Supplemental Digital Content is available in the text.
Abstract
Background:
Nonsurgical rhinoplasty with hyaluronic acid (HA) has gained popularity due to its efficacy and minimal downtime. From a structural standpoint, it is like performing a tridimensional reshaping where only enhancement by grafts is allowed. To date, indications, technique, and products are still debated. The aim of this study is to describe the author’s experience with nonsurgical nasal reshaping, focusing on the indications and maneuvers to safely achieve, by mean of HA, the grafts previously described for surgical rhinoplasty.
Materials and Methods:
A total of 70 consecutive patients underwent nonsurgical rhinoplasty using the same type of HA. The rhinoplasty module of FACE-Q was administered to all patients before treatment and 15 days posttreatment. Statistical analysis was performed.
Results:
No complication was experienced. Two (2.8%) patients required a retouch after 15 days for further dorsal correction. There was a statistically significant difference between preoperative and postoperative values in all domains and overall scores of the rhinoplasty module of FACE-Q.
Conclusions:
The graft-based technique proved to be safe, effective, and reliable. It may allow correction of selected nasal defects with reduced cost and minimal downtime.
INTRODUCTION
Nasal defects may often be a major concern for the cosmetic patient, due to their prominent exposure. Consistently, surgical rhinoplasty was the third most performed surgical procedure in 2017, with almost 219.000 cases in the United States alone.1 Although surgical rhinoplasty still stands as the gold standard to achieve both functional and aesthetic nasal improvements, nowadays patients often seek minimally invasive procedure with lower cost and downtime. Consequently, nasal reshaping with hyaluronic acid (HA) has gained increased popularity. However, there is still debate about indications, technique, and ideal product to address nasal deformities and prevent complications. In contrast, a solid body of evidence is available about the indications for cartilage grafts in surgical rhinoplasty. From a structural standpoint, nonsurgical rhinoplasty with filler is a 3-dimensional reshaping where only tissue enhancement is allowed: HA is placed instead of cartilage graft to account for tissue redistribution. The aim of this study is to describe the author’s experience with nonsurgical nasal reshaping, focusing on the type of defect and the maneuvers to safely achieve, by means of HA, the grafts previously described for surgical rhinoplasty.
MATERIALS AND METHODS
Seventy consecutive patients underwent nonsurgical rhinoplasty between January 2016 and June 2018. The study followed the guidelines of the Declaration of Helsinki. Demographic data are summarized in Table 1. Contraindications for treatment were pregnancy, breast feeding, autoimmune diseases, local infection, herpes, or inflammation. Juvederm 4 (Allergan plc, Dublin, Ireland) was used in all cases. All the injections were performed by the same author. The rhinoplasty module of FACE-Q was administered to all patients preoperatively and 15 days postoperatively. Wilcoxon signed rank and paired t test were used for statistical analysis. Only P values <0.05 were considered as statistically significant. Statistical analysis was performed using the STATA software.
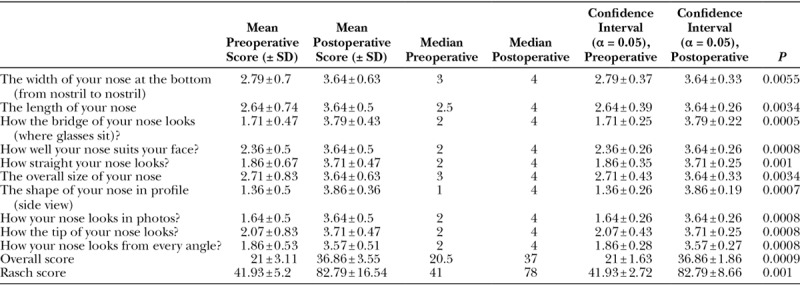
Table 1.
