Supplemental Digital Content is available in the text
Keywords: China, hypertension, TASHP, treatment adherence
Abstract
To assess the adherence level of antihypertensive treatment and identify any associated risk factors in a sample of hypertensive patients from China.
A cross-sectional study involving 488 Chinese hypertensive patients was conducted in a tertiary hospital in Xi’an, China. Data were collected regarding socio-demographic factors and hypertension-related clinical characteristics. The adherence to treatment was assessed using the previously validated instrument: therapeutic adherence scale for hypertensive patients.
A total of 27.46% of patients were compliant with their antihypertensive treatments. Three factors were identified to be independently associated with antihypertensive treatment adherence: gender (P = .034), residence (P = .029), duration of high blood pressure (P < .001). Gender, residence, occupation, and the duration of antihypertensive drugs treatment used were found to have significant effects on treatment adherence in certain categories.
Treatment adherence among hypertensive patients in China was poor. More attention and effective strategies should be designed to address factors affecting treatment adherence. Education about hypertension knowledge should be strengthened for patients. Moreover, the importance of lifestyle modification during hypertension treatment is often neglected by patients, therefore, there is an urgent need to educate hypertensive patients about the adherence to lifestyle modifications.
1. Introduction
High blood pressure (HBP) is considered one of the most challenging public health problems worldwide and reported as the leading risk factor for both cardiovascular death and hospitalizations.[1] HBP affects over 1.5 billion people globally and by 2025 an estimated 2 billion people will suffer from HBP.[2] One study showed that the leading cause of global disease burden was HBP, which accounted for approximately 7% of global disability adjusted life-years in 2010 and contributes to about 9.4 million deaths worldwide on an annual basis.[3]
However, the control of HBP is unsatisfactory. In the USA, an estimated 53.5% of people diagnosed with HBP did not adequately control their blood pressure (BP).[4] A study involved a total of 50,171 subjects showed that the prevalence of hypertension in China was 29.6% and the control rate among participants being treated for hypertension was only 27.4%.[5]
Poor adherence to treatment regimens is considered as one of the most important reasons for uncontrolled BP in hypertensive patients.[6] Adherence to hypertension treatment is defined as the process by which patients follow the agreed treatment regimens with their physician.[7] Therefore, it is necessary to measure hypertensive patient adherence and elucidate any barriers, thereby designing proper methods to improve adherence.
There are various ways used to assess adherence behaviors in hypertensive patients, which are divided into subjective reports (eg, questionnaire, inquiry), as well as indirect objective methods (eg, reminder packaging, mobile health, electronic medication monitoring).[8–13] However, self-reporting methods, which have the advantages of low cost and being the simplest way to gather information, are the most commonly used methods to assess adherence behaviors.[14] There are a variety of self-reported questionnaires that have been used to measure adherence behaviors in hypertensive patients[15–18]; each of these has its own advantages and disadvantages. There is no consensus as to how nonadherence is defined, and a gold-standard method for measuring adherence does not exist.[19] The Morisky Medication Adherence Scale (MMAS-4 and MMAS-8) are the most commonly used questionnaires and they have been established reliability and validity evidence.[20] However, the MMAS is limited because they do not include items related to lifestyle modifications[14] and includes only a small number of adherence barriers.[21] At present, most of the adherence questionnaires applied in China are translated versions of foreign questionnaires. Since cultural and economic characteristics are the key factors that lead to differences in adherence behaviors among different ethnic people,[22] translated versions of foreign questionnaires may not be suitable for Chinese populations.
To evaluate treatment adherence in Chinese hypertensive patients, Tang et al[23] developed the therapeutic adherence scale for hypertensive patients (TASHP). The TASHP has been demonstrated to have good psychometric properties by measuring internal consistency, test-retest reliability, and construct validity. It comprises 25 questions that are not only related to medication adherence, but also lifestyle intervention. Since this scale is designed according to the actual conditions of the Chinese hypertensive patients, it is more suitable for Chinese populations. There is a scarcity of studies using this scale to assess treatment adherence in Chinese hypertensive patients.
In this study, we aimed to use the TASHP scale to assess treatment adherence in Chinese hypertensive patients, evaluate the factors influencing adherence behaviors, and determine the interventions that improve adherence. The findings of the study can provide information for health care providers and policymakers for the improvement of treatment adherence in Chinese hypertensive patients.
2. Patients and methods
A cross-sectional survey was carried out by trained clinical pharmacists in the department of neurology, cardiology, and ophthalmology of the Xi’an Fourth Hospital. All the clinical pharmacists participating in this research had received standardized training on survey procedures and communication skills. This study was approved by the ethics committee of Xi’an Fourth Hospital and verbal consent was obtained from all participants.
The inclusion criteria for participants were:
-
(1)
≥18 years-old,
-
(2)
diagnosis of primary hypertension,
-
(3)
undergoing antihypertensive drug therapy, and
-
(4)
agreeing to participate in the study.
Exclusion criteria were:
-
(1)
patients with severe complications of hypertension (eg, stroke and severe heart failure),
-
(2)
patients who could not communicate due to physical or mental problems, and
-
(3)
pregnant women.
