Supplemental digital content is available in the text.
Key Words: Ultrasonography; Physical and Rehabilitation Medicine; Education, Medical, Graduate; Musculoskeletal System
Abstract
Objectives
The aims of the study were to evaluate integration of musculoskeletal ultrasonography education in physical medicine and rehabilitation training programs in 2014–2015, when the American Academy of Physical Medicine & Rehabilitation and Accreditation Council for Graduate Medical Education Residency Review Committee both recognized it as a fundamental component of physiatric practice, to identify common musculoskeletal ultrasonography components of physical medicine and rehabilitation residency curricula, and to identify common barriers to integration.
Design
Survey of 78 Accreditation Council for Graduate Medical Education–accredited physical medicine and rehabilitation residency programs was conducted.
Results
The 2015 survey response rate was more than 50%, and respondents were representative of programs across the United States. Most programs (80%) reported teaching musculoskeletal ultrasonography, whereas a minority (20%) required mastery of ultrasonography skills for graduation. Ultrasonography curricula varied, although most programs agreed that the scope of resident training in physical medicine and rehabilitation should include diagnostic and interventional musculoskeletal ultrasonography, especially for key joints (shoulder, elbow, knee, wrist, hip, and ankle) and nerves (median, ulnar, fibular, tibial, radial, and sciatic). Barriers to teaching included insufficient expertise of instructors, poor access to equipment, and lack of a structured curriculum.
Conclusions
Musculoskeletal ultrasonography has become a required component of physical medicine and rehabilitation residency training. Based on survey responses and expert recommendations, we propose a structure for musculoskeletal ultrasonography curricular standards and milestones for trainee competency.
In accordance with the American Medical Association Resolution 802, medical specialties including physical medicine and rehabilitation (PM&R) have begun to define their own scope of practice and training for ultrasonography.1 International surveys of practicing physiatrists reveal that most respondents perceive that neuro/musculoskeletal ultrasonography (MSKUS) belongs within the scope of physiatric practice.2 Within the United States, the American Academy of Physical Medicine and Rehabilitation has echoed this sentiment, calling MSKUS an essential tool and fundamental component of physiatric practice.3 Subsequently, PM&R residency training requirements were updated in 2015 through the Accreditation Council for Graduate Medical Education (ACGME) Residency Review Committee and American Board of Physical Medicine and Rehabilitation to require exposure to 15 MSKUS procedures.4,5
An evaluation of the state of resident training in 2014 found that 45% of the ACGME-accredited PM&R programs surveyed (or 97% of respondents) provided exposure to MSKUS during training.6 However, only 61% responded that MSKUS training was mandatory during residency. Among these programs, 44% had a formal written curriculum and 39% did not formally evaluate learners. A concurrent multispecialty survey of MSKUS education in residency and fellowship programs reported similar findings, although its response rates for PM&R were low (23%).7
The previous surveys suggest variability in training and educational practices among PM&R residency programs. However, a model PM&R curriculum for MSKUS was first published in 20108 and physician training guidelines for MSKUS have been articulated by multiple professional organizations.9–12 The aim of this study was to expand upon previous research to determine the following: what, if any, aspects of proposed curricula and training guidelines were being consistently implemented across the ACGME-accredited PM&R residency programs in 2015; whether there is consensus among program directors for what MSKUS topics should be taught; and whether common barriers prevented PM&R residency programs from teaching MSKUS.
METHODS
Population
The target population included program directors from all ACGME-accredited PM&R residency programs. The 2015 roster and contact information were obtained and confirmed through the Association of Academic Physiatrists, Association of American Medical Colleges (AAMC), and American Osteopathic Association. Additional program demographics, such as type of affiliated medical school (public vs. private); program size; region of the country (Northeast, Central, South, West); and most recent US News and World Reports (USNWR) PM&R ranking were obtained through online resources of the American Medical Association (FREIDA Online), AAMC (Regional Membership Rosters), and USNWR (http://health.usnews.com/best-hospitals/rehabilitation). US News and World Reports rankings were divided into the following three tiers: Tier 1 comprised the top 25% of programs (n = 20), all of which had reputation scores of higher than 5; Tier 2 included the programs in the top 26%–50% (n = 18), all of which had reputation scores of higher than 1, and all remaining programs (n = 40) were in Tier 3. Program size was divided into quartiles based on the number of enrolled residents (<25th percentile, 25th–50th percentile, 50th–75th percentile, >75th percentile).
Survey Development
Survey content was drawn from material developed for evaluation of ultrasonography education for medical students13,14 as well as curricular topics proposed for specialties using MSKUS, including PM&R,8,15–17 rheumatology,18 pain medicine,19 and sports medicine.20 A survey development specialist formatted items into a questionnaire, which was reviewed iteratively until both the survey developer and MSKUS educators on the team were satisfied with the questions and survey format.
The final survey covered 18 topic areas including program and faculty demographics, curriculum content, educational methods and resources, and barriers to integrating MSKUS into residency training. Program director characteristics included duration of clinical practice, level of ultrasonography training, and clinical experience with MSKUS. Curriculum content covered the following three broad topics: introductory ultrasonography concepts; diagnostic imaging for joints and peripheral nerves; and interventional procedures with ultrasonography. The survey further evaluated whether certain ultrasound-guided procedures were within the scope of PM&R training, taught with ultrasound guidance, or required by programs for graduation from residency. The survey did not ask how programs evaluated MSKUS competency for graduation from residency.
