Abstract
The goal of this research was to obtain initial estimates of the prevalence of each of four types of motor speech disorders in children with idiopathic Speech Delay (SD) and to use findings to estimate the population-based prevalence of each disorder.
Analyses were completed on audio-recorded conversational speech samples from 415 children recruited for research in idiopathic SD in six USA cities during the past three decades. The speech and motor speech status of each participant was cross-classified using standardized measures in the finalized version of the Speech Disorders Classification System described in the Supplement. Population-based prevalence estimates for the four motor speech disorders were calculated from epidemiological studies of SD conducted in Australia, England, and the USA.
A total of 82.2% of the 415 participants with SD met criteria for No Motor Speech Disorder at assessment, 12% met criteria for Speech Motor Delay, 3.4% met criteria for Childhood Dysarthria, 2.4% met criteria for Childhood Apraxia of Speech, and 0% met criteria for concurrent Childhood Dysarthria and Childhood Apraxia of Speech. The estimated population-based prevalence of each of the first three motor speech disorders at 4 to 8 years of age were Speech Motor Delay: 4 children per 1,000; Childhood Dysarthria: 1 child per 1,000; and Childhood Apraxia of Speech: 1 child per 1,000. The latter finding cross-validates a prior prevalence estimate for Childhood Apraxia of Speech of 1–2 children per 1,000. Findings are interpreted to indicate a substantial prevalence of motor speech disorders in children with idiopathic SD.
Keywords: Apraxia, dysarthria, speech motor delay, speech sound disorders
Speech sound disorders in children
The 1970’s international paradigm shift from Articulation Disorders to Phonological Disorders had far reaching consequences for research and clinical practice. As described in reviews of the many explanatory accounts of what are now termed Speech Sound Disorders (i.e., excluding dysfluency) and the treatment approaches consistent with these accounts, the dominant theoretical frameworks are variants of a neurocognitive perspective that developmental delays in encoding and retrieving linguistic representations are the core deficits underlying speech sound deletions and substitutions (c.f., Baker, Williams, McLeod, & McCauley, 2018; Bernthal, Bankson, & Flipsen, 2017; Bowen, 2015; McLeod & Baker, 2017; Rvachew & Brosseau-Lapré, 2018). Substantial genetic and behavioural support for this perspective has been provided by findings indicating that idiopathic speech sound disorders are associated with disabilities in four other heritable verbal traits: language, reading, writing, and spelling (e.g., Lewis et al., 2011; Truong et al., 2016). As discussed presently, the classification system in this paper uses the term Speech Delay (SD) for one of two classes of speech sound disorders of known or unknown (idiopathic) origin defined by the presence of age-inappropriate speech sound deletions and/or substitutions. The other class of speech sound disorders, termed Speech Errors (SE) in this research is defined by age-inappropriate common or uncommon speech sound distortions (Shriberg, 1993).
Speech delay and motor speech disorders
The predominance of neurocognitive accounts of SD notwithstanding, there is substantial historical and contemporary research on the hypothesis that some children with idiopathic SD also have motor speech deficits that constrain the development of articulate speech. In research cited in a following section, the error profiles of some children recruited for research in SD suggest that they may have one of the four motor speech classifications described in the next two sections.
Childhood dysarthria, childhood apraxia of speech, and concurrent childhood dysarthria and childhood apraxia of speech
Unlike children with only the early and sometimes persistent consonant deletion and/or substitution errors that define SD, Childhood Dysarthria (CD) or Childhood Apraxia of Speech (CAS) are suspected in children who, in addition to such errors, have imprecise and/ or unstable spatiotemporal distortions of vowels and consonants, inappropriate prosody, and deficits in voice. Reviews of the research and clinical literatures in CD and in CAS are beyond the scope of the present focus on the prevalence of idiopathic childhood motor speech disorders. Estimates of the prevalence of idiopathic forms of CD and CAS are not currently available (American Speech-Language-Hearing Association, 2007; Duffy, 2013). Literature reviews and relevant discussions stress the lack of international or national consensus on the assessment and classification measures used to identify CD and CAS required for the development of biomarkers for each motor speech disorder (e.g., Allison, Cordova, Iuzzini-Seigel, & Green, 2017; Allison & Hustad, 2018; Morgan & Liégeois, 2010; Shriberg et al., 2010a).
Lack of consensus on inclusionary and exclusionary criteria for CD and CAS has limited the conduct of epidemiological studies of the prevalence of idiopathic childhood motor speech disorders. Whereas the lack of widely used measures to identify and classify CD in children with idiopathic speech impairment may be associated with under-diagnosis of CD (e.g., Morgan & Liégeois, 2010), prevalence estimates suggesting over-diagnosis of CAS have been widely discussed (e.g., American Speech-Language-Hearing Association, 2007; Davis, Jakielski, & Marquardt, 1998; Forrest, 2003; Royal College of Speech and Language Therapists, 2011). Two early estimates of the population-based prevalence of CAS were that CAS occurs in 1.3 children per 100 (Morley, 1972) and 1 child per 100 (Yoss, 1975). Approximately two decades later, a population-based estimate based on referrals to a university speech clinic in one city was considerably lower at 1–2 children per 1,000 (Shriberg, Aram, & Kwiatkowski, 1997).
Speech motor delay
In addition to CD, CAS, and concurrent CD & CAS, a fourth classification of childhood motor speech disorder has been a topic of speculation, but to date, has not been the focus of epidemiologic research. The hypothesis is that a presently unknown percentage of children with idiopathic speech-language delay have a ‘motor component’ associated with the delay. Such children may be found within groups of children posited to have general delays in motor development aggregated under such terms such as motor immaturity (Bishop, 2002), developmental coordination disorder (American Psychiatric Association, 2013; Duchow et al., in press), and others that posit developmental deficits in sensorimotor domains that underlie the acquisition of articulate speech. More frequently, a subgroup of children with motor disorder is posited for children with idiopathic SD who perform lower than age-sex norms on one or more gross-, fine-, or oral-motor tasks.
A central question for research and practice is whether a nosological classification is needed for children whose assessment findings are consistent with some type of motor component that does not meet standardized criteria for CD or CAS. Some examples of research and reviews of research relevant to the motor speech characteristic of children with idiopathic speech-language impairment include Archibald and Alloway (2008); Bradford, Murdoch, Thompson, and Stokes (1997); Cermak, Ward, and Ward (1986); Cheng, Chen, Tsai, Chen, and Cherng (2009); Flipsen (2003); Gaines and Missiuna (2007); Goffman (1999); Goozée et al. (2007); Hill (2001); Newmeyer et al. (2007); Nip, Green, and Marx (2011); Owen and McKinlay (1997); Powell and Bishop (1992); Rechetnikov and Maitra (2009); Redle et al. (2015); Richtsmeier and Goffman (2015); Vick et al. (2014); Visscher et al. (2010); Visscher, Houwen, Scherder, Moolenaar, and Hartman (2007); Webster et al. (2006); Zelaznik and Goffman (2010); and Zwicker, Missiuna, and Boyd (2009).
The third paper in this research series includes citations to psychometric and substantive reports supporting a standardized measure developed to identify children with a third type of motor speech disorder that does not meet criteria for dysarthria and/or apraxia (Shriberg, Campbell, Mabie, & McGlothlin, 2019). The measure was designed to identify children who are below an arbitrary percentile criterion on an age-sex standardized measure of their speech, prosody, and voice precision and stability. To parallel the classification terms used for such clinical entities in other verbal traits (i.e., Speech Delay, Language Delay, Reading Delay), the term for this classification is Speech Motor Delay (SMD: Shriberg, 2017). The following section describes relevant concepts and terms in a classification system for speech sound disorders that includes SMD as a childhood motor speech disorder. The measure to identify SMD is described in the Method section.
Speech disorders classification system
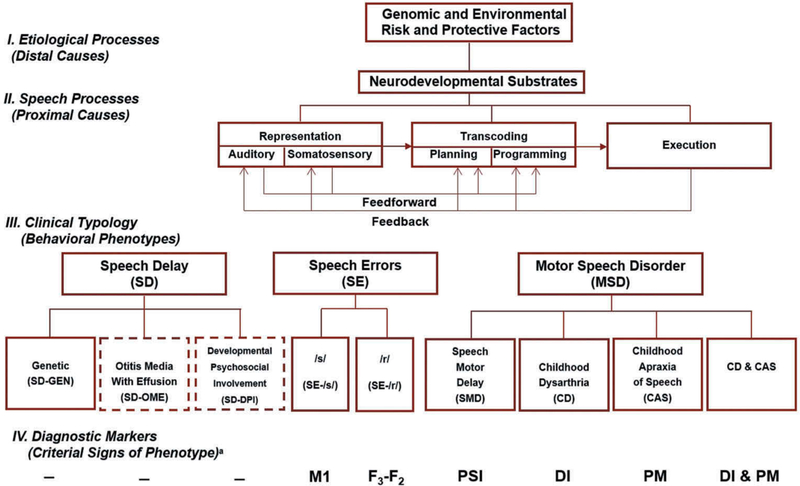
Figure 1 is the finalized version of a research framework for childhood speech sound disorders in development over several decades (Shriberg, 1993, 1994, 2010b, 2017; Shriberg, Austin, Lewis, McSweeny, & Wilson, 1997; Shriberg et al., 2010a, 2017a). Shriberg et al. (2017a) describes the primary features of each of the four levels (I – IV) of the Speech Disorders Classification System (SDCS) shown in Figure 1. The present focus is on Level III, which divides motor speech disorders into four classifications that may co-occur with idiopathic speech disorder or speech disorder in the context of Complex Neurodevelopmental Disorders (CND; e.g., Down syndrome, fragile X syndrome, Galactosemia, Velocardiofacial syndrome).
Figure 1.
The Speech Disorders Classification System (SDCS).
aM1: First Spectral Moment; F3 - F3: Format 3 - Format 2; PSI: Precision-Stability Index; DS/DSI: Dysarthria Index/Dysarthria Subtype Indices; PM: Pause Maker
Some new terms and minor changes in Figure 1 replace terms in prior versions of the SDCS. As indicated by the solid border, the etiological subtype termed Speech Delay-Genetic has been widely supported in genetic studies of idiopathic speech-language and other verbal trait disorders (e.g., Deriziotis & Fisher, 2017; Eising et al., 2018; Guerra & Cacabelos, 2018; Truong et al., 2016). In comparison, two proposed etiological subtypes of SD – SD associated with early recurrent otitis media with effusion (SD-OME) and SD associated with developmental psychosocial involvement – have dashed border lines indicating that they currently are considered risk factors for SD. Although the concurrent validity of each of these latter two proposed etiological subtypes has been supported in small-scale studies reported over several decades, neither has been cross-validated as an etiological subtype of SD in larger scale research using SDCS classification methods and measures (Shriberg, 2010b). Specifically for SD-OME, although large scale studies using differing methods and measures report no significant associations between OME and speech impairment (e.g., Paradise et al., 2005, 2000; Roberts, Burchinal, Koch, Footo, & Henderson, 1988; Roberts, Rosenfeld, & Zeisel, 2004), findings reviewed in Shriberg (2010b) are interpreted as support for the need for continued research on OME as a risk factor for SD. The two subtypes of SE are substantially unchanged from prior versions of the SDCS.
