Abstract
To assess the impact of multidisciplinary rounds (MDR) on 30-day readmissions and length of stay in hospitalized patients with a diagnosis of congestive heart failure in a community teaching hospital.
Patients with primary admission diagnosis of congestive heart failure (CHF) were included. A before and after retrospective study was conducted once the intervention was implemented in 2014. The before and after study periods were each of 1-year duration and included 181 and 151 patients, respectively. Our multidisciplinary heart failure rounding team consisted of a staff cardiologist, case manager, pharmacist, social worker, and a nutritionist.
The mean length of stay decreased from 5.7 days to 5 days, and 30-day readmissions decreased from 27.6% to 17.22% (P-value .026) after implementation of the multidisciplinary rounding. We observed a significant decrease of readmissions in ischemic cardiomyopathy (ICM) (from 33.61% to 14.01%; P-value .007) and heart failure with reduced ejection fraction (HFrEF) (from 31.34% to 16.05%; P-value .028) patients. There was an increase in the percentage of patients hospitalized with non-ischemic cardiomyopathy (NICM) and heart failure with preserved ejection fraction (HFpEF) and, in particular, women patients with heart failure.
Implementation of MDR program on CHF patients resulted in significant decrease in both readmission rate and length of stay in our hospital.
Keywords: heart failure, multidisciplinary rounds, readmissions
1. Introduction
Heart failure is a leading cause of hospitalization and readmission and more Medicare dollars are spent on heart failure than any other medical condition.[1] As reported in the Atherosclerosis Risk in Communities (ARIC) study, there are >915,000 new cases of heart failure every year[2] in United States alone. Up to 50% of patients with heart failure are readmitted within 6 months of discharge[3] with 23.5% of 30 days readmission rate and costing 2.7 billion dollars to the health care system in USA alone (Agency for Healthcare Research and Quality [AHRQ] data-2013). We conducted a retrospective analysis of the impact of multidisciplinary rounds (MDR) on 30-day readmissions and length of stay in hospitalized patients with a diagnosis of congestive heart failure in a community teaching hospital in Baltimore.
Educating patients and families regarding the chronicity and challenges of managing heart failure, as well as strategies to manage heart failure such as weight monitoring, dietary and medication compliance, and close post discharge follow-ups have been shown to decrease the chance of readmissions.[4] Unfortunately, these valuable measures are often underutilized.
Many hospitals and health systems have developed their own quality assessment teams based on CMS requirements to ensure that all heart failure patients are discharged with appropriate medications (Guideline Directed Medical Therapy [GDMT]) including beta-blockers, angiotensin converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARB), diuretics and aldosterone antagonists based on AHA/ACC guidelines unless contraindicated.[5,6]
2. Methods
We conducted a retrospective review of heart failure hospital admission and readmission data to assess the efficacy of multidisciplinary rounds (MDR) on patients admitted with primary diagnosis of heart failure in reducing the 30-day all-cause readmissions and decreasing length of stay in a community teaching hospital. “Our study was granted exempt status by our institutional review board for analysis of deidentified data.”
2.1. Study population
We included all patients hospitalized with a primary diagnosis of heart failure to our community teaching hospital during the study period. Study patients were divided into 2 groups. The control group included patients admitted before the implementation of MDR, from June 2012 to May 2013. The MDR group included patients admitted after implementation of MDR, from June 2015 to May 2016. Patients were excluded from review if they were younger than 18 years of age, died during their hospitalization, were transferred to either hospice or another acute care facility, or were pregnant at the time of admission.
2.2. Study outcomes
The primary endpoint of this study was 30-day all cause readmission rate and the secondary end point was length of stay.
2.3. Multidisciplinary team
Our MDR team consists of a cardiologist, case manager, pharmacist, social worker, and a nutritionist. The MDR team rounds on all patients hospitalized with a primary diagnosis of heart failure and communicates directly with the primary medical team. The MDR team reviews clinical status, medication and dietary compliance, medication optimization as per GDMT, socioeconomic issues that may affect management of heart failure, and post-discharge follow up care. Additionally, the team educates patients and families on diet, weight monitoring, and fluid restriction.
