Abstract
Purpose of review
The current review gives a concise and updated overview of the relative new field of anticytokine autoantibodies (ACAA) and associated infections with a focus on recent findings regarding clinical manifestions, diagnostic and treatments.
Recent findings
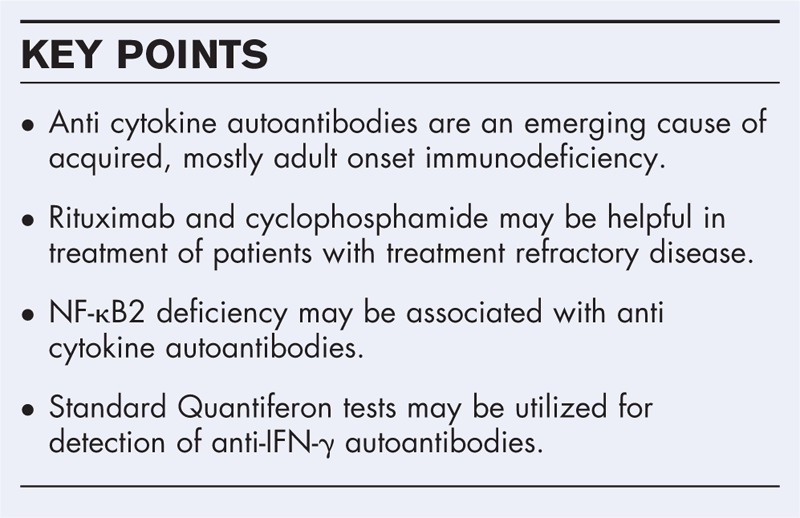
Several recent case reports of unusual presentations of patients with neutralizing autoantibodies to IFN-γ and granulocyt macrophage colony-stimulating factor and expand the spectrum of clinical manifestations and suggest that anticytokine-mediated acquired immunodeficiency causing susceptibility to infection may be underdiagnosed. There is an expanding geographical distribution of antigranulocyt macrophage colony-stimulating factor associated Cryptococcus gattii infection. The spectrum of identified infections in patients with neutralizing antibodies to IFN-γ has a strong endemic component. Rituximab or cyclophophamide in addition to antimycobacterials could be a treatment options in refractory cases. NF-κB2 deficiency may be associated with a complex pattern of high titre neutralizing ACAA similar to autoimmune polyglandular syndrome type I and Thymoma. New technique for the detection of anticytokine antibodies are presented. Quantiferon testing, which is widely available for TB-diagnostic, may be repurposed to detect anti-IFN-γ autoantibodies. We propose that this test could be as well used to show if they are neutralizing.
Summary
ACAA are an emerging cause of acquired immunodeficiency which is likely underdiagnosed. Recent case reports document expanding spectra of clinical manifestations. NF-κB2 deficiency may be associated with a complex anti cytokine autoantibody pattern.
Keywords: anticytokine autoantibodies, granulocyt macrophage colony-stimulating factor, IFN-γ, IL-6, infection, secondary immunodeficiency, Th17 cytokines
INTRODUCTION
Infectious diseases can be considered as normal events in any organisms life time. They are in most cases transient, self-limiting events which would not suggest any significant abnormality or deficiency within the hosts immune defence. However, if opportunistic organisms cause disease, and/or a patient experiences recurrent, chronic or unusual severe infections of more common pathogens when compared with disease controls, then an underlying impairment of the immune defence may be considered. This state of immunodeficiency can be caused by various mechanisms which may be primary or secondary. Primary mechanisms for example include genetic impairments within the immune system (primary immunodeficiencies, PIDs) which cause susceptibility to infectious diseases usually from birth or early age.
Secondary impairments may be caused by the infectious agent themselves such as HIV, which may target crucial nonredundant components of the hosts immune defence with the consequence of severe susceptibility to a wide array of pathogens; by certain noninfectious diseases which may compromise the immune system such as blood born cancers or, disruption of natural barriers as may be found for example in certain skin diseases and protein loosing enteropathies; by therapeutic interventions, for example immunosuppressive drugs for treatments in cancer, autoinflammatory diseases and transplantation; environmental toxins; or ‘extreme’ situations such as malnutrition, very young age (some parts of immunity not fully developed) or old age (immune senescence); autoimmunity to cytokines which will be the topic of this review.
Cytokines are key signalling molecules which orchestrate the immune response and are indispensable for the host defence against pathogens [1]. Primary immunodeficiency are often associated with defects in cytokine production or signalling. Autoantibodies to cytokines have been identified as an emerging alternative pathological mechanism leading to a compromised immune response and susceptibility to infection and may be considered as autoimmune phenocopies of primary immunodeficiencies [2–4].
