Abstract
Background:
Genicular nerve radiofrequency ablation (GNRFA), including conventional, cooled, and pulsed techniques, has been used in the management of symptomatic knee osteoarthritis (OA). This new and innovative treatment option has the capacity to decrease pain and improve function and quality of life in certain patients. GNRFA is reserved for patients with symptomatic knee OA who have had failure of conservative treatment and have had failure of or are poor candidates for surgery. GNRFA has been shown to consistently provide short-term (3 to 6-month), and sometimes longer, pain relief in patients. GNRFA has been demonstrated to be safe to administer repeatedly in patients who respond well to this minimally invasive procedure.
Description:
GNRFA is a 2-step procedure. First, patients are given a diagnostic block under fluoroscopy or ultrasound guidance. Specifically, 1 mL of lidocaine is injected using a 20-gauge, 3.5-in (8.9-cm) spinal needle around the superior lateral, superior medial, and inferior medial genicular nerve branches. The diagnostic block is extra-articular. If the patient reports a ≥50% reduction in baseline pain for a minimum of 24 hours following the injection, then the patient is a candidate for genicular ablation. The osseous landmarks for the diagnostic block are exactly the same as for the ablation procedure. Both procedures are well tolerated in the office setting under local skin anesthesia or can be done in the operating room under conscious sedation using a low-dose sedative such as midazolam for anxious patients. General anesthesia is not required for GNRFA. This procedure is most commonly performed by interventional pain specialists but may also be performed by any physician with appropriate training. In some jurisdictions, physician assistants and nurse practitioners may perform this procedure subject to their supervision requirements.
Alternatives:
Conservative treatment for symptomatic knee OA includes weight loss management, physical and aquatic therapy, bracing, lateral wedge insoles, transcutaneous nerve stimulation, nonsteroidal anti-inflammatory drugs in combination with a proton pump inhibitor, autologous blood-based therapies, and cortisone and hyaluronic acid injections1,2. Surgical treatment for symptomatic knee OA includes knee arthroscopy, high tibial osteotomy, total knee replacement, and unicompartmental knee replacement in patients without lateral compartment disease2. It should be noted that there is some evidence suggesting that steroid injection, viscosupplements, and arthroscopy are not effective for the management of knee OA.
Rationale:
Thermal GNRFA differs from all other treatment alternatives because this procedure causes denaturing of the 3 sensory nerves primarily responsible for transmitting knee pain from an arthritic joint to the central nervous system. In this procedure, heating occurs from an intense alternating electrical field at the tip of the cannula, which produces sufficient heat to denature the proteins in the target tissue. The accepted heating parameters for this procedure are 70° to 80°C for 60 or 90 seconds. A commonly raised question is whether this procedure precipitates a Charcot-type joint. The Charcot joint involves much more than reduced innervation; it occurs in the context of chronically compromised vascularity and altered soft-tissue characteristics as well as peripheral neuropathy. Moreover, a Charcot-type joint does not develop because the deafferentation of the weight-bearing joint is partial3. To our knowledge, no Charcot-type joints have been reported after this procedure. Conversely, data from an animal study have shown that selective joint denervation may lead to the progression of knee OA4. The ablation procedure is done outside the knee joint, unlike alternatives such as intra-articular therapies and surgery. The effectiveness of nonsurgical knee OA interventions in alleviating pain and improving joint function is generally inadequate1. However, GNRFA appears to be an emerging alternative for patients who have had failure of conservative and surgical treatments. It is not uncommon in our clinical practice for patients to achieve adequate pain control following ablation for up to 1 year. GNRFA provides temporary relief from symptomatic knee OA because it does not eliminate the potential for peripheral nerve regrowth and regeneration, and thus pain, to return.
Introductory Statement
Radiofrequency ablation of the genicular nerves is more effective when performed parallel to the target nerve.
Indications & Contraindications
Indications
Patients with symptomatic knee osteoarthritis (OA) that is recalcitrant to conservative modalities. No specific severity of OA has been established as an indication for the procedure; however, these patients typically have moderate to severe OA (Kellgren-Lawrence grade 3 or 4) for which surgery would be considered or has already been done5.