In the Motor Speech Disorder (MSD) arm of the finalized SDCS (Figure 1), the primary change is the classification SMD described previously, which replaces the former provisional term, Motor Speech Disorder-Not Otherwise Specified (MSD-NOS; Shriberg et al., 2010a). Replacing the placeholder term MSD-NOS with SMD was motivated by preliminary prevalence findings for this proposed clinical entity (Shriberg, 2017), cross-validation of the preliminary prevalence findings reported in the present report, and by phenotype and persistence findings for SMD reported in Shriberg, Campbell, et al. (2019). Psychometric and substantive findings for SMD are available for children with SMD in the context of idiopathic SD (Mabie & Shriberg, 2017) and for speakers with SMD in the context of several types of CND (Baylis & Shriberg, 2018; Shriberg & Mabie, 2017; Shriberg, Strand, Jakielski, & Mabie, 2019; Wilson, Abbeduto, Camarata, & Shriberg, 2019).
In addition to shortening the classification terms for the other three motor speech disorder classifications in Figure 1, there are small wording changes from prior versions of the SDCS. Also, Level IV in Figure 1 includes, where available, the measures and diagnostic markers used to identify each speech and motor speech classification. A Supplement for this research series, Motor Speech Disorders in Idiopathic Speech Delay and in Complex Neurodevelopmental Disorders Using the Speech Disorders Classification System, provides detailed information on classification methods and measures [Supplementary Data].
Statement of purpose
Estimates of the prevalence of motor speech disorders in children with idiopathic SD are needed for genetic and other basic and applied research studies in speech sound disorders. The first goal of the present research was to obtain initial estimates of the prevalence of each of the four MSD classifications (Figure 1) in children with idiopathic SD. The second goal was to use these prevalence findings, together with prevalence findings from epidemiological studies of idiopathic SD from three countries, to estimate the population-based point-prevalence of each of the four MSD classifications.
Methods
Participants
Table 1 includes summary assessment, demographic, cognitive-language, and speech information for 415 participants recruited for studies of idiopathic SD in local and collaborative research conducted in six cities in the USA over several decades. The largest number of participants (Group 1) were recruited from Madison, WI and surrounding municipalities. Participants assented and/or consented to participate using procedures and forms approved by institutional review boards at the University of Wisconsin-Madison and at universities and/or hospitals at each of the other five collaborative research sites (Cincinnati, Cleveland, Dallas, Denver, and Pittsburgh).
Table 1.
Assessment, demographic, cognitive-language, and speech information for participants in six groups of children in six USA cities recruited for idiopathic SD. The groups are listed in descending order by the number of participants in each original sample. Cell values and percentages for demographic, cognitive-language, and speech variables are for the 415 of the original 448 (93.5%) participants that were able to be classified using the SDCSS.
| Assessment |
Demographic |
Cognitive-Language |
Speech |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Original Group |
SDCSS Classified |
Age (yrs) |
Sex (%) |
Cognitiona |
Languageb |
PCCc |
IId |
||||||||
| Group | n | n | % | M | SD | % Female | % Male | M | SD | M | SD | M | SD | M | SD |
| Idiopathic SD | |||||||||||||||
| Group 1 | 200 | 188 | 94.0 | 4.4 | 1.1 | 33.5 | 66.5 | 109.4 | 13.3 | 99.1 | 10.5 | 69.5 | 12.0 | 91.3 | 8.1 |
| Group 2 | 84 | 72 | 85.7 | 4.0 | 0.7 | 26.4 | 73.6 | * | * | * | * | 70.0 | 9.6 | 88.5 | 8.9 |
| Group 3 | 71 | 67 | 94.4 | 5.1 | 1.5 | 22.4 | 77.6 | 96.3 | 12.8 | 95.3 | 14.5 | 80.6 | 11.2 | 94.4 | 7.2 |
| Group 4 | 26 | 26 | 100.0 | 7.8 | 1.1 | 30.8 | 69.2 | 104.7 | 12.6 | 95.0 | 20.2 | 89.8 | 7.1 | 97.3 | 2.7 |
| Group 5 | 22 | 21 | 95.5 | 5.5 | 0.6 | 23.8 | 76.2 | * | * | * | * | 82.8 | 6.1 | 91.7 | 12.2 |
| Group 6 | 45 | 41 | 91.1 | 6.2 | 2.6 | 19.5 | 80.5 | * | * | * | * | 77.5 | 11.4 | 86.8 | 11.0 |
| Total | 448 | 415 | 93.5 | 5.5 | 1.3 | 26.1 | 73.9 | 103.5 | 12.9 | 96.5 | 15.1 | 78.4 | 9.6 | 91.7 | 8.4 |
Notes: SD = Speech Delay; SDCSS = Speech Disorders Classification System Summary; PCC = Percentage of Consonants Correct; II = Intelligibility Index, * = no data.
Standard scores for IQ Composite: Kaufman Brief Intelligence Test – Second Edition; Kaufman and Kaufman (2004). IQ Scores: Stanford-Binet-4th Edition; Thorndike, Hagen, and Sattler (1986).
Standard scores for Oral Composite: Oral and Written Language Scales (OWLS); Carrow-Woolfolk (1995). Standard scores for Core Language: Clinical Evaluation of Language Fundamentals-4 (CELF–4); Semel, Wiig, and Secord (2003).
Participants in the six cities were assessed using preliminary or final versions of the Madison Speech Assessment Protocol (Shriberg et al., 2010a), each version of which included a 5–8 minute conversational speech sample. As shown in the first four columns in Table 1, only findings for the 415 participants who met SDCS criteria for classification of their motor speech status (to be described) were included in the present study. The group-wise percentages of classifiable participants in the six SD groups ranged from 85.7% to 100% (M = 93.5%; SD = 4.8). As shown in Table 1, 6.5% of the original group-averaged SD participants could not be classified (i.e., 93.5% – 100% were classifiable). The most frequent reason a participant’s motor speech status could not be classified was because the conversational speech sample did not include the minimum of 40 pause opportunities needed to compute a score on the Pause Marker (PM; see Supplement), the measure described presently used to identify CAS. In practice, such children typically are resampled on the same or another day to obtain a sufficient number of pause opportunities, but such information was not available in the present retrospective database samples. The other reason samples could not be classified was that a participant’s PM status could not be resolved using scores from their responses on a nonword repetition task (cf., Mabie & Shriberg, 2017) because the task had not yet become available for research.
The demographic characteristics of the classifiable participants in Table 1 are consistent with the literature in SD. Most participants were preschool age or in early primary grades (M = 5.5 years of age; SD = 1.3). Male:female ratios averaged 2.8:1, which is generally consistent with findings from prevalence studies of SD internationally (cf., Wren, Miller, Peters, Emond, & Roulstone, 2016, Tables 1 and 2). Standardized scores available from three of the six groups were within the typical range for cognitive (M = 103.5; SD = 12.9) and language (M = 96.5; SD = 15.1) measures. The means and standard deviations of the six groups of participants with SD were also consistent with the ranges of scores on the Percentage of Consonants Correct and the Intelligibility Index reported in a prior technical report on children with SD (McSweeny et al., 2012).
Table 2.
The five speech classifications and five motor speech classifications in the SDCS are each mutually exclusive. The five dysarthria subtype classifications are not mutually exclusive. That is, a speaker can meet percentile criteria for more than one of the five listed dysarthria subtype classifications (i.e., mixed dysarthria). See Supplement for the procedures and measures used to classify each motor speech disorder.
| SDCS Classifications and Dysarthria Subtypes | Abbreviation | Age (yrs;mos) at Assessment | Description | Referencesa |
|---|---|---|---|---|
| Five Speech Classifications | ||||
| Normal(ized) Speech Acquisition | NSA | 3–80 | Does not meet criteria for any of the four Speech Disorder classifications | 2, 3, 4 |
| Speech Errors | SE | 6–8;11 | Age-inappropriate speech sound distortions | 3, 4 |
| Persistent Speech Errors | PSE | 9–80 | Age-inappropriate speech sound distortions that persist past 9 years of age | 4, 5 |
| Speech Delay | SD | 3–8;11 | Age-inappropriate speech sound deletions and/or substitutions | 3, 4 |
| Persistent Speech Delay | PSD | 9–80 | Age-inappropriate speech sound deletions and/or substitutions that persist past 9 years of age | 3, 4, 5 |
| Five Motor Speech Classifications | ||||
| No Motor Speech Disorder | No MSD | 3–80 | Does not meet criteria for any of the four Motor Speech Disorders classifications | 2, 6, 8 |
| Speech Motor Delay | SMD | 3–80 | Meets PSI criterion for SMD | 2, 6, 8 |
| Childhood Dysarthria | CD | 3–80 | Meets DI and DSI criteria for CD | 2, 6, 8 |
| Childhood Apraxia of Speech | CAS | 3–80 | Meets PM criterion for CAS | 6, 7, 8 |
| Childhood Dysarthria & Childhood Apraxia of Speech | CD & CAS | 3–80 | Meets SDCS criteria for CD & CAS | 2, 6, 8 |
| Five Dysarthria Subtypes | ||||
| Ataxic | 3–80 | Cerebellar disorder | 1, 2 | |
| Spastic | 3–80 | Upper motor neuron disorder | 1, 2 | |
| Hyperkinetic | 3–80 | Basal ganglia disorder; increased movement | 1, 2 | |
| Hypokinetic | 3–80 | Basal ganglia disorder; decreased movement | 1, 2 | |
| Flaccid | 3–80 | Lower motor neuron disorder | 1, 2 |
Notes: SDCS = Speech Disorders Classification System; PSI = Precision-Stability Index; DI = Dysarthria Index; DSI = Dysarthria Subtype Index; PM = Pause Marker.