So far autoantibodies to three cytokines, granulocyt macrophage colony-stimulating factor (GM-CSF), IFN-γ and IL-6 and a group of related TH-17 cytokines, IL-17A, IL-17F, IL-22, IL-23 have been found to be causative or closely associated with susceptibility to infection. This review gives an overview about the field of infections caused by or associated with ACAA and recent developments.
Box 1.
no caption available
AUTOANTIBODIES TO IFN-γ CAUSE SUSCEPTIBILITY TO OPPORTUNISTIC MYCOBACTERIA AND OTHER INTRACELLULAR PATHOGENS
IFN-γ is a key cytokine in the host defence against intracellular pathogens. It is mainly produced by type 1 helper T-cells cells and natural killer cell and acts primarily on monocytes. It is essential for the control of mycobacterial infections. Mendelian susceptibility to mycobacterial disease (MSMD) is a rare condition which predisposes to clinical disease by weakly virulent mycobacteria such as Bacille Calmette Guerin and nontuberculous environmental mycobacteria (NTM). Patients with MSMD have either a defective response to IFN-γ, for example with genetic impairments in the IFN-γ receptor (IFNGR1, IFNGR2) or downstream signalling elements such as STAT1, or a defective production of IFN-γ, for example with genetic defects in IL12B (the shared subcomponent of IL-12 and IL-23) or IL12RB1 (the shared receptor component for IL-12 and IL-23). Patients with MSMD are also susceptible to Salmonella, Candida and Mycobacterium tuberculosis and more rarely to other intramacrophagic bacteria, fungi, parasites and some viruses [5].
Neutralizing autoantibodies to IFN-γ (AIGA) are the autoimmune correlate to primary Mendelian defects in the IFN-γ signalling pathway. The first reports showing a conclusive association to infection with severe atypical mycobacteriosis where published in 2004 [6,7]. Several hundred cases had been described worldwide between 2004 and 2016 [8▪▪]. Browne et al. published a large series of 80 patients with high titre neutralizing anti interferon gamma autoantibodies (nAIGA), thus establishing autoimmune acquired IFN-γ deficiency as a syndrome of a secondary adult-onset immunodeficiency with disseminated mainly nontuberculous mycobacterial infections. Other opportunistic pathogens may include bacteria (e.g. Salmonella, Burkholderia); fungi (e.g. Penicillium, Histoplasma, Cryptococcus) and viruses, in particular varicella zoster virus (VZV) [9]. Further reports confirmed a high prevalence rate among patients with disseminated NTM infections of nearly entirely south east Asian origin [3,4]. This was subsequently explained by the discovery of a strong endemic HLA association [10]. Lin et al.[11] identified a major target epitope.
Some interesting reports with more unusual presentations of nAIGA-related infection were recently published. Ikeda et al.[12] reported a 65-year-old man from Japan with disseminated Mycobacterium avium infection involving both optic nerves in the context of wide dissemination. The neutralizing capacity of the AIGA was confirmed by STAT1 phosphorylation testing and as well reflected by an ‘invalid’ quantiferon assay showing no IFN-γ response to phytohemagglutinine [12]. Koizumi et al.[13] presented a case of a 66-year-old Japanese HIV negative man with M. avium peritonitis and chylous ascites and nAIGA. The patient was previously treated for an angioimmunoblastic T-cell lymphoma with complete remission [13]. Van de Vosse et al.[14] reported nAIFNG in a 38–year-old women of African descent, who presented with necrotizing lymphadenitis due to Histoplasma capsulatum. Her HLA haplotype did not overlap with the one found to be associated with AIGA [10,14]. Miyashita et al.[15] describe nAIGA associated disseminated M. avium infection presenting as bladder lesions and sterile pyuria in a 63-year-old Japanese women. Saba et al.[16], presented a case of AIGA-related refractory Mycobacterium avium complex (MAC) pneumonia in a 45-year-old women of Thai origin, but living in the United States. The patient had been previously diagnosed with Kikuchi lymphadenopathy which was treated with corticosteroids. Her course was further complicated by VZV reactivation, which required intravenous acyclovir treatment [16].