Patients with a failed knee replacement. These are patients for whom no identifiable cause of the pain at the site of the total knee arthroplasty has been diagnosed.
Patients who are not good surgical candidates because of medical comorbidities and/or a high body mass index (BMI).
Patients who want to avoid surgery.
Patients who have had a previously successful genicular nerve radiofrequency ablation (GNRFA), as this procedure can be repeated to address recurrent symptomatic knee OA.
Contraindications
Pregnancy.
Acute knee injury.
Unstable knee joint.
Chronic pain syndrome.
Psychological overlay.
Uncontrolled diabetes mellitus.
Bleeding disorder. (This diagnosis would be important to discuss during the consent process, but it would not necessarily be a contraindication.)
Presence of an implantable defibrillator.
Presence of a peripheral nerve stimulator.
Presence of a pacemaker.
Current active, or history of, chronic knee infection. (The infection may be an important, treatable cause of the pain.)
Step-by-Step Description of Procedure (Video 1)
Video 1.
The video demonstrates GNRFA in a patient with pain at the site of a total knee arthroplasty who underwent diagnostic and laboratory workup without any etiology identified. The workup did not reveal implant failure, mechanical instability, or infection.
Step 1: Select a Radiofrequency Generator Machine
In this video, we used the Cosman G4 Radiofrequency Generator to perform conventional thermal GNRFA.
Other radiofrequency generator machines that can be used for this procedure include those manufactured by NeuroTherm, Halyard Health, and Stryker.
Step 2: Preparing the Patient
Position and prepare the patient for the ablation procedure.
Place the patient in the supine position. Place a bump behind the knee to allow for 30° of flexion.
Prepare the knee with chloride-based or an iodine-based product and drape the knee in a sterile manner.
Place the ground pad on the contralateral or ipsilateral extremity, which depends on the radiofrequency machine that is used for the procedure. The position is not dependent on the presence of an existing joint implant. Wrinkles in the ground pad can lead to skin burns.
Step 3: Skin Preparation
Provide appropriate skin analgesia prior to ablation.
Use fluoroscopy to identify the 3 entry sites for the planned percutaneous insertion of the cannulas (Figs. 1, 2, and 3) at the base of the medial and lateral femoral condyles and at the base of the medial tibial condyle.
Inject the lidocaine (1% or 2%) to form a skin wheal over the 3 sites where the cannulas are to be inserted.
Fig. 1.
Fluoroscopic anteroposterior image showing planned placement of the cannula directed at the superior lateral genicular nerve.
Fig. 2.
Fluoroscopic anteroposterior image showing planned placement of the cannula directed at the superior medial genicular nerve.
Fig. 3.

Fluoroscopic lateral image showing planned placement of the cannula directed at the inferior medial genicular nerve.
Step 4: Placement of the Radiofrequency Cannulas
Use C-arm fluoroscopy guidance when inserting the cannulas.
Use a fluoroscopic anteroposterior image to target the superior lateral genicular nerve by advancing the 20-gauge, 3.5-in (8.9-cm) cannula with a 10-mm active tip percutaneously down to the junction of the femoral shaft and lateral epicondyle, contacting bone.
Using the fluoroscopic anteroposterior image, target the superior medial genicular nerve. Percutaneously advance a second cannula to the medial aspect of the distal femoral diaphysis approximately 1 cm anterior to the adductor tubercle until the bone is contacted (Figs. 4-A and 4-B).
Using the fluoroscopic anteroposterior view, target the inferior medial genicular nerve and advance a third cannula percutaneously to the proximal tibial diaphysis, along the margin of the medial tibial condyle, until the needle contacts the bone (Fig. 5).
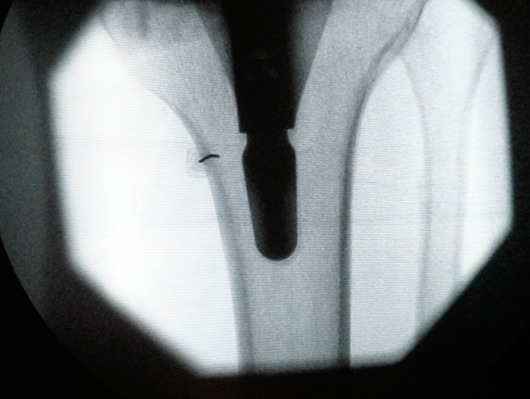
Figs. 4-A and 4-B Fluoroscopic anteroposterior image showing cannula insertion near the superior lateral genicular nerve and superior medial genicular nerve.
