Supplemental Digital Content is available in the text.
Summary:
In this review, we present the current role of nerve transfers in the management of nerve injuries. The outcome of a literature review comparing the results of nerve graft versus nerve transfer and the experience of select surgical societies’ members regarding experience and adoption of nerve transfer are reported. Nerve transfer publications have increased more than nerve graft or repair articles. The surgeon survey revealed an increase in nerve transfers and that more motor nerve transfers have been adopted into practice compared to sensory nerve transfers. The meta-analyses and systematic reviews of motor nerve transfers for shoulder and elbow function presented variable outcomes related to donor nerve selection. Comprehensive patient assessment is essential to evaluate the immediate functional needs and consider future reconstruction that may be necessary. Optimal outcome following nerve injury may involve a combination of different surgical options and more than one type of reconstruction. Nerve transfer is a logical extension of the paradigm shift from nerve repair and nerve graft and offers a new rung on the reconstruction ladder.
INTRODUCTION
Management of nerve injuries has advanced over the last century from limb amputation to tendon transfer to nerve repair to nerve graft. Nerve surgery has taken a quantum leap in the last 2 decades,1 moving into “the postgrafting era of nerve surgery.”2 The reintroduction of nerve transfers has created debate, controversy, and the opportunity to improve the management of patients with nerve injury.
Each surgical innovation provides a new option for improved functional recovery. The concept, development, and refinement of nerve transfers expands the surgical options and adds to the nerve reconstruction ladder. The impetus for change along this surgical path was clinical failures and disappointing outcomes as the existing techniques expanded and limits were exceeded.3,4 Nerve repairs yielded excellent results under ideal conditions when performed early, with sharp injuries, and close to end organ target, but failed as indications expanded to more proximal injuries with longer gaps. Poor clinical outcomes following nerve repair were the stimulus for alternative reconstructions such as bone excision to shorten long nerve gaps or nerve grafts to bridge these gaps. A nerve symposium at Duke University in 1978 illustrated the paradigm shift from nerve repair to nerve graft with presentations by Leonard Goldner on managing a long radial nerve gap with bone excision and by Raymond Curtis on a patient series with long nerve grafts with better results (Personal Communication, Hanno Millesi, 2012). As short nerve grafts yielded superior results compared to nerve repair under tension, the nerve graft length increased and when lengths exceeded critical intervals,5,6 clinical results deteriorated. Nerve transfer was the logical progression for nerve graft failure. Nerve transfer involves bringing an innervated donor nerve to a denervated target nerve to provide reinnervation to the target muscle or sensory end organ. When the donor nerve is closer to the target end organ, the nerve transfer will provide faster reinnervation and the opportunity for superior results with better sensorimotor function.
In this review, we present our perspective on the current role of nerve transfers in the management of nerve injuries. We performed a literature search of the publication history of the surgical management of nerve injuries and an assessment of the current surgical practice. The outcomes of the literature review comparing nerve graft and nerve transfer and the experience of several surgical societies’ members regarding current nerve transfer experience are reported.
METHODS
Publication Trends
An index search was performed in PubMed/Medline (1919–2016) using the keywords: “nerve repair,” “nerve graft,” “nerve transfer,” and “tendon transfer” to assess the publication numbers. A second search evaluated specific research and clinical articles by adding the keywords “animal” and “patient” to identify the basic science research from the clinical articles. The second keyword search was added due to PubMed/Medline databases not indexing early abstracts; thus, this search method would not reveal the appropriate research or clinical articles unless located within the article title. The search methodology scanned the publication titles and abstracts for a match to the keywords. Our institution librarian confirmed this approach to retrieve broad publication trends.
Outcomes in the Literature
To evaluate the outcomes following nerve graft or transfer, we performed a literature review, examining publications that specifically compared these surgical procedures in the upper extremity. PubMed/Medline and EMBASE databases were searched for English language articles containing “nerve graft” and “nerve transfer”. All primary clinical studies and meta-analyses and systematic reviews comparing reconstruction results were evaluated. We excluded studies which focused on pediatric/obstetrical palsies and those studies that did not directly examine differences between nerve graft and transfer outcomes. Our initial database searches were supplemented with the PubMed “Related Articles” section, and associated reference lists as relevant articles that did not appear in the initial keyword search were identified.