FACE-Q Questionnaire Results
VASCULAR ANATOMY AND DANGER ZONES
Branches of the ophthalmic and facial arteries supply the external nose. The dorsal nasal artery arises from the ophthalmic artery, together with the supratrochlear artery and the supraorbital artery, and runs over the dorsal surface of the nasal bone, reaching the nasal tip, where it contributes to the arterial arcade of the nasal tip.2,3 The lateral nasal artery branches off the facial artery or angular artery (distal branch of the facial artery that anastomoses the facial artery directly with the ophthalmic artery) and proceeds medially above the alar groove to meet the columellar artery, thus giving rise to the alar arcade (along the cephalic margin of the lateral crura).2,3 The columellar artery supplies the base of the nose and branches off the facial artery or the superior labial artery. In some cases, branches of both the dorsal nasal artery and the lateral nasal artery anastomoses with the contralateral ones.4 The vascular anatomy of the nose includes several anastomoses; thus, the widespread embolism through the connected blood vessels results in skin necrosis with a geographic pattern.5 The major arterial, venous, and lymphatic vasculature courses in or above the musculoaponeurotic layer of the nose.3 Dorsal nasal arteries (1 mm in diameter) run under the superficial musculoaponeurotic system plane at the nasal root and gradually ascend superiorly from the nasal fascia plane to the subcutaneous plane at the lower part of the nose. Large vessels are located above the muscle layer.3 Only smaller perforating vessels branching off the lateral and dorsal nasal arteries course between the muscoloaponeurotic layer and the cartilage or bone.3 Danger zones are shown in figure, Supplemental Digital Content 1, which displays the vascular danger zones: green: low risk; yellow: moderate risk; red: high risk, http://links.lww.com/PRSGO/B60.
TOPOGRAPHIC LANDMARKS
Dorsum
On the lateral view, the nasion (figure, Supplemental Digital Content 2, left, which displays nasion positioning. Left, red line: nasion position. Right, red line: planned nasion relocation; blue area: area to be filled to camouflage the dorsal hump, http://links.lww.com/PRSGO/B61) and the starting point of the dorsal hump must be taken into account prior to considering nonsurgical correction. The nasion is the deepest point of the nasofrontal angle. The aim of the injections is to fill the triangular space between the nasion, the most projecting point of the dorsal hump and the new nasion (figure, Supplemental Digital Content 2, right, which displays nasion positioning. Left, red line: nasion position. Right, red line: planned nasion relocation; blue area: area to be filled to camouflage the dorsal hump, http://links.lww.com/PRSGO/B61). In white people, the nasion should be ideally located between the lashes and crease line, 2–3 mm higher than the lashes when looking forward, protruding about 11–14 mm from the upper eyelid.6 Generally, if preoperatively located lower and/or protruding less than such value, the patient is a good candidate for dorsal hump correction by mean of HA injection. In cases of higher nasion location and/or severe hump protrusion, nonsurgical rhinoplasty could not be a viable option unless the patient is compliant with a postoperative high, straight nose. On the frontal view, the dorsal lines and the lateral wall inclinations must be assessed.
Tip
On the lateral view, the following 5 main characteristics must be assessed: the supratip break, the lobulocolumellar angle, the columellar–lobule ratio, the nasolabial angle (figure, Supplemental Digital Content 3, which displays topographic landmarks. STB: supratip break; LC: lobulocolumellar angle; NL: nasolabial angle, http://links.lww.com/PRSGO/B62), and caudal tip retraction when smiling. The supratip break is the transition point between dorsum and tip, and it should be slightly concave. The ideal nasolabial angle is 100 degrees in men and 105 degrees in women, whereas the lobulocolumellar angle should be 40–45 degrees. The columellar–lobule ratio should be 2:1. On the frontal view, the distance between the tip defining points is paramount. Ideally, in white people, it should be 6–8 mm for females and 8–10 mm for males. Moreover, it should be of the same width as the parallel “dorsal lines” and philtral columns.
SURGICAL TECHNIQUE
Anesthetic cream (EMLA; AstraZeneca, Basiglio, MI, Italy) is applied 20 minutes before the procedure. Meticulous disinfection is performed with chlorhexidine gluconate 2%.
