Abstract
Purpose:
The prognosis of patients with relapsed/refractory (R/R) acute myeloid leukemia (AML) remains poor and novel therapies are needed. The proteasome pathway represents a potential therapeutic target. A phase 1 trial of the second generation proteasome inhibitor, ixazomib in combination with MEC (mitoxantrone, etoposide, and cytarabine) was conducted in patients with R/R AML.
Experimental Design:
Dose escalation of ixazomib was performed using a standard 3×3 design. Gene expression profiling was performed on pre- and post-treatment bone marrow or blood samples.
Results:
The maximum tolerated dose of ixazomib in combination with MEC was 1.0 mg. The dose limiting toxicity was thrombocytopenia. Despite a poor risk population, the response rate [complete remission (CR)/ CR with incomplete count recovery (CRi)] was encouraging at 53%. Gene expression analysis identified 2 genes, IFI30 (γ-interferon inducible lysosomal thiol reductase) and RORα (retinoic orphan receptor A) which were significantly differentially expressed between responding and resistant patients and could classify CR.
Conclusion/ Discussion:
These results are encouraging but a randomized trial is needed to address whether the addition of ixazomib to MEC improves outcome. Gene expression profiling also helped us identify predictors of response and potentially novel therapeutic targets.
Introduction:
A high percentage of acute myeloid leukemia (AML) patients achieve remission with induction chemotherapy. However, more than half of patients relapse, and the outcomes of patients with relapsed/refractory AML remain poor. Seven drugs have been recently FDA approved for the treatment of AML (midostaurin, enasidenib, ivosidenib, CPX-351, gemtuzumab ozogamicin, glasdegib and venatoclax in combination with low dose chemotherapy). Glasdegib and venatoclax have been FDA approved in the setting of newly diagnosed elderly AML. Of the other agents, other than gemtuzumab ozogamicin, their use is indicated for very specific small subsets of patients (FLT3 mutated, IDH½ mutated, treatment-related AML, AML with myelodysplasia-related changes). This underscores the need for new treatment strategies that induce remission in relapsed/refractory patients and subsequently enable them to proceed to allogeneic hematopoietic stem cell transplant (AHSCT), which ultimately remains the only curative option.
Protein homeostasis is essential for many critical cellular processes including cell cycle progression, signal transduction, and cell death. The high protein synthesis rates and rapid division of cancer cells make them particularly dependent on the ubiquitin proteasome system (UPS) to maintain protein degradation and limit proteotoxicity. Genetic abnormalities such as point mutations, amplifications, deletions and aneuploidy in malignant cells also contribute to aberrant and unbalanced protein production and increases the burden on the UPS [1]. Agents that target elements of the UPS may be effective as AML therapy in patients who have relapsed or are refractory to standard induction regimens [2–5]. Indeed, proteasome inhibitors or a decoy NF-KB oligonucleotide increase chemosensitivity to both anthracyclines and cytarabine [6–7]. A previous study, CALGB (Alliance) 10502, evaluated the addition of the proteasome inhibitor bortezomib to daunorubicin/cytarabine during induction therapy and to intermediate-dose cytarabine for consolidation in patients with previously untreated AML 60–75 years of age [8]. The combination was tolerable and the addition of bortezomib to standard induction chemotherapy resulted in an encouraging remission rate (65%) [8]. An additional study evaluating bortezomib in combination with MEC (mitoxantrone, etoposide, and cytarabine) and midostaurin demonstrated encouraging results in patients with relapsed/ refractory AML (83% overall response rate and 57% CR rate) [4]. To further investigate the safety and benefit of targeting the UPS to augment salvage therapy in the relapsed/ refractory patient population, we conducted a Phase 1 trial in which we combined the second generation proteasome inhibitor ixazomib with a standard AML salvage regimen MEC [9]. Here, we present our results of the maximum tolerated dose, final efficacy results in the expansion cohort, and the association of gene expression profiling with response.
Methods:
Study Design:
Patients were treated at the Cleveland Clinic and University Hospitals of Cleveland from October 2014 to January 2017. Written informed consent was obtained from all patients and the study was conducted in accordance with recognized ethical guidelines (Declaration of Helinski). An IND was approved by the FDA, and the protocol (NCT02070458) was approved by each institutional review board. Patients receive MEC: mitoxantrone (8 mg/m2), etoposide (80 mg/m2), and cytarabine (1000 mg/m2) intravenously on Days 1–6. Ixazomib (Millennium Pharmaceuticals, Inc.; Cambridge, MA) was given orally on Days 1, 4, 8 and 11 and escalated using a standard 3×3 design. Dose levels: 1 (1.0 mg), 2 (2.0 mg), 3 (3.0 mg). An additional 18 patients were to be treated at the maximum tolerated dose to gain a better understanding of preliminary efficacy and to get additional correlative data. One cycle of treatment was administered. Supportive care was performed according to institutional guidelines. Response was assessed by bone marrow aspirate/ biopsy at the time of count recovery or by Day 45 and complete remission (CR) was defined by IWG criteria [10]. Toxicities were graded according to NCI CTCAE version 4.03. Toxicities secondary to neutropenia or sepsis were not considered dose limiting toxicities. Dose limiting toxicities included: (1) ≥ Grade 4 non-hematologic toxicity (NHT) with the exception of nausea, vomiting/ alopecia and drug-related fevers; (2) any ≥ Grade 3 neurologic toxicity; (3) grade 4 platelet or neutrophil count 50 days beyond the start of chemotherapy and not related to leukemia; (4) any Grade 4 NHT > grade 2 by 45 days beyond the start of chemotherapy. Grade 2, 3, and 4 hyperbilirubinemia were redefined as 1.5≤ 10x upper limits of normal (ULN), 10–20x ULN, and > 20 x ULN as in other Phase 1 acute leukemia studies [11].
