Abstract
Background
primary myelofibrosis (PMF) is a myeloproliferative neoplasm which is associated with clonal molecular and cytogenetic abnormalities (CA) and varied clinical manifestations. While various CA have been previously described, t(15; 17) has not been reported in association with this condition.
Case presentation
A 69-year-old male presented with constitutional symptoms, cytopenias and bone marrow biopsy revealed immature blasts with fibrosis. Cytogenetic analysis showed a t(15;17) which initially suggested a diagnosis of acute promyelocytic leukemia (APL). However, flourescence in situ hybridization (FISH) and reverse transcriptase polymerase chain reaction (RT-PCR) studies were negative for transcripts promyelocytic leukemia (PML) gene and retinoic acid receptor alpha (RARA) or PML-RARA fusion. Along with these results, a second review of bone marrow histology, flowcytometry and the detection of a calreticulin gene (CALR) mutation helped with the correct diagnosis of PMF. Patient was then treated with ruxolitinib, a JAK (Janus kinase) 1 and 2 inhibitor, and eventually proceeded to receive a matched unrelated reduced intensity conditioning (RIC) allogeneic stem cell transplantation (ASCT) and has been doing well at the 6-month follow up.
Conclusions
Our case highlights two points, that the t(15;17) is diagnostic of Acute Promyelocytic Leukemia (APL) in most cases, there are exceptions and it can be associated with other malignancies without causing any APL like features, as noted in this case. Also, that t(15; 17) by itself is never sufficient to diagnose APL without confirmation by other methods and relying solely on cytogenetics without timely confirmatory tests can lead to risks of delay in diagnosis and appropriate management.
Keywords: primary myelofibrosis, atypical t(15;17), cytogenetics, FISH, case report
Introduction
Myelofibrosis (MF) is a clonal myeloproliferative neoplasm which can manifest with a constellation of findings such as anemia, constitutional symptoms, hepatosplenomegaly or thrombosis. It can present as primary myelofibrosis (PMF) or as secondary MF progressing from polycythemia vera or essential thrombocythemia (post-PV/post ET MF).1,2 According to the revised WHO 2016 update on myeloid neoplasms, presence of JAK2, CALR and MPL mutations, or, in their absence, other frequently seen mutations such as ASXL1, EZH2, TET2, IDH1/IDH2, SRSF2, SF3B1 are one of the essential major criteria to establish clonality.1 Cytogenetic abnormalities (CA) are observed only in about 40–45% of the cases and although not considered essential for diagnosis, they carry prognostic significance.3 While no disease-characteristic cytogenetic abnormalities have been associated with PMF, some are more commonly observed than others.
Many case reports in literature described various sporadic cytogenetic abnormalities associated with PMF. Here, we report one such unique case of a patient who was diagnosed with PMF associated with a t(15; 17) which led to a misdiagnosis and treatment directed toward APL initially and resulted in an adverse event for the patient. The possibility of sporadic occurrence of classic translocations without a disease phenotype means that a diagnosis cannot be entirely relied on one diagnostic aspect, such as the cytogenetics in this case, however characteristic it may be of the disease.
Case discussion
A 69-year-old male patient without a significant past medical history presented to an outpatient clinic with symptoms of worsening left upper quadrant pain, and abdominal distention that have been going on for the previous 3–4 months. On further questioning, he reported worsening fatigue and night sweats for the same duration and a gradual loss of about 6% weight from his baseline over the previous 1 year, associated with poor appetite and intake. He also reported numbness and tingling in bilateral lower extremities.
Physical examination was only remarkable for splenomegaly extending 10 cm below costal margin. Computed Tomography (CT) of the abdomen showed marked splenomegaly, measuring 25.5 cm with non-specific enlarged retroperitoneal lymph nodes.
Peripheral blood complete blood count with differential revealed white blood cell (WBC) count of 3800×109/L with absolute neutrophil count (ANC) 1538 x 109/L, absolute lymphocyte count (ALC) 733×109/L, absolute and total blasts of 47 (1.8%). Hemoglobin was 6.3 gram/dL with a hematocrit of 22, mean corpuscular volume (MCV) 99 and platelets were 43 x 109/L. Lactate dehydrogenase was elevated at 1,547 international units (IU)/L (reference 94–250 IU/L) and erythrocyte sedimentation rate was elevated at 99 mm/hour. Coagulation parameters were normal. Patient was also noted to have a low serum vitamin B12 level at 134 picograms (pg)/mL (reference 200–900 pg/mL) with normal folate level 10.2 nanograms (ng)/mL (reference 3.0–20.0 ng/mL). Peripheral smear showed leucoerythroblastic picture with nucleated red blood cells, anisocytosis and left shifted neutrophils and no promyelocytes were reported.