Procedures
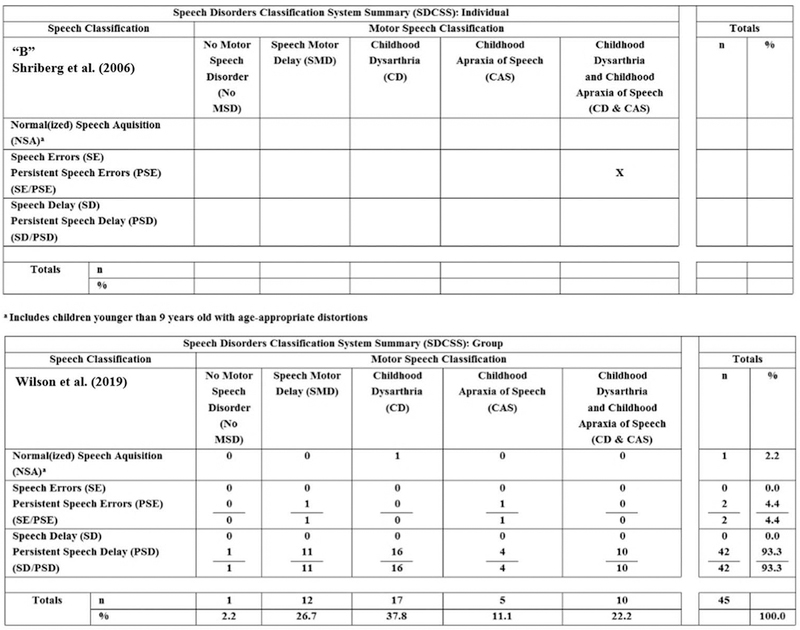
Cross-classification of the speech and motor speech status of all participants was completed using an analytic termed the Speech Disorders Classification System Summary (SDCSS). Figure 2 includes sample SDCSS outputs from the SDCS software (Programs to Examine Phonetic and Phonologic Evaluation Records, 2019). The SDCSS cross-classifies an individual speaker’s (upper panel) or a group of speakers’ (lower panel) speech and motor speech status using perceptual and acoustic findings obtained from a conversational speech sample. SDCSS data provide the primary prevalence information for the present report. It is efficient first to describe the elements of the SDCSS, followed by descriptions of the measures used to identify each of the speech and motor speech classifications in Figure 2.
Figure 2.
Sample output from the Speech Disorders Classification System Summary (SDCSS). The upper SDCSS includes cross-classification findings for a family member with a disruption in FOXP2 (Shriberg et al., 2006). The lower SDCSS includes speech and motor speech cross-classification findings for 45 speakers with Down syndrome (Wilson et al., 2019).
a Includes children younger than 9 years old with age appropriate distortions
Speech classifications
The rows in the SDCSS (Figure 2) include five speech classifications arranged vertically in order of increasing severity of involvement. Normal (or Normalized) Speech Acquisition (NSA) is assigned to speakers who do not have in a conversational speech sample obtained at assessment, speech sound deletions, substitutions, or distortions (including additions) that are inappropriate for their age or sex. SE, or Persistent Speech Errors (PSE) if the speaker is older than 9 years of age, are the classifications assigned to speakers with age-sex inappropriate speech sound distortions. SD, or Persistent Speech Delay (PSD) if the speaker is older than 9 years of age, are classifications assigned to speakers with age-sex inappropriate speech sound deletions and/or substitutions. A slash convention is used to aggregate speakers younger and older than 9 years of age with the same speech disorder (i.e., SE/PSE and SD/PSD). As shown on the speech axis in the lower panel of Figure 2, 93.3% of the speakers in this study met criteria for PSD.
Motor speech classifications
The columns in the sample SDCSS in Figure 2 include five motor speech classifications arranged horizontally left to right putatively in order of increasing severity of involvement: No Motor Speech Disorder (No MSD), Speech Motor Delay (SMD), Childhood Dysarthria (CD), Childhood Apraxia of Speech (CAS), and concurrent CD & CAS. A comment on the concurrent CD & CAS classification is warranted. Speakers with deficits in both neuromotor planning/programming (CAS) and neuromotor execution (CD) are increasingly reported in speech disorder literatures, with implications for genetic and behavioural correlates (e.g., Carrigg, Parry, Baker, Shriberg, & Ballard, 2016; Eising et al., 2018; Peter, Matsushita, & Raskind, 2012; Rice et al., 2012; Turner et al., 2013). Table 2 and a Supplement [Supplementary Data] in this research series include descriptions of the methods and measures in the software that accomplishes the speech and motor speech classifications.
Notice that the “X” in the upper panel of Figure 2 cross-classifies a speaker’s speech and motor speech status – in the present example, a 50-year-old woman identified as “B” in a genetic case study. As shown, this participant is cross-classified as having PSE on the speech axis and persistent CD & CAS on the motor speech axis. In the lower panel of Figure 2, the example percentages in the cells and marginal totals are group-wise findings from 45 speakers with Down syndrome. As shown in Figure 2, 93.3% of these speakers met criteria for PSD on the speech axis, and their most prevalent types of motor speech disorder were CD (37.8%) and SMD (26.7%).
Classification conventions
The SDCSS is a behavioural phenotype matrix in which the five classifications within speech disorders and the five classifications within motor speech disorders are each mutually exclusive. Therefore, as shown in the example of grouped SDCSS data in Figure 2, the marginal values for each axis total 100%. This is accomplished using two conventions.
First, in addition to identifying speakers with no speech errors, the NSA classification identifies speakers with age-appropriate distortions, deletions, and substitutions (speakers with such behaviours in conversational speech are coded NSA-in the SDCS software). Thus, the NSA classification includes speakers with no speech errors, and is also the default classification for participants with speech errors that do not meet criteria for SE or PSE, or for SD or PSD.
Second, the SDCS software classifies speakers who meet criteria for both SE/PSE and SD/PSD as having the more severe disorder, SD/PSD. Similarly, for a speaker who meets criteria for both SMD and any of the other three motor speech disorders classifications (CD, CAS, or CD & CAS), the program classifies the speaker as having the other, more severe motor speech disorder classification (i.e., CD, CAS, or CD & CAS).
Methods and measures
Table 2 includes descriptions of the five speech and motor speech classifications in the SDCSS, and for participants meeting classification criteria for CD, the five dysarthria subtypes. The perceptual and acoustic signs of dysarthria and dysarthria subtypes in measures listed in the footnotes for Table 2 were based on operationalized adaptations of Duffy’s (2013) diagnostic signs of neurogenic motor speech disorders. As indicated previously, SDCS classifications are completed by software that provides standardized speech, prosody, and voice data (z-scores) using two reference databases of typical speakers 3 to 80 years of age (Potter et al., 2012; Scheer-Cohen et al., 2013).
The Supplement for the six papers in this research series includes a graphic illustrating classification procedures and rules for classification, description of the three measures used for motor speech classification, and copies of two of the three measures, including item-level calculation information. Supplement table S1 is the Precision-Stability Index (PSI), which is used to identify and quantify SMD and table S3 is the Dysarthria Index (DI) and Dysarthria Subtype Indices (DSI), used to identify CD, five subtypes of CD, and CD & CAS. Supplement tables S2 and S4 include the calculations completed by the Programs to Examine Phonetic and Phonologic Evaluation Records (2019) software for each of the 32 PSI signs and the 34 DI signs, respectively. The Supplement also includes a brief description of the PM and Pause Marker Index (PMI), used respectively to identify and to quantify the severity of CAS occurring by itself or concurrent with CD (Shriberg et al., 2017b; Tilkens et al., 2017). As described in the Supplement, a nonword repetition task (Syllable Repetition Task [SRT]; Shriberg et al., 2009) was used to resolve indeterminate PM findings. The SRT was included in the assessment protocols of those participants who were assessed when this task became available.
Data reduction and reliability estimates
Data reduction
Four research specialists completed transcription, prosody-voice coding, and acoustic analyses of the conversational speech samples and transcription of the nonword repetition task. Data reduction procedures are described in Shriberg et al. (2010b) and Shriberg, Potter, and Strand (2011). Perceptual and acoustic analyses were accomplished using utility programs and statistical routines in Programs to Examine Phonetic and Phonologic Evaluation Records (2019).
Reliability estimates
To estimate the interjudge and intrajudge point-to-point agreement percentages for the three types of data reduction (transcription, prosody-voice coding, and acoustic analyses), 60 conversational samples from the 415 participants (14.5%) were randomly selected in approximate proportion to the prevalence of each of the five motor speech classifications obtained and described in Results and Discussion. The 60 files included 30 randomly selected from the 341 participants with No MSD, 20 from the 50 participants with SMD, and 10 from the 24 participants with CD and/or CAS.
The right-most column in Table 3 includes the percentage of agreement findings for the point-to-point estimates of the interjudge and intrajudge reliability of the phonetic transcription, prosody-voice coding, and acoustic analyses. The percentage of agreement findings ranged from 74.9% (narrow transcription of vowels) to 97.3% (F0 for vowels), with a mean and standard deviation of 87.9% and 5.9%, respectively across the 26 estimates. The range of agreement percentages are consistent with those reported using the diverse data reduction methods described in the speech sound disorders literatures.
Table 3.
Reliability estimates for interjudge and intrajudge agreement for phonetic transcription, prosody- voice coding, and acoustic analyses.
| Data | Agreement Types |
||||
|---|---|---|---|---|---|
| Interjudge | Intrajudge | No. of Tokens Analyzed | Variable | Percentage of Agreement | |
| Phonetic Transcription | X | Consonants | |||
| 5562 utterances; | Broad | 89.5 | |||
| 12,813 words | Narrow | 76.2 | |||
| Vowels | |||||
| Broad | 85.9 | ||||
| Narrow | 74.9 | ||||
| X | Consonants | ||||
| 5562 utterances; | Broad | 94.5 | |||
| 12,907 words | Narrow | 85.7 | |||
| Vowels | |||||
| Broad | 89.9 | ||||
| Narrow | 81.9 | ||||
| Prosody-Voice Coding | X | 1413 utterances | Appropriate-Inappropriate | 90.7 | |
| X | Appropriate-Inappropriate | 93.9 | |||
| Acoustic Analyses | X | Phoneme Duration | |||
| 1093 Consonants | Consonants | 82.6 | |||
| 4497 Vowels | Vowels | 85.6 | |||
| X | Phoneme Duration | ||||
| 1095 Consonants | Consonants | 88.9 | |||
| 4484 Vowels | Vowels | 88.8 | |||
| X | Vowel Frequency | ||||
| 4213 Vowels | F0 | 97.3 | |||
| 770 Vowels | F1 | 89.3 | |||
| 744 Vowels | F2 | 92.4 | |||
| X | Vowel Frequency | ||||
| 4225 Vowels | F0 | 97.1 | |||
| 1011 Vowels | F1 | 91.3 | |||
| 977 Vowels | F2 | 94.7 | |||
| X | Pause Variables | ||||
| 689 Pauses | Pause–Non-Pause | 81.1 | |||
| 559 Pauses | Appropriate–Not Appropriate | 84.9 | |||
| 19 Pauses | Type 1 –Type 2 | 89.5 | |||
| X | Pause Variables | ||||
| 684 Pauses | Pause–Non-Pause | 80.7 | |||
| 556 Pauses | Appropriate–Not Appropriate | 85.4 | |||
| 13 Pauses | Type 1–Type 2 | 92.3 | |||
Results and discussion
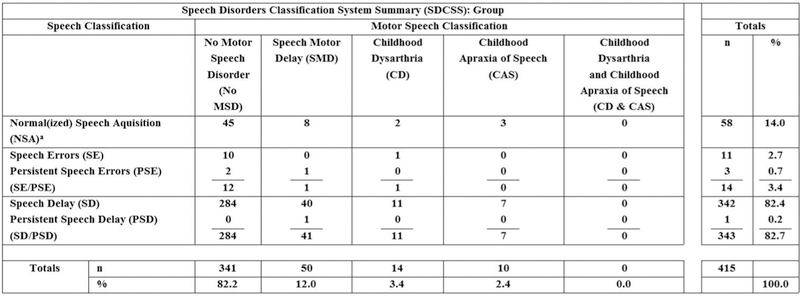
It is efficient to provide combined results and discussion sections for each of the five speech classifications and each of the five motor speech classifications. Figure 3 includes SDCSS findings for the 415 participants described in Table 1.