The minimum sample size was calculated using the following formula:
where s is the minimum sample size, z is the standard normal variate, p is an estimate of the proportion of the patients who complied with their antihypertensive treatment,[24]d is the sample error to be tolerated, and the confidence interval was 5%; therefore, d is 0.05, z is 1.96, and p was estimated to be 35%, which was consistent with a related study.[25] As a result, the minimum sample size required for the study was 350, and 500 patients were finally recruited in this study. These patients were hospitalized in the neurology, cardiology, and ophthalmology unit during the period from January 1, 2018 to June 30, 2018.
The patient data regarding socio-demographic factors, as well as clinical data that included duration of HBP, duration of antihypertensive drugs used, and BP categories, were collected by reviewing the electronic medical records of each patient. HBP treatment adherence was measured using the TASHP questionnaire. For illiterate patients, the questions were read by the trained clinical pharmacists to facilitate survey completion.
The TASHP questionnaire consists of 25 questions, which are divided into 4 categories. Category 1 includes 5 items that reflect whether medication was taken according to the type of medicine, dose, time, and frequency as prescribed by the physicians. It was called “adherence with taking medicines.” Category 2, which is termed “poor medication behavior” includes 8 items describing whether patients do not adhere to medication therapy. For example, “How often do you forget to take your HBP pills?” and “How often do you miss taking your HBP medications when you feel better?” These 2 categories belong to medication therapy.
Category 3 (10 items) refers to adherence about lifestyle modifications, such as salt restriction, low-fat diet, consumption of vegetables and fruits, weight reduction, regular physical exercise, monitoring BP, release of stress, and so on, that was called “daily life management.” Category 4 (2 items) refers to adherence regarding the control of tobacco and alcohol, which was called “smoking and alcohol management.” Each item uses a 5-point Likert response scale:
-
(1)
never/very rarely,
-
(2)
rarely,
-
(3)
sometimes,
-
(4)
mostly, and
-
(5)
all of the time, with 1 to 5 points assigned, respectively, and reverse scores are assigned for reverse questions (5–1 points) (See the TASHP scale in Appendix).
Possible scores range from 25 to 125, with a higher score indicating greater adherence. A cutoff score of 109 was used to distinguish satisfactory and low adherence behaviors.[14] The total Cronbach α coefficient of the scale was 0.862 and the test-retest reliability coefficient of the total scale was 0.958.[23] The scoring criteria was used in a pilot study on a group of 30 patients diagnosed with HBP (Cronbach's alpha 0.904).