He was referred to a community oncology clinic and a bone marrow biopsy was performed immediately. The preliminary results reported hypercellularity (100%) with severe, diffuse fibrosis (3+) on Reticulin staining. CD 34+ blasts were estimated at around 3% by Immunohistochemistry (IHC). While awaiting a full report, preliminary cytogenetic analysis was reported after 5 days showing 46 XY, t(15; 17)(q24;q21)[8]/46 XY[12] in 8 out of 20 metaphase cells evaluated.
With the t(15; 17) result, patient was urgently transferred to a tertiary care center with acute promyelocytic leukemia (APL) suspicion. A bone marrow biopsy was repeated along with cytogenetics, flowcytometry, FISH, RT-PCR and myeloid mutation profile and he was started on all-trans retinoic acid (ATRA) therapy. Platelet transfusions were given preemptively upon arrival for thrombocytopenia. After the second dose of ATRA, patient complained of shortness of breath and chest tightness associated with a drop in blood pressure and oxygen saturation. He was managed in the ICU conservatively and he eventually recovered. This episode was attributed to an anaphylactic reaction either to the ATRA or to platelets.
Bone marrow morphology again demonstrated hyper-cellularity (90–100%) with severe fibrosis (MF Grade 3 of 3), atypical megakaryocytes and 4% blasts. Flowcytometry showed 4.9% population of intermediate to large cells with the following immunophenotype: CD7-, CD11B-, heterogeneous CD13+, CD14-, CD15-, CD16-, dim CD33+, CD34+, CD38+, dim CD45+, subset CD56+ (expressed on 7% of the blasts), CD64-, heterogeneous CD71+, heterogeneous CD117+, HLADR+ and the findings suggested clonal myeloid neoplasm. Repeat cytogenetic analysis confirmed 46 XY with t(15; 17), and also showed a 20q- abnormality in 2 cells. FISH testing, however, did not reveal the PML/RARA t(15; 17) translocation in 300 cells that were analyzed. RT-PCR also did not detect PML-RARA fusion transcripts. Further doses of ATRA were held at this time because of the severe anaphylactic reaction and also now that the additional information ruled out an APL. Together, with the FISH and RT-PCR being negative for PML-RARA fusion transcripts and with bone marrow fibrosis showing only a 4% blasts, the final diagnosis was felt to be more consistent with a chronic myeloproliferative neoplasm, and likely MF. Eventually, the NGS myeloid molecular mutation profile from the bone marrow biopsy aspirate revealed a c.1154_1155insTTGTC (5bpins) CALR mutation in 47.6% cells. No other mutations were detected. The patient met the diagnostic criteria for primary myelofibrosis.
According to DIPSS plus score of 4, the patient was classified as high risk. We initiated ruxolitinib 5 mg twice daily for symptomatic splenomegaly and constitutional symptoms and referred him to stem cell transplant consult. At 6-month follow-up, although the constitutional symptoms improved, unfortunately the size of the spleen did not decrease and he continued to require red blood cell transfusions.
Therefore, we referred the patient for laparoscopic splenectomy in preparation for allogeneic stem cell transplantation. Roughly 4 weeks after recovery from the surgery, a RIC fludarabine/melphalan regimen based matched unrelated allogeneic stem cell transplantation was performed.
Day 90 bone marrow biopsy showed marked fibrosis in a hyper-cellular marrow (60%), 2% blasts with normal immunophenotype by flow cytometry, diploid 46 XX karyotype, consistent with normal female donor. CALR mutation was not detected by next-generation sequencing (NGS). Day 90 post-transplant peripheral blood short tandem repeat (PB-STR) analysis showed 100% donor chimerism in CD 33+ and 44% donor in CD 3+ compartments, respectively.
At his most recent 6-month follow-up post-transplant, the patient remained well engrafted and transfusion independent. CBC showed normal WBC count of 6600×109/L, hemoglobin of 14.6 g/dL and a platelet count of 222×109/L and CALR mutation testing remained negative.
