Summary:
An unusual complication of percutaneous fixation of a schapoid fracture in a 36-year-old man is described. After this surgery, the patient complained of numbness and tingling within the median nerve distribution and thenar weakness. An Electromyography showing moderate CTS had led to carpal tunnel decompression, which resulted unsuccessful. When the patient presented to us, both sensory and motor median nerve impairment were present, interfering with his professional activity. A computed tomography scan performed to assess the scaphoid screw position, showed that the screw had been placed volar to the scaphoid, adjacent to the median nerve. Surgery confirmed median nerve compression by the screw, especially during complete wrist extension. The surgical removal of the screw led to immediate improvement of both the motor and sensory functions of the nerve, with complete clinical restoration of nerve function and resolution of the symptoms 2 months postoperatively.
Scaphoid fractures are common after falls on the outstretched wrist, and are the most frequent within the carpal bones. Conservative treatment was historically destined to nondisplaced ones, whereas surgery is required when the fragments are displaced, to increase the chances of healing. Over time, the operative treatment with percutaneous fixation has also been proposed instead of the cast for the simple, nondisplaced fractures, to improve bone consolidation and reduce the immobilization period. This has many advantages, such as an early return to work and recreational activities.1
Nevertheless, a risk of injury to the surrounding structures exists. Depending on whether a volar or dorsal approach is used, lesions of the flexor carpi radialis tendon, the superficial volar branch of the radial artery, the superficial radial nerve, the tendons of the first dorsal compartment, and the recurrent motor branch of the median nerve can occur.2 These risks increase if the procedure is performed by surgeons without sufficient experience.
In this report, the authors present a late complication of a percutaneous fixation of a nondisplaced scaphoid fracture with a misplaced screw.
CASE REPORT
A right-handed, 36-year-old male dentist with a Herbert’s type B2 fracture of the right scaphoid was treated in another institution with a percutaneaous screw from a volar approach. The 8-week x-rays showed the complete healing of the scaphoid, even in the presence of a misplaced screw from the beginning. Two years later, the patient developed a symptomatology of carpal tunnel compression, and a surgical decompression was performed, with no clinical improvement. Subsequently, the patient presented to our institution because of progressive worsening of his neuropathic median nerve symptoms, with a significant impairment in his usual professional and day-life activities.
At the clinical examination, thumb opposition strength was graded M4 according to the Medical Research Council Scale, and there was diminished sensation to light touch over the right index and middle finger and diminished protective sensation in the thumb, measured with the Semmes Weinstein monofilaments. The patient also complained of burning pain within the median nerve distribution area, triggered by full active extension of the wrist, radiating from the wrist to his thumb. Tinel’s sign was also positive over the median nerve at the wrist level, particularly close to the distal portion of the flexor carpi radialis. The EMG identified a markedly increased latency of response of the opponens pollicis muscle. Based on the patient’s clinical history, a computed tomography (CT) scan was also performed to rule out symptoms potentially caused by scaphoid screw protrusion. The CT revealed that the screw was completely out of the scaphoid bone, adjacent to the volar surface of the scaphoid (Fig. 1), near the median nerve. Scaphoid fracture healing was confirmed on CT. The patient underwent urgent screw removal (Fig. 2), and surgical exploration identified that compression of the radial fibers of the median nerve was caused by the distal portion of the screw, during complete extension of the wrist. However, the median nerve appeared intact. Scar tissue was also identified around the screw, in close proximity of the median nerve. The surgical removal of the screw led to immediate improvement of both the motor and sensory functions of the median nerve, with complete clinical restoration of nerve function and resolution of the symptoms 2 months postoperatively.
Fig. 1.
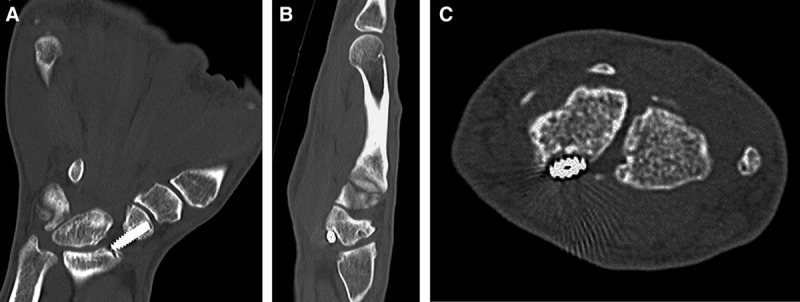
CT showing the screw out of the scaphoid bone. A, Frontal view. B, Lateral view. C, Transversal view.
