, randomised, placebo controlled trial of lithium carbonate for the management of cannabis withdrawal: paper 220. Drug Alcohol Rev. 2013;32:43. [Google Scholar]
- 9.Gates PJ, Sabioni P, Copeland J, Le Foll B, Gowing L. Psychosocial interventions for cannabis use disorder. Cochrane Database Syst Rev. 2016;(5):CD005336. doi: 10.1002/14651858.CD005336.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Danovitch I, Gorelick DA. State of the art treatments for cannabis dependence. Psychiatr Clin North Am. 2012;35(2):309-326. doi: 10.1016/j.psc.2012.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vandrey R, Haney M. Pharmacotherapy for cannabis dependence: how close are we? CNS Drugs. 2009;23(7):543-553. doi: 10.2165/00023210-200923070-00001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Darke S, Farrell M. Would legalizing illicit opioids reduce overdose fatalities? implications from a natural experiment. Addiction. 2014;109(8):1237-1242. doi: 10.1111/add.12456 [DOI] [PubMed] [Google Scholar]
- 13.Haney M, Hart CL, Vosburg SK, Comer SD, Reed SC, Foltin RW. Effects of THC and lofexidine in a human laboratory model of marijuana withdrawal and relapse. Psychopharmacology (Berl). 2008;197(1):157-168. doi: 10.1007/s00213-007-1020-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Huestis MA, Sampson AH, Holicky BJ, Henningfield JE, Cone EJ. Characterization of the absorption phase of marijuana smoking. Clin Pharmacol Ther. 1992;52(1):31-41. doi: 10.1038/clpt.1992.100 [DOI] [PubMed] [Google Scholar]
- 15.Karschner EL, Darwin WD, Goodwin RS, Wright S, Huestis MA. Plasma cannabinoid pharmacokinetics following controlled oral Δ9-tetrahydrocannabinol and oromucosal cannabis extract administration. Clin Chem. 2011;57(1):66-75. doi: 10.1373/clinchem.2010.152439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Levin FR, Mariani JJ, Brooks DJ, Pavlicova M, Cheng W, Nunes EV. Dronabinol for the treatment of cannabis dependence: a randomized, double-blind, placebo-controlled trial. Drug Alcohol Depend. 2011;116(1-3):142-150. doi: 10.1016/j.drugalcdep.2010.12.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Trigo JM, Soliman A, Quilty LC, et al. Nabiximols combined with motivational enhancement/cognitive behavioral therapy for the treatment of cannabis dependence: a pilot randomized clinical trial. PLoS One. 2018;13(1):e0190768. doi: 10.1371/journal.pone.0190768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bhardwaj AK, Allsop DJ, Copeland J, et al. ; Agonist Replacement for Cannabis Dependence (ARCD) study group . Randomised controlled trial (RCT) of cannabinoid replacement therapy (nabiximols) for the management of treatment-resistant cannabis dependent patients: a study protocol. BMC Psychiatry. 2018;18(1):140. doi: 10.1186/s12888-018-1682-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.World Health Organization International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10). 2nd ed. Geneva, Switzerland: World Health Organization; 2005. [Google Scholar]
- 20.Copeland J. Marijuana Brief Intervention: An SBIRT Approach. Center City, MN: Hazelden Publishing; 2017. [Google Scholar]
- 21.Sobell LC, Sobell MB. Timeline follow-back: a technique for assessing self-reported alcohol consumption In: Litten RZ, Allen JP, eds. Measuring Alcohol Consumption: Psychosocial and Biochemical Methods. Totowa, NJ: Humana Press Inc; 1992:41-72. doi: 10.1007/978-1-4612-0357-5_3 [DOI] [Google Scholar]