Methods
Flowcytometry
Leukocyte immunophenotyping is an immunofluorescence assay used to identify and characterize individual cells in a single-cell preparation. The process for qualitative analysis is lyse and stain.4 The cells are bulk lysed, ie 1 mL of sample to 14 mL of BD recipe Ammonium Chloride Lyse. Then incubated on a Nutator rocker for 10 mins, and spun to collect a button of White cells. The isolated cells are adjusted to an appropriate concentration, incubated with a panel of characterized fluorochrome conjugated antibodies, washed, and then introduced to a properly calibrated Flow Cytometer. The subsequent collection is analyzed for quality assurance, and interpreted and reported by a pathologist. When a diagnosis of pancytopenia, myelodysplastic syndrome or other non-descript diagnosis is shared, a panel which looks for evidence of lymphoma or acute leukemia is stained. This panel is called Scout, and is characterized in Table 1:
Table 1.
Bm screen/scout
| FITC | PE | PERCP-CY5.5 | PE-CY7 | APC | APC R700 | APC-H7 | BV 421 | V500 | BV605 |
|---|---|---|---|---|---|---|---|---|---|
| LAMBDA | KAPPA | CD4 | CD5 | CD10 | – | CD8 | CD3 | CD45 | CD19 |
| CD57 | CD34 | CD13 | CD16 | CD117 | CD64 | CD3 | CD33 | CD45 | CD56 |
Abbreviations: FITC, fluorescin isothiocyanate; PE, phycoerythrin; PERCP, peridinin chlorophyll protein; PE-CY, phycoeryhthrin-cyanine; APC, allophycocyanin; V, violoet; BV, brilliant violet; CD, cluster of differentiation markers.
Cytogenetics
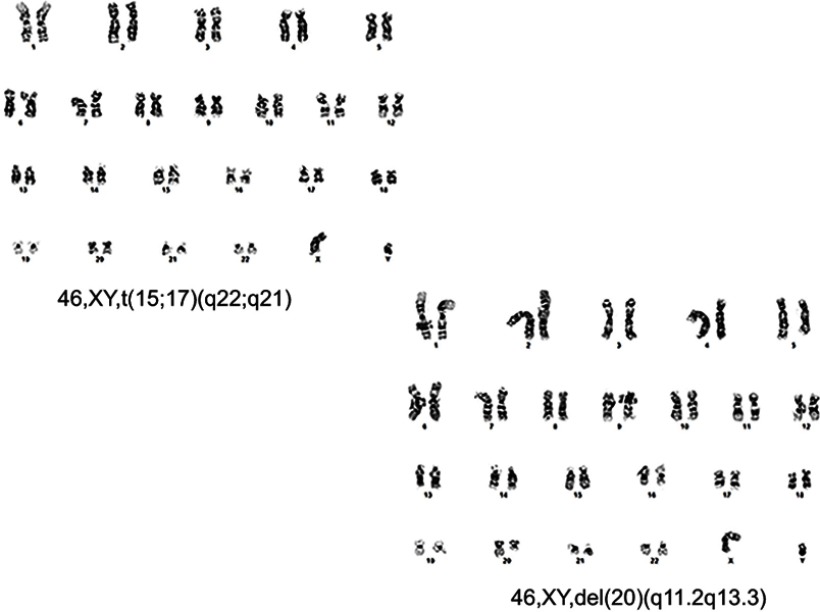
Cells from unstimulated 24 hrs cultures from a bone marrow aspirate were arrested at metaphase with colcemid. Chromosomes were stained by the G-banding method. The chromosome number was determined by microscopic analysis and these cells were examined for the presence or absence of detectable structural rearrangements. Karyotypes were prepared from computer-assisted digital images of these metaphases as shown in Figure 1.
Figure 1.
Cytogenetic analysis showing two separate clonal populations showing translocation between the long arm of chromosome 15 and the long arm of chromosome 17, with breakpoints at 15q22 and 17q21 [46, XY, t(15; 17)(q22;q21)] and an interstitial deletion in the long arm of chromosome 20 with the breakpoints at q11.2 and q13.3 [46, XY, del (20)(q11.2q13.3)], respectively.
