Abstract
The aim of the study was to determine the financial burden of complications and examine the cost differentials between complicated and uncomplicated hospital stays, including the differences in cost due to extent of resection and operative technique.
Liver resection carries a high financial cost. Despite improvements in perioperative care, postoperative morbidity remains high. The contribution of postoperative complications to the cost of liver resection is poorly quantified, and there is little data to help guide cost containment strategies.
Complications for 317 consecutive adult patients undergoing liver resection were recorded using the Clavien-Dindo classification. Patients were stratified based on the grade of their worst complication to assess the contribution of morbidity to resource use of specific cost centers. Costs were calculated using an activity-based costing methodology.
Complications dramatically increased median hospital cost ($22,954 vs $15,593, P < .001). Major resection cost over $10,000 more than minor resection and carried greater morbidity (82% vs 59%, P < .001). Similarly, open resection cost more than laparoscopic resection ($21,548 vs $15,235, P < .001) and carried higher rates of complications (72% vs 41.5%, P < .001). Hospital cost increased with increasing incidence and severity of complications. Complications increased costs across all cost centers. Minor complications (Clavien-Dindo Grade I and II) were shown to significantly increase costs compared with uncomplicated patients.
Liver resection continues to carry a high incidence of complications, and these result in a substantial financial burden. Hospital cost and length of stay increase with greater severity and number of complications. Our findings provide an in-depth analysis by stratifying total costs by cost centers, therefore guiding future economic studies and strategies aimed at cost containment for liver resection.
Keywords: cost analysis, costs, hospital costs, liver resection, postoperative complications
1. Introduction
Improving perioperative outcomes for liver resection, along with developments in the diagnosis and management of liver tumors over the last 2 decades, have broadened indications for hepatic resection.[1,2] Simultaneously, increasing knowledge of liver anatomy and physiology has fostered an increase in the complexity and extent of disease that is considered operable, with repeat and 2-stage resections becoming increasingly more common.[3–5] Increasing complexity and extent of hepatic resection, however, carries an increase in the incidence and severity of postoperative complications,[6,7] with typically >50% of patients experiencing complications,[1,8,9] even in high-volume centers. Complications after liver resection not only carry a substantial clinical burden, they also place a growing economic burden upon healthcare providers. Complications present the greatest contribution to increased costs after hepatic resection,[7,10] and consequently provide an important target for interventions seeking to reduce healthcare expenditure.
As the demand for healthcare grows, utilizing limited resources in an era of mounting costs is becoming paramount in maintaining an effective and universally available healthcare system. Despite this, there is limited financial data available on the topic of hepatic resection, and even less so quantifying the cost of complications. Aiming to address this need, we conducted a retrospective cohort study in a high-volume tertiary center with expertise in hepatic resection, with the primary objective of examining the sources of cost differentials between complicated and uncomplicated patients. Secondary objectives were to assess the impact of surgical technique and extent of resection on the incidence and severity of complications and associated costs. We also sought to identify patient and anesthetic factors associated with the clinical and economic outcomes.
We hypothesized that with increasing incidence and severity of complications there would be a corresponding increase in costs, and that cost increases would be associated with more extensive hepatic resection (open vs laparoscopic and major vs minor).
2. Methods
Following Human Research Ethics Committee approval (no: LNR/17/Austin/78), adult patients undergoing elective or emergent hepatic resection between July 2010 and June 2017 at the Austin Hospital, a tertiary hospital with hepatobiliary expertise, were identified using International Statistical Classification of Diseases (ICD) codes specific to liver resection. The study period was chosen as during this period there was a well-established enhanced recovery after surgery program in place and minimal changes in perioperative care delivered by the same team of surgeons and anesthetists. We elected not to extend the study period further into the past to minimize potential confounding from patients treated before an enhanced recovery after surgery program being in place. High volume surgeons performed all operations. Austin Health use Cerner electronic medical records that allow comprehensive electronic data capture and access to patient health information in the perioperative setting.
2.1. Definitions
ICD codes of the following surgical categories were included: “excision of lesion of liver,” “segmental resection of liver,” “lobectomy of liver,” “trisegmental resection of liver,” “segmental resection of liver for trauma,” “lobectomy of liver for trauma,” and “trisegmental resection of liver for trauma.” The principal procedure performed was then confirmed using the operation record, and in the case of discrepancies, the procedure outlined in the detailed operation record was used. A “major” liver resection was defined as 4 or more segments resected,[11] with the remainder of procedures considered as “minor” resections. Nonanatomical segmental resections and wedge resections were considered as half a segment, with the total number rounded down where necessary. Patients undergoing concomitant procedures were included, unless the liver procedure was minor and secondary to another major procedure, in which case they were excluded. Patients undergoing a “deroofing of liver cyst” and liver biopsies were excluded, unless there was sufficient parenchymal resection (1 or more segments).