Figure 3.
Speech and motor speech classification prevalence estimates from six samples of children (n = 415) recruited for idiopathic speech delay.
a Includes children younger than 9 years old with age appropriate distortions
Normal(ized) speech acquisition
Prevalence findings
Of the 415 participants recruited for SD, 58 (14%) met SDCS criteria for NSA at assessment. As described previously, NSA includes speakers who have age-sex typical speech production or who do not have the type and/or frequency of distortion, deletion, or substitution errors required to meet the criteria for SE/PSE or for SD/PSD (i.e., classified as NSA-in the SDCS software). Of the 58 participants classified as NSA, 49 (84.5%) were classified as NSA-.
Discussion
A number of factors could have contributed to the 14% of children that were referred for SD, but met SDCS criteria for NSA or NSA-at assessment. The most likely sources are differences between the SDCS criteria for SD (i.e., age-sex inappropriate speech sound deletions and substitutions in conversational speech using narrow phonetic transcription), and alternative definitional criteria for SD used by recruitment sources (e.g., children referred to the study who may have met percentile criteria for SD on a citation-form articulation test scored using broad phonetic transcription; children who may have met severity criteria for SD based on findings from an intelligibility rating scale). Another possible source of NSA or NSA-was normalization of SD with or without treatment in the time period between recruitment for the research project and completion of the assessment protocol.
Speech errors/persistent speech errors
Prevalence findings
As shown in the combined SE/PSE data in Figure 3, 14 participants (3.4%) in the six groups recruited for SD met criteria for SE or PSE (the latter if older than 9 years). As described previously, speakers who met criteria for both SE/PSE and SD/PSD were classified as having the presumably more severe disorder, either SD or PSD. Analyses indicated that the 14 children who met criteria for only SE/PSE comprised 48.3% or approximately half of the original 29 children with SE/PSE. That is, an additional 15 children with SE/PSE (51.7%) also met classification criteria for and were classified as SD/PSD.
Discussion
There presently is no professional consensus on the phonetic, phonological, and speech-processing distinctions between SE and SD proposed in the SDCS (Figure 1). As with the NSA findings, one explanation for the 3.4% of participants with SE/PSE in the six study samples of children recruited for SD/PSD is that these participants’ prior SD/PSD resolved by the time they were assessed for the research. Alternatively, and more likely, this finding attests to the lack of standardized classification of speech sound disorders, as discussed in virtually all textbook chapters and reviews of speech sound disorders. A continuing problem for genetic research is that without reliable historical speech data on probands and older immediate and extended family members with PSE at research assessment, anecdotal information is generally the only source available to attempt to retrieve prior SD versus persistent SE classification status (Flipsen, 2015; Shriberg, 2010b, Figure 1–6).
Speech delay
Prevalence findings
In addition to participants classified as either NSA or SE/PSE at assessment, the remaining 343 of the 415 (82.7%) participants recruited for studies of SD met SDCS criteria for SD or PSD. As shown in Figure 3, only one of these participants met age criteria in the present study for PSD. Thus, with one exception, the 343 participants who met SDCS criteria for SD in the present study were younger than 9 years of age at assessment.
Discussion
As considered previously, a methodological question was whether to base the following estimates of the prevalence of motor speech disorders in SD on the entire group of 415 participants, or to restrict the analyses to just the subset of 343 children who met SDCS criteria for SD/PSD at assessment. For the following three reasons, the decision was to calculate estimates both ways to determine if findings supported basing prevalence estimates on the entire group of classifiable participants who were referred by speech pathologists for a study of children with SD. First, the inclusion of all children who met criteria for SD by certified speech clinicians in six different catchment areas lends face validity to the nosological construct of SD as defined by certified speech clinicians. That is, in the absence of a national or international classification standard for SD, as for example there is for methods and criteria to identify and quantify hearing loss, SD is currently defined by standards developed in local special education communities. Second, as indicated previously, due to scheduling contingencies, participants referred for research may have normalized SD/PSD to SE/PSE or to NSA by the date they were able to be scheduled for research assessment. Third, we note in Figure 3 that a number of participants classified as NSA or SE/PSE at assessment met criteria for one of the four motor speech disorders (n = 15). That is, they were cross-classified on the SDCSS as NSA or SE/PSE, and met classification criteria for one of the four motor speech disorders. For these reasons, the following analyses report prevalence findings for motor speech disorders computed for both the entire group of participants referred for a research study in idiopathic SD, and for only the subset who met SDCS criteria for SD/PSD at assessment.
No motor speech disorder
Prevalence findings
The first data column in Figure 3 includes prevalence findings for participants who met SDCS criteria for No MSD. 341 (82.2%) of the 415 participants recruited for SD met criteria for No MSD, including 45 of the 58 (77.6%) participants with speech classifications of NSA, 12 of the 14 (85.7%) participants with speech classifications of SE, and 284 of the 343 (82.7%) participants who met SDCS criteria for SD at assessment. By subtraction, these findings estimate the prevalence of any of the four motor speech disorders in children recruited for SD at 17.8% (i.e., 100% – 82.2% of participants with No MSD). A nearly similar estimate of the prevalence of motor speech disorder in SD is obtained using only the subset of participants who met SDCS criteria for SD at assessment (i.e., deleting participants classified as NSA or SE). As shown in Figure 3, of the 343 participants who met SDCS criteria for SD at assessment, 284 (82.7%) had No MSD. By subtraction, 17.3% of participants with SD (100% – 82.7% with No MSD) met SDCS criteria for one of the four motor speech disorders, with the latter estimate within 0.5% of the 17.8% previous estimate. Consistent with the SD literature, 238 of the 341 (69.8%) participants with No MSD were male, compared to 103 of the 341 (32.2%) who were female; the percentage difference was significant (Fisher’s exact test p = 0.000).
Discussion
The finding that 17.8% of children with idiopathic SD at the ages assessed also met criteria for one of the four types of motor speech disorder may seem unexpectedly high, given the conventional description of idiopathic speech delay as a cognitive-linguistic childhood disorder. It is important to underscore that for the reason reviewed previously, SMD is included as a subtype of childhood motor speech disorder. As described next, SMD comprised two-thirds of the 17.8% of participants with SD with one of the four types of concurrent motor speech disorders.
Speech motor delay
Prevalence findings
SMD was originally developed to provide a classification for speakers suspected to have motor speech deficits, but who do not meet SDCS quantitative requirements for CD and/ or CAS. Speakers who meet criteria for SMD and any of the motor speech classifications (CD, CAS, CD & CAS) are classified as having the other, putatively more severe motor speech classification. In the present sample of 415 children recruited for SD, 50 (12%) participants (Figure 3) met criteria for SMD and did not meet criteria for CD, CAS, or CD & CAS. Figure 3 also contains the information needed to estimate the prevalence of SMD in the subgroup of participants who met SDCS criteria for SD/PSD. As found for the Speech Disorder classifications, the two estimates are nearly identical. Compared to the 12% prevalence of SMD in the entire sample of 415 participants, 41 of 343 participants who met the SDCS criteria for SD also met criteria for SMD, yielding a prevalence estimate of 11.95% for SMD concurrent with SD.
A test of differences between two proportions was calculated to determine if there was a significant difference in the sex of participants classified as SMD compared to the percentage meeting SDCS criteria for No MSD. 40 of the 50 (80%) participants meeting criteria for SMD were male, compared to 238 of the 341 (69.8%) participants with No MSD. The difference was non-significant (Fisher’s exact test p = 0.181).
Discussion
The present estimate of the prevalence of SMD, 12%, is higher than a preliminary estimate of 8.3% SMD in participants with idiopathic SD using the same measures and methods (Shriberg, Strand, & Mabie, 2016). It is more consistent with findings in Vick et al. (2014) that 10.3% of children recruited for SD ‘exhibited significantly higher variability in measures of articulatory kinematics and poor ability to imitate iambic lexical stress, suggesting atypical speech motor control’ (p. 2033). Based on the confidence interval obtained, Vick and colleagues estimated the population-based prevalence of this possible subtype of SD (titled ‘Group B’ in Vick et al., 2014) at 4.3% – 16.5%. This prevalence range is generally consistent with the range of prevalence percentages across the 6 samples of participants with SD (Table 1) discussed in Shriberg, Campbell, et al. (2019).
Childhood dysarthria
Prevalence findings
The prevalence estimate for CD calculated using all 415 participants was 3.4% (Figure 3). The estimate for CD using only the 343 participants who met SDCS criteria for SD/PSD at assessment was 3.2%. A total of 11 of the 14 (78.6%) participants who met criteria for CD were male, compared to the percentage of participants with No MSD who were male (238/341; 69.8%). The difference in percentages was non-significant (Fisher’s exact test p = 0.567).
Dysarthria subtype trends
Prevalence estimates for the five dysarthria subtypes are preliminary due to the few (n = 14) participants meeting criteria for CD on the Dysarthria Index/Dysarthria Subtype Index. As indicated in the Supplement, the five dysarthria subtypes are each comprised of 12–19 of the 34 signs in the Dysarthria Index (DI). Following Duffy (2013), each sign in an index is weighted by 1 or 2 points, depending on its proposed diagnostic sensitivity to each dysarthria subtype. As described in the Supplement, subtype signs are not mutually exclusive, with some signs in Duffy (2013) proposed to be diagnostic of 2 of the 5 subtypes of dysarthria.
Table 4 is a summary of the dysarthria subtype findings for each of the 14 participants who met the three criteria for CD on the DI (see Supplement). The entries in the column for each dysarthria subtype is the percentile score for each participant, based on a reference database of 442 speakers with a CND and at risk for a motor speech disorder (Mabie & Shriberg, 2017; pp. 203–204). Percentile scores that are equal to or less than the 10th percentile (bolded) are considered positive for that dysarthria subtype. Two findings in Table 4 warrant comment.
Table 4.