Twenty cells were analyzed and three cell lines were detected. Nine (9/20=45%) cells (clone 1) had a modal number of 46 chromosomes, including the X and Y chromosomes. These cells contained a translocation between the long arm of chromosome 15 and the long arm of chromosome 17, with breakpoints at 15q22 and 17q21 [46, XY, t(15; 17)(q22;q21)]. Two (2/20=10%) cells (clone 2) had a modal number of 46 chromosomes, including the X and Y chromosomes. These cells contained an interstitial deletion in the long arm of chromosome 20 with the breakpoints at q11.2 and q13.3 [46, XY, del (20)(q11.2q13.3)]. The remaining nine (9/20=45%) cells (clone 3) appeared to be normal [46, XY].
Fish
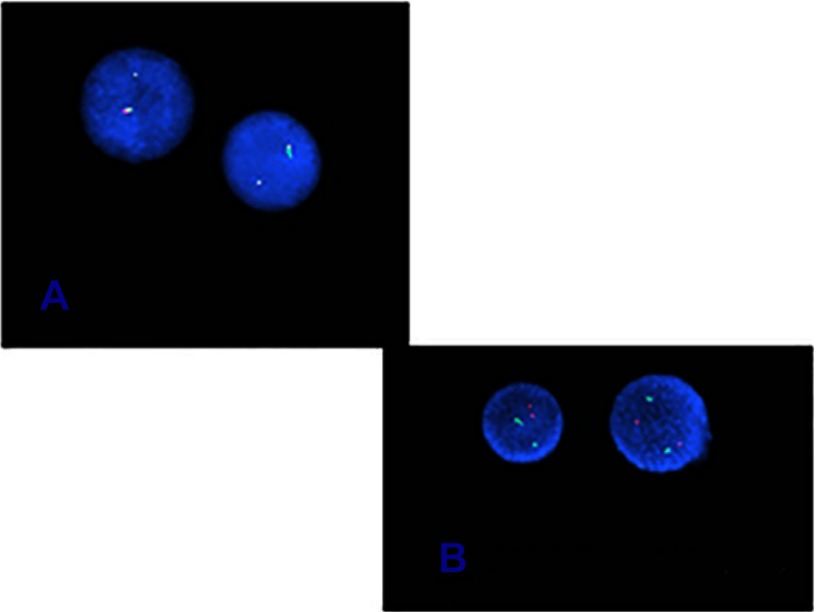
Fluorescence in situ hybridization studies were performed on nuclei using the DNA probes EGR1[5q31], D7S522 [7q31], CEP8 [8cen], MLL [11q23], PML/RARA [15q22/17q21.1], CBFB [16q22], RUNX1/RUNX1T1 [21q22/8q22] and RARA break apart probe [17q21.1]. A total of 300 nuclei were analyzed for each probe set and they exhibited normal signal patterns as shown in Figure 2.
Figure 2.
FISH studies were performed using dual color dual fusion and the RARA BAP probe and the results were normal. (A) RARA breakapart: 3ʹ green and 5 ‘red; (B) PML/RARA: PML (red signal) and RARA (green signal).
Abbreviations: PML, promyelocytic leukemia gene; RARA, retinoic acid receptor alpha gene.
RT-PCR
Patient RNA was isolated, reverse transcribed into complimentary DNA (cDNA) and amplified using primers specific for the PML and RARA genes. RT-PCR was then performed to detect t(15; 17). PML-RARA and ABL (control) transcripts were quantified. Results were reported as a normalized ratio of PML-RARA transcripts to Abelson gene (ABL) transcripts present in the sample.
Next-generation sequencing
The University of Iowa Hospitals and Clinics Acute Myeloid Leukemia Mutation (AML) Profiling assay entails massively parallel DNA sequencing using semi-conductor-based detection of pH.5,6 The sequenced DNA sample is a PCR-amplified fragment library in which each sample is uniquely identified by ligation of short oligonucleotide bar codes. The amplicons span 95,000 bp of the human genome, targeting discrete regions of 30 AML- and myelodysplasia-related genes, based upon previously identified mutations listed catalog of somatic mutations in cancer database (COSMIC: http://cancer.sanger.ac.uk/cancergenome/projects/cosmic/). Each DNA sample is monitored for quality that ensures reliable variant detection as low as 4% variant frequency for single nucleotide variants or polymorphisms (SNV or SNP), and 8% variant frequency for insertions (INS), duplications (DUP) and deletions (DEL) up to 50 nt in length. Variants are identified by an automated process that takes into account statistical confidence of base calling and alignment/mapping quality that ensures an error rate not greater than 0.01 (Torrent Technical Notes). Variants are annotated using the Annovar software tool (http://www.openbioinformatics.org/annovar/), which includes a determination of minor allele frequency (MAF) in the population (a combination of dbSNP, 1,000 genomes and ESP6500 databases) genomic position and, for exonic missense mutations, predicted nonsynonymous amino acid changes. Exonic insertions, deletions and non-synonymous missense mutations (with MAF <0.1), and exon-intron splice site mutations are reported.