Each collected article was assessed for level/distribution of nerve injuries assessed, types of nerve repairs and transfers evaluated, number of patients included (original clinical studies)/number of studies included (meta-analysis/systematic reviews), and results of statistical comparisons between transfer and graft outcomes (ie, muscle strength and range of motion). We summarized these findings in tabular form for this literature review. Because we did not execute a meta-analysis or systematic review, no rigorous quantitative analyses were performed on the findings.
Current Surgical Practice
A survey was developed to assess the current use of nerve transfers. The questionnaire was pilot tested (relevance and readability) by several peripheral nerve surgeons. The 13-item survey included surgeon demographics and current use of nerve transfers. Consent information was provided and survey completion served as implied consent. Following our Institutional Review Board approval, the electronic survey was sent by email (between April 2017 and June 2017) to 5,436 email recipients in the American Society for Peripheral Nerve, PASSIOeducation.com, World Society for Reconstructive Microsurgery, American Society for Reconstructive Microsurgery, and American Society for Surgery of the Hand. De-identifiable data were imported to IBM SPSS Statistics 23.0 (Armonk, N.Y.) and categorical data were analyzed with Mantel-Haenszel χ2 test.
RESULTS
Publication Trends in the Literature
The total number of nerve repair, graft, and transfer and tendon transfer articles published from 1919 to 2016 are presented in Table 1 and the clinical articles for each technique in SDC1 (see figure, Supplemental Digital Content 1, which displays the PubMed/Medline search results and publication history for surgical paradigms, http://links.lww.com/PRSGO/B126).
Table 1.
PubMed/Medline Index Search Results for Surgical Paradigms in Respect to Research and Clinical Articles

Research articles focusing on nerve repair were more prevalent than for other nerve reconstructions or tendon transfers.
In a yearly comparison, the articles for each reconstruction type increased. Once modern nerve graft publications appeared in the literature in the 1970s, the numbers of nerve graft and repair articles were similar until the early 1990s. For most years from the mid-1990s to 2016, nerve repair articles were more frequent than nerve grafts. Only a small number of nerve transfer articles were identified before the 1990s, and in the mid-2000s, the nerve transfer articles increased more than the nerve graft or repair articles. At all time points, tendon transfer articles exceeded other types of nerve reconstruction.
Outcomes in the Literature
We identified 4 meta-analyses/systematic reviews and 9 original studies that met our inclusion criteria (Tables 2 and 3).
Table 2.
Meta-analyses and systematic reviews of nerve graft versus nerve transfer for restoration of elbow flexion strength and shoulder function*
Table 3.
Original articles examining outcomes nerve graft versus nerve transfer for restoration of function

Three meta-analyses/systematic reviews examined the results of brachial plexus nerve graft and transfer techniques, specifically elbow flexion and shoulder motion.4,7–9 One systematic review examined shoulder function following nerve graft and nerve transfer for isolated axillary nerve injuries and included a variety of nerve transfers. There were variable outcomes related to different donor nerve selection for elbow and shoulder function and these analyses suggest that certain distal transfers are equivalent to or better than graft (Table 2).
In high ulnar nerve injuries, an anterior interosseous nerve (AIN) to ulnar motor nerve transfer (end-to-end or end-to-side) was beneficial for restoration of intrinsic muscle strength, although the benefit of a supercharged end-to-side (SETS) transfer was apparent only for traumatic injuries.
We identified original studies comparing nerve graft and nerve transfers for a variety of upper extremity brachial plexus and terminal nerve injuries.10–18 Functional differences following these 2 reconstructions often failed to reach statistical significance and may be limited by low statistical power due to small sample sizes. When statistical significance was reached, results varied based on location of lesion and functional outcome examined (Table 3).
