Summary:
Femoral artery reconstructive operations pose the risk of damage to the lymphatic system and leakage of lymph fluid into the groin. This leakage establishes a stagnant reservoir of protein-rich fluid, further placing the patient at risk for complications, especially a higher infection rate. The use of SPY technology (Stryker Corp/Novadaq Technologies, Kalamazoo, Mich) for lymphatic leaks have been described in previous studies. However, the management of persistent high-output lymphatic leaks addressed secondarily with SPY lymphangiography have yet to be reported. This case report describes a young male who underwent thrombectomy in the left common femoral artery, who presented several days later with a high-output chylous leak. The lymphatic leak was initially managed and failed conventional muscle flaps, and SPY lymphangiography was performed to manage the lymphatic leak during the secondary surgery. The lymphatic vessels were ligated and confirmed with SPY lymphangiography. The management of lymphatic groin complications aided by the use of SPY lymphangiography provided valuable data and allowed for better intraoperative visualization. Utilization of SPY technology allowed the surgeons to properly address all sites of leakage in an otherwise persistent lymphatic leak. Resolution of lymphatic leak was further confirmed with SPY. Lymphatic complications, particularly those in the groin area, are of significant concern to physicians. Any suspected chylous leak should be followed with SPY lymphangiography to ensure proper treatment and resolution. Prophylactic use of SPY technology in high-risk patients during lymphatic surgery of the groin may also be considered.
Disruption of the lymphatic system during lymphadenectomies, infrainguinal reconstructions, or aortic aneurysm repairs is a well-documented postoperative complication, which can lead to lymphedema or lymphatic fistulas.1 Leakage of lymphatic fluid can result in loss of fluid, triglycerides, lymphocytes, immunoglobulins, resulting in dehydration, nutritional deficiency, longer hospital stays, and increased infection rate.2,3 These complications often cause prolonged hospital stays and increased costs to the healthcare system. Despite recommendations of a stepwise approach from conservative management to surgical intervention, studies have shown superior outcomes in patients who return to the operating room immediately.4 In surgical management, visualization of damaged lymphatic channels is paramount to correction of persistent lymphatic leaks. In this manuscript, we describe the use of SPY Elite laser angiographic system (Stryker Corp/Novadaq Technologies, Kalamazoo, Mich.) for lymphatic mapping after conservative measures have failed.
CLINICAL REPORT
A 24-year-old male with medical history significant for congestive heart failure and nonischemic cardiomyopathy presented to an outside hospital with left lower extremity pain and underwent open thrombectomy of his left common femoral artery. Several days later, he presented with increased output from his groin incision. CT confirmed left groin seroma due to a suspected lymphatic leak. Vascular surgery evaluated the patient intraoperatively using isosulfan blue and was unable to visualize any overt lymphatic leak. Plastic surgery reconstructed the wound bed with a sartorius muscle flap. Patient was discharged from the hospital on postoperative day (POD) 7. At his outpatient follow-up appointment on POD 8, patient reported high output of 1000 mL per day with persistent left groin pain and fatigue after ambulation. This output was suspected to be due to an underlying concomitant chronic heart failure.
The patient was brought back to the operating room. The sartorius flap was taken down and the area explored. The presence of a lymphatic leak was confirmed by lymphatic mapping using SPY lymphangiography. Five milliliters of indocyanine green (ICG) was injected into the first toe web space and anterior ankle intradermally. ICG was evident in the wound site within minutes. As the camera moved cephalad, moderate diffuse staining of tissues was identified. In the caudal portion of the wound, individual large lymphatic channel leaks were identified and ligated with small clips, whereas diffuse lymphatic leaks were ligated with the LigaSure Vessel Sealing System (Valleylab, Boulder, Colo.; SDC1, see video, Supplemental Digital Content 1, which displays the areas of leakage, http://links.lww.com/PRSGO/B113). Successful ligation of lymphatic vessels was confirmed visually with SPY. The sartorius flap was sutured back in place. A 15-French drain was placed in the superficial layers. A vacuum-assisted closure (VAC) was placed over the incision at the left groin wound with no air leak noted.
Video Graphic 1.
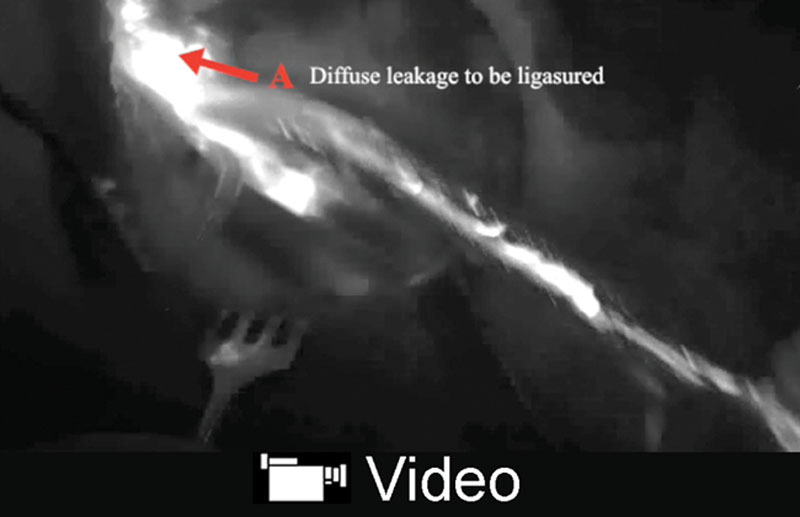
See video, Supplemental Digital Content 1, which displays identification of lymphatic leakage. Using SPY technology, diffuse and more pinpoint lymphatic leakage were identified and appropriately addressed. This video is available in the “Related Videos” section of the Full-Text article at PRSGlobalOpen.com or at http://links.lww.com/PRSGO/B113.