2.1. Data analysis
Socio-demographic data and clinical characteristics of HBP among the study patients were analyzed using descriptive statistics. The chi-square test was used to analyze univariate factors for treatment adherence. Binary logistic regression analysis was used to analyze independent risks factor for patient's antihypertensive treatment adherence. To analyze the association of demographic and clinical variables to treatment adherence in each TASHP category, general linear model was used with the total score of each category as the outcome variable. Since the total score of each category was normal, a generalized linear model with a normal distribution and identity link function was used. P < .05 was considered to be statistically significant. All statistical analyses were performed using SPSS version 19 (IBM Corp, Armonk, NY).
3. Results
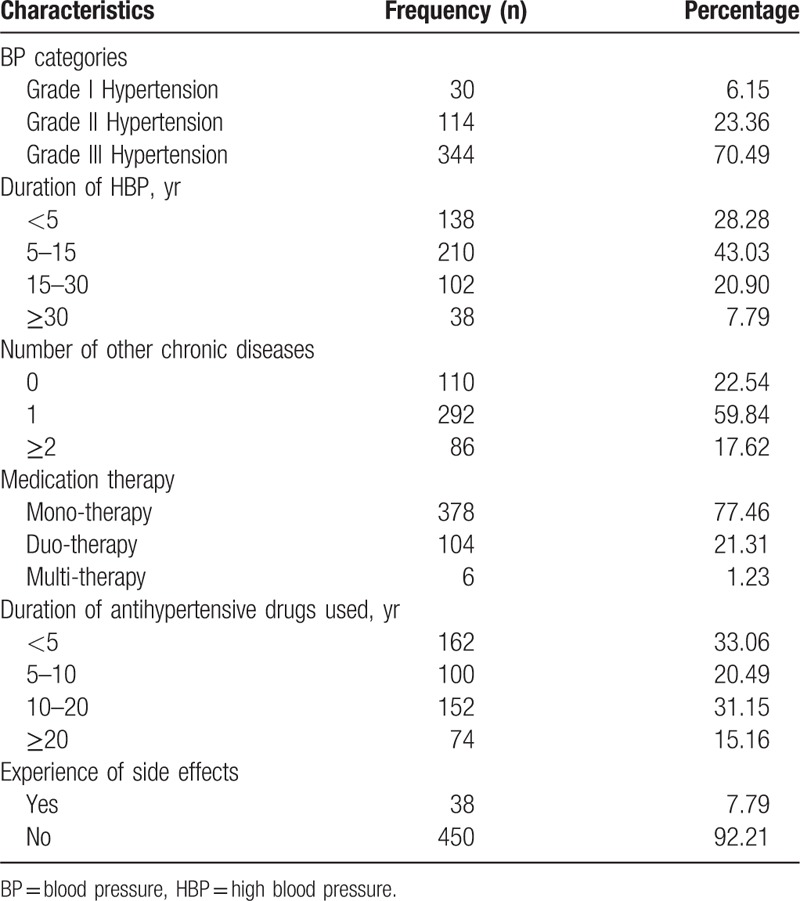
Twelve patients were excluded because of incomplete TASHP questionnaires. Finally, 488 patients were included in this study, of which 242 (49.59%) were male and 352 (72.13%) were retired. Most of the patients (97.54%) were middle and old age (age ≥45 years old). A total of 424 (86.89%) patients were from urban areas, of whom 420 patients had health insurance, while 64 (13.11%) patients were from rural areas, and only 28 of these patients had health insurance. Twenty-two patients (4.51%) were illiterate, and 92 (18.85%) patients had a college or university degree (Table 1). Most patients (70.49%) were diagnosed with stage III HBP. Almost half of the patients (43.03%) were diagnosed with HBP in the last 5 to 10 years. In addition, 110 patients (22.54%) had no other chronic diseases, and 86 (17.62%) patients had more than 2 other chronic diseases. A total of 378 patients (77.46%) took an anti-HBP medication every day, with 162 (33.06%) patients having taken antihypertensive drugs for less than 5 years and 226 (46.31%) patients took antihypertensive drugs more than 10 years. Furthermore, 450 patients (92.21%) did not experience medication-related side effects during the duration of anti-HBP drugs (Table 2).
Table 1.
Socio-demographic characteristic of hypertensive patients.
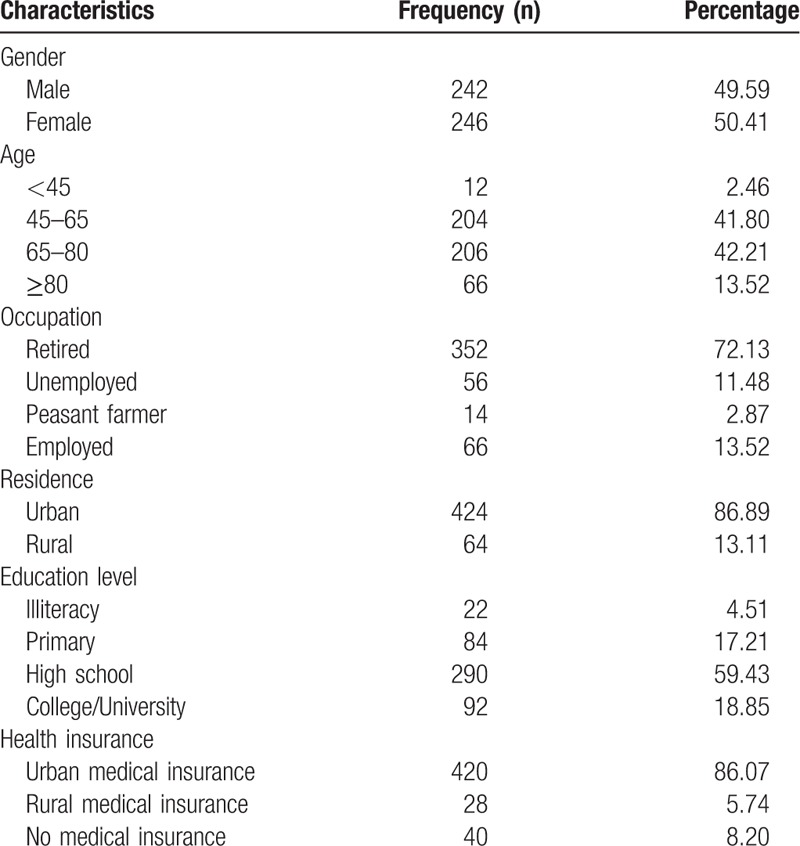
Table 2.
Clinical characteristics of hypertensive patients.
Base on the TASHP cutoff score, 134 patients (27.46%) had satisfactory adherence behaviors, while the remaining 354 (72.54%) patients were noncompliant. The univariate analysis of the socio-demographic and clinical factors for treatment adherence is provided in Table 3. Three factors were significantly associated with adherence: gender (P = .018), residence (P = .004), and duration of HBP (P = .048).
Table 3.
Factors associated with optimal treatment adherence (n = 488).