When suprascapular nerve (SSN) function was normal, results of axillary nerve graft and transfer were equivalent. When both nerves were injured, reconstruction with nerve transfer was superior to grafting. With musculocutaneous nerve injuries, results with nerve transfer were also superior to grafting.
Evaluation of Current Surgical Practices
There were 670 survey responses. The 12% response rate may be an underestimate due to multiple society membership and duplication in the total numbers from each society. Respondent demographics included: 64% (n = 430) orthopedic surgeons and 31% (n = 207) plastic and reconstructive surgeons. The majority of respondents (80%) practiced in North America. Of the 670 respondents, 93% (n = 623) perform nerve reconstruction with 72% (n = 447) of those performing nerve transfer surgery.
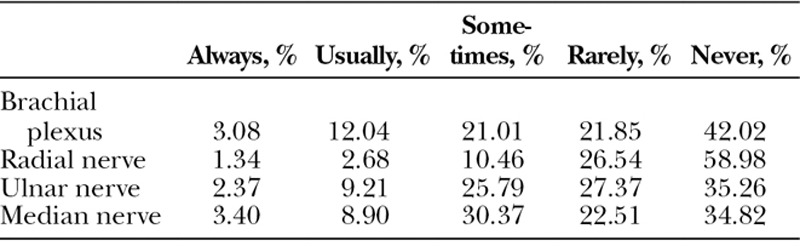
Of surgeons using nerve transfer surgery, 48% reported “always or usually” using transfers for brachial plexus injuries, 33% for ulnar nerve injuries, 17% for median nerve injuries, and 14% for radial nerve injuries (SDC2 and Table 4; see figure, Supplemental Digital Content 2, which displays the graphical representation of the trends in nerve transfer surgery for various peripheral nerve injuries, http://links.lww.com/PRSGO/B127). Surgeons (78%) reported increased use of motor nerve transfers in the past 3 years. Fewer surgeons reported using sensory nerve transfers (Table 5). The frequency of sensory nerve transfers, “always or usually,” was 15% with brachial plexus injuries (12% median, 12% ulnar, and 4% radial nerve). In the last 3 years, 37% reported increased use of sensory nerve transfers. There was no statistical difference in the increased use of motor or sensory nerve transfers among plastic, reconstructive, and orthopedic surgeons (χ2=2.05, P = 0.153; χ2=2.55, P = 0.110).
Table 4.
Frequency of Use of Nerve Transfer Surgery for Motor Nerve Injury
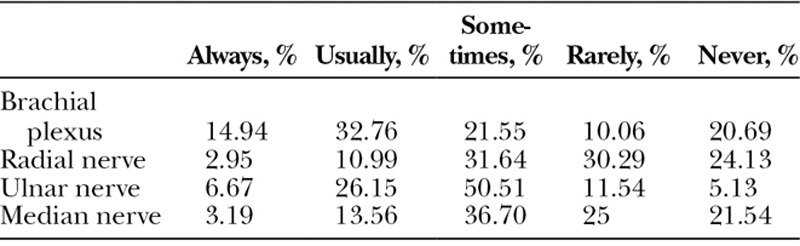
Table 5.
Frequency of Use of Nerve Transfer Surgery for Sensory Nerve Injury
The survey presented 2 case scenarios (sharp ulnar nerve injury either 9 cm proximal or 9 cm distal to the elbow) and respondents selected the operative procedures that would be considered, including nerve repair, transposition, autograft, allograft, and nerve transfer (end-to-end or end-to-side AIN to ulnar motor). For proximal elbow injury, 74% would consider nerve repair, 46% transposition, or 40% autograft; 57% would perform distal end-to-end nerve transfer; and 13% would allograft. For distal elbow injury, 79%, would consider nerve repair, 42%, autograft, or 31% transposition; 35% would perform distal end-to-side nerve transfer and 29% would perform an end-to-end nerve transfer; and 14% would allograft. There were significantly more surgeons using distal end-to-end nerve transfer for proximal injury than distal injury with end-to-side nerve transfer (χ2 = 63.48, P < 0.001).