The patient’s postoperative course was complicated by hypotension, cardiogenic shock, and acure kideny injury (AKI), due to his underlying chronic heart failure, which was managed by his medical team. On POD 2, 180 mL of output was noted from the drain and this continued to decrease daily. On POD 7, his drain was pulled due to continuous low output. The wound VAC remained in place and the patient was discharged on POD 22, after hemodynamic stabilization. The patient moved out of state and was last seen in clinic 2-month postoperatively, with minimal output from the wound VAC. Follow-up from his current local team showed the wound healed well with no additional fluid drainage and the wound VAC was removed.
DISCUSSION
Lymphatic injury after femoral arterial reconstruction occurs in approximately 5%–7% of cases and could cause serious complications.5 The use of ICG and SPY in repairing lymphatic injuries have been reported in two similar cases with successful outcomes.6
Traditional lymphangiography is injected in the same manner as ICG but uses isosulfan blue, patent blue V dye, or Lipiodol, which may cause tissue necrosis, fat embolisms, and hypersensitivity reactions. Additionally, traditional dyes make repeating the test difficult due to staining of the wound bed and have a high false-negative rate.7 As described in this case report, the second surgery utilizing SPY lymphangiography led the surgeons to visualize and ligate the areas of leakage. In the senior author’s experience, LigaSure is best used for diffuse areas of leakage, whereas clips are best for areas of localized leakage. SPY lymphangiography provides a more reliable method of visualizing lymphatic flow and can be utilized multiple times for both pre- and postligation and for confirmation. This case has demonstrated SPY to be a useful tool in addressing recalcitrant lymphatic leak.
Some may argue that utilizing SPY technology may be cost prohibitive. However, in recent years, the cost of SPY technology has downtrended dramatically. The cost of employing SPY has been reported to outweigh the hefty cost of complications in skin flap necrosis when utilized in selective high-risk patients.8 This same principle can be applied to patients with lymphatic leaks. High-risk patients can be defined as those, like this patient, with high output, failure of primary procedure, and/or use of synthetic grafts. The presence of synthetic grafts poses a greater risk of infection and complications. Using SPY in this patient group would decrease the risk of complications and reduce the risk of significant morbidity and outweigh the economic costs of managing these complications.
SPY technology has been used in increasing frequency and with proven efficacy to identify lymphatic channels of the upper and lower extremity during lymphatic reconstruction. In our opinion, SPY improves the accuracy of operative techniques during lymphatic leak surgeries. Additionally, in high-risk lymphatic cases, the use of SPY can augment clinical decision making during surgery and could prevent future complications. Our case report demonstrates that SPY lymphangiography can be used to visualize lymphatic leaks, which permitted a successful operation.
SUMMARY
Groin lymphatic complications pose a significant challenge for physicians and patients. SPY technology identifies lymphatic leaks in real time and is an asset in the management of lymphatic leak complications. As seen with this case report, SPY lymphangiography can be used to effectively visualize lymphatic leaks.
Footnotes
Published online 19 June 2019.
Abstract presented as an oral presentation at iSPIES Summit, Las Vegas, September 26, 2015.
Products used for this research are SPY Elite laser angiographic system (Stryker Corp/Novadaq Technologies, Kalamazoo, Mich.) and LigaSure Vessel Sealing System (Valleylab, Boulder, Colo.)
The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by an education grant from Stryker Corp/Novadaq Inc. for SPY Elite laser angiographic system.
REFERENCES
- 1.Kalman PG, Walker PM, Johnston KW. Consequences of groin lymphatic fistulae after vascular reconstruction. Vasc Surg. 1991;25:210–213. [Google Scholar]
- 2.Pan W, Yang C, Cai SY, et al. Incidence and risk factors of chylous ascites after pancreatic resection. Int J Clin Exp Med. 2015;8:4494–4500. [PMC free article] [PubMed] [Google Scholar]
- 3.Hara H, Mihara M, Hayashi A, et al. Therapeutic strategy for lower limb lymphedema and lymphatic fistula after resection of a malignant tumor in the hip joint region: a case report. Microsurgery. 2014;34:224–228. [DOI] [PubMed] [Google Scholar]
- 4.Tyndall SH, Shepard AD, Wilczewski JM, et al. Groin lymphatic complications after arterial reconstruction. J Vasc Surg. 1994;19:858–863. [DOI] [PubMed] [Google Scholar]
- 5.Kwaan JH, Bernstein JM, Connolly JE. Management of lymph fistula in the groin after arterial reconstruction. Arch Surg. 1979;114:1416–1418. [DOI] [PubMed] [Google Scholar]
- 6.Maddox JS, Sabino JM, Buckingham EB, et al. Utility of indocyanine green fluorescence lymphography in identifying the source of persistent groin lymphorrhea. Plast Reconstr Surg Glob Open. 2014;2:e210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee EW, Shin JH, Ko HK, et al. Lymphangiography to treat postoperative lymphatic leakage: a technical review. Korean J Radiol. 2014;15:724–732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kanuri A, Liu AS, Guo L. Whom should we SPY? A cost analysis of laser-assisted indocyanine green angiography in prevention of mastectomy skin flap necrosis during prosthesis-based breast reconstruction. Plast Reconstr Surg. 2014;133:448e–454e. [DOI] [PubMed] [Google Scholar]


