Abstract
A 67‐year‐old woman was admitted to our hospital because of frequent asthma attacks and refractory chronic rhinosinusitis. She was diagnosed with allergic bronchopulmonary aspergillosis (ABPA) concomitant with eosinophilic chronic rhinosinusitis (ECRS) on the basis of peripheral blood eosinophilia, precipitating antibodies against Aspergillus fumigatus, elevated total serum IgE, pulmonary infiltration, central bronchiectasis, mucoid impaction, and bilateral rhinosinusitis with nasal polyps, which showed remarkable eosinophil accumulation histologically, especially in the ethmoid sinuses. Treatment with mepolizumab, 100 mg every 4 weeks, was initiated for both the ABPA and ECRS. Consistent with the decrease in the peripheral eosinophil count, the asthma and rhinosinusitis symptoms were drastically ameliorated. Not only her airway symptoms but also her exercise tolerance and pulmonary function test results remarkably improved. Mepolizumab therapy enhanced the quality of life for this patient with intractable ABPA and ECRS.
Keywords: Allergic bronchopulmonary aspergillosis, eosinophilic chronic rhinosinusitis, mepolizumab
Introduction
Allergic bronchopulmonary aspergillosis (ABPA) is an eosinophilic pulmonary disorder resulting from a hypersensitivity reaction to Aspergillus fumigatus. ABPA is characterized by bronchial asthma, peripheral eosinophilia, elevated levels of serum IgE, pulmonary infiltration, central bronchiectasis, and mucoid impaction. Because ABPA is usually progressive and seldom remits completely, patients require long‐term treatment with corticosteroids and antifungal agents, potentially leading to various adverse events.
Eosinophilic chronic rhinosinusitis (ECRS) is a refractory chronic rhinosinusitis associated with bilateral nasal polyps, predominantly in the ethmoid sinuses, and blood eosinophilia 1. Despite medical and surgical treatment, ECRS tends to recur.
We describe a case of ABPA concomitant with histologically confirmed ECRS that was successfully treated with mepolizumab, a recombinant anti‐interleukin‐5 (IL‐5) antibody.
Case Report
A 67‐year‐old woman was admitted to our hospital because of poorly controlled severe asthma and chronic rhinosinusitis with nasal polyps. She was diagnosed with asthma and chronic rhinosinusitis 20 years earlier. Since then, her asthma control gradually deteriorated. Sinus surgery, which showed that 90% of the accumulated inflammatory cells were eosinophils, provided only transient improvement. In the last 3 years, she experienced continuous nasal congestion, loss of smell, airway mucus production, frequent asthma attacks, and dyspnoea on exertion. She required an emergent admission due to asthma exacerbation or airway infection three or four times a year despite treatment with high doses of inhaled corticosteroids and long‐acting beta‐agonists, oral leukotriene receptor antagonists, theophylline, and systemic corticosteroids.
On admission, she had peripheral blood eosinophilia, precipitating antibodies against A. fumigatus, and elevated total serum IgE. Chest and head computed tomography demonstrated pulmonary infiltration, central bronchiectasis, diffuse distributed centrilobular small nodules, and mucoid impaction (Fig. 1A, 1B), as well as bilateral rhinosinusitis with nasal polyps, especially in the ethmoid sinuses (Fig. 2A). Sputum cytology and culture demonstrated numerous eosinophils and Charcot–Leyden crystals but no pathogen. On the basis of the history of illness, laboratory findings, and chest and head image findings, she was diagnosed with ABPA. She was also diagnosed with ECRS according to the definition proposed by the Japanese Epidemiological Survey of Refractory Eosinophilic Chronic Rhinosinusitis (JESREC) study group.
Figure 1.