Complications were defined as any deviation from the normal postoperative course, guided by the European Perioperative Clinical Outcome definitions.[12] Bile leak was defined as presence of bile in the drainage fluid that persisted on postoperative day 4, and acute pancreatitis, defined as an elevation in serum lipase > 3× normal laboratory reference range. Complications were recorded by 2 independent clinicians, and then graded according to Clavien-Dindo classification.[13] The Clavien-Dindo classification is a validated approach to surgical outcome assessment that assigns severity grades to surgical complications. In case of disagreement on grading by 2 assessors, the case was discussed with reference to the classification guide with a third author. Assessors grading complications were blinded to the cost associated with each patient aiming to eliminate observer bias. In addition, patients were assigned a score using the Comprehensive Complication Index,[14] a novel surgical risk calculator that integrates all morbid events with their severity. This was completed largely for comparison with the Clavien-Dindo classification, which was used as the primary complication grading tool due to its ease of interpretation, recognizability, and generalizability.
Length of stay was determined by the period from completion of surgery to discharge, excluding days in the hospital-in-the-home unit. Days in the hospital-in-the-home unit were not considered as they are costed as a separate admission at our institution and were considered beyond the scope of this study, which focuses on the index surgical admission. Readmission was defined as unplanned readmission to the hospital within a 30-day follow-up period. Mortality was considered when it occurred within 30 days of the index admission.
2.2. Cost analysis
All costs related to the index admission for liver resection and any consequent readmissions were included. Costs related to preoperative course were not considered. Allocation of costs was done based on service volume, and costs were calculated using an activity-based costing methodology. Raw costing data were allocated into a priori clinical cost centers based on individual itemization codes for costs incurred during the admission. These categories included “intensive care unit (ICU),” “medical” (e.g., medical consults, allied health, pathology, blood products, and radiology), “operative,” “pharmacy,” and “ward” costs. For detailed cost analysis of complication incidence and severity, cost centers were further separated into “allied health” (e.g., physiotherapy, speech pathology, dietician), “blood products” (e.g., albumin, packed red cells), “ICU,” “medical consults” (consults external to the treating team), “pathology” (e.g., tissue diagnosis, blood testing), “pharmacy” (drug dispensing), “operative” (anesthesia and theater resources), “radiology” (e.g., scans, radiological procedures), and “ward” (e.g., hospital bed, nursing, catering). Only in-hospital costs were considered, with both direct and indirect costs assessed to produce a total cost for each patient. Costs are displayed as medians with interquartile range (IQR).
Costs were inflated to 2018 dollars based upon the average Australian Consumer Price Index (CPI) from 2010 to 2017 inclusive, as reported by the Reserve Bank of Australia.[15] The average CPI was applied pro rata to each patient based on the number of days between the admission date and the 1st of January 2018, to ensure accurate inflation and reduce error in comparison. Conversion to United States Dollar ($) was completed using the market rate on the 1st of January 2018.
2.3. Subgroup analysis
In addition to analyzing the impact of complications on hospital cost, we undertook subgroup analysis by extent of resection (major resection vs minor resection) and operative technique (open vs laparoscopic).
2.4. Statistical analysis
Continuous and categorical characteristics were summarized as medians with IQRs and counts (proportions), respectively. The Mann-Whitney U and Kruskal-Wallis tests were used to compare costs. The Mann-Whitney U was also used to compare continuous variables relating to patient characteristics. The Fisher exact and Pearson χ2 test were used to compare proportions relating to patient characteristics as appropriate.
A 2-sided P value of ≤.05 was considered significant; however, given that multiple comparisons were used when comparing cost categories, we applied the following Bonferroni corrections: for the analysis of complications versus no complications, laparoscopic versus open, segments resected, and extent of resection costs by individual cost centers, a P value of ≤.002 was considered as indicative of statistical significance and for the analysis of Clavien-Dindo costs by individual cost centers, a P value of ≤.005 was considered as indicative of statistical significance. The data set collected was almost complete, with only 9 patients missing values for height and consequently body mass index (BMI). This was not considered to be a risk in introducing bias, and so these patients were included in statistical analysis as normal. Statistical analysis was performed using commercial statistical software STATA/IC v.13 and Prism 7.0 GraphPad software (La Jolla, CA).
3. Results
3.1. Patient characteristics
We identified 335 patients who underwent liver resection at the Austin Hospital between July 2010 and June 2017. Based on our selection criteria, 18 were excluded. The remaining 317 patients had a median patient age of 60 years (IQR 50, 67) with 183 (58%) men. Median BMI and Charlson Comorbidity Index (CCI) were 26.3 kg/m2 (IQR 23.2, 30.6) and 6 (IQR 4, 8), respectively. The principle diagnosis and indication for resection was benign in 55 (17%) patients and malignant in 262 (83%) patients. Four (1%) patients were emergent cases. Forty-six (15%) patients had received chemotherapy within 3 months of surgery, and 25 (8%) had prior liver resections. There were 82 (26%) patients with cirrhosis of the liver, the majority being Child Pugh class A.