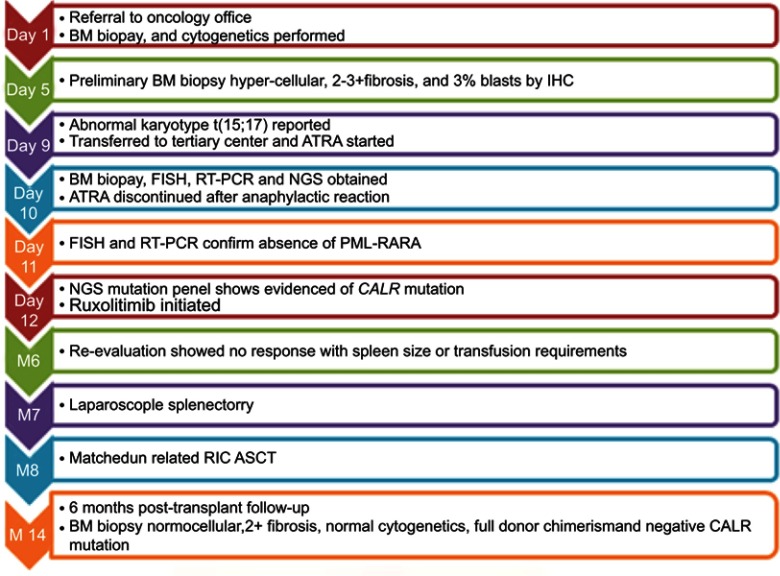
Summary of events
Sequence of events from the time of patient’s initial presentation to 6-month post-transplant follow-up is summarized here in Figure 3.
Figure 3.
Timeline of events from first presentation to 6-month post-transplant follow-up.
Abbreviations: BM, bone marrow; IHC, immunohistochemistry; ATRA, all-trans retinoic acid; FISH, fluorescence in situ hybridization; RT-PCT, reverse-transcriptase polymerase chain reaction; NGS, next-generation sequencing; PML-RARA, promyelocytic leukemia and retinoic acid receptor alpha; CALR, calreticulin gene; RIC, reduced intensity conditioning; ASCT, allogeneic stem cell transplantation.
Discussion
This is a unique case of PMF associated with a t(15; 17) which caused a diagnostic conundrum. Initially, due to a lower percentage of blasts (3%) and absence of promyelocytes in the peripheral blood, and absence of information from flowcytometry and other confirmatory testing, an acute leukemia was not suspected. However, upon the report of the cytogenetics which showed classic t(15; 17) (q22; q21), APL was immediately considered despite the less than 20% bone marrow blasts and absence of increased promyelocytes in the bone marrow or peripheral blood, because of the characteristic cytogenetic abnormality. It should be noted that suspicion of APL should arise with the morphological evidence of hypergranular promyelocytes in the bone marrow or peripheral blood along with other typical clinical features which should prompt an initiation of ATRA and confirmatory testing.7 A final correct diagnosis of primary myelofibrosis was promptly made in our case after obtaining flowcytometry, FISH and PCR for PML-RARA and reviewing the bone marrow morphology at the tertiary center.