DISCUSSION
The rise in publications regarding nerve transfers since the early 1990s has continued and parallels the reintroduction of nerve transfers as an alternative reconstruction. Following the early descriptions of successful nerve transfer for restoration of ulnar and musculocutaneous nerve function, an increasing number of unique nerve transfers and clinical outcomes have been described. Novel donor-recipient combinations, modified techniques of coaptation, including end-to-side, and sensory nerve transfers continue to evolve as surgeons seek solutions to difficult reconstructive challenges. Each new technique stimulates discussion, and comparisons to alternative reconstructive methods, to determine optimal management of nerve injuries.
Our surgeon survey and literature review provide insight into the change in surgical practice and increased use of nerve transfers. Outcome studies and reviews have compared results after nerve graft and nerve transfers and the conclusions vary depending on multiple factors (injury, patient, and surgical), including injury location (proximal brachial plexus versus distal nerves), specific function to be restored, and nerve transfer technique. Although studies frequently report data trends, many studies lack statistical power due to small samples, and seemingly large differences between outcomes fail to reach statistical significance. In our review, we included results that were statistically significant as the criterion for outcome differences. Therefore, in some cases our interpretation of the findings differed from authors’ conclusions, where authors discussed their results based on apparent statistical trends. In Tables 2 and 3, we have included detailed findings (often presented as a percentage reaching a threshold strength) and those trends failing to reach significance can still be appreciated.
Overall, the literature supports roles for both nerve transfer and graft reconstruction for upper extremity peripheral nerve lesions, although their relative utilities are best examined for different functions individually.
Shoulder Function
Shoulder function occurs via the coordinated actions of multiple musculoskeletal structures from the scapula and glenohumeral joint. Functional shoulder restoration following nerve injury has been difficult, and nerve transfers and grafts can generate useful shoulder motion.12–14,19 The SSN and axillary nerve are the predominant targets for muscle reinnervation. With isolated axillary nerve injuries and normal SSN function, overall postoperative results of the shoulder seem roughly equivalent following both nerve transfer and nerve graft techniques. With brachial plexus injuries, functional impairment is more severe and surgical results depend on reconstructed nerves.19 The SSN function is essential for overall shoulder function and traditional nerve graft reconstruction from C5 and C6 roots or the upper trunk has yielded only fair results. Nerve transfers utilizing the spinal accessory nerve to the SSN have not proven superior. This may be in part due to the importance of the scapular motion associated with the spinal accessory nerve and it is not “particularly” expendable. Efforts have been made to preserve function by performing an end-to-side transfer with crush injury via an anterior approach,20 and more distal end-to-end transfers via posterior approaches.21,22 No study has reported improved results for SSN nerve transfer compared to graft. Similarly, nerve transfers to the axillary nerve alone have not produced superior function compared to nerve grafting. As with SSN reconstruction, nerve transfer techniques are not standardized. The axillary nerve transfer is performed typically using a triceps branch of the radial nerve but variation has been reported in the recipient axillary nerve branch being reinnervated and the selected donor triceps branch. These specific technical differences may affect outcomes, although the extent of that impact remains unknown.
Whereas nerve transfer for isolated SSN or axillary nerve injuries has not improved results, simultaneous transfers have resulted in superior outcomes and are highlighted in the systematic review by Yang et al. of separate graft and transfer studies.9 When performed in combination, the restoration of SSN and axillary nerve function is superior following nerve transfer. Although the majority of studies assessing dual transfers utilized the spinal accessory nerve and a triceps branch of the radial nerve, there was variation in the specific details regarding the donors, recipients, and surgical approaches. The relative utility of grafts and transfers remains unclear if one of the preferred donors is unavailable (such as C5–C7 injuries).