Summary of dysarthria subtype findings for the 14 participants who met Speech Disorders Classification System criteria for childhood dysarthria.
| Dysarthria Subtypesa | ||||||
|---|---|---|---|---|---|---|
| Participants | Ataxic | Spastic | Hyperkinetic | Hypokinetic | Flaccid | No. of Subtypes ≤10th %ile |
| 1 | 35 | 30 | 21 | 10 | 20 | 1 |
| 2 | 35 | 15 | 26 | 6 | 43 | 1 |
| 3 | 45 | 30 | 21 | 4 | 5 | 2 |
| 4 | 26 | 4 | 3 | 49 | 35 | 2 |
| 5 | 2 | 30 | 8 | 18 | 60 | 2 |
| 6 | 56 | 51 | 69 | 7 | 2 | 2 |
| 7 | 35 | 72 | 37 | 18 | 2 | 1 |
| 8 | 10 | 17 | 21 | 30 | 20 | 1 |
| 9 | 26 | 25 | 30 | 30 | 10 | 1 |
| 10 | 45 | 60 | 13 | 7 | 1 | 2 |
| 11 | 45 | 72 | 46 | 7 | 5 | 2 |
| 12 | 45 | 30 | 37 | 4 | 5 | 2 |
| 13 | 45 | 51 | 46 | 2 | 2 | 2 |
| 14 | 56 | 17 | 13 | 4 | 20 | 1 |
| n ≤ 10th %ile | 2 | 1 | 2 | 9 | 8 | |
| Percentage ≤10th %ile | 14.3 | 7.1 | 14.3 | 64.3 | 57.1 | |
Dysarthria Subtype Indices Percentile Scores ≤10th percentile are bolded.
First, as shown in the bottom row in Table 4, 64.3% and 57.1% of the 14 participants, respectively, had scores ≤the 10th percentile for Hypokinetic and Flaccid dysarthria. In comparison to the 9 and 8 participants of the total 14 with CD, respectively, who met the percentile criterion for these subtypes, only 1 or 2 participants met the percentile criterion for any of the other three dysarthria subtypes. Also, as shown in the right most column, 8 of the 14 participants met the percentile criterion for 2 subtypes, with 6 of the 8 meeting the percentile criterion for both Hypokinetic and Flaccid dysarthria. Thus, for the present small initial sample, Hypokinetic and Flaccid dysarthria as identified using the present methods would appear to be the strongest candidates for the most frequent subtypes of CD in children recruited for idiopathic SD.
Second, it is interesting to compare the present prevalence estimates for subtypes of dysarthria to estimates reported for 46 children who met SDCS criteria for CD in 7 of the 8 groups of children with CND described in Shriberg, Strand, et al. (2019). The five entries in the bottom row of Table 4 are the percentages of 14 children recruited for idiopathic SD positive for each dysarthria subtype: Ataxic: 14.3%, Spastic: 7.1%, Hyperkinetic: 14.3%, Hypokinetic: 64.3%, and Flaccid: 57.1%. In comparison, the percentages meeting the ≤10th percentile for the subtypes for 46 children with CD in the context of one of 7 CND were Ataxic: 47.8%, Spastic: 30.4%, Hyperkinetic: 34.8%, Hypokinetic: 41.3%, and Flaccid: 41.3%. The latter notably compact distribution of prevalence percentages among the five subtypes, ranging from 30.4%−47.8% is likely due to averaging of subtypes across the 7 different CND. Alternatively, the small range could reflect collinearity among subtype scores in the larger sample, due to signs used in two or more subtypes (e.g., slow rate; Shriberg, Strand, et al., 2019). Again, the present subtype findings for Hypokinetic and Flaccid CD based on only 14 participants are considered preliminary. Considerably larger databases of children with idiopathic SD are needed to yield sufficient numbers of children with CD based on the present initial prevalence estimate of 3.4% CD concurrent with idiopathic SD.
Childhood apraxia of speech
Prevalence findings
The prevalence estimate for CAS in children recruited for idiopathic SD was 2.4% when calculated using all 415 children recruited for SD (Figure 3) and 2.0% using only the 343 participants who met criteria for SD/PSD at assessment.
Discussion
If the difference in the two prevalence estimates is cross-validated in larger samples it could suggest that some true positives for CAS could be missed (i.e., 2.0% compared to 2.4%) if their consonant deletions and/or substitutions in continuous speech samples had normalized earlier than other signs associated with true positive CAS (i.e., they no longer met criteria for SD). Examples of speakers with CAS who later meet criteria for NSA, but have some residual signs of CAS, have been reported (e.g., Jakielski, 2008a, 2008b).
Findings for the Pause Marker Index (PMI; Shriberg et al., 2017d) indicated that 9 of the 10 (90%) participants with CAS in the present sample of children with SD met cutoff values for Mild CAS. Findings from three other studies using the PMI provide interesting comparison data. In a technical report that included 28 children who met both SDCS and Mayo Clinic criteria for CAS (Shriberg & Strand, 2018), the percentages of participants with the four PMI classifications were Mild: 50%, Mild-Moderate: 17.9%, Moderate-Severe: 14.3%, and Severe: 17.9%. In the study of 346 children with CND described previously (Shriberg, Strand, et al., 2019), PMI percentage findings for the 15 children with CAS were Mild: 73.3%, Mild-Moderate: 20.0%, Moderate-Severe: 6.7%, and Severe: 0%. Last, in a study that included 19 participants with adult-onset Apraxia of Speech (Shriberg et al., 2017d), the percentages of participants with each of the four PMI severity classifications were Mild: 42.1%, Mild-Moderate: 15.7%, Moderate-Severe: 21.1%, and Severe: 21.1%. Thus, in comparison to a range of 42.1% to 73.4% Mild CAS in participants in these latter three groups, 90% of the present 10 speakers with CAS in children recruited for idiopathic SD were classified as Mild, with implications for genetic research and for treatment. Alternatively, Mild CAS for 9 of the 10 speakers, as determined by the percentage of inappropriate pauses on the PMI, could have been associated with the explicit or tacit inclusionary/exclusionary criteria for referral of children with idiopathic SD to the present study, or with a finding that does not replicate.
Childhood dysarthria & childhood apraxia of speech
Prevalence findings
As shown in Figure 3, none of the 415 participants recruited for SD in the present sample met SDCS criteria for concurrent idiopathic CD & CAS.
Discussion
The CD & CAS classification is included in the SDCS because, as indicated previously, research indicates that CD frequently co-occurs with CAS. This trend has been increasingly reported in the CAS literature in both children and adults, notably in the FOXP2 speech-genetics literature (French et al., 2018; Morgan, Fisher, Scheffer, & Hildebrand, 2016; Morgan, Liégeois, & Vargha-Khadem, 2010; Morgan & Webster, 2018; Turner et al., 2013; see review in Carrigg et al., 2016). In the study of motor speech disorders in 346 children with CND (Shriberg, Strand, et al., 2019), prevalence findings were 4.3% for CAS alone and 4.9% for CAS concurrent with CD. In the study cited previously of 28 children who met both SDCS and Mayo Clinic criteria for CAS (Shriberg & Strand, 2018), prevalence findings were 53% for CAS and 46.4% for CD & CAS. SDCS analyses of the 19 adults recruited for adult-onset Apraxia of Speech cited above (Shriberg et al., 2017d) indicated that 21.1% met criteria for apraxia of speech alone; 78.9% met criteria for apraxia of speech concurrent with dysarthria. Despite presumed differences in the loci of speech processing deficits in apraxia and dysarthria, such findings in childhood and adult-onset apraxia of speech support the likelihood of common neurological pathways for some forms of developmental and acquired apraxia and dysarthria.
Population-based estimates of the prevalence of idiopathic motor speech disorders
The present estimates of the prevalence of motor speech disorders in 415 children recruited for SD were based on findings from data collected from convenience samples in six cities in the USA. An estimate of the population-based point-prevalence of motor speech disorders can be obtained by multiplying the prevalence estimates from these samples by population-based estimates of the prevalence of idiopathic SD. Three population-based estimates of the prevalence of idiopathic SD in children, each speaking a different dialect of English, have been reported in the past two decades. The three studies described next in Table 5 each include detailed discussions of the sampling, speech measures, and constraints associated with the methods used in the study.
Table 5.
Estimates of the prevalence of idiopathic MSD. Estimates of the prevalence of MSD in idiopathic SD are from the present study. Estimates of the prevalence of idiopathic SD are from studies in Australia, England, and the USA.
| Present Study |
Prevalence of idiopathic SD from three population-based samples of children in three countries |
Estimates of the population prevalence of idiopathic MSD |
|||||
|---|---|---|---|---|---|---|---|
| SDCS MSD Classifications | Abbreviation | Prevalence Estimate in Idiopathic SD | Eadie et al. (2015) | Shriberg et al. (1999) | Wren et al. (2016) | ||
| Age: | 4 yrs | 6 yrs | 8 yrs | 4–8 yrs | |||
| No Motor Speech Disorder | No MSD | 82.2% | n: | 1,494 | 1,328 | 7, 390 | 10,212 |
| Speech Motor Delay | SMD | 12.0% | Population-based estimates of | ||||
| Childhood Dysarthria | CD | 3.4% | the prevalence of idiopathic SD: | 3.4% | 3.8% | 3.6% | 3.4 – 3.8/100 |
| Childhood Apraxia of Speech | CAS | 2.4% | SMD | 0.4% | 0.5% | 0.4% | 4/1000 |
| CD | 0.1% | 0.1% | 0.1% | 1/1000 | |||
| Childhood Dysarthria & Childhood Apraxia of Speech | CD & CAS | 0.0% | CAS | 0.1% | 0.1% | 0.1% | 1/1000 |
| CD & CAS | 0.0% | 0.0% | 0.0% | 0/1000 | |||
Note: MSD = Motor Speech Disorder; SD = Speech Delay; SDCSS = Speech Disorders Classification System Summary.
The left-most section of Table 5 includes the prevalence estimates just reviewed for the four SDCS motor speech classification groups in the present study of children recruited for SD. The middle section of Table 5 includes information on the three population-based estimates of the prevalence of idiopathic SD, including 1,494 4-year-old children from Australia (Eadie et al., 2015), 1,328 6-year-old children from the United States (Shriberg, Tomblin, & McSweeny, 1999), and 7,390 8-year-old children from England (Wren et al., 2016). As shown in Table 5, the three studies indicate that the population-based estimate of the point prevalence of idiopathic SD in children ages 4 to 8 years is 3.4% – 3.8%.
The right-most section in Table 5 includes the population-based prevalence estimates for each of the four motor speech disorders. Point-prevalence, population-based estimates for each of the four motor speech disorders were obtained by multiplying the prevalence estimates for each classification in the present study by the averaged population-based estimates of the prevalence of idiopathic SD. It is important to underscore that the point-prevalence estimates in Table 5 apply to children 4 to 8 years of age with idiopathic SD as defined in the three studies. The prevalence estimates in Table 5 for childhood motor speech disorders in children with idiopathic SD are SMD: 4 children per 1,000; CD: 1 child per 1,000; CAS: 1 child per 1,000; and CD & CAS: 0 children per 1,000.
Summary and conclusions
Summary
We estimated the prevalence of five motor speech classifications in children recruited for studies of idiopathic SD. The percentage of children with no concurrent MSD in a sample of 415 children with idiopathic SD was 82.2%. Of the 17.8% participants with idiopathic SD and a concurrent MSD at assessment, the prevalences of the four types of MSD were SMD: 12%; CD: 3.4%; CAS: 2.4%; and CD & CAS: 0%. These findings, together with findings from population-based point-prevalence studies of idiopathic SD in three countries were used to estimate the population prevalence rates of MSD in 4-to 8-year-old children with idiopathic SD. The estimated rates were approximately 4 children per 1,000 with SMD, approximately 1 child per 1,000 with CD, approximately 1 child per 1,000 with CAS, and 0 children per 1,000 with concurrent CD & CAS.