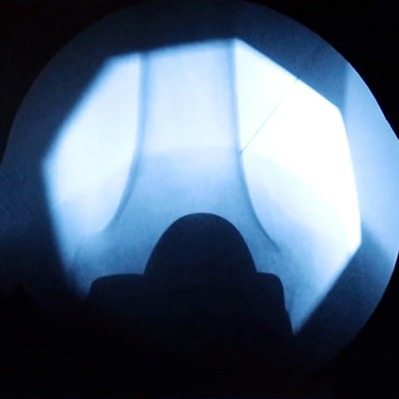
Fig. 4-A.
Initial placement.
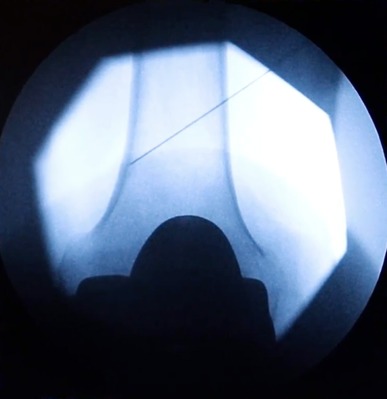
Fig. 4-B.
Final placement after advancement to the bone.
Fig. 5.
Fluoroscopic anteroposterior image showing cannula insertion near the inferior medial genicular nerve.
Step 5: Adjust Radiofrequency Cannula Placement
Make minor adjustments to all 3 cannulas to improve their position, if needed.
Obtain a fluoroscopic true lateral image to confirm cannula placement at the midpoint of the diaphysis in both the tibia and the femur6. If cannula placement is beyond the midpoint of the diaphysis, withdraw each cannula 3 to 5 mm to ensure correct placement (Figs. 6-A and 6-B).
Figs. 6-A and 6-B Fluoroscopic lateral images obtained to confirm cannula placement at the midpoint of the diaphysis of the femur.
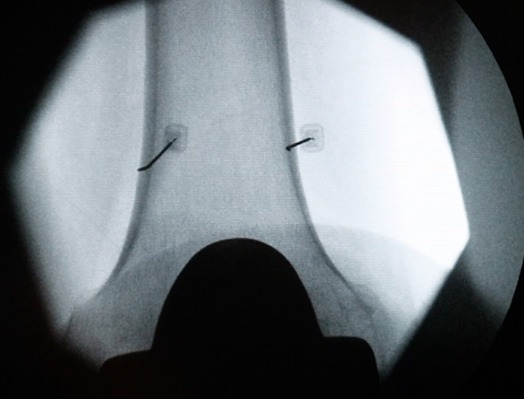
Fig. 6-A.
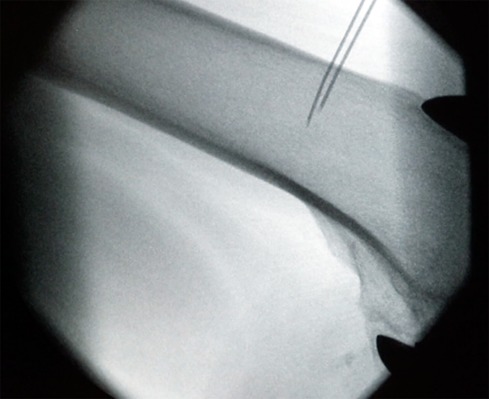
Initial placement of the cannula.