Patients:
Eligibility: age 18–70 years, relapsed/refractory AML, adequate organ function, peripheral neuropathy < Grade 2, and cardiac ejection fraction ≥ 45%. Relapsed/ refractory AML was defined as: patients not achieving CR with their last therapy or patients who relapsed after achieving previous CR. Any number of relapses were allowed. The bone marrow blast count had to be > 5%.
Correlative studies:
Bone marrow or blood samples (with sufficient blast counts) were stored for gene expression pre- and post-treatment (at the time of response assessment). For gene expression profiling, whole-transcriptome analysis was performed using the TruSeq stranded total RNA library prep kit with Ribo-Zero (Illumina). Sequencing reads generated from the Illumina platform were assessed for quality using FastQC. The reads were trimmed for adapter sequences using TrimGalore (https://www.bioinformatics.babraham.ac.uk/projects/trim galore/). Reads that passed quality control were then aligned to the human genome (GRCh38) using STAR aligner [12]. The alignment for the sequences were guided using the GENCODE gene annotation for GRChg38. The aligned STAR results were analyzed for differential expression using cufflinks, a RNASeq analysis package which reports the fragments per kilobase of exon per million fragments mapped (FPKM) for each gene [13]. Differential genes were identified using a significance cutoff of false discovery rate (FDR) < 0.05. These genes were then subjected to gene set enrichment analysis to determine any relevant pathways that may be differentially over represented for the conditions tested using GenePattern (Broad Institute).
Statistical methods:
Overall and relapse-free survival were estimated using Kaplan-Meier method. Overall survival started from registration date, and relapse-free survival started from transplant date.
Results:
Baseline characteristics:
Thirty patients were enrolled on this study: 27 treated at dose level 1 and 3 treated at dose Level 2. Patient characteristics are shown in Table 1. The median age of enrolled subjects was 58 years (range 31–70), 16 patients (53%) were male, and the median baseline white blood count at registration was 1.79 K/uL (range 0.1–35.6). The median time from initial diagnosis to registration was 7.6 months and 8 patients (27%) had a history of an antecedent hematologic disorder. Fourteen patients were in first relapse and 13 patients were refractory to their last treatment. Two patients had received a prior allogeneic hematopoietic stem cell transplant, 7 had FLT3 ITD mutations, and 7/29 patients (24%) had adverse cytogenetics per CALGB 8461 criteria [14].
Table 1.
Patient Characteristics 30 patients: 27 patients (Dose Level 1); 3 patients (Dose Level 2). n=number of patients.
| Age (median) | 58 years (range 31–70) | |
| Gender | 13 (53% male) | |
| Baseline white blood count (median) | 1.79 K/ uL (range 0.1–35.55) | |
| Time from diagnosis to registration (median) | 7.6 months | |
| History of antecedent hematologic disorder (n, %) | 8 (27%) | |
| Relapse status (n, %) | ||
| Prior allogeneic HSCT (n) | 2 | |
| FLT3 ITD mutations (n) | 7 | |
| Adverse cytogenetics (CALGB 8461 criteria) (n, %) | 7 (24%) |
Adverse events:
Grade 3–5 non-hematologic toxicities are summarized in Table 2. The most common Grade 3–5 non-hematologic toxicities occurring in ≥ 15% of patients included: infection (74%), febrile neutropenia (85%), hypotension (18%), hypoxia (19%), and mucositis. In terms of gastrointestinal and neurologic side effects related to ixazomib, the following were noted: constipation (7% Grade 1/ 2 at Dose Level 1, 33% Grade 1/ 2 at Dose Level 2); other gastrointestinal symptoms (4% Grade 1/ 2 at Dose Level 1, 0% at Dose Level 2); neurologic symptoms (7% Grade 1/ 2 at Dose Level 1, 3% Grade 3 at Dose Level 1, 0% at Dose Level 2). Only 2 patients had 1 dose of ixazomib held due to: increased bilirubin and diarrhea, respectively.
Table 2.
Grade 3–5 Non-hematologic toxicities occurring in ≥ 15% of patients
| Toxicity | Incidence |
|---|---|
| Infection | 74% |
| Febrile neutropenia | 85% |
| Hypotension | 18% |
| Hypoxia | 19% |
| Mucositis | 15% |
| Hypokalemia | 33% |
| Hypoalbuminemia | 30% |
Dose determination:
At dose level 1, one dose limiting toxicity occurred (grade 4 thrombocytopenia), so this dose level was initially expanded to 6 patients. At dose level 2, two patients developed grade 4 thrombocytopenia 50 days beyond the start of chemotherapy (unrelated to leukemia). Therefore, the maximum tolerated dose of ixazomib was 1.0 mg. Of the patients developing a dose limiting toxicity, 1 patient had a history of an antecedent hematologic disorder. Of the other 2 patients, 1 had mutations in ASXL1, SRSF2, IDH2, and STAG2. The other patient had mutations in FLT3 ITD, TET2, NPM1, and DNMT3. Some of these mutations could be consistent with an antecedent MDS and could explain the prolonged thrombocytopenia.