“Major” liver resection was performed on 66 (20%) patients and the remaining 251 (80%) had “minor” resections. The median number of liver segments resected was 2 (IQR 1, 3). Eighty-nine (28%) patients were operated on laparoscopically, and 228 (72%) had open procedures, 19 (8%) of which were converted from laparoscopy, most commonly due to bleeding or difficult access. Patients selected for laparoscopy were younger [58 (IQR 46, 66) vs 60 (IQR 51, 68) years; P = .03], larger [BMI 27.6 (IQR 24.1, 31.6) vs 26.1 (IQR 23, 30.4) kg/m2; P = .04] and had fewer comorbidities [CCI 5 (IQR 4, 7) vs 7 (IQR 4, 8), P = .004]. The range of procedures included 4 (1%) 2-stage right hepatectomies (ALPPS procedures), 1 central hepatectomy, 7 (2%) extended left hepatectomies, 17 (5%) extended right hepatectomies, 17 (5%) left hepatectomies, 36 (11%) right hepatectomies, 32 (10%) left lateral hepatectomies, 128 (40%) segmental resections, and 75 (24%) wedge resections. There were 142 (45%) patients who had concomitant procedures, the most common of which was cholecystectomy (n = 100). Tables 1 to 3 show the preoperative and intraoperative characteristics of patients grouped by occurrence of complication, extent of resection, and operative technique respectively.
Table 1.
Patient characteristics for complicated and uncomplicated patients presented as median [interquartile range] and number (proportion).
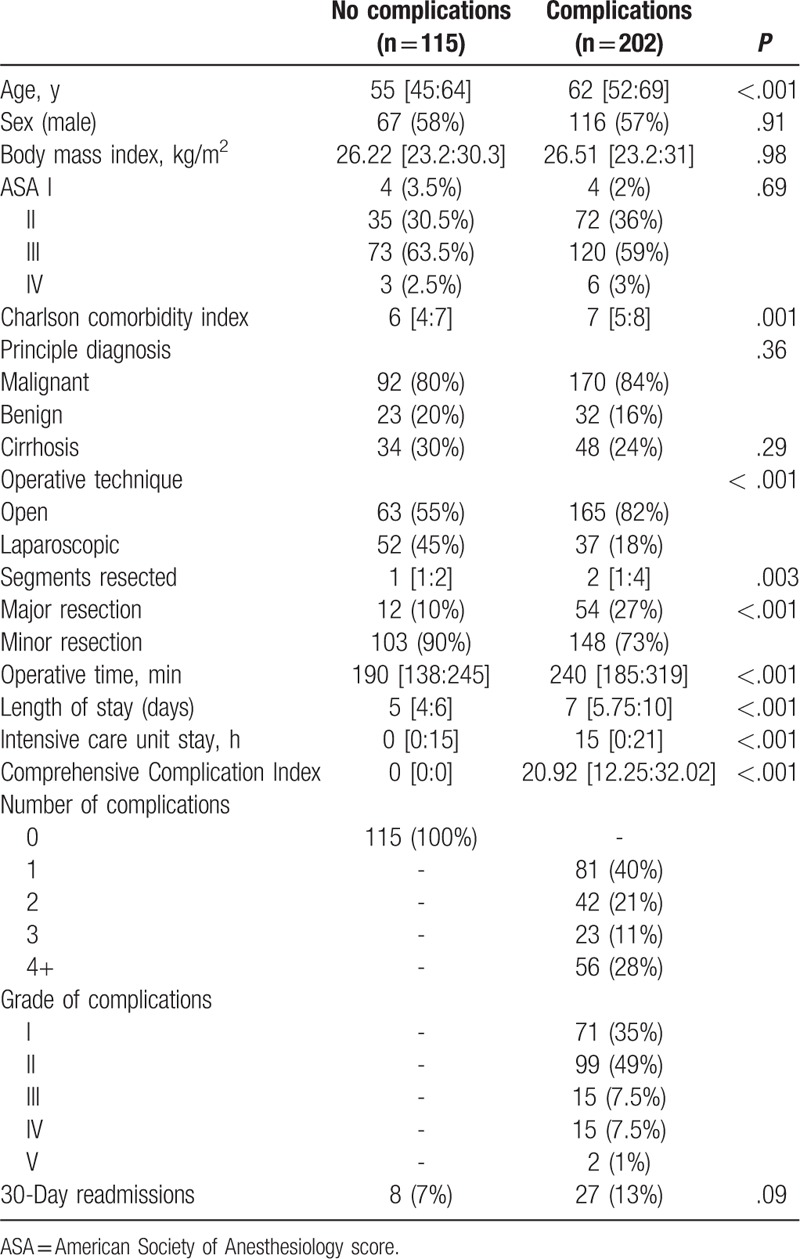
Table 3.