2.4. Statistical methods and analysis
Data were collected by reviewing patient paper charts and electronic medical records. Total number of patients in control group was 181 with a mean age of 70.8 years and the test or MDR group had 151 patients with a mean age of 69.8 years. Remaining patient characteristics are listed in Table 1.
Table 1.
Basic characteristics of the study population.
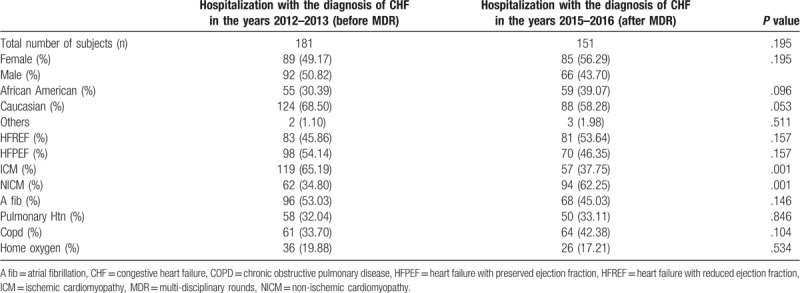
We conducted chi-square test to compare categorical data and Student t test to compare continuous data. We considered a P-value of <.05 to be statistically significant. We conducted all analyses in Microsoft Excel (2017).
3. Results
All-cause 30-day readmission rates were significantly decreased (27.56% vs 17.22%; relative risk (RR) 0.62; P value .026) and mean length of stay decreased from 5.6 days versus 5.0 days after MDR.
Readmission rates were analyzed based on heart failure etiology, systolic function, and sex. In patients with ischemic cardiomyopathy (ICM), we observed a significant reduction in readmissions (33.61% vs 14.01%; RR 0.42; P value .007). In patients with non-ischemic cardiomyopathy (NICM), there was no significant difference in readmission rate after MDR implementation (16.12% vs 19.15%; RR 1.19; P value .676).
We also observed a significant decrease in readmission rates in heart failure patients with reduced ejection fraction (31.34% vs 16.05%; RR 0.51; P value .028), ischemic cardiomyopathy (33.61% vs 14.01%; RR 0.42; P value .007) and also in male patients (27.17% vs 10.56%, RR 0.39; P value .015) after implementation of MDR. On the contrary we didn’t find any significant decrease in readmissions in heart failure patients with preserved ejection fraction (24.49% vs 18.57%; RR 0.76; P value .451), non-ischemic cardiomyopathy (16.12% vs 19.15%; RR 1.19; P value .676), and also in female patients (28.08% vs 22.35%; RR 0.80; P value .486) (Fig. 1).
Figure 1.
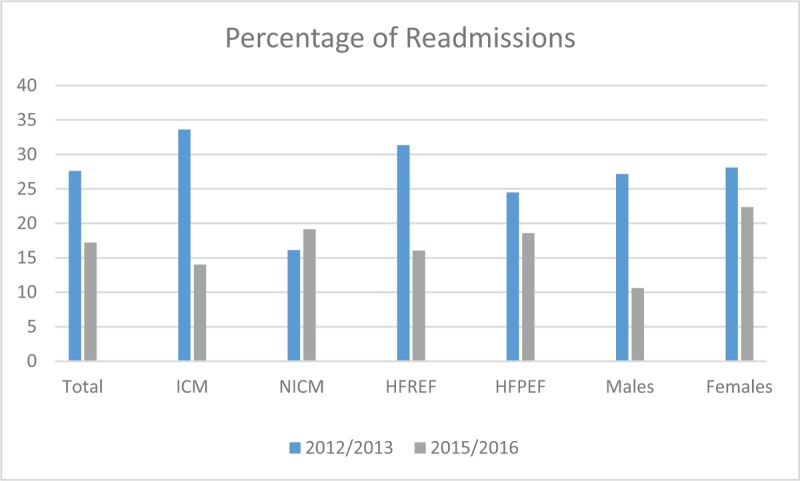
Bar graph showing the percentage of re-admissions, before (2012/2013) and after (2015/2016) implementation of the multidisciplinary rounds (MDR). HFPEF = heart failure with preserved ejection fraction, HFREF = heart failure with reduced ejection fraction, ICM = ischemic cardiomyopathy, NICM = non-ischemic cardiomyopathy.