Survey Implementation
The survey was implemented in 2014–2015 using the Dillman Tailored Survey Design Method.21 A link to an electronic version of the survey was e-mailed to program directors via SurveyMonkey (http://www.surveymonkey.com). The e-mail included a cover letter describing the project, an invitation to participate, and explanation that survey response constituted implied consent to participate. Two follow-up e-mails were sent at 1-wk intervals, the final one informing the respondent that they would also receive paper versions of the survey through the US mail. Delivery of the paper versions of the survey were timed to arrive at approximately 1 and 3 mos after the final electronic version. Survey responses were tracked for follow-up but were deidentified after data collection was completed. All results were reported in an aggregate manner, so that individual survey responses were not identifiable. The study protocol (2014E0275) and consent process were approved by the committee on research ethics at the institution at which the research was conducted in accordance with the Declaration of the World Medical Association.
Data Analysis
Respondents who reported having no formal MSKUS curriculum or who had missing responses for a question were scored as not including individual topics in their curriculum. Descriptive and inferential statistics were computed in IBM SPSS Statistics for Windows (v22). χ2 tests of proportion and Fisher's exact test were used to evaluate for response bias between survey respondents and nonrespondents. Inferential statistics were used to draw conclusions about programs across Tiers and to compare relative curricular representation of introductory ultrasonography topics versus diagnostic or interventional procedures. An α level of 0.05 was used across tests. Rasch analysis was conducted on rank data for MSKUS barriers, converting ordinal rankings into interval scale logit scores,22 which facilitated comparison and interpretation of severity of barriers to teaching MSKUS.
RESULTS
Respondent Demographics and Bias Analyses
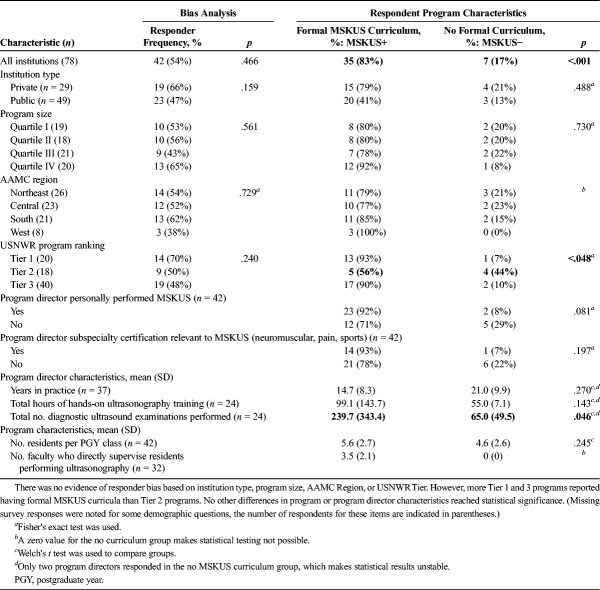
Program directors or their delegates from 42 (54%) of 78 ACGME-accredited physiatry training programs responded with completed surveys. Bias analyses reported in Table 1 revealed that the responding programs were representative of all ACGME-accredited PM&R programs with regard to type of affiliated medical school (public vs. private), program size (quartiles I–IV), region of the country (Northeast, Central, South, West), and USNWR Tier in 2014 (1–3).
TABLE 1.
Respondent demographics and bias analyses for the PM&R MSKUS education survey
Characteristics of respondent programs with formal MSKUS training (MSKUS+) were compared with respondents without formal MSKUS (MSKUS−) (Table 1). Significantly more responders incorporated MSKUS in residency curricula than not (35 vs. 7), χ2(1) = 18.7, P < 0.001. US News and World Reports Tier discriminated between MSKUS+ and MSKUS− programs, χ2(2) = 6.4, P < 0.05, such that Tier 1 and Tier 3 programs were more likely than Tier 2 to have formal MSKUS curricula. However, MSKUS+ programs were not found to be associated with a specific AAMC region, institution type, program size, or program director subspecialty certification (Supplemental Table 1, Supplemental Digital Content 1, http://links.lww.com/PHM/A777), years in practice, or training with MSKUS. One program director characteristic differed significantly between groups: MSKUS+ program directors reported performing more diagnostic scans than those from MSKUS− programs (239.7 ± 343.4 vs. 65 ± 49.5, Welch's t(15.1) = 2.15, P < 0.046). However, there were only two responders in the MSKUS− group, so it is unclear whether this difference would remain significant given a larger sample of PM&R programs.
Educational Resources
The MSKUS+ programs reported an average of 3.5 ± 2.1 faculty (range = 1–8) engaged in supervising residents in MSKUS. All reported that ultrasound machines were available for residents to use. Machines were located with PM&R outpatient services (76% of respondents), at bedside for point-of-care MSKUS (43%), in sports medicine clinics (38%), and with PM&R inpatient services (33%). Only 1 program reported having ultrasound machines available in their simulation center.
Educational Practices
Nearly all MSKUS+ programs reported that MSKUS was taught through didactics (81% of respondents). Other popular teaching methods included point-of-care MSKUS at bedside (67%), facilitated proctor guidance (62%), simulation (including cadaver courses, 50%), and resident-initiated instruction (45%). Independent study or use of online learning modules as teaching resources were less common (24%); however, one program reported offering a 1-mo elective ultrasonography rotation.