Elbow Flexion
Elbow flexion reconstruction is less challenging than shoulder function, with superior results following both nerve graft and transfer. Although the literature supports the use of either single or double fascicular nerve transfer compared to nerve graft, variation in surgical technique impacts functional recovery and donor deficits.18 The advantages of these 2 nerve transfer techniques compared to nerve graft would be moderated with a more distal injury (such as at the lateral cord level or isolated musculocutaneous nerve) due to the similar reinnervation distances.
Nerve transfers for restoration of triceps function, accessory nerve injuries, hand function in lower brachial plexus injuries, and C7 tetraplegia patients have been reported in small sample studies.23,24 The results following these nerve transfers are encouraging but there are no comparison studies between techniques.
Distal Functions
With increasing distance between the nerve injury and target muscle, the time duration to muscle reinnervation increases. To minimize the time for neural regeneration, distal AIN transfers to reinnervate the ulnar intrinsic muscles were performed.25 Direct comparisons between ulnar nerve transfer and graft reconstructions have been performed. Generally, nerve transfers have been considered superior to nerve grafting for neurotmetic ulnar nerve injuries in the arm.15 This transfer has been reported using an end-to-side coaptation (supercharge technique) to supplement recovering axonotmetic injuries or repaired neurotmetic injuries in the proximal forearm26 or more proximal ulnar nerve injuries in patients with a Martin-Gruber anastomosis. The relative utility of this technique has been clinically reported.16
Radial and median nerve transfers are more recent developments, and there are no clinical studies directly comparing nerve graft and transfers. For radial nerve injuries, the debate continues over the use of nerve transfers versus tendon transfers.27 Tendon transfers have been used reliably for functional restoration when nerve graft or repair fails or is not feasible. Whereas tendon transfers provide rapid, consistent recovery, nerve transfers offer the opportunity for independent finger movement. Our nerve transfer results have been driven by modification of surgical technique, postoperative motor reeducation, and most importantly, appropriate patient selection. With different advantages and indications, the selection of tendon or nerve transfer remains patient-specific depending on individual needs. Similar to radial nerve palsy, distal median nerve lesions are often amenable to tendon transfer. However, nerve transfers have facilitated recovery of pronation and is effective for these otherwise challenging injuries. No comparative median nerve studies between nerve transfer and graft or tendon transfer were identified.
Innovation, Paradigm Shift, and Nerve Transfer
Changes in practice to manage patients with nerve injury are inevitable. Surgical innovation is initiated by pioneers, frequently from preeminent departments of surgery, who spend their careers developing, promoting, and teaching their techniques (eminence-based surgery). Each innovation has strong advocates and supporters and new paradigms are met with confrontation, criticism, skepticism, and anger. Thomas S. Kuhn identified a paradigm shift as a fundamental change in the practice of a scientific discipline, described as a scientific revolution.28 Kuhn emphasized that “failure of existing rules is the prelude to a scientific search for new ones and when enough information has accrued against a current paradigm, the scientific discipline is thrown into a state of crisis, and a new paradigm forms with new followers; frequently with an intellectual battle between the new paradigm supporters and old paradigm holdouts.” Kuhn outlines the challenge of transferring allegiance between paradigms and notes that resistance is inevitable.28 Kuhn continues, “Still, to say that resistance is inevitable and legitimate, that paradigm change cannot be justified by proof, is not to say that no arguments are relevant or that scientists cannot be persuaded to change their minds. Though a generation is sometimes required to effect the change, scientific communities over time have been converted to new paradigms.”
CONCLUSIONS
Many surgical options exist on the reconstructive ladder for functional restoration following nerve injuries and depending on the nerve, results may be maximized by different techniques. The literature suggests that for most nerve lesions, nerve transfers are at least equivalent to grafts, and, in some cases, generate superior results. Nerve transfer eliminates the major issues associated with poor clinical results (proximal injuries with long target end-organ distances, delayed repair, sensorimotor topographical mismatching, nerve repair tension, or for nerve graft 2 coaptation sites and cellular changes in long grafts that inhibit nerve regeneration).6 The reconstruction approach requires a comprehensive preoperative and intraoperative assessment and consideration of patient and injury factors.29 Selection of the reconstruction should include consideration of the immediate functional needs, potential future reconstruction and a combination of different surgical options may be optimal. We acknowledge the low response rate with the surgeon survey and this is not unique for a physician survey. Low response rates have the potential for response bias and previous studies have evaluated methods to increase survey response.30 Because surgeons represent a relatively homogeneous sample, the sample in this study is likely representative of the population sampled. Therefore, the results from the surgeon survey can be generalized to the current practice and management of nerve injuries.