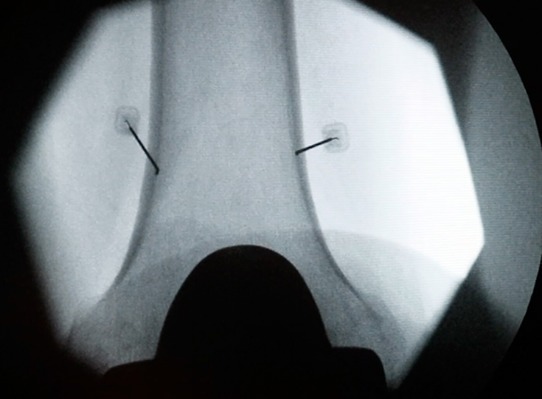
Fig. 6-B.

Final placement of the cannula after advancement.
Step 6: Conduct Sensory and Motor Testing Using Lesion Generator
Conduct electrical testing to confirm that the cannulas are positioned near the 3 genicular nerves.
Sensory confirmation is desirable, but not absolutely required, prior to ablation. Conduct sensory testing at approximately 50 Hz to confirm correct placement of the cannula at the targeted genicular nerves. Sensory testing is completed once the patient experiences pain or pressure that may be consistent with his or her usual knee pain.
Once you have achieved localization by sensory stimulation, conduct motor stimulation using the parameters of 2 V and 2 Hz.
Perform motor stimulation to ensure the absence of undesired motor fiber activity such as fasciculations and to avoid ablating motor nerves. If there is motor activation during motor stimulation, the radiofrequency ablation needles should be repositioned and retested. The procedure is aborted if the patient cannot tolerate it.
Step 7: Injection
Provide lidocaine to reduce pain associated with the ablation.
Prior to the deep injection of lidocaine, withdraw each cannula 2 to 3 mm.
Inject 1 mL of 1% lidocaine prior to ablation (lesioning) through each cannula.
Wait 90 seconds for lidocaine to have a full effect before proceeding with ablation.
Step 8: Ablation and Post-Ablation Procedures
Insert the radiofrequency electrode through the cannulas, increase the temperature, and then advance the cannulas and repeat ablation.
Insert the radiofrequency electrode through the cannulas and increase the temperature to 80°C for 1 minute. Then advance the cannulas at each site 3 to 5 mm (which is done to achieve a slight increase in the lesion volume in the anteroposterior dimension) and repeat the ablation using the same settings.
After the ablation procedure, inject a 1-mL solution containing 27 mg of methylprednisolone through each cannula to decrease postoperative pain and possible neuritis. Then remove the cannulas and apply bandages.
Results
A review of the literature appeared to show that GNRFA may be an effective alternative for people with symptomatic knee OA7-9. For example, 1 study found that, on average, GNRFA led to improvement of >60% from the baseline knee pain in their patient population for at least 6 months9. However, there remains a substantial paucity of high-quality studies on the efficacy of this procedure. In our practice, patients who do not respond to GNRFA have been considered for arthroplasty or have had an arthroplasty already and are usually managed on chronic pain medications. The radiofrequency ablation is generally not repeated if it is not effective the first time. Predicting treatment success with ablation is predicated on a favorable response to a diagnostic genicular block as defined by a reduction of ≥50% in baseline pain.
Pitfalls & Challenges
Although GNRFA targets osseous landmarks, it may be difficult to isolate the exact anatomic location of ≥1 of the genicular nerves10,11. Nevertheless, it is important to place the electrode tip parallel to the genicular nerve next to the periosteum of the target sites8 (Fig. 7).
Although rare, skin burns can occur if the insulation of the needle is compromised or if there is poor contact quality between the patient and the dispersive grounding pad. Avoid placing the ground pad over scar tissue, compromised skin, or osseous prominence. Surgeons should carefully review the manufacturer’s instructions on the use of the ground pad. Staff should be trained on how to reduce the risk of a burn when assisting the physician with radiofrequency ablation procedures. Additionally, the patient should be instructed to alert the physician if he or she experiences any pain or discomfort near or at the site of the ground pad during GNRFA.
A recent literature review and anatomic study found that iatrogenic vascular injury is a possible risk of GNRFA8,12.
Fig. 7.