Dorsum
With the patient lying down, the lowest point of the dorsum is visualized and injected. To reduce the risk for intravascular injection and HA displacement, the author performs the “pinch, push, and pull” (3P) and the “tripod” maneuvers. The dorsal skin is pinched medially with the index and thumb fingers of the nondominant hand, and then, the 2 fingers slide pushing the skin laterally and compressing it onto the nasal bone. The needle is then inserted on the midline, with a 90-degree inclination, until the periosteum or the perichondrium is touched. With the needle inserted, 2–3 seconds are waited and, then, the index and thumb fingers slightly slide medially pulling the skin up, followed by the waiting of another 3 seconds. Subsequently, HA is slowly injected and gently massaged. Two more dorsal injections are performed at least, just above and below the first one, to provide a gentle curve to the dorsum. To avoid cranial or caudal dislocation of the HA the tripod maneuver is done: the thumb and middle (or index) fingers perform the 3P whereas the index (or middle) finger compresses cranially or caudally to prevent displacement of HA. Lateral deviations are addressed similarly, being cautious of the dorsal nasal artery. All dorsal injections are performed with a 90-degree inclination to minimize the subdermal course of the needle, thus reducing the risk for vessel incannulation. The beveling of the needle is oriented toward the finger compressing the dorsum. The medial dorsum is slightly overcorrected, whereas injection is more conservative laterally. The injected area is gently massaged to avoid bumps. Except for very rare and selected cases, the dorsum is not augmented below the hump to avoid blunting of the supratip break. The most commonly performed dorsal “grafts” are shown in Figures 1 and 2 and figure, Supplemental Digital Content 4, which displays dorsal onlay injection: it allows an increase of the nasal dorsum, http://links.lww.com/PRSGO/B63.
Fig. 1.
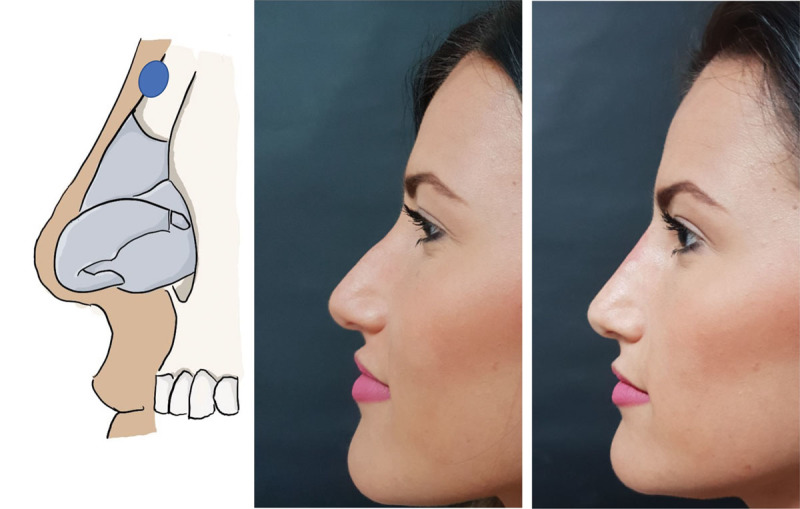
Radix injection: the most commonly used dorsal injection in patients seeking nonsurgical rhinoplasty. It allows to camouflage the dorsal hump, redefining the radix breakpoint cephalad. A total of 0.2 cm3 of HA were used in this patient.
Fig. 2.

Dorsal sidewall onlay injection: it allows to camouflage irregularities, depressions, concave deviations, and collapse of the upper lateral cartilages. A total of 0.3 cm3 of HA were used in this patient.
Tip
Nasolabial angle
The naslabial angle is addressed first. The white lip is retracted downward pushing on the midline with the index finger of the nondominant hand, and the needle is inserted with a 45-degree inclination addressing the inferior border of the nasal spine. Before starting the injection, the index and thumb fingers of the nondominant hand should pinch the columellar base to avoid lateral displacement of the product. Injection should start submuscularly with the needle touching the nasal spine. Besides providing tip support, the submuscular injection also lengthens the depressor septi muscle, thus reducing its retracting effect on the tip. Injection is continued in a retrograde fashion, intra- and premuscularly, with the thumb finger of the nondominant hand cranially retracting the tip to increase the virtual filling space between the nasal spine and the columellar footplate. Such a procedure, besides reducing tip retraction when smiling, induces upward tip rotation (more than elongation) due to the fibrous adherences between the upper and lower lateral cartilages acting as a hinge.