It is striking that the t(15; 17) (q22; q21), which is the most common translocation associated with APL, seen in over 98% of the cases with a t(15; 17), was found in our patient with no features of APL.8–11 While t(15; 17) is a hallmark of APL, there have been several reports in literature that described the sporadic association of t(15; 17) with various other solid malignancies or with acute myeloid leukemia without an apparent phenotype of APL,12–15 although none have reported this in association with PMF or other types of chronic myeloproliferative neoplasms. Conversely, it has also been reported that PML-RARA fusion transcripts can be detected by FISH or PCR methodologies even when there is no classic t(15;17) observed on conventional cytogenetic studies.16 Therefore, when clinical picture or bone marrow morphology raises concerns for APL, it is essential to obtain flowcytometry, FISH and PCR with rapid turnaround times at the time of initial diagnostic testing to avoid delays in diagnosis and unwarranted adverse events from inappropriate management.7,10
Furthermore, any consideration or suspicion of APL diagnosis needs prompt initiation of ATRA until the final diagnosis has been confirmed or excluded.7 Remarkable survival rates ranging >90% in APL patients have been reported recently by major clinical trials, whereas the observed survival rates in “real world” or community practices in patients not enrolled in trials as reported by SEER database analyses were in the range of 71% and 65% 1 year and 5 years overall survival (OS), respectively.17 Similarly, population-based studies by Swedish and Brazilian registries and other European studies reported mortality anywhere from 20% to 30% during induction phase.7,18–20 The majority of the deaths occur early during induction and are largely attributed to coagulation abnormalities, infections and differentiation syndrome in part due to delay in diagnosis, initiation of supportive care as well as chemotherapy.21
Cytogenetic abnormalities and their significance in primary myelofibrosis
Although there are no diagnostic cytogenetic abnormalities specific for PMF, unlike APL and CML (chronic myeloid leukemia), there are data suggesting a strong prognostic role of CA in PMF. Wassie et al reported that roughly 43% of the patients with PMF carry abnormal karyotypes of which the more commonly seen are 20q-, 13q- 8+, +9, 1q+ and −7/7q-.22 Many other rare abnormalities have also been reported in the literature. Complex and monosomal karyotypes including +8, −7/7q-, i(17q), inv(3), −5/5q- were found to have unfavorable prognosis and a more frequent association with a higher DIPSS plus score,22 while the 20q-, 13q- and +9 are considered to have favorable survival akin to normal karyotype. Recently, Tefferi et al reclassified the cytogenetic risks into a three-tier system consisting of favorable, unfavorable and very high risk (VHR) groups and they are associated with survival and leukemia-free survival.23 Clonal evolution can impact the natural history of disease and acquisition of new cytogenetic abnormalities may lead to progression of disease and poor outcomes.24 Acquisition of chromosome 17 abnormality has been found to have the most unfavorable prognosis with shortened survival in this study,24 although the number of patients in this study was small. Recent report presented by Nicolosi et al at the ASH 2018 annual meeting showed that clonal evolution with progression was much more common with PMF compared to ET or PV, and it affected survival.25
Our patient had 20q- and t(15; 17) abnormalities along with a type-2 CALR mutation and high-risk disease features at the time of his presentation.
There is limited understanding about the pathogenesis and how the chromosomal abnormalities result in genetic alterations leading to disease processes in PMF. This was studied in more detail about 20q- abnormality with regard to myeloid malignancies including primary myelofibrosis but the information regarding other chromosomal abnormalities and the molecular pathways are not clearly defined.26,27 It is possible that the t(15; 17) in this patient could be just a variant of unknown significance or it could have been a marker of clonal evolution as reported by a prior study which suggested chromosome 17 abnormality as a poor prognostic marker in disease progression,24 but this cannot be definitively established in our patient as we do not have a prior bone marrow and cytogenetics evaluation. Since the FISH testing did not detect any fusion partners, RNA sequencing could have potentially helped determine the novel fusion transcript protein involved with this translocation. Unfortunately, this could not be performed in our patient due to inadequate sample.
Conclusions
In conclusion, this case brings to attention that classic t(15; 17) (q24; q21) aberration that is typical of APL can sporadically associate with other myeloid malignancies such as myelofibrosis, without an apparent APL phenotype. In our patient, the delay in obtaining the FISH and PCR results in turn delayed the diagnosis of PMF. The patient experienced an adverse event likely related to the platelet transfusion or ATRA administration but it should be still emphasized that initiation of ATRA must be considered with any clinical suspicion of APL as any potential risks that may occur with this treatment are still outweighed by the benefits of preventing early deaths from APL. However, relying solely on cytogenetic markers can be misleading as this is often inadequate and therefore all the appropriate investigations as discussed above need to be obtained from the outset and discussion with a pathologist can be helpful in cases such as this.