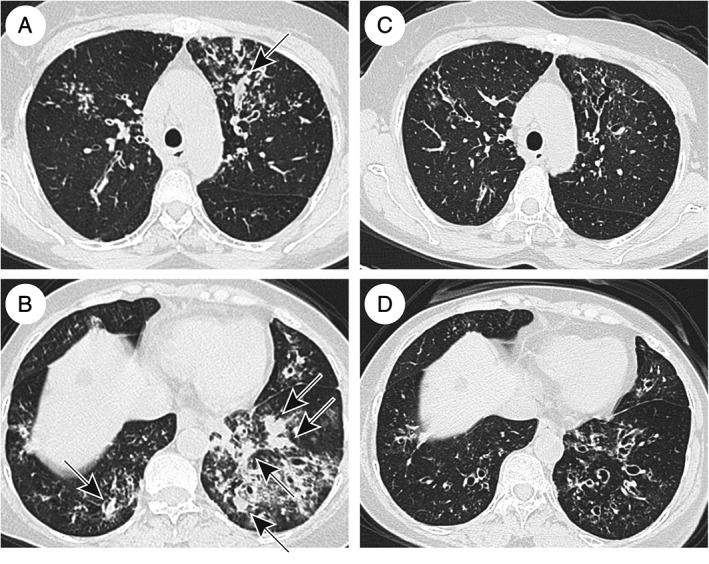
Chest high‐resolution computed tomography before (A, B) and 12 months after (C, D) mepolizumab administration. Panels A and B show remarkable pulmonary infiltration, bronchiectasis, centrilobular small nodules, and mucoid impaction (arrow). Panels C and D show improvement of these findings and disappearance of the mucoid impaction.
Figure 2.
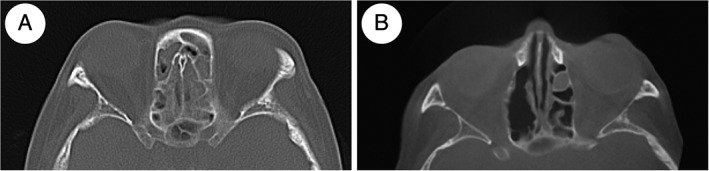
Computed tomography of the ethmoid sinuses before (A) and 12 months after (B) mepolizumab administration. Panel A shows inflammatory opacification of the ethmoid sinuses, and panel B shows improvement of the findings.
Treatment with mepolizumab (100 mg subcutaneously every 4 weeks) was initiated. Two weeks after the initial mepolizumab administration, her peripheral blood eosinophil count decreased from 1163 to 121/μL, and her serum IgE levels decreased from 3163 to 2863 IU/mL. Along with normalization of the peripheral blood eosinophilia, the patient's airway symptoms, including nasal discharge, nasal obstruction, wheezing, and dyspnoea on exertion, were remarkably improved. Her exercise tolerance also improved, and her 6‐min walk distance increased from 120 to 390 m. Twelve months after starting mepolizumab therapy, the forced expiratory volume in the 1‐s (FEV1) and FEV1/forced vital capacity (FVC) ratio increased from 0.77 L and 50.0% to 1.76 L and 81.5%, respectively, and simultaneous computed tomography of the chest and head showed remarkable amelioration of the pulmonary infiltration, diffuse distributed centrilobular small nodules, mucoid impaction (Fig. 1C, D), and sinusitis (Fig. 2B). At 20 months after initiating the mepolizumab treatment, she had experienced no ABPA exacerbation and no adverse events. Before mepolizumab therapy, oral prednisolone 5 mg/day on average was needed, but she currently takes no systemic corticosteroids.
Discussion
We report a case of ABPA with refractory ECRS that was successfully treated with mepolizumab. Mepolizumab exhibited excellent clinical effects for both ABPA and ECRS immediately following administration, as well as long‐term disease control and safety. The decrease in peripheral eosinophilia was associated with the improvement of her sinusitis‐ and asthma‐induced nasal and respiratory symptoms, pulmonary function, and exercise tolerance.