Outcomes:
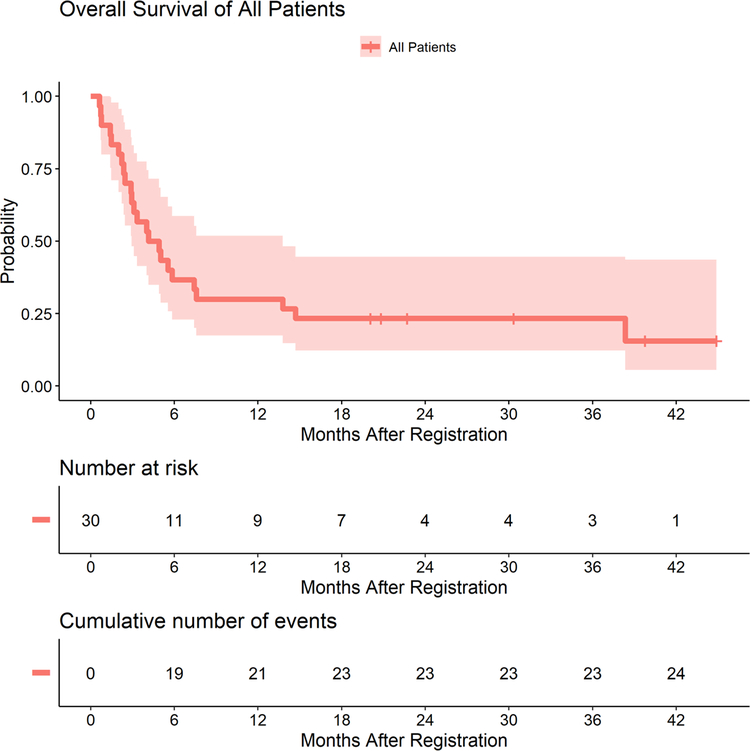
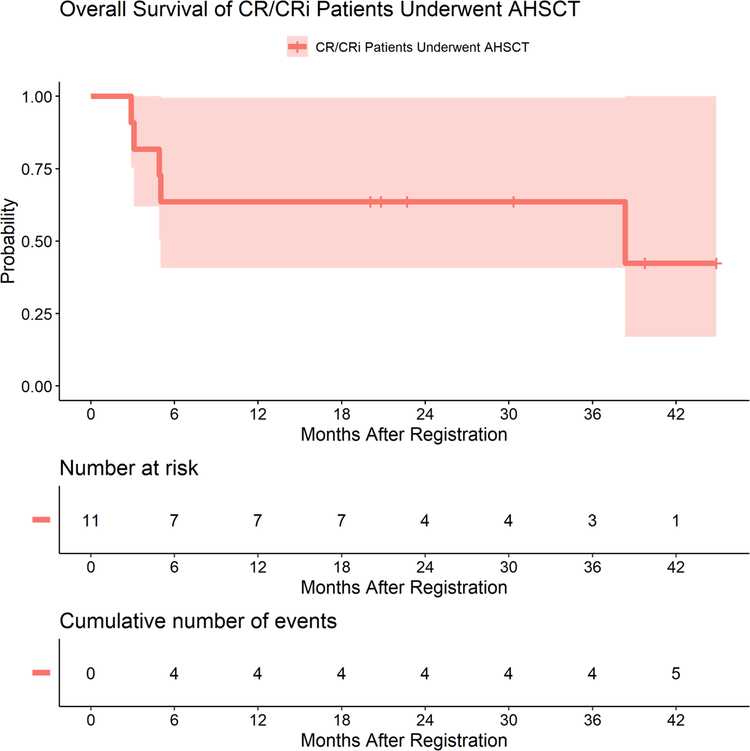
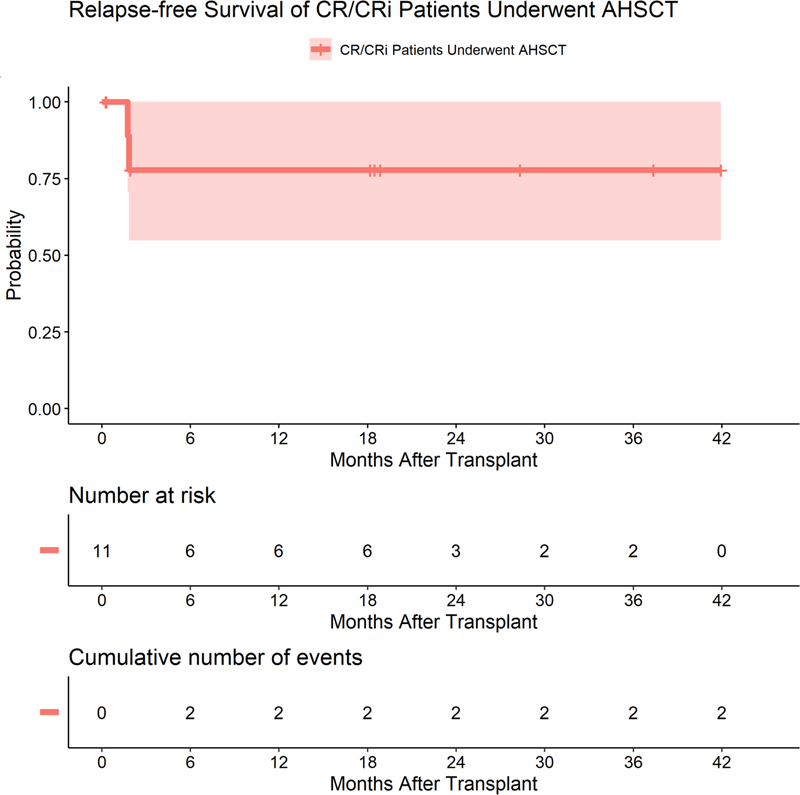
The overall response rate was 53% [CR/CR with incomplete count recovery (CRi)] [11 CRs/5 CRis] with a 10% early mortality rate (within 30 days of initiating treatment). The median overall survival for all patients was 4.5 months (95% CI 2.9–13.8 months) with a median follow-up of 26.5 months (range 20.0–44.9 months) for surviving patients (Figure 1A). One-year overall survival rate was 30.0% (95% CI: 17.4–51.8%). The median overall survival for patients achieving CR/ CRi was longer with a median overall survival of 11.1 months (95% CI: 4.9-NA months) and 1-year overall survival of 50.0% (95% CI: 30.6–81.6%). Thirteen patients (43%) proceeded to AHSCT and 1 patient received a donor lymphocyte infusion. The Kaplan-Meier estimated overall survival of patients who achieved CR/CRi and proceeded to AHSCT is shown in Figure 1B. The median overall survival was 38.3 months (95% CI: 5.0-NA months) and 1-year overall survival rate was 63.6% (95% CI: 40.7–99.5%) with a median follow-up time of 26.5 months. The median relapse-free survival of patients who achieved CR/ CRi and proceeded to AHSCT is shown in Figure 1C. The median relapse-free survival was not reached and 1-year relapse-free survival was 77.8% (95% CI: 54.9–100%). The median age was similar in those patients achieving a CR/ CRi versus those who did not. Both patients who had received a prior allogeneic hematopoietic stem cell transplant achieved a CR/ CRi. However, patients refractory to MEC/ ixazomib had a higher white blood count prior to trial therapy (7.7 K/ uL, compared to 1.79 K/ uL), had a higher incidence of FLT3 mutations (40% versus 19%), were more likely to have a prior antecedent hematologic disorder (45% versus 6%), were more likely to be refractory to their last therapy (55% versus 31%), were less likely to be in first relapse (27% versus 63%), and had a shorter median time from diagnosis to trial registration (median 89 days versus 314 days).