Ethical approval and consent to participate
The patient agreed and submitted a written informed consent to allow publication of the details of his case. Our institutional review guidelines do not require institutional approval for publication of case reports details.
Author Contributions
All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
Dr Margarida Silverman reports research funding from Incyte Corporation, Gilead Sciences, Inc, Merck, and Sharp & Dohme, outside the submitted work. The authors report no other conflicts of interest in this work.
References
- 1.Arber DA, Orazi A, Hasserjian R, et al. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. 2016;127(20):2391–2405. doi: 10.1182/blood-2016-03-643544 [DOI] [PubMed] [Google Scholar]
- 2.Passamonti F, Mora B, Giorgino T, et al. Driver mutations’ effect in secondary myelofibrosis: an international multicenter study based on 781 patients. Leukemia. 2017;31(4):970–973. doi: 10.1038/leu.2016.351 [DOI] [PubMed] [Google Scholar]
- 3.Tefferi A. Primary myelofibrosis: 2019 update on diagnosis, risk-stratification and management. Am J Hematol. 2018;93(12):1551–1560. doi: 10.1002/ajh.25230 [DOI] [PubMed] [Google Scholar]
- 4.Foucar K, Chen IM, Crago S. Organization and operation of a flow cytometric immunophenotyping laboratory. Semin Diagn Pathol. 1989;6(1):13–36. [PubMed] [Google Scholar]
- 5.Beadling C, Neff TL, Heinrich MC, et al. Combining highly multiplexed PCR with semiconductor-based sequencing for rapid cancer genotyping. J Mol Diagn. 2013;15(2):171–176. doi: 10.1016/j.jmoldx.2012.09.003 [DOI] [PubMed] [Google Scholar]
- 6.Pennisi E. Genomics. Semiconductors inspire new sequencing technologies. Science. 2010;327(5970):1190. doi: 10.1126/science.327.5970.1190 [DOI] [PubMed] [Google Scholar]
- 7.Cicconi L, Lo-Coco F. Current management of newly diagnosed acute promyelocytic leukemia. Ann Oncol. 2016;27(8):1474–1481. doi: 10.1093/annonc/mdw171 [DOI] [PubMed] [Google Scholar]
- 8.Adams J, Nassiri M. Acute promyelocytic leukemia: a review and discussion of variant translocations. Arch Pathol Lab Med. 2015;139(10):1308–1313. doi: 10.5858/arpa.2013-0345-RS [DOI] [PubMed] [Google Scholar]
- 9.de The H, Lavau C, Marchio A, Chomienne C, Degos L, Dejean A. The PML-RAR alpha fusion mRNA generated by the t(15;17) translocation in acute promyelocytic leukemia encodes a functionally altered RAR. Cell. 1991;66(4):675–684. [DOI] [PubMed] [Google Scholar]
- 10.Grimwade D, Biondi A, Mozziconacci MJ, et al. Characterization of acute promyelocytic leukemia cases lacking the classic t(15;17): results of the European working party. Groupe Francais de cytogenetique hematologique, Groupe de Francais d’Hematologie cellulaire, UK cancer cytogenetics group and BIOMED 1 European community-concerted action “Molecular cytogenetic diagnosis in haematological malignancies”. Blood. 2000;96(4):1297–1308. [PubMed] [Google Scholar]
- 11.Kakizuka A, Miller WH Jr., Umesono K, et al. Chromosomal translocation t(15;17) in human acute promyelocytic leukemia fuses RAR alpha with a novel putative transcription factor, PML. Cell. 1991;66(4):663–674. [DOI] [PubMed] [Google Scholar]
- 12.Allford S, Grimwade D, Langabeer S, et al. Identification of the t(15;17) in AML FAB types other than M3: evaluation of the role of molecular screening for the PML/RARalpha rearrangement in newly diagnosed AML. The Medical Research Council (MRC) Adult leukaemia working party. Br J Haematol. 1999;105(1):198–207. [PubMed] [Google Scholar]
- 13.Di Bona E, Montaldi A, Guercini N, et al. A (15;17) translocation not associated with acute promyelocytic leukaemia. Br J Haematol. 1996;95(4):706–709. [DOI] [PubMed] [Google Scholar]