Systolic function affected readmission rates independent of HF etiology: In patients with HFREF (both ICM and NICM) readmission rates were significantly lower after MDR implementation (31.34% vs 16.05%; RR 0.51; P value .028). There was no statistically significant change in readmission rate observed in patients with HFPEF (24.49% vs 18.57%; RR 0.76; P value .451).
Female patients demonstrated no difference in readmission rate after MDR implementation (28.08% vs 22.35%; RR 0.80; P value .486). Male patients had a significant decrease in readmissions after MDR (27.17% vs 10.6%, RR 0.39; P value .015).
4. Discussion
In our study patients with HFrEF (both ICM and NICM) readmission rates were significantly lower after MDR implementation but no statistical difference in patients with HFpEF.
Decreasing the frequency of readmissions in HF patients would not only markedly decrease the overall cost of medical care but would also improve clinical outcomes and quality of life.[7] A substantial proportion of patients admitted with HF have significant treatment gaps.[8] The purpose of a multidisciplinary rounds program is to minimize the impact of educational and socioeconomic barriers in management of HF. The goal is to affect lifestyle modification, dietary patterns, and medication compliance to optimize management of HF.
However, we did not observe improvement in readmission rates in patients with non-ischemic cardiomyopathy, in patients with preserved EF, and in female patients. While we did not evaluate the causes for these differences, it is not surprising that the MDR strategy was most successful when applied to patients with HFREF as these are the patients in whom GDMT has been most thoroughly evaluated and found to be successful. The lack of success with MDR implementation when applied to patients with NICM and specifically those with HFPEF, may be explained by the more heterogeneous nature of this patient population and by the relative paucity of medical therapies specifically targeted to HFPEF.
A possible explanation for the sex difference may be that a higher proportion of female patients had either HFPEF or NICM as compared with male patients.
We noted a significant increase in the percentage of women hospitalized for heart failure (56.29% vs 49.17%; P value .19) and also an increased number of patients with NICM (62.25% vs 34.8%; P value .01) in the study period compared with control period. This increased rate of admissions for HF in women and in patients with HFPEF at our hospital matches nationally observed trends.[9] As this growth trend coincides with the groups of patients that appeared to derive less benefit from MDR implementation, we have identified an opportunity to improve our management of HF.
With the gradual increase in population of patients with HF and the advent of various expensive device therapies for patients with advanced HF, the cost burden expected to increase by 240% by the year 2030.[10] By decreasing 30-day readmissions, length of stay and increasing compliance with medications, we can decrease the avoidable financial burden on the health care system and patients.[11] Decreased readmissions is a marker for improvement in the clinical status and quality of life of patients. Clearly, challenges remain, particularly in managing patients with increasingly more common forms of HF, specifically HFPEF.
4.1. Clinical perspectives
Assigning a team which includes cardiologist, case manager, pharmacist, social worker, and nutritionist to participate in multidisciplinary rounds on regular basis on all hospitalized heart failure patients will overcome many of the educational, and socio-economic barriers in the management of HF that contribute to HF readmissions. Based on our study, other retrospective and case control studies from the literature and a meta-analysis,[6,12] it is possible to show significant decreases in 30 days and 6 months’ readmissions in the centers with innovative and creative approaches.[9,10]
4.2. Limitations
Our study was limited by the retrospective nature, small sample size, and it being a single-center study. Furthermore, we lacked the data to assess 30-day readmissions to other hospitals in our geographic area, therefore potentially underestimating the true readmission rate to other hospitals. Additionally, we were unable to segregate patients hospitalized with a new diagnosis of heart failure as compared with an established heart failure diagnosis. Socioeconomic status of the population and its impact was not evaluated in this study. Future prospective studies will be helpful in evaluating effectiveness of MDR in improvement of patient satisfaction, cost-effectiveness, and its impact on the community.
5. Conclusion
There is a significant drop in 30 days readmissions and length of stay of HF patients in our hospital after the implementation of multidisciplinary rounds. This strategy will decrease the chances of readmission, improves quality of care, clinical outcomes, patient's quality of life, and decreases financial burden on health care system.