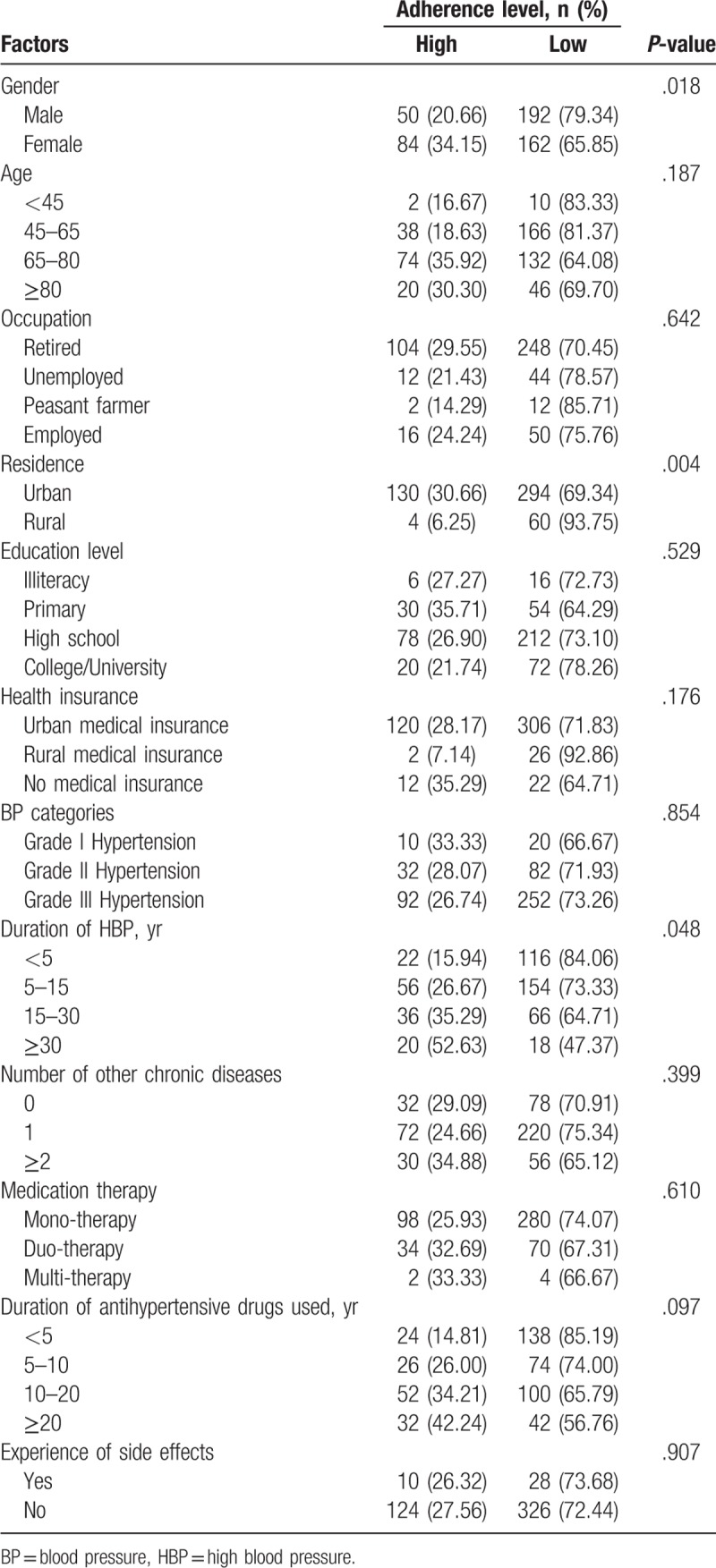
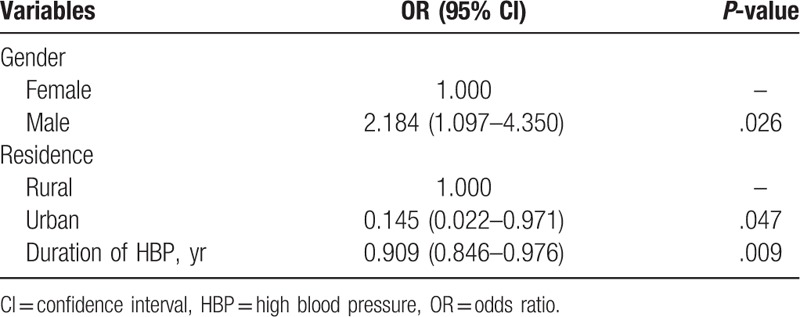
Table 4 summarizes the result of the binary logistic regression analysis. Gender (P = .034), residence (P = .029), and duration of HBP (P < .001) were identified as being independently associated with antihypertensive treatment adherence. Comparing to females, males were less compliant (P = .026, odds ratio [OR] = 2.184, 95% confidence interval [CI]: 1.097–4.350). Urban patients were more adherent to their treatment plan than those from rural areas (P = .047, OR = 0.145, 95% CI: 0.022–0.971). The longer the time since they were diagnosed with HBP resulted in greater adherence for the HBP patients in this study (P = .009, OR = 0.909, 95% CI: 0.846–0.976).
Table 4.
Binary logistic regression analysis of factors associated with treatment adherence in hypertensive patients.