Tip and lobule projection
Supratip break, lobule elongation, and lobulocolumellar angle are addressed with a “retraction–pinching” maneuver. The new supratip break is visualized by cranially retracting the lobule with the middle finger of the nondominant hand, using the thumb finger as a hinge on the nasal dorsum. The needle enters the skin midline, exactly at the desired point of the supratip break, sliding just above the cartilage and pointing toward the interdomal space. With the middle finger still retracting the lobule, the thumb and index fingers of the nondominant hand pinch the domes. With the retraction component of the maneuver, a virtual space between the cartilage and subcutaneous tissues is created, whereas the pinching prevents lateral domal displacement, resulting in a boxy tip. In the cases where lateral domal displacement is wanted, the pinching component of the maneuver may be avoided. Aspiration is always performed. Interdomal HA retrograde injection is performed along the inferior two thirds of the needle course, as injection in the upper third could result in polly beak deformity or blunting of the supratip break.
Tip definition
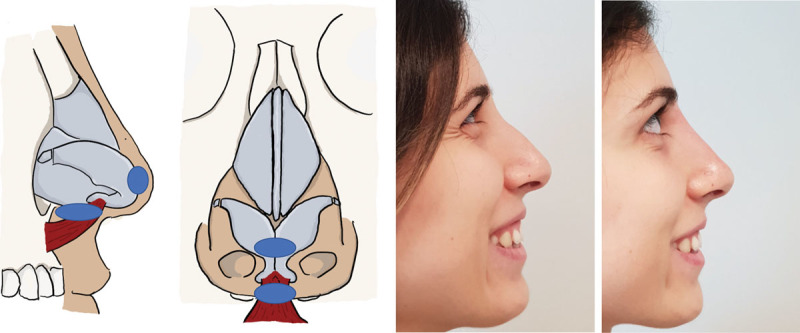
The possible grafts to be performed are shown in Figures 3–5 and in figure, Supplemental Digital Content 5, which displays anchor injection. The injection from the nasal spine to the columellar base accounted for the reduced tip retraction when smiling, http://links.lww.com/PRSGO/B64, and figure, Supplemental Digital Content 6, which displays onlay tip injection, http://links.lww.com/PRSGO/B65. In cases of severe tip hypoplasia, when further tip elongation or supratip break is needed, an anchor graft is performed. The needle is inserted at the infratip lobule, and for each side, it slides supraperichondrial to the dome. Injection is performed in a retrograde fashion, releasing less HA cranially and more caudally. Performing the central portion of the anchor by the same access at the infratip lobule may often result in cranial product displacement, thus blunting the supratip break or rounding the tip. As a consequence, in such cases or when a shield graft is needed, the author creates this central portion with a cap or onlay tip graft placed by central interdomal injection perpendicular to the skin. The simplified algorithm followed for the graft choice is reported in Figure 6.
Fig. 3.
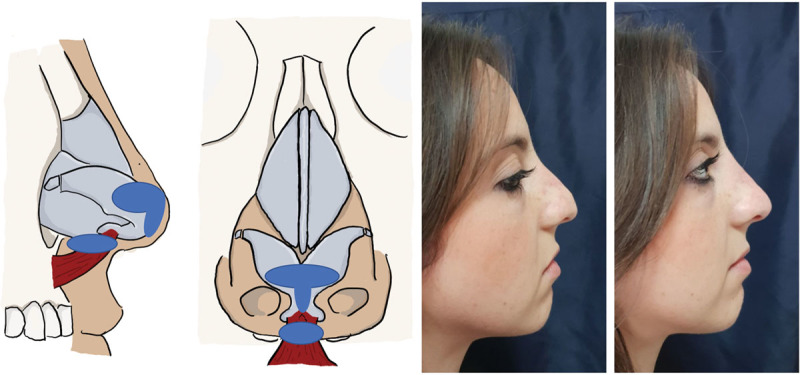
Anchor injection: the most versatile graft in tip reshaping with nonsurgical rhinoplasty. It allows to increase tip and lobule projection and to define the supratip break and the lobulocolumellar angle. The patient also underwent HA retrograde injection from the nasal spine to the columellar base, as described in the text, that may be considered as a midway between columellar plumping graft and strut. A total of 0.35 cm3 of HA were used for tip contouring (including the nasolabial angle injection).