Competency Expectations
Few respondents (8 programs or 19% of respondents) required MSKUS competency for graduation from residency (the survey did not ask how competency was measured). US News and World Reports Tier 1 programs were more likely to require MSKUS competency for graduation than either Tier 2 or 3 programs, χ2(2) = 7.9, P < 0.020. However, most programs (80% of respondents and 44% of programs surveyed) expected residents to perform and log clinical ultrasound scans during residency. On average, programs expected residents to perform 35 ± 52 muscle or joint examinations, 22 ± 30 peripheral nerve studies, and 30 ± 44 ultrasound-guided procedures.
Curriculum Content
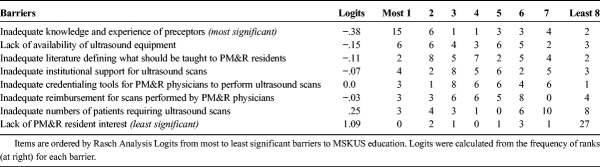
Figure 1 (left) and Supplemental Table 2 (Supplemental Digital Content 2, http://links.lww.com/PHM/A778) display proportion of PM&R programs reporting instruction in foundational ultrasonography topics (knobology/machine operation, ultrasound physics, imaging protocols) and basic MSKUS-specific topics (tissue characteristics, injection techniques).8 Only 50%–75% of programs taught foundational ultrasonography topics. Among MSKUS+ programs, three (8.6%) did not teach any and only ten (28.6%) taught all foundational topics. When proportion of foundational topics taught was compared between USNWR Tiers, no overall relationship was found (P = 0.630). However, Tier 1 programs tended to teach more basic ultrasonography topics (80% of topics) than Tier 3 programs (68% of topics). The most commonly covered foundational topics were how to adjust depth (71%), focus (71%) or gain (69%), probe selection (69% of respondents), and how to enter patient information (67%) and save images (67%). Tissue characteristics and injection technique were covered by 79% and 74% of survey respondents, respectively. Those programs that taught basic tissue characteristics, joint injection, and perineural injection skills also included an average of 78%, 79%, and 85% of foundational topics in their curriculum, respectively.
FIGURE 1.
Proportion of PM&R survey respondents who endorsed having MSKUS curriculum content for topics in ultrasound physics, imaging protocols, knobology, joints, and peripheral nerves.
Figure 1 (right) summarizes the proportion of responding programs that taught diagnostic imaging for joints and peripheral nerves. Core studies, ie, those most frequently taught by residency programs, included the shoulder (79%), elbow (74%), knee (74%), wrist (71%), hip (69%), and ankle (69%) joints and median (76%), ulnar (67%), fibular (peroneal) (57%), radial (55%), tibial (55%), and sciatic (50%) nerves. Those programs that taught diagnostic evaluation of at least one core joint also taught an average of 78%–81% of foundational topics (see Supplemental Table 3, Supplemental Digital Content 3, http://links.lww.com/PHM/A779). Similarly, programs teaching diagnostic evaluation of at least one core nerve covered an average of 79%–89% of foundational topics.
Table 2 shows the diagnostic joint and nerve studies taught by MSKUS+ programs by tier. Technical considerations (multiple cells with expected values <5) prohibited meaningful statistical comparisons, but there is a clear pattern indicating that diagnostic joint evaluations are more commonly taught than diagnostic nerve studies across tiers. In addition, there is a trend for lower tier programs to include a lower percentage of joint or nerve topics than higher tier programs.
TABLE 2.
Curriculum content for MSKUS+ PM&R residency programs by USNWR Tier
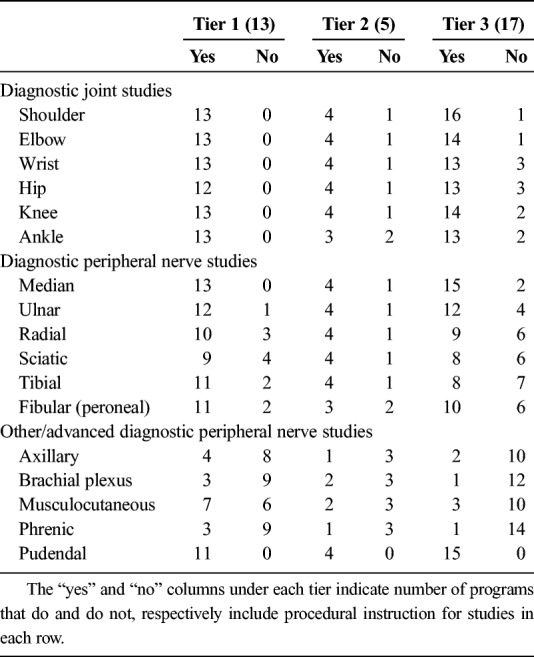
Figure 2 shows the disparity between ultrasound-guided interventional procedures that were reported to be within the scope of PM&R residency training (top bar), versus taught most of the time with ultrasonography (middle bar), or required for residency graduation (bottom bar). Most respondents (91%) indicated that ultrasound-guided joint injections were within the scope of residency training, 74% reported that their curriculum included ultrasound-guided joint injections, but only 40% taught these procedures with ultrasonography guidance most of the time, and 26% required competency for graduation. Similarly, most programs reported that ultrasound-guided nerve blocks (67%) or perineural steroid injections (79%) were within the scope of PM&R training, 45% reported that their curriculum included ultrasound-guided nerve injections, but only 31% and 36%, respectively, taught these injections with ultrasound guidance most of the time, and 12% and 14% required competency with these procedures for graduation.