Patient characteristics for operative technique presented as median [interquartile range] and number (proportion).
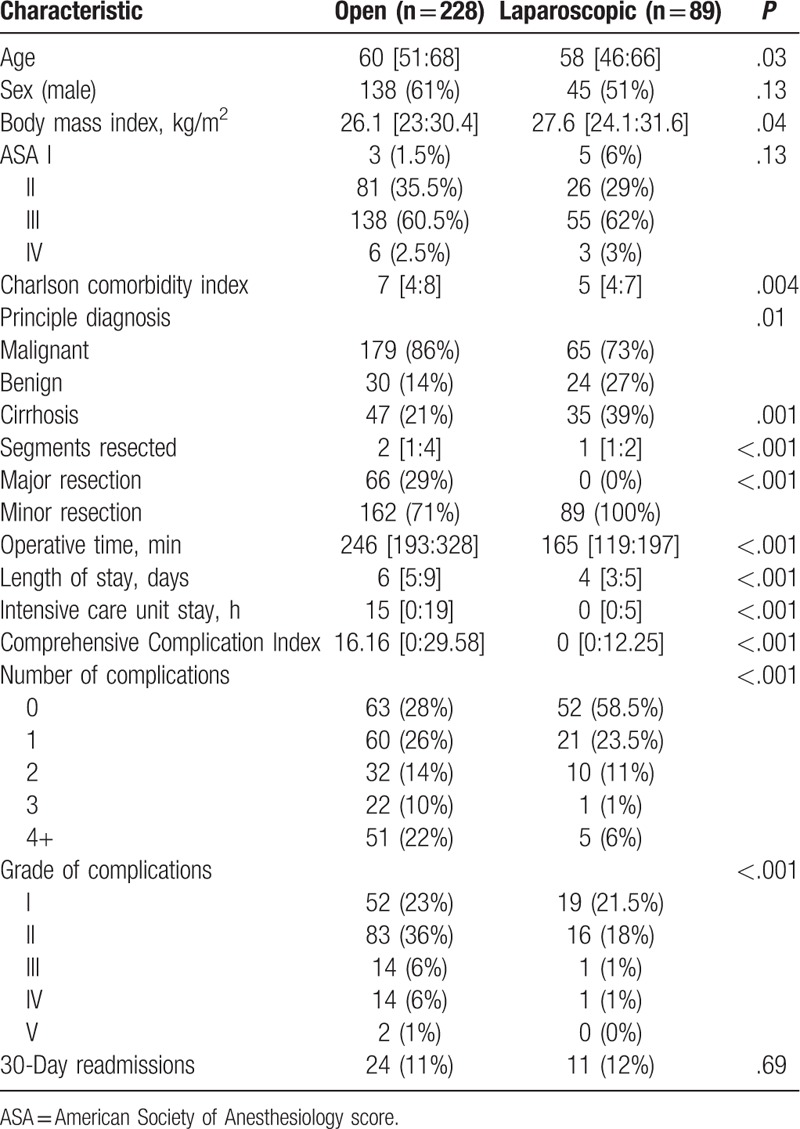
Table 2.
Patient characteristics for extent of resection presented as median [interquartile range] and number (proportion).

3.2. Complications
Patients experiencing a complication were older (62 vs 55 years, P < .001) and carried greater comorbidity [CCI 7 (IQR 5, 8) vs 6 (IQR 4, 7), P = .001]. The overall complication rate was 64% with complications significantly greater for open surgery compared with laparoscopy (72% vs 41.5%, P < .001). Major complications (Clavien-Dindo grade III–V) occurred in 10% of the cohort. Major resection carried the greatest association with morbidity (82% vs 59%, P < .001), and complication severity, with 21% of patients having a major complication, against 7% for minor resection (P < .001). Nearly all major complications occurred in patients having open surgery (n = 30 vs n = 2 complications, P < .001). Mortality for the cohort was 0.6% (2 patients). The median Comprehensive Complication Index score was 8.66 (IQR 0:24.24) for the entire cohort.
Stratification by complication incidence and severity is detailed in Tables 1 to 3. Aside from the stated differences, the cohorts for uncomplicated versus complicated, major versus minor resection, and open versus laparoscopic technique were largely similar. Length of stay was increased for patients undergoing major resection [8 (IQR 6, 16) vs 6 (IQR 4, 7) days, P < .001], open surgery [6 (IQR 5, 9) vs 4 (IQR 3, 5) days, P < .001], and those experiencing complications [7 (IQR 6, 10) vs 5 (IQR 4, 6) days, P < .001]. Similarly, ICU stay, and theater time were increased in patients having major resection, open surgery, and experiencing complications (Tables 1–3). No statistically significant difference in the occurrence of readmissions was identified between groups. Median length of stay for readmissions was 3 days (IQR 1, 6). Median length of stay did not differ between individual years across the study period (P = .14).