Hase et al.[8▪▪] performed a comprehensive retrospective analysis of 35 studies describing 111 patients with AIGA-associated NTM infections between 2004 and 2016. They calculated a mean age of onset of 52 years (range 15–87). A total of 106 patients (95%) were Asians. The frequencies of isolated NTM species varied according to the known geographical NTM distributions with rapid-growing mycobacteria being predominantly isolated from Thailand, China and Philippines and MAC from Japan, Europe, USA and South Africa. Concomitant organisms where found in 68% of cases and confirmed the strong endemic component. Lymphnodes were the most frequent site of infection (79%) in contrast to AIDS associated disseminate MAC presenting mostly as bacteremia. Based on own and previous studies using Rituximab, Hase et al.[8▪▪] and Koizumi et al.[17▪] concluded that Rituximab in addition to antimycobacterials chemotherapy could be a treatment option in refractory cases. Hase et al.[8▪▪] and Aoki et al.[18▪▪] emphasised the importance of long-term antibiotic therapies to prevent relapses, with Mycobacterium abscessus posing a particular problem. Baerlecken et al.[19], successfully treated a patient with a combination of Plasmaspheresis and pulsed cyclophosphamide. Chetchotisakd et al.[20▪] treated seven patients with refractory M. abscessus infection with cyclophosphamide and obtained clearance in two patients, stable disease without the need for hospitalization in three patients, but two patients did relapse. Nonresponders did not experience reductions of anti IFN-γ autoantibody levels as found in responders [20▪].
ANTIBODIES TO GRANULOCYT MACROPHAGE COLONY-STIMULATING FACTOR CAUSE PULMONARY ALVEOLAR PROTEINOSIS AND ARE ASSOCIATED WITH CRYPTOCOCCOSIS
Granulocyte macrophage colony-stimulating is a haematopoietic growth factor which in particular promotes the development of macrophages, dendritic cells and neutrophils. In the lung it is important for differentiation and function of alveolar macrophages. Auto-antibodies to GM-CSF are the autoimmune correlate of the much rarer primary GM-CSF-Receptor deficiency causing pulmonary alveolar proteinosis (PAP) by impairing the alveolar macrophage mediated surfactant lipid and protein metabolism and leading to accumulation and respiratory insufficiency. Patients suffer from recurrent common pulmonary infections, which may be secondary to the underlying lung dysfunction, but also from infections by opportunistic intracellular pathogens including NTM, Nocardia, Histoplasma[21]. High titre neutralizing anti-GM-CSF where found to be associated with extrapulmonary disseminated disease due to Cryptococcus gattii, Nocardia and Aspergillus in otherwise immunocompetent patients. PAP developed later however in some of them [22–24]. C. gattii, originally mainly identified in tropical regions, is geographically emerging and now increasingly found as well in the US and Europe [25,26]. Several recent studies confirm the link between the presence of neutralizing anti-GM-CSF autoantibodies and cerebral cryptococcosis in particular by C. gattii in the absence of PAP. Kuo et al.[27▪], screened eleven otherwise immunocompetent patients with cryptococcal meningitis from Taiwan and identified four patients (37–59 years old) with neutralizing autoantibodies to GM-CSF as shown by patients plasmas ability to block GM-CSF-induced STAT5 phosphorylation and MIP-1α production. Although the isolates could not be subtyped in this case, infection were likely due to Cryptococcus gattii. Crum-Cianflone et al.[28] identified neutralizing anti-GM-CSF autoantibodies in two previously healthy patients with unusual presentations of C. gattii infection. A 42-year-old white man presented with a spinal epidural abscess and a 34 years old Hispanic man presented with skin and brain involvement. His bronchoscopy showed no lesions but was found to be positive by Polymerase chain reaction (PCR). Patient plasmas were shown to inhibit GM-CSF-induced STAT5 phosphorylation [28]. Demir et al.[29▪] presented a 42-year-old male with C. gattii meningitis and anti-GM-CSF autoantibodies and in whom PAP developed 3 years later. Huynh et al.[30] reported another unusual presentation of endobronchial lesions due to C. gattii in the presence of anti-GM-CSF autoantibodies although their inhibitory activity was not formally ascertained. Clancey et al., recently described an interesting case of travel-acquired anti-GM-CSF associated C. deuterogattii meningitis in an otherwise immunocompetent 69-year-old man from North Carolina which occurred 3 month after he experienced a period of cough and shortness of breath. High titre anti-GM-CSF plasma antibodies were detected. Genomic analysis of the isolated strain showed that it originated from a Cryptococcus outbreak area in the Pacific Northwest, which the patient visited 3 years earlier [31▪]. These cases document the expanding clinical manifestations and geographical distribution of anti-GM-CSF associated C. gattii infection. Given the limited availability of anti-GM-CSF testing and possible still low awareness of this association, under diagnosis of anti-GM-CSF associated C. gattii infection in the absence of PAP is likely.