Figure 1A. Overall survival for all patients.
The solid line is the Kaplan-Meier estimated overall survival curve. The shaded area is the 95% confidence band.
Kaplan-Meier (KM) estimated overall survival (OS) of all patients. Solid line is the KM estimated OS curve, and shaded area is the 95% confidence band. Twenty-four patients died out of a total of 30 patients.
Median F/U time of patients alive was 26.5 months (range: 20.0–44.9 months). Median OS was 4.5 months (95% CI: 2.9–13.8 months). One-year OS rate was 30.0% (95% CI: 17.4–51.8%).
Figure 1B. Overall survival of CR/CRi patients who underwent AHSCT.
The solid line is the Kaplan-Meier estimated overall survival curve. The shaded area is the 95% confidence band.
Kaplan-Meier estimated overall survival (OS) of patients who achieved CR/CRi and proceeded to transplant. Solid line is the KM estimated OS curve, shaded area is the 95% confidence band. Five patients died out of a total of 11 patients. Median OS was 38.3 months (95% CI: 5.0-NA months). One-year OS rate was 63.6% (95% CI: 40.7–99.5%)
Median F/U time of the 6 patients alive was 26.5 months (range: 20.0–44.9 months).
Figure 1C. Relapse-free survival of CR/CRi patients who underwent AHSCT.
The solid line is the Kaplan-Meier estimated relapse-free survival curve. The shaded area is the 95% confidence band.
Kaplan-Meier estimated relapse-free survival (RFS) of patients who achieved CR/CRi and proceeded to transplant. Patients died without relapse was censored at death date. Solid line is the KM estimated RFS curve, shaded area is the 95% confidence band. Out of total 11 patients, only 2 relapsed after transplantation. Median RFS was not reached. One-year RFS rate was 77.8% (95% CI: 54.9–100%).