Complications most commonly occurred in the cardiopulmonary system (34%), followed by the gastrointestinal (21%), renal (7%), and neurologic (7%) systems. Bleeding occurred in 18% of patients and 15% of patients ended up with infections (inclusive of cellulitis, wound infections, and pneumonia). Postoperative liver failure (1.5%) and bile leak (4%) occurred more rarely. The most common complications were anemia (16%) and atelectasis (16%). A further 12% of patients had pleural effusions. Hypotension requiring treatment also occurred commonly (15%). Nausea and vomiting were experienced by 13% of patients. It was not uncommon for patients to become hypervolemic (11%) as a result iatrogenic fluid overload. Electrolyte derangements were common (12%) with hypokalemia occurring most frequently.
3.3. Cost analysis
Median hospital costs for all patients were $19,154 (IQR 15,442, 27,933). Hospital cost was greatly increased for patients undergoing open surgery compared to laparoscopy (P < .001). Patients undergoing major resection cost >$10,000 compared with minor resection (Table 4). Costs increased substantially between patients having 2 and 4 segments resected, whereas there was little variability in costs when 3 or fewer segments were resected (Table 4).
Table 4.
Median [interquartile range] hospital costs (2018 United States Dollar) by cost center.
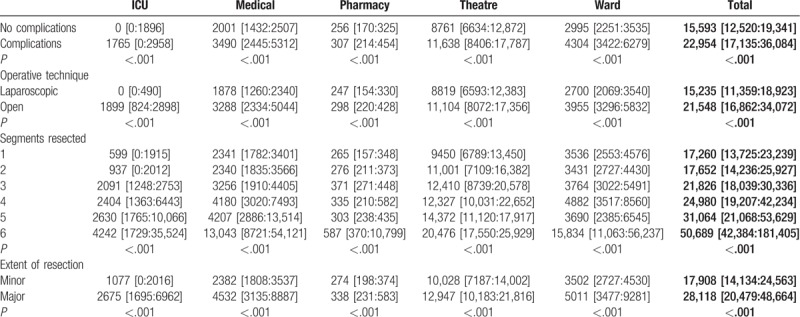
Patients who developed a complication cost $7,001 more than patients without complications (Table 4). Costs increased with both the incidence and severity of complications (Table 5), although mortality corresponded with reduced total costs compared to patients with major complications. Costs increased across all cost centers as complication severity increased (P < .001). Similarly, costs across all cost centers increased with greater number of complications (Fig. 1). The majority of costs for all patients were attributable to operative (56%), ward (19%), ICU (8%), and medical consults (6%). Readmissions carried a median hospital cost of $3,433 (IQR 948:6,577).
Table 5.
Hospital costs (2018 United States Dollar) by cost center and Clavien-Dindo (CD) classification.
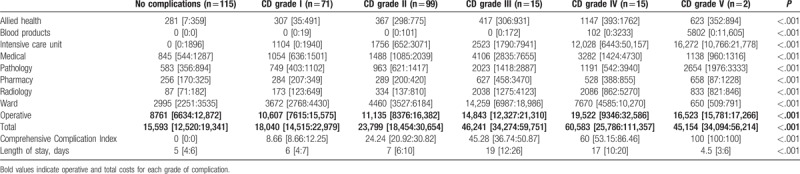
Figure 1.
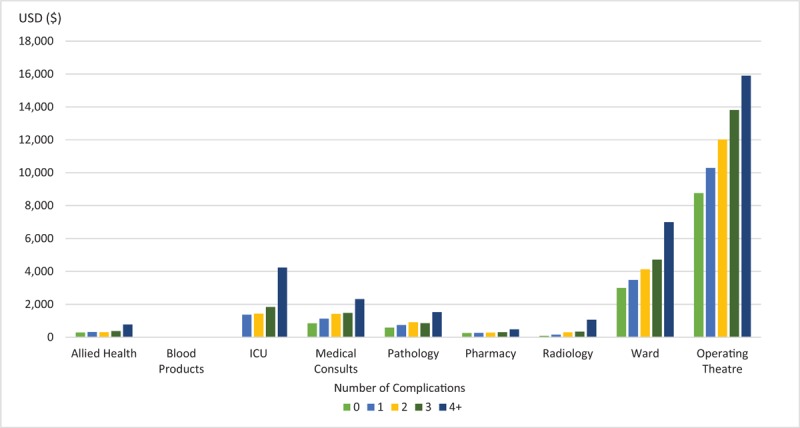
Median (IQR) hospital costs (2018 USD) by cost center and number of complications. The median hospital cost of blood products was $0 for all groups, and so the values have not been included. IQR = interquartile range, USD = United States Dollar.