Optimal outcome following nerve injury may involve a combination of different surgical options and more than one type of reconstruction. Nerve transfer is a logical extension of the paradigm shift from nerve repair and nerve graft and offers a new rung on the reconstruction ladder.
Supplementary Material
Footnotes
Published online 25 June 2019.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
Supplemental digital content is available for this article. Clickable URL citations appear in the text.
REFERENCES
- 1.Mackinnon SE. Future perspectives in the management of nerve injuries. J Reconstr Microsurg. 2018;34:672–674. [DOI] [PubMed] [Google Scholar]
- 2.Spinner RJ. Book review: Nerve Surgery, by Mackinnon, S. E. Neurosurgery. 2017;81:380–381. [Google Scholar]
- 3.Johnson S. Where Good Ideas Come From: The Natural History of Innovation. 2011New York, NY: Riverhead Books. [Google Scholar]
- 4.Ali ZS, Heuer GG, Faught RW, et al. Upper brachial plexus injury in adults: comparative effectiveness of different repair techniques. J Neurosurg. 2015;122:195–201. [DOI] [PubMed] [Google Scholar]
- 5.Poppler LH, Ee X, Schellhardt L, et al. Axonal growth arrests after an increased accumulation of Schwann cells expressing senescence markers and stromal cells in acellular nerve allografts. Tissue Eng Part A. 2016;22:949–961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Saheb-Al-Zamani M, Yan Y, Farber SJ, et al. Limited regeneration in long acellular nerve allografts is associated with increased Schwann cell senescence. Exp Neurol. 2013;247:165–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yang LJ, Chang KW, Chung KC. A systematic review of nerve transfer and nerve repair for the treatment of adult upper brachial plexus injury. Neurosurgery. 2012;71:417–429; discussion 429. [DOI] [PubMed] [Google Scholar]
- 8.Garg R, Merrell GA, Hillstrom HJ, et al. Comparison of nerve transfers and nerve grafting for traumatic upper plexus palsy: a systematic review and analysis. J Bone Joint Surg Am. 2011;93:819–829. [DOI] [PubMed] [Google Scholar]
- 9.Koshy JC, Agrawal NA, Seruya M. Nerve transfer versus interpositional nerve graft reconstruction for posttraumatic, isolated axillary nerve injuries: a systematic review. Plast Reconstr Surg. 2017;140:953–960. [DOI] [PubMed] [Google Scholar]
- 10.Socolovsky M, Martins RS, Di Masi G, et al. Upper brachial plexus injuries: grafts vs ulnar fascicle transfer to restore biceps muscle function. Neurosurgery. 2012;71(2 Suppl Operative):ons227–ons232. [DOI] [PubMed] [Google Scholar]
- 11.Bhandari PS, Deb P. Management of isolated musculocutaneous injury: comparing double fascicular nerve transfer with conventional nerve grafting. J Hand Surg Am. 2015;40:2003–2006. [DOI] [PubMed] [Google Scholar]
- 12.Wolfe SW, Johnsen PH, Lee SK, et al. Long-nerve grafts and nerve transfers demonstrate comparable outcomes for axillary nerve injuries. J Hand Surg Am. 2014;39:1351–1357. [DOI] [PubMed] [Google Scholar]
- 13.Baltzer HL, Kircher MF, Spinner RJ, et al. A comparison of outcomes of triceps motor branch-to-axillary nerve transfer or sural nerve interpositional grafting for isolated axillary nerve injury. Plast Reconstr Surg. 2016;138:256e–264e. [DOI] [PubMed] [Google Scholar]