Fig. 5.
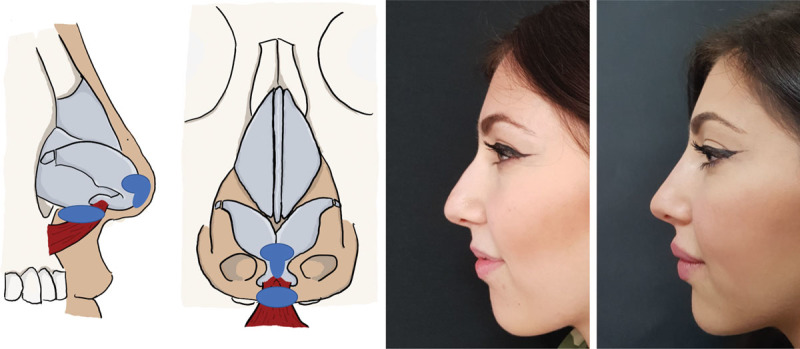
Shield injection: it increases tip projection, improves the infratip lobule, and defines the tip and the lobulocolumellar angle. A total of 0.3 cm3 of HA were used for tip contouring (including the nasolabial angle injection).
Fig. 6.
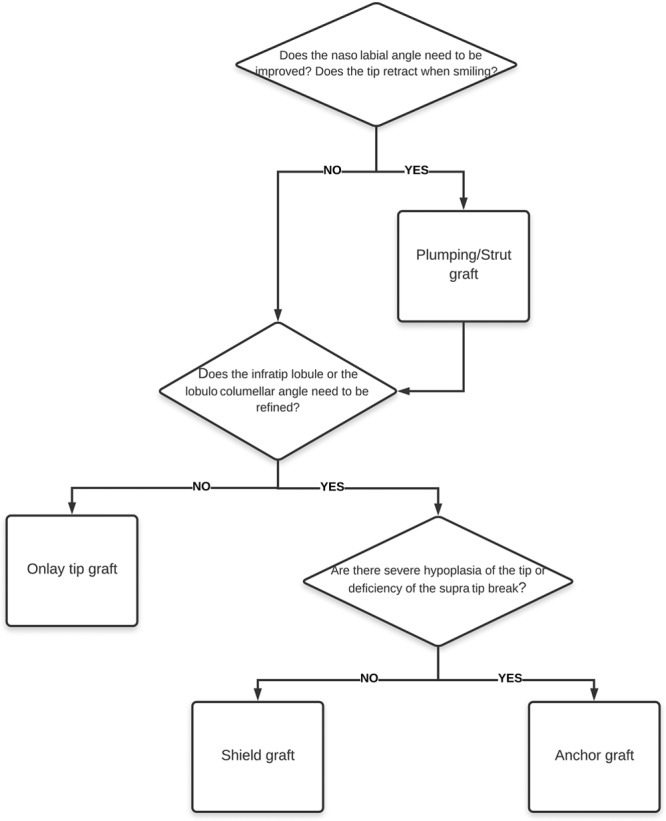
Flowchart for graft-based injections in nonsurgical rhinoplasty.
Fig. 4.
Onlay tip injection: it slightly increases tip projection. These patients also underwent HA retrograde injection from the nasal spine to the columellar base, as described in the text. A total of 0.25 cm3 of HA were used for tip contouring (including the nasolabial angle injection).
RESULTS
Nine patients were male, and 61 patients were female. The mean age of the patients was 27 (± 4.5) years. Four patients had correction following surgical rhinoplasty (inverted-V deformity and dorsal asymmetry). The quantity of injected HA ranged from 0.2 to 0.9 cm3. All the patients were followed up for at least 1 year. No complication was experienced. Two (2.8%) patients required a touchup after 15 days, both of them desiring further dorsal correction. All the patients filled the questionnaire. Results are summarized in Table 1. A statistically significant improvement was found in all domains of the rhinoplasty module of the FACE-Q and in the overall scores.