Several recent studies reported that IL‐5 signalling blockade had significant clinical effects on ABPA 2. IL‐5 is essential for eosinophil maturation and proliferation in the bone marrow and is important for prolonging eosinophil survival in the peripheral blood and tissue. Mucus plugging, which is included in Rosenberg and Patterson's criteria for ABPA, is a major pathological component and a characteristic feature of ABPA. Ueki et al. demonstrated that eosinophil extracellular DNA trap cell death (EETosis), which is characterized by the release of filamentous chromatin structures upon cell death, plays an essential role in eosinophil‐associated diseases 3, and Omokawa et al. recently described the existence of EETosis in bronchial secretions from patients with ABPA 4. The excellent clinical effects of mepolizumab on ABPA suggest the importance of EETosis in ABPA. In our case, over 20 months of mepolizumab therapy resulted in excellent disease control with no side effects. The long‐term standard treatment of ABPA, which includes a combination of systemic corticosteroids and antifungal agents, often causes serious adverse effects. Thus, mepolizumab could be an alternative treatment choice for ABPA.
ECRS is an inflammatory disorder of the nose and paranasal sinuses. As in our case, post‐nasal drip is a major factor affecting the poor asthma control, and appropriate and effective treatment of the rhinosinusitis is very important for preventing asthma exacerbation. EETosis has an important role in ECRS, as well as other eosinophilic disorders 3. Anti‐IL‐5 monoclonal antibody treatment significantly improves chronic rhinosinusitis with nasal polyps and eosinophilic inflammation 5. Of note, this previous study 5 used 750 mg of intravenous mepolizumab for the treatment of nasal polyp, and here, we have shown the efficacy of a much lower dose of 100 mg mepolizumab subcutaneously. Marked eosinophilic inflammation of the nasal polyps, diagnosed as ECRS according to the definition proposed by the JESREC study group, was confirmed histologically. This is the first report of histologically confirmed ECRS and ABPA successfully treated with mepolizumab.
In conclusion, we report a case of ABPA complicated by ECRS that was effectively treated with an IL‐5 signalling blockade. This result suggests the importance of eosinophilic inflammation and EETosis in the pathology of ABPA.
Disclosure Statement
Appropriate written informed consent was obtained for publication of this case report and accompanying images.
Matsumoto, N , Shigekusa, T , Matsuo, A , Tsubouchi, H , Yanagi, S , Nakazato, M . (2019) Allergic bronchopulmonary aspergillosis complicated by eosinophilic chronic rhinosinusitis successfully treated with mepolizumab. Respirology Case Reports, 7(7), ;e00465. 10.1002/rcr2.465
Associate Editor: Hiromasa Inoue
References
- 1. Sakuma Y, Ishitoya J, Komatsu M, et al. 2011. New clinical diagnostic criteria for eosinophilic chronic rhinosinusitis. Auris Nasus Larynx 38:583–588. [DOI] [PubMed] [Google Scholar]
- 2. Soeda S, To M, Kono Y, et al. 2019. Case series of allergic bronchopulmonary aspergillosis treated successfully and safely with long‐term mepolizumab. Allergol. Int 68:377–379. [DOI] [PubMed] [Google Scholar]
- 3. Ueki S, Melo RC, Ghiran I, et al. 2013. Eosinophil extracellular DNA trap cell death mediates lytic release of free secretion‐competent eosinophil granules in humans. Blood 121:2074–2083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Omokawa A, Ueki S, Kikuchi Y, et al. 2018. Mucus plugging in allergic bronchopulmonary aspergillosis: implication of the eosinophil DNA traps. Allergol. Int. 67:280–282. [DOI] [PubMed] [Google Scholar]
- 5. Gevaert P, Van Bruaene N, Cattaert T, et al. 2011. Mepolizumab, a humanized anti‐IL‐5 mAb, as a treatment option for severe nasal polyposis. J. Allergy Clin. Immunol. 128:989–995. [DOI] [PubMed] [Google Scholar]