Correlative science:
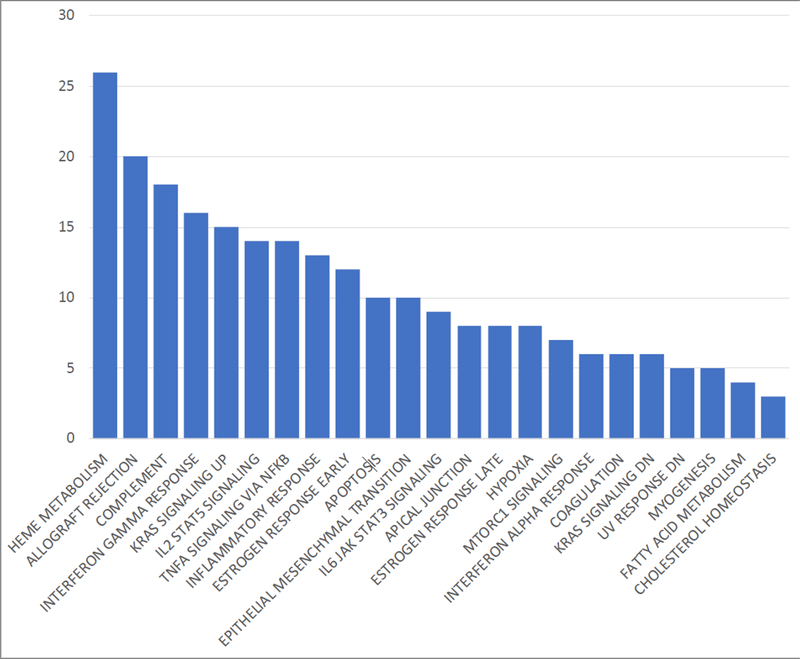
The number of mutations in DNTMT3A, TP53, ASXL1, and NRAS (0, 1, >1) has been previously shown to be associated with a worse response to salvage therapy [15]. Ten of 21 patients with available data had at least 1 of these mutations (Table 3) and 8/10 achieved CR/ CRi. Table 4 is a table of the various mutations and response rates for each molecular subset. To identify a signature predictive of response to treatment, we performed RNASeq analysis on 17 patients pre-treatment and 11 patients post-treatment. Nine patients had samples at both time points. Only 17/ 30 patients had pre-treatment samples because the remainder did not consent to the correlative part of the trial. The majority of these patients had undergone bone marrow exams prior to consenting for the trial. Only 9/ 30 patients had both time points since only 17/30 patients had pre-treatment samples and of these 17 patients, 8 patients either progressed, died, or did not have samples drawn at the appropriate time points. Of the 17 patients with pre-treatment samples, 11 patients achieved CR/ CRi, 4 patients were refractory, and 2 patients were not evaluable for response (they died during induction therapy). Genes were differentially expressed between resistant and responding patients in: 314 genes (pre-treatment), 217 genes (after-treatment), and 72 genes (at both time points). Gene set enrichment analysis was conducted by comparing genes at baseline in responding versus resistant patients in pre-treatment samples and identified significantly differentially expressed genes (Figure 2) clustering in heme-metabolism and erythroblast differentiation, inflammatory response (interferon -γ and α, TNFα), cytokine/ STAT signaling (IL2/STAT5 and IL6/JAK/STAT3), NF-KB, and hypoxia. Using logistic regression and linear discriminant analysis, we identified 2 genes [IFI30 (γ-interferon-inducible lysosomal thiol reductase, GILT)] and [RORα (retinoic acid-related orphan receptor A)] which were significantly different between responding and resistant patients and could classify CR if: 0.2012*RORα- 0.0215*IFI30 was > 0.1.
Table 3.
Mutations present on myeloid mutation panel next generation sequencing (n=21 patients)
| Mutations | Number of patients with mutations |
|---|---|
| FLT3 ITD | 5 |
| TET2 | 2 |
| JAK3 | 1 |
| ASXL1 | 4 |
| LUC7 | 2 |
| TP53 | 2 |
| SRSF2 | 2 |
| IDH2 | 2 |
| STAG2 | 2 |
| NPM1 | 5 |
| DNMT3 | 6 |
| WT1 | 2 |
| SMC1a | 2 |
| BCOR | 2 |
| STAT3 | 2 |
| NRAS | 3 |
| NSD1 | 1 |
| CBL | 1 |
| EZH2 | 1 |
| IDH1 | 2 |
| RUNX1 | 2 |
| RAD21 | 1 |
Table 4.
Response rates by molecular subgroup
| Molecular Mutations | Number of responding patients with mutation/ number of total patients with mutations (%) |
|---|---|
| FLT3 ITD | 4/7 (57%) |
| TET2 | 2/2 (100%) |
| JAK3 | 1/1 (100%) |
| ASXL1 | 3/3 (100%) |
| LUC7 | 1/ 2 (50%) |
| TP53 | 1/ 2 (50%) |
| CKIT | 0/1 (0%) |
| SRSF2 | 2/2 (100%) |
| IDH2 | 1/1 (100%) |
| STAG2 | 1/1 (100%) |
| NPM1 | 1/ 4 (25%) |
| DNMT3 | 3/3 (100%) |
| WT1 | 0/1 (0%) |
| SMC1a | 0/1 (0%) |
| BCORL1 | 0/ 1 (0%) |
| IDH1 | 2/2 (100%) |
| STAT3 | 1/1 (100%) |
Figure 2. Enriched gene sets (FDR<0.05) in hallmark pathways curated in the MSigDB (Broad Institute).
Graph indicates the number of genes in the set that were significantly differentially expressed between responders and resistant patients at baseline (pre-treatment).