FIGURE 2.

Proportion of PM&R programs reporting that ultrasound-guided procedures are within the training scope of residency (top bar), taught most of the time (middle bar), or required for graduation (bottom bar) by procedure type. Colored portion of bar represents respondents replying “yes,” gray area represents respondents replying “no,” and white portion represents “undecided” respondents. Most responders thought teaching joint injections, perineural steroid injections, and nerve blocks were within the scope of PM&R residency training, although few endorse teaching these procedures with MSKUS most of the time, and even fewer require competency for graduation. There was little consensus whether other named procedures belonged within the PM&R scope of training.
There was less of a consensus that ultrasound-guided botulinum toxin injection (51%), EMG needle placement (32%), baclofen pump refills (30%), paravertebral injections (22%), and other percutaneous procedures (54%) were within the scope of PM&R residency training. Few programs reported that these procedures (other percutaneous procedures [17%], botulinum toxin injection [14%], baclofen pump refills [7%], paravertebral injections [7%], or needle placement for EMG [5%]) were mostly taught with ultrasound guidance. Almost no programs reported that competency with ultrasound guidance for botulinum toxin injection (7%), EMG needle placement (0%), baclofen pump refills (2%), paravertebral joint injections (0%), or other percutaneous procedures (5%) were required for graduation from their PM&R residency program.
Most MSKUS+ programs that taught ultrasound-guided interventional procedures also reported teaching diagnostic evaluation of the same structures. All programs that reported teaching shoulder and elbow injections with ultrasonography also reported covering diagnostic shoulder (31/31) and elbow (29/29) studies in their curriculum. Nearly all programs that reported teaching ultrasound-guided injections of the wrist, hip, knee, and ankle also taught diagnostic evaluation of these joints (29/30, 28/29, 29/30, and 29/30, respectively). Similarly, all 19 programs that taught ultrasound-guided perineural injection of the median nerve also taught diagnostic evaluation of the carpal tunnel. However, not all programs teaching ultrasound-guided perineural injection of the radial, ulnar, fibular (peroneal), tibial, and sciatic nerves also taught diagnostic evaluation of these nerves (14/18, 16/18, 15/18, 16/18, and 14/17, respectively).
Barriers to MSKUS Education
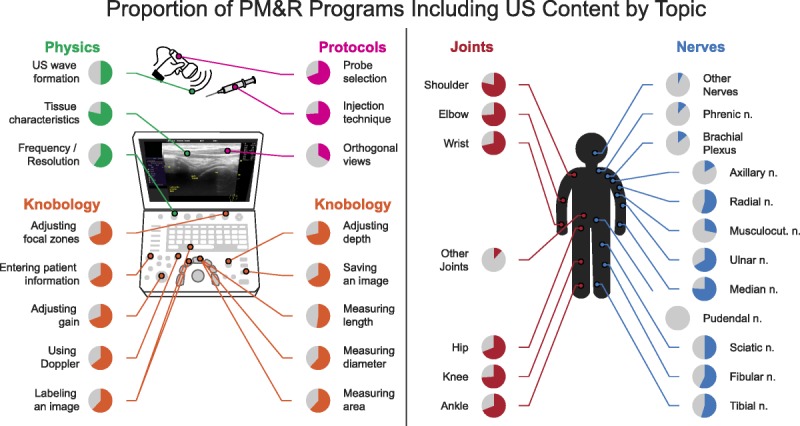
Table 3 lists barriers that survey respondents ranked by importance. “Inadequate knowledge and experience” among preceptors was identified as the most significant barrier to MSKUS education by nearly 43% of respondents. “Lack of availability of ultrasound equipment” and “inadequate literature defining what should be taught” were the next two most important barriers to MSKUS education. Neither “resident interest” nor “inadequate patient numbers” were considered important barriers; most (77%) respondents ranked “lack of PM&R resident interest” as their least significant barrier to MSKUS education.
TABLE 3.