DISCUSSION
Nonsurgical rhinoplasty has gained increased popularity in the last decade. It allows addressing selected defects in both nonoperated and surgically treated noses, although with higher risk of complications in the latter cases.7 To date, there is still some debate about indications, technique, and what is the ideal product to use. Moreover, there were multiple reports of severe complications, such as infection and vascular compromise, resulting in blindness8 or skin necrosis.9 Detailed knowledge of nasal anatomy is paramount before using fillers in such area. The maneuvers herewith described by the authors, such as the 3P with the needle perpendicular to the skin or the retraction–pinching with retrograde injection at the tip, account for the vascular safety of the procedure while minimizing the risk for HA displacement. The pinching phase of the 3P maneuver, for example, allows for temporary reduction in the local blood flow and, consequently, vessel diameter, thus reducing the risk for incannulation. Injection should always be performed in the preperichondrial and preperiosteal layers. Obviously, the fewer times the needle is inserted, the less the risk for vascular incannulation or damage, thus the importance of achieving adequate reshaping with the lowest possible number of injections. Similarly, the subdermal course of the needle should be minimized by keeping it perpendicular and avoiding tunneling parallel to the cutaneous layer. It is important to wait the described time among needle insertion, aspiration, and injection, to assess eventual preinjection blanching. Postinsertion blanching before injection may result from reactive vasospasm due to vessel incannulation or trauma: in such cases, the needle must be withdrawn and reinserted slightly far from that point. Injections must always be delicate, slow, and with low pressure. An increase in the interstitial pressure may also result in reduced capillary perfusion or external arterial compression. Therefore, it is paramount to assess the reversibility of any blanching noticed during the procedure. With the above-described maneuvers, a slight postinjection blanching does not require any action if it solves spontaneously or with massaging in 30–60 seconds. If the skin is very adherent to deep tissues and/or looks tense after the procedure, the author prescribes ebastine 10 mg per os (PO) once a day for 3 days to reduce posttreatment edema. Subcision is never performed, because there is no need to create a pocket when injecting supraperichondrially and to avoid any vascular/tissue damage. Special care must be taken when performing injections to correct postsurgical deformities, because the vascularization may be compromised and the scar could reduce tissue compliance, thus making exceeding increases in the interstitial pressure more likely. In such instances, the authors wait at least 12 months postoperatively before performing any injection and prefer to err on the conservative side with the quantity of HA. Initial reports, dating back to the middle of the 1980s, described the use of bovine collagen and silicone to address nasal reshaping.9,10 In the following decades, the use of several types of HA and calcium hydroxyapatite11–13 was described. The main concern with calcium hydroxyapatite is the lack of an antidote if any complication occurs. In contrast, hyaluronidase may be used following HA injection. Moldability, viscosity, elasticity, hydrophilicity, and lasting are the main parameters to take into account when choosing the HA to inject. In this clinical series, the authors preferred Juvederm Ultra 4 due to its high cohesivity, long duration, and moldability, allowing both delicate and precise tip contouring and adequate dorsal support with low number of injections. Moreover, in previous studies, it showed high resistance to compression and lift capacity.14 In the author’s experience, a slight overcorrection of the dorsum should be achieved immediately after the procedure, to compensate for the immediate postinjection edema. In contrast, no overcorrection of the tip area should be attempted. Botulinum toxin was previously described as a further option to address tip retraction resulting from depressor septi nasi muscle hyperactivity. In the present study, it was not used because placing the HA under the muscle achieved adequate reduction in the tip-retracting effect. The graft-based nonsurgical rhinoplasty allowed pleasant aesthetic remodeling in both primary and postsurgical cases. Care must be taken in secondary noses with scarring or severe surgical anatomical changes. To the authors’ knowledge, the maneuvers described here were previously unreported in literature. The reported algorithm is derived from the literature-supported indications for cartilage grafts in rhinoplasty. Starting from the surgical knowledge, the author’s approach sets a correlation between the defect and the graft to be reproduced with HA. However, the technique has some limitations: no nasal reduction is possible and it is not suitable for severely deviated or crooked noses and for those patients with a high nasion. However, large noses may also be addressed: injecting along the midline and defining the tip medially allow increased projection, thus resulting in the optical illusion of a thinner nose. A similar optical effect is found on the lateral view: when the hump is hidden by a radix graft and the tip is rotated upward, the absence of irregular lines makes the nose look smaller, despite the tissue filling. Although long lasting, the effect is not permanent, thus needing retreatments. In the author’s experience with the above-cited HA, the clinical effect lasted longer following the second treatment compared with the first one. This may be due to some degree of collagen synthesis or lower degradation rate associated with repeated HA injection.15,16
CONCLUSION
The nonsurgical rhinoplasty technique described here proved to be safe, effective, and reliable with excellent patient-reported outcome. It may allow correction of selected nasal defects with reduced cost and minimal downtime.