4. Discussion
We conducted a detailed cost analysis of all liver resections performed at a high-volume university hospital with expertise in hepatobiliary surgery, focusing on the impact of complications on hospital resource use. We found, as hypothesized, a significant increase in hospital costs associated with the incidence and severity of complications. Furthermore, we found that complications were common. Nearly two-thirds of patients had at least 1 complication, and 1 in 10 patients developed a major complication (Clavien-Dindo Grade III–V). Patients experiencing a complication were also older, sicker, and more likely to undergo a major (4 or more segments) resection via open surgery. This was supported by the Comprehensive Complication Index score, which was demonstrated to increase with major open surgery. Interestingly, we also found a significant health cost associated with patients experiencing minor complications.
In addition, our data provide strong evidence showing that as the number of liver segments resected increases, so does the major complication rate. Contrary to other studies,[11] this association was strongly associated when 3 or more segments were resected.
Using an activity-based costing methodology we found that hospital resource use increased across all predefined cost centers with increasing number of complications. Major complications placed an enormous burden on hospital resources, with grade III and IV complications costing 3 and 4 times, respectively, more than uncomplicated patients. The majority of resource use was due to large increases in the cost of ICU care, medical consults, operative, and ward costs. This was largely influenced by length of stay, although patients with grade IV complications had shorter stays than those with grade III complications, indicating that morbidity not only increases length of stay, but also the pro rata cost of care. This is supported by data from patients suffering mortality, who had the shortest length of stay but cost $29,561 more than uncomplicated patients.
Our data validate that minor complications carry a profound and significant financial burden. Minor complications were experienced by 54% of patients in our cohort, with these complications increasing length of stay compared to uncomplicated patients and resulting in significant increases in costs. Patients with grade I and II complications cost approximately $2500 and $8000, respectively more than uncomplicated patients. We found that most of these costs were attributable to ward stay, ICU, and operative costs. However smaller increases in the costs of medical consults, pathology, and radiology also contributed to the greater resource use of these patients and provide a target for cost reduction through judicious and rational prescribing of investigations.
The impact of minor complications on hospital resource use was largely unexpected, given that minor complications are often considered to be clinically trivial. Given the large number of patients experiencing minor complications, they present the greatest target for reducing hospital resource use. Major complications commonly result from complex high acuity surgery coupled with significant patient comorbidity risks, and may be difficult to constrain, whereas minor complications may be preventable and easily targeted for cost reduction through simple interventions, that is, effective prehabilitation with detection and treatment of anemia, optimization of preoperative glucose control, nutritional patient optimization for perioperative analgesia, use of advanced monitoring for rational fluid intervention, and enhanced recovery after surgery programs. In addition, we observed anecdotally that minor complications often occurred following deviations from surgical protocols, suggesting greater adherence to surgical protocols would likely reduce the incidence of minor complications. Given the financial burden resulting from the occurrence of minor complications, investment from health care providers into strategies aiming to further improve surgical protocol and increase adherence would likely prove to be financially beneficial.
Concerning hospital resource use, previous studies seeking to quantify the burden of complications have often only addressed major complications without consideration of minor complications.[7,10,16,17] The findings of our study indicate this to be clearly insufficient and demonstrate the significant contributions which minor complications have on both length of stay and hospital resource use. In this manner, our study adds valuable evidence to the existing literature, by demonstrating the financial burden of minor complications, and quantifying the cost across specific cost centers. Our study supports the findings of a similar study by Vonlanthen et al,[18] which demonstrated increasing costs with increasing severity of complications, whereas adding valuable information specific to liver resection and the impact of extent of resection on cost and complication incidence. In addition, our study corroborates findings from a previous study[19] by our research group investigating the impact of complications on the cost of pancreaticoduodenectomy. Both studies have demonstrated increasing costs with increasing complication severity and have highlighted the importance of minor complications with regards to both clinical and financial cost, and together demonstrate that this is likely applicable to other procedures outside of liver and pancreatic resection.
The complication rate in our study is consistent with contemporary literature on liver resection[7,17,20] when considering major complications. However, many previous studies have often neglected to report minor complications,[7,17,21–23] and as such our overall complication rate was much higher than previous literature suggests, although it is consistent with studies[6,10] that have included minor complications in their assessment. Furthermore, the difference we found in complication rate for open and laparoscopic resection is consistent with previous literature.[6,20,24] However, given the heterogeneity of liver resection procedures between techniques, it is difficult to draw a definitive comparison between techniques, and instead our data more meaningfully represent the overall complication rate for all liver resection at our institution.
Our decision to use the Clavien-Dindo classification for grading severity of complications was due to a few factors. The Clavien-Dindo classification assigns severity grades based on the interventions required to manage them, which makes it very easy to interpret from a clinical perspective, particularly with relation to costs. In addition, it is the most well established and recognizable tool for surgical outcome assessment, having greater generalizability and recognition compared with other outcome assessment tools. However, we felt it was important to compare the Clavien-Dindo classification with the Comprehensive Complication Index, a novel surgical risk calculator that integrates all morbid events with their severity, given the likelihood that this may become the preferred tool for surgical outcome assessment in the future. The Comprehensive Complication Index is based upon the Clavien-Dindo classification and assigns a score to each patient based on both the number and severity of postoperative complications during the assessed period. It is considered to be more sensitive than using the Clavien-Dindo classification alone.[14] However, by assigning morbidity to continuous variables it can make interpretation of complications difficult to understand, which was largely the reason we opted not to use this tool as our primary measure. Regardless, we found that as the Comprehensive Complication Index score increased, so too did hospital costs across all cost centers. In addition, the score was higher for patients who underwent major open surgery, and thus supports our findings based on the Clavien-Dindo classification.