The internal and external validity of these initial estimates of the prevalence of four motor speech classifications in children with idiopathic SD rest on the validity and reliability of the methods and operationalized and standardized measures of SMD, CD, and CAS described and referenced in the text and Supplement. These measures have only recently become available. Studies by other research groups using the present behavioural measures and other measurement modalities (e.g., neurologic, physiologic, kinematic) are needed to cross-validate and extend the present initial prevalence findings.
Conclusions
With the above methodological considerations in mind, the following five conclusions are offered about the prevalence of motor speech disorders in children with idiopathic SD and in the population.
The prevalence of motor speech disorders in children with idiopathic SD is theoretically and clinically substantial
If cross-validated, the present findings would appear to have implications for research, clinical training, and service delivery. Essentially, findings support the need for increased development of the knowledge base in childhood motor speech disorders that guides assessment and treatment, with implications for research in prevention.
Idiopathic SMD is a prevalent clinical entity
A primary finding in the present and associated research is additional support for SMD as a type of childhood motor speech disorder. Findings are interpreted to support the construct of an idiopathic neurodevelopmental delay posited to occur in the execution phase of speech processing that may be concurrent with SD in approximately four 4-to 8-year-old children per 1,000. Support for the term Speech Motor Delay is discussed in the context of longitudinal findings reported for SMD in Shriberg, Campbell, et al. (2019).
A speculation is that a significant proportion of children inappropriately identified and treated for CAS may meet criteria for SMD. That is, due to speech, prosody, and voice features common to both CAS and SMD (e.g., vowel distortions, slow rate, inappropriate stress, voice quality deficits), some percentage of children with SD who are false positives for CAS may be true positives for SMD (cf., Shriberg, Campbell, et al., 2019; Shriberg & Wren, 2019). Preliminary discussions consider treatment implications of SMD as an execution deficit (Shriberg, Campbell, et al., 2019) and CAS as a transcoding deficit (Shriberg et al., 2017b).
Findings are interpreted to support an idiopathic subtype of CD
A third finding in the present study is that 3.4% of children recruited for idiopathic SD met SDCS criteria for concurrent CD, with the point-population prevalence of CD concurrent with idiopathic SD estimated at one 4-to 8-year-old child per 1,000 children. As discussed, generalizations from the CD subtype findings are especially preliminary, given the low prevalence rates yielding phenotype findings in the present sample for only 14 participants. A comparative question to address in future research is the phenotypic similarities and differences associated with CD compared to those associated with SMD. As noted above, the speech processing deficits of both CD and SMD are posited to occur at the execution phase of speech production (Figure 1). Additional research is needed to explicate the type and severity of sensorimotor deficits associated with each classification.
Findings cross-validate a prior prevalence estimate for CAS of 1 child per 1,000
The population-based estimate of the prevalence of idiopathic CAS in the present study (1 child per 1,000) is essentially similar to a prevalence estimate of 1–2 children per 1,000 for idiopathic CAS reported over two decades previously using different diagnostic measures (Shriberg et al., 1997). The present finding constrains the earlier estimate to the point-prevalence age range of 4 to 8 years.
It is useful to note that each of the adjectives in a summary description of CAS over a decade ago, in which CAS was characterized as a rare, severe, and persistent disorder (American Speech-Language-Hearing Association, 2007), may not be accurate. On the rarity of CAS, although there is no international consensus on the criteria for rare diseases and disorders, a common epidemiological criteria for a rare disorder is a lifetime prevalence of 1 in 2,000 persons (https://rarediseases.info.nih.gov/diseases/pages/31/faqs-about-rare-diseases). This is a more rare prevalence rate for idiopathic CAS than the present population prevalence estimate (1 in 1,000 children), the rate approximately similar to the population prevalence rate estimated in the present study also for CD. On the issue of severity, CAS studies of children at the ages of the current samples (Table 1) indicate that rather than always expressed as a severe disorder, CAS can be expressed as only mild to moderate in severity (Murray & Iuzzini-Seigel, 2017; Shriberg & Strand, 2018, p. 28). Last, on the persistence of CAS, trends in treatment research include a variety of findings indicating efficacious treatment of children with idiopathic CAS (e.g., Murray & Iuzzini-Seigel, 2017).
Cross-validation is needed of the present findings of 0% CD & CAS in children with idiopathic SD
In comparison to the relatively high prevalence of concurrent dysarthria and apraxia of speech in children and adults with CND, the 0% prevalence finding for CD & CAS in the present moderately large sample of children with idiopathic SD warrants additional study. If the prevalence estimate is cross-validated, this finding has implications for comparative genomic and neuromotor studies of childhood and adult participants with CD, CAS, and concurrent CD & CAS in idiopathic contexts and in the context of well-characterized CND.
Supplementary Material
Acknowledgments
We thank each of the following colleagues for her or his contribution to this research: Richard Boada, Roger Brown, Thomas Campbell, Joseph Duffy, Marios Fourakis, Lisa Freebairn, Jordan Green, Sheryl Hall, Kathy Jakielski, Heather Karlsson, Barbara Lewis, Jennifer McGlothlin, Jane McSweeny, Christopher Moore, Bruce Pennington, Nancy Potter, Erin Redle, Heather Rusiewicz, Alison Scheer-Cohen, Edythe Strand, Christie Tilkens, Jennifer Vannest, Jennell Vick, and David Wilson.
Funding
This research was supported by National Institute on Deafness and Other Communication Disorders Grant DC000496 and in part by a core grant to the Waisman Center from the National Institute of Child Health and Human Development (U54 HD090256).
Abbreviations:
- CAS
childhood apraxia of speech
- CD
childhood dysarthria
- CND
complex neurodevelopmental disorders
- DI
dysarthria index
- DSI
dysarthria subtype indices
- MSD
motor speech disorder
- No MSD
no motor speech disorder
- NSA
normal(ized) speech acquisition
- PEPPER
programs to examine phonetic and phonologic evaluation records
- PM
pause marker
- PMI
pause marker index
- PSD
persistent speech delay
- PSE
persistent speech errors
- SD
speech delay
- SDCS
speech disorders classification system
- SDCSS
speech disorders classification system summary
- SE
speech errors
- SMD
speech motor delay
Footnotes
Color versions of one or more of the figures in the article can be found online at www.tandfonline.com/iclp.
This article was originally published with formatting errors, which have now been corrected in the online version. Please see Correction (http://dx.doi.org/10.1080/02699206.2019.1616869)
Disclosure Statement
The authors report no declarations of interest.
References
- Allison K, Cordova C, Iuzzini-Seigel J,& Green J (2017, November). Diagnosing apraxia: A systematic review of recent literature on differential diagnosis of AOS and CAS Los Angeles, CA: Technical Talk at the annual convention of the American Speech, Language, and Hearing Association. [Google Scholar]
- Allison KM, & Hustad KC (2018). Data-driven classification of dysarthria profiles in children with cerebral palsy. Journal of Speech, Language, and Hearing Research, 61, 2837–2853. doi: 10.1044/2018_JSLHR-S-17-0356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed. ed.). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- American Speech-Language-Hearing Association. (2007). Childhood apraxia of speech [Technical report] Retrieved from
- Archibald LM, & Alloway TP (2008). Comparing language profiles: Children with specific language impairment and developmental coordination disorder. International Journal of Language & Communication Disorders, 43, 165–180. doi: 10.1080/13682820701422809 [DOI] [PubMed] [Google Scholar]
- Baker E, Williams AL, McLeod S, & McCauley R (2018). Elements of phonological interventions for children with speech sound disorders: The development of a taxonomy. American Journal of Speech-Language Pathology, 27, 906–935. doi: 10.1044/2018_AJSLP-17-0127 [DOI] [PubMed] [Google Scholar]
- Baylis AL, & Shriberg LD (2018). Estimates of the prevalence of speech and motor speech disorders in youth with 22q11.2 Deletion syndrome. American Journal of Speech-Language Pathology Advance online publication. doi: 10.1044/2018_AJSLP-18-0037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernthal JE, Bankson NW, & Flipsen P Jr. (2017). Articulation and phonological disorders: Speech sound disorders in children (8th ed.). Boston, MA: Pearson Education. [Google Scholar]
- Bishop DV (2002). Motor immaturity and specific speech and language impairment: Evidence for a common genetic basis. American Journal of Medical Genetics, 114, 56–63. doi: 10.1002/ajmg.1630 [DOI] [PubMed] [Google Scholar]
- Bowen C (2015). Children’s speech sound disorders (2nd ed.). Chichester, England: Wiley-Blackwell. [Google Scholar]
- Bradford A, Murdoch B, Thompson E, & Stokes P (1997). Lip and tongue function in children with developmental speech disorders: A preliminary investigation. Clinical Linguistics & Phonetics, 11, 363–387. doi: 10.1080/02699209708985201 [DOI] [Google Scholar]
- Carrigg B, Parry L, Baker E, Shriberg LD, & Ballard KJ (2016). Cognitive, linguistic, and motor abilities in a multigenerational family with Childhood Apraxia of Speech. Archives of Clinical Neuropsychology 10.1093/arclin/acw077. [DOI] [PMC free article] [PubMed]
- Carrow-Woolfolk E (1995). Oral and Written Language Scales (OWLS) Bloomington, MN: Pearson Assessment. [Google Scholar]
- Cermak SA, Ward EA, & Ward LM (1986). The relationship between articulation disorders and motor coordination in children. American Journal of Occupational Therapy, 40, 546–550. [DOI] [PubMed] [Google Scholar]
- Cheng HC, Chen HY, Tsai CL, Chen YJ, & Cherng RJ (2009). Comorbidity of motor and language impairments in preschool children of Taiwan. Research in Developmental Disabilities, 30, 1054–1061. doi: 10.1016/j.ridd.2009.02.008 [DOI] [PubMed] [Google Scholar]