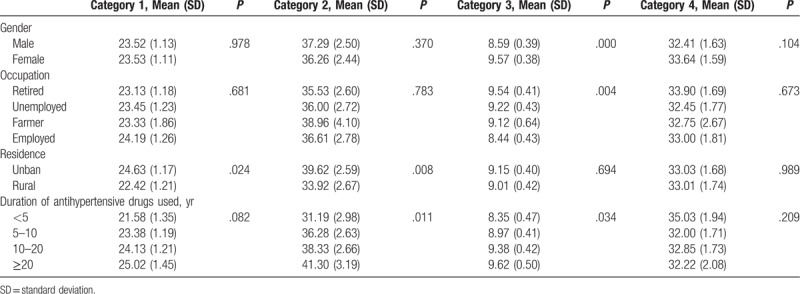
The results of the general linear model analysis are shown in Table 5. The score for each category is the sum of the scores of all items in the category. There were 4 factors for which the scores were significantly different in specific categories: gender, occupation, residence, and duration of antihypertensive drug use. For example, the scores obtained for gender were found to be significantly different in category 3 (daily life management). Female scores in category 3 were higher than those for males (P < .001). Since a higher score indicates greater adherence, females were more compliant in daily life management. In addition, category 3 was the main aspect of the compliance difference between genders. Category 3 was also the main aspect influenced by occupation. Retired patients earned the highest score, with employed patients having the lowest (P = .004), which indicates that the retired people were the most compliant individuals regarding daily life management. Patients in urban areas were more adherent than those in rural with the higher scores in category1 (adherence with taking medicines) (P = .024) and category2 (poor medication behavior) (P = .008). The longer of the time used antihypertensive drugs, the more adherent patients were in category 2 (P = .011) and category 3 (P = .034).
Table 5.
General linear model analysis in certain categories of risk factors.
4. Discussion
Due to an increasingly aging population, hypertension has become a common global public health problem. Nonadherence to antihypertensive treatment in patients with hypertension is associated with an increased risk of stroke and cardiovascular disease.[6,26] The purpose of this investigation was to study the treatment adherence of Chinese hypertensive patients and the associated risk factors. Since culture and economy are important factors that affect the treatment compliance of hypertensive patients, treatment compliance scales, and questionnaires produced in different cultural and economic backgrounds cannot be fully applied to other populations. In this study, we used the TASHP, which was demonstrated to be a validated and reliable instrument and suitable for the Chinese population.
This study revealed that only 134 patients (27.46%) adhered to their antihypertensive treatment, and most patients (72.54%) do not have satisfactory adherence behaviors. The adherence rate found in this study was much lower than that reported in some developed countries, developing countries, and other developed regions in China.[27–32] Cultural and economic characteristics are crucial factors that may explain different levels of adherence among different populations.[22] This study was conducted in the northwestern region of China, which is an underdeveloped region. The treatment adherence of hypertensive patients in underdeveloped regions should be pained more attention and be provided additional health care resources by health care professionals and policymakers.
There are many factors that may be associated with the rates of nonadherence, including gender, age, location, cost of the medications, and socioeconomic status.[33] In this study, there were 3 independent risk factors related to antihypertensive treatment adherence: gender, residence, and the duration of hypertension. By dividing the impact of each risk factor on treatment adherence into 4 different categories, we found that gender, residence, occupation, and duration of antihypertensive drugs used had significant effects on treatment compliance in certain categories.
The association between gender and antihypertensive treatment adherence remains a subject of debate. Both negative and positive relationships have been reported in the literature. In this study, gender was a predictor of antihypertensive treatment adherence with females reporting better adherence than males. This finding was consistent with some previous studies,[25,34] but opposite to several others.[35,36] Another study showed that medication adherence in females was 1.531 times higher than that of males, but the difference was not statistically significant.[37] Our study revealed that the higher compliance of females is mainly in the category of daily life management (category 3). This finding is consistent with a previous study conducted on a Korean population, which showed that males were generally more associated with nonadherence to lifestyle recommendations, even if they were aware of their disease.[38] The possible reason is that females perceive and report their health problems more obstinately than men[39] and they would like to pay more attention to diet, weight reduction, physical exercise, BP monitor, and so on. In addition, males are usually busier than females and experience more heavy pressure from work, which may prohibit spending more time to make lifestyle modifications.
This study found that location of hypertension patients also affected treatment adherence. It was determined that patients lived in rural areas were less adherent than those living in an urban setting. This finding was not consistent with most of the previous studies, which showed no association between place of residence and nonadherence to treatment.[40,41] This study revealed that the lower compliance of rural people than urban people was mainly in the category of adherence with taking medicines (category 1) and poor medication behavior (category 2). There exist large differences in cultural levels, economic status, and medical conditions between rural and urban people in China. A recent paper showed that although the urban-rural gaps in health care utilization have gradually narrowed, the urban-rural disparities are still evident in health care resources.[42]
Rural residents tend to have less education, lower income, and more barriers to accessing healthcare than urban residents.[41] The main reasons for the unsatisfactory treatment adherence of rural patents were probably attributed to lack of adequate knowledge and the economic factors also being a contributing factor. Both drug adherence and BP control rate were significantly associated with hypertension knowledge.[43]
Lack of health knowledge is common among the elderly in the areas of rural China. Low levels of economic development lead to minimal health knowledge transmission among the population in rural areas.[44] As better awareness of hypertension is a significant factor in improving treatment adherence, more appropriate health education strategies may be needed for rural hypertensive patients. Health education about hypertension is usually organized by healthcare professionals in hospitals or communities in the urban setting. Therefore, it is necessary for medical professionals to go to rural areas to convey hypertension knowledge. Furthermore, the society, government, and medical institutions should collaborate to help patients improve their hypertension awareness in rural China.