Author contributions
Conceptualization: Raghuram Chava, Kerunne Ketlogetswe.
Data curation: Raghuram Chava, Nabin Karki.
Formal analysis: Raghuram Chava.
Methodology: Raghuram Chava.
Project administration: Raghuram Chava.
Supervision: Kerunne Ketlogetswe, Tomas Ayala.
Validation: Raghuram Chava.
Writing – original draft: Raghuram Chava.
Writing – review & editing: Kerunne Ketlogetswe, Tomas Ayala.
Footnotes
Abbreviations: A fib = atrial fibrillation, ACC = American College of Cardiology, ACE = angiotensin converting enzyme, AHA = American Heart Association, AHRQ = Agency for Healthcare Research and Quality, ARB = angiotensin receptor blockers, CHF = congestive heart failure, COPD = chronic obstructive pulmonary disease, GDMT = Guideline Directed Medical Therapy, HFPEF = heart failure with preserved ejection fraction, HFREF = heart failure with reduced ejection fraction, ICM = ischemic cardiomyopathy, MDR = multi-disciplinary rounds, NICM = non-ischemic cardiomyopathy.
The authors have no conflicts of interest to disclose.
References
- [1].Massie BM, Shah NB. Evolving trends in the epidemiologic factors of heart failure: rationale for preventive strategies and comprehensive disease management. Am Heart J 1997;133:703–12. [DOI] [PubMed] [Google Scholar]
- [2].Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics--2015 update: a report from the American Heart Association. Circulation 2015;131:e29–322. [DOI] [PubMed] [Google Scholar]
- [3].Hunt SA, Abraham WT, Chin MH, et al. American College of Cardiology Foundation. American Heart Association. 2009 Focused update incorporated into the ACC/AHA 2005 Guidelines for the diagnosis and management of heart failure in adults. A report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines developed in collaboration with the International Society for Heart and Lung Transplantation. J Am Coll Cardiol 2009;53:e1–90. [DOI] [PubMed] [Google Scholar]
- [4].Donzé J, Lipsitz S, Bates DW, Schnipper JL. Causes and patterns of readmissions in patients with common comorbidities: retrospective cohort study. BMJ 2013;347:f7171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Rich MW, Beckham V, Wittenberg C, et al. A multidisciplinary intervention to prevent the readmission of elderly patients with congestive heart failure. N Engl J Med 1995;333:1213–4. [DOI] [PubMed] [Google Scholar]
- [6].Kociol RD, Peterson ED, Hammill BG, et al. National survey of hospital strategies to reduce heart failure readmissions: findings from the get with the Guidelines-Heart Failure registry. Circ Heart Fail 2012;5:680–7. [DOI] [PubMed] [Google Scholar]
- [7].Rice H, Say R, Betihavas V. The effect of nurse-led education on hospitalization, readmission, quality of life and cost in adults with heart failure. A systemic review. Patient Educ Couns 2018;101:363–74. [DOI] [PubMed] [Google Scholar]
- [8].Biglane JB, Becnel MF, Ventura HO, et al. Pharmacologic therapy for heart failure with reduced ejection fraction: closing the gap between Clinical Guidelines and Practice. Prog Cardiovasc Dis 2017;60:187–97. [DOI] [PubMed] [Google Scholar]
- [9].Ryan J, Andrews R, Barry MB, et al. Preventability of 30-day readmissions for heart failure patients before and after a quality improvement initiative. Am J Med Qual 2014;29:220–6. [DOI] [PubMed] [Google Scholar]
- [10].Basoor A, Doshi NC, Cotant JF, et al. Decreased readmissions and improved quality of care with the use of an inexpensive checklist in heart failure. Congest Heart Fail 2013;19:200–6. [DOI] [PubMed] [Google Scholar]
- [11].Kocher RP, Adashi EY. Hospital readmissions and the affordable care act: paying for coordinated quality care. JAMA 2011;306:1794–5. [DOI] [PubMed] [Google Scholar]
- [12].Phillips CO, Wright SM, Kern DE, et al. Comprehensive discharge planning with post discharge support for older patients with congestive heart failure: a meta-analysis. JAMA 2004;291:1358–67. [DOI] [PubMed] [Google Scholar]