- Davis BL, Jakielski KJ, & Marquardt TP (1998). Developmental apraxia of speech: Determiners of differential diagnosis. Clinical Linguistics & Phonetics, 12, 25–45. doi: 10.3109/02699209808985211 [DOI] [Google Scholar]
- Deriziotis P, & Fisher SE (2017). Speech and language: Translating the genome. Trends in Genetics : TIG, 33, 642–656. doi: 10.1016/j.tig.2017.07.002 [DOI] [PubMed] [Google Scholar]
- Duchow H, Lindsay A, Roth K, Schell S, Allen D, & Boliek CA (in press). The co-occurrence of possible developmental coordination disorder and suspected childhood apraxia of speech. Canadian Journal of Speech-Language Pathology and Audiology
- Duffy JR (2013). Motor speech disorders: Substrates, differential diagnosis, and management (3rd ed.). St. Louis, MO: Mosby. [Google Scholar]
- Eadie P, Morgan A, Ukoumunne OC, Ttofari Eecen K, Wake M, & Reilly S (2015). Speech sound disorder at 4 years: Prevalence, comorbidities, and predictors in a community cohort of children. Developmental Medicine and Child Neurology, 57, 578–584. doi: 10.1111/dmcn.12635 [DOI] [PubMed] [Google Scholar]
- Eising E, Carrion-Castillo A, Vino A, Strand EA, Jakielski KJ, Scerri TS, … Fisher SE (2018). A set of regulatory genes co-expressed in embryonic human brain is implicated in disrupted speech development. Molecular Psychiatry Advance online publication. doi: 10.1038/s41380-018-0020-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flipsen P Jr. (2003). Articulation rate and speech-sound normalization failure. Journal of Speech, Language, and Hearing Research, 46, 724–737. doi: 10.1044/1092-4388(2003/058) [DOI] [PubMed] [Google Scholar]
- Flipsen P Jr. (2015). Emergence and prevalence of persistent and residual speech errors. Seminars in Speech and Language, 36, 217–223. doi: 10.1055/s-0035-1562905 [DOI] [PubMed] [Google Scholar]
- Forrest K (2003). Diagnostic criteria of developmental apraxia of speech used by clinical speech-language pathologists. American Journal of Speech-Language Pathology, 12, 376–380. doi: 10.1044/1058-0360(2003/083) [DOI] [PubMed] [Google Scholar]
- French CA, Vinueza Veloz MF, Zhou K, Peter S, Fisher SE, Costa RM, & De Zeeuw CI (2018). Differential effects of Foxp2 disruption in distinct motor circuits. Molecular Psychiatry. Advance online publication doi: 10.1038/s41380-018-0199-x. [DOI] [PMC free article] [PubMed]
- Gaines R, & Missiuna C (2007). Early identification: Are speech/language-impaired toddlers at increased risk for Developmental Coordination Disorder? Child: Care, Health, and Development, 33, 325–332. [DOI] [PubMed] [Google Scholar]
- Goffman L (1999). Prosodic influences on speech production in children with Specific Language Impairment and speech deficits: Kinematic, acoustic, and transcription evidence. Journal of Speech, Language, and Hearing Research, 42, 1499–1517. doi: 10.1044/jslhr.4206.1499 [DOI] [PubMed] [Google Scholar]
- Goozée J, Murdoch B, Ozanne A, Cheng Y, Hill A, & Gibbon F (2007). Lingual kinematics and coordination in speech-disordered children exhibiting differentiated versus undifferentiated lingual gestures. International Journal of Language & Communication Disorders, 42, 703–724. doi: 10.1080/13682820601104960 [DOI] [PubMed] [Google Scholar]
- Guerra J, & Cacabelos R (2018). Genomics of speech and language disorders. Embo Reports doi: 10.20944/preprints201809.0492.v2 [DOI]
- Hill EL (2001). Non-specific nature of specific language impairment: A review of the literature with regard to concomitant motor impairments. International Journal of Language and Communication Disorders, 36, 149–171. doi: 10.1080/13682820010019874 [DOI] [PubMed] [Google Scholar]
- Jakielski KJ (2008a, July). Beginning at the end: What does resolved apraxia really mean? Keynote address at the National Conference on Childhood Apraxia of Speech, Williamsburg, VA. [Google Scholar]
- Jakielski KJ (2008b, July). Persistent speech and language needs of children and teens with CAS. Presentation at the National Conference on Childhood Apraxia of Speech, Williamsburg, VA. [Google Scholar]
- Kaufman AS, & Kaufman NL (2004). Kaufman Brief Intelligence Test – (KBIT-2) (2nd ed.). San Antonio, TX: Pearson Assessments. [Google Scholar]
- Lewis BA, Avrich AA, Freebairn LA, Taylor HG, Iyengar SK, & Stein CM (2011). Subtyping children with speech sound disorders by endophenotypes. Topics in Language Disorders, 31, 112–127. doi: 10.1097/TLD.0b013e318217b5dd [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mabie HL, & Shriberg LD (2017). Speech and motor speech measures and reference data for the Speech Disorders Classification System (SDCS). (Technical Report No. 23). Phonology Project, Madison: Waisman Center, University of Wisconsin–Madison; Retrieved from Phonology Project website: http://www.waisman.wisc.edu/phonology/ [Google Scholar]
- McLeod S, & Baker E (2017). Children’s speech: An evidence-based approach to assessment and intervention Boston, MA: Pearson Education. [Google Scholar]
- McSweeny JL, Fourakis M, Hall SD, Karlsson HB, Lohmeier HL, Tilkens CM, … Shriberg LD (2012). Reference data for the Madison Speech Assessment Protocol (MSAP): A database of 28 participants, 3-to-6 years of age, with speech delay. (Technical Report No. 19). Phonology Project, Madison: Waisman Center, University of Wisconsin–Madison; Retrieved from Phonology Project website: http://www.waisman.wisc.edu/phonology/ [Google Scholar]
- Morgan A, Fisher SE, Scheffer I, & Hildebrand M (2016). FOXP2-related speech and language disorders. In Pagon RA, Adam MP, Ardinger HH, Wallace SE, Amemiya A, Bean LJ, … Stephens K (Eds.), GeneReviews® [internet] Seattle: University of Washington. [Google Scholar]
- Morgan AT, Liégeois F, & Vargha-Khadem F (2010). Motor speech outcome as a function of the site of brain pathology: A developmental perspective. In Maassen B & van Lieshout P (Eds.), Speech motor control: New developments in basic and applied research (pp. 95–115). Oxford, NY: Oxford University Press. [Google Scholar]
- Morgan AT, & Liégeois F (2010). Re-thinking diagnostic classification of the dysarthrias: A developmental perspective. Folia Phoniatrica et Logopaedica: Official Organ of the International Association of Logopedics and Phoniatrics (IALP), 62, 120–126. doi: 10.1159/000287210 [DOI] [PubMed] [Google Scholar]
- Morgan AT, & Webster R (2018). Aetiology of childhood apraxia of speech: A clinical practice update for paediatricians. Journal of Paediatrics and Child Health, 54, 1090–1095. doi: 10.1111/jpc.14150 [DOI] [PubMed] [Google Scholar]
- Morley ME (1972). The development and disorders of speech in childhood (3rd ed.). Baltimore, MD: Williams & Wilkins. [Google Scholar]
- Murray E, & Iuzzini-Seigel J (2017). Efficacious treatment of children with childhood apraxia of speech according to the international classification of functioning, disability and health. Perspectives of the ASHA Special Interest Groups, 2, 61–76. doi: 10.1044/persp2.SIG2.61 [DOI] [Google Scholar]
- Newmeyer AJ, Grether S, Grasha C, White J, Akers R, Aylward C, … Degrauw T (2007). Fine motor function and oral-motor imitation skills in preschool-age children with speech-sound disorders. Clinical Pediatrics, 46, 604–611. doi: 10.1177/0009922807299545 [DOI] [PubMed] [Google Scholar]
- Nip ISB, Green JR, & Marx DB (2011). The co-emergence of cognition, language, and speech motor control in early development: A longitudinal correlation study. Journal of Communication Disorders, 44, 149–160. doi: 10.1016/j.jcomdis.2010.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owen SE, & McKinlay IA (1997). Motor difficulties in children with developmental disorders of speech and language. Child: Care, Health, and Development, 23, 315–325. [DOI] [PubMed] [Google Scholar]
- Paradise JL, Campbell TF, Dollaghan CA, Feldman HM, Bernard BS, Colborn DK, … Smith CG (2005). Effect of early or delayed insertion of tympanostomy tubes for persistent otitis media on developmental outcomes at age 6 years. The New England Journal of Medicine, 353(6), 576–586. doi: 10.1056/NEJMoa050406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paradise JL, Dollaghan CA, Campbell TF, Feldman HM, Bernard BS, Colborn DK, … Rockette HE (2000). Language, speech sound production, and cognition in three-year-old children in relation to otitis media in their first three years of life. Pediatrics, 105, 1119–1130. doi: 10.1542/peds.105.5.1119 [DOI] [PubMed] [Google Scholar]
- Peter B, Matsushita M, & Raskind WH (2012). Motor sequencing deficit as an endophenotype of speech sound disorder: A genome-wide linkage analysis in a multigenerational family. Psychiatric Genetics, 22, 226–234. doi: 10.1097/YPG.0b013e328353ae92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potter NL, Hall S, Karlsson HB, Fourakis M, Lohmeier HL, McSweeny JL, … Shriberg LD (2012). Reference data for the Madison Speech Assessment Protocol (MSAP): A database of 150 participants 3-to-18 years of age with typical speech. (Technical Report No. 18). Phonology Project, Madison: Waisman Center, University of Wisconsin–Madison; Retrieved from Phonology Project website: http://www.waisman.wisc.edu/phonology/ [Google Scholar]
- Powell RP, & Bishop DVM (1992). Clumsiness and perceptual problems in children with specific language impairment. Developmental Medicine and Child Neurology, 34, 755–765. [DOI] [PubMed] [Google Scholar]
- Programs to Examine Phonetic and Phonologic Evaluation Records. (2019). [PEPPER: Computer software] Madison: Waisman Center, University of Wisconsin–Madison. [Google Scholar]
- Rechetnikov RP, & Maitra K (2009). Motor impairments in children associated with impairments of speech or language: A meta-analytic review of research literature. The American Journal of Occupational Therapy: Official Publication of the American Occupational Therapy Association, 63, 255–263. [DOI] [PubMed] [Google Scholar]
- Redle E, Vannest J, Maloney T, Tsevat RK, Eikenberry S, Lewis B, … Holland SK (2015). Functional MRI evidence for fine motor praxis dysfunction in children with persistent speech disorders. Brain Research, 1597, 47–56. doi: 10.1016/j.brainres.2014.11.047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rice GM, Raca G, Jakielski KJ, Laffin JJ, Iyama-Kurtycz C, Hartley SL, … Shriberg LD (2012). Phenotype of FOXP2 haploinsufficiency in a mother and son. American Journal of Medical Genetics: Part A, 158A, 174–181. doi: 10.1002/ajmg.a.34354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richtsmeier PT, & Goffman L (2015). Learning trajectories for speech motor performance in children with specific language impairment. Journal of Communication Disorders, 55, 31–43. doi: 10.1016/j.jcomdis.2015.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts JE, Burchinal MR, Koch MA, Footo MM, & Henderson FW (1988). Otitis media in early childhood and its relationship to later phonological development. Journal of Speech and Hearing Disorders, 53, 424–432. doi: 10.1044/jshd.5304.424 [DOI] [PubMed] [Google Scholar]