Our study has several strengths. Our data are the first to provide data quantifying hospital resource use by specific cost centers stratified by postoperative complications of liver surgery by stringently applying Clavien-Dindo classification for all complications. In a previous study, Lock et al[16] addressed the impact of postoperative liver failure on the resource use of specific cost centers; however, our study has expanded on this to include all complications graded by severity. In addition, our study has included all complications, not only major complications, providing comprehensive financial data for liver resection.
Our study has some limitations. Our study was completed at a single center with expertise in hepatobiliary surgery, and this may limit the external validity of our findings, although our center shares many of the same operative and anesthetic characteristics of other tertiary centers. As all hepatobiliary surgeons and anesthetists were part of a dedicated hepatobiliary-anesthesia service, we did not collect outcomes of individual anesthetists or surgeons. There may have been individual variation in practice between clinicians affecting outcomes and an increase in skill base or cases completed may have affected improvement in outcomes. These inherent confounders are difficult to quantify and may be considered a limitation. However, during the study there were no major changes to the enhanced recovery after surgery program or perioperative care of patients, ensuring standardization of care for patients across the study period. Given the retrospective nature of our study, the collection of data may have been subject to observation bias through human error regarding the interpretation and recording of data. This may have led to an under-reporting of complication incidence, particularly for minor complications which may not have been recorded as stringently as major complications in medical records. However, we consider this an unlikely source of error given the comprehensive crosschecks required for data entry at our institution, the use of electronic medical records, and the detailed data provided by the hospital Business Intelligence Unit, which collects adverse outcome data independently. In addition, we applied a stringent and systematic methodology when recording data, with multiple crosschecks. Lastly, although we considered the incidence and cost of 30-day readmissions, we did not investigate the long-term and community centered costs of patients, for example, visits to the general practitioner, postoperative chemoradiotherapy costs, quality of life measures, etc, and as such we were unable to quantify the long-term economic burden of morbidity. Furthermore, exclusion of days spent in the hospital-in-the-home unit along with primary care follow-up will have likely underestimated the occurrence of minor complications which may have occurred after discharge. The likely impact of this is a slight underestimation of the financial and clinical burden of minor complications. However, given that our study has highlighted the significance of minor complications, the possibility of a slight underestimation of this impact will not have affected the outcome.
5. Conclusions
Complications remain common after liver resection and contribute to increased length of stay and increased hospital costs. Hospital resource use increases with the severity and incidence of complications. Although the largest increases in cost are seen with major complications, minor complications present a significant target for cost reduction despite often being clinically insignificant. Our study has identified key cost centers associated with increased resource use due to patient morbidity, and as such has provided targets for interventions and further investigation.
Author contributions
Data analysis: Luka Cosic, Leonid Churilov, Laurence Weinberg.
Data collection: Luka Cosic, Ronald Ma, David Debono.
Manuscript drafting and editing: Luka Cosic, Mehrdad Nikfarjam, Christopher Christophi, Laurence Weinberg.
Manuscript editing: Ronald Ma.
Study design: Luka Cosic, Leonid Churilov, Laurence Weinberg.
Footnotes
Abbreviations: BMI = body mass index, CCI = Charlson Comorbidity Index, EPCO = European Perioperative Clinical Outcome, ICD = International Statistical Classification of Diseases, ICU = intensive care unit, IQR = interquartile range.
Clinical trial registration: Australia New Zealand Clinical Trials Registry Trial Id: ACTRN12618001021268
The authors report no conflicts of interest.