Barriers to teaching MSKUS identified by PM&R residency program directors
DISCUSSION
The aim of this study was to identify aspects of MSKUS curricula and training that were consistently implemented across ACGME-accredited PM&R residency programs in 2015, identify whether there was a consensus among program directors for what MSKUS topics should be taught, and address barriers to learning MSKUS during PM&R residency. At the time of this survey, the ACGME made exposure to ultrasonography a formal requirement for graduation from PM&R residency. However, the PM&R Milestones for assessing trainee competency refer to ultrasonography only in the context of procedural skills for image guidance (PC6). This is reflected in procedural logs of residents graduating in 2015, who averaged 21 ± 45 ultrasound studies for image guidance and 11 ± 28 studies for limb evaluation.23
Comparison with contemporaneous surveys of MSKUS integration in PM&R programs revealed a similar bias toward respondents reporting exposure to MSKUS (83% of 42 responders in the present study, 97% of 36 programs responding in Siddiqui et al.,6 and 100% of 18 programs responding in Berko et al.7). However, the present study had the highest response rate (54% compared with 46% and 23%, respectively), and more programs reported having a formal MSKUS curriculum in our 2015 survey (83% or n = 35 of 42) compared with the 2014 Sidiqqui survey6 (44% or n = 16 of 36) and the 2015 Berko survey7 (100% or n = 18 of 18). Based on the present survey, at least 45% of ACGME-accredited PM&R programs included formal MSKUS curricula by 2015 (35/78, including nonresponders), whereas estimates from the Siddiqui survey6 (16/78 or 21%) and Berko survey7 (18/80 or 23%) are lower, potentially because of lower response rates. Other similarities include the average number of faculty per program teaching MSKUS (3.5 in the present survey, 3 in the Siddiqui survey6), inclusion of didactics and hands-on scanning by programs as teaching methods (81% and 50% in the present study, 89% and 89% in the Siddiqui study,6 and 100% and 80% in the study by Berko et al.7), and the importance of dedicated teaching faculty with adequate MSKUS knowledge and experience.
All three surveys supported the increasing acceptance of MSKUS within the scope of PM&R residency (91% of responders in the present survey) and high resident interest in MSKUS (100%). Responders to the present survey reported that residents were expected to perform an average total of 35 ± 52 muscle or joint examinations, 22 ± 30 peripheral nerve studies, and 30 ± 44 ultrasound-guided procedures by graduation. Survey by Berko et al.7 found that most PM&R programs expected residents to interpret an average of 11–25 diagnostic MSKUS scans, perform an average of 26–50 diagnostic MSKUS scans, and perform an average of 26–50 ultrasound-guided procedures by graduation.
The present survey (see Supplemental Table 4, Supplemental Digital Content 4, http://links.lww.com/PHM/A780) differed from previous surveys by exploring curricular content, relative barriers to curricular implementation, and program director attitudes toward what should be included in a formal MSKUS curriculum. Survey results indicate that the presence and breadth of MSKUS instruction varies across PM&R residency programs and may differentiate programs, such that late or incomplete adopters of a formal curriculum are less likely to be rated in the top USNWR Tier. Indeed, a 2010 survey noted that presence of a strong MSKUS curriculum influenced applicants' rank of PM&R residency programs.8
The variability in MSKUS curricular depth and breadth is consistent with program directors' consensus (63%) belief that there is “inadequate literature defining what should be taught.” For example, programs teaching diagnostic joint or nerve imaging tended to include foundational topics in ultrasound physics, machine instrumentation, and imaging protocols; however, 25% taught only half of the foundational topics in Figure 1. Similarly, most programs teaching interventional ultrasonography procedures for common joints and nerves also taught diagnostic imaging of these structures. However, no single joint or nerve study was taught by all 35 MSKUS+ programs. The studies most commonly taught (>85% of MSKUS+ programs) were diagnostic shoulder, elbow, knee, and wrist examinations; diagnostic median nerve imaging; and ultrasound-guided shoulder injections.
Another component of MSKUS education that deserves study and debate is how to best evaluate the combination of procedural skills, knowledge, and medical decision-making that reflects sufficient MSKUS competency for graduation from residency. At the time of this survey, only eight of the existing PM&R residency programs considered MSKUS competency a graduation requirement and these programs' evaluation methods were not reported. However, the survey results of Siddiqui et al.6 suggest that a range of tools are used for MSKUS competency assessment, including procedure logs and portfolios, patient encounters and checklists, written and oral examinations, objective structured clinical examinations and standardized patient examinations, global performance ratings, record review, and patient surveys. Because additional programs adopt MSKUS curricula, an important future direction will be to establish agreement across training sites regarding both evaluation methods and minimum standards for competency.
Resources exist to guide PM&R decisions regarding resident MSKUS training, curricula, and competency assessments. Stepwise undergraduate medical education curricula establish common ground for learners in the fundamentals (physics, image optimization, and tissue characteristics) and progress to specialty-specific focused ultrasonography.24 Guidelines for focused ultrasonography instruction delineate the clinical knowledge and skills needed for minimum competency (I-AIM: Indication, Acquisition, Interpretation, and Medical decision-making),25 whereas image evaluation tools (B-QUIET: Brightness mode Quality Ultrasound Imaging Evaluation Technique) aid in standardized assessment and feedback of technical ultrasonography skills.26 Using these concepts, specialties such as PM&R can create a framework for diagnostic and interventional MSKUS Milestones (Fig. 3) populated with specialty-specific content across levels (pre-residency through graduation and aspirational targets). Physical medicine and rehabilitation–specific content can be borrowed from ultrasonography curricula of medical schools14,24,27; PM&R residency programs8; sports medicine,11 rheumatology,28 and pain medicine19 fellowships; clinical practice guidelines29; educational demonstrations30–32; and program director responses to this survey. Figure 3 depicts exemplar MSKUS Milestones developed for a PM&R residency program that can serve as a starting point for conversation and debate among medical educators responsible for defining PM&R curricula through the ACGME and American Board of Physical Medicine and Rehabilitation. For example, the Level 4 (Graduation Target) number of MSKUS scans for diagnosis and injection guidance in Figure 3 are 25 and 15, respectively. These numbers corresponded to the exemplar program's local hospital credentialing requirements for MSKUS billing. One might argue that for the purposes of competency assessment, Graduation Target numbers should be higher, eg, a total of 40 good quality scans for diagnosis and 25 for guided injection. These minimum competency benchmarks require further discussion at the ACGME Residency Review Committee and American Board of Physical Medicine and Rehabilitation level.