- 22.Suraev A, Lintzeris N, Stuart J, et al. Composition and use of cannabis extracts for childhood epilepsy in the Australian community. Sci Rep. 2018;8(1):10154. doi: 10.1038/s41598-018-28127-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kevin RC, Allsop DJ, Lintzeris N, Dunlop AJ, Booth J, McGregor IS. Urinary cannabinoid levels during nabiximols (Sativex)-medicated inpatient cannabis withdrawal. Forensic Toxicol. 2017;35(1):33-44. doi: 10.1007/s11419-016-0330-0 29367861 [DOI] [Google Scholar]
- 24.Overall JE, Gorham DR. The Brief Psychiatric Rating Scale. Psychol Rep. 1962;10(3):799-812. doi: 10.2466/pr0.1962.10.3.799 [DOI] [Google Scholar]
- 25.Larance B, Bruno R, Lintzeris N, et al. Development of a brief tool for monitoring aberrant behaviours among patients receiving long-term opioid therapy: the Opioid-Related Behaviours In Treatment (ORBIT) scale. Drug Alcohol Depend. 2016;159:42-52. doi: 10.1016/j.drugalcdep.2015.11.026 [DOI] [PubMed] [Google Scholar]
- 26.Allsop DJ, Norberg MM, Copeland J, Fu S, Budney AJ. The Cannabis Withdrawal Scale development: patterns and predictors of cannabis withdrawal and distress. Drug Alcohol Depend. 2011;119(1-2):123-129. doi: 10.1016/j.drugalcdep.2011.06.003 [DOI] [PubMed] [Google Scholar]
- 27.Heishman SJ, Singleton EG, Liguori A. Marijuana Craving Questionnaire: development and initial validation of a self-report instrument. Addiction. 2001;96(7):1023-1034. doi: 10.1046/j.1360-0443.2001.967102312.x [DOI] [PubMed] [Google Scholar]
- 28.Copeland J, Gilmour S, Gates P, Swift W. The Cannabis Problems Questionnaire: factor structure, reliability, and validity. Drug Alcohol Depend. 2005;80(3):313-319. doi: 10.1016/j.drugalcdep.2005.04.009 [DOI] [PubMed] [Google Scholar]
- 29.Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption—II. Addiction. 1993;88(6):791-804. doi: 10.1111/j.1360-0443.1993.tb02093.x [DOI] [PubMed] [Google Scholar]
- 30.Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO. The Fagerström Test for Nicotine Dependence: a revision of the Fagerström Tolerance Questionnaire. Br J Addict. 1991;86(9):1119-1127. doi: 10.1111/j.1360-0443.1991.tb01879.x [DOI] [PubMed] [Google Scholar]
- 31.Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36), I: conceptual framework and item selection. Med Care. 1992;30(6):473-483. doi: 10.1097/00005650-199206000-00002 [DOI] [PubMed] [Google Scholar]
- 32.Darke S, Hall W, Wodak A, Heather N, Ward J. Development and validation of a multi-dimensional instrument for assessing outcome of treatment among opiate users: the Opiate Treatment Index. Br J Addict. 1992;87(5):733-742. doi: 10.1111/j.1360-0443.1992.tb02719.x [DOI] [PubMed] [Google Scholar]
- 33.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Series B Stat Methodol. 1995;57(1):289-300. [Google Scholar]
- 34.Baker NL, Gray KM, Sherman BJ, et al. Biological correlates of self-reported new and continued abstinence in cannabis cessation treatment clinical trials. Drug Alcohol Depend. 2018;187:270-277. doi: 10.1016/j.drugalcdep.2018.03.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.R: a language and environment for statistical computing [computer program]. Vienna, Austria: R Foundation for Statistical Computing; 2016.
- 36.Bates D, Mächler M, Bolker B, Steve W. Fitting linear mixed-effects models using lme4. J Stat Softw. 2015;67(1):1-48. doi: 10.18637/jss.v067.i01 [DOI] [Google Scholar]
- 37.Wickham H. tidyverse: Easily install and load the ’tidyverse.’ R package version 1.2.1. https://cran.r-project.org/web/packages/tidyverse/index.html. Accessed March 12, 2018.