Presence of anti-GM-CSF autoantibodies should be considered in all patients with symptoms suggesting PAP proteinosis or with extrapulmonary disease, in particular with C. gattii or Nocardia. Identification of the causative anti-GM-CSF autoantibodies has a direct impact on treatment and management. Long-term or even indefinite secondary antifungal prophylaxis must be considered [28]. In more severe antimicrobial treatment refractory cases, plasmaspheresis, exogenous GM-CSF supplementation or B-cell depletion (Rituximab) may be further options [21,32].
SYNDROMIC AUTOANTIBODIES TO TH17 CYTOKINES (IL17A, IL17F, IL-22, IL-23) AND CHRONIC MUCOCUTANEOUS CANDIDIASIS
The cytokines IL-17A, IL-17F and IL-22 are mainly produced by Th17 cells and play an important role in the mucosal defence against Candida. IL-23 is mainly produced by dendritic cells and macrophages and is required for the development of TH17 cells. Primary deficiencies in the IL17 axis including IL-17F, IL-17RA, IL17RF and the intracellular adaptor ACT1 have been found to predispose to chronic mucocutaneous candidiasis (CMC). Patients with impaired IL12/IL23 signalling show as well an increased incidence of CMC. Furthermore, syndromic primary deficiencies in CARD9, STAT3, STAT1 and RORγT and in which CMC is part of the infectious spectrum show as well diminished TH17 immunity [33,34].
Auto immune regulator (AIRE) deficiency causes autoimmune polyglandular syndrome type I (APS1), which is a complex autoimmune syndrome with CMC as its only infectious manifestation [33,34]. A subset of patients with thymoma, a thymic epithelial cancer, may as well present with CMC which may be in the context of more complex infectious complications and dysregulated expression of AIRE. Both conditions present with complex anticytokine serologies secondary to a failure of central tolerance [35].
Puel et al.[36] and Kisand et al.[37] described neutralizing autoantibodies to Th17 cytokines, including IL-17A, IL-17F, IL-22 as part of more complex anticytokine patterns in patient with APS1 and thymoma to be associated with CMC. Rosenberg et al.[38] reported an interesting patient with thymoma and CMC without antibodies to IL17A/F or IL-22 but with high titre autoantibodies to IL-23.
NF-κB2 DEFICIENCY MAY BE ASSOCIATED WITH HIGH TITRE NEUTRALIZING ANTICYTOKINE AUTOANTIBODIES
Ramakrishnan et al.[39▪▪] presented a patient with chronic variable immunodeficiency caused by a heterozygous NFKB2 mutation. The patient developed severe pyogenic bacterial infections but also recurrent viral infections despite Ig replacement therapy. Multiplexed anticytokine serology showed a complex pattern of high titre autoantibodies to Type-I IFNs, and IL12/23 reminiscent to what can be seen in thymoma patients. Rituximab treatment which resulted in a marked reduction of some anticytokine titres and clinical improvement with no further invasive infections was observed. It is unclear, if this improvement is secondary to the reductions in the observed anticytokine titres, given the broad range of so far observed ACAA and potentially many as yet unknown related targets [39▪▪]. In line with this are findings in hypomorphic recombination activation gene deficient patients and Thymoma patients where the incidence and complexity of the patients anticytokine patterns where positively correlated with increased susceptibilities to infections [40,41].
ANTIBODIES TO IL-6 AND SEVERE BACTERIAL INFECTIONS
IL-6 is a pleiotropic cytokine, which is rapidly produced in response to tissue damage and infection. It is a key activator in the acute phase response and induces for example the production of C-reactive protein. It may be overexpressed in autoinflammatory diseases and its therapeutic inhibition has for example been shown to be effective in the treatment of various forms of arthritis [42]. Several PID have been described with either impaired IL-6 signalling or IL-6 production [43,44]. One patient with complete gp130 deficiency presented early onset severe recurrent bacterial infections including Staphylococcus aureus, Streptococcus milleri and GrpA Streptococci, but not fungal infections and an impaired acute phase response [44]. So far, only three patients have been reported with high titre neutralizing antibodies to IL-6 and impaired acute phase response. A 56-year-old women and a 67-year-old man from Japan presented with chronic Staphylococcal aureus cellulitis and empyema due to Streptococcus intermedius and Escherichia coli, respectively [45]. A Haitian boy presented at 11 months with recurrent Staphylococcus aureus cellulitis and subcutaneous abscesses [46]. Significantly, the boy's infections resolved despite persistence of the anti-IL-6 autoantibody. High levels of neutralizing autoantibodies have been identified in healthy individuals [47] and, in fact, we are following up a similar healthy control subject in our own laboratory (Doffinger laboratory, unpublished). This may suggest, that second ‘hits’ are needed for disease development. Unpublished findings from our and other laboratories suggest that this may be an underdiagnosed condition.