Since hypertensive patients requires lifelong continuous medical treatment, each hypertensive patient needs to allocate a specific budget every month to purchase medications. Furthermore, there is a wide range of rural people without any medical insurance coverage, even those who have medical insurance may not have all medications covered, and the patients may have to pay out-of-pocket.[36] The government should invest more in medicine, thereby expanding the scope and reimbursement ratio of rural medical insurance.
In this study, the duration of hypertension was found to affect treatment adherence. The longer of the duration since they were diagnosed with hypertension, the more adherent the patients were; this founding was consistent with previous studies.[32,45] One possible reason for this was that it is convenient for elderly hypertensive patients to become knowledgeable about hypertension and its risks, so they have better medication-taking behaviors and tend to implement preventive measures such as decreasing salt intake, performing more regular exercise, controlling body weight, regularly monitoring BP, and managing stress. A study conducted on Canadian patients reported that few patients had lifestyle changes within 2 years after their diagnosis of hypertension.[46]
We also found that the longer the duration they were using antihypertensive drugs, the more adherent were the patients in the categories of poor medication behavior (category 2) and daily life management (category 3). A possible reason for this is that with the extension of treatment time, patients gradually accept the fact that they are supposed to take their medication every day, and some patients who have negative attitudes eventually change their medicine taking and lifestyle habits.
As for occupations, farmers and employed patients tended to have poorer medication adherence when compared to unemployed or retired patients in daily life management; this is consistent with the findings of a previous study.[47] A lack of awareness and busy work are the main reasons for this finding.
Our study findings highlight the importance of lifestyle modifications for better hypertensive treatment adherence. In the study, differences in compliance with hypertension caused by different genders, occupations, and duration of antihypertensive drugs used were mainly reflected in daily life management (category 3). Although effective antihypertensive medications are available for many people, especially urban dwellers, the hypertensive treatment adherence and control rate are still unsatisfactory.[48] According to previous reports, lifestyle modifications that mainly include dietary adjustment, exercise, weight management, and stress release was a promising tool for promoting the prevention and control rate of hypertension.[49,50] However, some hypertensive patients principally rely on medication and do not comply with lifestyle recommendations. Therefore, it is necessary for hypertensive patients to understand that lifestyle modifications are also essential for BP control. Health education on lifestyle changes of patients in self-managing their hypertension should be strengthened.
Our study has some policy implications. It was found that gender, residence, and duration of HBP were significantly associated with treatment adherence. Hence, evidence-based interventions, such as educational programs, could be used to target hypertensive patients who are male, live in rural areas, and/or have a short duration of HBP, to improve their treatment adherence. Meanwhile, differences in hypertension treatment compliance caused by different genders, occupations, and duration of antihypertensive drug use were mainly reflected in daily life management, which suggests that changing patient perceptions towards the role of life modifications could be a primary focus of patient education initiatives.
There are some limitations to this study. First, samples in this investigation were selected from a limited area in Western China with a relatively homogeneous population; therefore, the result may not be generalizable. Second, the measurement of treatment adherence was based on self-reported questionnaires, which may introduce recall bias. Third, the sample size was small, larger-scale investigations should be carried out in the future.
5. Conclusion
In conclusion, we used the TASHP criteria to evaluate the risk factors associated with hypertension treatment adherence in Chinese hypertensive patients. A total of 72.54% of the study patients were nonadherent to antihypertensive treatment. Gender, residence, and the duration of hypertension were found to be the main factors affecting treatment adherence. We also found that gender, residence, occupation, and duration of antihypertensive drug use had significant effects on treatment adherence in certain categories. The education and awareness regarding hypertension knowledge need to be strengthened. Furthermore, the importance of lifestyle modifications in compliance with hypertension treatment needs to be emphasized.
Author contributions
Data curation: Jingjing Pan, Tao Lei, Bin Hu, Xiaorong Xue.
Investigation: Jingjing Pan.
Project administration: Lian Wu.
Software: Qiongge Li.
Supervision: Huichuan Wang.
Validation: Qiongge Li.
Writing – original draft: Jingjing Pan.
Writing – review and editing: Lian Wu.
Supplementary Material
Footnotes
Abbreviations: BP = blood pressure, HBP = high blood pressure, TASHP = therapeutic adherence scale for hypertensive patients.
The authors report no conflicts of interest in this work.
Supplemental Digital Content is available for this article.