- 14.Saito M, Izumiyama K, Mori A, et al. Biphenotypic acute leukemia with t(15;17) lacking promyelocytic-retinoid acid receptor alpha rearrangement. Hematol Rep. 2013;5(4):e16. doi: 10.4081/hr.2013.e16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Soni A, Djokic M, Hou JZ, Redner RL, Boyiadzis M. Outcomes of acute myeloid leukemia with t(15;17) not associated with acute promyelocytic leukemia. Leuk Lymphoma. 2015;56(11):3236–3239. doi: 10.3109/10428194.2015.1036262 [DOI] [PubMed] [Google Scholar]
- 16.Han JY, Kim KE, Kim KH, Park JI, Kim JS. Identification of PML-RARA rearrangement by RT-PCR and sequencing in an acute promyelocytic leukemia without t(15;17) on G-banding and FISH. Leuk Res. 2007;31(2):239–243. doi: 10.1016/j.leukres.2006.05.011 [DOI] [PubMed] [Google Scholar]
- 17.Park JH, Panageas KS, Schymura MJ, et al. A population-based study in Acute Promyelocytic Leukemia (APL) suggests a higher early death rate and lower overall survival than commonly reported in clinical trials: data from the surveillance, epidemiology, and end results (SEER) program and the New York state cancer registry in the United States between 1992–2007. Blood. 2010;116(21):872–872. [Google Scholar]
- 18.Jacomo RH, Melo RA, Souto FR, et al. Clinical features and outcomes of 134 Brazilians with acute promyelocytic leukemia who received ATRA and anthracyclines. Haematologica. 2007;92(10):1431–1432. doi: 10.3324/haematol.10874 [DOI] [PubMed] [Google Scholar]
- 19.Lehmann S, Deneberg S, Antunovic P, et al. Early death rates remain high in high-risk APL: update from the Swedish acute leukemia registry 1997–2013. Leukemia. 2017;31(6):1457–1459. doi: 10.1038/leu.2017.71 [DOI] [PubMed] [Google Scholar]
- 20.Micol JB, Raffoux E, Boissel N, et al. Management and treatment results in patients with acute promyelocytic leukaemia (APL) not enrolled in clinical trials. Eur J Cancer. 2014;50(6):1159–1168. doi: 10.1016/j.ejca.2013.11.023 [DOI] [PubMed] [Google Scholar]
- 21.Jillella AP, Kota VK. The global problem of early deaths in acute promyelocytic leukemia: a strategy to decrease induction mortality in the most curable leukemia. Blood Rev. 2018;32(2):89–95. doi: 10.1016/j.blre.2017.09.001 [DOI] [PubMed] [Google Scholar]
- 22.Wassie E, Finke C, Gangat N, et al. A compendium of cytogenetic abnormalities in myelofibrosis: molecular and phenotypic correlates in 826 patients. Br J Haematol. 2015;169(1):71–76. doi: 10.1111/bjh.13260 [DOI] [PubMed] [Google Scholar]
- 23.Tefferi A, Nicolosi M, Mudireddy M, et al. Revised cytogenetic risk stratification in primary myelofibrosis: analysis based on 1002 informative patients. Leukemia. 2018;32(5):1189–1199. doi: 10.1038/s41375-018-0018-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tam CS, Abruzzo LV, Lin KI, et al. The role of cytogenetic abnormalities as a prognostic marker in primary myelofibrosis: applicability at the time of diagnosis and later during disease course. Blood. 2009;113(18):4171–4178. doi: 10.1182/blood-2008-09-178541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nicolosi M Cytogenetic clonal evolution in myeloproliferative neoplasms: contexts and prognostic impact among 650 patients with serial bone marrow biopsies. Poster presented at Anerican Society of Hematology Annual Meeting; November 21, 2018; 2018; Sandiego, California. [Google Scholar]
- 26.Asimakopoulos FA, Green AR. Deletions of chromosome 20q and the pathogenesis of myeloproliferative disorders. Br J Haematol. 1996;95(2):219–226. [DOI] [PubMed] [Google Scholar]
- 27.Reilly JT, Snowden JA, Spearing RL, et al. Cytogenetic abnormalities and their prognostic significance in idiopathic myelofibrosis: a study of 106 cases. Br J Haematol. 1997;98(1):96–102. [DOI] [PubMed] [Google Scholar]