DETECTION AND FUNCTIONAL EVALUATION OF ANTICYTOKINE AUTOANTIBODIES
Anti cytokine autoantibodies may be highly diagnostic in the correct clinical context. Early detection of serum anticytokine antibodies is of high importance to initiate early and appropriate treatment as patient are more likely to be refractory to standard antimicrobial therapy, would need longer treatment and have a higher risk to relapse [8▪▪,9,48,49▪]. They should be considered in particular in otherwise unexplained mostly late onset cases of unusual infection.
Various methods have been used for screening including ELISA, chip-based techniques, protein arrays and fluid phase assays [50,51]. The most widely used screening tool is probably multiplexed Luminex-based assays, which are in particular useful to describe the complex anticytokine patterns found for example in APS1 and thymoma patients (e.g. [52]). The most used functional tests for ascertainment of neutralizing activities of ACAA include cellular cytokine release tests and STAT phosphorylation assays (e.g. [12,27▪,49▪]).
Several recent reports noted indeterminate or invalid results when using standard clinical IFN-γ release testing such as Quantiferon or Elispot assays showing negative mitogen responses in patients with high titre AIGA in the context of disseminated NTM infection, probably mostly reflecting interference as the patients AIGA would mask any induced IFN-γ (e.g. [8▪▪,12]). Recent studies evaluated and showed an excellent usefulness of the mitogen component of the whole blood Quantiferon in-tube assays for the detection of clinical relevant AIGA [53▪,54▪]. The limitation of this test is that it formally does not measure the neutralizing capacity of the AIGA. However in addition, we would propose to take further advantage of the widely available Quantiferon assay: Addition of IFN gamma to the tuberculosis tube, if necessary in the presence or absence of a suitable costimulus such as lipopolysaccharide, should theoretically induce the production of TNF-α and IL12, which would be suppressed in the presence of nAIGA. Rattanathammethee et al.[55▪] propose a simple easy to perform dot-ELISA assay which, although based on qualitative visual evaluation, shows excellent positive and negative predictive values. This test should be economical and could be performed even in remote places with limited testing capabilities. More bespoke functional in vitro Whole Blood assays, if available, have the advantage to be able not only to indicate the presence of nAIGA but also to reveal other impairments for example causing IFN-γ production defects [49▪].
CONCLUSION
Autoantibodies to cytokines may cause acquired susceptibility to infection. They are likely to be underdiagnosed and should be considered in otherwise immunocompetent individuals who experience infections with opportunistic organisms and/or a patient with recurrent, chronic or unusual severe infections of more common pathogens
Acknowledgements
Institute of Health Research (NIHR), Cambridge 385 Biomedical Research Centre (R.D.) and from UNAM-DGAPA-PAPIIT program (IN217312 and IN220815) and UNAM-FESC-PIAPI, Project No. 1642 (G.B.-M.).
Financial support and sponsorship
None.
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.Dinarello CA. Historical insights into cytokines. Eur J Immunol 2007; 37 Suppl. 1:S34–S45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Picard C, Bobby Gaspar H, Al-Herz W, et al. International Union of Immunological Societies: 2017 primary immunodeficiency diseases committee report on inborn errors of immunity. J Clin Immunol 2018; 38:96–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Browne SK. Anticytokine autoantibody-associated immunodeficiency. Annu Rev Immunol 2014; 32:635–657. [DOI] [PubMed] [Google Scholar]
- 4.Barcenas-Morales G, Jandus P, Doffinger R. Anticytokine autoantibodies in infection and inflammation: an update. Curr Opin Allergy Clin Immunol 2016; 16:523–529. [DOI] [PubMed] [Google Scholar]
- 5.Bustamante J, Boisson-Dupuis S, Abel L, Casanova JL. Mendelian susceptibility to mycobacterial disease: genetic, immunological, and clinical features of inborn errors of IFN-gamma immunity. Semin Immunol 2014; 26:454–470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Doffinger R, Helbert MR, Barcenas-Morales G, et al. Autoantibodies to interferon-gamma in a patient with selective susceptibility to mycobacterial infection and organ-specific autoimmunity. Clin Infect Dis 2004; 38:e10–e14. [DOI] [PubMed] [Google Scholar]
- 7.Hoflich C, Sabat R, Rosseau S, et al. Naturally occurring anti-IFN-gamma autoantibody and severe infections with Mycobacterium cheloneae and Burkholderia cocovenenans. Blood 2004; 103:673–675. [DOI] [PubMed] [Google Scholar]
- 8▪▪.Hase I, Morimoto K, Sakagami T, et al. Patient ethnicity and causative species determine the manifestations of anti-interferon-gamma autoantibody-associated nontuberculous mycobacterial disease: a review. Diagn Microbiol Infect Dis 2017; 88:308–315. [DOI] [PubMed] [Google Scholar]; A very comprehensive retrospective analysis of studies with AIGA associated NTM infection and highlighting the usefulness of Rituximab.