Discussion:
Relapsed/ refractory AML in a transplant-eligible patient should be treated aggressively to maximize the chance of a patient achieving remission and proceeding to AHSCT. Our phase 1 study demonstrates that the combination of MEC and ixazomib (1.0 mg) has a favorable safety profile and is associated with significant efficacy in patients with relapsed/refractory AML. This would be the dose going forward in future studies. Although the dose of ixazomib is lower, ixazomib is likely acting through 2 mechanisms: (1) through increasing chemosensitivity to chemotherapy; (2) through inhibition of proteasomes within the AML cell; and it is not clear that a higher dose is needed in combination with intensive chemotherapy. Notably, the addition of ixazomib at a dose of 1.0 mg did not appear to increase the toxicity of the MEC regimen as the observed toxicities were consistent with characteristics for administration of MEC alone [9]. It is also important to note that the response rates we observed in this study were higher than what we would expect with MEC (CR rates of 24–25%) or other salvage therapies (CR rates of 18–41% when the patient is 6–12 months out of induction CR) [16]. This is particularly true given the poor risk population that we enrolled on this study. Although the CR rates quoted above are lower than those noted in other references, where rates may be as high as 65% [17], these latter rates tend to be in more favorable risk groups. We consider our population “poor risk” based on the European prognostic scoring system [17] and based on the number of molecular mutations in DNMT3, TP53, ASXL1, and NRAS [15]. With respect to molecular mutations, the number of mutations in the genes listed above has been associated with a worse response to salvage therapy [15]. Ten of 21 patients with available data had at least 1 of these mutations. Based on the scoring system, mutation in 1 of these genes had an equivalent prognostic impact to poor risk cytogenetics and greater than 1 mutation had an even worse prognostic impact than poor risk cytogenetics. Based on the European prognostic scoring system and using the median values for our patients, most patients would be considered poor risk (score =10): CR1 duration 7–18 months (3 points), other cytogenetics (5 points), > 45 years (2 points). In addition, 43% of our patients had been refractory to their last therapy.
To date, new agents have demonstrated limited activity in the relapsed/refractory setting unless they are specifically targeted to specific mutations (IDH1, IDH2, and FLT3) [18–20]. Although the BCL-2 and hedgehog pathways appear to be promising targets in AML, the hedgehog inhibitor, glasdegib, and BCL-2 inhibitor, venatoclax, have demonstrated the most activity and been FDA approved with low dose chemotherapy in the upfront setting in elderly patients with newly diagnosed AML. Venatoclax appears to have limited activity as a single agent with much of this thought to be related to increased association of bim with the prosurvival protein MCL-1. Preclinical studies have demonstrated combined MCL-1 and BCL-2 inhibition, appear to be promising in the relapsed/ refractory setting [21] and clinical trials are just starting to address this question. The results of our trial indicates that thoughtfully repositioning existing agents as part of a novel regimen may ultimately represent a more effective strategy for the salvage therapy of patients with poor risk features whose disease is unlikely to be driven by the specific mutations that are actionable with recently approved drugs. The mechanism of ixazomib action in AML is not totally clear and further correlatives studies will be needed to evaluate this. Pre-clinical studies to date with ixazomib have demonstrated upregulation of MCL-1 in hepatocellular cancer cells and suggests that combined MCL-1 inhibition may have benefit [22].
In addition, the correlative studies we conducted as part of this trial suggests that transcriptome profiling may help us predict which patients respond to and/or are resistant to treatment upfront. If this is validated, we could potentially increase the response rate to this regimen even further by “pre-selecting” patients who are most likely to benefit based on specific gene expression features. Although various pathways were noted to be differentially expressed in responders and non-responders, the genes IFI30 and RORα clearly were predictive of response. This would not have been predicted a priori. IFI30 was identified in 2000 by Phan et al and there is relatively little literature on this gamma-interferon-inducible lysosomal thiol reductase [23]. However, the protein is constitutively expressed in antigen-presenting cells and catalyzes disulfide bond reduction both in vitro and in vivo [23]. Therefore, one hypothesis is that higher levels of IFI30 may increase the levels of anti-oxidants and lead to a decreased endoplasmic-reticulum stress response to therapy. IFI30 is expressed at increased levels in various other cancers including breast cancer and melanoma and polymorphisms in IFI30 have been linked to disease progression in prostate cancer [24–26]. The second gene we identified as predictive of response, RORα, is involved in the inhibition of cellular proliferation and acts as a potent tumor suppressor gene [27]. The retinoic acid related orphan receptor genes have demonstrated critical roles in tumorigenesis [27]. Increased levels of RORα in this trial were associated with improved response. This is consistent with data from other malignancies where decreased expression of RORα has been associated with melanoma progression as well as poor outcome in other tumors [28–29]. RORalpha has been identified as a potential therapeutic target for breast cancer and has been investigated in melanoma, colorectal cancer, and gastric cancer [27]. Because IFI30 and RORalpha appear to be potentially independent of the proteasome pathway and to be prognostic in other tumors, it is possible they may be important prognostically in response to other salvage therapies in relapsed/ refractory AML. Further studies are required to determine whether these 2 genes are predictive of response to the specific regimen we tested here or whether they may also predict a favorable response for patients with relapsed/refractory AML who are treated with other salvage regimens.