References
- [1].Jarnagin WR, Gonen M, Fong Y, et al. Improvement in perioperative outcome after hepatic resection: analysis of 1,803 consecutive cases over the past decade. Ann Surg 2002;236:397–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Poon RT, Fan ST, Lo CM, et al. Improving perioperative outcome expands the role of hepatectomy in management of benign and malignant hepatobiliary diseases: analysis of 1222 consecutive patients from a prospective database. Ann Surg 2004;240:698–708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Vennarecci G, Laurenzi A, Santoro R, et al. The ALPPS procedure: a surgical option for hepatocellular carcinoma with major vascular invasion. World J Surg 2014;38:1498–503. [DOI] [PubMed] [Google Scholar]
- [4].Jaeck D, Oussoultzoglou E, Rosso E, et al. A two-stage hepatectomy procedure combined with portal vein embolization to achieve curative resection for initially unresectable multiple and bilobar colorectal liver metastases. Ann Surg 2004;240:1037–49. discussion 1049–1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Petrowsky H, Gonen M, Jarnagin W, et al. Second liver resections are safe and effective treatment for recurrent hepatic metastases from colorectal cancer: a bi-institutional analysis. Ann Surg 2002;235:863–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Cannon RM, Scoggins CR, Callender GG, et al. Financial comparison of laparoscopic versus open hepatic resection using deviation-based cost modeling. Ann Surg Oncol 2013;20:2887–92. [DOI] [PubMed] [Google Scholar]
- [7].Idrees JJ, Johnston FM, Canner JK, et al. Cost of major complications after liver resection in the United States: are high-volume centers cost-effective? Ann Surg 2017;11:11. [DOI] [PubMed] [Google Scholar]
- [8].Virani S, Michaelson JS, Hutter MM, et al. Morbidity and mortality after liver resection: results of the patient safety in surgery study. J Am Coll Surg 2007;204:1284–92. [DOI] [PubMed] [Google Scholar]
- [9].Dimick JB, Cowan JA, Jr, Knol JA, et al. Hepatic resection in the United States: indications, outcomes, and hospital procedural volumes from a nationally representative database. Arch Surg 2003;138:185–91. [DOI] [PubMed] [Google Scholar]
- [10].Breitenstein S, De Oliveira ML, Raptis DA, et al. Novel and simple preoperative score predicting complications after liver resection in noncirrhotic patients. Ann Surg 2010;252:726–34. [DOI] [PubMed] [Google Scholar]
- [11].Reddy SK, Barbas AS, Turley RS, et al. A standard definition of major hepatectomy: resection of four or more liver segments. HPB (Oxford) 2011;13:494–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Jammer I, Wickboldt N, Sander M, et al. Standards for definitions and use of outcome measures for clinical effectiveness research in perioperative medicine: European Perioperative Clinical Outcome (EPCO) definitions: a statement from the ESA-ESICM joint taskforce on perioperative outcome measures. Eur J Anaesthesiol 2015;32:88–105. [DOI] [PubMed] [Google Scholar]
- [13].Dindo D, Demartines N, Clavien P. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004;240:205–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Slankamenac K, Graf R, Barkun J, et al. The comprehensive complication index: a novel continuous scale to measure surgical morbidity. Ann Surg 2013;258:1–7. [DOI] [PubMed] [Google Scholar]
- [15].Reserve Bank of Australia, Measures of Consumer Price Inflation. Available at: https://www.rba.gov.au/inflation/measures-cpi.html Accessed April 2018. [Google Scholar]
- [16].Lock JF, Reinhold T, Malinowski M, et al. The costs of postoperative liver failure and the economic impact of liver function capacity after extended liver resection—a single-center experience. Langenbecks Arch Surg 2009;394:1047–56. [DOI] [PubMed] [Google Scholar]
- [17].Manecke GR, Asemota A, Michard F. Tackling the economic burden of postsurgical complications: would perioperative goal-directed fluid therapy help? Critical Care 2014;18:566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Vonlanthen R, Slankamenac K, Breitenstein S, et al. The impact of complications on costs of major surgical procedures: a cost analysis of 1200 patients. Ann Surg 2011;254:907–13. [DOI] [PubMed] [Google Scholar]
- [19].Wang J, Ma R, Eleftheriou P, et al. Health economic implications of complications associated with pancreaticoduodenectomy at a University Hospital: a retrospective cohort cost study. HPB (Oxford) 2018;20:423–31. [DOI] [PubMed] [Google Scholar]
- [20].Fretland AA, Dagenborg VJ, Bjornelv GMW, et al. Laparoscopic versus open resection for colorectal liver metastases: the OSLO-COMET randomized controlled trial. Ann Surg 2018;267:199–207. [DOI] [PubMed] [Google Scholar]
- [21].Knechtle WS, Perez SD, Medbery RL, et al. The association between hospital finances and complications after complex abdominal surgery: deficiencies in the current health care reimbursement system and implications for the future. Ann Surg 2015;262:273–9. [DOI] [PubMed] [Google Scholar]
- [22].Gani F, Hundt J, Makary MA, et al. Financial impact of postoperative complication following hepato-pancreatico-biliary surgery for cancer. Ann Surg Oncol 2016;23:1064–70. [DOI] [PubMed] [Google Scholar]
- [23].Gani F, Pawlik TM. Assessing the costs associated with volume-based referral for hepatic surgery. J Gastrointest Surg 2016;20:945–52. [DOI] [PubMed] [Google Scholar]
- [24].Vanounou T, Steel JL, Nguyen KT, et al. Comparing the clinical and economic impact of laparoscopic versus open liver resection. Ann Surg Oncol 2010;17:998–1009. [DOI] [PMC free article] [PubMed] [Google Scholar]