Supplementary Material
Footnotes
Published online 25 June 2019.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
Supplemental digital content is available for this article. Clickable URL citations appear in the text.
REFERENCES
- 1.American Society of Plastic Surgeons. 2017 Plastic Surgery Statistics Report. Available at https://www.plasticsurgery.org/documents/News/Statistics/2017/plastic-surgery-statistics-full-report-2017.pdf. Accessed November 14, 2018.
- 2.Wu S, Pan L, Wu H, et al. Anatomic study of ophthalmic artery embolism following cosmetic injection. J Craniofac Surg. 2017;28:1578–1581. [DOI] [PubMed] [Google Scholar]
- 3.Toriumi DM, Mueller RA, Grosch T, et al. Vascular anatomy of the nose and the external rhinoplasty approach. Arch Otolaryngol Head Neck Surg. 1996;122:24–34. [DOI] [PubMed] [Google Scholar]
- 4.Pilsl U, Anderhuber F. The external nose: the nasal arteries and their course in relation to the nasolabial fold and groove. Plast Reconstr Surg. 2016;138:830e–835e. [DOI] [PubMed] [Google Scholar]
- 5.Moon HJ. Injection rhinoplasty using filler. Facial Plast Surg Clin North Am. 2018;26:323–330. [DOI] [PubMed] [Google Scholar]
- 6.Rolling KD. Mastering Rhinoplasty. 20102nd ed Berlin, Germany: Springer. [Google Scholar]
- 7.Kurkjian TJ, Ahmad J, Rohrich RJ. Soft-tissue fillers in rhinoplasty. Plast Reconstr Surg. 2014;133:121e–126e. [DOI] [PubMed] [Google Scholar]
- 8.Li X, Du L, Lu JJ. A novel hypothesis of visual loss secondary to cosmetic facial filler injection. Ann Plast Surg. 2015;75:258–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jasin ME. Nonsurgical rhinoplasty using dermal fillers. Facial Plast Surg Clin North Am. 2013;21:241–252. [DOI] [PubMed] [Google Scholar]
- 10.Webster RC, Hamdan US, Gaunt JM, et al. Rhinoplastic revisions with injectable silicone. Arch Otolaryngol Head Neck Surg. 1986;112:269–276. [DOI] [PubMed] [Google Scholar]
- 11.Rivkin A, Soliemanzadeh P. Nonsurgical injection rhinoplasty with calcium hydroxylapatite in a carrier gel (Radiesse): a 4-year, retrospective, clinical review. Cosmet Dermatol. 2009;22:619–625. [Google Scholar]
- 12.Kim P, Ahn JT. Structured nonsurgical Asian rhinoplasty. Aesthetic Plast Surg. 2012;36:698–703. [DOI] [PubMed] [Google Scholar]
- 13.Rauso R, Colella G, Zerbinati N, et al. Safety and early satisfaction assessment of patients seeking nonsurgical rhinoplasty with filler. J Cutan Aesthet Surg. 2017;10:207–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hee CK, Shumate GT, Narurkar V, et al. Rheological properties and in vivo performance characteristics of soft tissue fillers. Dermatol Surg. 2015;41(suppl 1):S373–S381. [DOI] [PubMed] [Google Scholar]
- 15.Quan T, Wang F, Shao Y, et al. Enhancing structural support of the dermal microenvironment activates fibroblasts, endothelial cells, and keratinocytes in aged human skin in vivo. J Invest Dermatol. 2013;133:658–667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang F, Garza LA, Kang S, et al. In vivo stimulation of de novo collagen production caused by cross-linked hyaluronic acid dermal filler injections in photodamaged human skin. Arch Dermatol. 2007;143:155–163. [DOI] [PubMed] [Google Scholar]