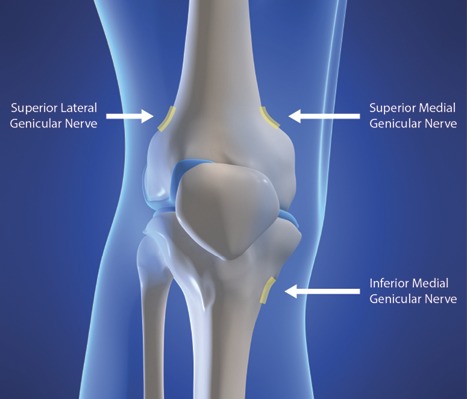
Illustration of the genicular nerves targeted for ablation. (Reproduced with permission of Dr. Corey Hunter [http://ainsworthinstitute.com/genicular-neurotomy/].)
Acknowledgments
Note: The authors thank Jacqueline Ash for her digital expertise during the development of the video.
Footnotes
Published outcomes of this procedure can be found at: JBJS JOPA. 2018;6(1):e10, and Pain. 2011 Mar;152(3):481-7.
Disclosure: The authors indicated that no external funding was received for any aspect of this work. The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJSEST/A241).
References
- 1.Crawford DC, Miller LE, Block JE. Conservative management of symptomatic knee osteoarthritis: a flawed strategy? Orthop Rev (Pavia). 2013. February 22;5(1):e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wehling P, Evans C, Wehling J, Maixner W. Effectiveness of intra-articular therapies in osteoarthritis: a literature review. Ther Adv Musculoskelet Dis. 2017. August;9(8):183-96. Epub 2017 Jun 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dellon AL. Partial knee joint denervation for the knee pain: a review. Orthop Muscul Syst. 2014;3:167. [Google Scholar]
- 4.Salo PT, Hogervorst T, Seerattan RA, Rucker D, Bray RC. Selective joint denervation promotes knee osteoarthritis in the aging rat. J Orthop Res. 2002. November;20(6):1256-64. [DOI] [PubMed] [Google Scholar]
- 5.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957. December;16(4):494-502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Franco CD, Buvanendran A, Petersohn JD, Menzies RD, Menzies LP. Innervation of the anterior capsule of the human knee: implications for radiofrequency ablation. Reg Anesth Pain Med. 2015. Jul-Aug;40(4):363-8. [DOI] [PubMed] [Google Scholar]
- 7.Kidd VD. Genicular nerve radiofrequency ablation: a novel approach to symptomatic knee osteoarthritis. JBJS JOPA. 2018;6(1):e10. [Google Scholar]
- 8.Choi WJ, Hwang SJ, Song JG, Leem JG, Kang YU, Park PH, Shin JW. Radiofrequency treatment relieves chronic knee osteoarthritis pain: a double-blind randomized controlled trial. Pain. 2011. March;152(3):481-7. Epub 2010 Nov 4. [DOI] [PubMed] [Google Scholar]
- 9.Iannaccone F, Dixon S, Kaufman A. A review of long-term pain relief after genicular nerve radiofrequency ablation in chronic knee osteoarthritis. Pain Physician 2017. March;20(3):E437-E444. [PubMed] [Google Scholar]
- 10.Iannaccone F, Le PU, Kim JH, Kim SY. Anatomical basis of genicular nerves: implications for radiofrequency ablation as a treatment for chronic knee pain. Presented as a poster exhibit at the 15th Annual Pain Medicine Meeting; 2016. November 17-19; San Diego, CA. [Google Scholar]
- 11.Orduña Valls JM, Vallejo R, López Pais P, Soto E, Torres Rodríguez D, Cedeño DL, Tornero Tornero C, Quintáns Rodríguez M, Baluja González A, Álvarez Escudero J. Anatomic and ultrasonographic evaluation of the knee sensory innervation: a cadaveric study to determine anatomic targets in the treatment of chronic knee pain. Reg Anesth Pain Med. 2017. Jan-Feb;42(1):90-8. [DOI] [PubMed] [Google Scholar]
- 12.Kim SY, Le PU, Kosharskyy B, Kaye AD, Shaparin N, Downie SA. Is genicular nerve radiofrequency ablation safe? A literature review and anatomical study. Pain Physician. 2016. July;19(5):E697-705. [PubMed] [Google Scholar]