- 9.Browne SK, Burbelo PD, Chetchotisakd P, et al. Adult-onset immunodeficiency in Thailand and Taiwan. N Engl J Med 2012; 367:725–734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ku CL, Lin CH, Chang SW, et al. Anti-IFN-gamma autoantibodies are strongly associated with HLA-DR∗15:02/16:02 and HLA-DQ∗05:01/05:02 across Southeast Asia. J Allergy Clin Immunol 2016; 137:945–948.e8. [DOI] [PubMed] [Google Scholar]
- 11.Lin CH, Chi CY, Shih HP, et al. Identification of a major epitope by anti-interferon-gamma autoantibodies in patients with mycobacterial disease. Nat Med 2016; 22:994–1001. [DOI] [PubMed] [Google Scholar]
- 12.Ikeda H, Nakamura K, Ikenori M, et al. Severe disseminated Mycobacterium avium infection in a patient with a positive serum autoantibody to interferon-gamma. Intern Med 2016; 55:3053–3058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Koizumi Y, Sakagami T, Minamiguchi H, et al. Chylous ascites, anti-interferon-gamma autoantibody, and angioimmunoblastic T-cell lymphoma: a rare but intriguing connection over Mycobacterium avium. Med Microbiol Immunol 2019; 208:33–37. [DOI] [PubMed] [Google Scholar]
- 14.van de Vosse E, van Wengen A, van der Meide WF, et al. A 38-year-old woman with necrotising cervical lymphadenitis due to Histoplasma capsulatum. Infection 2017; 45:917–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Miyashita K, Matsuura S, Tajima K, et al. Disseminated Mycobacterium avium infection presenting with bladder lesions in a patient with interferon-gamma-neutralizing autoantibodies. Intern Med 2018; 57:3041–3045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Saba M, Greene JN. Refractory Mycobacterium avium complex pneumonia and anti-interferon-g autoantibodies – a case report. Infect Dis Clin Pract 2019; 27:110–113. [Google Scholar]
- 17▪.Koizumi Y, Sakagami T, Nishiyama N, et al. Rituximab restores IFN-gamma-STAT1 function and ameliorates disseminated Mycobacterium avium infection in a patient with anti-interferon-gamma autoantibody. J Clin Immunol 2017; 37:644–649. [DOI] [PubMed] [Google Scholar]; Interesting case report showing the efficacy of Rituximab by functional testing.
- 18▪▪.Aoki A, Sakagami T, Yoshizawa K, et al. Clinical significance of interferon-gamma neutralizing autoantibodies against disseminated nontuberculous mycobacterial disease. Clin Infect Dis 2018; 66:1239–1245. [DOI] [PubMed] [Google Scholar]; A comprehensive retrospective study empasizes the importance of long term antibiotic treatment in AIGA associated NTM disease.
- 19.Baerlecken N, Jacobs R, Stoll M, et al. Recurrent, multifocal Mycobacterium avium-intercellulare infection in a patient with interferon-gamma autoantibody. Clin Infect Dis 2009; 49:e76–e78. [DOI] [PubMed] [Google Scholar]
- 20▪.Chetchotisakd P, Anunnatsiri S, Nanagara R, et al. Intravenous cyclophosphamide therapy for anti-IFN-gamma autoantibody-associated Mycobacterium abscessus infection. J Immunol Res 2018; 2018:6473629. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study shows the usefulness of adjunctive treatment with cyclophosphamide in refractory disease.