Fig. 2.

Screw removal.
DISCUSSION
After our operative findings, we can hypothesize that the screw, observed along the volar aspect of the scaphoid, was probably misplaced since the beginning. However, it may have provided sufficient stability to the fracture to aid its healing, acting as a guide. The distal part of the screw appeared to protrude volarly during the extension of the wrist, and the surrounding scar tissue may have contributed to the local median nerve compression, leading over time to a neuropraxia.
Compression of a nerve typically results in nerve edema, ischemia, thinning of the myelin sheath and focal demyelination, triggering neurophatic pain, sensory deficit, and motor impairment. Because neuropraxia is an injury to the myelin sheath only, recovery is expected with a correct treatment,3 as demonstrated by the favorable course of our patient after removal of the screw and fibrosis.
Within scaphoid fractures, the median nerve can be damaged in some ways. A displaced fracture could determine an acute4 or progressive nerve compression,5,6,7 whereas in nondisplaced ones, this eventuality could occur by the fracture hematoma.8 Furthermore, when surgery is performed, the recurrent branch of the median nerve may be placed at risk in percutaneous procedures if a volar approach is used.2
In this case, the nerve underwent a progressive compression without direct lesions, caused by both the protrusion of the screw and by the reactive scar tissue around it. Considering the clinical history and the previous osteosynthesis, this should have been suspected before performing the carpal tunnel decompression. The persistency of neurological symptoms confirmed the misdiagnosis.
In the clinical practice, expecially for surgeons not accustomed to this type of interventions, attention must be payed to the positioning and the length of the screw, which should be shorter than the measured guidewire to avoid the protrusion from the far cortex.9 Furthermore, when a carpal tunnel syndrome is diagnosed in the presence of plates or screws previously positioned, a secondary compression should be suspected and further investigations have to be considered, to plan the proper surgery.
CONCLUSIONS
In this case report, we focused the attention on the late onset of a median nerve symptomatology, because of screw malposition and excessive lengths, with subsequent exuberant scar tissue formation that determined a secondary carpal tunnel syndrome. The diagnosis was initially missed and an unnecessary decompression was performed, delaying and potentially compromise patient recovery. Inexperienced surgeons must consider the whole clinical history of the patient to choose the appropriate investigations and get the correct diagnosis and treatment.
Footnotes
Published online 25 June 2019.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
REFERENCES
- 1.Schädel-Höpfner M, Marent-Huber M, Gazyakan E, et al. Acute non-displaced fractures of the scaphoid: earlier return to activities after operative treatment. A controlled multicenter cohort study. Arch Orthop Trauma Surg. 2010;130:1117–1127. [DOI] [PubMed] [Google Scholar]
- 2.Evans S, Brantley J, Brady C, et al. Structures at risk during volar percutaneous fixation of scaphoid fractures: a cadaver study. Iowa Orthop J. 2015;35:119–123. [PMC free article] [PubMed] [Google Scholar]
- 3.Griffin MF, Malahias M, Hindocha S, et al. Peripheral nerve injury: principles for repair and regeneration. Open Orthop J. 2014;8:199–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kannan A, Khatri D, Trikha V, et al. Isolated volar fracture-dislocation of the scaphoid with acute carpal tunnel syndrome: a case report. Acta Orthop Belg. 2010;76:552–554. [PubMed] [Google Scholar]
- 5.Lee DJ, Fechter J, Schnall SB. Old displaced fracture of the scaphoid. An unusual cause of carpal tunnel syndrome. Orthop Rev. 1993;22:842–844. [PubMed] [Google Scholar]
- 6.Leung YF, Wai YL, Kam WL, et al. Solitary dislocation of the scaphoid. From case report to literature review. J Hand Surg Br. 1998;23:88–92. [DOI] [PubMed] [Google Scholar]
- 7.Takami H, Takahashi S, Ando M. Dislocation of the carpal scaphoid associated with median nerve compression: case report. J Trauma. 1992;33:921–923. [DOI] [PubMed] [Google Scholar]
- 8.Olerud C, Lönnquist L. Acute carpal tunnel syndrome caused by fracture of the scaphoid and the 5th metacarpal bones. Injury. 1984;16:198–199. [DOI] [PubMed] [Google Scholar]
- 9.Meyer C, Chang J, Stern P, et al. Complications of distal radial and scaphoid fracture treatment. J Bone Jt Surg. 2013;95:1517–1526 [DOI] [PubMed] [Google Scholar]