References
- [1].Wolf M, Ewen S, Mahfoud F, et al. Hypertension: history and development of established and novel treatments. Clin Res Cardiol 2018;107Suppl 2:16–29. [DOI] [PubMed] [Google Scholar]
- [2].Uchmanowicz I, Jankowska-Polanska B, Chudiak A, et al. Psychometric evaluation of the polish adaptation of the hill-bone compliance to high blood pressure therapy scale. BMC Cardiovasc Disord 2016;16:87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet (London, England) 2012;380:2224–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Gleason-Comstock J, Streater A, Goodman A, et al. Willingness to pay and willingness to accept in a patient-centered blood pressure control study. BMC Health Serv Res 2017;17:538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Wang J, Zhang L, Wang F, et al. Prevalence, awareness, treatment, and control of hypertension in China: results from a national survey. Am J Hypertens 2014;27:1355–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Yang Q, Chang A, Ritchey MD, et al. Antihypertensive medication adherence and risk of cardiovascular disease among older adults: a population-based cohort study. J Am Heart Assoc 2017;6:e006056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Vrijens B, De Geest S, Hughes DA, et al. A new taxonomy for describing and defining adherence to medications. Br J Clin Pharmacol 2012;73:691–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Shehab A, Elnour AA, Swaidi SA, et al. Evaluation and implementation of behavioral and educational tools that improves the patients’ intentional and unintentional non-adherence to cardiovascular medications in family medicine clinics. Saudi Pharm J 2016;24:182–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Akhu-Zaheya LM, Shiyab WY. The effect of short message system (SMS) reminder on adherence to a healthy diet, medication, and cessation of smoking among adult patients with cardiovascular diseases. Int J Med Inform 2017;98:65–75. [DOI] [PubMed] [Google Scholar]
- [10].Christensen A, Osterberg LG, Hansen EH. Electronic monitoring of patient adherence to oral antihypertensive medical treatment: a systematic review. J Hypertens 2009;27:1540–51. [DOI] [PubMed] [Google Scholar]
- [11].Hou MY, Hurwitz S, Kavanagh E, et al. Using daily text-message reminders to improve adherence with oral contraceptives: a randomized controlled trial. Obstet Gynecol 2010;116:633–40. [DOI] [PubMed] [Google Scholar]
- [12].Gupta P, Patel P, Horne R, et al. How to screen for non-adherence to antihypertensive therapy. Curr Hypertens Rep 2016;18:89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Piette JD, Datwani H, Gaudioso S, et al. Hypertension management using mobile technology and home blood pressure monitoring: results of a randomized trial in two low/middle-income countries. Telemed J E Health 2012;18:613–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].He W, Bonner A, Anderson D. Patient reported adherence to hypertension treatment: a revalidation study. Eur J Cardiovasc Nurs 2016;15:150–6. [DOI] [PubMed] [Google Scholar]
- [15].Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care 1986;24:67–74. [DOI] [PubMed] [Google Scholar]
- [16].Morisky DE, Ang A, Krousel-Wood M, et al. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens (Greenwich, Conn) 2008;10:348–54. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- [17].Lahdenpera TS, Wright CC, Kyngas HA. Development of a scale to assess the compliance of hypertensive patients. Int J Nurs Stud 2003;40:677–84. [DOI] [PubMed] [Google Scholar]
- [18].Kim MT, Hill MN, Bone LR, et al. Development and testing of the hill-bone compliance to high blood pressure therapy scale. Prog Cardiovasc Nurs 2000;15:90–6. [DOI] [PubMed] [Google Scholar]
- [19].Cate H, Bhattacharya D, Clark A, et al. A comparison of measures used to describe adherence to glaucoma medication in a randomised controlled trial. Clin Trials (London, England) 2015;12:608–17. [DOI] [PubMed] [Google Scholar]
- [20].AlGhurair SA, Hughes CA, Simpson SH, et al. A systematic review of patient self-reported barriers of adherence to antihypertensive medications using the world health organization multidimensional adherence model. J Clin Hypertens (Greenwich Conn) 2012;14:877–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Jank S, Bertsche T, Schellberg D, et al. The A14-scale: development and evaluation of a questionnaire for assessment of adherence and individual barriers. Pharm World Sci 2009;31:426–31. [DOI] [PubMed] [Google Scholar]
- [22].Lee GK, Wang HH, Liu KQ, et al. Determinants of medication adherence to antihypertensive medications among a Chinese population using Morisky Medication Adherence Scale. PloS One 2013;8:e62775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Tang H, Zhu J, He H, et al. Development and evaluation of a new therapeutic adherence scale for hypertensive patients. J Third Military Med Univ (in Chinese) 2011;33:1400–3. [Google Scholar]
- [24].Akoko BM, Fon PN, Ngu RC, et al. Knowledge of hypertension and compliance with therapy among hypertensive patients in the Bamenda health district of Cameroon: a cross-sectional study. Cardiol Ther 2017;6:53–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Pan J, Lei T, Hu B, et al. Post-discharge evaluation of medication adherence and knowledge of hypertension among hypertensive stroke patients in northwestern China. Patient Prefer Adherence 2017;11:1915–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Lee HJ, Jang SI, Park EC. Effect of adherence to antihypertensive medication on stroke incidence in patients with hypertension: a population-based retrospective cohort study. BMJ Open 2017;7:e014486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Schulz M, Krueger K, Schuessel K, et al. Medication adherence and persistence according to different antihypertensive drug classes: a retrospective cohort study of 255,500 patients. Int J Cardiol 2016;220:668–76. [DOI] [PubMed] [Google Scholar]