- Roberts JE, Rosenfeld RM, & Zeisel SA (2004). Otitis media and speech and language: A meta-analysis of prospective studies. Pediatrics, 113, 237–247. doi: 10.1542/peds.113.3.e238 [DOI] [PubMed] [Google Scholar]
- Royal College of Speech and Language Therapists. (2011). Developmental Verbal Dyspraxia London: Royal College of Speech and Language Therapists. [Google Scholar]
- Rvachew S, & Brosseau-Lapré F (2018). Developmental phonological disorders: Foundations of clinical practice (2nd ed.). San Diego, CA: Plural Publishing. [Google Scholar]
- Scheer-Cohen AR, Holt AS, Karlsson HB, Mabie HL, McSweeny JL, Tilkens CM, & Shriberg LD (2013). Reference Data for the Madison Speech Assessment Protocol (MSAP): A Database of Fifty 20-to-80 year old Participants with Typical Speech. (Technical Report No. 20). Phonology Project, Madison: Waisman Center, University of Wisconsin–Madison; Retrieved from Phonology Project website: http://www.waisman.wisc.edu/phonology/ [Google Scholar]
- Semel E, Wiig E, & Secord W (2003). Clinical Evaluation of Language Fundamentals-4 (CELF– 4) San Antonio, TX: Harcourt Assessment. [Google Scholar]
- Shriberg LD (1993). Four new speech and prosody-voice measures for genetics research and other studies in developmental phonological disorders. Journal of Speech and Hearing Research, 36, 105–140. doi: 10.1044/jshr.3601.105 [DOI] [PubMed] [Google Scholar]
- Shriberg LD (1994). Five subtypes of developmental phonological disorders. Clinics in Communication Disorders, 4, 38–53. [PubMed] [Google Scholar]
- Shriberg LD (2010a). A neurodevelopmental framework for research in Childhood Apraxia of Speech. In Maassen B & van Lieshout P (Eds.), Speech Motor Control: New developments in basic and applied research (pp. 259–270). Oxford: Oxford University Press. [Google Scholar]
- Shriberg LD (2010b). Childhood speech sound disorders: From post-behaviorism to the post-genomic era. In Paul R & Flipsen P (Eds.), Speech sound disorders in children (pp. 1–34). San Diego, CA: Plural Publishing. [Google Scholar]
- Shriberg LD (2017, July). Motor speech disorder-not otherwise specified: Prevalence and phenotype. Paper presented at the 7th International Conference on Speech Motor Control, Groningen, the Netherlands. [Google Scholar]
- Shriberg LD, Aram DM, & Kwiatkowski J (1997). Developmental apraxia of speech: I. Descriptive perspectives. Journal of Speech, Language, and Hearing Research, 40, 273–285. doi: 10.1044/jslhr.4002.273 [DOI] [PubMed] [Google Scholar]
- Shriberg LD, Austin D, Lewis BA, McSweeny JL, & Wilson DL (1997). The Percentage of Consonants Correct matrix (PCC): Extensions and reliability data. Journal of Speech, Language, and Hearing Research, 40, 708–722. doi: 10.1044/jslhr.4004.708 [DOI] [PubMed] [Google Scholar]
- Shriberg LD, Ballard KJ, Tomblin JB, Duffy JR, Odell KH, & Williams CA (2006). Speech, prosody, and voice characteristics of a mother and daughter with a 7;13 translocation affecting FOXP2. Journal of Speech, Language, and Hearing Research, 49, 500–525. doi: 10.1044/1092-4388(2006/038) [DOI] [PubMed] [Google Scholar]
- Shriberg LD, Campbell TF, Mabie HL, & McGlothlin JH (2019). Initial studies of the phenotype and persistence of Speech Motor Delay (SMD). Clinical Linguistics & Phonetics [DOI] [PMC free article] [PubMed]
- Shriberg LD, Fourakis M, Hall S, Karlsson HB, Lohmeier HL, McSweeny JL, … Wilson DL (2010a). Extensions to the Speech Disorders Classification System (SDCS). Clinical Linguistics & Phonetics, 24, 795–824. doi: 10.3109/02699206.2010.503006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shriberg LD, Fourakis M, Hall S, Karlsson HB, Lohmeier HL, McSweeny JL, … Wilson DL (2010b). Perceptual and acoustic reliability estimates for the Speech Disorders Classification System (SDCS). Clinical Linguistics & Phonetics, 24, 825–846. doi: 10.3109/02699206.2010.503007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shriberg LD, Lohmeier HL, Campbell TF, Dollaghan CA, Green JR, & Moore CA (2009). A nonword repetition task for speakers with misarticulations: The Syllable Repetition Task (SRT). Journal of Speech, Language, and Hearing Research, 52, 1189–1212. doi: 10.1044/1092-4388(2009/08-0047) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shriberg LD, & Mabie HL (2017). Speech and motor speech assessment findings in eight complex neurodevelopmental disorders. (Technical Report No. 24). Phonology Project, Madison: Waisman Center, University of Wisconsin–Madison; Retrieved from Phonology Project website http://www.waisman.wisc.edu/phonology/: [Google Scholar]
- Shriberg LD, Potter NL, & Strand EA (2011). Prevalence and phenotype of childhood apraxia of speech in youth with galactosemia. Journal of Speech, Language, and Hearing Research, 54, 487–519. doi: 10.1044/1092-4388(2010/10-0068) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shriberg LD, & Strand EA (2018). Speech and motor speech characteristics of a consensus group of 28 children with childhood apraxia of speech. (Technical Report No. 25). Phonology Project, Madison, WI: Waisman Center, University of Wisconsin–Madison; Retrieved from Phonology Project website: http://www.waisman.wisc.edu/phonology/ [Google Scholar]
- Shriberg LD, Strand EA, Fourakis M, Jakielski KJ, Hall SD, Karlsson HB, … Wilson DL (2017a). A diagnostic marker to discriminate of childhood apraxia of speech from speech delay: I. Development and description of the pause marker. Journal of Speech, Language, and Hearing Research, 60, S1096–S1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shriberg LD, Strand EA, Fourakis M, Jakielski KJ, Hall SD, Karlsson HB, … Wilson DL (2017b). A diagnostic marker to discriminate childhood apraxia of speech from speech delay: IV. The pause marker index. Journal of Speech, Language, and Hearing Research, 60, S1153–S1169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shriberg LD, Strand EA, Jakielski KJ, & Mabie HL (2019). Estimates of the prevalence of speech and motor speech disorders in persons with complex neurodevelopmental disorders. Clinical Linguistics & Phonetics [DOI] [PMC free article] [PubMed]
- Shriberg LD, Strand EA, & Mabie HL (2016, March). Prevalence estimates for three types of motor speech disorders in Complex Neurodevelopmental Disorders (CND). Paper presented at the Eighteenth Biennial Conference on Motor Speech: Motor Speech Disorders & Speech Motor Control, Newport Beach, CA. [Google Scholar]
- Shriberg LD, Tomblin JB, & McSweeny JL (1999). Prevalence of speech delay in 6-year-old children and co-morbidity with language impairment. Journal of Speech, Language, and Hearing Research, 42, 1461–1481. doi: 10.1044/jslhr.4206.1461 [DOI] [PubMed] [Google Scholar]
- Shriberg LD, & Wren Y (2019). A frequent acoustic sign of Speech Motor Delay (SMD). Clinical Linguistics & Phonetics [DOI] [PMC free article] [PubMed]
- Thorndike RL, Hagen EP, & Sattler JM (1986). Stanford-binet intelligence scale (4th ed.). Chicago, IL: Riverside. [Google Scholar]
- Tilkens CM, Karlsson HB, Fourakis M, Hall SD, Mabie HL, McSweeny JL, ., & Shriberg LD (2017). A diagnostic marker to discriminate Childhood Apraxia of Speech (CAS) from Speech Delay (SD). (Technical Report No. 22). Phonology Project, Madison: Waisman Center, University of Wisconsin–Madison; Retrieved from Phonology Project website: http://www.waisman.wisc.edu/phonology/ [Google Scholar]
- Truong DT, Shriberg LD, Smith SD, Chapman KL, Scheer-Cohen AR, DeMille MMC, … Gruen JR (2016). Multipoint genome-wide linkage scan for nonword repetition in a multigenerational family further supports chromosome 13q as a locus for verbal trait disorders. Human Genetics, 135, 1329–1341. doi: 10.1007/s00439-016-1717-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner SJ, Hildebrand MS, Block S, Damiano J, Fahey M, Reilly S, … Morgan AT (2013). Small intragenic deletion in FOXP2 associated with Childhood Apraxia of Speech and dysarthria. American Journal of Medical Genetics: Part A, 161A, 2321–2326. doi: 10.1002/ajmg.a.36055 [DOI] [PubMed] [Google Scholar]
- Vick JC, Campbell TC, Shriberg LD, Green JR, Truemper K, Rusiewicz HL, & Moore CA (2014). Data-driven subclassification of speech sound disorders in preschool children. Journal of Speech, Language, and Hearing Research, 57, 2033–2050. doi: 10.1044/2014_JSLHR-S-12-0193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Visscher C, Houwen S, Moolenaar B, Lyons J, Scherder EJA, & Hartman E (2010). Motor proficiency of 6-to 9-year-old children with speech and language problems. Developmental Medicine & Child Neurology, 52, e254–e258. doi: 10.1111/j.1469-8749.2010.03774.x [DOI] [PubMed] [Google Scholar]
- Visscher C, Houwen S, Scherder EJA, Moolenaar B, & Hartman E (2007). Motor profile of children with developmental speech and language disorders. Pediatrics, 120, e158–e163. doi: 10.1542/peds.2007-2361 [DOI] [PubMed] [Google Scholar]
- Webster RI, Erdos C, Evans K, Majnemer A, Kehayia E, Thordardottir E, … Shevell MI (2006). The clinical spectrum of developmental language impairment in school-aged children: Language, cognitive, and motor findings. Pediatrics, 118, e1541–e1549. doi: 10.1542/peds.2005-2761 [DOI] [PubMed] [Google Scholar]
- Wilson EM, Abbeduto L, Camarata SM, & Shriberg LD (2019). Estimates of the prevalence of speech and motor speech disorders in adolescents with Down syndrome. Clinical Linguistics & Phonetics [DOI] [PMC free article] [PubMed]
- Wren Y, Miller LL, Peters TJ, Emond A, & Roulstone S (2016). Prevalence and predictors of persistent speech sound disorder at eight years old: Findings from a population cohort study. Journal of Speech, Language, and Hearing Research, 59, 647–673. doi: 10.1044/2015_JSLHR-S-14-0282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoss KA (1975, May). Developmental apraxia of speech in children: Familial patterns and behavioral characteristics. Paper presented at the American Speech-Language-Hearing Association North Central Regional Conference, Minneapolis, MN. [Google Scholar]
- Zelaznik HN, & Goffman L (2010). Generalized motor abilities and timing behavior in children with specific language impairment. Journal of Speech, Language, and Hearing Research, 53, 383–393. doi: 10.1044/1092-4388(2009/08-0204) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zwicker JG, Missiuna C, & Boyd LA (2009). Neural correlates of developmental coordination disorder: A review of hypotheses. Journal of Child Neurology, 24, 1273–1281. doi: 10.1177/0883073809333537 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.