- 21.Trapnell BC, Nakata K, Bonella F, et al. Pulmonary alveolar proteinosis. Nat Rev Dis Primers 2019; 5:16. [DOI] [PubMed] [Google Scholar]
- 22.Rosen LB, Freeman AF, Yang LM, et al. Anti-GM-CSF autoantibodies in patients with cryptococcal meningitis. J Immunol 2013; 190:3959–3966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rosen LB, Rocha Pereira N, Figueiredo C, et al. Nocardia-induced granulocyte macrophage colony-stimulating factor is neutralized by autoantibodies in disseminated/extrapulmonary nocardiosis. Clin Infect Dis 2015; 60:1017–1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Saijo T, Chen J, Chen SC, et al. Anti-granulocyte-macrophage colony-stimulating factor auto-antibodies bare a risk factor for central nervous system infection by Cryptococcus gatii in otherwise immunocompotent patients. mBio 2014; 5:e00912–e00914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sellers B, Hall P, Cine-Gowdie S, et al. Cryptococcus gattii: an emerging fungal pathogen in the Southeastern United States. Am J Med Sci 2012; 343:510–511. [DOI] [PubMed] [Google Scholar]
- 26.Hagen F, Colom MF, Swinne D, et al. Autochthonous and dormant Cryptococcus gattii infections in Europe. Emerg Infect Dis 2012; 18:1618–1624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27▪.Kuo CY, Wang SY, Shih HP, et al. Disseminated cryptococcosis due to anti-granulocyte-macrophage colony-stimulating factor autoantibodies in the absence of pulmonary alveolar proteinosis. J Clin Immunol 2017; 37:143–152. [DOI] [PubMed] [Google Scholar]; Kuo et al., together with Demir et al., highlight that aGM-CSF antibodies are associated with cryptococcal disease in the absence of signs of pulmonary alveolar proteinosis.
- 28.Crum-Cianflone NF, Lam PV, Ross-Walker S, et al. Autoantibodies to granulocyte-macrophage colony-stimulating factor associated with severe and unusual manifestations of Cryptococcus gattii infections. Open Forum Infect Dis 2017; 4:ofx211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29▪.Demir S, Chebib N, Thivolet-Bejui F, Cottin V. Pulmonary alveolar proteinosis following cryptococcal meningitis: a possible cause? BMJ Case Rep 2018; 2018: doi: 10.1136/bcr-2017-222940. [DOI] [PMC free article] [PubMed] [Google Scholar]; See ref. [27▪].
- 30.Huynh J, Saddi V, Cooper P, et al. Unusual presentation of severe endobronchial obstruction caused by Cryptococcus gattii in a child: case report and literature review severe endobronchial cryptococcosis in a child. J Pediatric Infect Dis Soc 2018; doi: 10.1093/jpids/piy100. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 31▪.Applen Clancey S, Ciccone EJ, Coelho MA, et al. Cryptococcus deuterogattii VGIIa infection associated with travel to the pacific northwest outbreak region in an anti-granulocyte-macrophage colony-stimulating factor autoantibody-positive patient in the United States. MBio 2019; 10: doi: 10.1128/mBio.02733-18. [DOI] [PMC free article] [PubMed] [Google Scholar]; Interesting case report of a patient with cryptococcal meningitis tracing the strain back to an outbreak region to which patient traveled 3 years before.
- 32.Borie R, Debray MP, Laine C, et al. Rituximab therapy in autoimmune pulmonary alveolar proteinosis. Eur Respir J 2009; 33:1503–1506. [DOI] [PubMed] [Google Scholar]
- 33.Li J, Casanova JL, Puel A. Mucocutaneous IL-17 immunity in mice and humans: host defense vs. excessive inflammation. Mucosal Immunol 2018; 11:581–589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Li J, Vinh DC, Casanova JL, Puel A. Inborn errors of immunity underlying fungal diseases in otherwise healthy individuals. Curr Opin Microbiol 2017; 40:46–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cheng M, Anderson MS. Thymic tolerance as a key brake on autoimmunity. Nat Immunol 2018; 19:659–664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Puel A, Doffinger R, Natividad A, et al. Autoantibodies against IL-17A, IL-17F, and IL-22 in patients with chronic mucocutaneous candidiasis and autoimmune polyendocrine syndrome type I. J Exp Med 2010; 207:291–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kisand K, Boe Wolff AS, Podkrajsek KT, et al. Chronic mucocutaneous candidiasis in APECED or thymoma patients correlates with autoimmunity to Th17-associated cytokines. J Exp Med 2010; 207:299–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rosenberg JM, Price JV, Barcenas-Morales G, et al. Protein microarrays identify disease-specific anti-cytokine autoantibody profiles in the landscape of immunodeficiency. J Allergy Clin Immunol 2016; 137:204–213.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39▪▪.Ramakrishnan KA, Rae W, Barcenas-Morales G, et al. Anticytokine autoantibodies in a patient with a heterozygous NFKB2 mutation. J Allergy Clin Immunol 2018; 141:1479–1482.e6. [DOI] [PubMed] [Google Scholar]; Interesting report showing an hitherto unreported association of ACAA.