FIGURE 3.
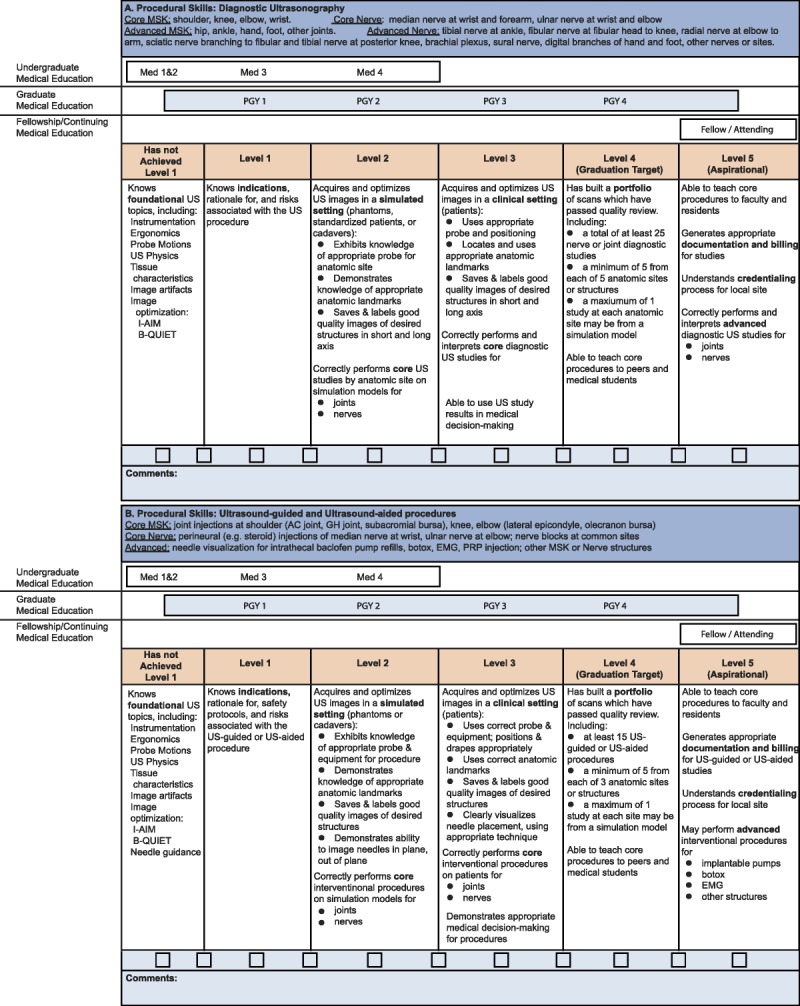
Sample MSKUS Milestones for (A) diagnostic nerve and joint studies and (B) interventional procedures. Foundational ultrasonography concepts (ultrasound physics, machine operation) and basic MSKUS skills (tissue characteristics, needle guidance technique) are medical student or intern-level competencies. Musculoskeletal ultrasonography knowledge and skills across core topics comprise graduation target competencies for PM&R residents (Level 4), whereas advanced topics are reserved for fellowship or practicing clinicians. Core and advanced topic divisions are a potential subject for debate by the PM&R Residency Review Committee.
Other significant barriers to MSKUS education endorsed by respondents, namely, “inadequate knowledge & experience of preceptors” (66%) and “lack of availability of ultrasound equipment” (54%), may be slowly resolving. Near-peer teaching of learners by senior trainees can supplement preceptor-mediated training.33,34 Meanwhile, MSKUS training opportunities are expanding through professional associations' clinician certificate programs and train-the-trainer sessions (eg, American Academy of Physical Medicine and Rehabilitation's STEP: Skills, Training, Evaluation and Performance, American Association of Neuromuscular and Electrodiagnostic Medicine's Neuromuscular Ultrasound Workshops, AAP's Faculty Development course on Teaching MSKUS Education). This is important because our survey data show a possible bias toward programs having a structured curriculum if the program director performs MSKUS himself/herself. Furthermore, portable, hand-held machines (eg, Butterfly IQ by Butterfly, Lumify by Phillips, IViz by Fuji/Sonosite, and Vscan by GE) are becoming increasingly affordable and thus potentially available at PM&R residency training sites.
In summary, although MSKUS is tracked through the ACGME as a procedural skill, most programs with a formal MSKUS curriculum recognize that didactics are required to convey fundamental knowledge (eg, neuromusculoskeletal anatomy, disease conditions, and basics of ultrasonography) before hands-on skill acquisition. Enthusiasm for MSKUS is high among PM&R residents and program directors. Nevertheless, curricula vary in their coverage of foundational concepts, practical skills, anatomic regions, and assessment methods. The next steps in integrating MSKUS education across PM&R training programs should include standardization of a competency-based curriculum with MSKUS-specific milestones, continuing to train MSKUS educators, and allocating residency training resources to buy inexpensive, portable, point-of-care ultrasound machines.