- 14.Malessy MJ, de Ruiter GC, de Boer KS, et al. Evaluation of suprascapular nerve neurotization after nerve graft or transfer in the treatment of brachial plexus traction lesions. J Neurosurg. 2004;101:377–389. [DOI] [PubMed] [Google Scholar]
- 15.Flores LP. Comparative study of nerve grafting versus distal nerve transfer for treatment of proximal injuries of the ulnar nerve. J Reconstr Microsurg. 2015;31:647–653. [DOI] [PubMed] [Google Scholar]
- 16.Baltzer H, Woo A, Oh C, et al. Comparison of ulnar intrinsic function following supercharge end-to-side anterior interosseous-to-ulnar motor nerve transfer: a matched cohort study of proximal ulnar nerve injury patients. Plast Reconstr Surg. 2016;138:1264–1272. [DOI] [PubMed] [Google Scholar]
- 17.Sallam AA, El-Deeb MS, Imam MA. Nerve transfer versus nerve graft for reconstruction of high ulnar nerve injuries. J Hand Surg Am. 2017;42:265–273. [DOI] [PubMed] [Google Scholar]
- 18.Hu CH, Chang TN, Lu JC, et al. Comparison of surgical strategies between proximal nerve graft and/or nerve transfer and distal nerve transfer based on functional restoration of elbow flexion: a retrospective review of 147 patients. Plast Reconstr Surg. 2018;141:68e–79e. [DOI] [PubMed] [Google Scholar]
- 19.Terzis JK, Barmpitsioti A. Axillary nerve reconstruction in 176 posttraumatic plexopathy patients. Plast Reconstr Surg. 2010;125:233–247. [DOI] [PubMed] [Google Scholar]
- 20.Ray WZ, Kasukurthi R, Yee A, et al. Functional recovery following an end to side neurorrhaphy of the accessory nerve to the suprascapular nerve: case report. Hand (N Y). 2010;5:313–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bahm J, Noaman H, Becker M. The dorsal approach to the suprascapular nerve in neuromuscular reanimation for obstetric brachial plexus lesions. Plast Reconstr Surg. 2005;115:240–244. [PubMed] [Google Scholar]
- 22.Colbert SH, Mackinnon S. Posterior approach for double nerve transfer for restoration of shoulder function in upper brachial plexus palsy. Hand (N Y). 2006;1:71–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fox IK. Nerve transfers in tetraplegia. Hand Clin. 2016;32:227–242. [DOI] [PubMed] [Google Scholar]
- 24.Mackinnon SE, Yee A, Ray WZ. Nerve transfers for the restoration of hand function after spinal cord injury. J Neurosurg. 2012;117:176–185. [DOI] [PubMed] [Google Scholar]
- 25.Mackinnon SE, Novak CB. Nerve transfers. New options for reconstruction following nerve injury. Hand Clin. 1999;15:643–66, ix. [PubMed] [Google Scholar]
- 26.Davidge KM, Yee A, Moore AM, et al. The supercharge end-to-side anterior interosseous-to-ulnar motor nerve transfer for restoring intrinsic function: clinical experience. Plast Reconstr Surg. 2015;136:344e–352e. [DOI] [PubMed] [Google Scholar]
- 27.Ray WZ, Mackinnon SE. Clinical outcomes following median to radial nerve transfers. J Hand Surg Am. 2011;36:201–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kuhn TS. The Structure of Scientific Revolutions. 19963rd ed Chicago and London: University of Chicago Press. [Google Scholar]
- 29.Mackinnon SE. Donor distal, recipient proximal and other personal perspectives on nerve transfers. Hand Clin. 2016;32:141–151. [DOI] [PubMed] [Google Scholar]
- 30.Kellerman SE, Herold J. Physician response to surveys. A review of the literature. Am J Prev Med. 2001;20:61–67. [DOI] [PubMed] [Google Scholar]