In summary, our study demonstrates that the regimen of MEC and ixazomib was well tolerated and associated with a clinical response rate that was higher than expected in the context of salvage therapy for relapsed/refractory patients with poor risk disease features. We are currently planning a larger randomized phase 2 trial to further investigate the benefit of adding ixazomib to MEC as well as the potential value of baseline transcriptome profiling as a predictive tool for the precision selection of patients most likely to benefit from this regimen and other therapies used in the salvage setting.
Contributors: This trial was developed by the principal investigator (AA) in collaboration with translational investigators (AM, JP, and JC). All data have been reviewed by AA and PE. RC reviewed the translational data. Statistical analyses were performed by PE and WW. Data were collected by all authors. The manuscript drafts were written by AA, PE, JC, RC, and MS. All authors approved the final version of the manuscript.
Statement of Significance.
The response rate with the regimen of MEC plus ixazomib was encouraging in a poor risk population of relapsed/ refractory AML patients. High ROR alpha expression was associated with an increased response to therapy in this trial and suggests that modulation of RORalpha may represent a promising therapeutic target in AML.
Acknowledgement:
This trial was funded by Takeda/ Millennium and ixazomib was also provided by Takeda/ Millennium for this trial. The Case Comprehensive Cancer also provided partial support for correlative studies through an EPCRS grant, the Translational Research Shared Resource of the Case Comprehensive Cancer Center (P30 CA043703), and the Genomics Core Facility of the CWRU School of Medicine’s Genetics and Genome Sciences Department. We thank all patients for their willingness to participate in this trial. In addition, we thank our protocol and data coordinators (Jaime Fensterl, Allison Unger, Christopher Goebel); research nurses (Mary Lynn Rush, Samjhana Bogati, Eric Parsons, Rachael Diligente, Donna Kane); and laboratory/ translational personnel (Nita Hoxha, Alek Nielsen, Cassandra Hirsch, and Simone Edelheit) for their enormous contributions to this trial.
Footnotes
Competing interests’ statement: Anjali Advani received research funding from Takeda/ Millennium to conduct this trial. Jennifer Carew receives research funding from Takeda/ Millennium. Ixazomib was provided by Takeda/ Millennium for this trial. The Case Comprehensive Cancer also provided partial support for correlative studies through an EPCRS grant, the Translational Research Shared Resource of the Case Comprehensive Cancer Center (P30 CA043703), and the Genomics Core Facility of the CWRU School of Medicine’s Genetics and Genome Sciences Department.
References:
- 1.Deshaies RJ. Proteotoxic crisis, the ubiquitin-proteasome system, and cancer therapy. BMC Biol 2014; 12: 94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nawrocki ST, Kelly RR, Smith PG, Keaton M, Carraway H, Sekeres MA, et al. The NEDD8-activating enzyme inhibitor MLN4924 disrupts nucleotide metabolism and augments the activity of cytarabine. Clin Cancer Res 2015; 21: 439–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Swords RT, Erba HP, DeAngelo DJ, Bixby DL, Altman JK, Maris M, et al. Pevonedistat (MLN4924), a first-in-class NEDD8-activating enzyme inhibitor, in patients with acute myeloid leukaemia and myelodysplastic syndromes: a phase 1 study. Br J Haematol 2015; 169: 534–43. [DOI] [PubMed] [Google Scholar]
- 4.Walker AR, Wang H, Walsh K, Bhatnagar B, Vasu S, Garzon R, et al. Midostaurin, bortezomib, and MEC in relapsed/ refractory acute myeloid leukemia. Leuk Lymphoma 2016; 57: 2100–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Csizmar CM, Kim DH, Sachs Z. The role of the proteasome in AML. Blood Cancer J 2016; 6: e503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Griffin JD. Leukemia cells and constitutive activation of NF-KB. Blood 2001; 98: 2291. [DOI] [PubMed] [Google Scholar]
- 7.Adams J Proteasome inhibition in cancer: development of PS-341. Semin Oncol 2001; 28: 613–19. [DOI] [PubMed] [Google Scholar]
- 8.Attar EC, Johnson JL, Amrein PC, Lozanski G, Wadleigh M, DeAngelo DJ, et al. Bortezomib added to daunorubicin and cytarabine during induction therapy and to intermediate-dose cytarabine for consolidation in patients with previously untreated acute myeloid leukemia age 60–75 years: CALGB (Alliance) study 10502. J Clin Oncol 2013; 31(7): 923–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Amadori S, Arcese W, Iscacchi G, Meloni G, Petti MC, Monarca B, et al. Mitoxantrone, etoposide, and intermediate-dose cytarabine: an effective and tolerable regimen for the treatment of refractory acute myeloid leukemia. J Clin Oncol 1991; 9(7): 1210–14. [DOI] [PubMed] [Google Scholar]