Limitations
Response rate was limited to 42 of 78 PM&R training programs. Although respondents were evenly distributed across ACGME region, program size, USNWR program status, and institution type, response was likely biased toward programs already integrating MSKUS in their curriculum. Furthermore, response rate may have been negatively influenced by other MSKUS surveys collected coincident with this study. Data reported here represent the state of MSKUS education in PM&R in 2015, before institution of ACGME program requirements for MSKUS; a similar survey will need to be conducted to evaluate how educational practices have changed in the interim and how MSKUS competency is assessed by residency programs. Finally, resident interest in MSKUS was inferred from program directors' ratings about barriers and not from resident responses.
CONCLUSIONS
Cognitive and technical MSKUS skills are becoming an accepted part of PM&R residency training; however, resident experiences vary by program. As a result, standardization of preceptor training, MSKUS curriculum, and competency-based Ultrasonography Milestones for PM&R residency are needed. The suggested MSKUS Milestones for PM&R proposed here may serve as a starting point for further discussion among PM&R educators. As more programs integrate MSKUS exposure, there will be opportunities to codify milestones matched to minimal core and enriched competencies for ultrasonography in physiatry.
Supplementary Material
Footnotes
The study was supported by the Ohio State University Faculty Teaching Scholars Certificate Program, the Association of Academic Physiatrists Program for Academic Leadership, and Department of Physical Medicine & Rehabilitation of the Ohio State University.
Portions of this study were presented at the Program for Academic Leadership during the 2015 and 2016 Annual Meetings of the Association of Academic Physiatrists (San Antonio, Texas, March 11–14, 2015, and Sacramento, California, February 17–20, 2016), Society of Ultrasound in Medical Education (Portland, Oregon, October 10–12, 2014), and at the 2015 and 2016 Annual Conventions of the American Institute for Ultrasound in Medicine (Orlando, Florida, March 21–25, 2015, and New York, New York, March 17–21, 2016).
Ryan D. Thompson is in training.
Financial disclosure statements have been obtained, and no conflicts of interest have been reported by the authors or by any individuals in control of the content of this article.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.ajpmr.com).
REFERENCES
- 1.American Medical Association: Privileging for Ultrasound Imaging. Resolution 802. Vol H-230Dec 1999; Reaffirmed; Sub. res 108, Jun 2000:960
- 2.Özçakar L, Tok F, Kesikburun S, et al. : Musculoskeletal sonography in physical and rehabilitation medicine: results of the first worldwide survey study. Arch Phys Med Rehabil 2010;91:326–31 [DOI] [PubMed] [Google Scholar]
- 3.American Academy of Physical Medicine and Rehabilitation: AAPM&R Position Statement on Diagnostic Musculoskeletal Ultrasound or Musculoskeletal Ultrasound-Guided Procedures. Rosemont, IL: AAPM&R; 2014
- 4.Bockenek WL, Massagli TL, Swing SR, et al. : The development of physical medicine and rehabilitation milestones. J Grad Med Educ 2014;6(1 suppl 1):204–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Accreditation Council for Graduate Medical Education, American Board of Physical Medicine & Rehabilitation: The Physical Medicine and Rehabilitation Milestone Project. J Grad Med Educ 2014;6(1 suppl 1):207–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Siddiqui IJ, Luz J, Borg-Stein J, et al. : The current state of musculoskeletal ultrasound education in physical medicine and rehabilitation residency programs. PMR 2016;8:660–6 [DOI] [PubMed] [Google Scholar]
- 7.Berko NS, Goldberg-Stein S, Thornhill BA, et al. : Survey of current trends in postgraduate musculoskeletal ultrasound education in the United States. Skeletal Radiol 2016;45:475–82 [DOI] [PubMed] [Google Scholar]
- 8.Finnoff J, Smith J, Nutz DJ, et al. : A musculoskeletal ultrasound course for physical medicine and rehabilitation residents. Am J Phys Med Rehabil 2010;89:56–69 [DOI] [PubMed] [Google Scholar]
- 9.American Institute of Ultrasound in Medicine: AIUM Training Guidelines for Physicians and Chiropractors Who Evaluate and Interpret Diagnostic Musculoskeletal Ultrasound Examinations. 2014. Available at: http://www.aium.org/resources/viewStatement.aspx?id=51 Accessed March 16, 2015
- 10.American Institute of Ultrasound in Medicine: AIUM Training Guidelines for Physicians and Chiropractors Who Perform Ultrasound-Guided Musculoskeletal Interventional Procedures. 2014. Available at: http://www.aium.org/resources/viewStatement.aspx?id=61 Accessed March 16, 2015
- 11.Finnoff JT, Berkoff DJ, Brennan F, et al. : American Medical Society for Sports Medicine (AMSSM) recommended sports ultrasound curriculum for sports medicine fellowships. Br J Sports Med 2015;49:145–50 [DOI] [PubMed] [Google Scholar]