- 40.Walter JE, Rosen LB, Csomos K, et al. Broad-spectrum antibodies against self-antigens and cytokines in RAG deficiency. J Clin Invest 2015; 125:4135–4148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Burbelo PD, Browne SK, Sampaio EP, et al. Anti-cytokine autoantibodies are associated with opportunistic infection in patients with thymic neoplasia. Blood 2010; 116:4848–4858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hunter CA, Jones SA. IL-6 as a keystone cytokine in health and disease. Nat Immunol 2015; 16:448–457. [DOI] [PubMed] [Google Scholar]
- 43.Bucciol G, Moens L, Bosch B, et al. Lessons learned from the study of human inborn errors of innate immunity. J Allergy Clin Immunol 2019; 143:507–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Schwerd T, Twigg SRF, Aschenbrenner D, et al. A biallelic mutation in IL6ST encoding the GP130 co-receptor causes immunodeficiency and craniosynostosis. J Exp Med 2017; 214:2547–2562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nanki T, Onoue I, Nagasaka K, et al. Suppression of elevations in serum C reactive protein levels by anti-IL-6 autoantibodies in two patients with severe bacterial infections. Ann Rheum Dis 2013; 72:1100–1102. [DOI] [PubMed] [Google Scholar]
- 46.Puel A, Picard C, Lorrot M, et al. Recurrent staphylococcal cellulitis and subcutaneous abscesses in a child with autoantibodies against IL-6. J Immunol 2008; 180:647–654. [DOI] [PubMed] [Google Scholar]
- 47.Watanabe M, Uchida K, Nakagaki K, et al. Anti-cytokine autoantibodies are ubiquitous in healthy individuals. FEBS Lett 2007; 581:2017–2021. [DOI] [PubMed] [Google Scholar]
- 48.Chi CY, Lin CH, Ho MW, et al. Clinical manifestations, course, and outcome of patients with neutralizing anti-interferon-gamma autoantibodies and disseminated nontuberculous mycobacterial infections. Medicine (Baltimore) 2016; 95:e3927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49▪.Valour F, Perpoint T, Senechal A, et al. Interferon-gamma autoantibodies as predisposing factor for nontuberculous mycobacterial infection. Emerg Infect Dis 2016; 22:1124–1126. [DOI] [PMC free article] [PubMed] [Google Scholar]; Interesting case study and review of treatment options which also shows the usefulness of in vitro functional testing.
- 50.Meager A, Wadhwa M. Detection of anti-cytokine antibodies and their clinical relevance. Expert Rev Clin Immunol 2014; 10:1029–1047. [DOI] [PubMed] [Google Scholar]
- 51.Zhong Y, Tang X, Li J, et al. A nanozyme tag enabled chemiluminescence imaging immunoassay for multiplexed cytokine monitoring. Chem Commun (Camb) 2018; 54:13813–13816. [DOI] [PubMed] [Google Scholar]
- 52.von Stemann JH, Rigas AS, Thorner LW, et al. Prevalence and correlation of cytokine-specific autoantibodies with epidemiological factors and C-reactive protein in 8,972 healthy individuals: results from the Danish Blood Donor Study. PLoS One 2017; 12:e0179981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53▪.Suarez I, Lehmann C, Gruell H, et al. Repurposing QuantiFERON for detection of neutralizing interferon-gamma autoantibodies in patients with nontuberculous mycobacterial infections. Clin Infect Dis 2017; 65:518–521. [DOI] [PubMed] [Google Scholar]; Suarez et al. together with Wu et al., show that the widely available QuantiFERON may be used for detection of AIGA.
- 54▪.Wu UI, Chuang YC, Sheng WH, et al. Use of QuantiFERON-TB Gold In-tube assay in screening for neutralizing anti-interferon-gamma autoantibodies in patients with disseminated nontuberculous mycobacterial infection. Clin Microbiol Infect 2018; 24:159–165. [DOI] [PubMed] [Google Scholar]; See ref. [53▪].
- 55▪.Rattanathammethee K, Chawansuntati K, Chaiwarith R, et al. Dot enzyme-linked immunosorbent assay strip as a screening tool for detection of autoantibody to interferon gamma in sera of suspected cases of adult-onset immunodeficiency. J Clin Lab Anal 2018; 32:e22460. [DOI] [PMC free article] [PubMed] [Google Scholar]; Authors present a simple, economical test with excellent positive and negative predictive values, which could be performed in remote places and places with limited testing capabilities.