- 38.Therneau TM, Grambsch PM. Modeling Survival Data: Extending the Cox Model. New York, NY: Springer Science & Business Media; 2013. [Google Scholar]
- 39.Van Buuren S, Groothuis-Oudshoorn K. mice: Multivariate imputation by chained equations in R. J Stat Softw. 2011;45(3):1-67. doi: 10.18637/jss.v045.i03 [DOI] [Google Scholar]
- 40.Teruya C, Schwartz RP, Mitchell SG, et al. Patient perspectives on buprenorphine/naloxone: a qualitative study of retention during the Starting Treatment With Agonist Replacement Therapies (START) Study. J Psychoactive Drugs. 2014;46(5):412-426. doi: 10.1080/02791072.2014.921743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Morgan CJ, Freeman TP, Schafer GL, Curran HV. Cannabidiol attenuates the appetitive effects of Δ 9-tetrahydrocannabinol in humans smoking their chosen cannabis. Neuropsychopharmacology. 2010;35(9):1879-1885. doi: 10.1038/npp.2010.58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Crippa JAS, Hallak JEC, Machado-de-Sousa JP, et al. Cannabidiol for the treatment of cannabis withdrawal syndrome: a case report. J Clin Pharm Ther. 2013;38(2):162-164. doi: 10.1111/jcpt.12018 [DOI] [PubMed] [Google Scholar]
- 43.Hermann D, Sartorius A, Welzel H, et al. Dorsolateral prefrontal cortex N-acetylaspartate/total creatine (NAA/tCr) loss in male recreational cannabis users. Biol Psychiatry. 2007;61(11):1281-1289. doi: 10.1016/j.biopsych.2006.08.027 [DOI] [PubMed] [Google Scholar]
- 44.Hermann D, Schneider M. Potential protective effects of cannabidiol on neuroanatomical alterations in cannabis users and psychosis: a critical review. Curr Pharm Des. 2012;18(32):4897-4905. doi: 10.2174/138161212802884825 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial Protocol
eTable 1. Comparison of Characteristics of Participants Who Were Randomized but Received No Medication to Those Who Were Randomized and Commenced Treatment
eAppendix 1. Site Comparisons of Biohistorical Values at Baseline
eAppendix 2. Primary Analysis: Effect of Treatment on Total Days of Cannabis Use Across the 12-Week Trial
eTable 2. Effect of Treatment on Total Days Used From Three Different Datasets, Controlling for Site, Treatment x Site Interaction, and Baseline Use
eAppendix 3. Note on Multiple-Imputation Analysis
eTable 3. Mean Days Used Across the 12-Week Trial by Site and Treatment Group
eAppendix 4. Interpretation
eFigure 1. QQ-Plots of Residuals for 12-Week Cannabis Use
eAppendix 5. Analysis
eFigure 2. Histogram of Model Residuals for 12-Week Cannabis Use
eTable 4. Adverse Event Reported by Group
eTable 5. Comparison of Numbers of Each Type of Adverse Event and Total Adverse Events
eTable 6. Group Difference in Incidence Rate of AEs
eAppendix 6. Analysis and Interpretation
eTable 7. Incidence Rates of Aberrant Behaviours by Group (ORBIT)
eAppendix 7. Analysis
eTable 8. Comparison of Incidence Rate of Aberrant Behaviours Between Groups
eAppendix 8. Interpretation
eTable 9. Comparison of Incidence Rate of Aberrant Behaviours Across Groups
eAppendix 9. Analysis
eTable 10. Pearson’s Chi-Square Test of Between-Group Difference in Rate of Aberrant Behaviours
eAppendix 10. Interpretation
eAppendix 11. Analysis 1: Testing the Ability of Self-Reported Days Use to Predict Urinary Cannabinoid Concentration
eTable 11. Results of Regressing Three Cannabinoids on Self-Reported Days Use of Illicit Cannabis, Age, and Gender at Four Different Timepoints in the Placebo Group
eFigure 3. Results of Regressing Three Cannabinoids on Self-Reported Days Use of Illicit Cannabis, Age, Gender, and Age First Used Cannabis, at Four Different Timepoints in the Placebo Group
eAppendix 12. Interpretation
eAppendix 13. Method 2
eTable 12. Confusion Matrix of Numbers in the Placebo Group With Self-Reported Cannabis Use or Abstinence Versus Numbers Who Met Threshold Urinary THC-COOH Levels (Left) and Receiver Operating Characteristics Analysis (Right)
eTable 13. Relationship Between Self-Reported Cannabis Use and Urinary THC-COOH Levels
eAppendix 14. Interpretation
Data Sharing Statement