- 12.Möller I, Janta I, Backhaus M, et al. : The 2017 EULAR standardised procedures for ultrasound imaging in rheumatology. Ann Rheum Dis 2017;76:1974–9 [DOI] [PubMed] [Google Scholar]
- 13.Bahner DP, Goldman E, Way D, et al. : The state of ultrasound education in U. S. medical schools: results of a national survey. Acad Med 2014;89:1681–6 [DOI] [PubMed] [Google Scholar]
- 14.Fox JC, Schlang JR, Maldonado G, et al. : Proactive medicine: the “UCI 30,” an ultrasound-based clinical initiative from the University of California Irvine. Acad Med 2014;89:1–6 [DOI] [PubMed] [Google Scholar]
- 15.Smith J, Finnoff JT: Diagnostic and interventional musculoskeletal ultrasound: part 2. Clinical applications. PM R 2009;1:162–77 [DOI] [PubMed] [Google Scholar]
- 16.Lento PH, Strakowski JA: The use of ultrasound in guiding musculoskeletal interventional procedures. Phys Med Rehabil Clin N Am 2010;21:559–83 [DOI] [PubMed] [Google Scholar]
- 17.De Muynck M, Parlevliet T, De Cock K, et al. : Musculoskeletal ultrasound for interventional physiatry. Eur J Rehabil Med 2012;48:675–87 [PubMed] [Google Scholar]
- 18.Mandl P, Naredo E, Conaghan PG, et al. : Practice of ultrasound-guided arthrocentesis and joint injection, including training and implementation, in Europe: results of a survey of experts and scientific societies. Rheumatology (Oxford) 2012;51:184–90 [DOI] [PubMed] [Google Scholar]
- 19.Antonakakis JG, Ting PH, Sites B: Ultrasound-guided regional anesthesia for peripheral nerve blocks: an evidence-based outcome review. Anesthesiol Clin 2011;29:179–91 [DOI] [PubMed] [Google Scholar]
- 20.Finnoff JT, Hall MM, Adams E, et al. : American Medical Society for Sports Medicine (AMSSM) Position Statement: Interventional Musculoskeletal Ultrasound in Sports Medicine. Clin J Sport Med 2015;25:6–22 [DOI] [PubMed] [Google Scholar]
- 21.Dillman DA: Mail and Internet Surveys: The Tailored Design Method, 2nd ed Hoboken, NJ: John Wiley & Sons, Inc.; 2007 [Google Scholar]
- 22.Wright BD, Masters GN: Rating Scale Analysis. Chicago, IL: MESA Press; 1982 [Google Scholar]
- 23.Accreditation Council for Graduate Medical Education: ACGME Physical Medicine and Rehabilitation Case Logs:National Data Report. Chicago, IL; 2015 [Google Scholar]
- 24.Bahner DP, Adkins EJ, Hughes D, et al. : Integrated medical school ultrasound: development of an ultrasound vertical curriculum. Crit Ultrasound J 2013;5:1–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bahner DP, Hughes D, Royall NA: I-AIM: a novel model for teaching and performing focused sonography. J Ultrasound Med 2012;31:295–300 [DOI] [PubMed] [Google Scholar]
- 26.Bahner DP, Adkins EJ, Nagel R, et al. : Brightness Mode Quality Ultrasound Imaging Examination Technique (B-QUIET). J Ultrasound Med 2011;30:1649–55 [DOI] [PubMed] [Google Scholar]
- 27.Rao S, van Holsbeeck L, Musial JL, et al. : A pilot study of comprehensive ultrasound education at the Wayne State University School of Medicine. J Ultrasound Med 2008;27:745–9 [DOI] [PubMed] [Google Scholar]
- 28.Criscione-Schreiber LG, Bolster MB, Jonas BL, et al. : Competency-based goals, objectives, and linked evaluations for rheumatology training programs: a standardized template of learning activities from the carolinas fellows collaborative. Arthritis Care Res (Hoboken) 2013;65:846–53 [DOI] [PubMed] [Google Scholar]
- 29.American College of Radiology: ACR–AIUM–SPR–SRU Practice Parameter for the Performance of the Musculoskeletal Ultrasound Examination. 2014. Available at: https://www.acr.org/-/media/ACR/Files/PracticeParameters/US-Perf-Interpret.pdf. Accessed March 30, 2015
- 30.Wu C-H, Chang K-V, Özçakar L, et al. : Sonographic tracking of the upper limb peripheral nerves: a pictorial essay and video demonstration. Am J Phys Med Rehabil 2015;94:740–7 [DOI] [PubMed] [Google Scholar]
- 31.Chang KV, Lin CP, Hung CY, et al. : Sonographic nerve tracking in the cervical region: a pictorial essay and video demonstration. Am J Phys Med Rehabil 2016;95:862–70 [DOI] [PubMed] [Google Scholar]
- 32.Hung CY, Hsiao MY, Özçakar L, et al. : Sonographic tracking of the lower limb peripheral nerves: a pictorial essay and video demonstration. Am J Phys Med Rehabil 2016;95:698–708 [DOI] [PubMed] [Google Scholar]
- 33.Luz J, Siddiqui I, Jain NB, et al. : Resident-perceived benefit of a diagnostic and interventional musculoskeletal ultrasound curriculum: a multifaceted approach using independent study, peer teaching, and interdisciplinary collaboration. Am J Phys Med Rehabil 2015;94:1095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rosenberg CJ, Nanos KN, Newcomer KL: The “near-peer” approach to teaching musculoskeletal physical examination skills benefits residents and Medical Students. PMR 2017;9:251–7 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.