- [28].Gupta P, Patel P, Strauch B, et al. Risk factors for non-adherence to antihypertensive treatment. Hypertension 2017;69:1113–20. [DOI] [PubMed] [Google Scholar]
- [29].Lauffenburger JC, Landon JE, Fischer MA. Effect of combination therapy on adherence among US patients initiating therapy for hypertension: a cohort study. J Gen Intern Med 2017;32:619–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Fontil V, Bibbins-Domingo K, Kazi DS, et al. Simulating strategies for improving control of hypertension among patients with usual source of care in the United States: the blood pressure control model. J Gen Intern Med 2015;30:1147–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Alhaddad IA, Hamoui O, Hammoudeh A, et al. Treatment adherence and quality of life in patients on antihypertensive medications in a Middle Eastern population: adherence. Vasc Health Risk Manag 2016;12:407–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Yue Z, Bin W, Weilin Q, et al. Effect of medication adherence on blood pressure control and risk factors for antihypertensive medication adherence. J Eval Clin Pract 2015;21:166–72. [DOI] [PubMed] [Google Scholar]
- [33].Arbuckle C, Tomaszewski D, Aronson BD, et al. Evaluating factors impacting medication adherence among rural, urban, and suburban populations. J Rural Health 2018;34:339–46. [DOI] [PubMed] [Google Scholar]
- [34].Yassine M, Al-Hajje A, Awada S, et al. Evaluation of medication adherence in Lebanese hypertensive patients. J Epidemiol Glob Health 2016;6:157–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Zhang X, Zhu M, Dib HH, et al. Knowledge, awareness, behavior (KAB) and control of hypertension among urban elderly in western China. Int J Cardiol 2009;137:9–15. [DOI] [PubMed] [Google Scholar]
- [36].Abegaz TM, Shehab A, Gebreyohannes EA, et al. Nonadherence to antihypertensive drugs: a systematic review and meta-analysis. Medicine 2017;96:e5641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Nguyen TP, Schuiling-Veninga CC, Nguyen TB, et al. Adherence to hypertension medication: quantitative and qualitative investigations in a rural Northern Vietnamese community. PloS One 2017;12:e0171203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Kim Y, Kong KA. Do hypertensive individuals who are aware of their disease follow lifestyle recommendations better than those who are not aware? PloS One 2015;10:e0136858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Santa Helena ETNM, Eluf-Neto J. Evaluation of care provided for people with arterial hypertension in family health strategy services. Saúde Soc 2010;19:614–26. [Google Scholar]
- [40].Murphy GK, McAlister FA, Weir DL, et al. Cardiovascular medication utilization and adherence among adults living in rural and urban areas: a systematic review and meta-analysis. BMC Public Health 2014;14:544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Magnabosco P, Teraoka EC, de Oliveira EM, et al. Comparative analysis of non-adherence to medication treatment for systemic arterial hypertension in urban and rural populations. Rev Lat Am Enfermagem 2015;23:20–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Li J, Shi L, Liang H, et al. Urban-rural disparities in health care utilization among Chinese adults from 1993 to 2011. BMC Health Serv Res 2018;18:102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Malik A, Yoshida Y, Erkin T, et al. Hypertension-related knowledge, practice and drug adherence among inpatients of a hospital in Samarkand, Uzbekistan. Nagoya J Med Sci 2014;76:255–63. [PMC free article] [PubMed] [Google Scholar]
- [44].He Z, Cheng Z, Shao T, et al. Factors influencing health knowledge and behaviors among the elderly in rural China. Int J Environ Res Public Health 2016;13:975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Hultgren F, Jonasson G, Billhult A. From resistance to rescue–patients’ shifting attitudes to antihypertensives: a qualitative study. Scand J Prim Health Care 2014;32:163–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Neutel CI, Campbell N. Changes in lifestyle after hypertension diagnosis in Canada. Can J Cardiol 2008;24:199–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Kang CD, Tsang PP, Li WT, et al. Determinants of medication adherence and blood pressure control among hypertensive patients in Hong Kong: a cross-sectional study. Int J Cardiol 2015;182:250–7. [DOI] [PubMed] [Google Scholar]
- [48].Chung N, Baek S, Chen MF, et al. Expert recommendations on the challenges of hypertension in Asia. Int J Clin Pract 2008;62:1306–12. [DOI] [PubMed] [Google Scholar]
- [49].Su TT, Majid HA, Nahar AM, et al. The effectiveness of a life style modification and peer support home blood pressure monitoring in control of hypertension: protocol for a cluster randomized controlled trial. BMC Public Health 2014;14Suppl 3:S4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Scisney-Matlock M, Bosworth HB, Giger JN, et al. Strategies for implementing and sustaining therapeutic lifestyle changes as part of hypertension management in African Americans. Postgrad Med 2009;121:147–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