- 10.Cheson BD, Bennett JM, Kopecky KJ, Buchner T, Willman CL, Estey EH, et al. Revised recommendations of the international working group for diagnosis, standardization of response criteria, treatment outcomes, and reporting standardization for therapeutic trials in acute myeloid leukemia. J Clin Oncol 2003; 21: 4642–49. [DOI] [PubMed] [Google Scholar]
- 11.Attar EC, DeAngelo DJ, Supko JG, D’Amato F, Zahrieh D, Sirulnik A, et al. Phase 1 and pharmacokinetic study of bortezomib in combination with idarubicin and cytarabine in patients with acute myelogenous leukemia. Clin Cancer Res 2008; 14(5): 1446–54. [DOI] [PubMed] [Google Scholar]
- 12.Dobin A, Davis CA, Schlesinger F, Drenkow J, Zaleski C, Jha S, et al. STAR: ultrafast universal RNA-seq aligner. Bioinformatics 2013; 29(1): 15–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Trapnell C, Williams BA, Pertea G, Mortazavi A, Kwan G, van Baren MJ, et al. Transcript assembly and quantification by RNA-Seq reveals unannotated transcripts and isoform switching during cell differentiation. Nat Biotechnol 2010; 28(5): 511–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Byrd JC, Mrozek K, Dodge RK, Carroll AJ, Edwards CG, Arthur DC, et al. Pretreatment cytogenetic abnormalities are predictive of induction success, cumulative incidence of relapse, and overall survival in adult patients with de novo acute myeloid leukemia: results from Cancer and Leukemia Group B (CALGB 8461).Group B (CALGB 8461). Blood 2002; 100(13): 4325–36. [DOI] [PubMed] [Google Scholar]
- 15.Advani AS, Elson P, Visconte V, Carew J, Fensterl J, Przychodzen B, et al. Prognostic impact of molecular mutations in AML at first relapse. Blood 2015: 126: 3825. [Google Scholar]
- 16.Price SL, Lancet JE, George TJ, Wetzstein GA, List AF, Ho VQ, et al. Salvage chemotherapy regimens for acute myeloid leukemia. Is one better? Efficacy comparison between CLAG and MEC regimens. Leuk Res 2011; 35(3): 301–4. [DOI] [PubMed] [Google Scholar]
- 17.Thol F, Schlenk RF, Heuser M, Ganser A. How I treat refractory and early relapsed acute myeloid leukemia. Blood 2015; 126(3): 319–27. [DOI] [PubMed] [Google Scholar]
- 18.DiNardo CD, Stein EM, de Botton S, Roboz GJ, Altman JK, Mims AS, et al. Durable remissions with ivosidenib in IDH1-mutated relapsed or refractory AML. N Engl J Med 2018; 378(25): 2386–98. [DOI] [PubMed] [Google Scholar]
- 19.Stein EM, DiNardo CD, Pollyea DA, Fathi AT, Roboz GJ, Altman JK, et al. Enasidenib in mutant IDH2 relapsed or refractory acute myeloid leukemia. Blood 2017; 130(6):722–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stone RM, Mandrekar SJ, Sanford BL, Laumann K, Geyer S, Bloomfield CD, et al. Midostaurin plus chemotherapy for acute myeloid leukemia with a FLT3 mutation. N Engl J Med 2017; 377(5): 454–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Luedtke DA, Niu X, Pan Y, Zhao J, Liu S, Edwards H, et al. Inhibition of Mcl-1 enhances cell death induced by the Bcl-2 selective inhibitor ABT-199 in acute myeloid leukemia cells. Signal Transduct Targ Ther 2017; 2: 17012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Augello G, Modica M, Azzolina A, Puleio R, Cassata G, Emma MR, et al. Preclinical evaluation of antitumor activity of the proteasome inhibitor MLN2238 (ixazomib) in hepatocellular carcinoma cells. Cell Death Dis 2018; 9(2): 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Phan UT, Arunachalam B, Cresswell P. Gamma-interferon-inducible lysosomal thiol reductase (GILT). Maturation, activity and mechanism of action. J Biol Chem 2000; 275(34): 25907–14. [DOI] [PubMed] [Google Scholar]
- 24.Xiang YJ, Guo MM. Zhou CJ, Liu L, Han B, Kong LY, et al. Absence of gamma-interferon-inducible lyosomal thiol reductase (GILT) is associated with poor disease-free survival in breast cancer patients. PLoS One 2014; 9(10): e109449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nguygen J, Bernert R, In K, Kang P, Sebastiao N, Hu C, et al. Gamma-interferon-inducible lysosomal thiol reductase is upregulated in human melanoma. Melanoma Research 2016; 26(2): 125–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bao BY, Pao JB, Huang CN, Pu YS, Chang TY, Lan YH, et al. Polymorphisms inside microRNAs and microRNA target sites predict outcomes in prostate cancer patients receiving androgen-deprivation therapy. Clin Canc Res 2011; 17(4): 928–36. [DOI] [PubMed] [Google Scholar]
- 27.Fan J, Ly Z, Yang G, Liao TT, Xu J, Wu F, et al. Retinoic acid receptor-related orphan receptors: critical roles in tumorigenesis. Front Immunol 2018; 9:1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brozyna AA, Jozwicki W, Roszkowski K, Filipiak J, Slominski AT. Melanin content in melanoma metastases affects the outcome of radiotherapy. Oncotarget 2016; 27(14):17844– [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Slominski AT, Brozyna AA, Skobowiat C, Zmijewski MA, Kim TK, Janjetovic Z, et al. On the role of classical and novel forms of vitamin D in melanoma progression and management. J Steroid Biochem Mol Biol 2018; 177:159–70. [DOI] [PMC free article] [PubMed] [Google Scholar]